TMJ Introduction Joint between temporal bone cranial bone
TMJ
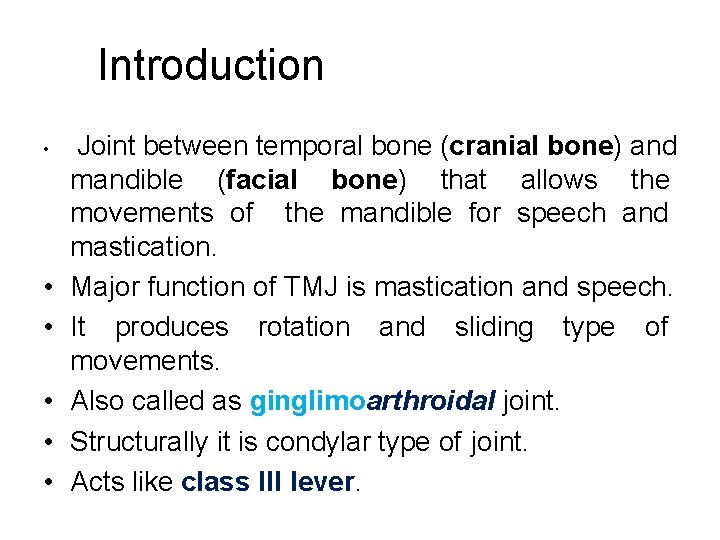
Introduction • • • Joint between temporal bone (cranial bone) and mandible (facial bone) that allows the movements of the mandible for speech and mastication. Major function of TMJ is mastication and speech. It produces rotation and sliding type of movements. Also called as ginglimoarthroidal joint. Structurally it is condylar type of joint. Acts like class III lever.
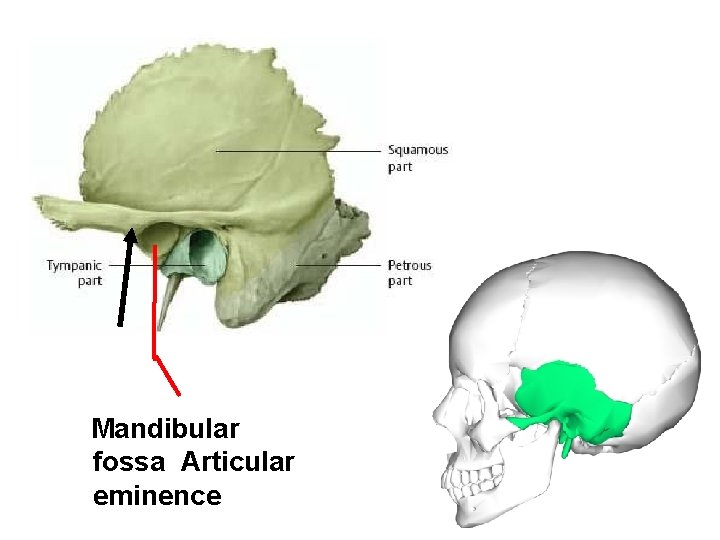
Mandibular fossa Articular eminence
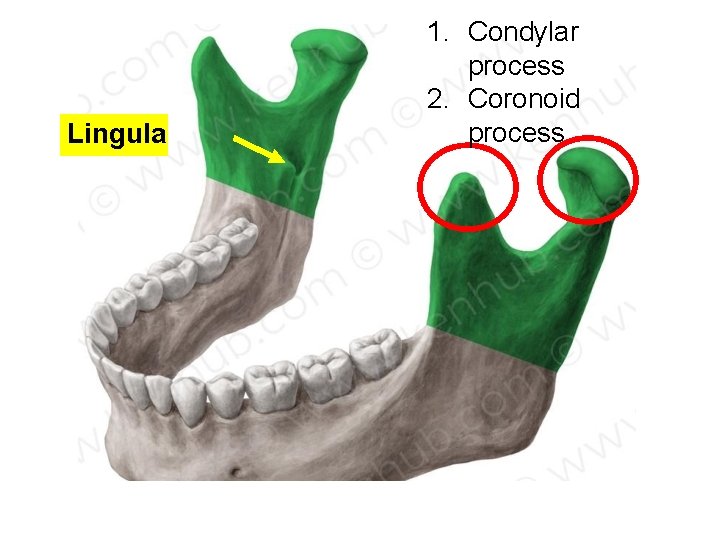
Lingula 1. Condylar process 2. Coronoid process
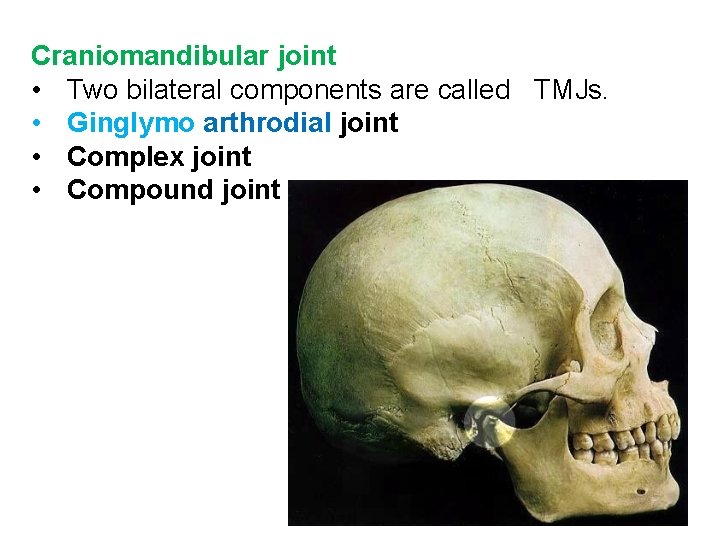
Craniomandibular joint • Two bilateral components are called TMJs. • Ginglymo arthrodial joint • Complex joint • Compound joint

