TORTORA FUNKE CASE Microbiology AN INTRODUCTION EIGHTH EDITION
TORTORA • FUNKE • CASE Microbiology AN INTRODUCTION EIGHTH EDITION B. E Pruitt & Jane J. Stein Chapter 21, part A Microbial Diseases of the Skin and Eyes
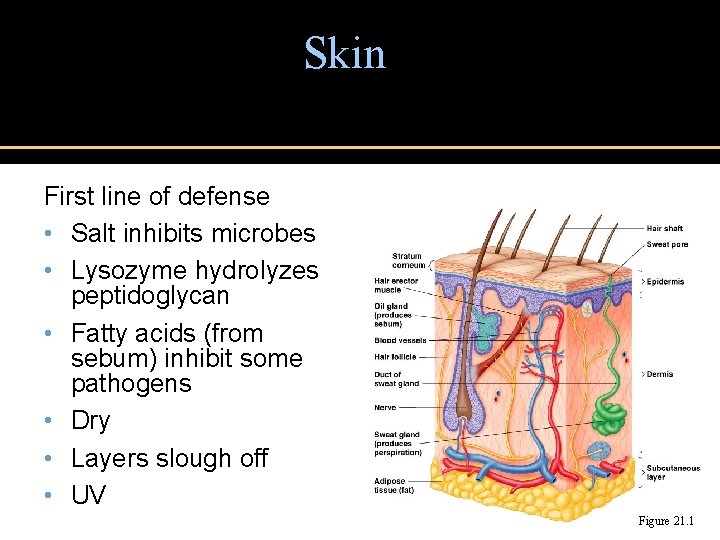
Skin First line of defense • Salt inhibits microbes • Lysozyme hydrolyzes peptidoglycan • Fatty acids (from sebum) inhibit some pathogens • Dry • Layers slough off • UV Figure 21. 1
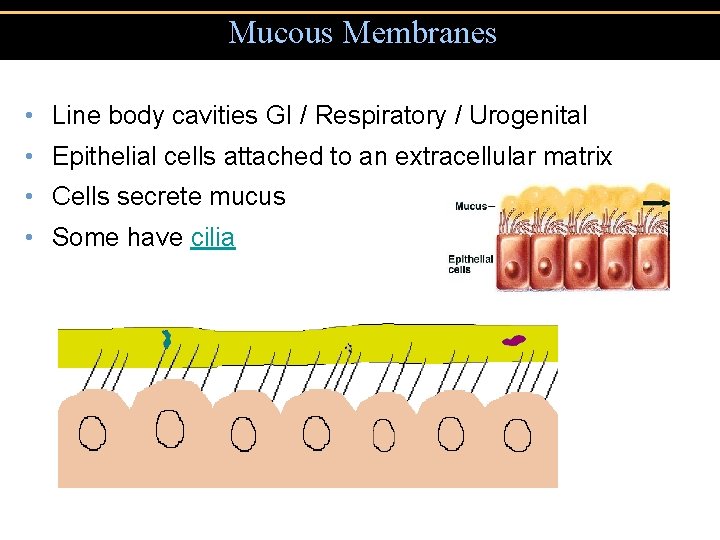
Mucous Membranes • Line body cavities GI / Respiratory / Urogenital • Epithelial cells attached to an extracellular matrix • Cells secrete mucus • Some have cilia
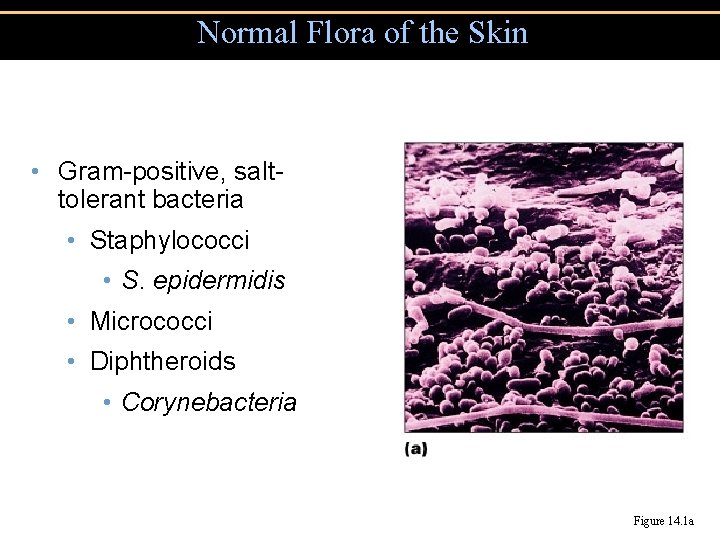
Normal Flora of the Skin • Gram-positive, salttolerant bacteria • Staphylococci • S. epidermidis • Micrococci • Diphtheroids • Corynebacteria Figure 14. 1 a
