To know the epidemiology etiology pathogenesis clinical presentation





- Slides: 33
• To know the epidemiology , etiology, pathogenesis , clinical presentation, investigation , diagnosis , treatment , complication , prognosis
Bronchiolitis Bronchioles • are small airways of <2 mm diameter, . • increased airway resistance unresponsive to β 2 stimulants. Pathophysiology is unclear there is probably an initial injury to the epithelium of the bronchioles with subsequent inflammation. Adjacent alveoli are often also involved.
the commonest situations in which a diagnosis of bronchiolitis is useful: • Viral bronchiolitis (e. g. RSV) • Post-lung transplant. • Post-bone marrow transplant • Connective tissue disease (usually RA) • In association with ILD and airways disease • Diffuse pan-bronchiolitis.
Clinical features Insidious onset of cough and dyspnoea over weeks to months. There may be an associated medical history, such as recent viral illness, transplant, connective tissue disease, or vasculitis, or a history of mineral dust or drug exposure.
Investigations • • • PFTs • CXR • HRCT • Open or thoracoscopic lung biopsy may be required.
Management • Treat any underlying disorder • Cough suppressants • Long-term macrolide antibiotics, • Steroids

Bronchiectasis • Bronchiectasis means abnormal dilatation of the bronchi. • Chronic suppurative airway infection with sputum production, progressive scarring and lung damage are present, whatever the cause.

