Ticagrelor With Asp Irin or ALone In Hi


- Slides: 24
Ticagrelor With Asp. Irin or ALone In Hi. GHRisk Patients After Coronary In. Tervention for Acute Coronary Syndrome TWILIGHT-ACS Usman Baber, MD MS on behalf of Roxana Mehran, MD and the TWILIGHT Investigators Icahn School of Medicine at Mount Sinai, New York, NY Clinical. Trials. gov Number: NCT 02270242
Disclosures Affiliation/Financial Relationship Advisory board/personal fees Research Funding to Institution Scientific. Sessions. org Company Amgen; Astra. Zeneca; Boston Scientific Astra. Zeneca #AHA 19
Background • The prevailing construct of dual antiplatelet therapy (DAPT) as the preferred treatment for patients with acute coronary syndromes (ACS) originated from clinical trials showing that the addition of an oral P 2 Y 12 inhibitor to aspirin significantly lowers recurrent ischemic events as compared with aspirin alone. 1, 2 • The benefits, or harms, of maintaining aspirin as a long-term component of DAPT in the setting of ACS remains unknown, however, as aspirin served as a background agent in earlier studies. • Recent studies have suggested that aspirin-free strategies lower bleeding without increasing ischemic risk as compared with conventional DAPT in select patients undergoing percutaneous coronary intervention (PCI). 3, 4, 5 1 Mehta et al. , Lancet 2001; 2 Levine et al. , JACC 2016; 3 Mehran et al. , NEJM 2019; 4 Watanabe et al. , JAMA 2019; 5 Hahn et al. , JAMA 2019 Scientific. Sessions. org #AHA 19
Study Objective To examine the effect of antiplatelet monotherapy with ticagrelor alone versus ticagrelor plus aspirin among patients with non-ST elevation acute coronary syndromes (NSTE-ACS) undergoing PCI with drug eluting stents who had already completed a 3 -month course of DAPT Scientific. Sessions. org #AHA 19
