Toxoplasmosis in pregnancy dr Wulan M Soemardji Sp

- Slides: 27
Toxoplasmosis in pregnancy dr. Wulan M. Soemardji, Sp. OG
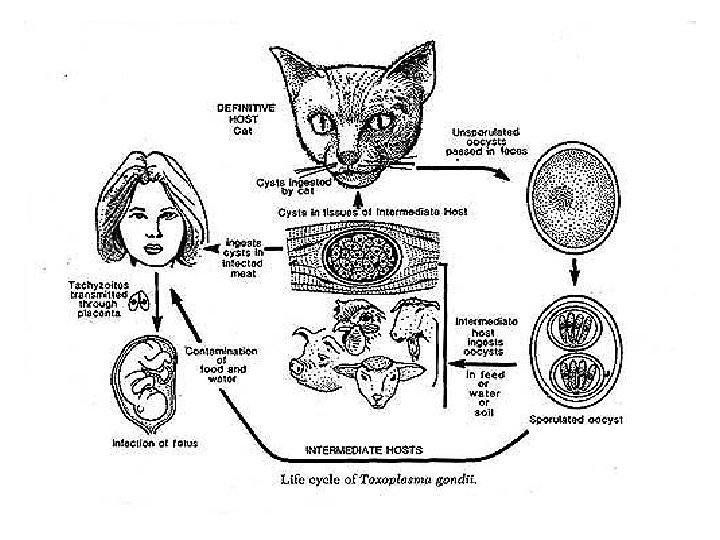
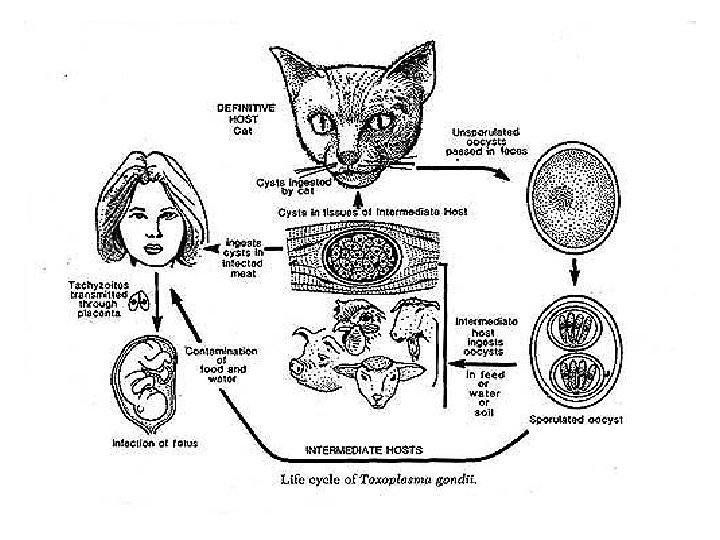
TOXOPLASMOSIS • Parasitic infection • Caused by protozoa: Toxoplasma Gondii exists oin three forms: 1. Trophozoite 2. Tissue cysts 3. Oocysts
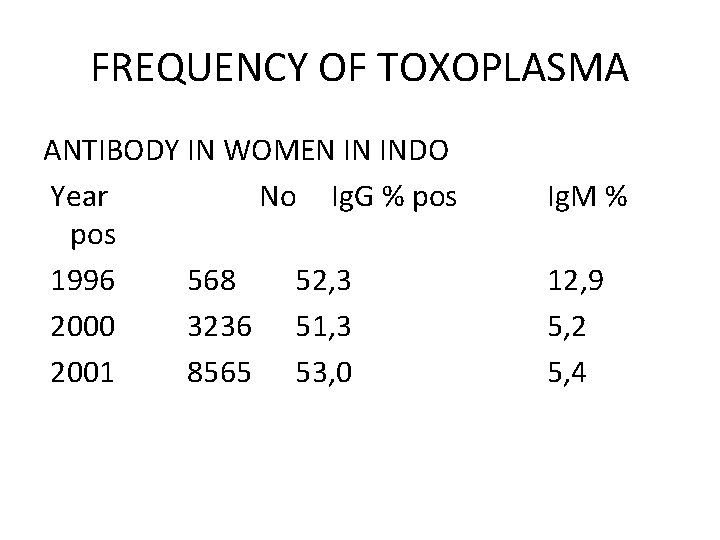
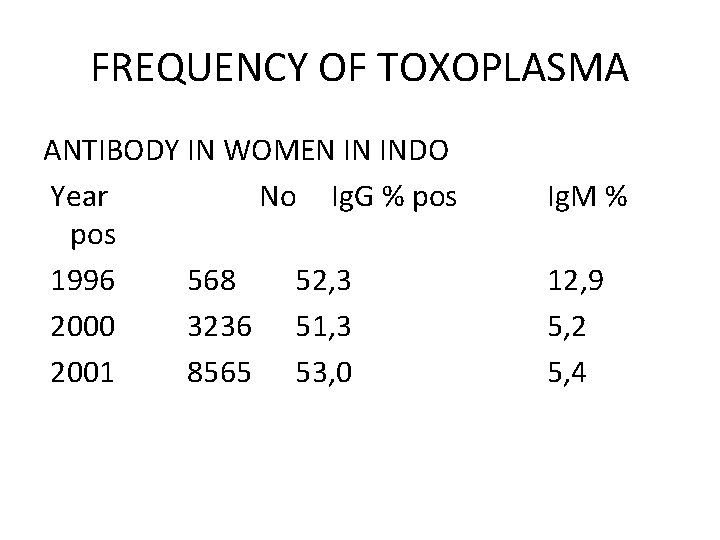
FREQUENCY OF TOXOPLASMA ANTIBODY IN WOMEN IN INDO Year No Ig. G % pos 1996 568 52, 3 2000 3236 51, 3 2001 8565 53, 0 Ig. M % 12, 9 5, 2 5, 4
TOXOPLASMA GONDII Trophozoite: • Requires in intracellular habitat to survive and multiply • Reproduction is endogenous • During the acute phase, it invades every type of cell • After invasion the organisms multiply until cell cytoplasm is so filled that the cell is disrupted
