Topic 7 Introduction to methods for quality improvement
- Slides: 30
Topic 7 Introduction to methods for quality improvement
Learning objective • the objectives of this topic are to: – describe the basic principles of quality improvement – introduce students to the methods and tools for improving the quality of health care
Performance requirement • know how to use a range of improvement activities and tools
Knowledge requirements • • • the science of improvement the quality improvement model change concepts two examples of continuous improvement methods for providing information on clinical care
The science of improvement • • appreciation of a system understanding of variation theory of knowledge psychology W Edwards Deming
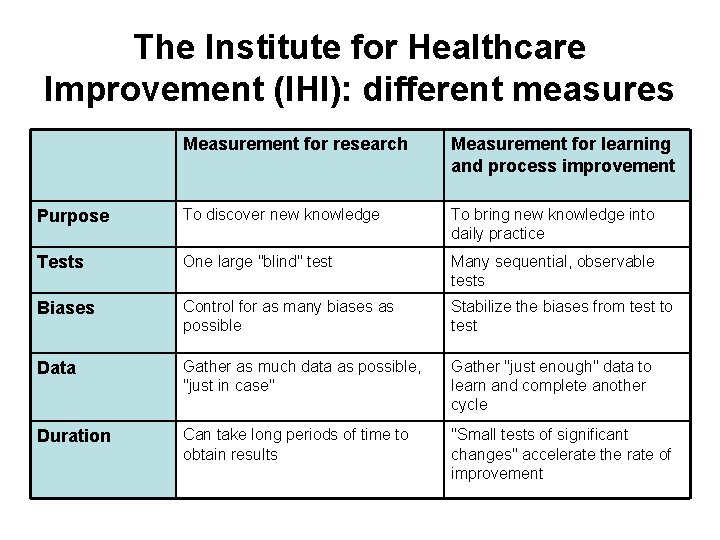
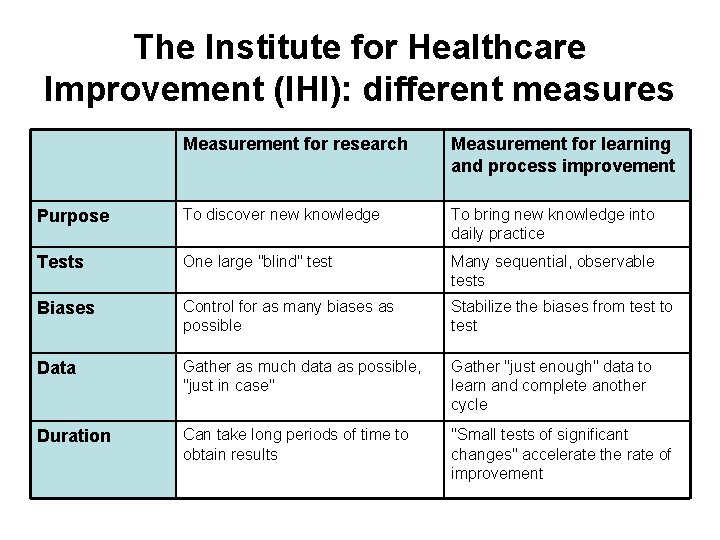
The Institute for Healthcare Improvement (IHI): different measures Measurement for research Measurement for learning and process improvement Purpose To discover new knowledge To bring new knowledge into daily practice Tests One large "blind" test Many sequential, observable tests Biases Control for as many biases as possible Stabilize the biases from test to test Data Gather as much data as possible, "just in case" Gather "just enough" data to learn and complete another cycle Duration Can take long periods of time to obtain results "Small tests of significant changes" accelerate the rate of improvement
Three types of measures • outcome measures • process measures • balancing measures
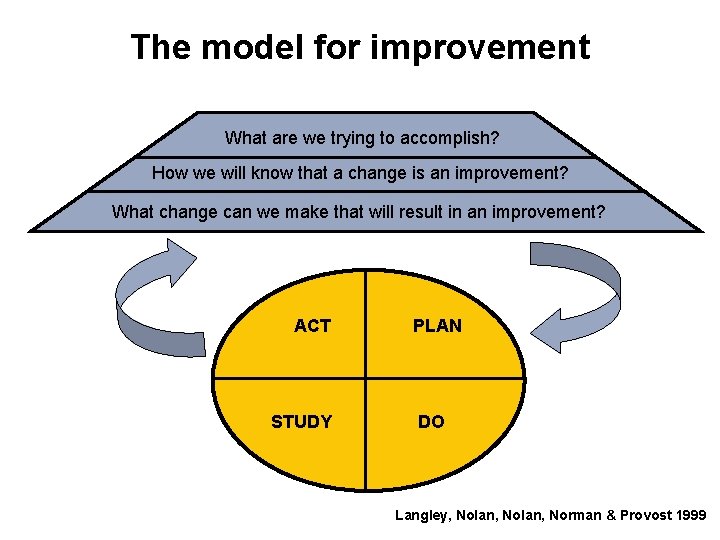
The quality improvement model-the PDSA cycle • What are we trying to accomplish? • How will we know that a change is an improvement? • What changes can we make that will result in an improvement?