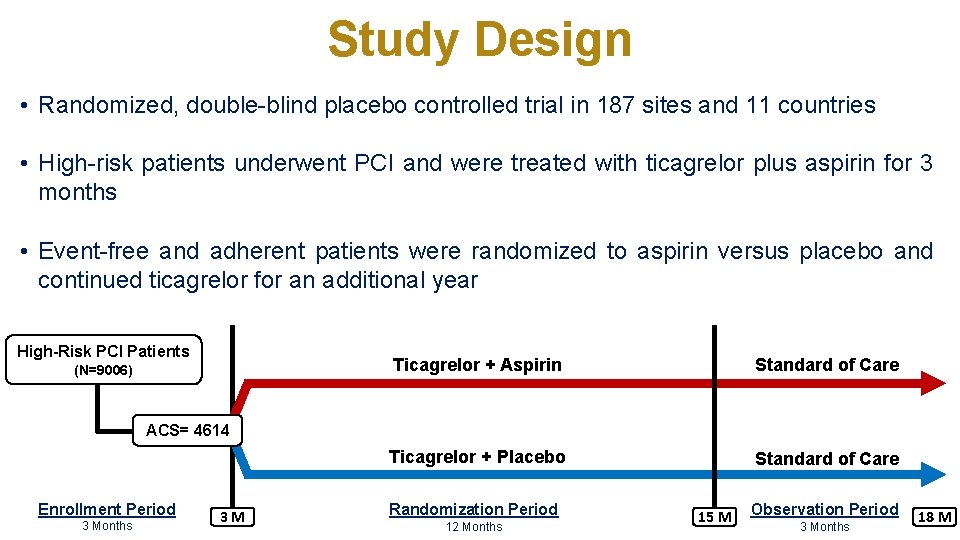
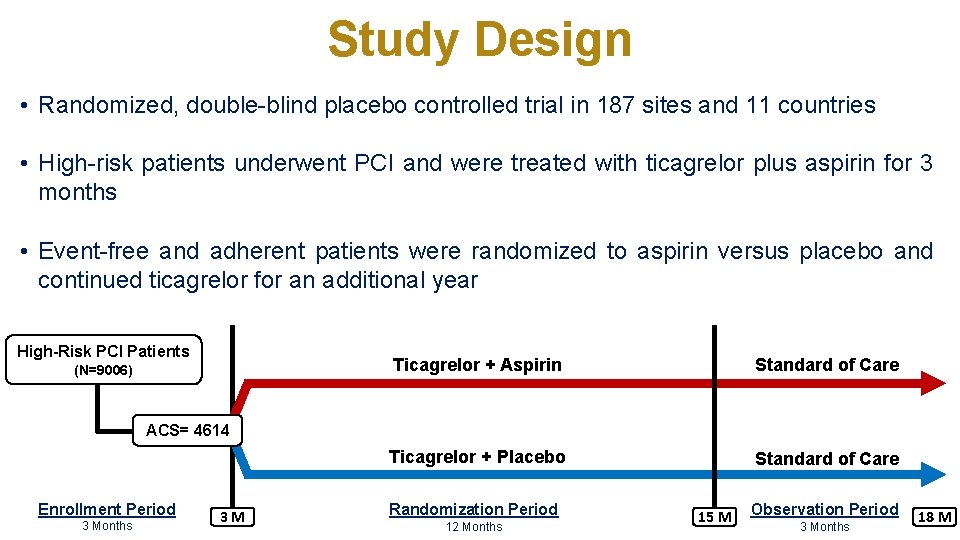
Study Design • Randomized, double-blind placebo controlled trial in 187 sites and 11 countries • High-risk patients underwent PCI and were treated with ticagrelor plus aspirin for 3 months • Event-free and adherent patients were randomized to aspirin versus placebo and continued ticagrelor for an additional year High-Risk PCI Patients (N=9006) Ticagrelor + Aspirin Standard of Care Ticagrelor + Placebo Standard of Care ACS= 4614 Enrollment Period 3 Months 3 M Randomization Period 12 Months 15 M Observation Period 3 Months 18 M
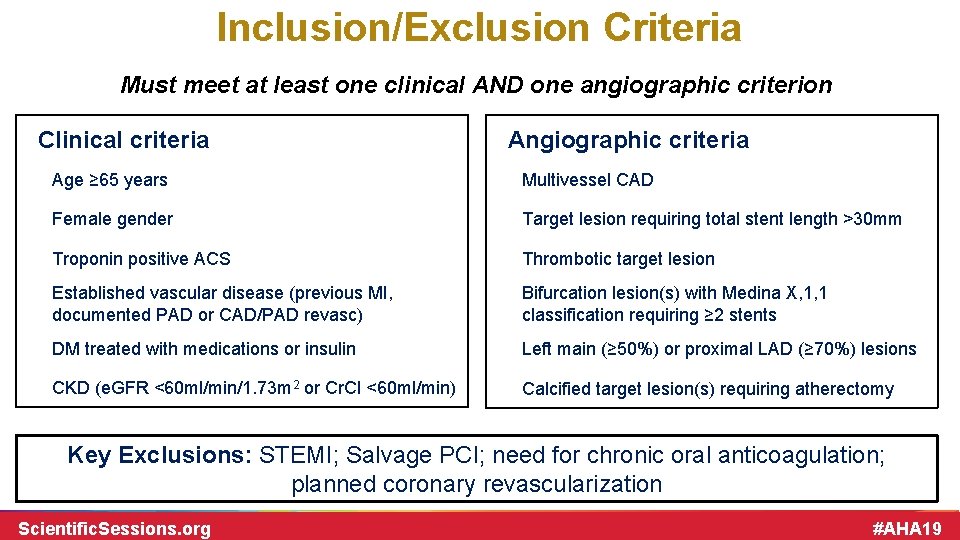
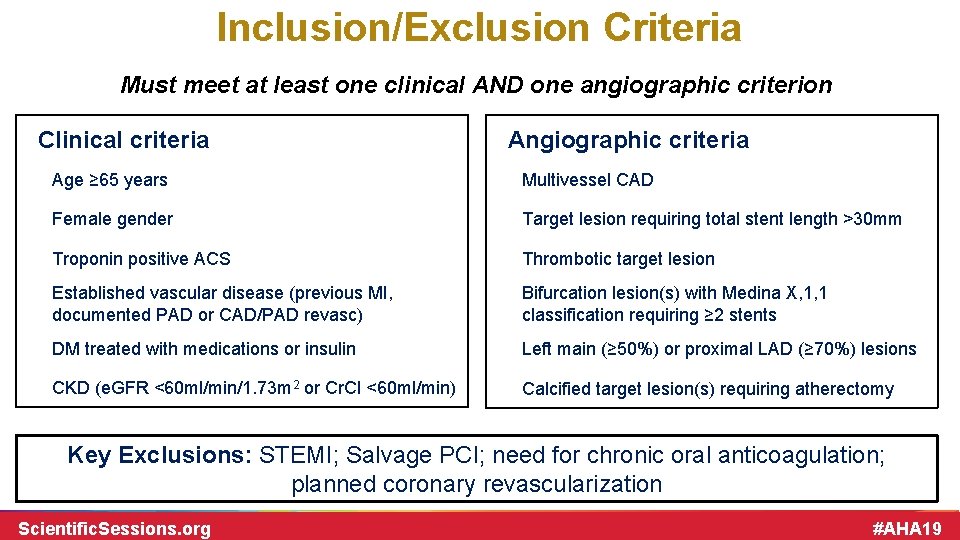
Inclusion/Exclusion Criteria Must meet at least one clinical AND one angiographic criterion Clinical criteria Angiographic criteria Age ≥ 65 years Multivessel CAD Female gender Target lesion requiring total stent