TOXOPLASMA GONDII Tissue cysts: • Formed within the host cells as early as eight day of an acute infection • Probably persist throughout the life of the host • Skeleton, heart muscle and brain are the most common sites for latent infections
TOXOPLASMA GONDII Oocyst: • Produced in the small intestine of the cat • One shed, the oocyte sporulates in 1 to 5 days and become infectious • Under appropriate condition it remain infectiousfor more than 1 year • The parasite transmitted by direct handling of contaminated soil and cat feces • All form of parasite are destroyed by adequate freezing and heating
MATERNAL INFECTION • Transmission of toxoplasma to human occurs through the ingestion of under-cooked meat • Through other foods contaminated with oocyte, or by transfusion of whole blood. • Syndrome including: fatigue, malaise, cervicallymphadenopathy and atypical lymphocytosis • Placental and fetal infection occur during thespreading phase of the parasitemia • Fetal infection 30 -40%, increase with gestational age
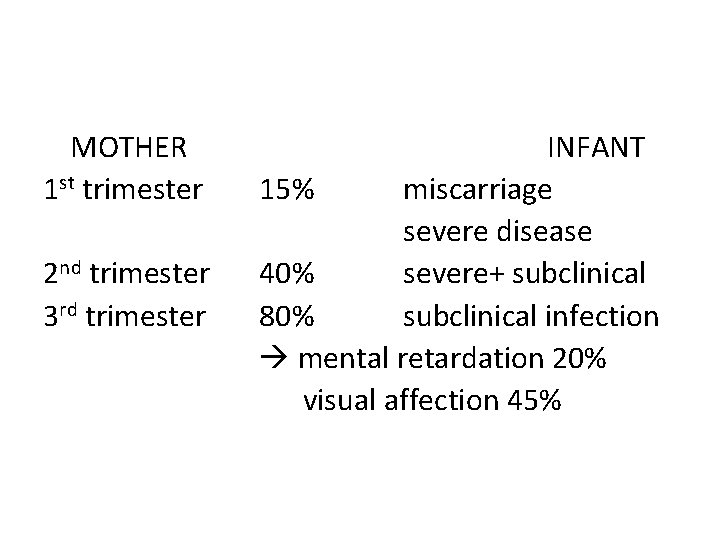
FETAL INFECTION • During 1 st trim, the rate of transmission is approximately 15%, the rate of 2 nd trim is approximately 30 % and 3 rd trim is 60 % • Fetal morbidity and mortality rate are higher afterearly transmission • Infected neonates often have evidence of disease: LBW. Hepatosplenomegaly, icterus, anemia, hydrocephalus, intracranial calcification • Sequelae vision loss, psychomotor and mentalretardation, hearing loss and chorioretinitis

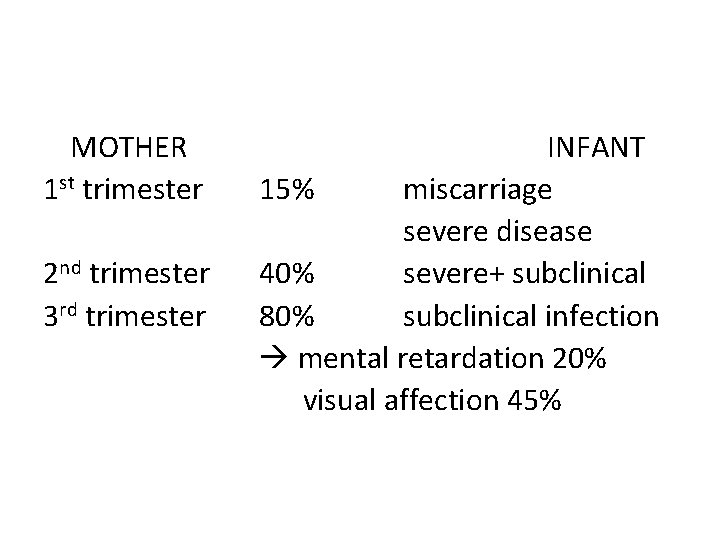
MOTHER 1 st trimester 2 nd trimester 3 rd trimester INFANT 15% miscarriage severe disease 40% severe+ subclinical 80% subclinical infection mental retardation 20% visual affection 45%
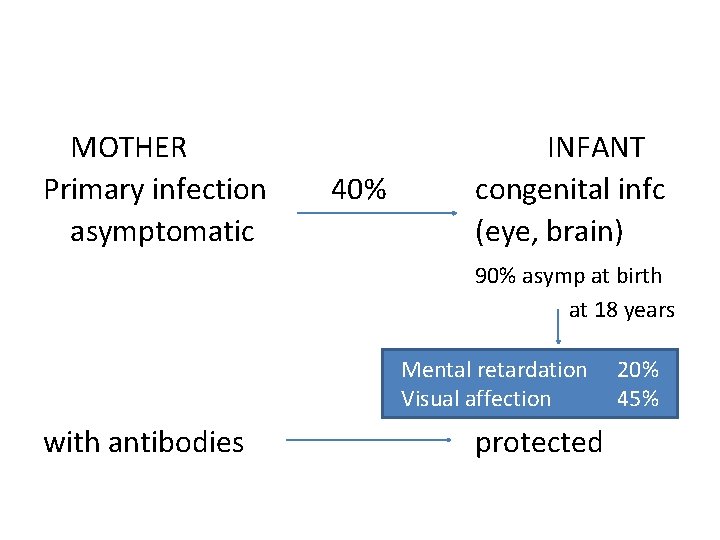