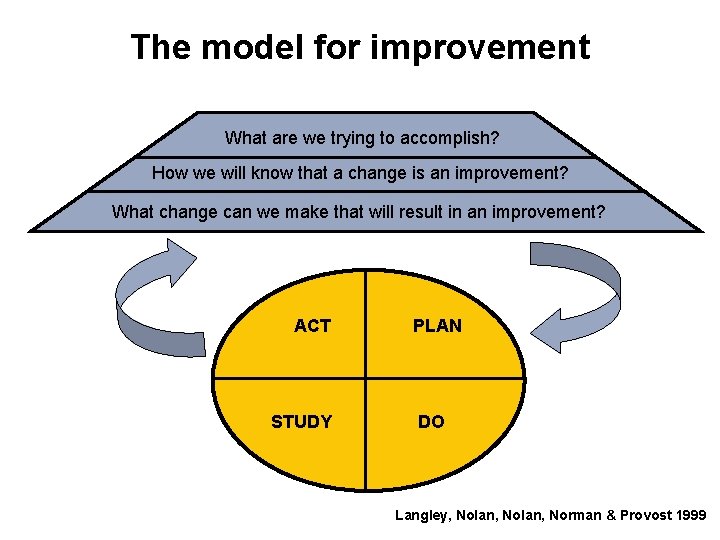
The model for improvement What are we trying to accomplish? How we will know that a change is an improvement? What change can we make that will result in an improvement? ACT STUDY PLAN DO Langley, Nolan, Norman & Provost 1999
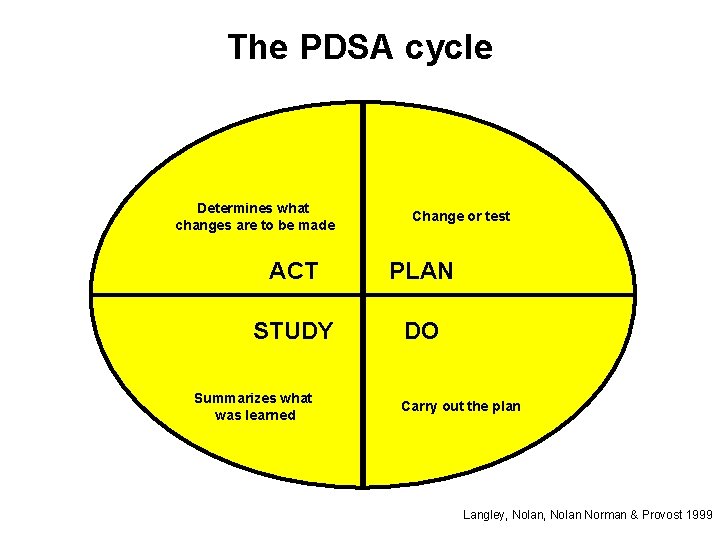
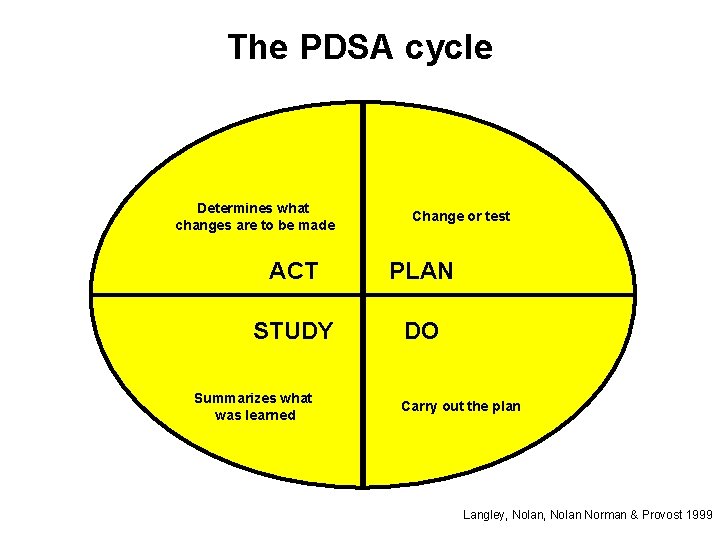
The PDSA cycle Determines what changes are to be made Change or test ACT PLAN STUDY DO Summarizes what was learned Carry out the plan Langley, Nolan Norman & Provost 1999
Change concepts … … are general ideas, with proven merit and sound scientific or logical foundation that can stimulate specific ideas for changes that lead to improvement. Nolan & Schall, 1996
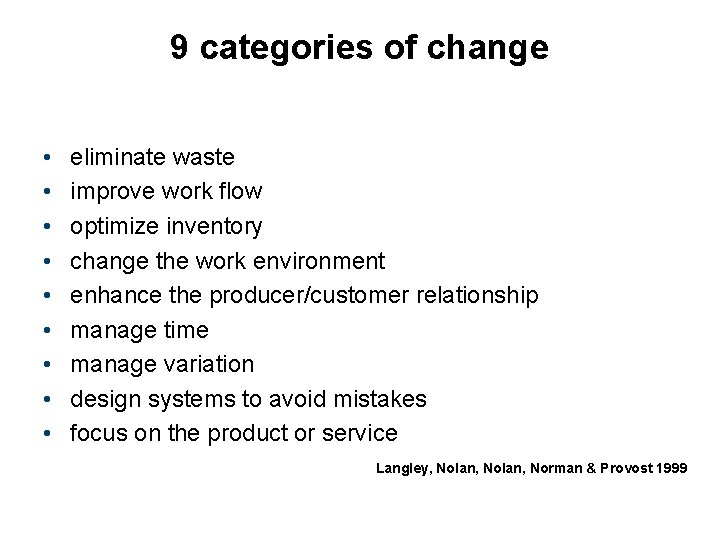
9 categories of change • • • eliminate waste improve work flow optimize inventory change the work environment enhance the producer/customer relationship manage time manage variation design systems to avoid mistakes focus on the product or service Langley, Nolan, Norman & Provost 1999
Two continuous improvement methods • clinical practice improvement methodology (CPI) • root cause analysis
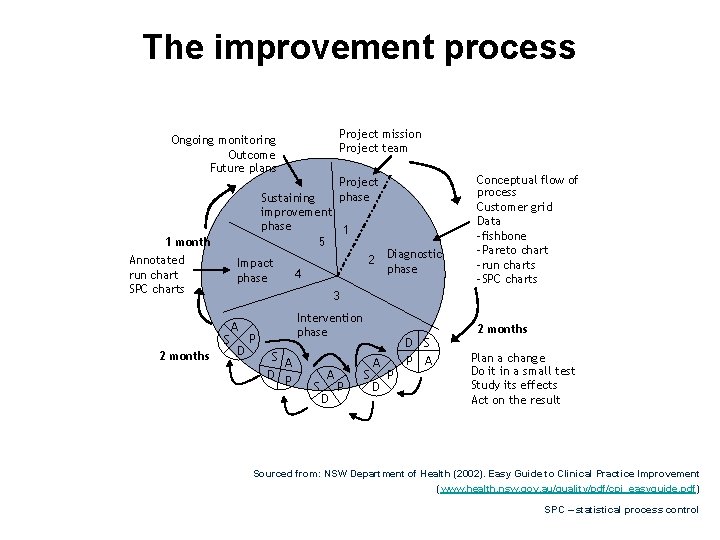
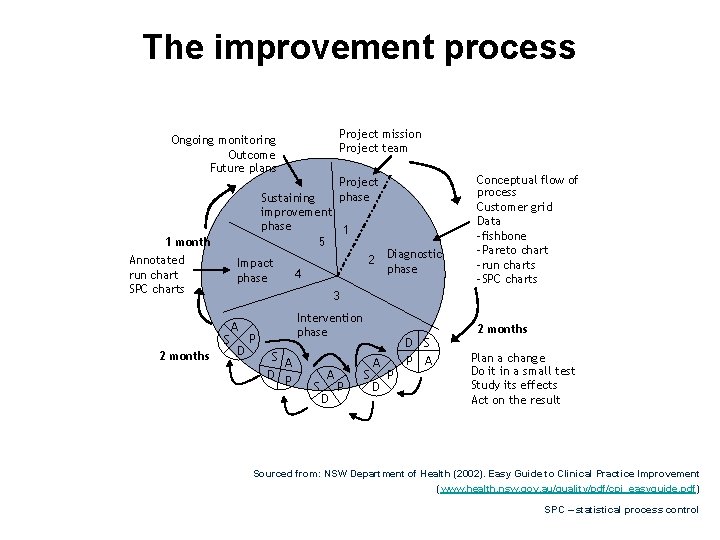