Normal Microbiota of the Skin • Grow on oils • Aerobes on surface • Corynebacterium xerosis • Anaerobes in hair follicles § Propionibacterium acnes • Yeast • Malassezia furfur
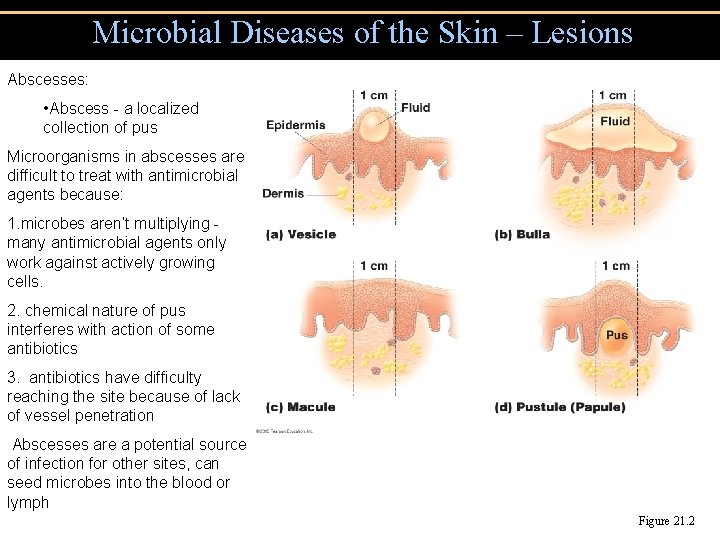
Microbial Diseases of the Skin – Lesions Abscesses: • Abscess - a localized collection of pus Microorganisms in abscesses are difficult to treat with antimicrobial agents because: 1. microbes aren’t multiplying - many antimicrobial agents only work against actively growing cells. 2. chemical nature of pus interferes with action of some antibiotics 3. antibiotics have difficulty reaching the site because of lack of vessel penetration Abscesses are a potential source of infection for other sites, can seed microbes into the blood or lymph Figure 21. 2
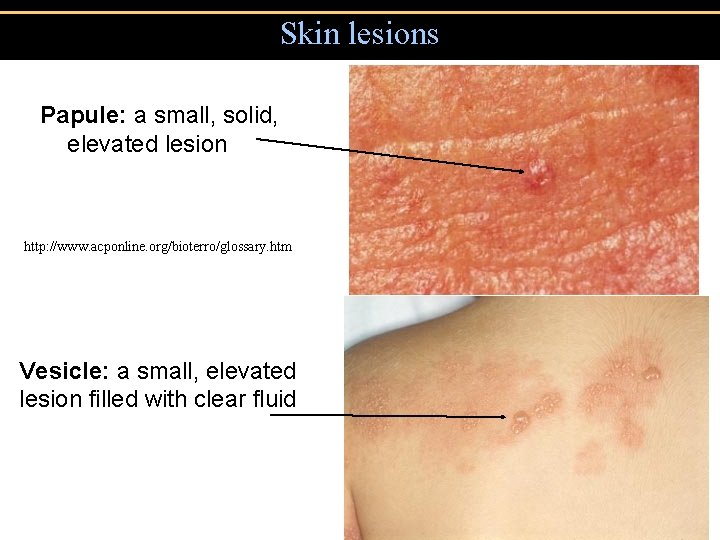
Skin lesions Papule: a small, solid, elevated lesion http: //www. acponline. org/bioterro/glossary. htm Vesicle: a small, elevated lesion filled with clear fluid