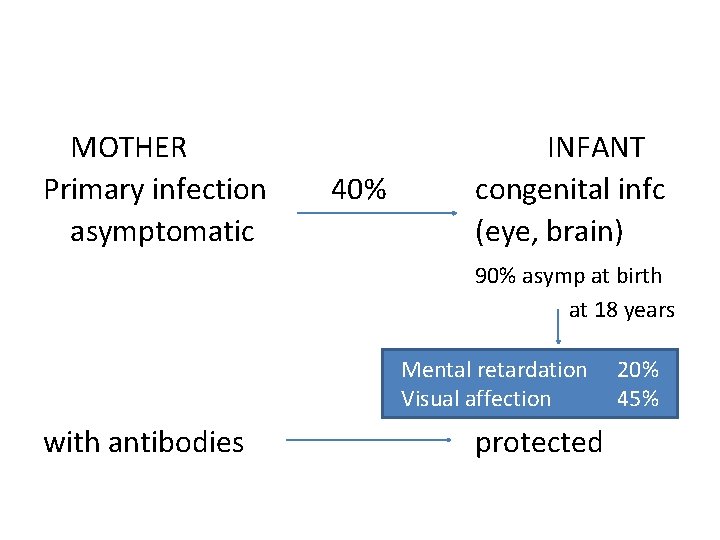
MOTHER Primary infection asymptomatic 40% INFANT congenital infc (eye, brain) 90% asymp at birth at 18 years Mental retardation Visual affection with antibodies protected 20% 45%
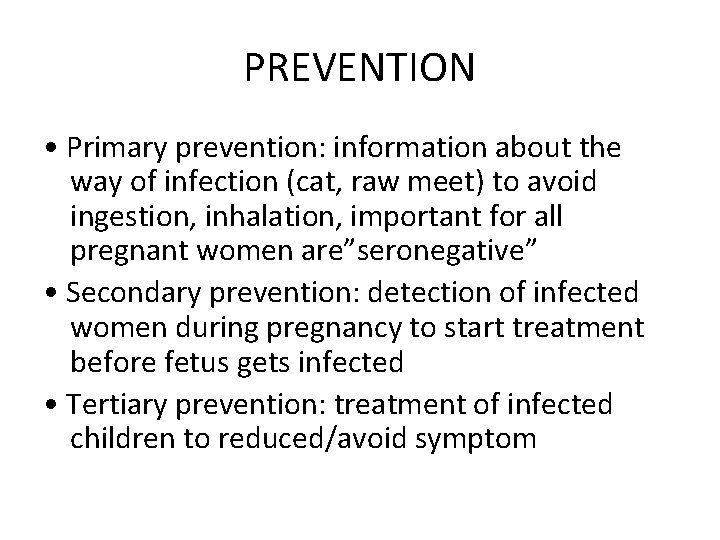
PREVENTION • Primary prevention: information about the way of infection (cat, raw meet) to avoid ingestion, inhalation, important for all pregnant women are”seronegative” • Secondary prevention: detection of infected women during pregnancy to start treatment before fetus gets infected • Tertiary prevention: treatment of infected children to reduced/avoid symptom
HYGIENIC AND DIETITIC EDUCATION • Avoid eating raw or uncooked meat • Wash salads, vegetables, fruits and berries • Have good kitchen hygiene • Avoid contact with cat feces (kittens) • Wash hands after contact with sand soil • Use gloves when gardening
