TIPS FOR BEING A SUCCCESSFUL PRECEPTOR Ian Jones
TIPS FOR BEING A SUCCCESSFUL PRECEPTOR Ian Jones, CCPA and John Shea, CCPA Saturday October 29 th, 2016
At the conclusion of this session, participants will be able to: Assess learning needs and set goals for PA-Students Develop and implement a learning plan Teach time management and prioritization in providing care to a patient population Evaluate clinical competence and documenting learning and clinical progress Teach and promote clinical reasoning, critical thinking, and problemsolving Provide constructive feedback and coaching Role-model evidence-based professional practice
Let’s begin by saying thank you The clinical setting synthesizes concepts and application of principles for quality health care delivery. You, as a clinical preceptor, are the key to successful learning experiences in the clinical setting Physician Assistant Education Association
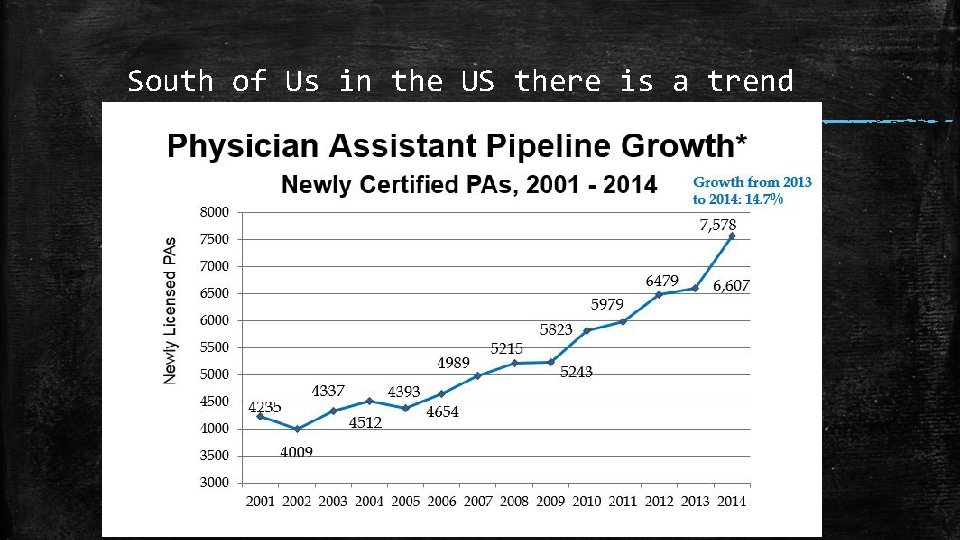
South of Us in the US there is a trend
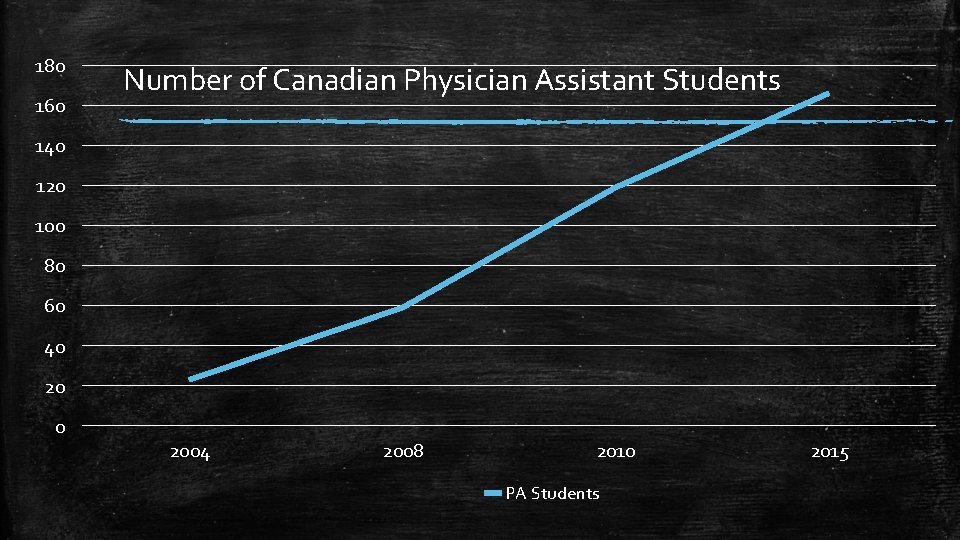
180 160 Number of Canadian Physician Assistant Students 140 120 100 80 60 40 2004 2008 2010 PA Students 2015

The Preceptor Role Model, Mentor, Critic, Supporter, Teacher, Director, Candlestick Maker Ian J.