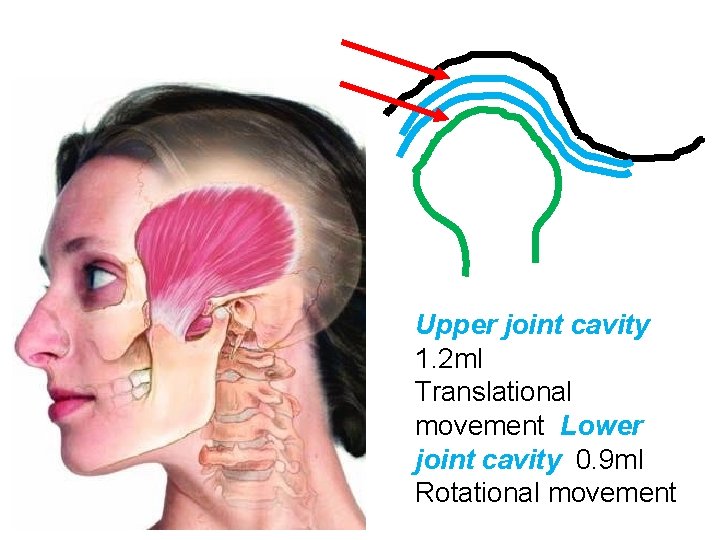
Upper joint cavity 1. 2 ml Translational movement Lower joint cavity 0. 9 ml Rotational movement
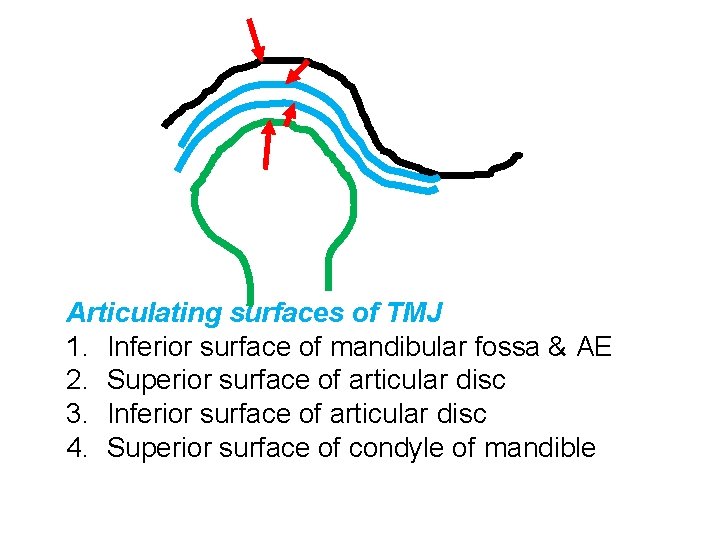
Articulating surfaces of TMJ 1. Inferior surface of mandibular fossa & AE 2. Superior surface of articular disc 3. Inferior surface of articular disc 4. Superior surface of condyle of mandible
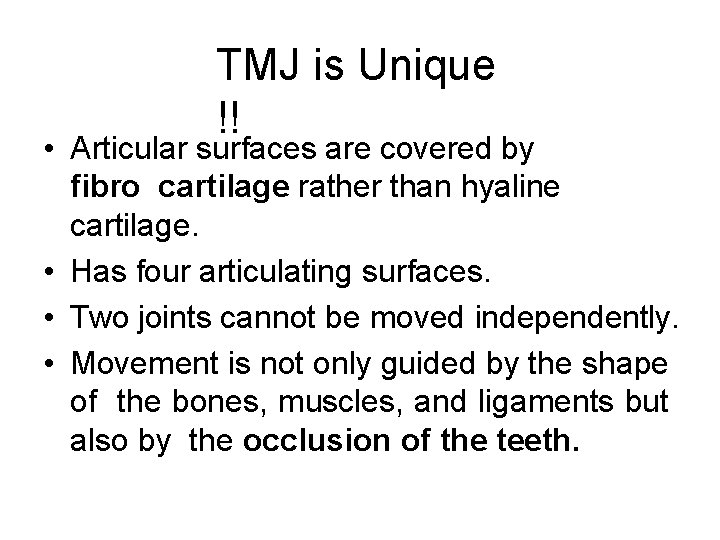
TMJ is Unique !! • Articular surfaces are covered by fibro cartilage rather than hyaline cartilage. • Has four articulating surfaces. • Two joints cannot be moved independently. • Movement is not only guided by the shape of the bones, muscles, and ligaments but also by the occlusion of the teeth.