Pathology • The bronchiectatic cavities. • Inflammatory changes in the deeper layers of the bronchial wall and hypertrophy of the bronchial arteries. • Chronic inflammatory and fibrotic changes are usually found in the surrounding lung tissue
Causes of bronchiectasis • Congenital • Cystic fibrosis • Ciliary dysfunction syndromes – Primary ciliary dyskinesia (immotile cilia syndrome) – Kartagener's syndrome (sinusitis and transposition of the viscera) • Primary hypogammaglobulinaemia
• Acquired: children • Pneumonia (complicating whooping cough or measles) • Primary TB • Inhaled foreign body • Acquired: adults • Suppurative pneumonia • Pulmonary TB • Allergic bronchopulmonary aspergillosis complicating asthma. • Bronchial tumours
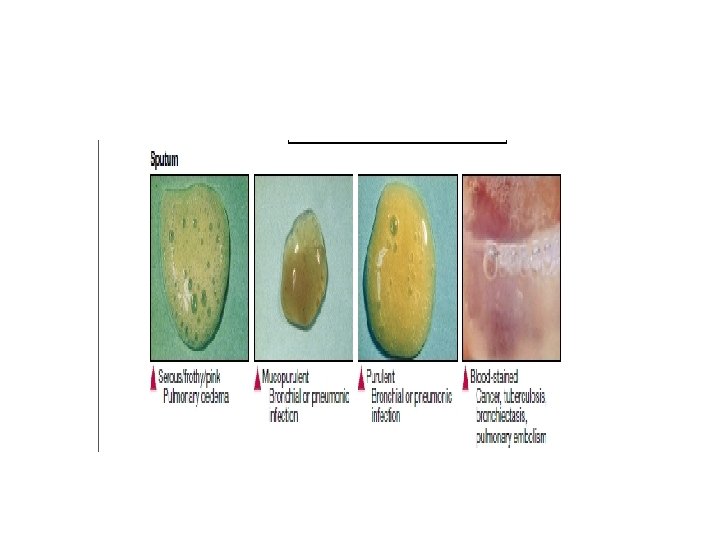
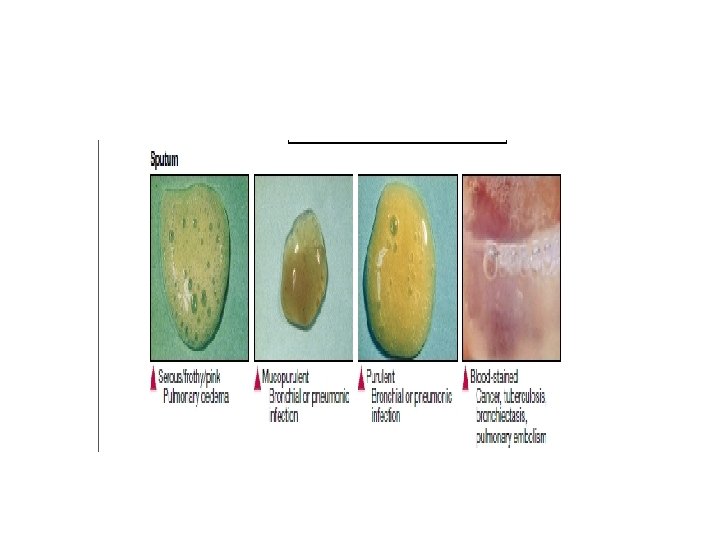
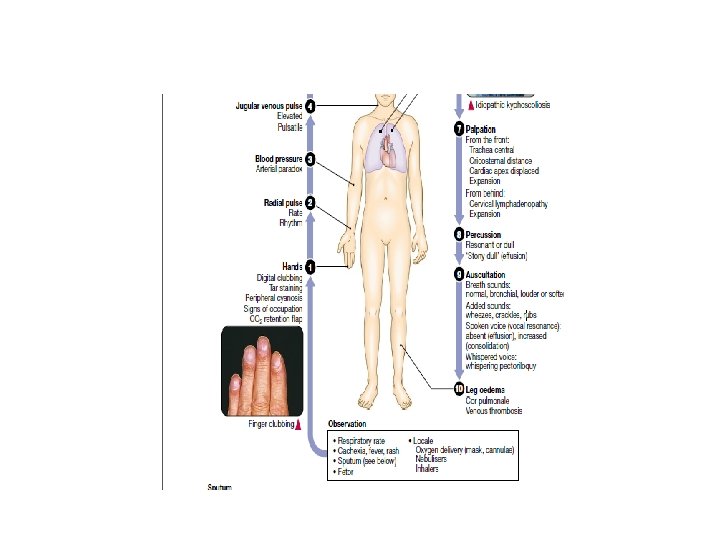
Clinical features Symptoms of bronchiectasis 1 -Cough • Chronic productive cough • worse in mornings and often brought on by changes of posture. 2 -Sputum • often copious and persistently purulent. • Halitosis.
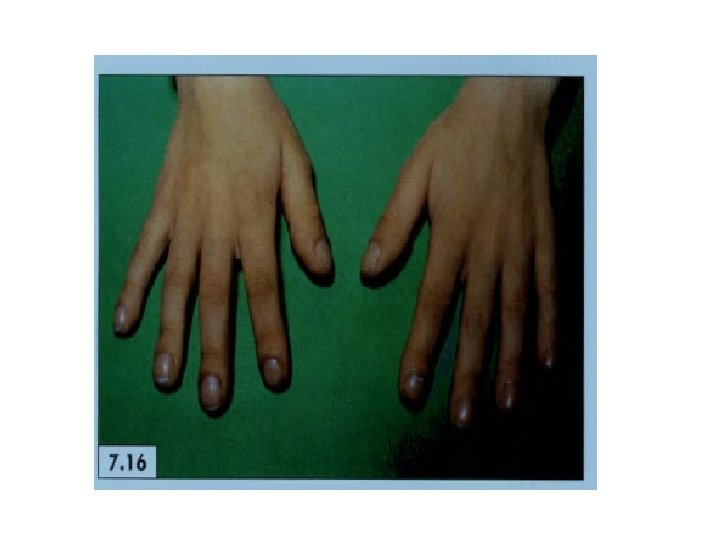
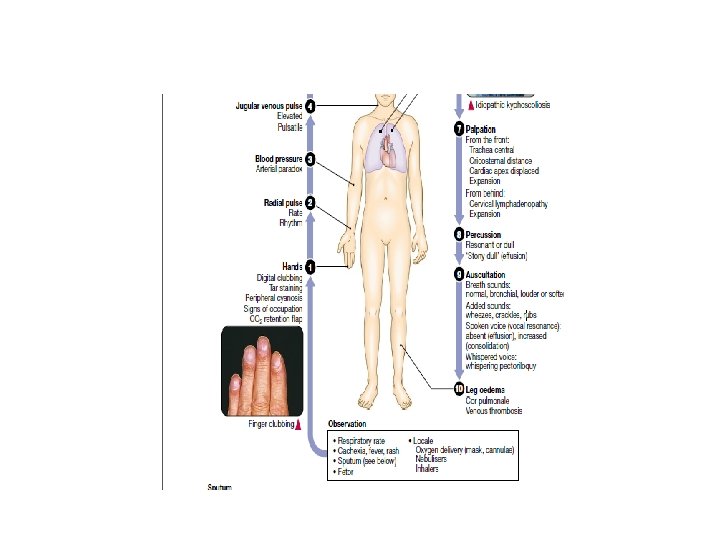
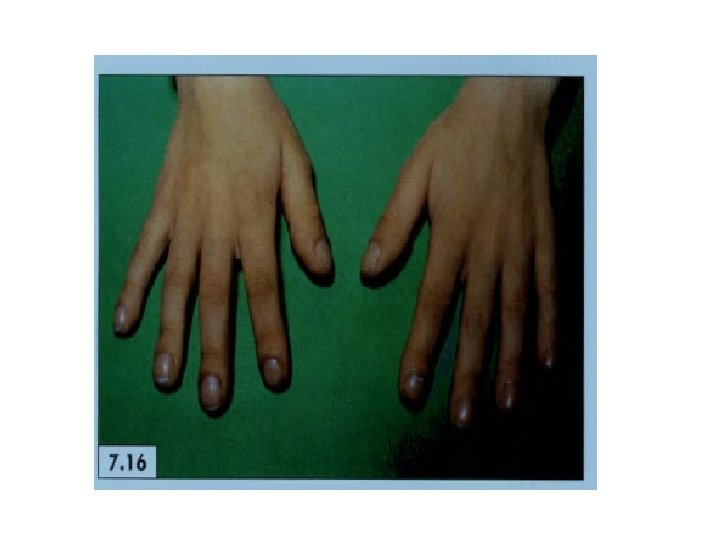
3 -Poor general health • weight loss. • anorexia. • lassitude, • low-grade fever, • failure to thrive in children. 4 -digital clubbing.
