TORCH Infections SAQR ALSAKARNEH Index of Suspicion When


- Slides: 32

TORCH Infections SAQR ALSAKARNEH
Index of Suspicion When do you think of TORCH infections? IUGR infants HSM Thrombocytopenia Unusual rash Concerning maternal history “Classic” findings of any specific infection
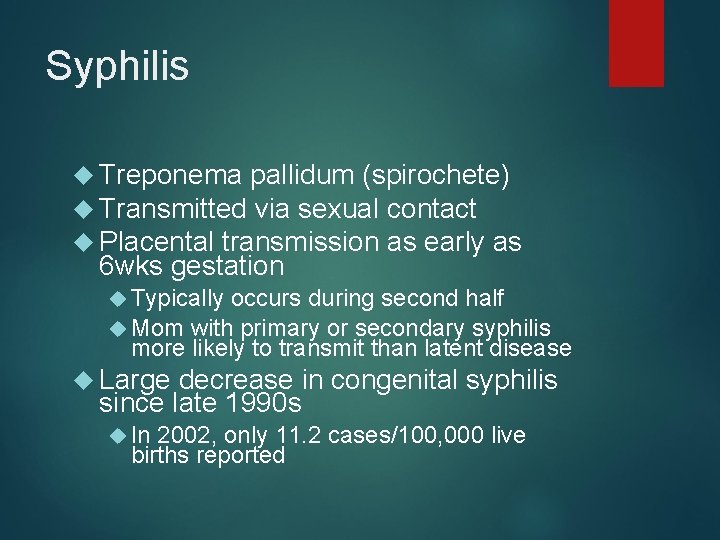
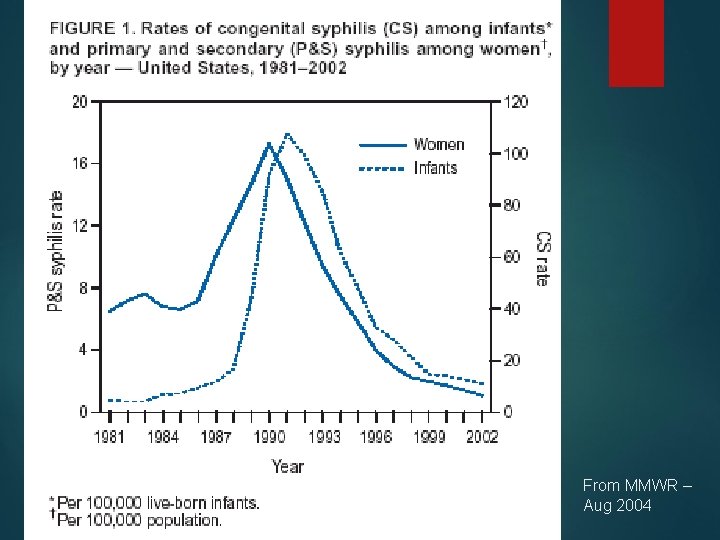
Syphilis Treponema pallidum (spirochete) Transmitted via sexual contact Placental transmission as early as 6 wks gestation Typically occurs during second half Mom with primary or secondary syphilis more likely to transmit than latent disease Large decrease in congenital syphilis since late 1990 s In 2002, only 11. 2 cases/100, 000 live births reported
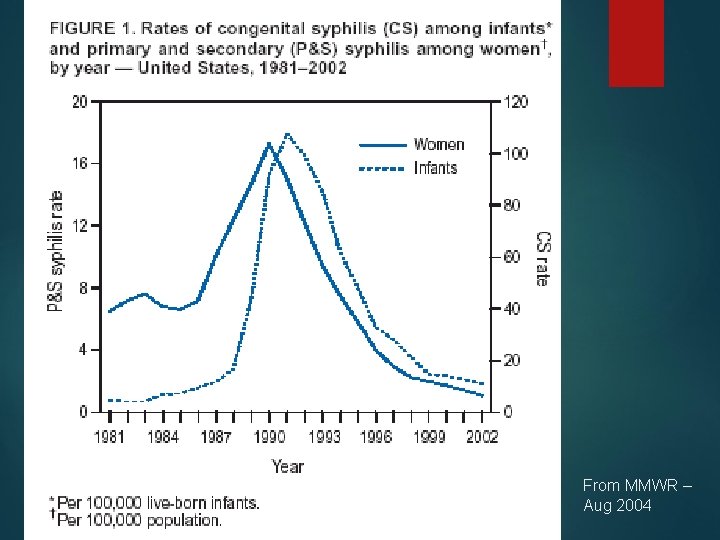
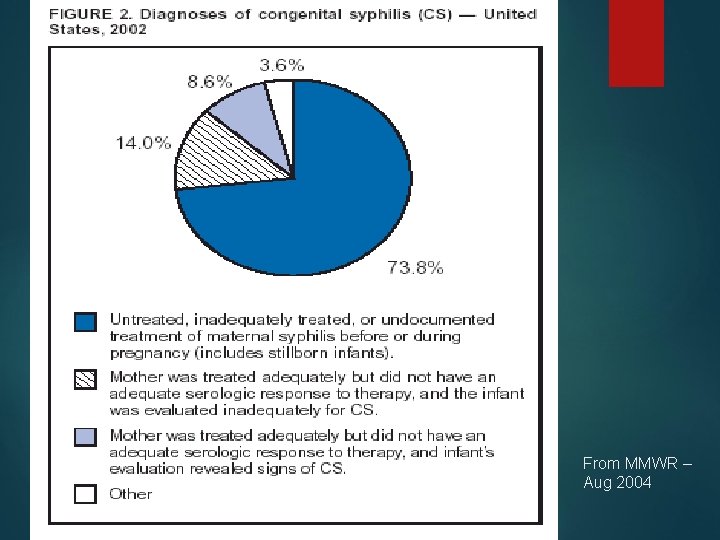