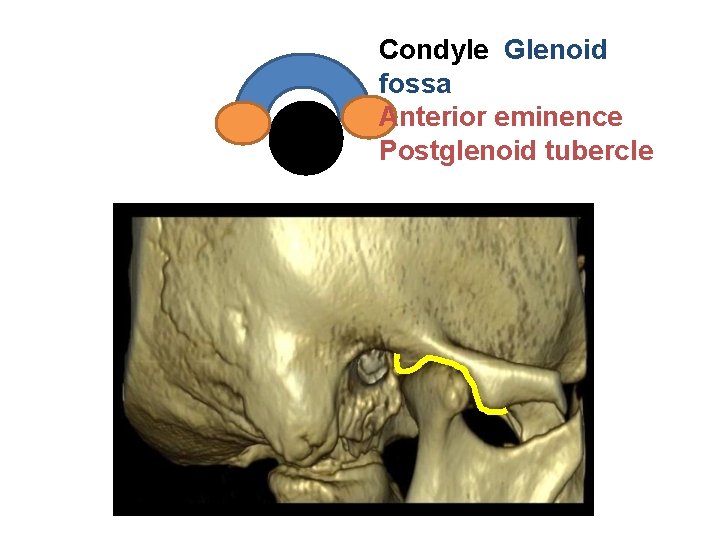
Condyle Glenoid fossa Anterior eminence Postglenoid tubercle
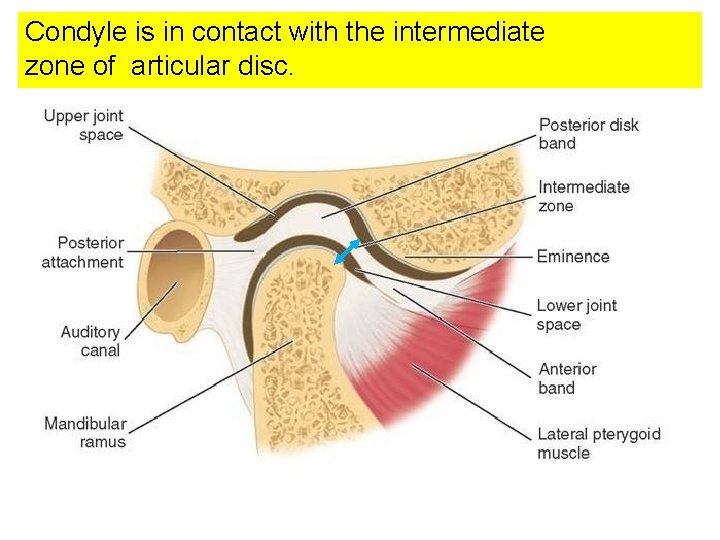
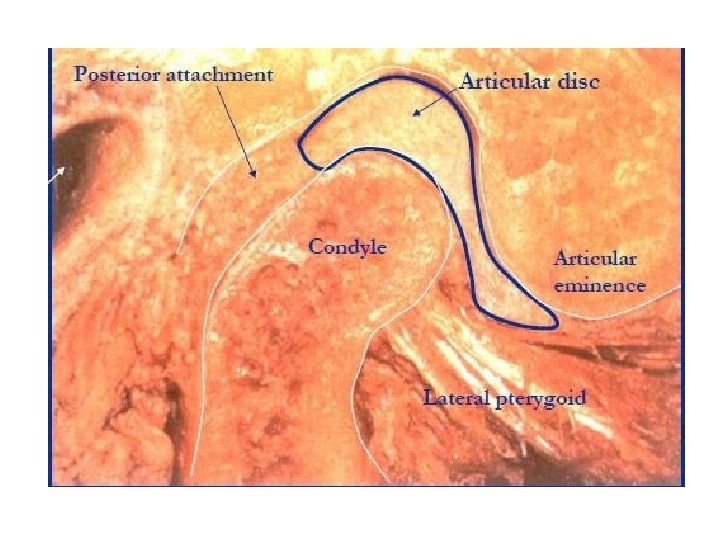
Condyle is in contact with the intermediate zone of articular disc.