length >30 mm Troponin positive ACS Thrombotic target lesion Established vascular disease (previous MI, documented PAD or CAD/PAD revasc) Bifurcation lesion(s) with Medina X, 1, 1 classification requiring ≥ 2 stents DM treated with medications or insulin Left main (≥ 50%) or proximal LAD (≥ 70%) lesions CKD (e. GFR <60 ml/min/1. 73 m 2 or Cr. Cl <60 ml/min) Calcified target lesion(s) requiring atherectomy Key Exclusions: STEMI; Salvage PCI; need for chronic oral anticoagulation; planned coronary revascularization Scientific. Sessions. org #AHA 19
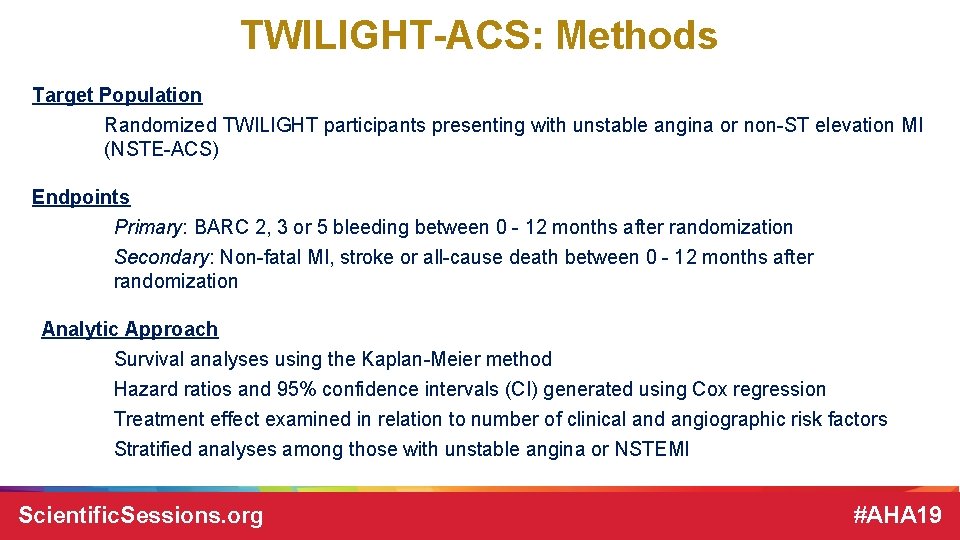
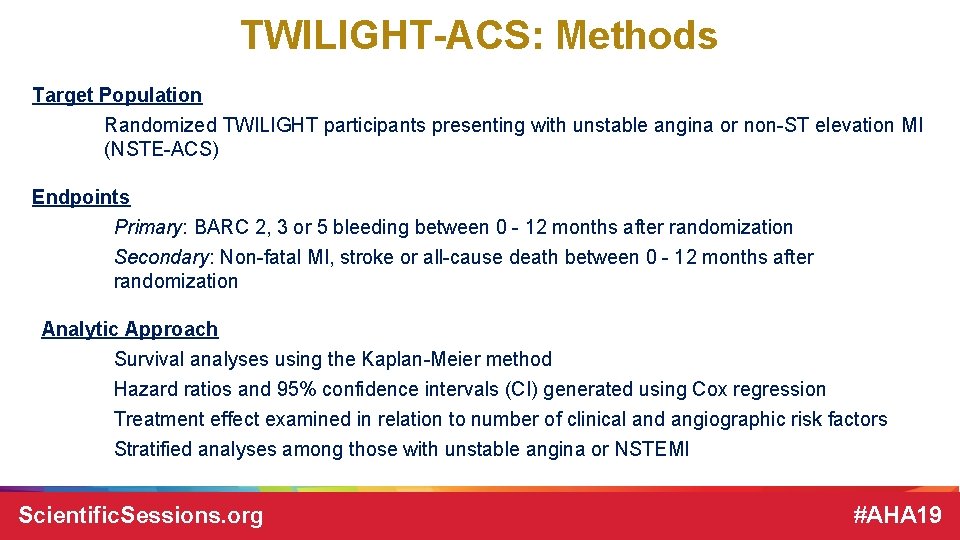
TWILIGHT-ACS: Methods Target Population Randomized TWILIGHT participants presenting with unstable angina or non-ST elevation MI (NSTE-ACS) Endpoints Primary: BARC 2, 3 or 5 bleeding between 0 - 12 months after randomization Secondary: Non-fatal MI, stroke or all-cause