From MMWR – Aug 2004
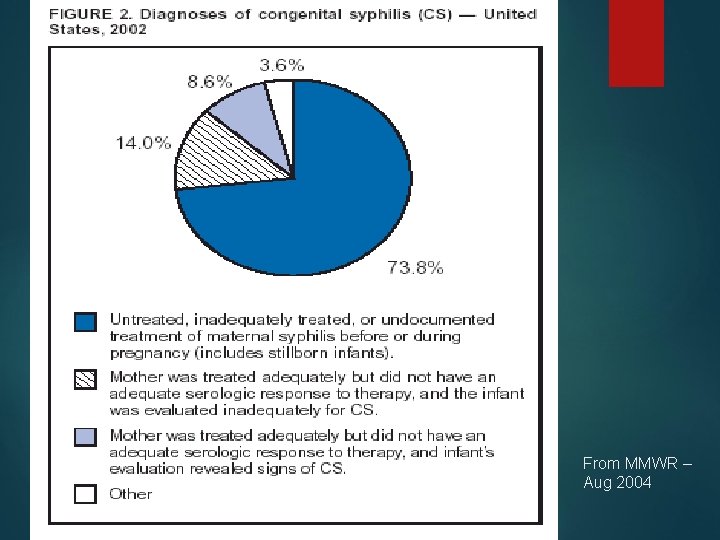
From MMWR – Aug 2004
Congenital Syphilis 2/3 of affected live-born infants are asymptomatic at birth Clinical symptoms split into early or late (2 years is cutoff) 3 major classifications: Fetal effects Early effects Late effects
Clinical Manifestations Fetal: Stillbirth Neonatal death Hydrops fetalis Intrauterine death in 25% Perinatal mortality in 25 -30% if untreated
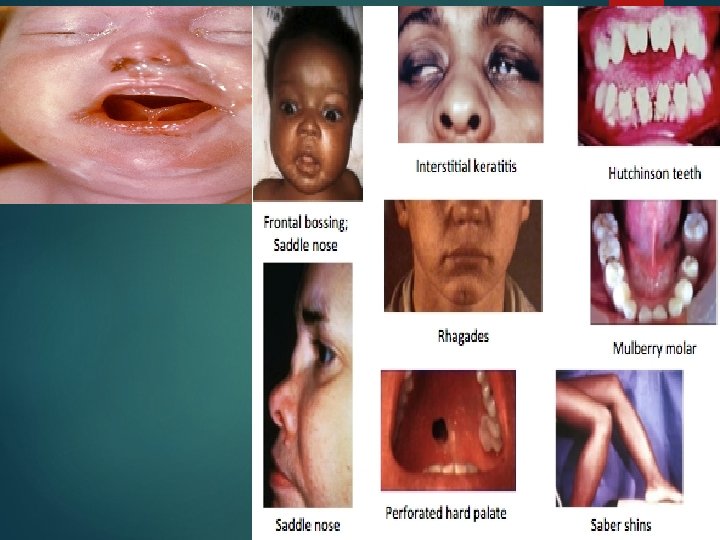
Clinical Manifestations Early congenital (typically 1 st 5 weeks): Cutaneous lesions (palms/soles) HSM Jaundice Anemia Snuffles Periostitis and metaphysial dystrophy Funisitis (umbilical cord vasculitis)

Periostitis of long bones seen in neonatal syphilis
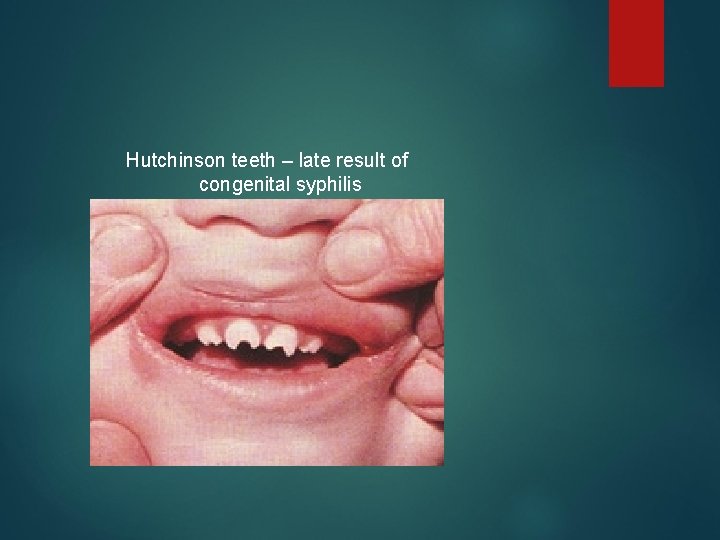