The improvement process Project mission Project team Ongoing monitoring Outcome Future plans Project phase Sustaining improvement phase 1 5 1 month Annotated run chart SPC charts Impact phase 3 S 2 months 4 2 Diagnostic phase Conceptual flow of process Customer grid Data -fishbone -Pareto chart -run charts -SPC charts A D Intervention phase P S A D P D S P A 2 months Plan a change Do it in a small test Study its effects Act on the result Sourced from: NSW Department of Health (2002). Easy Guide to Clinical Practice Improvement (www. health. nsw. gov. au/quality/pdf/cpi_easyguide. pdf) SPC – statistical process control
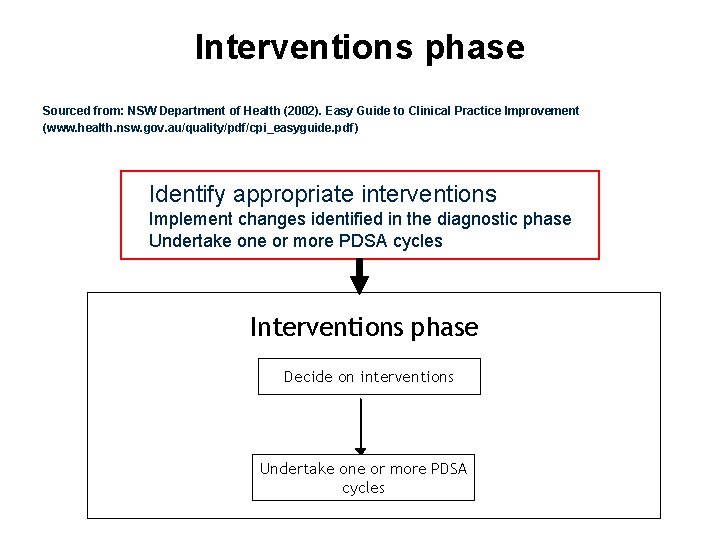
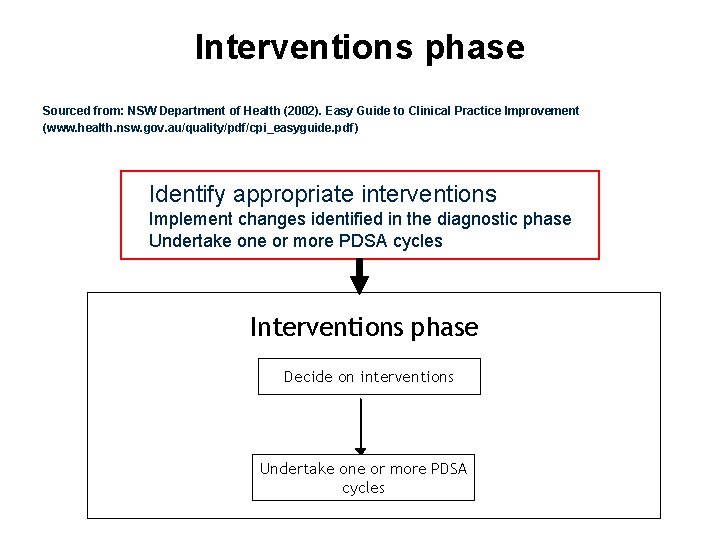
Interventions phase Sourced from: NSW Department of Health (2002). Easy Guide to Clinical Practice Improvement (www. health. nsw. gov. au/quality/pdf/cpi_easyguide. pdf) Identify appropriate interventions Implement changes identified in the diagnostic phase Undertake one or more PDSA cycles Interventions phase Decide on interventions Undertake one or more PDSA cycles
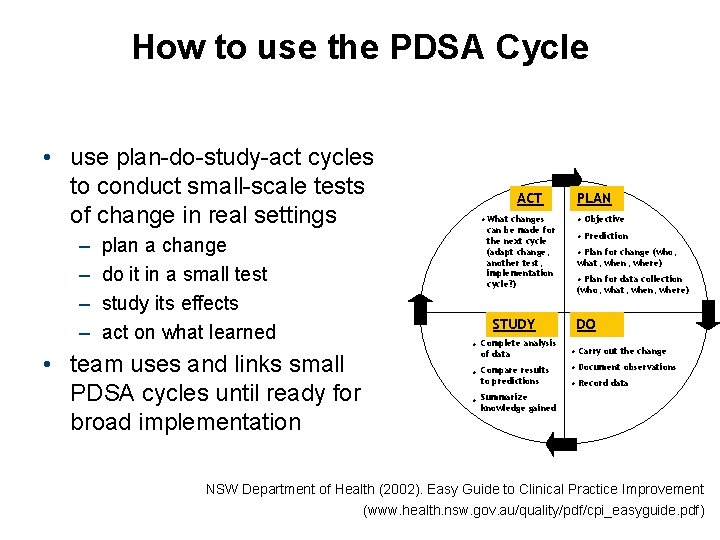
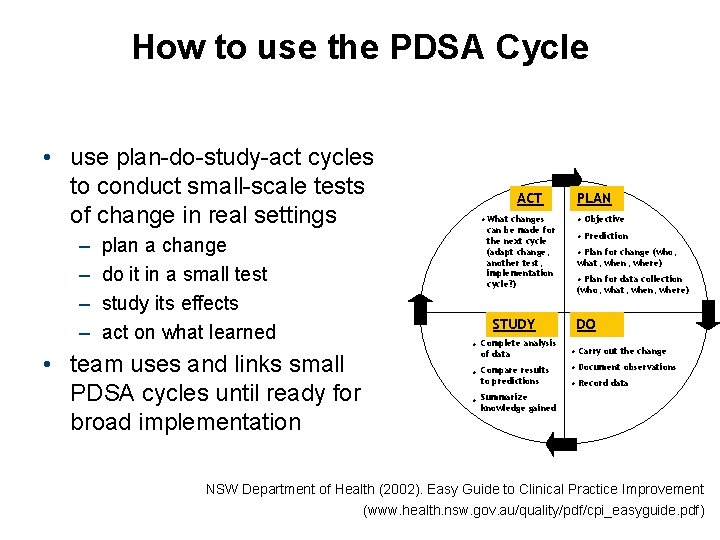
How to use the PDSA Cycle • use plan-do-study-act cycles to conduct small-scale tests of change in real settings – – plan a change do it in a small test study its effects act on what learned • team uses and links small PDSA cycles until ready for broad implementation ACT • What changes can be made for the next cycle (adapt change, another test, implementation cycle? ) STUDY • Complete analysis of data • Compare results to predictions PLAN • Objective • Prediction • Plan for change (who, what, when, where) • Plan for data collection (who, what, when, where) DO • Carry out the change • Document observations • Record data • Summarize knowledge gained NSW Department of Health (2002). Easy Guide to Clinical Practice Improvement (www. health. nsw. gov. au/quality/pdf/cpi_easyguide. pdf)
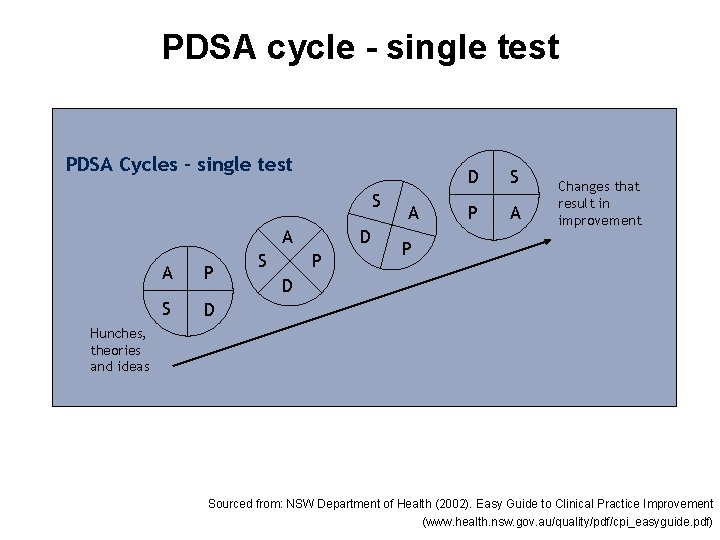
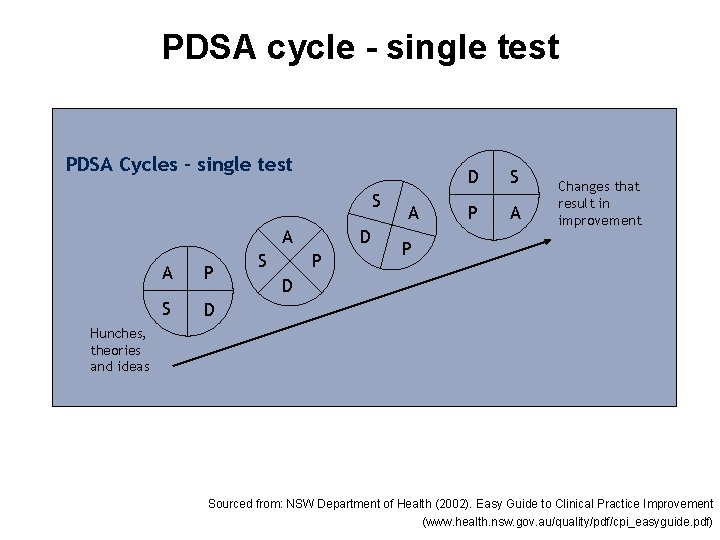
PDSA cycle - single test PDSA Cycles – single test S A A P S D P A D S P A Changes that result in improvement P D Hunches, theories and ideas Sourced from: NSW Department of Health (2002). Easy Guide to Clinical Practice Improvement (www. health. nsw. gov. au/quality/pdf/cpi_easyguide. pdf)
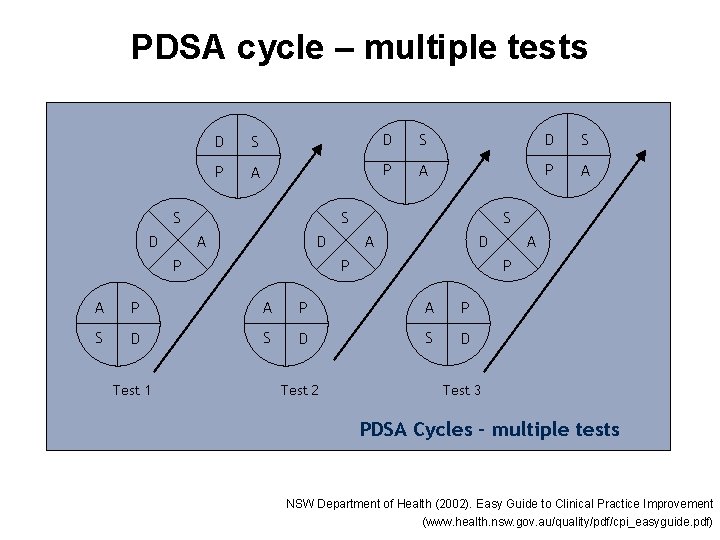
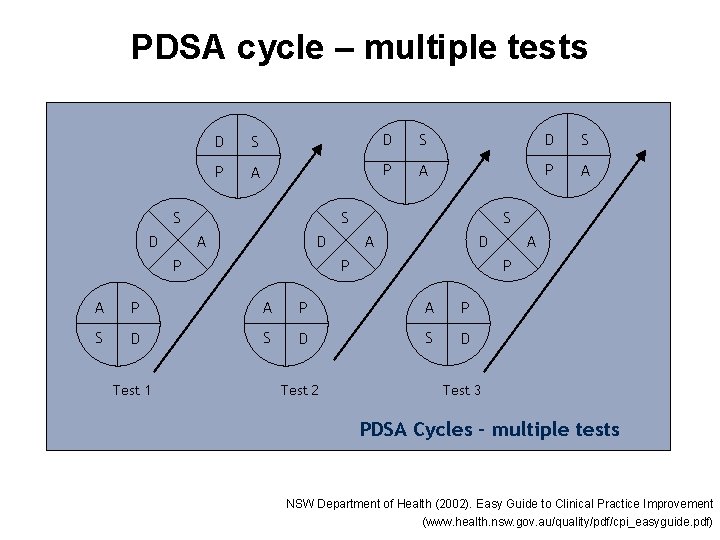
PDSA cycle – multiple tests D S D S P A P A S D S A D P P A P A P S D S D Test 1 Test 2 A Test 3 PDSA Cycles – multiple tests NSW Department of Health (2002). Easy Guide to Clinical Practice Improvement (www. health. nsw. gov. au/quality/pdf/cpi_easyguide. pdf)
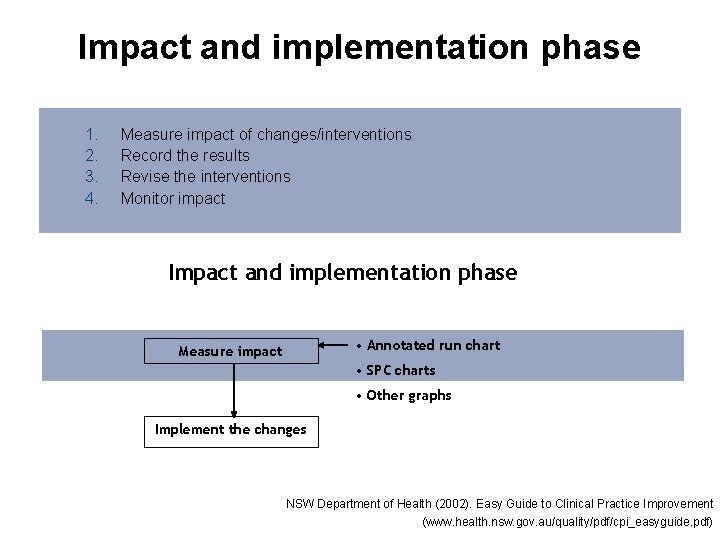
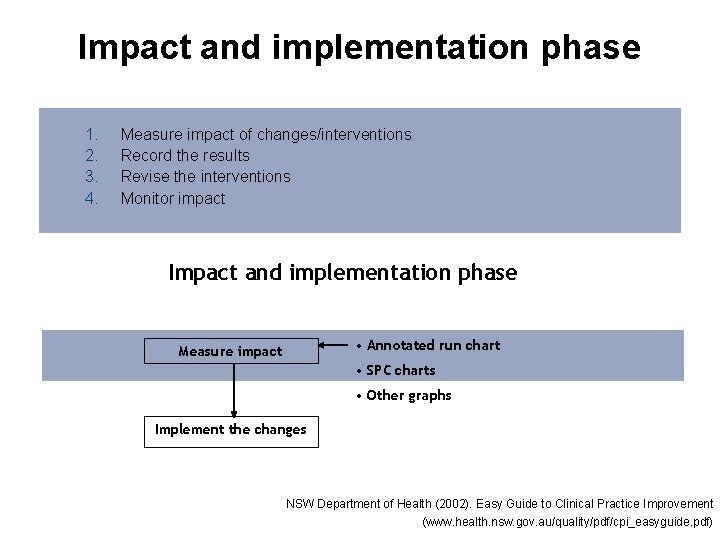
Impact and implementation phase 1. 2. 3. 4. Measure impact of changes/interventions Record the results Revise the interventions Monitor impact Impact and implementation phase • Annotated run chart Measure impact • SPC charts • Other graphs Implement the changes NSW Department of Health (2002). Easy Guide to Clinical Practice Improvement (www. health. nsw. gov. au/quality/pdf/cpi_easyguide. pdf)