death between 0 - 12 months after randomization Analytic Approach Survival analyses using the Kaplan-Meier method Hazard ratios and 95% confidence intervals (CI) generated using Cox regression Treatment effect examined in relation to number of clinical and angiographic risk factors Stratified analyses among those with unstable angina or NSTEMI Scientific. Sessions. org #AHA 19
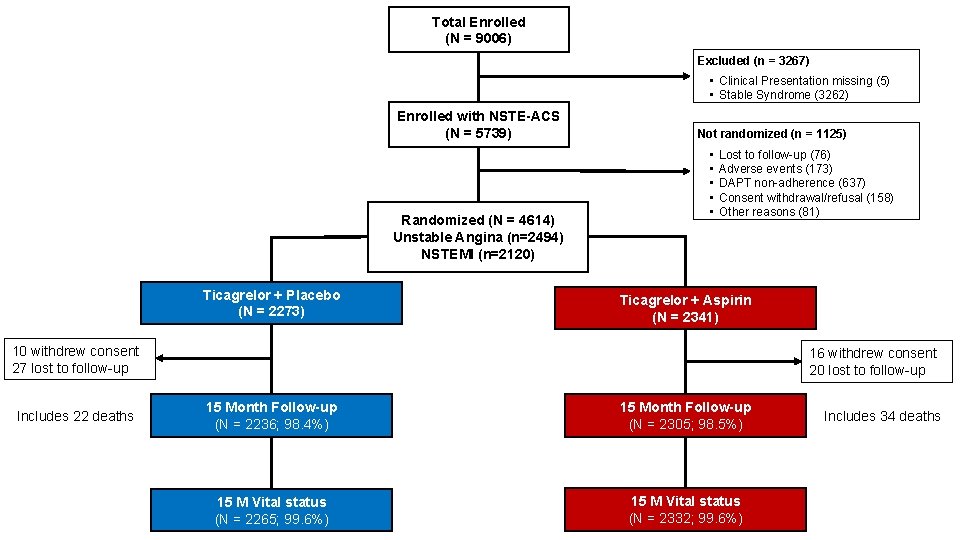
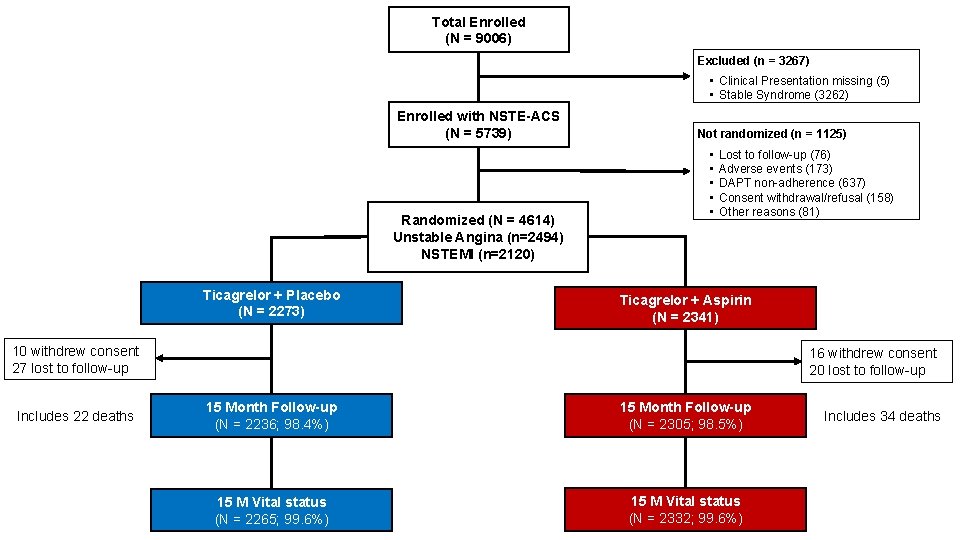
Total Enrolled (N = 9006) Excluded (n = 3267) • Clinical Presentation missing (5) • Stable Syndrome (3262) Enrolled with NSTE-ACS (N = 5739) Randomized (N = 4614) Unstable Angina (n=2494) NSTEMI (n=2120) Ticagrelor + Placebo (N = 2273) Not randomized (n = 1125) • • • Lost to follow-up (76) Adverse events (173) DAPT non-adherence (637) Consent withdrawal/refusal (158) Other reasons (81) Ticagrelor + Aspirin (N = 2341) 10 withdrew consent 27 lost to follow-up Includes 22 deaths 16 withdrew consent 20 lost to follow-up 15 Month Follow-up (N = 2236; 98. 