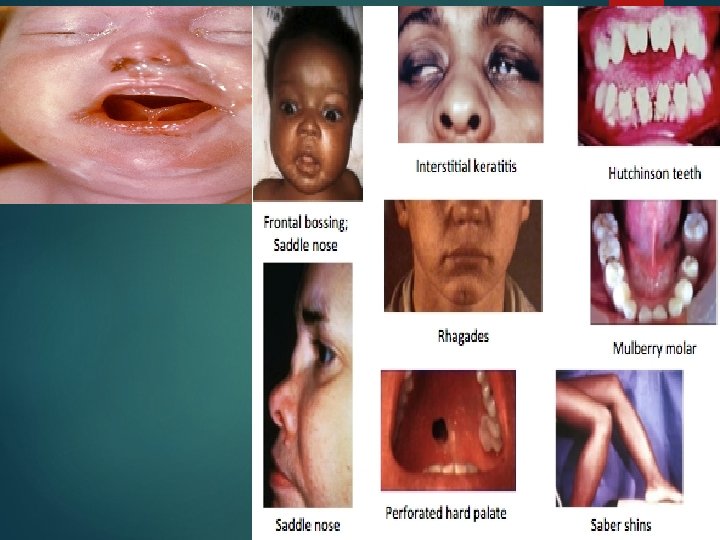
Clinical Manifestations Late congenital: Frontal bossing Short maxilla High palatal arch Hutchinson teeth 8 th nerve deafness Saddle nose Perioral fissures Can be prevented with appropriate treatment
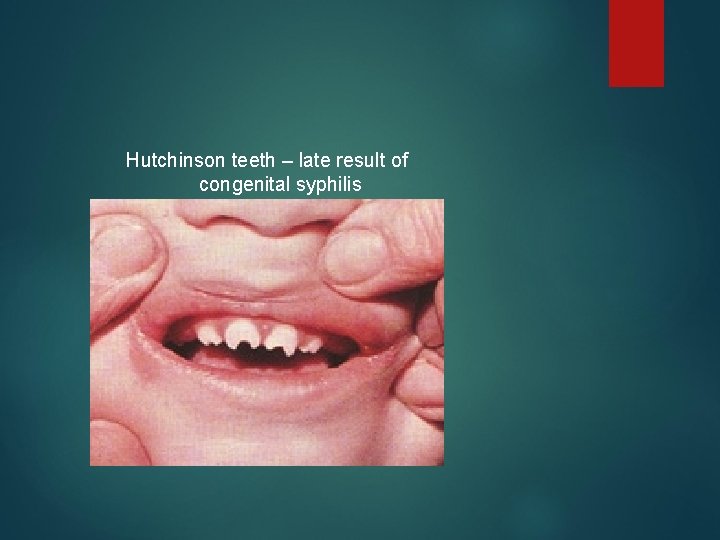
Hutchinson teeth – late result of congenital syphilis
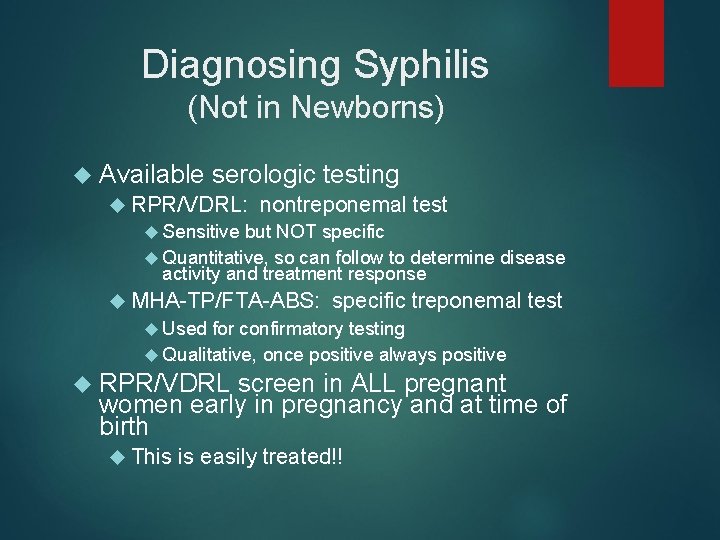
Diagnosing Syphilis (Not in Newborns) Available serologic testing RPR/VDRL: nontreponemal test Sensitive but NOT specific Quantitative, so can follow to determine disease activity and treatment response MHA-TP/FTA-ABS: specific treponemal test Used for confirmatory testing Qualitative, once positive always positive RPR/VDRL screen in ALL pregnant women early in pregnancy and at time of birth This is easily treated!!