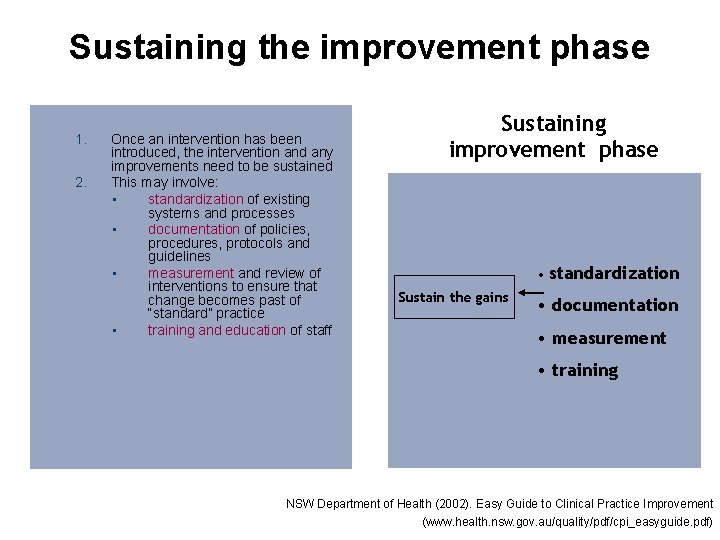
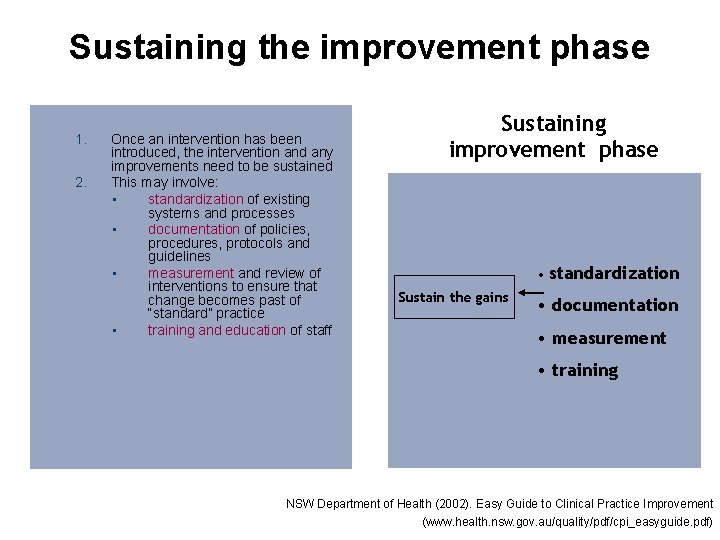
Sustaining the improvement phase 1. 2. Once an intervention has been introduced, the intervention and any improvements need to be sustained This may involve: • standardization of existing systems and processes • documentation of policies, procedures, protocols and guidelines • measurement and review of interventions to ensure that change becomes past of “standard” practice • training and education of staff Sustaining improvement phase • standardization Sustain the gains • documentation • measurement • training NSW Department of Health (2002). Easy Guide to Clinical Practice Improvement (www. health. nsw. gov. au/quality/pdf/cpi_easyguide. pdf)
Root cause analysis • a multidisciplinary team • the root cause analysis effort is directed towards finding out what happened • establishing the contributing factors of root causes
Performance requirements Know how to use a range of improvement activities and tools • • flowcharts cause and effect diagrams (Ishikawa/fishbone) Pareto charts run charts
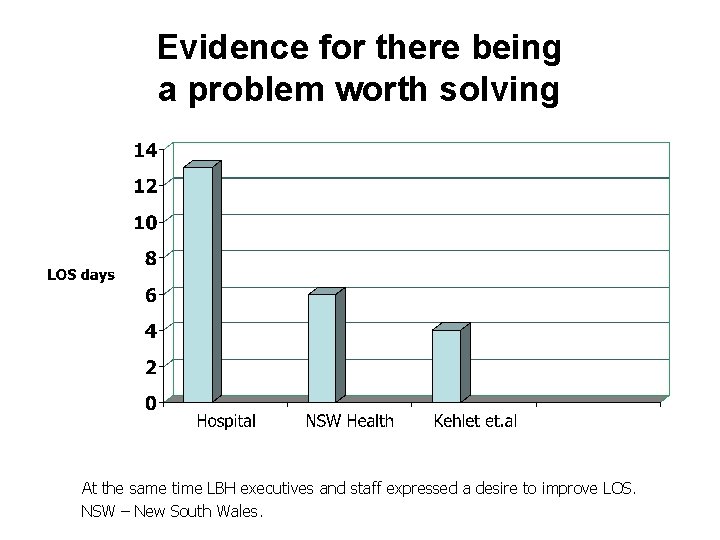
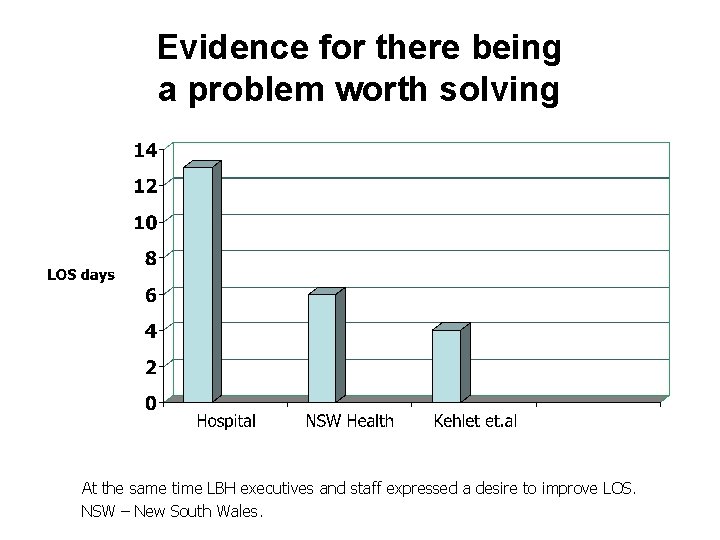
Evidence for there being a problem worth solving At the same time LBH executives and staff expressed a desire to improve LOS. NSW – New South Wales.