General Goals of the Clinical Year Move from theoretical to active Prepare a lifetime of continued refinement of skills Expand knowledge as a practicing PA ▪ Expand develop the medical fund of knowledge ▪ Perfect the art of history taking and physical examination skills ▪ Sharpen and refine oral presentation and written documentation skills ▪ Develop interpersonal skills and professionalism necessary to function as part of a medical team

Preceptor Responsibilities ▪ Orient students at the onset of the rotation ▪ Provide ongoing and timely feedback ▪ Supervise, demonstrate, teach, and observe ▪ Delegate to the student increasing levels of responsibility Supervision, Observation, Teaching, Evaluation, Promotion of learning Dialogue (faculty)
Modelling Ethical Approach Cultural Competency Clinical Practice Critical Thinking Communication Professionalism
Preceptor−Student Relationship ▪ Professional boundaries ▪ Avoid Social Media Exchanges ▪ Social activities & personal relationships outside of the professional learning environment should be appropriate and carefully selected so as not to put the student or preceptor in a compromising situation. ▪ Avoid taking them for a drink
Preparing Staff ▪ Student need to learn about office, clinic, or ward routines and the location of critical resources ▪ Students should communicate with the staff about procedures for making appointments, retrieving medical records, bringing patients into examination rooms, ordering tests, retrieving test results, and charting.
Do not assume all know what role the student will have in a practice Reach out to receptionists, schedulers, and nursing staff in advance of the student’s arrival to discuss: ▪ Student’s name, Schedule, Expected role in patient care ▪ Expected effect of the student on office operation: Will fewer patients be scheduled? Will the preceptor be busier? ▪ How patients will be scheduled for the student
Successful Clinical Experiences Setting it up to be positive John S.

The Successful Clinical Experience Setting the Stage Your Expectations Student’s Expectations Discussion Mutual agreement on the clinical experience