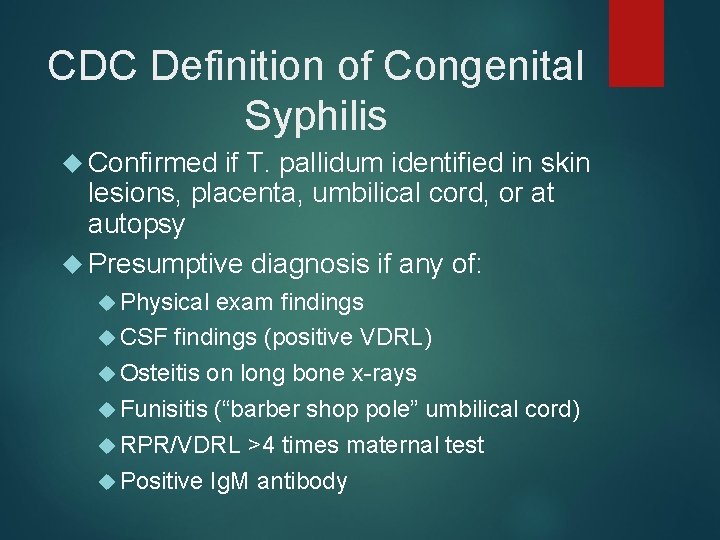
CDC Definition of Congenital Syphilis Confirmed if T. pallidum identified in skin lesions, placenta, umbilical cord, or at autopsy Presumptive diagnosis if any of: Physical exam findings CSF findings (positive VDRL) Osteitis on long bone x-rays Funisitis (“barber shop pole” umbilical cord) RPR/VDRL >4 times maternal test Positive Ig. M antibody
Diagnosing Congenital Syphilis Ig. G can represent maternal antibody, not infant infection This is VERY intricate and often confusing Consult your Red. Book (or peds ID folks) when faced with this situation
Treatment Penicillin G is THE drug of choice for ALL syphilis infections Maternal treatment during pregnancy very effective (overall 98% success) Treat newborn if: They meet CDC diagnostic criteria Mom was treated <4 wks before delivery Mom treated with non-PCN med Maternal titers do not show adequate response (less than 4 -fold decline)