q. Pneumonia and pleurisy • fever, • Malaise • Recurrent pleurisy in the same site. q. Haemoptysis • Can, be the only symptom in so-called 'dry bronchiectasis'
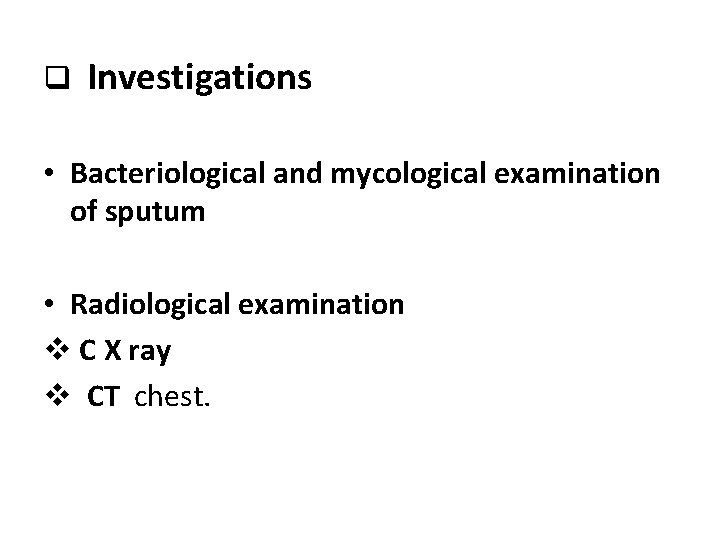
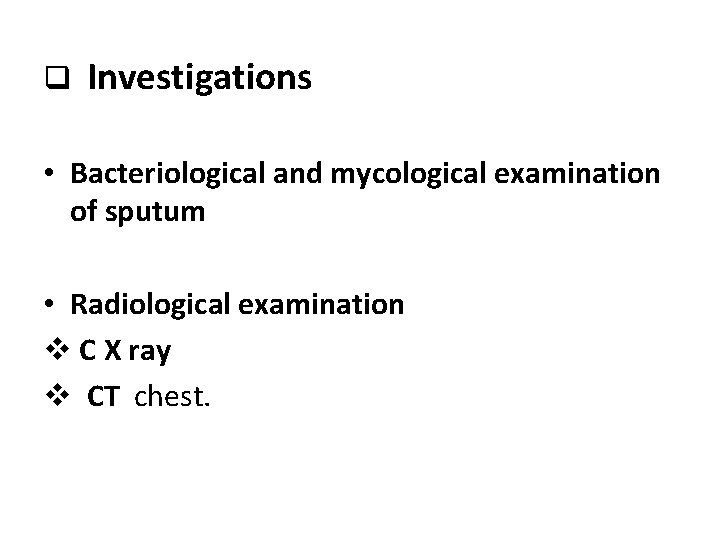
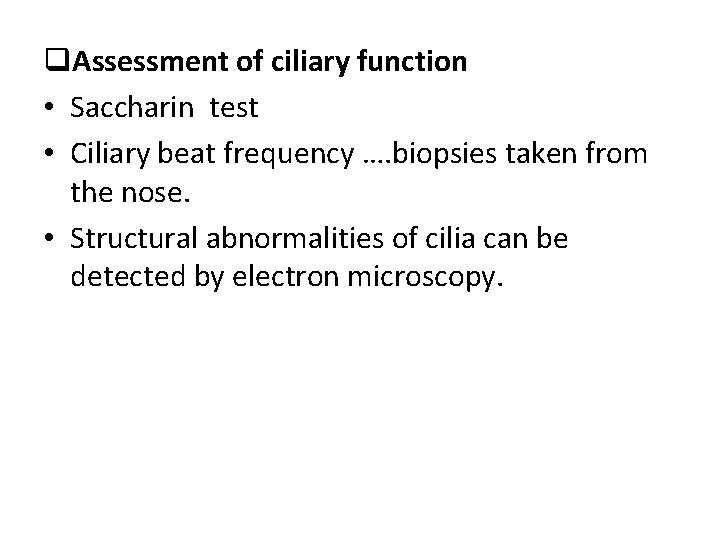
q Investigations • Bacteriological and mycological examination of sputum • Radiological examination v C X ray v CT chest.