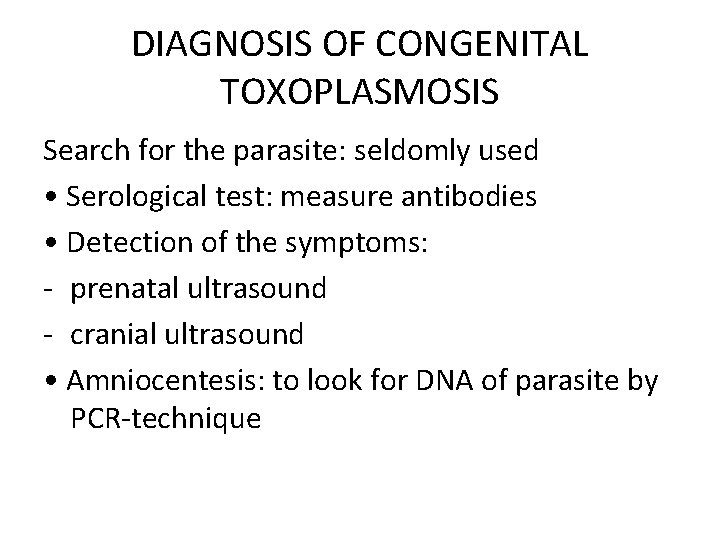
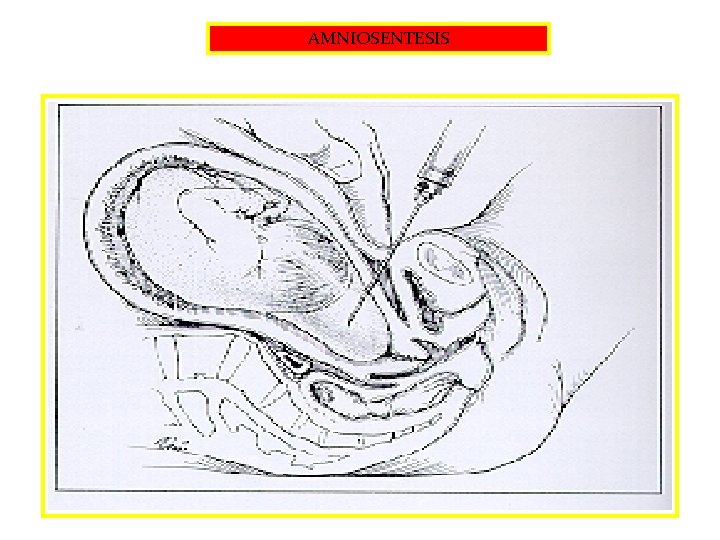
DIAGNOSIS OF CONGENITAL TOXOPLASMOSIS Search for the parasite: seldomly used • Serological test: measure antibodies • Detection of the symptoms: - prenatal ultrasound - cranial ultrasound • Amniocentesis: to look for DNA of parasite by PCR-technique
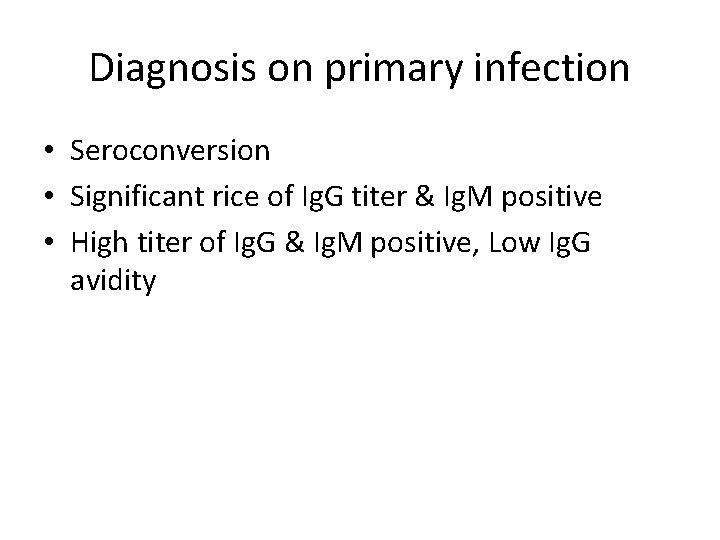
Diagnosis on primary infection • Seroconversion • Significant rice of Ig. G titer & Ig. M positive • High titer of Ig. G & Ig. M positive, Low Ig. G avidity
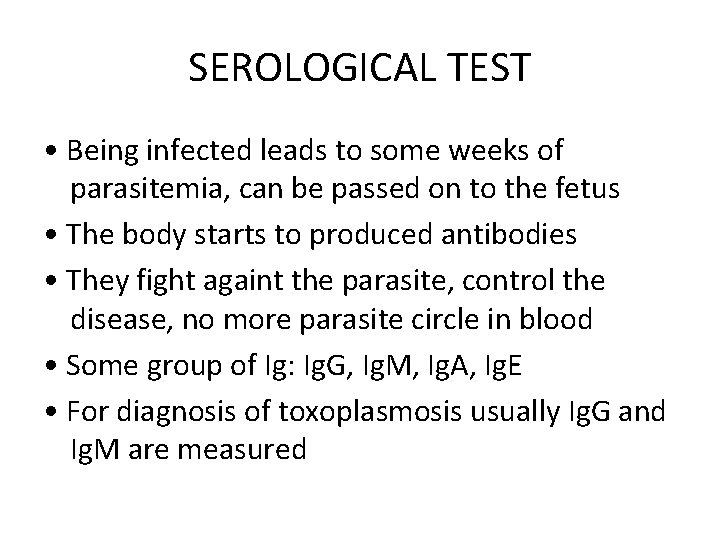
SEROLOGICAL TEST • Being infected leads to some weeks of parasitemia, can be passed on to the fetus • The body starts to produced antibodies • They fight againt the parasite, control the disease, no more parasite circle in blood • Some group of Ig: Ig. G, Ig. M, Ig. A, Ig. E • For diagnosis of toxoplasmosis usually Ig. G and Ig. M are measured