Cytomegalovirus (CMV) Most common congenital viral infection ~40, 000 infants per year in the U. S. Mild, self limiting illness Transmission can occur with primary infection or reactivation of virus 40% risk of transmission in primary infxn Studies suggest increased risk of transmission later in pregnancy However, more severe sequalae associated with earlier acquisition
Clinical Manifestations 90% are asymptomatic at birth! Up to 15% develop symptoms later, notably sensorineural hearing loss Symptomatic infection SGA, HSM, petechiae, jaundice, chorioretinitis, periventricular calcifications, neurological deficits >80% develop long term complications Hearing loss, vision impairment, developmental delay
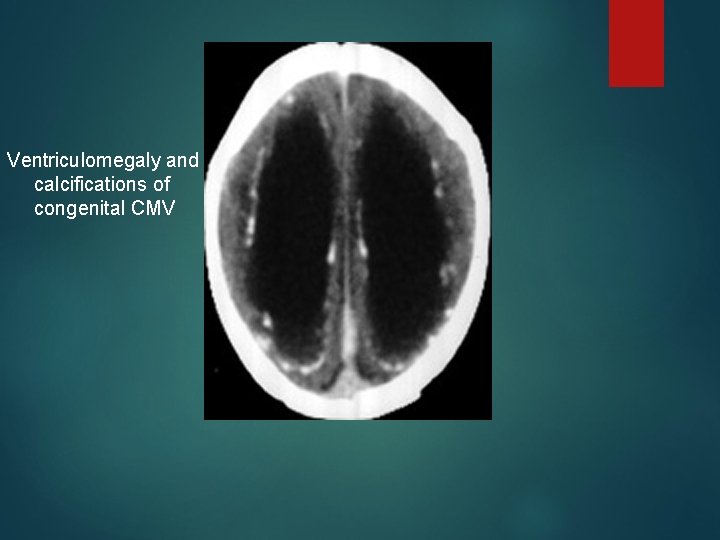
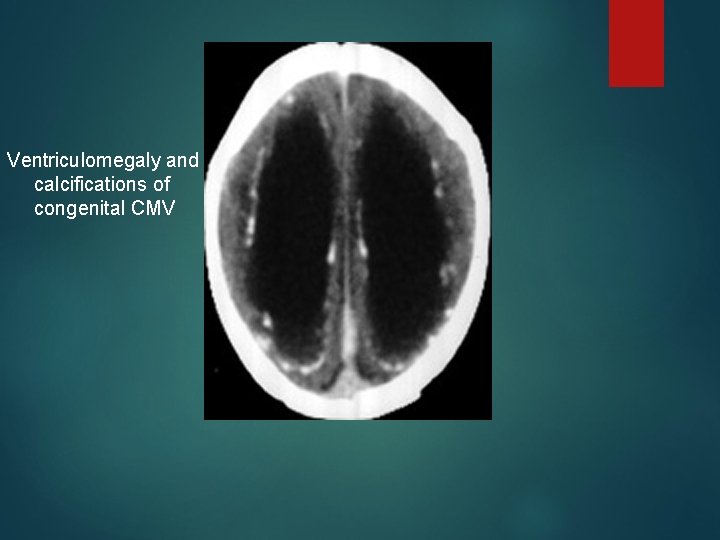