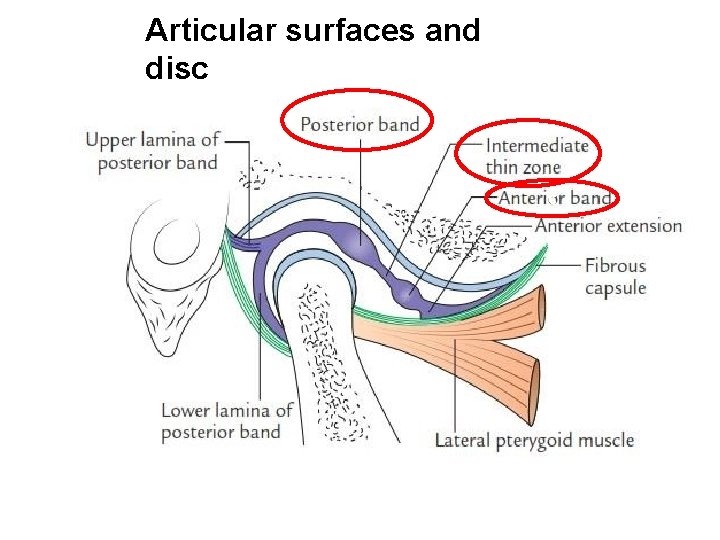
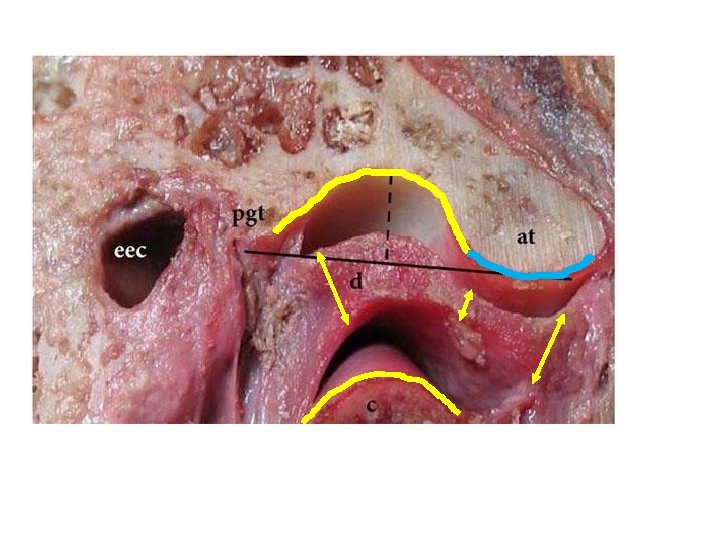
Articular surfaces and disc c
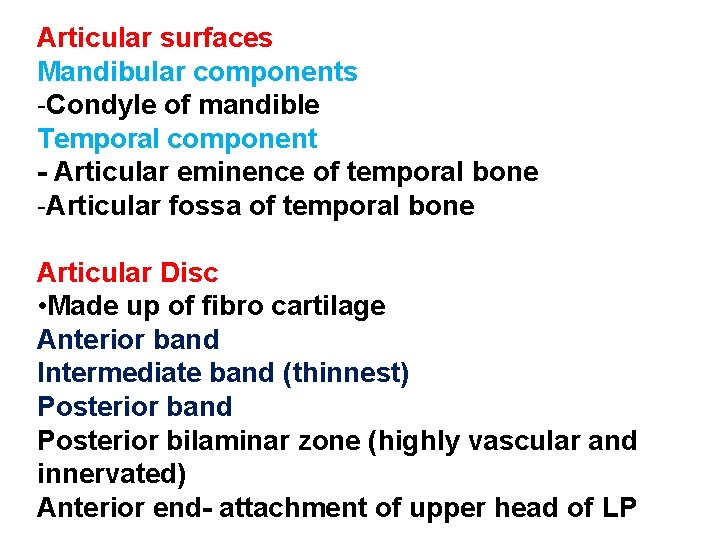
Articular surfaces Mandibular components -Condyle of mandible Temporal component - Articular eminence of temporal bone -Articular fossa of temporal bone Articular Disc • Made up of fibro cartilage Anterior band Intermediate band (thinnest) Posterior band Posterior bilaminar zone (highly vascular and innervated) Anterior end- attachment of upper head of LP
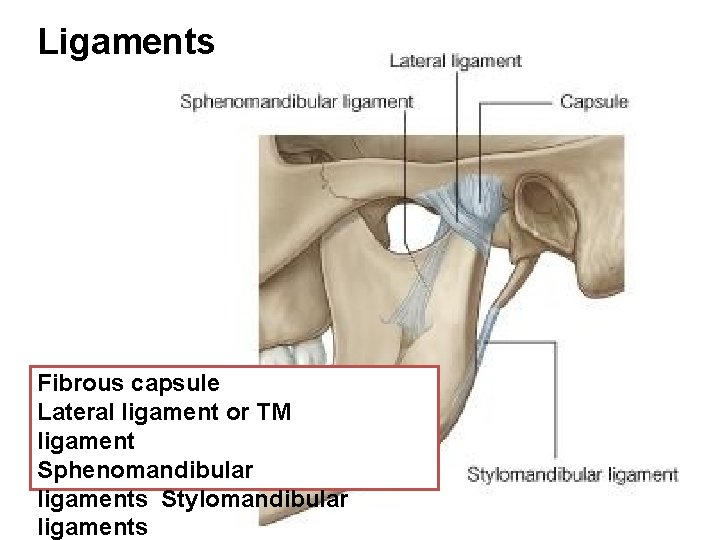