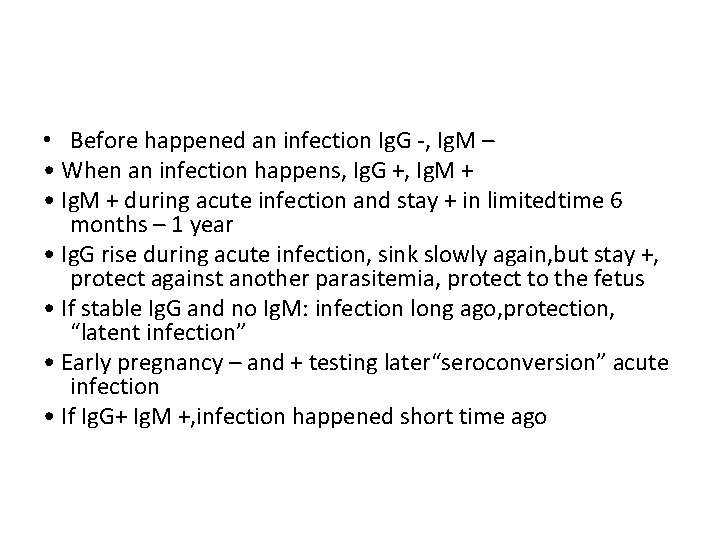
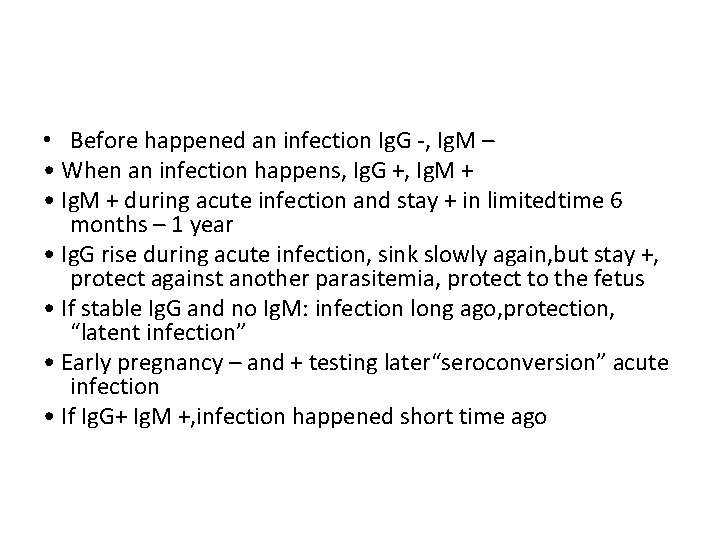
• Before happened an infection Ig. G -, Ig. M – • When an infection happens, Ig. G +, Ig. M + • Ig. M + during acute infection and stay + in limitedtime 6 months – 1 year • Ig. G rise during acute infection, sink slowly again, but stay +, protect against another parasitemia, protect to the fetus • If stable Ig. G and no Ig. M: infection long ago, protection, “latent infection” • Early pregnancy – and + testing later“seroconversion” acute infection • If Ig. G+ Ig. M +, infection happened short time ago
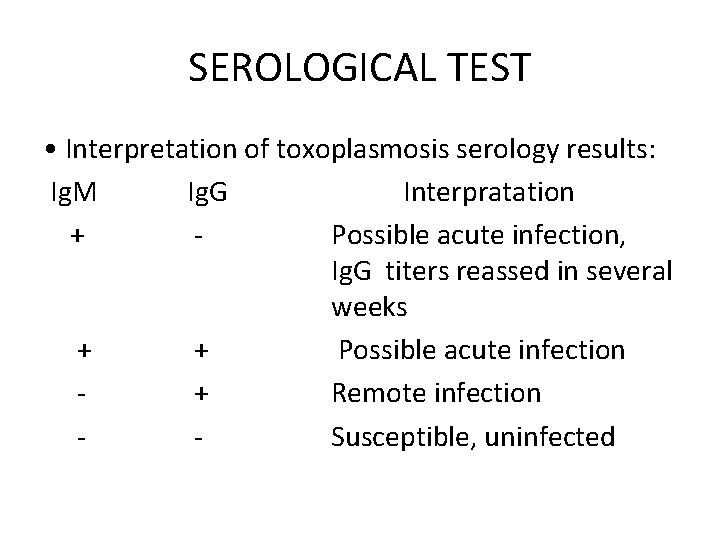
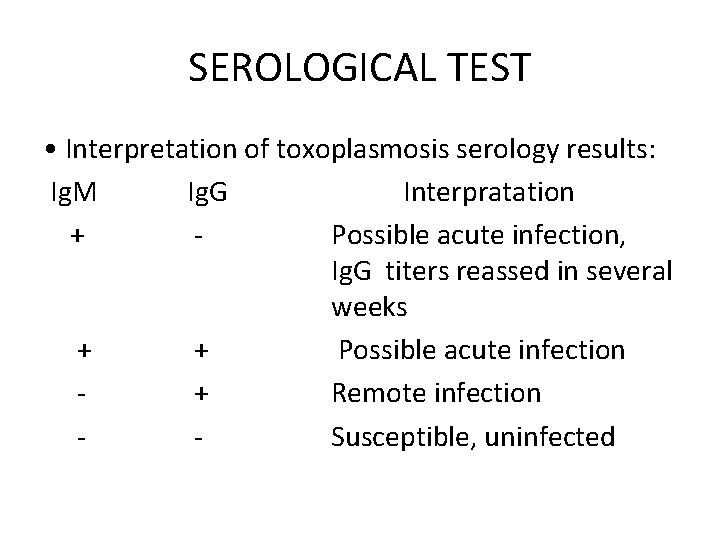
SEROLOGICAL TEST • Interpretation of toxoplasmosis serology results: Ig. M Ig. G Interpratation + Possible acute infection, Ig. G titers reassed in several weeks + + Possible acute infection + Remote infection Susceptible, uninfected