Ventriculomegaly and calcifications of congenital CMV
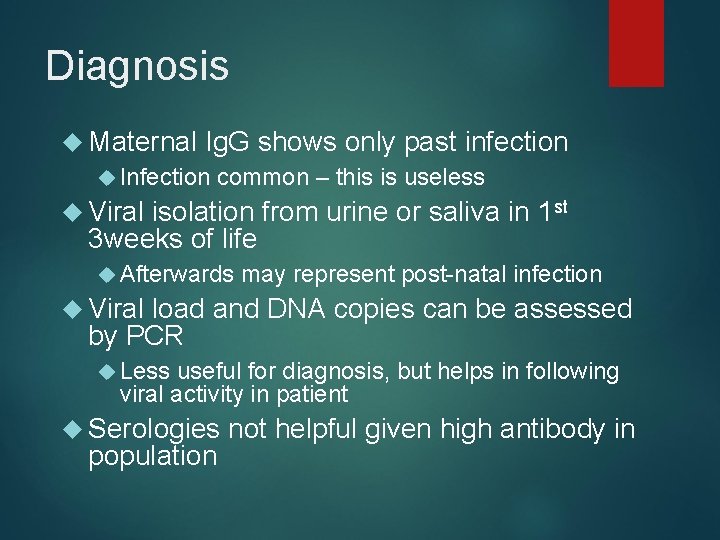
Diagnosis Maternal Ig. G shows only past infection Infection common – this is useless Viral isolation from urine or saliva in 1 st 3 weeks of life Afterwards may represent post-natal infection Viral load and DNA copies can be assessed by PCR Less useful for diagnosis, but helps in following viral activity in patient Serologies population not helpful given high antibody in
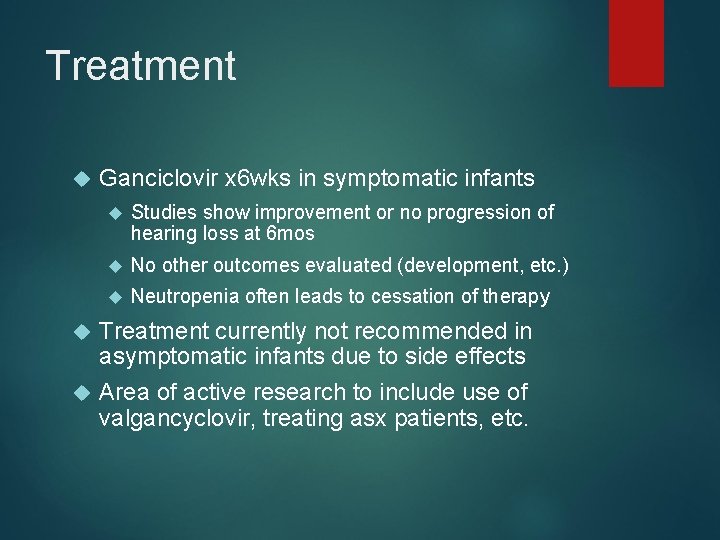
Treatment Ganciclovir x 6 wks in symptomatic infants Studies show improvement or no progression of hearing loss at 6 mos No other outcomes evaluated (development, etc. ) Neutropenia often leads to cessation of therapy Treatment currently not recommended in asymptomatic infants due to side effects Area of active research to include use of valgancyclovir, treating asx patients, etc.