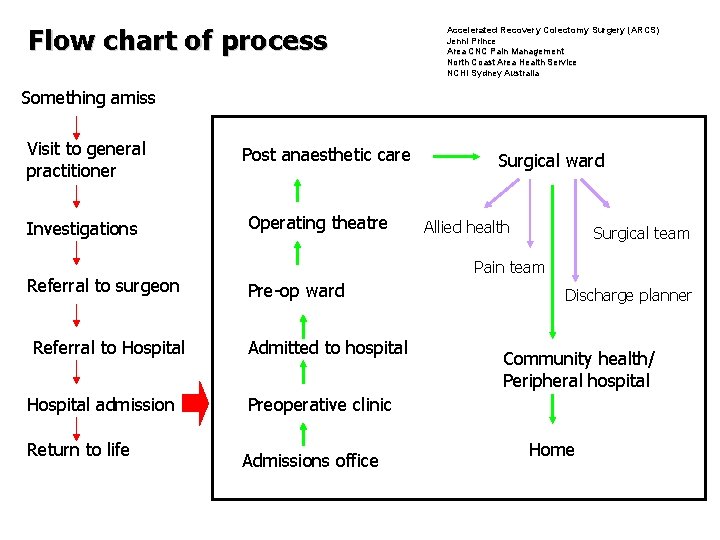
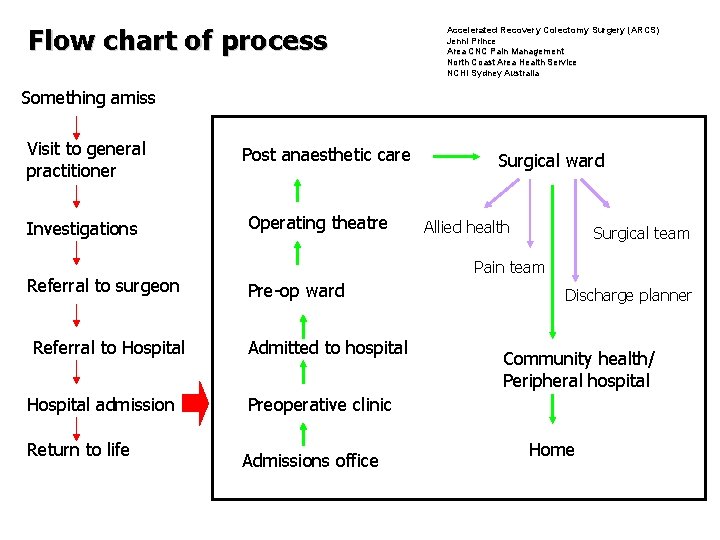
Flow chart of process Accelerated Recovery Colectomy Surgery (ARCS) Jenni Prince Area CNC Pain Management North Coast Area Health Service NCHI Sydney Australia Something amiss Visit to general practitioner Investigations Referral to surgeon Referral to Hospital admission Return to life Post anaesthetic care Operating theatre Surgical ward Allied health Surgical team Pain team Pre-op ward Admitted to hospital Discharge planner Community health/ Peripheral hospital Preoperative clinic Admissions office Home
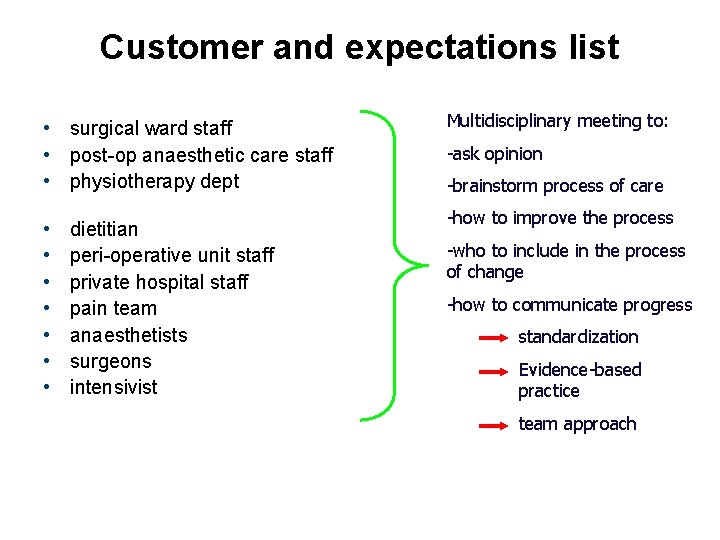
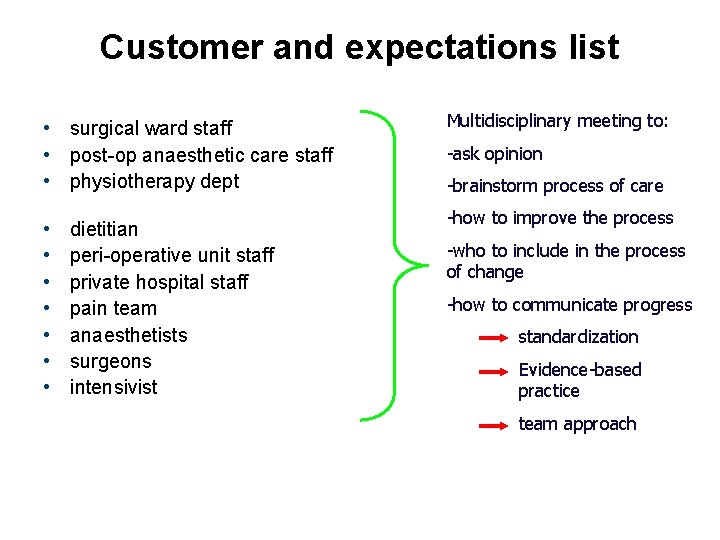
Customer and expectations list • surgical ward staff • post-op anaesthetic care staff • physiotherapy dept • • dietitian peri-operative unit staff private hospital staff pain team anaesthetists surgeons intensivist Multidisciplinary meeting to: -ask opinion -brainstorm process of care -how to improve the process -who to include in the process of change -how to communicate progress standardization Evidence-based practice team approach