Orientation and Communicating Student Expectations – First Day make it clear Hours , General attendance, Call schedules, Overnight/weekend schedules Where to park, eat, sleep, dump (their gear) Participation during rounds and conferences Expectations for clinical care, patient interaction, and procedures Oral presentations, Assignments Written documentation, Write-ups, Signing Interactions with office and professional staff Anything additional that the preceptor feels is necessary
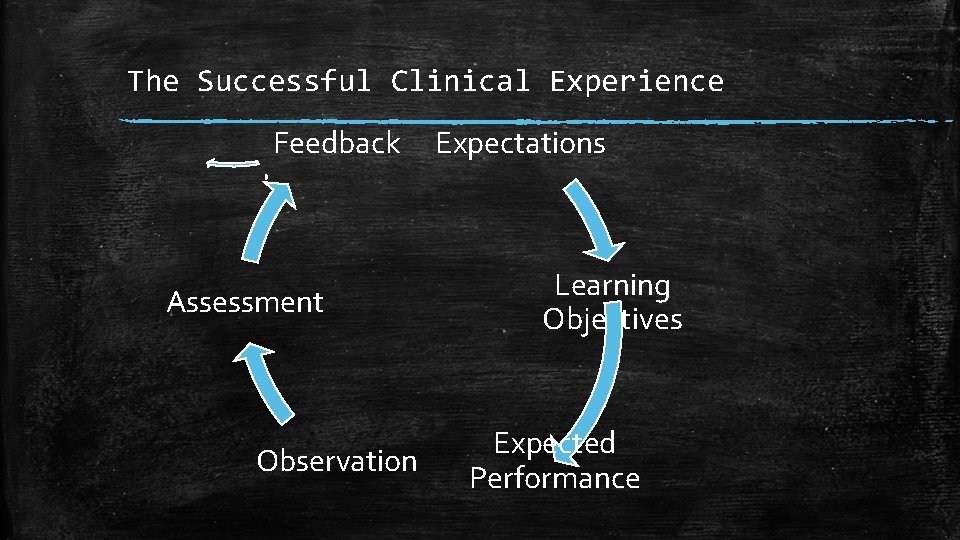
The Successful Clinical Experience Feedback Assessment Observation Expectations Learning Objectives Expected Performance
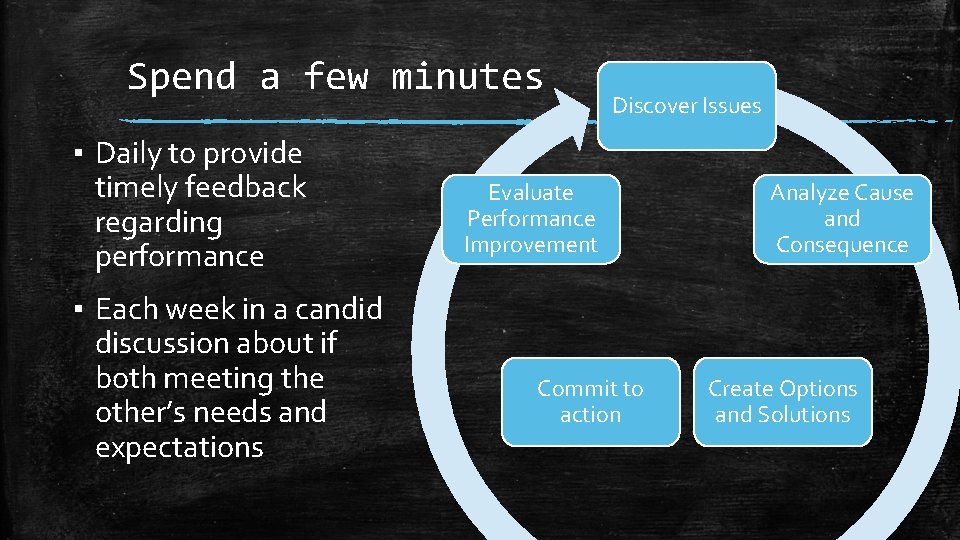
Spend a few minutes ▪ Daily to provide timely feedback regarding performance ▪ Each week in a candid discussion about if both meeting the other’s needs and expectations Discover Issues Evaluate Performance Improvement Commit to action Analyze Cause and Consequence Create Options and Solutions
What is Feedback? Feedback is about sharing information with learners, with a view to narrowing the gap between observed and desired performance; it encourages learners to reflect on what they have done and to think about making appropriate changes. Cantillon 2008
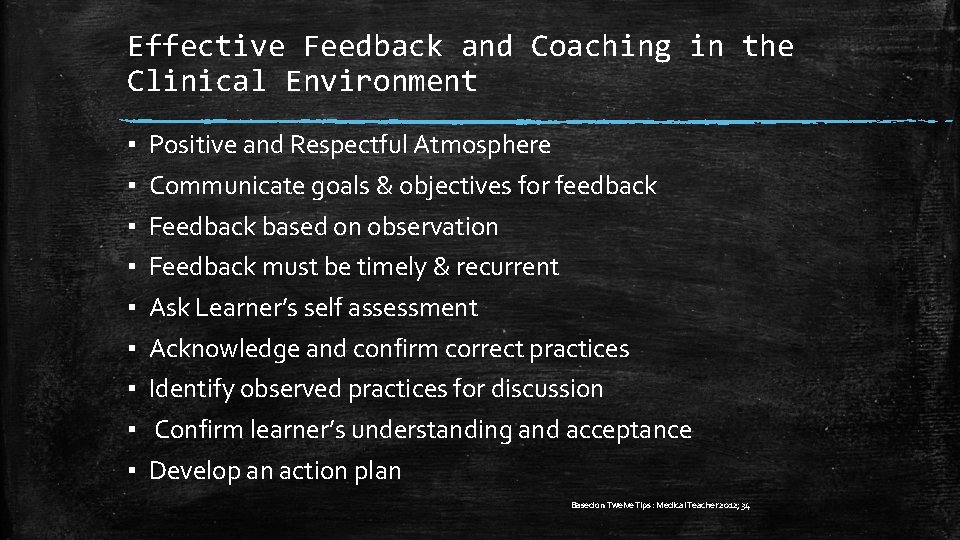
Effective Feedback and Coaching in the Clinical Environment ▪ ▪ ▪ ▪ ▪ Positive and Respectful Atmosphere Communicate goals & objectives for feedback Feedback based on observation Feedback must be timely & recurrent Ask Learner’s self assessment Acknowledge and confirm correct practices Identify observed practices for discussion Confirm learner’s understanding and acceptance Develop an action plan Based on Twelve Tips : Medical Teacher 2012; 34
Assessing Learning needs Relevant Concern Identification - What is the concern? Knowledge, Skill or Attitude - Who is the problem? Learner, Educator or System Identification to Concern Definition - What is the issue? - What is the Learner’s Perception? - What are the learner’s strengths & weaknesses? - What factors are contributing influences? - What are your strengths & weaknesses? - How do other see the learner ?