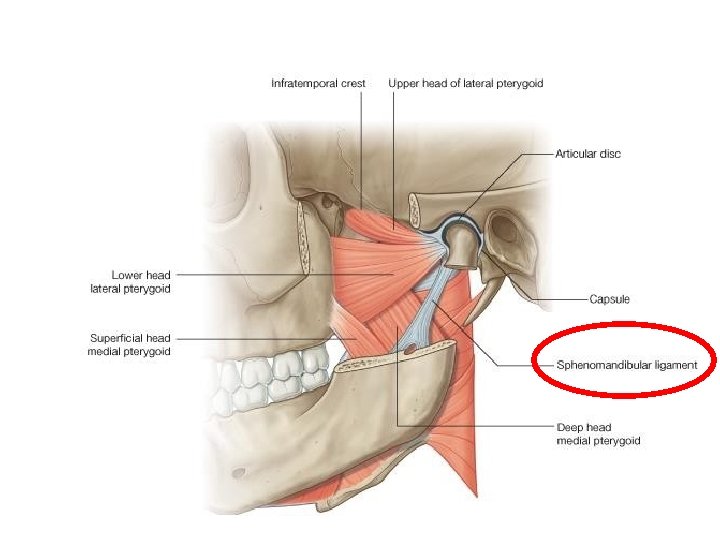
Ligaments Fibrous capsule Lateral ligament or TM ligament Sphenomandibular ligaments Stylomandibular ligaments
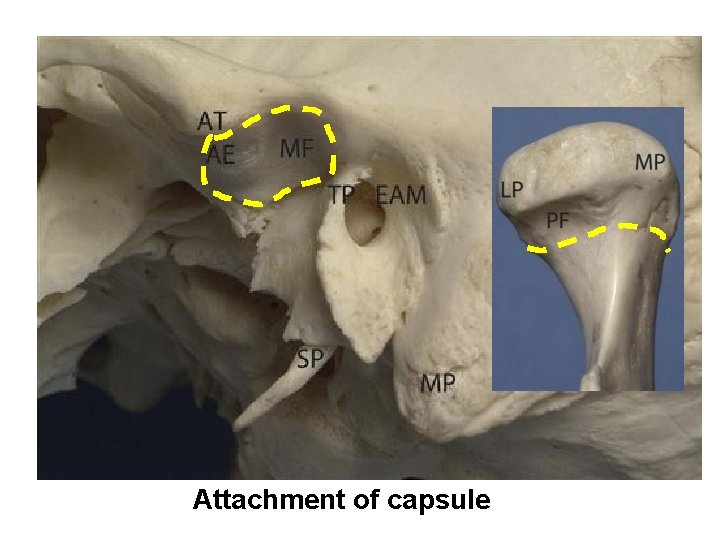
Attachment of capsule
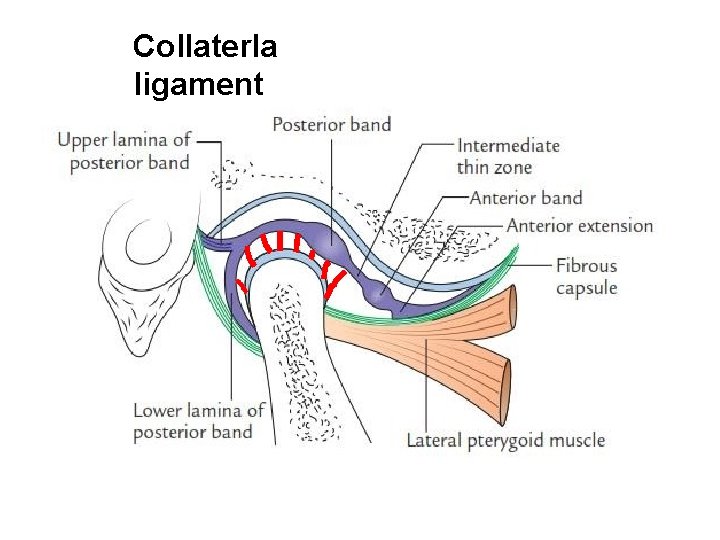
Collaterla ligament
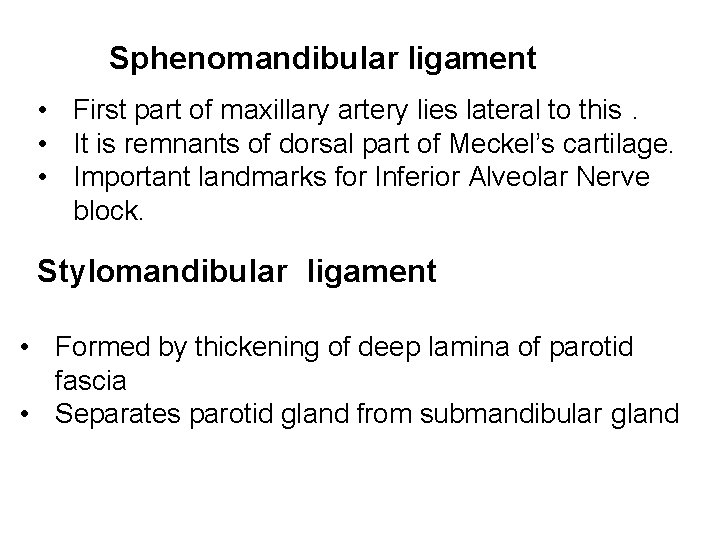
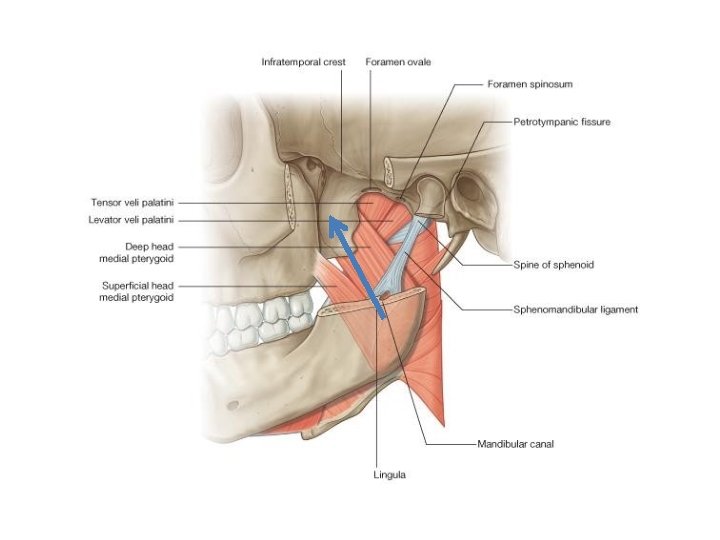
Sphenomandibular ligament • First part of maxillary artery lies lateral to this. • It is remnants of dorsal part of Meckel’s cartilage. • Important landmarks for Inferior Alveolar Nerve block. Stylomandibular ligament • Formed by thickening of deep lamina of parotid fascia • Separates parotid gland from submandibular gland
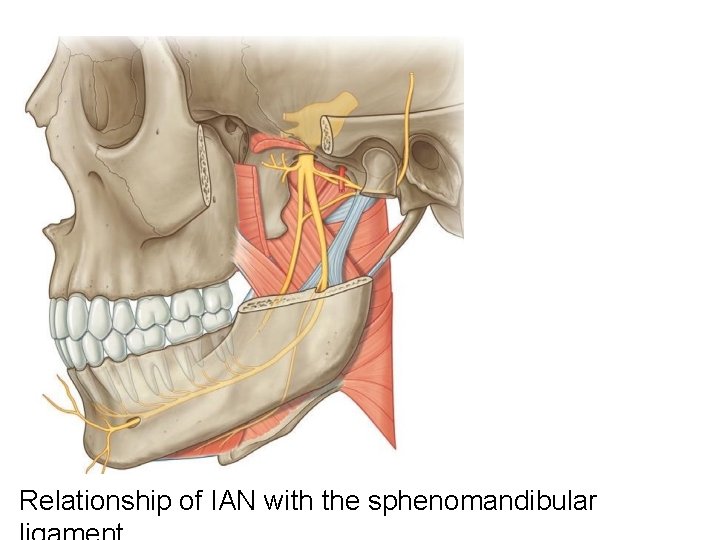
Relationship of IAN with the sphenomandibular
Resting position of TMJ • Condyle lies in mandibular fossa. • Lip are closed. • Teeth are separated with slight space.
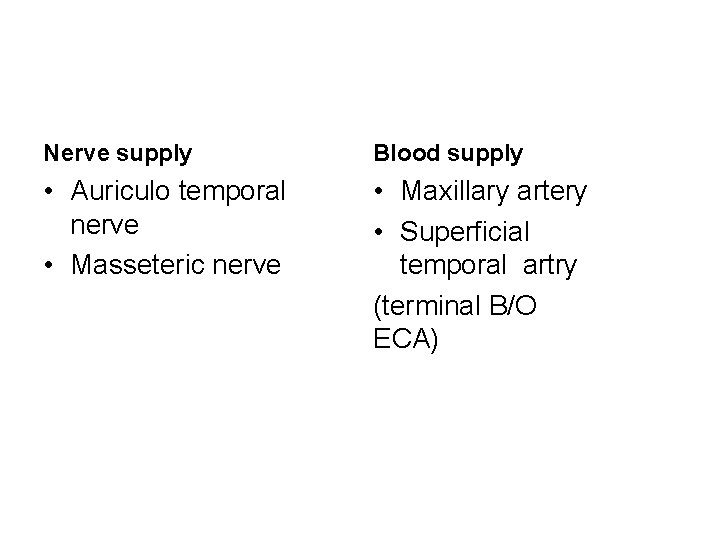
Nerve supply Blood supply • Auriculo temporal nerve • Masseteric nerve • Maxillary artery • Superficial temporal artry (terminal B/O ECA)
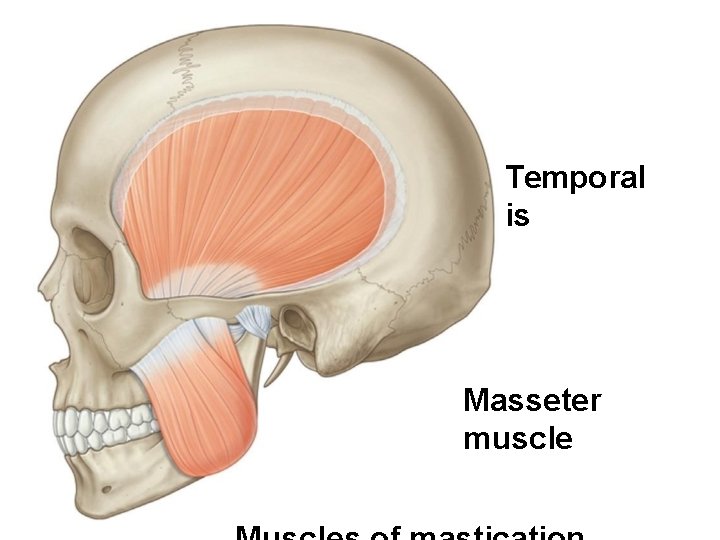
Temporal is Masseter muscle
