Tools to Implement and Teach the Care Team
- Slides: 23
Tools to Implement and Teach the “Care Team Model” in a Family Medicine Residency Clinic Richard Backman MD Jennifer Leiser MD Sonja Van. Hala MD University of Utah
Sharing our Toolkit
Learning Objectives o o o Describe the Care Team Model (CTM) in a resident-faculty practice to achieve a redesigned office practice Explain the “graduated mentorship” model as a framework for teaching the CTM Utilize evaluation tools to assess implementation of the CTM
Mission Integration o o o Train residents in PCMH (Care by Design) Create a state-of-the-art faculty and resident practice Redesign residency Practice Management curriculum n New home for training in PCMH
Care By Design o o o Developed by University of Utah Community Clinics (about 2004) Empiric plan to increase efficiency and quality of care in large outpatient primary care system Elements map to Patient Centered Medical Home concepts
Care Team Model o o o Visit provided by a coordinated team Expanded MA role: deliver the visit from start to finish Physician does what only a physician can do
Tool: Blueprint (Create a Clear Design)
Tool: Blueprint (Create a Clear Design) Resident Skill Set: o Daily huddle o Utilize technology n n o o o EHR Communication Conduct visit with advanced MA role Manage inbox (rx’s, labs, phone calls) Describe clinic workflow processes
Tool: Cement Mixer (Pour the Foundation)
Tool: Cement Mixer (Pour the Foundation) o Faculty Development n n Establish unified vision Enhance skills o EHR training o Demonstration of CTM Orientation to Graduated Mentorship Model o Clear educational goals o Faculty role-play and debriefing Identify faculty mentors