4%) 15 Month Follow-up (N = 2305; 98. 5%) 15 M Vital status (N = 2265; 99. 6%) 15 M Vital status (N = 2332; 99. 6%) Includes 34 deaths
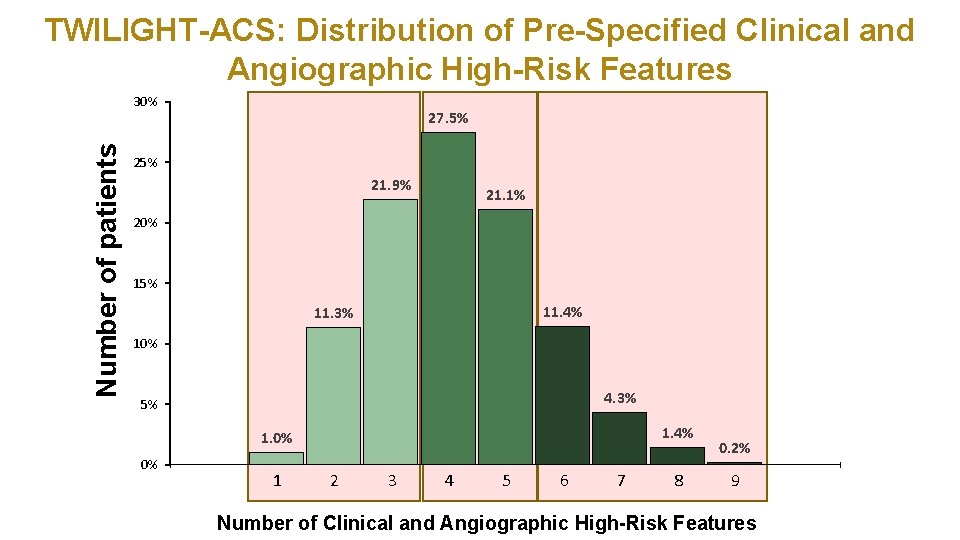
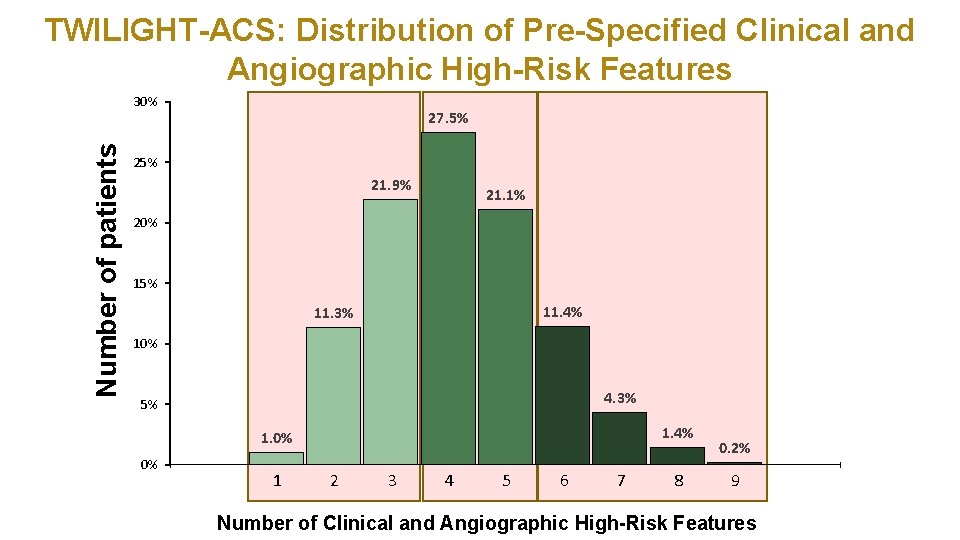
TWILIGHT-ACS: Distribution of Pre-Specified Clinical and Angiographic High-Risk Features Number of patients 30% 27. 5% 21. 9% 21. 1% 20% 15% 11. 4% 11. 3% 10% 4. 3% 5% 1. 4% 1. 0% 0% 1 2 3 4 5 6 7 8 0. 2% 9 Number of Clinical and Angiographic High-Risk Features
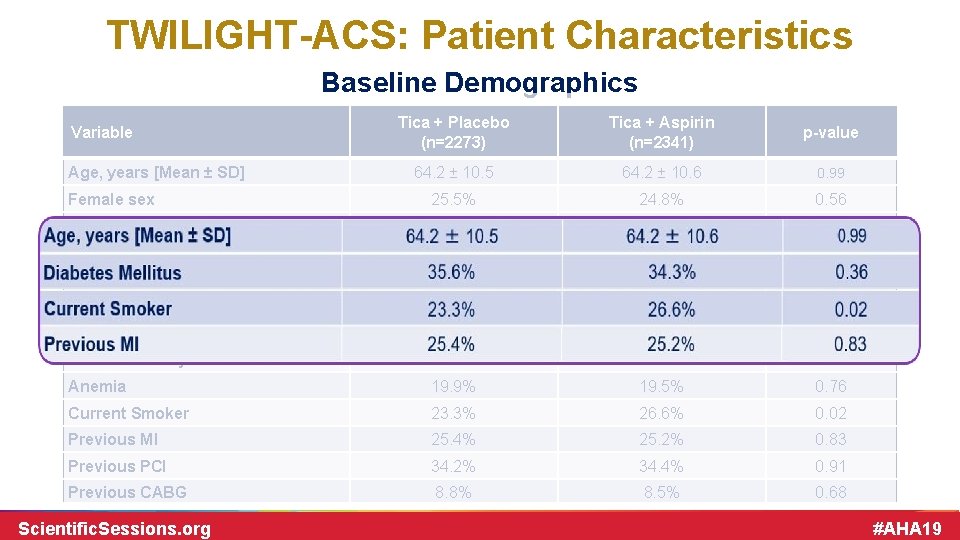
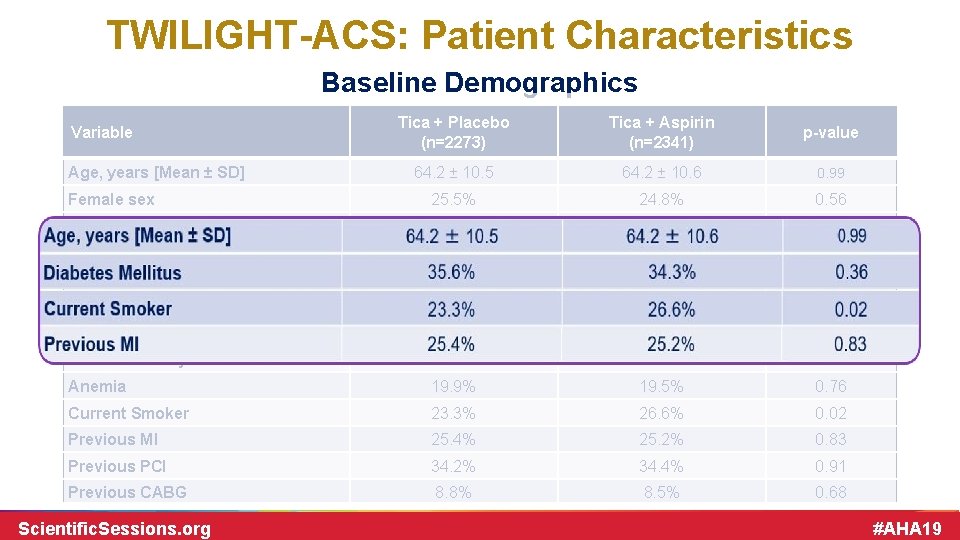
TWILIGHT-ACS: Patient Characteristics Baseline Demographics Tica + Placebo (n=2273) Tica + Aspirin (n=2341) p-value 64. 2 ± 10. 5 64. 2 ± 10. 6 0. 99 Female sex 25. 5% 24. 8% 0. 56 Nonwhite race 38. 4% 36. 5% 0. 62 28. 4 ± 5. 5 28. 