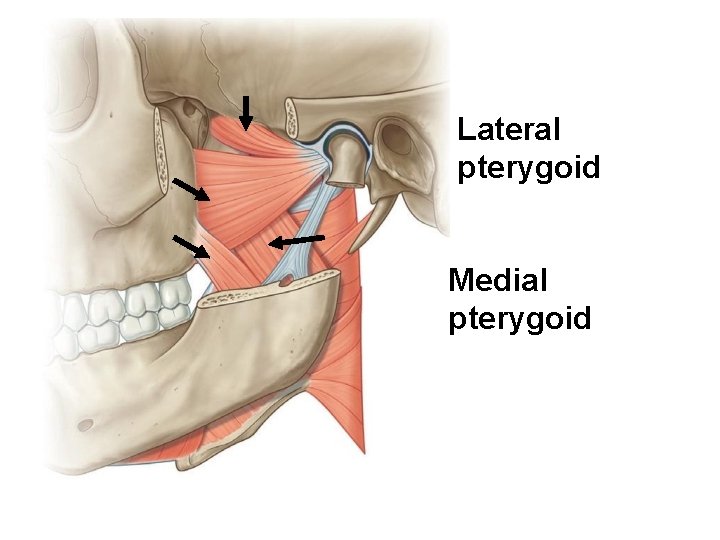
Lateral pterygoid Medial pterygoid
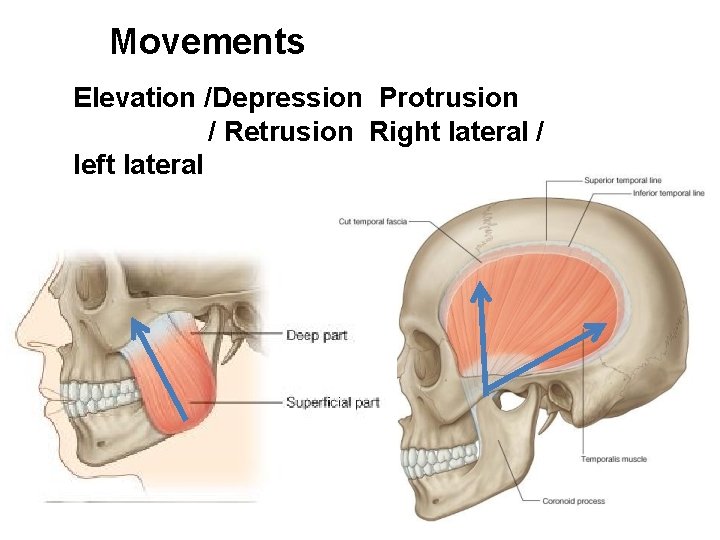
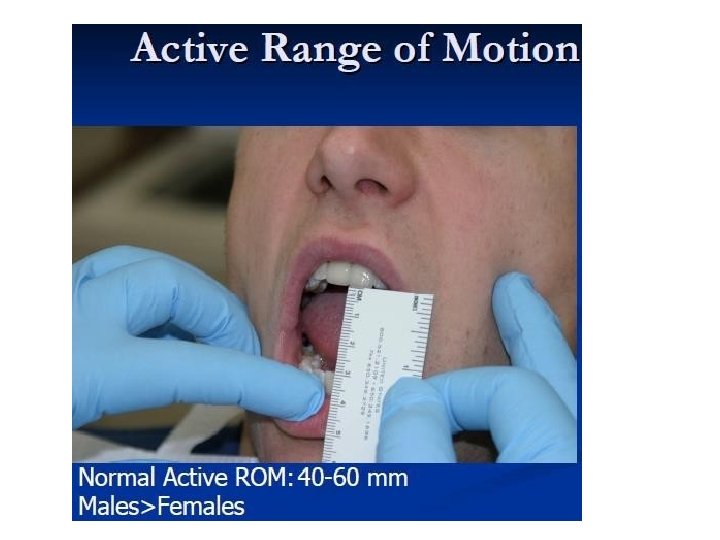
Movements Elevation /Depression Protrusion / Retrusion Right lateral / left lateral
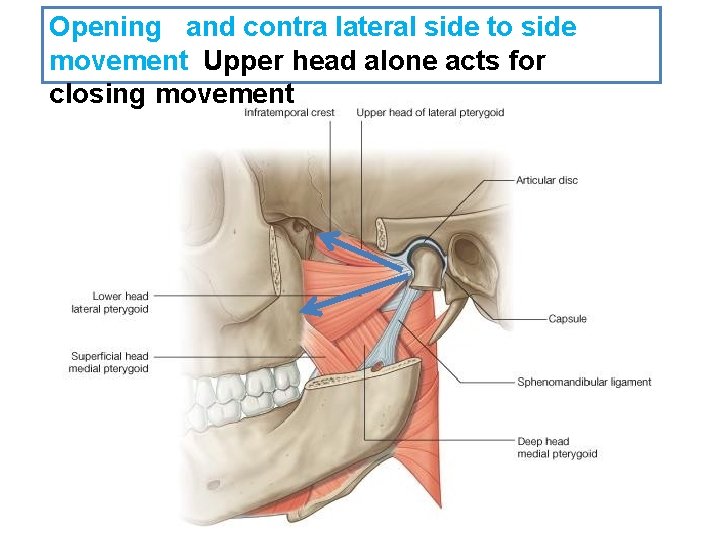
Opening and contra lateral side to side movement Upper head alone acts for closing movement
Movements of TMJ Elevation: all the muscles except LP Depression : LP Protrusion : LP and MP Retrusion: posterior fibers of temporalis Side to side: LP and MP together