Skin lesions • Bullae • Large fluid filled lesion
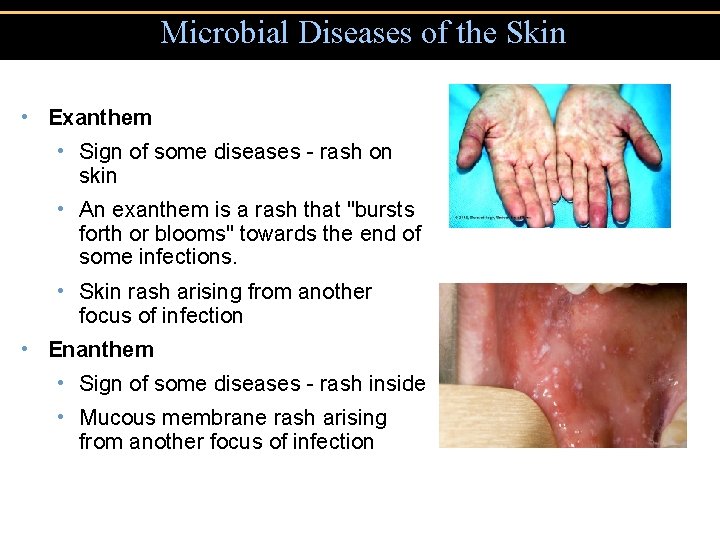
Microbial Diseases of the Skin • Exanthem • Sign of some diseases - rash on skin • An exanthem is a rash that "bursts forth or blooms" towards the end of some infections. • Skin rash arising from another focus of infection • Enanthem • Sign of some diseases - rash inside • Mucous membrane rash arising from another focus of infection
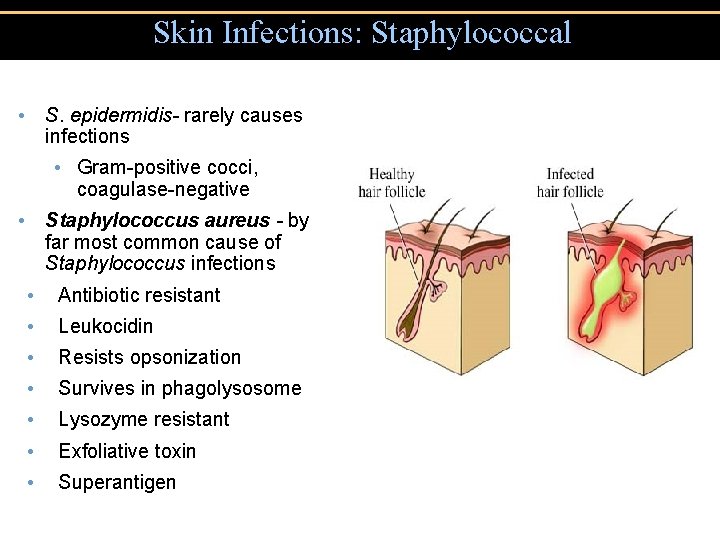
Skin Infections: Staphylococcal • S. epidermidis- rarely causes infections • Gram-positive cocci, coagulase-negative • Staphylococcus aureus - by far most common cause of Staphylococcus infections • Antibiotic resistant • Leukocidin • Resists opsonization • Survives in phagolysosome • Lysozyme resistant • Exfoliative toxin • Superantigen
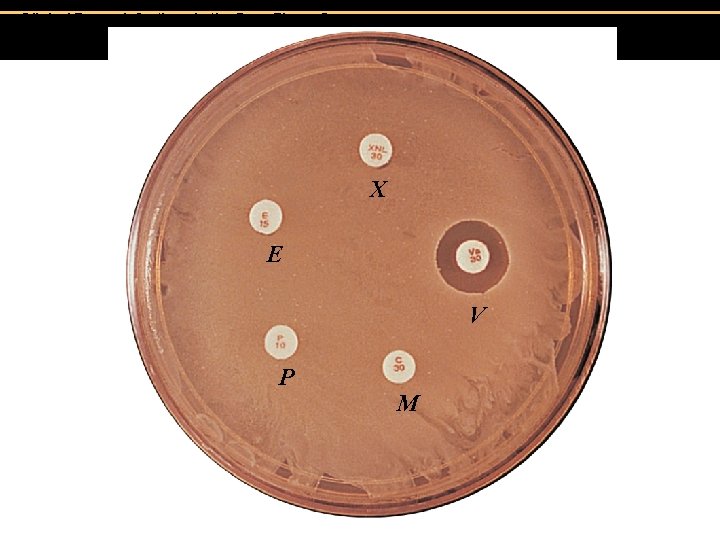