4 ± 5. 7 0. 85 35. 6% 34. 3% 0. 36 Insulin requiring 9. 7% 10. 1% 0. 47 NSTEMI 45. 1% 46. 8% 0. 23 Chronic Kidney Disease 14. 6% 15. 1% 0. 68 Anemia 19. 9% 19. 5% 0. 76 Current Smoker 23. 3% 26. 6% 0. 02 Previous MI 25. 4% 25. 2% 0. 83 Previous PCI 34. 2% 34. 4% 0. 91 Previous CABG 8. 8% 8. 5% 0. 68 Variable Age, years [Mean ± SD] BMI, kg/m 2 Diabetes Mellitus Scientific. Sessions. org #AHA 19
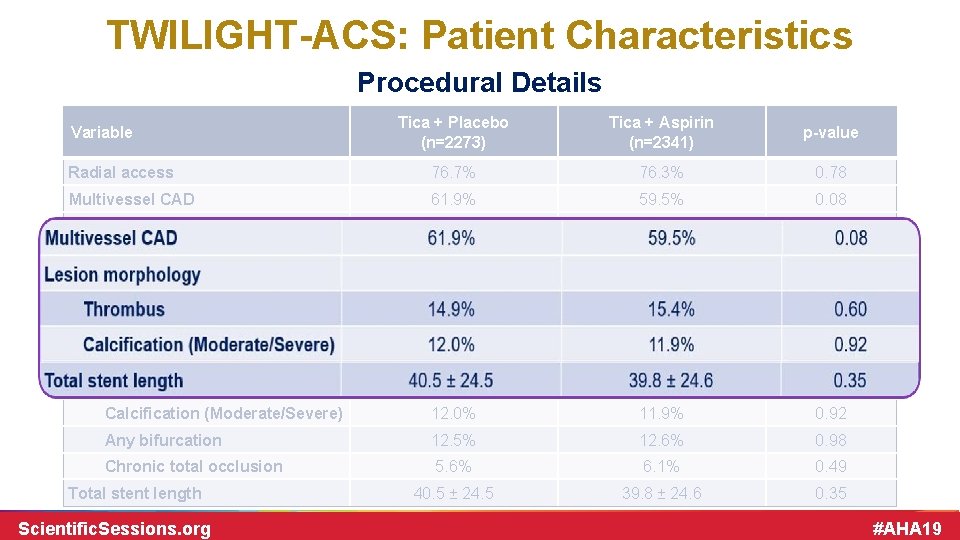
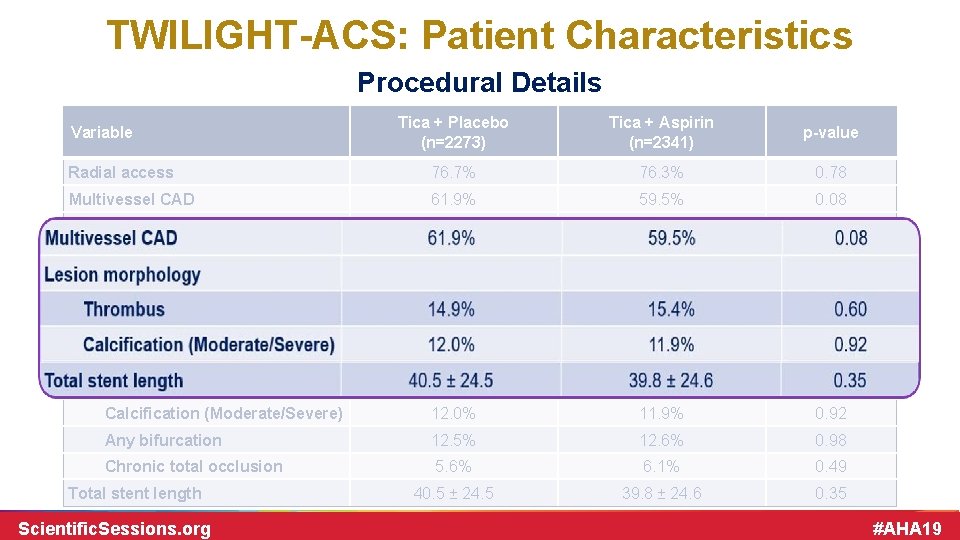
TWILIGHT-ACS: Patient Characteristics Procedural Details Tica + Placebo (n=2273) Tica + Aspirin (n=2341) p-value Radial access 76. 7% 76. 3% 0. 78 Multivessel CAD 61. 9% 59. 5% 0. 08 LAD 57. 7% 58. 4% 0. 6 RCA 34. 9% 33. 9% 0. 47 LCX 32. 6% 32. 9% 0. 83 1. 5 ± 0. 7 0. 52 Thrombus 14. 9% 15. 4% 0. 60 Calcification (Moderate/Severe) 12. 0% 11. 9% 0. 92 Any bifurcation 12. 5% 12. 6% 0. 98 Chronic total occlusion 5. 6% 6. 1% 0. 