TMJ disorders • The most common condition affecting the region is temporomandibul ar mandibular dysfunction, or myofascial pain dysfunction syndrome(MPDS) Pain Muscle spasm Limited jaw opening Joint sounds
TMJ dislocation • Condyle displaced anterior to articular eminence • Causes: Too wide mouth opening Missing teeth Trauma • Anterior dislocation is more common.
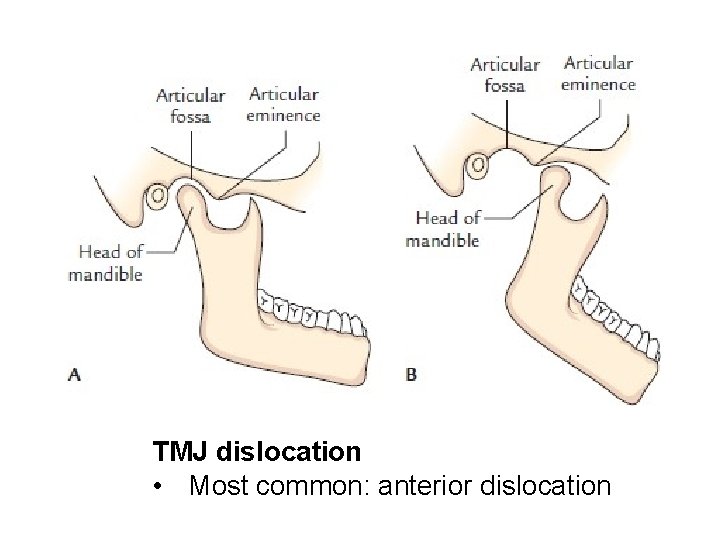
TMJ dislocation • Most common: anterior dislocation
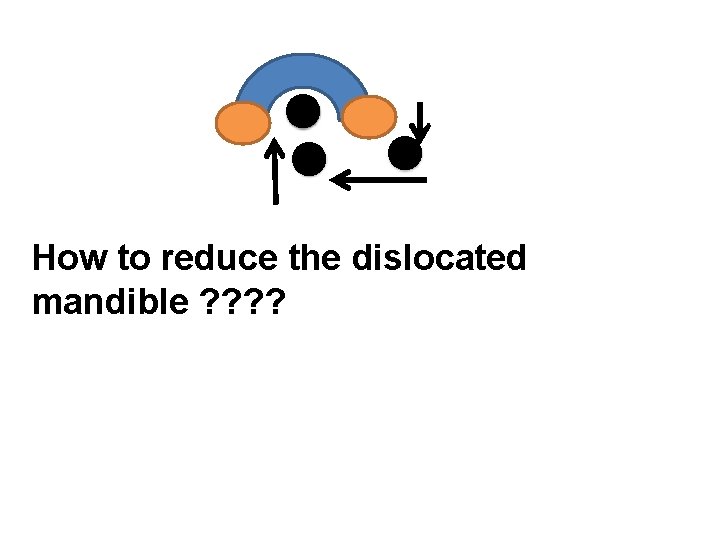
How to reduce the dislocated mandible ? ?

Barton’s Bandage for mandibular fracture.
- Slides: 35