Clinical Focus, Infections in the Gym, Figure C. X E V P M

Staphylococcal Skin Infections Figure 21. 3
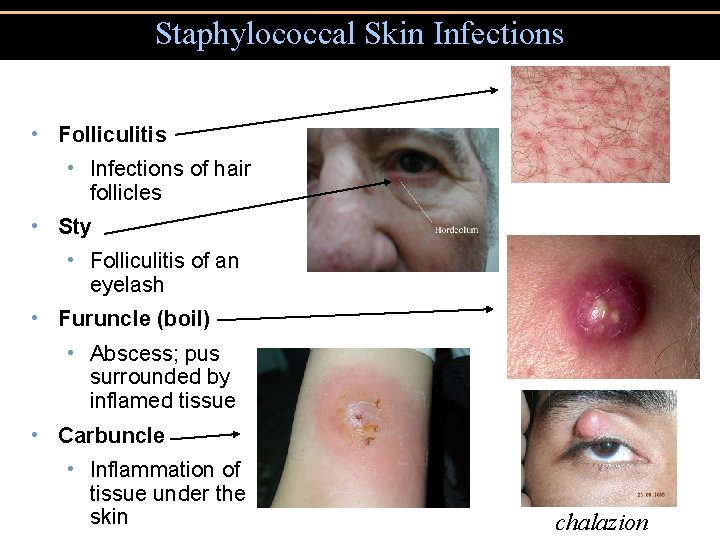
Staphylococcal Skin Infections • Folliculitis • Infections of hair follicles • Sty • Folliculitis of an eyelash • Furuncle (boil) • Abscess; pus surrounded by inflamed tissue • Carbuncle • Inflammation of tissue under the skin chalazion
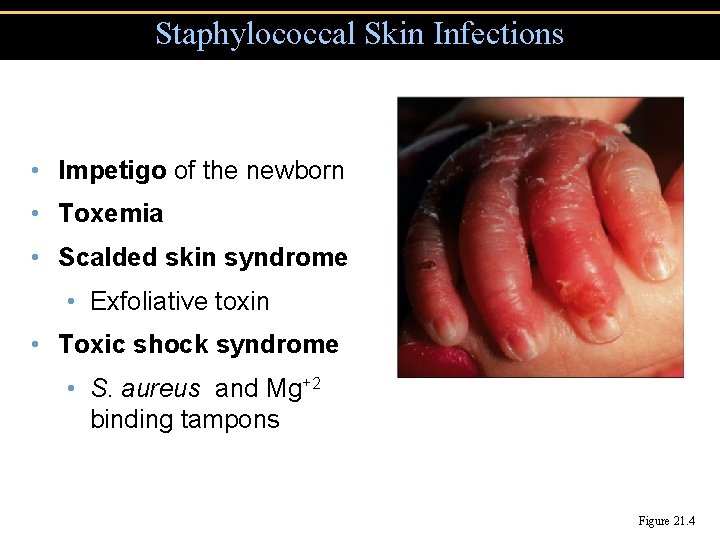
Staphylococcal Skin Infections • Impetigo of the newborn • Toxemia • Scalded skin syndrome • Exfoliative toxin • Toxic shock syndrome • S. aureus and Mg+2 binding tampons Figure 21. 4

Figure 21. 4 Lesions of impetigo. Insert Fig 21. 4
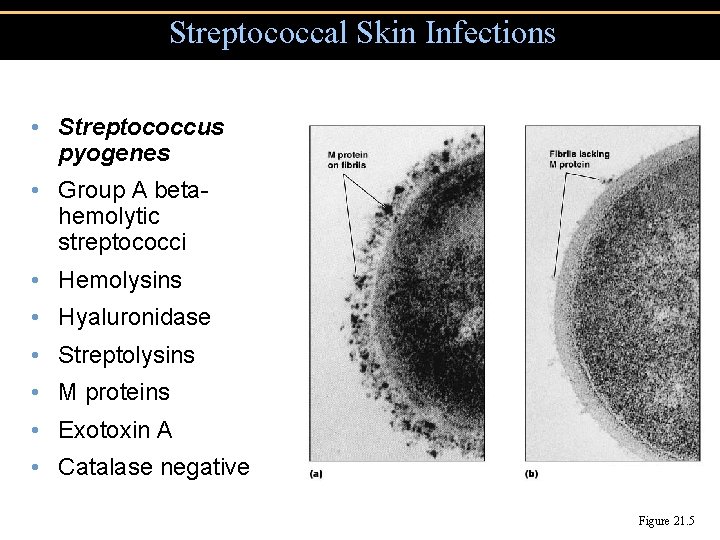
Streptococcal Skin Infections • Streptococcus pyogenes • Group A betahemolytic streptococci • Hemolysins • Hyaluronidase • Streptolysins • M proteins • Exotoxin A • Catalase negative Figure 21. 5
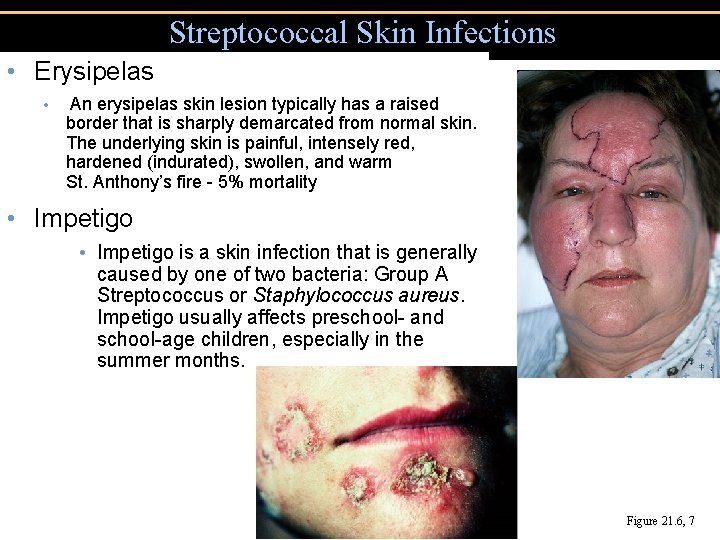