CX RAY

CT CHEST
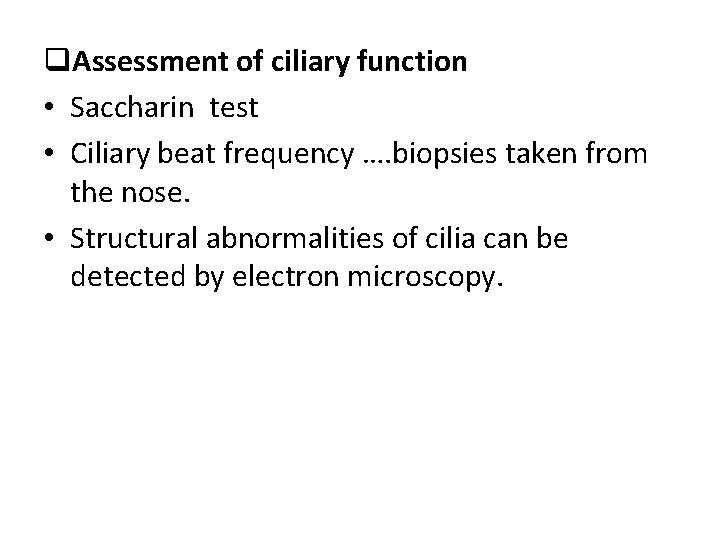
q. Assessment of ciliary function • Saccharin test • Ciliary beat frequency …. biopsies taken from the nose. • Structural abnormalities of cilia can be detected by electron microscopy.
q Physical signs • in the chest may be • 1 - unilateral 2 - bilateral. • May be no abnormal physical signs. • Numerous biphasic coarse crackles heard over the affected areas. • Collapse.
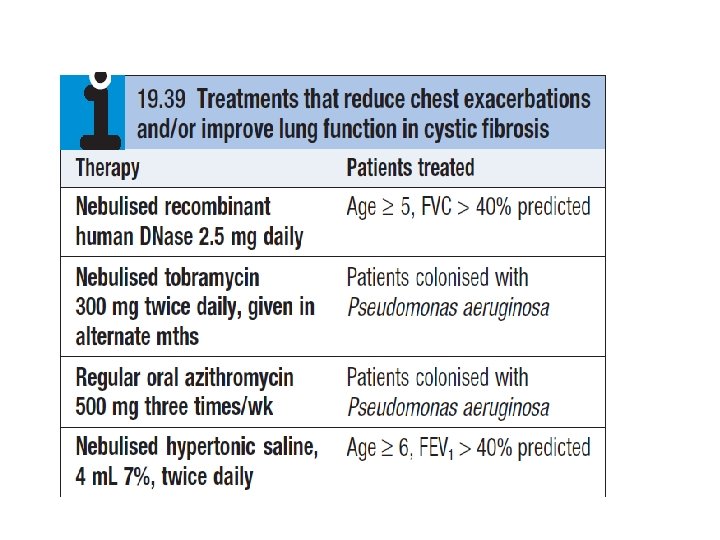
q Management v. In patients with airflow obstruction : • inhaled bronchodilators • corticosteroids. v. Physiotherapy : • 5 -10 minutes once or twice daily. v. Antibiotic therapy: • same as those used in COPD • larger doses and longer courses are required, .
secondary infection vstaphylococci and Gram-negative bacilli, in particular Pseudomonas species, antibiotic therapy should be guided by the microbiological sensitivities. v. For Pseudomonas, • oral ciprofloxacin (250 -750 mg 12 -hourly) or ceftazidime by intravenous injection or infusion (1 -2 g 8 -hourly) may be required.