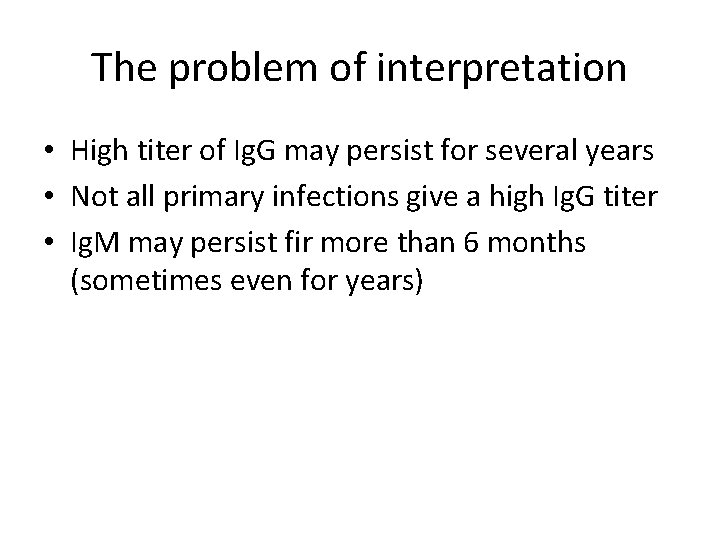
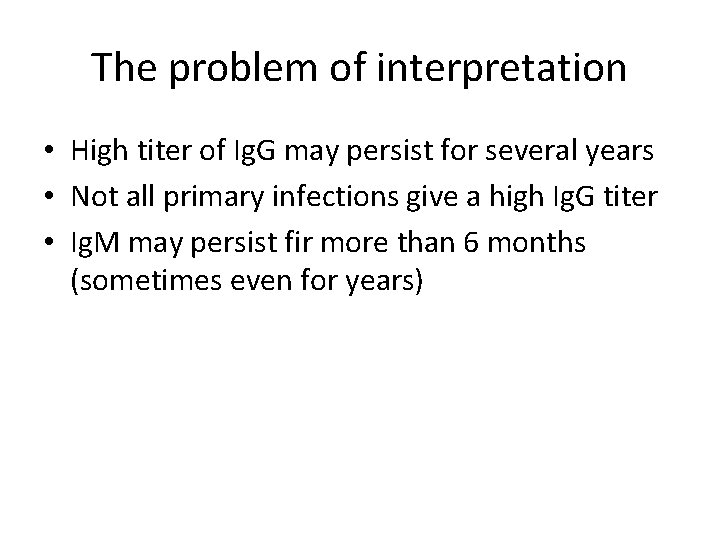
The problem of interpretation • High titer of Ig. G may persist for several years • Not all primary infections give a high Ig. G titer • Ig. M may persist fir more than 6 months (sometimes even for years)
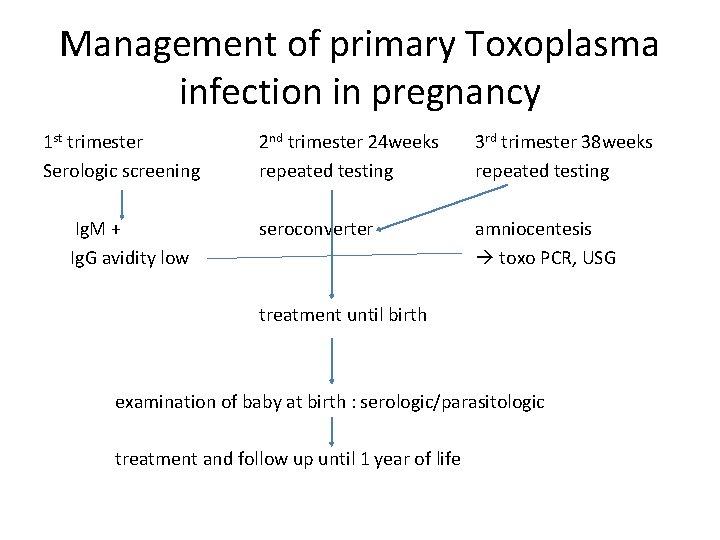
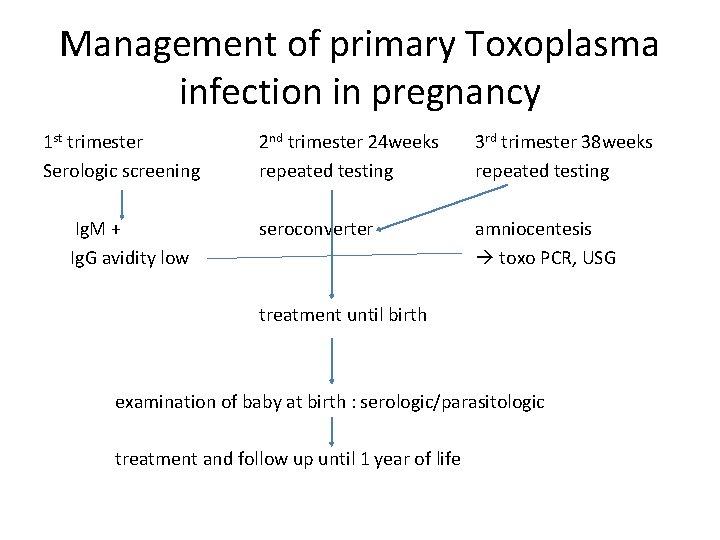
Management of primary Toxoplasma infection in pregnancy 1 st trimester Serologic screening Ig. M + Ig. G avidity low 2 nd trimester 24 weeks repeated testing 3 rd trimester 38 weeks repeated testing seroconverter amniocentesis toxo PCR, USG treatment until birth examination of baby at birth : serologic/parasitologic treatment and follow up until 1 year of life
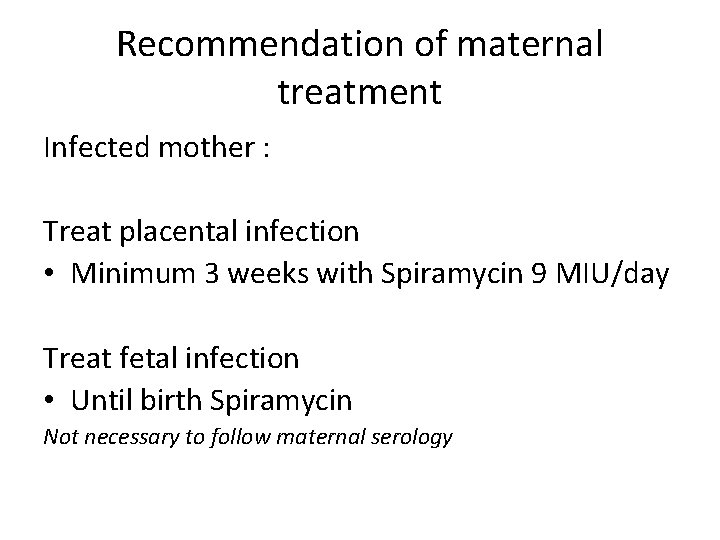