Developing and Implementing a Learning Plan (con’t) Definition to Intervention - What problem are you trying to address - How will the problem be addressed - Who will be involved in the intervention - What is the time line for the intervention - How will the intervention be evaluated
SMART Learning Plan ▪ Specific -- Detailed and focused ▪ Measurable -- Quantifiable ▪ Attainable -- Must be consistent with the level of education & training ▪ Relevant -- Within your scope of practice ▪ Time -- limited with a set endpoint Doran GT 1981/CNO 2014
Documentation (If allowed) ▪ Remind that the medical record is a legal document ▪ All medical entries must be identified as “student” and must include the PA student’s signature with the designation “PA-S. ” ▪ Preceptors are required to document the services (to bill, medical-legal)
Evaluating Clinical competence Competency Frameworks Ian J.
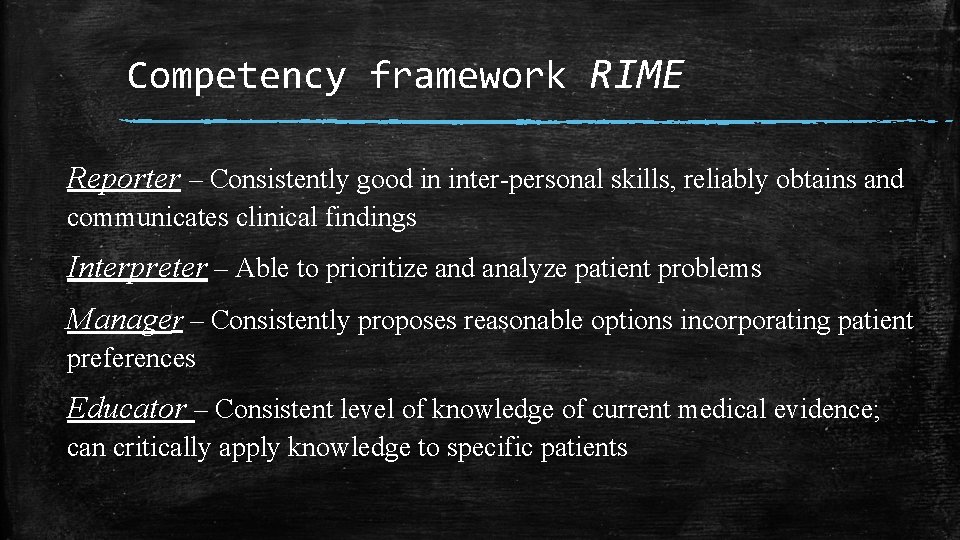
Competency framework RIME Reporter – Consistently good in inter-personal skills, reliably obtains and communicates clinical findings Interpreter – Able to prioritize and analyze patient problems Manager – Consistently proposes reasonable options incorporating patient preferences Educator – Consistent level of knowledge of current medical evidence; can critically apply knowledge to specific patients
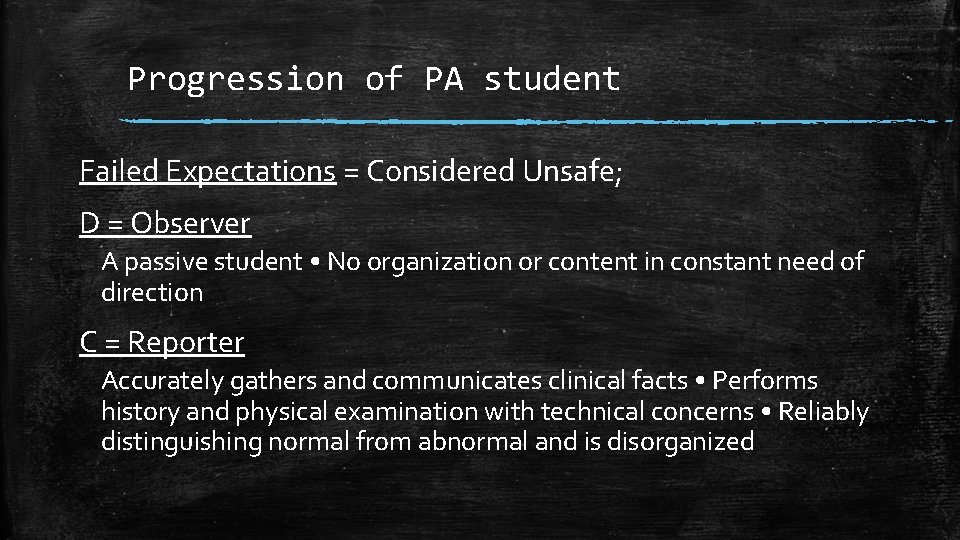