Tool: Cement Mixer (Pour the Foundation) o Grant Support n n Align mission with University of Utah performance goals Partner with Community Clinic system and University of Utah Medical Group
Tool: Hammer (Build the Frame)
Tool: Hammer (Build the Frame) o Graduated Mentorship Model n n n o Shadowing Shared appointment Coaching Structure n n Faculty clinic 4 continuity patients, 2 acute visits
Tool: Screwgun (Hang the Walls)
Tool: Screwgun (Hang the Walls) o Orientation Overview n n o o o Future of Family Medicine Care Team Model Group EHR training 2 sessions with EHR trainer in clinic Graduated mentorship sessions
Tool: Nailgun (Cap it with a Roof)
Tool: Nailgun (Cap it with a Roof) o “Survival Skills: ” intern small group didactic session n n o Review of Care Team Model Simulated patient visit and discussion Fall intern retreat n n n Leadership Teamwork and communication Debriefing on CTM training
The Inspector Drops By… o Evaluation Measures
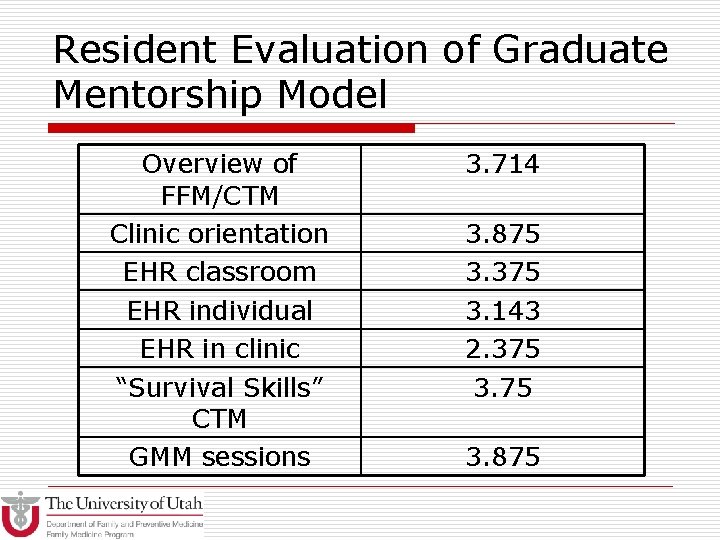
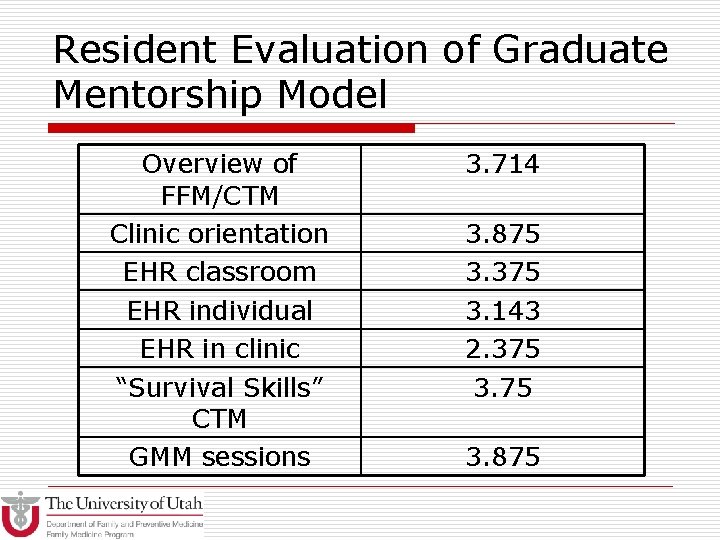
Resident Evaluation of Graduate Mentorship Model Overview of FFM/CTM Clinic orientation EHR classroom EHR individual EHR in clinic “Survival Skills” CTM GMM sessions 3. 714 3. 875 3. 375 3. 143 2. 375 3. 875
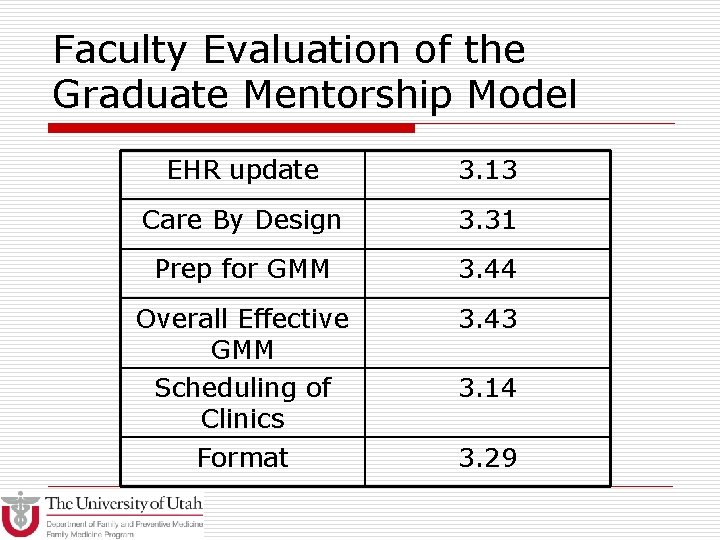
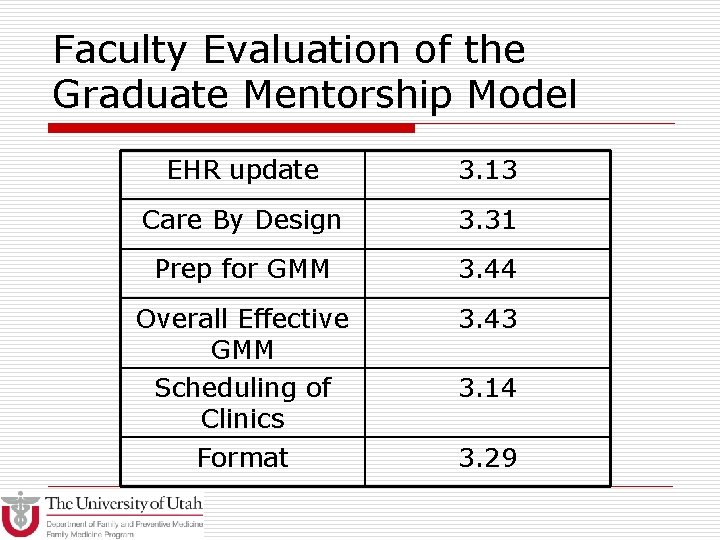
Faculty Evaluation of the Graduate Mentorship Model EHR update 3. 13 Care By Design 3. 31 Prep for GMM 3. 44 Overall Effective GMM Scheduling of Clinics Format 3. 43 3. 14 3. 29
Looking in the Mirror
Looking in the Mirror: changes for next year o o o Practice sessions with Medical Assistants prior to live clinics Additional EHR training later Variability of clinic workflow interfered with training Two sessions instead of three: Shadow and Mentoring Limit to 4 patients per session; residents have their own schedule
Safe at Home o Questions