Recommendation of maternal treatment Infected mother : Treat placental infection • Minimum 3 weeks with Spiramycin 9 MIU/day Treat fetal infection • Until birth Spiramycin Not necessary to follow maternal serology
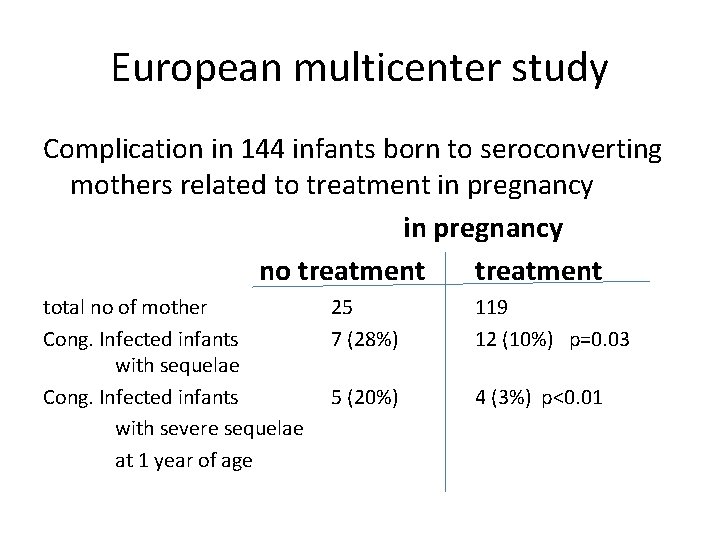
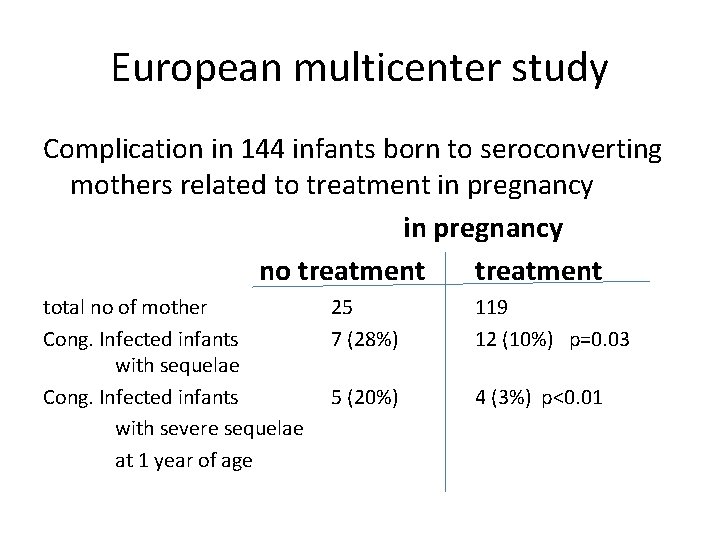
European multicenter study Complication in 144 infants born to seroconverting mothers related to treatment in pregnancy no treatment total no of mother Cong. Infected infants with sequelae Cong. Infected infants with severe sequelae at 1 year of age 25 7 (28%) 119 12 (10%) p=0. 03 5 (20%) 4 (3%) p<0. 01
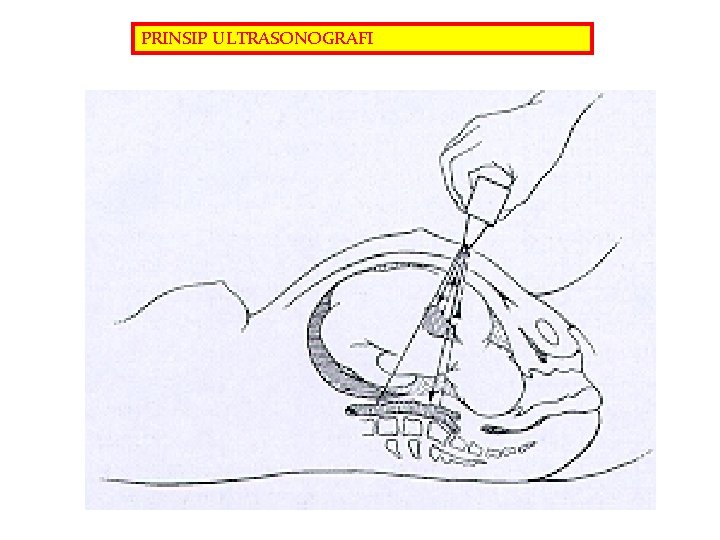
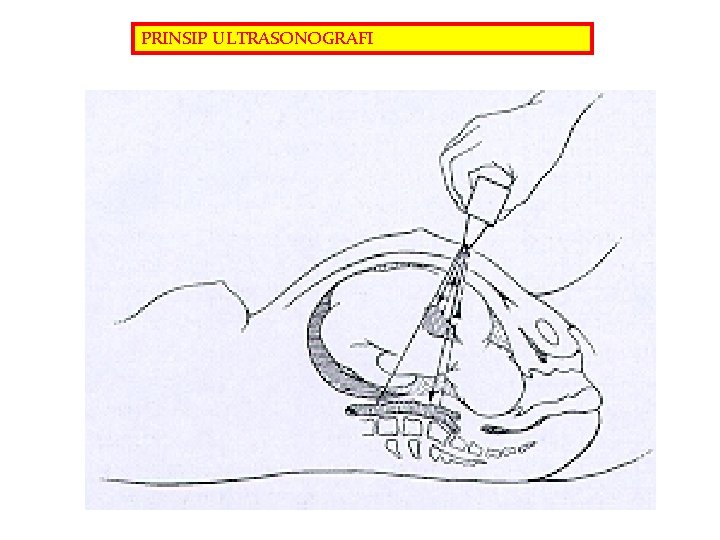
PRINSIP ULTRASONOGRAFI
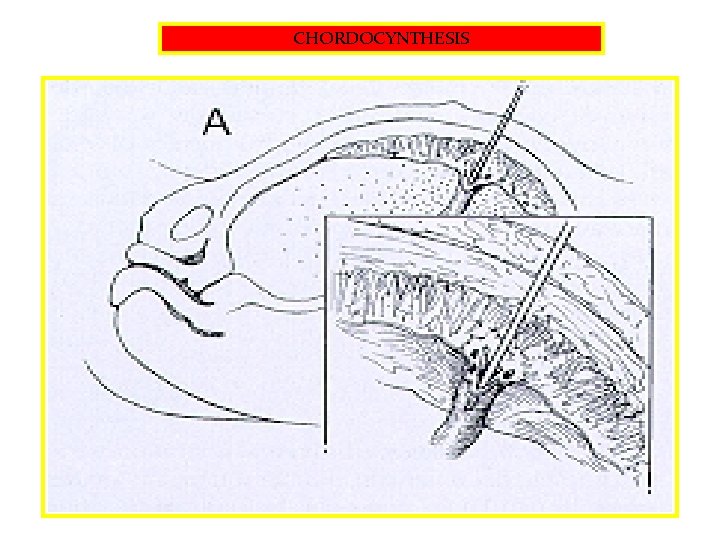
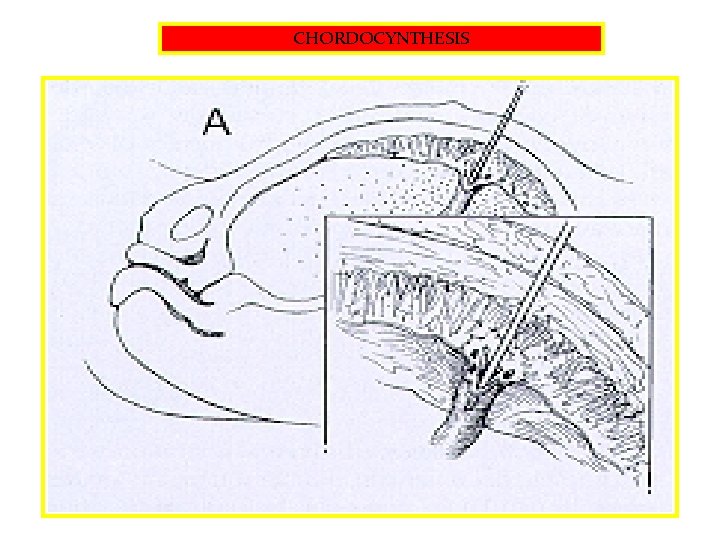
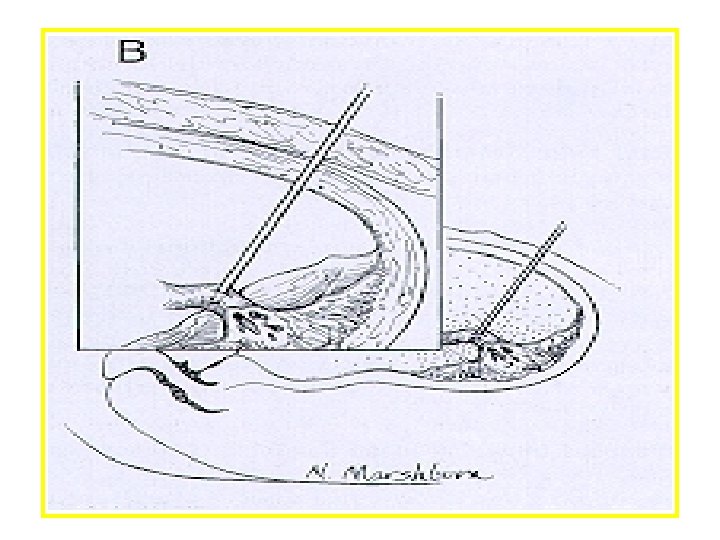
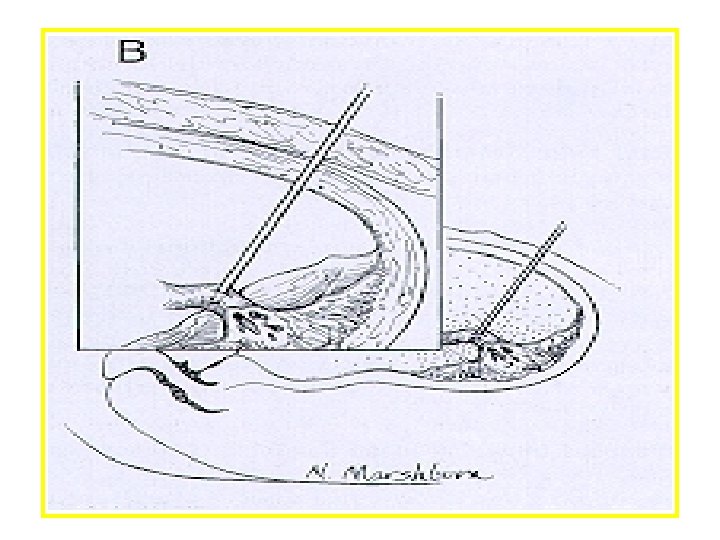
CHORDOCYNTHESIS
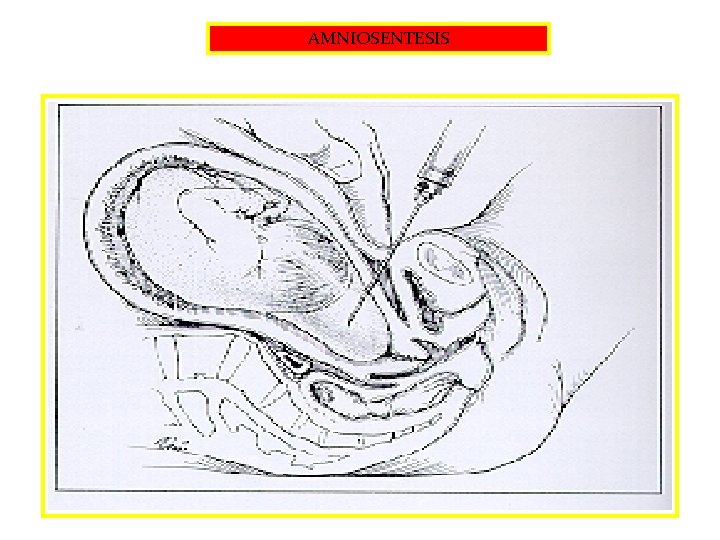
AMNIOSENTESIS