Streptococcal Skin Infections • Erysipelas • An erysipelas skin lesion typically has a raised border that is sharply demarcated from normal skin. The underlying skin is painful, intensely red, hardened (indurated), swollen, and warm St. Anthony’s fire - 5% mortality • Impetigo is a skin infection that is generally caused by one of two bacteria: Group A Streptococcus or Staphylococcus aureus. Impetigo usually affects preschool- and school-age children, especially in the summer months. Figure 21. 6, 7
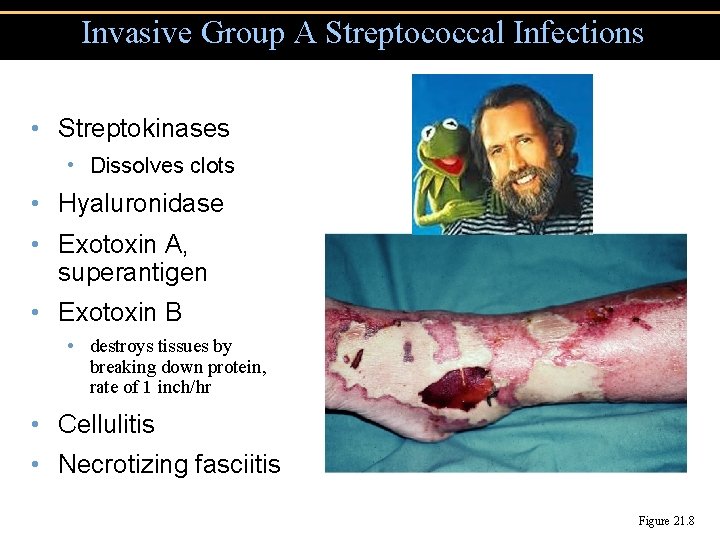
Invasive Group A Streptococcal Infections • Streptokinases • Dissolves clots • Hyaluronidase • Exotoxin A, superantigen • Exotoxin B • destroys tissues by breaking down protein, rate of 1 inch/hr • Cellulitis • Necrotizing fasciitis Figure 21. 8

Figure 21. 7 Lesions of erysipelas, caused by group A beta-hemolytic streptococcal toxins.