Herpes Simplex (HSV) HSV 1 or HSV 2 Primarily transmitted through infected maternal genital tract Rationale for C-section delivery prior to membrane rupture Primary infection with greater transmission risk than reactivation
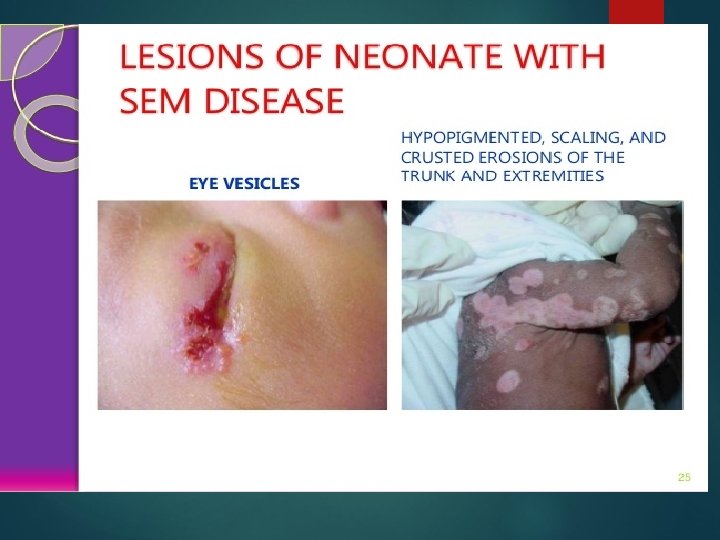
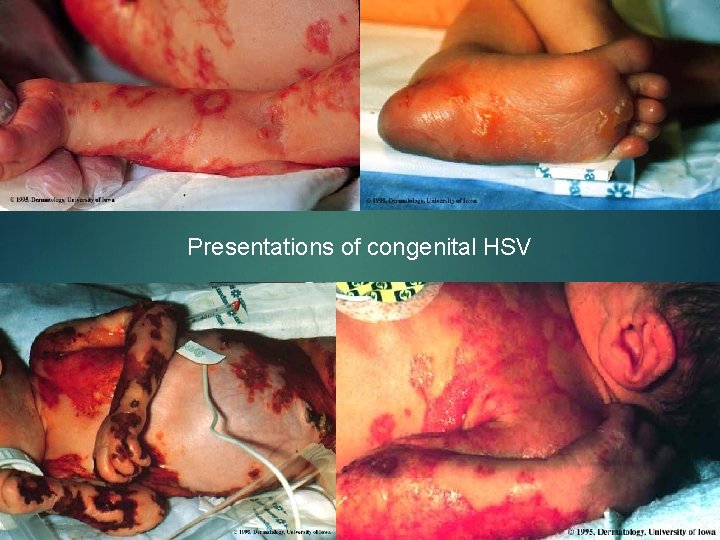
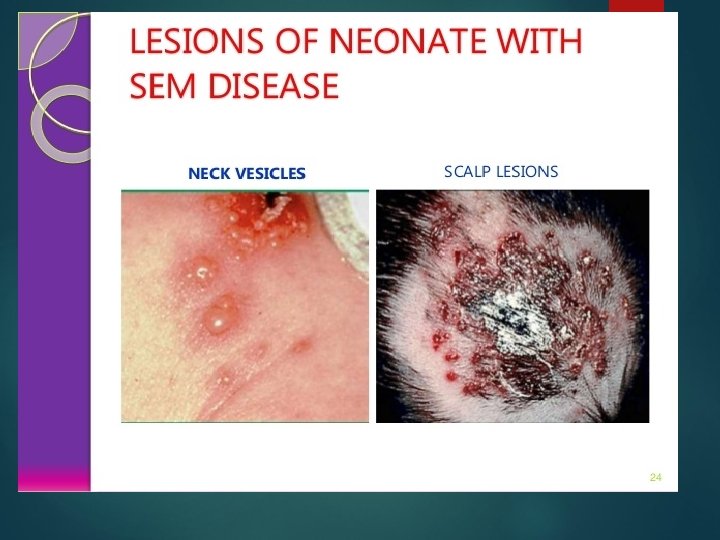
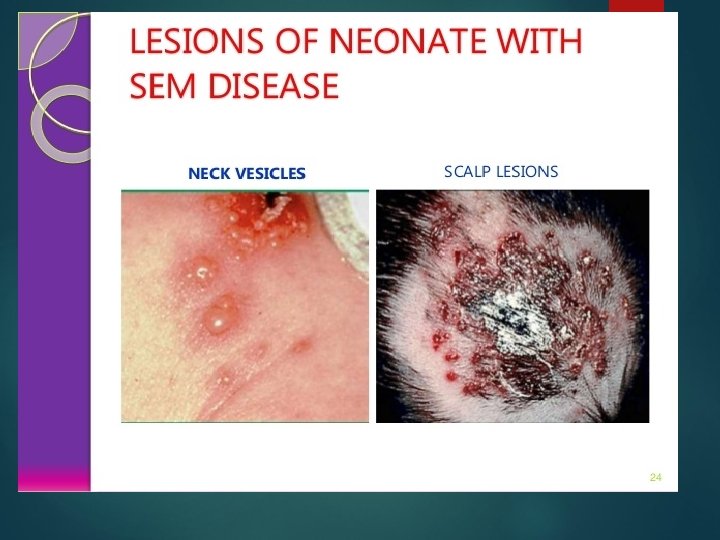
Clinical Manifestations Most are asymptomatic at birth 3 patterns of ~ equal frequency with symptoms between birth and 4 wks: Skin, eyes, mouth (SEM) CNS disease Disseminated Initial disease (present earliest) manifestations very nonspecific with skin lesions NOT necessarily present
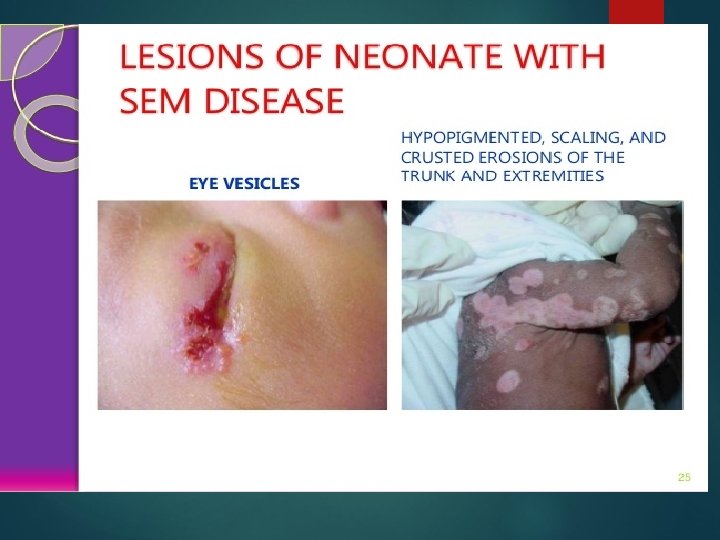
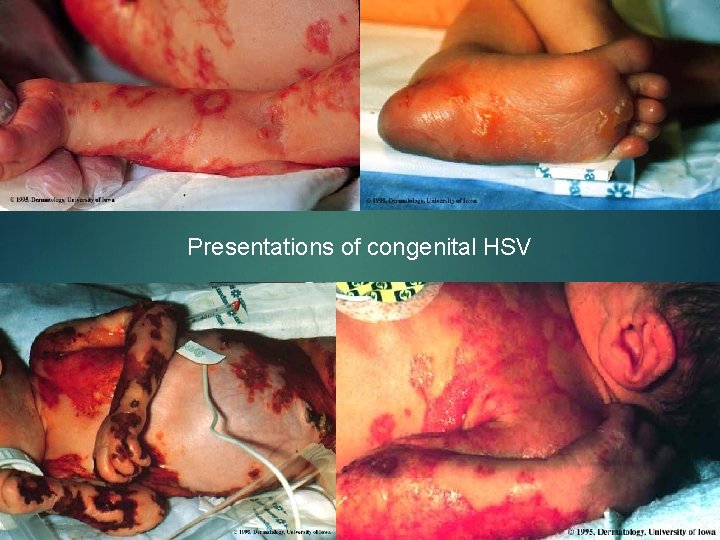
Presentations of congenital HSV