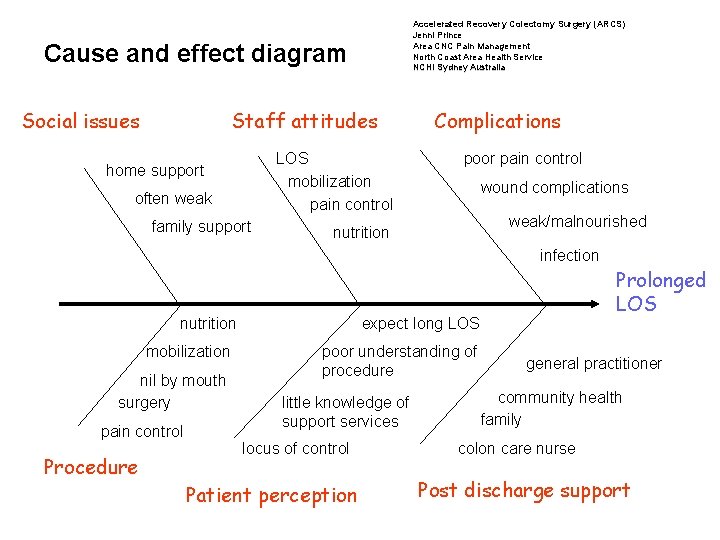
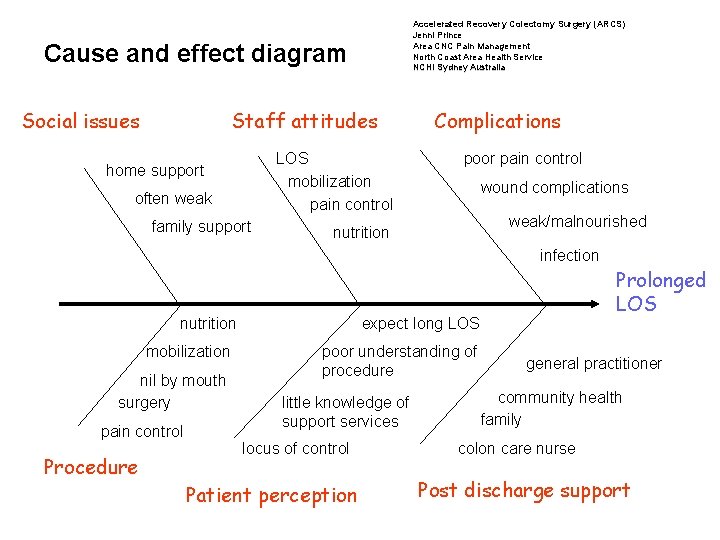
Accelerated Recovery Colectomy Surgery (ARCS) Jenni Prince Area CNC Pain Management North Coast Area Health Service NCHI Sydney Australia Cause and effect diagram Social issues Staff attitudes LOS mobilization pain control home support often weak family support Complications poor pain control wound complications weak/malnourished nutrition infection nutrition mobilization nil by mouth surgery pain control Procedure Prolonged LOS expect long LOS poor understanding of procedure little knowledge of support services locus of control Patient perception general practitioner community health family colon care nurse Post discharge support
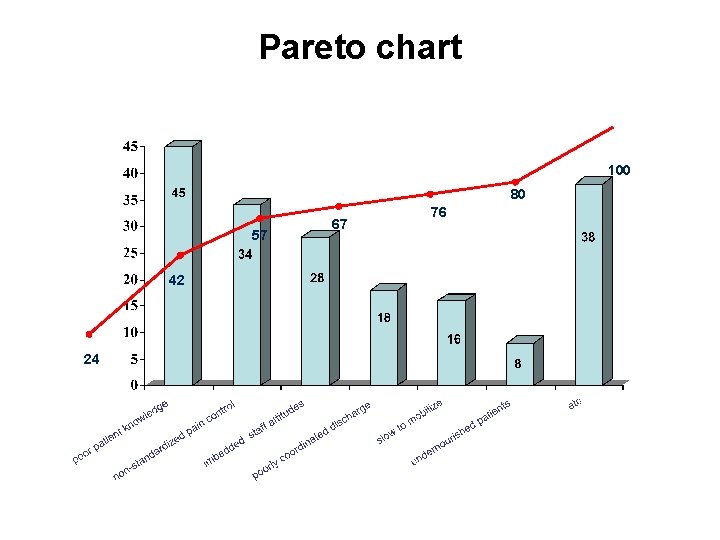
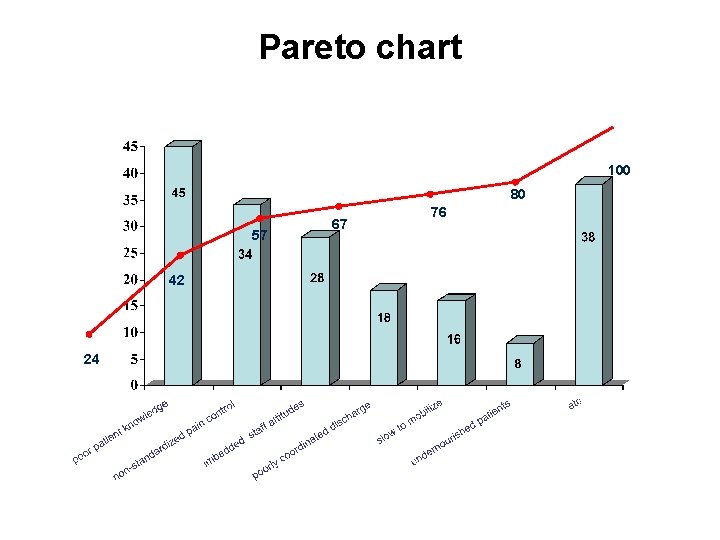
Pareto chart 100 80 57 42 24 67 76
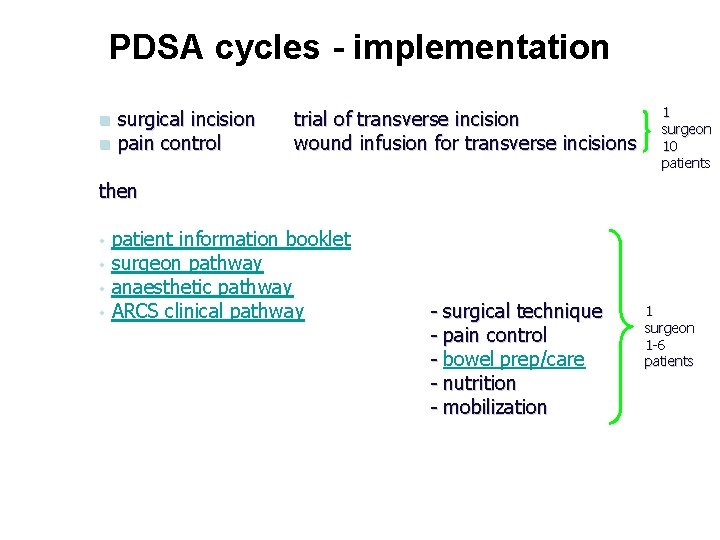
