Tissue Response to Injury Pages 272 292 Objectives
Tissue Response to Injury Pages 272 -292
Objectives 1= Unable to define terms, explain or apply this to any examples. 2= Able to define terms and/or explain this idea. 3= Able to define terms, explain and apply this to examples. • _____ Contrast the three phases of the healing process • _____ Classify the physiological events that must take place during each phase of healing • _____ ID factors that will impede the healing process • _____ Discuss healing process relative to various soft tissue structures including cartilage, ligament, muscle, tendon, and nerve tissue • _____ Describe the healing process in bones • _____ Formulate a management plan for treating acute fractures • _____ Define pain and discuss types of pain • _____ Understand the neurophysiology of pain • _____ Examine techniques for assessing pain
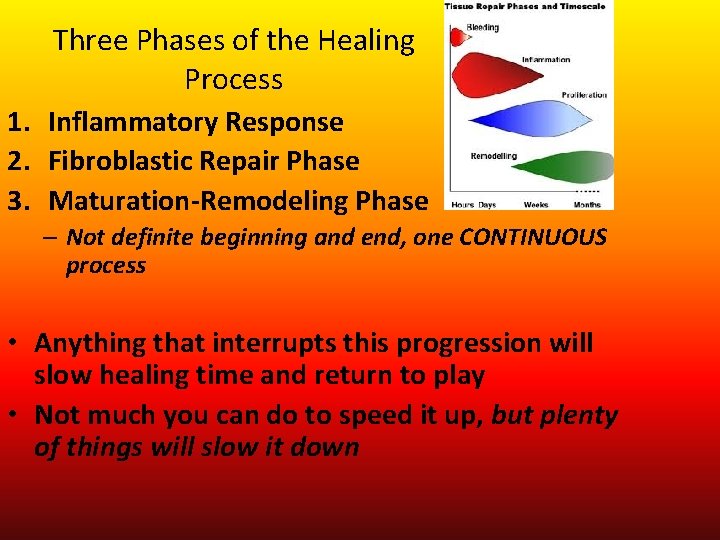
Three Phases of the Healing Process 1. Inflammatory Response 2. Fibroblastic Repair Phase 3. Maturation-Remodeling Phase – Not definite beginning and end, one CONTINUOUS process • Anything that interrupts this progression will slow healing time and return to play • Not much you can do to speed it up, but plenty of things will slow it down

Inflammatory Response • Begins IMMEDIATELY after an injury occurs • Result of injury to the cells themselves • • • Rubor: redness Tumor: swelling Dolor: pain and tenderness Calor: increased temp Functio laesa: decreased function • INFLAMMATION MUST OCCUR! • Leukocytes (white blood cells) phagocytize (digest and destroy) which gets rid of injury by-products