Progression of PA student Failed Expectations = Considered Unsafe; D = Observer A passive student • No organization or content in constant need of direction C = Reporter Accurately gathers and communicates clinical facts • Performs history and physical examination with technical concerns • Reliably distinguishing normal from abnormal and is disorganized
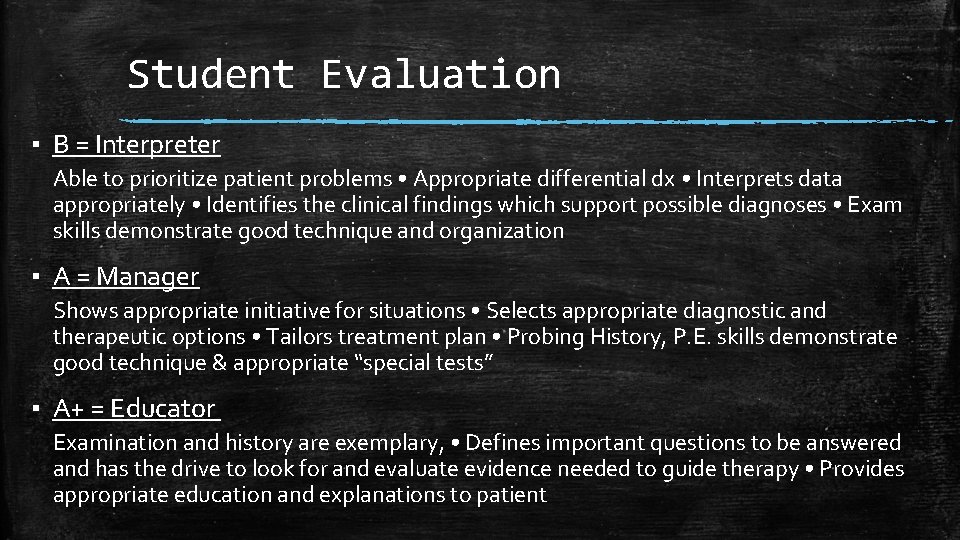
Student Evaluation ▪ B = Interpreter Able to prioritize patient problems • Appropriate differential dx • Interprets data appropriately • Identifies the clinical findings which support possible diagnoses • Exam skills demonstrate good technique and organization ▪ A = Manager Shows appropriate initiative for situations • Selects appropriate diagnostic and therapeutic options • Tailors treatment plan • Probing History, P. E. skills demonstrate good technique & appropriate “special tests” ▪ A+ = Educator Examination and history are exemplary, • Defines important questions to be answered and has the drive to look for and evaluate evidence needed to guide therapy • Provides appropriate education and explanations to patient

Student Feedback One Minute Preceptor 1. Get a commitment 2. Probe for supporting evidence 3. Teach general rules 4. Reinforce what is right 5. Correct Mistakes ▪ Neher et al J Am Board Fam Prac 1992; 5: 419 -24
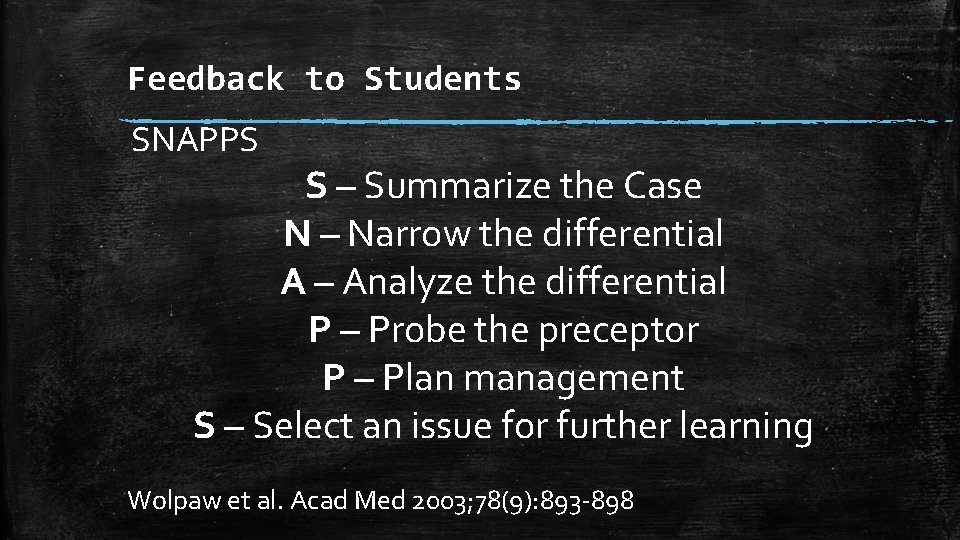