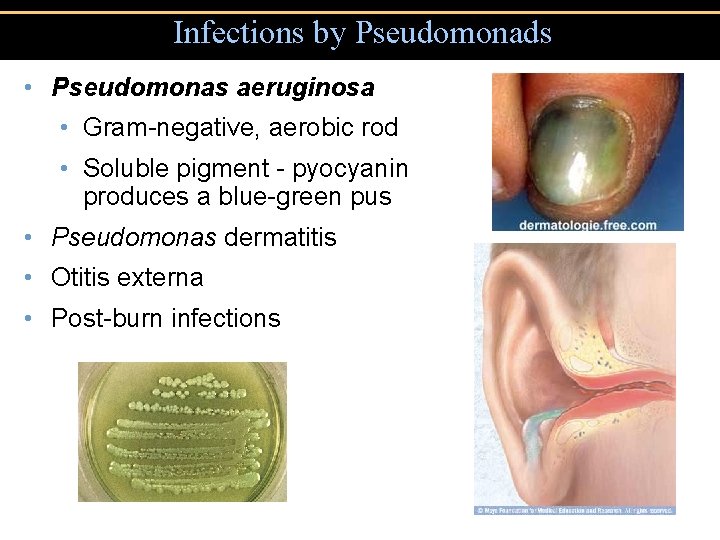
Infections by Pseudomonads • Pseudomonas aeruginosa • Gram-negative, aerobic rod • Soluble pigment - pyocyanin produces a blue-green pus • Pseudomonas dermatitis • Otitis externa • Post-burn infections
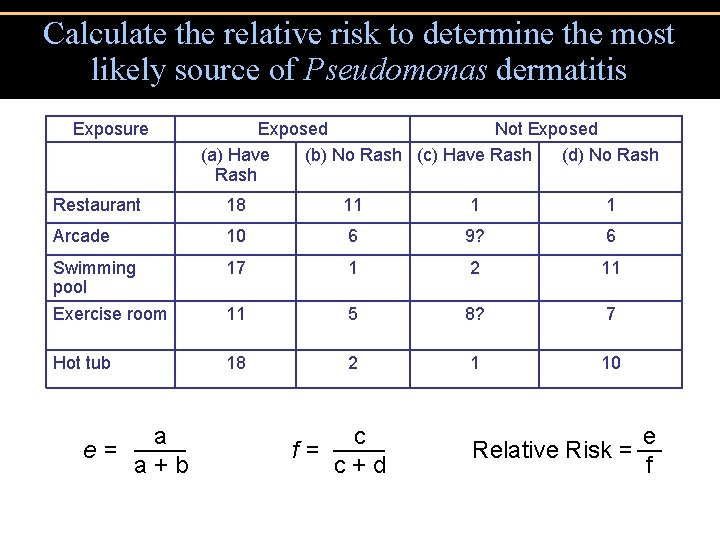
Calculate the relative risk to determine the most likely source of Pseudomonas dermatitis Exposure Exposed Not Exposed (a) Have (b) No Rash (c) Have Rash (d) No Rash Restaurant 18 11 1 1 Arcade 10 6 9? 6 Swimming pool Exercise room 17 1 2 11 11 5 8? 7 Hot tub 18 2 1 10 e= a a + b f= c c + d Relative Risk = e f
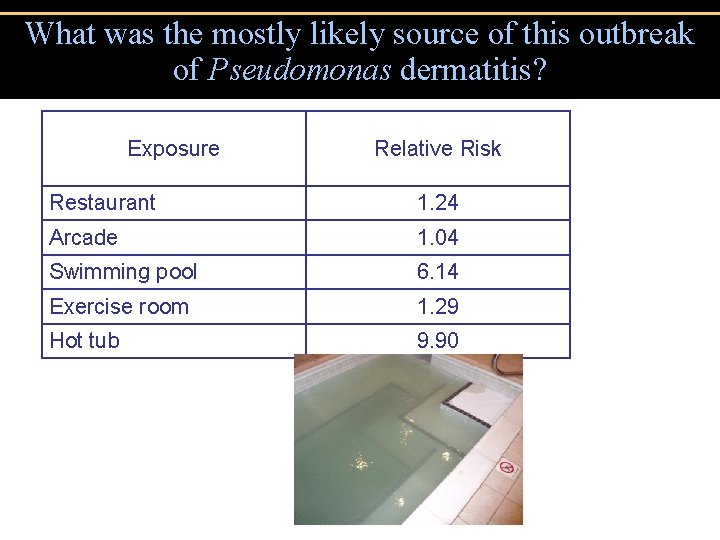
What was the mostly likely source of this outbreak of Pseudomonas dermatitis? Exposure Relative Risk Restaurant 1. 24 Arcade 1. 04 Swimming pool 6. 14 Exercise room 1. 29 Hot tub 9. 90
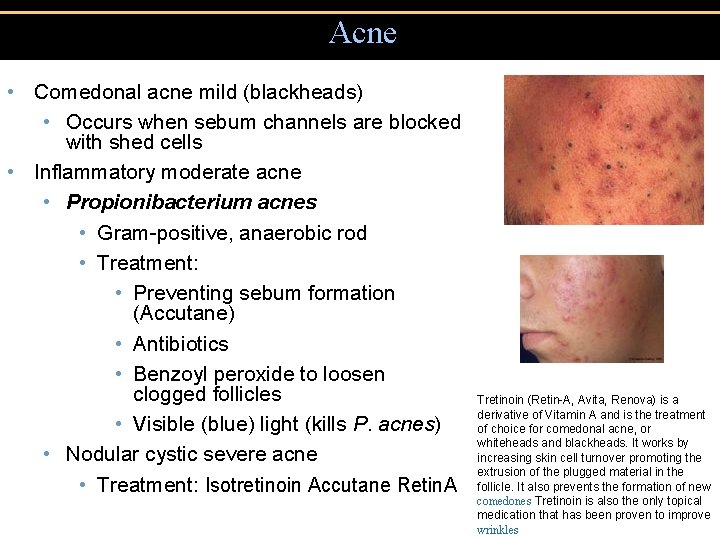
Acne • Comedonal acne mild (blackheads) • Occurs when sebum channels are blocked with shed cells • Inflammatory moderate acne • Propionibacterium acnes • Gram-positive, anaerobic rod • Treatment: • Preventing sebum formation (Accutane) • Antibiotics • Benzoyl peroxide to loosen clogged follicles • Visible (blue) light (kills P. acnes) • Nodular cystic severe acne • Treatment: Isotretinoin Accutane Retin. A Tretinoin (Retin-A, Avita, Renova) is a derivative of Vitamin A and is the treatment of choice for comedonal acne, or whiteheads and blackheads. It works by increasing skin cell turnover promoting the extrusion of the plugged material in the follicle. It also prevents the formation of new comedones Tretinoin is also the only topical medication that has been proven to improve wrinkles
Viral Skin infections: Warts • Papillomaviruses • Treatment: • Removal • Imiquimod Aldara (stimulate interferon production) • Interferon • Laser • Acid • freezing
- Slides: 24