Inflammation Stages 1. Acute Inflammation – – • Vascular Reaction Clot formation 2 -4 days 2. Chronic inflammation – Occurs when acute response does not eliminate the injuring agent
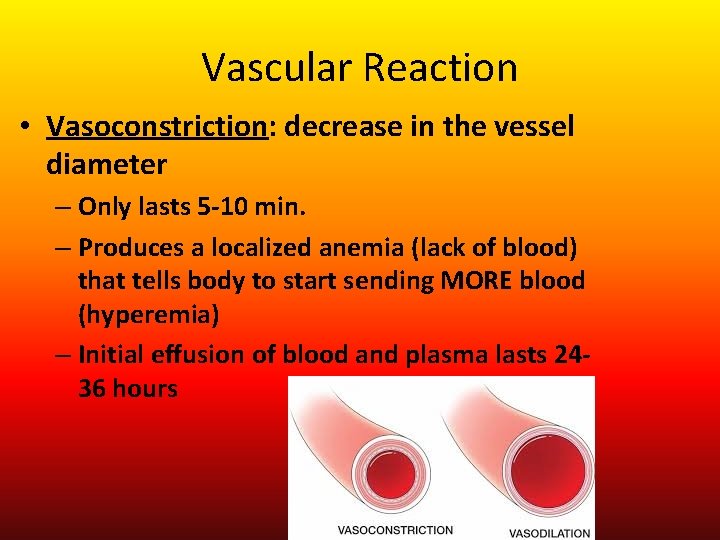
Vascular Reaction • Vasoconstriction: decrease in the vessel diameter – Only lasts 5 -10 min. – Produces a localized anemia (lack of blood) that tells body to start sending MORE blood (hyperemia) – Initial effusion of blood and plasma lasts 2436 hours
Vascular Reaction • Chemical Mediators: help limit the amount of swelling, more damage causes more swelling 1. Histamine: released by mast cells, causes vasodilation and increases vessels permeability to WBC’s 2. Leukotaxin: helps WBC’s line up along blood vessel walls, also increases cell permeability 3. Necrosin: increases phagocytic activity of WBC’s
Clot Formation • Platelets don’t normally stick to vessels walls but injury exposes collagen fibers – Platelets like collagen fibers • Lasts from 12 -48 hours after an injury • Thromboplastin: protein that converts prothrombin to thrombin – This transformation causes soluble fibrinogen to turn to insoluble fibrin (CLOT) • Process “walls off” injured area for the rest of the healing process https: //www. youtube. com/watch? v=--b. ZUeb 83 u. U 2 min clot fomration
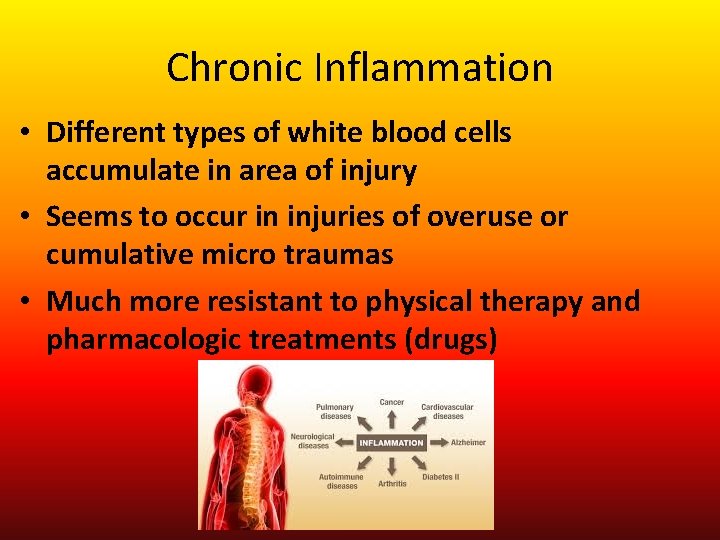
Chronic Inflammation • Different types of white blood cells accumulate in area of injury • Seems to occur in injuries of overuse or cumulative micro traumas • Much more resistant to physical therapy and pharmacologic treatments (drugs)
Fibroblastic Repair • Scar formation and tissue repair • Fibroplasia: period of scar formation – Lasts up to 6 weeks – Complaints of tenderness and pain disappear – Oxygen supply is increased – Blood flow increased • Granulation Tissue replaces clot: – Fibroblasts: line up parallel to capillaries – Collagen – Capillaries reform
Extracellular Matrix • Collagen: strong connective tissues arranged randomly – Increases tensile strength • Elastin • Ground Substance – Proteoglycans – Glycosaminoglycans

Scar Formation • If the repair stage goes correctly min. scarring is formed • If inflammation keeps reappearing: – Longer Repair time – Large Scars – Irreversible tissue damage • Adhesive capsulitis • Permanently tight connective tissue
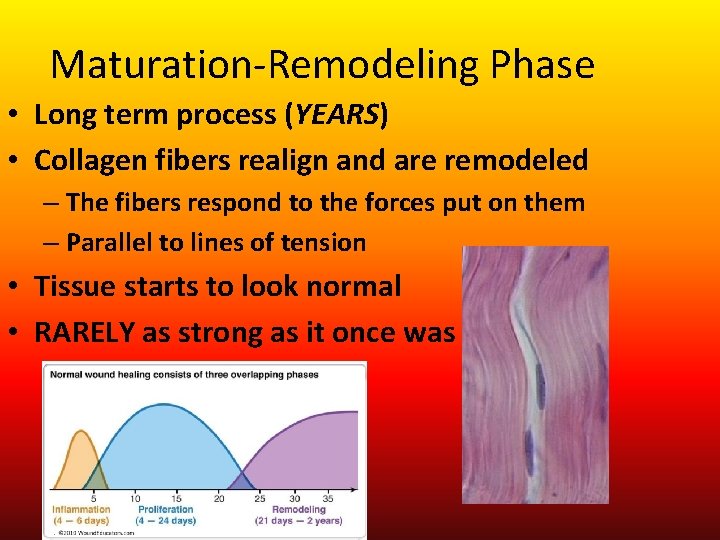
Maturation-Remodeling Phase • Long term process (YEARS) • Collagen fibers realign and are remodeled – The fibers respond to the forces put on them – Parallel to lines of tension • Tissue starts to look normal • RARELY as strong as it once was
Controlled Movement during Healing • Wolfes Law: bone and soft tissue will respond to the physical demands placed on them, causing them to remodel or realign along lines of tensile force – you must expose injured structures to force during rehab!

Mobility per phase • Immobilization should be limited to the inflammatory stage • Repair stage: controlled activity aimed at return to normal flexibility and strength – with protective equipment • Remodeling Phase: aggressive active ROM and strengthening exercises – helps with collagen realignment • PAIN DICTATES PROGRESSION THROUGH REHAB
- Slides: 15