Feedback to Students SNAPPS S – Summarize the Case N – Narrow the differential A – Analyze the differential P – Probe the preceptor P – Plan management S – Select an issue for further learning Wolpaw et al. Acad Med 2003; 78(9): 893 -898
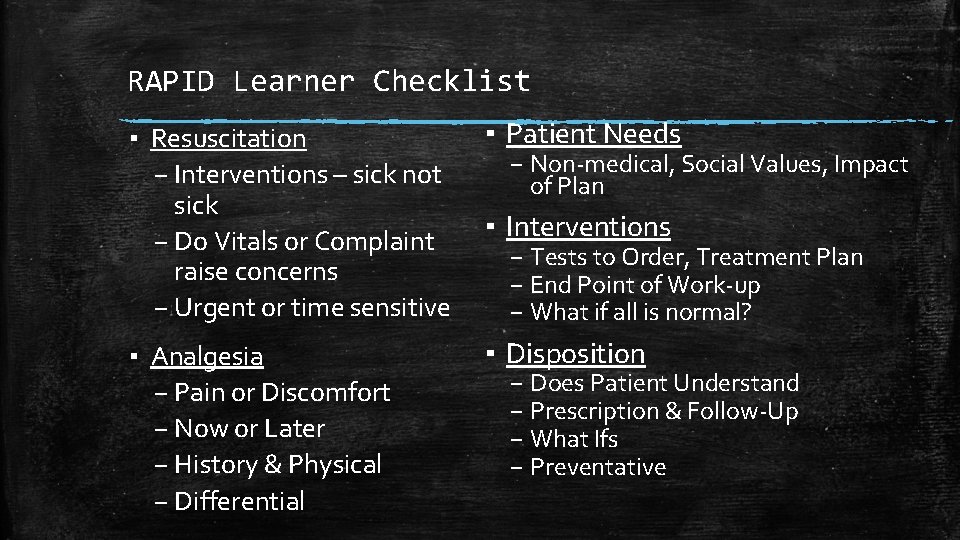
RAPID Learner Checklist ▪ Resuscitation – Interventions – sick not sick – Do Vitals or Complaint raise concerns – Urgent or time sensitive ▪ Patient Needs ▪ Analgesia – Pain or Discomfort – Now or Later – History & Physical – Differential ▪ Disposition – Non-medical, Social Values, Impact of Plan ▪ Interventions – Tests to Order, Treatment Plan – End Point of Work-up – What if all is normal? – Does Patient Understand – Prescription & Follow-Up – What Ifs – Preventative
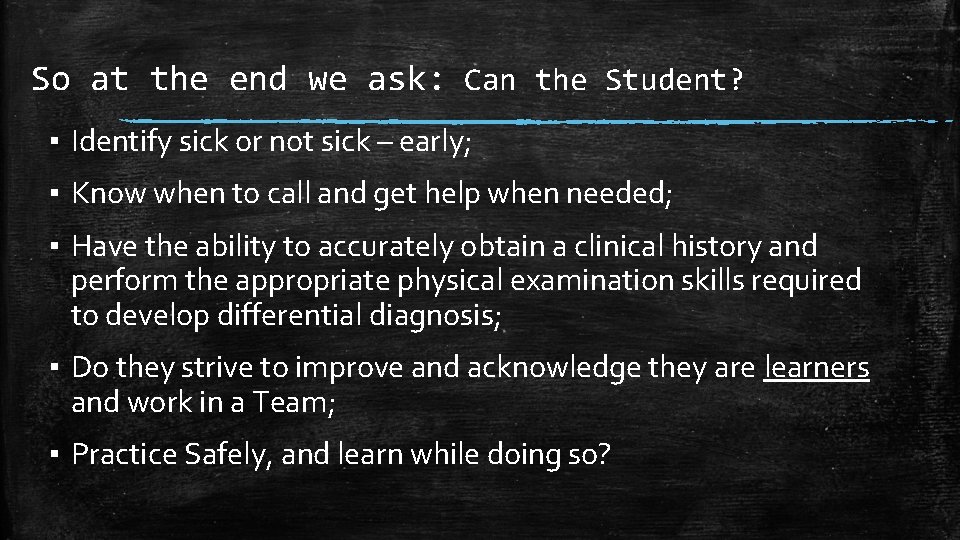
So at the end we ask: Can the Student? ▪ Identify sick or not sick – early; ▪ Know when to call and get help when needed; ▪ Have the ability to accurately obtain a clinical history and perform the appropriate physical examination skills required to develop differential diagnosis; ▪ Do they strive to improve and acknowledge they are learners and work in a Team; ▪ Practice Safely, and learn while doing so?
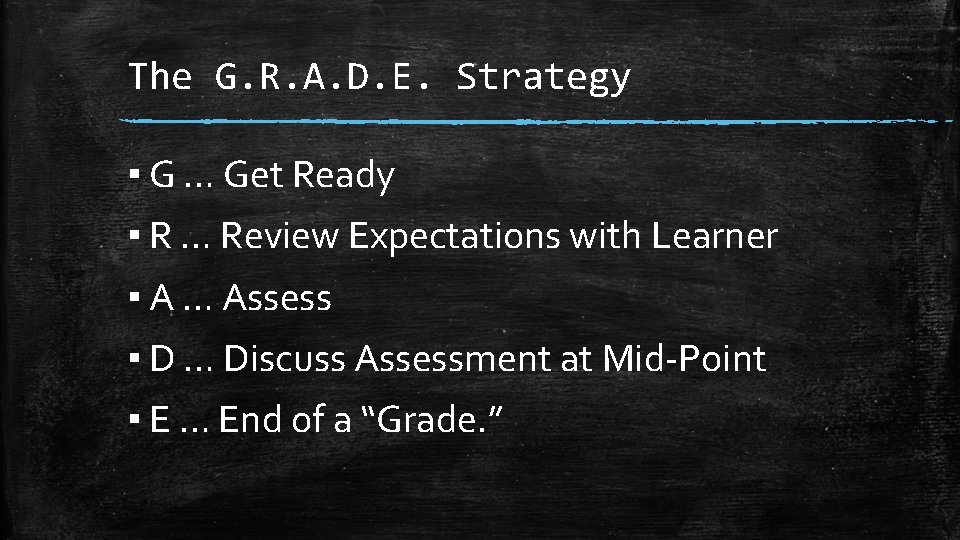
The G. R. A. D. E. Strategy ▪ G … Get Ready ▪ R … Review Expectations with Learner ▪ A … Assess ▪ D … Discuss Assessment at Mid-Point ▪ E … End of a “Grade. ”
It goes without saying that no man can teach successfully who is not at the same time a student. Thank you for participating in the education of a future professional. We encourage contacting the Programs’ Clinical Coordinators with questions and feedback on the curriculum and the learners.

Standards of Professional Conduct As Medical Experts, PAs integrate all of the Can. MEDS Roles, As Communicators, PAs effectively facilitate patient-centered care and the dynamic exchanges As Collaborators, PAs work within a formalized relationship with a physician(s) and informally with members of the inter-professional healthcare team As Leaders, PAs are integral participants in health care organizations working with their supervising physician and others to contribute to sustainable practices, As Health Advocates, PAs responsibly use their expertise and influence to advance the health and well-being of individual patients, communities, and populations. As Scholars, PAs demonstrate a lifelong commitment to reflective learning, evaluating evidence and the application and translation of medical knowledge. As Professionals, PAs are committed to the health and well-being of individuals and society through ethical practice, profession-led association, and high personal standards of behavior

Thank You
- Slides: 36