q Haemoptysis • treating the underlying infection, • severe cases percutaneous embolisation by an interventional radiologist. q Surgical treatment • Excision of bronchiectatic areas.
q. Prognosis • progressive when associated with ciliary dysfunction and cystic fibrosis, • respiratory failure. • Good if physiotherapy is performed regularly and antibiotics are used. q Prevention • Childhood infection prophylaxis and treatment. • The early recognition and treatment of bronchial obstruction.
Cystic fibrosis • Genetics, pathogenesis and epidemiology • Cystic fibrosis (CF) is the most common fatal genetic disease in Caucasians, with autosomal recessive inheritance, . • CF is the result of mutations affecting a gene
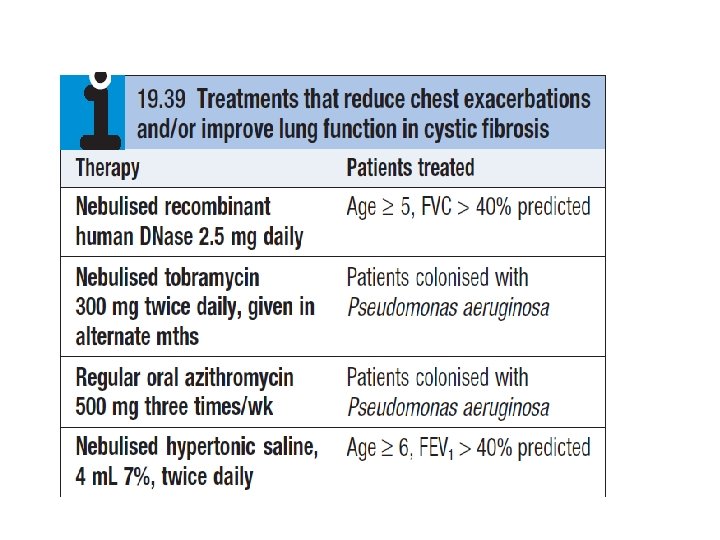
• • • • Clinical features The lungs are macroscopically normal at birth, bronchiectasis in childhood. Recurrent exacerbations of bronchiectasis, initially in the upper lobes but subsequently throughout both lungs. • Most men with CF are infertile
Complications of cystic fibrosis 1 -Respiratory • Infective exacerbations of bronchiectasis • Spontaneous pneumothorax • Haemoptysis • Nasal polyps • Respiratory failure • Cor pulmonale • Lobar collapse due to secretions
2 -Gastrointestinal • Malabsorption and steatorrhoea • others 3 -Others • Diabetes (25% of adults) • Male infertility
Thank you • Any Q
 Oncocytoma salivary gland
Oncocytoma salivary gland Uremia pathogenesis
Uremia pathogenesis Pathogenesis of cholecystitis
Pathogenesis of cholecystitis Acute cholecystitis clinical features
Acute cholecystitis clinical features Bacterial pathogenesis
Bacterial pathogenesis Cholecystitis pathogenesis
Cholecystitis pathogenesis Bacterial pathogenesis
Bacterial pathogenesis Risus sardonicus
Risus sardonicus Jaundice pathogenesis
Jaundice pathogenesis Pathogenesis dengue fever
Pathogenesis dengue fever Rabies pathogenesis
Rabies pathogenesis Prepenetration
Prepenetration Pathogenesis game
Pathogenesis game Pathogenesis of copd
Pathogenesis of copd Cirrhosis pathogenesis
Cirrhosis pathogenesis Histoplasma capsulatum pathogenesis
Histoplasma capsulatum pathogenesis Pathogenesis of chronic pyelonephritis
Pathogenesis of chronic pyelonephritis Pathogenesis of hemolytic anemia
Pathogenesis of hemolytic anemia Mechanism of ischemic stroke
Mechanism of ischemic stroke Pathogenesis of tuberculosis
Pathogenesis of tuberculosis Etiology in criminology
Etiology in criminology Multicausal model of addiction
Multicausal model of addiction Mild moderate severe asthma exacerbation
Mild moderate severe asthma exacerbation Asthmatic lung x ray
Asthmatic lung x ray Pathophysiology of appendicitis
Pathophysiology of appendicitis Difference between rampant caries and nursing bottle caries
Difference between rampant caries and nursing bottle caries Examples of pes
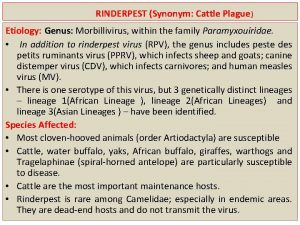
Examples of pes Etiology
Etiology Circling back synonym
Circling back synonym Etiology
Etiology Periradicular
Periradicular Color of amniotic fluid
Color of amniotic fluid Tccdtccd
Tccdtccd Etiology synonym
Etiology synonym