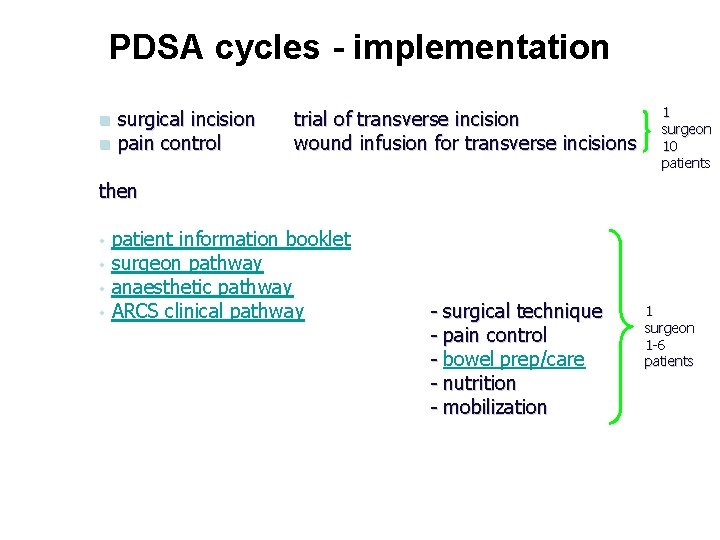
PDSA cycles - implementation n n surgical incision pain control trial of transverse incision wound infusion for transverse incisions 1 surgeon 10 patients then • • patient information booklet surgeon pathway anaesthetic pathway ARCS clinical pathway - surgical technique - pain control - bowel prep/care - nutrition - mobilization 1 surgeon 1 -6 patients
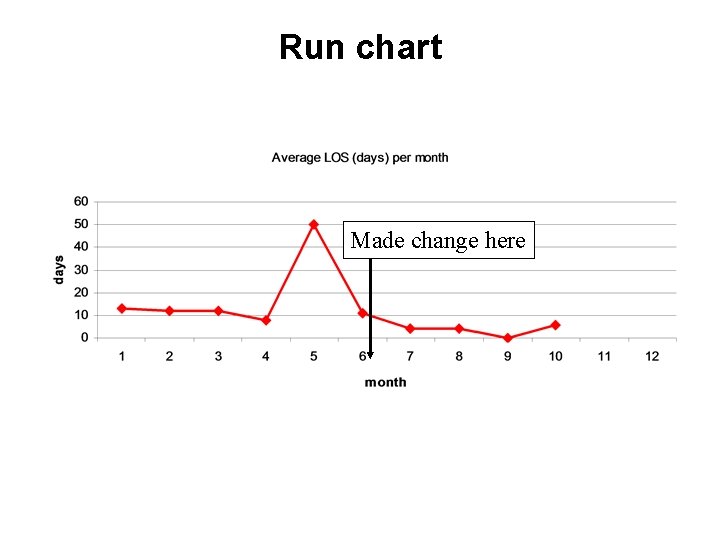
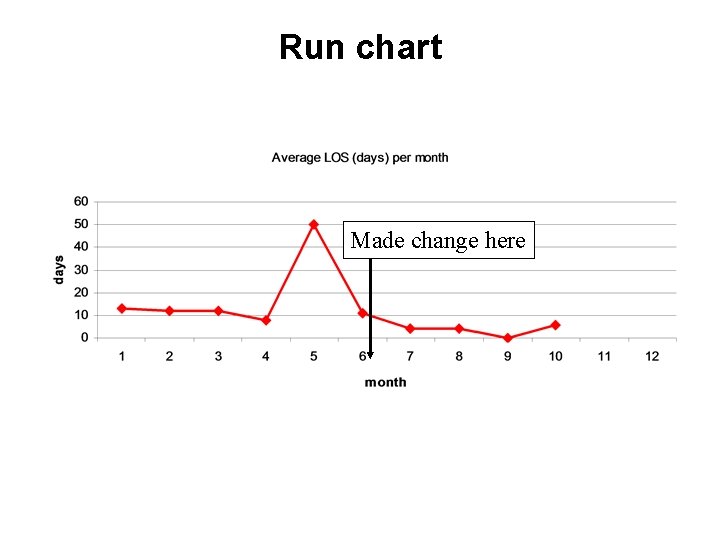
Run chart Made change here
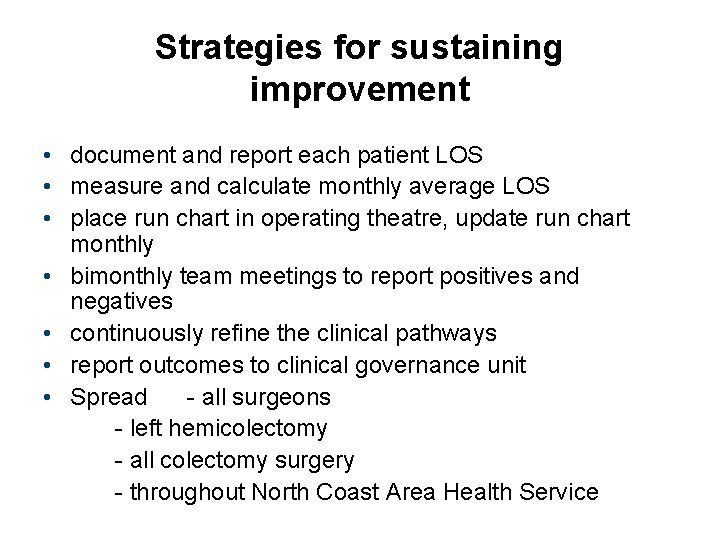
Strategies for sustaining improvement • document and report each patient LOS • measure and calculate monthly average LOS • place run chart in operating theatre, update run chart monthly • bimonthly team meetings to report positives and negatives • continuously refine the clinical pathways • report outcomes to clinical governance unit • Spread - all surgeons - left hemicolectomy - all colectomy surgery - throughout North Coast Area Health Service