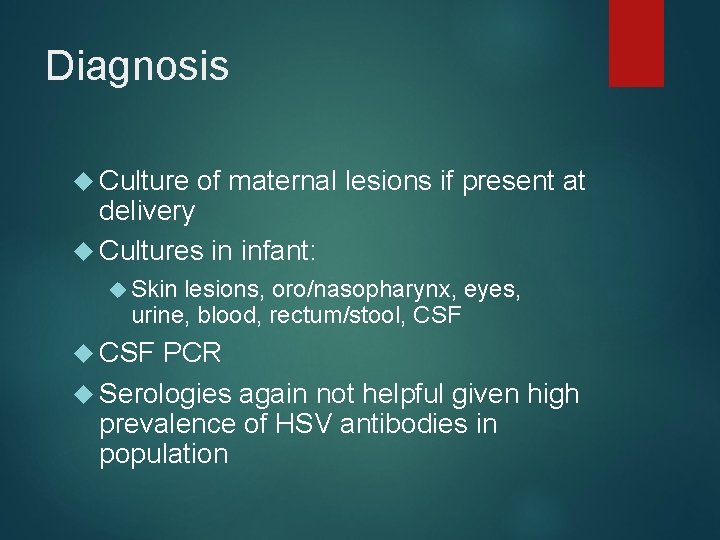
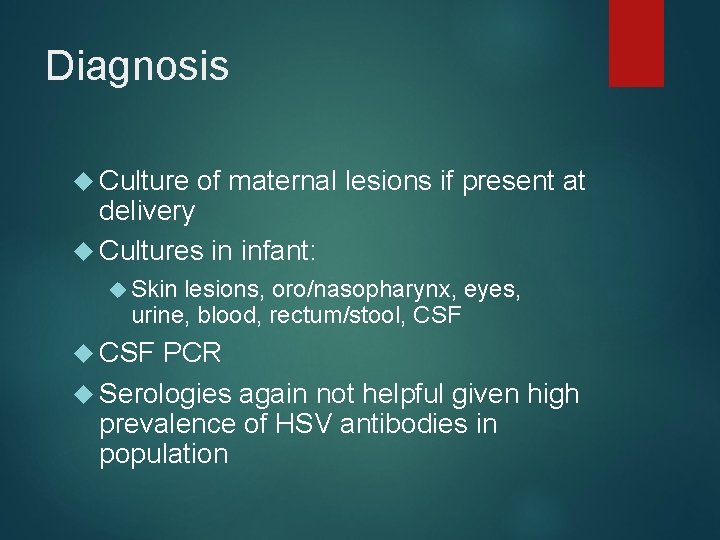
Diagnosis Culture of maternal lesions if present at delivery Cultures in infant: Skin lesions, oro/nasopharynx, eyes, urine, blood, rectum/stool, CSF PCR Serologies again not helpful given high prevalence of HSV antibodies in population
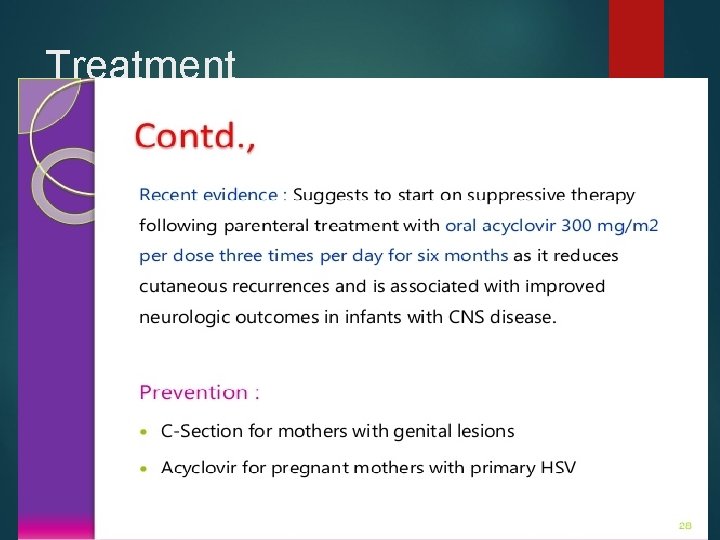
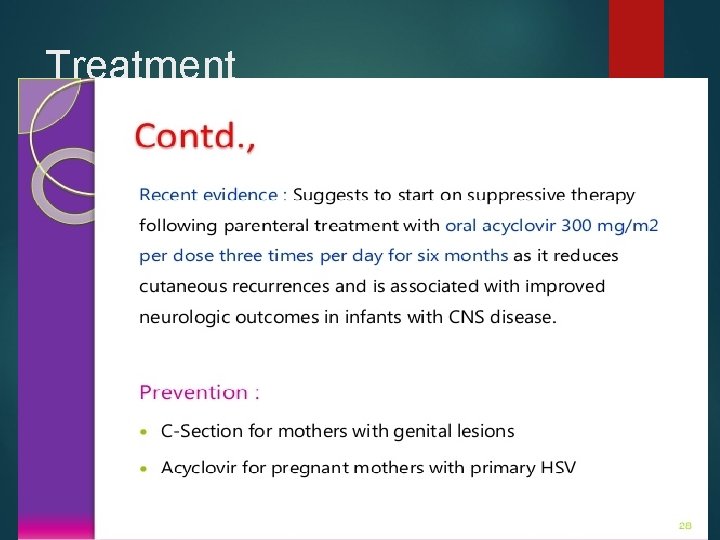
Treatment
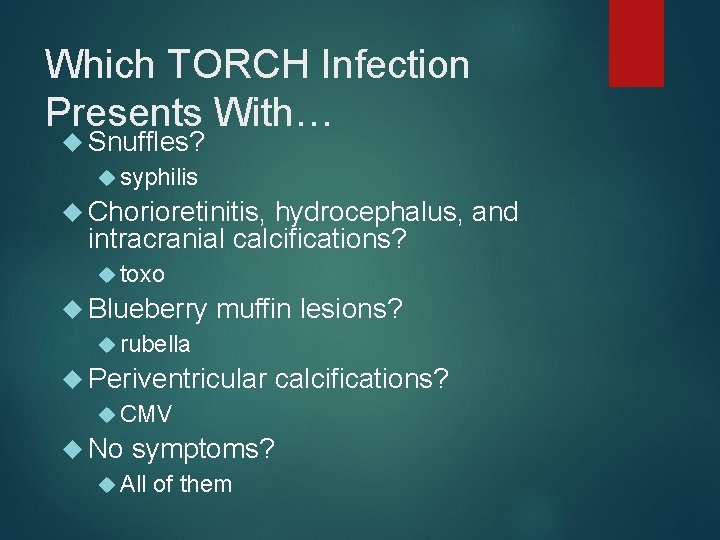
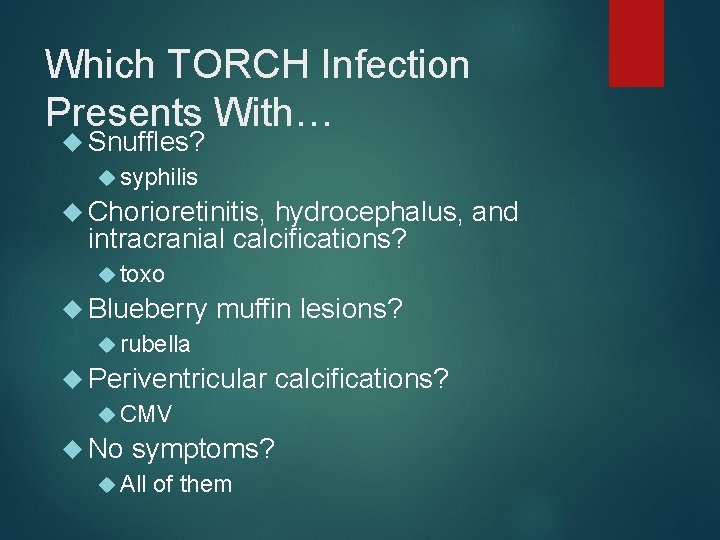
Which TORCH Infection Presents With… Snuffles? syphilis Chorioretinitis, hydrocephalus, and intracranial calcifications? toxo Blueberry rubella muffin lesions? Periventricular CMV calcifications? No symptoms? All of them
Which TORCH Infections Can Absolutely Be Prevented? Rubella Syphilis
When Are TORCH Titers Helpful in Diagnosing Congenital Infection? NEVER!
Questions?