49 40. 5 ± 24. 5 39. 8 ± 24. 6 0. 35 Variable Target vessel Number of lesions treated Lesion morphology Total stent length Scientific. Sessions. org #AHA 19
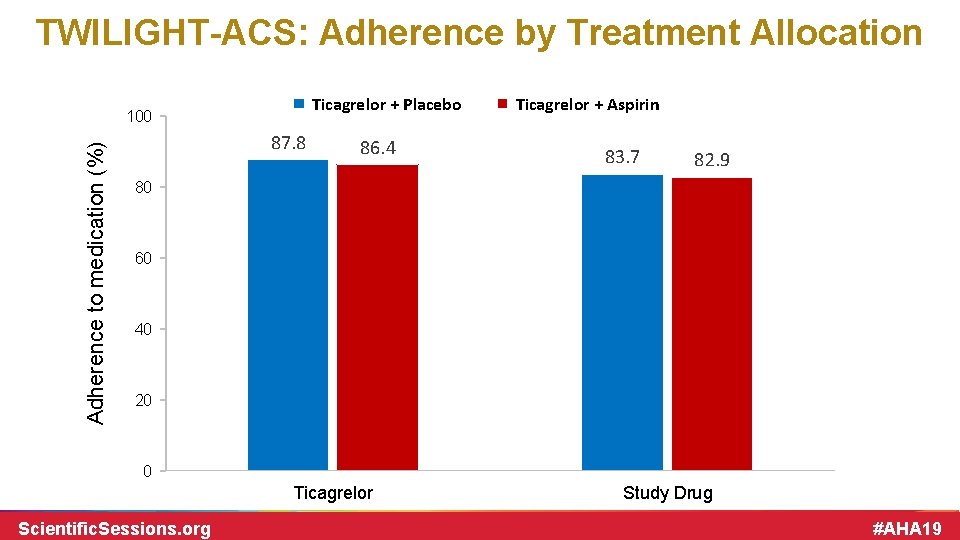
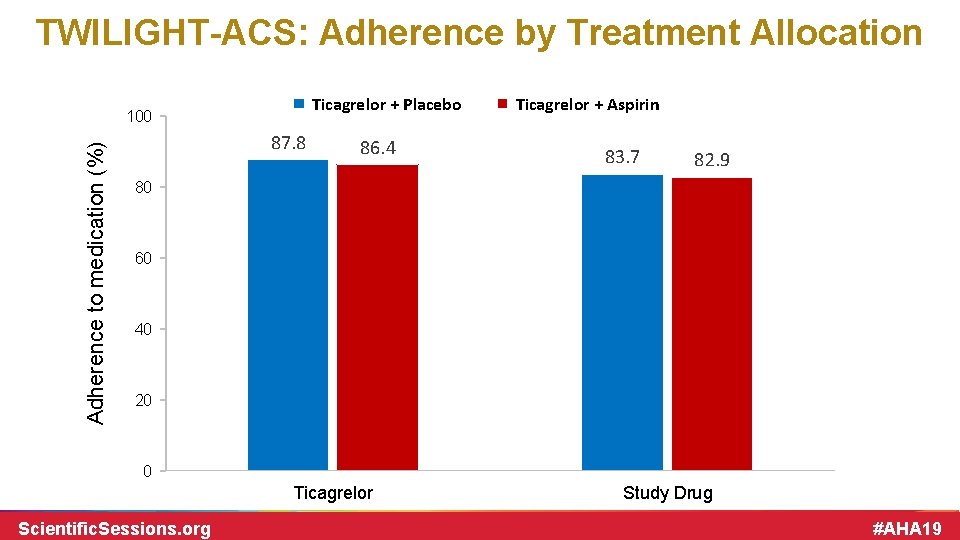
TWILIGHT-ACS: Adherence by Treatment Allocation Ticagrelor + Placebo Adherence to medication (%) 100 87. 8 86. 4 Ticagrelor + Aspirin 83. 7 82. 9 80 60 40 20 0 Ticagrelor Scientific. Sessions. org Study Drug #AHA 19
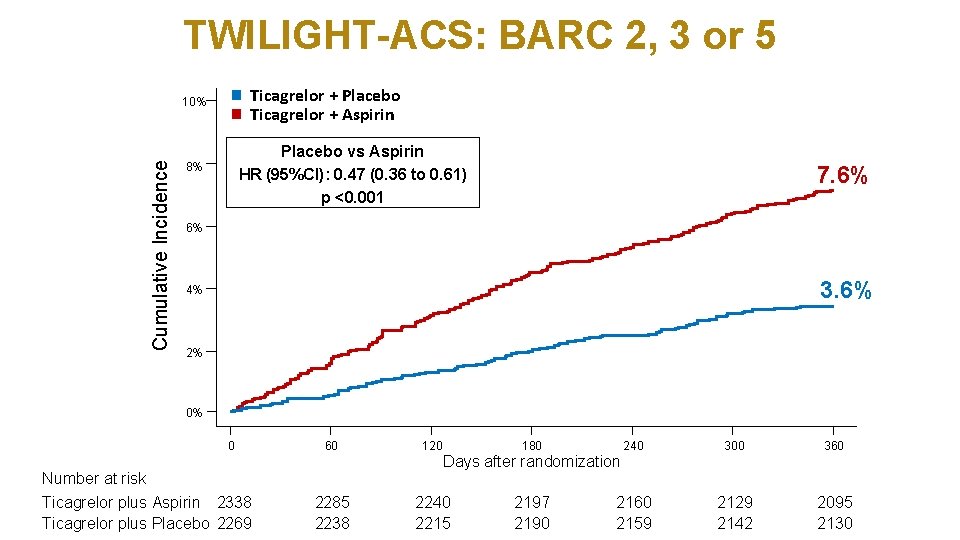
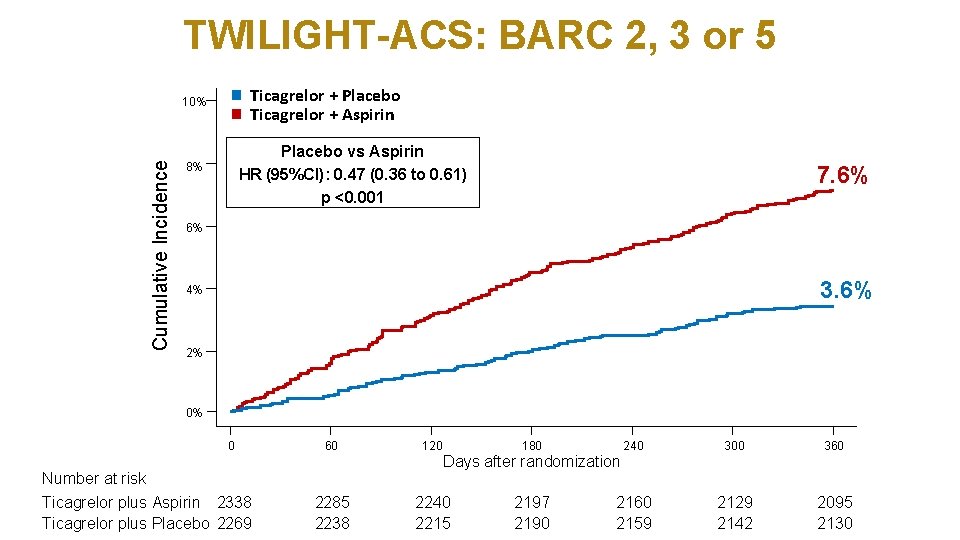
TWILIGHT-ACS: BARC 2, 3 or 5 Ticagrelor + Placebo Ticagrelor + Aspirin Cumulative Incidence 10% Placebo vs Aspirin HR (95%CI): 0. 47 (0. 36 to 0. 61) p <0. 001 8% 7. 6% 6% 3. 6% 4% 2% 0% 0 60 120 2285 2238 2240 2215 Number at risk Ticagrelor plus Aspirin 2338 Ticagrelor plus Placebo 2269 180 240 300 360 2197 2190 2160 2159 2129 2142 2095 2130 Days after randomization
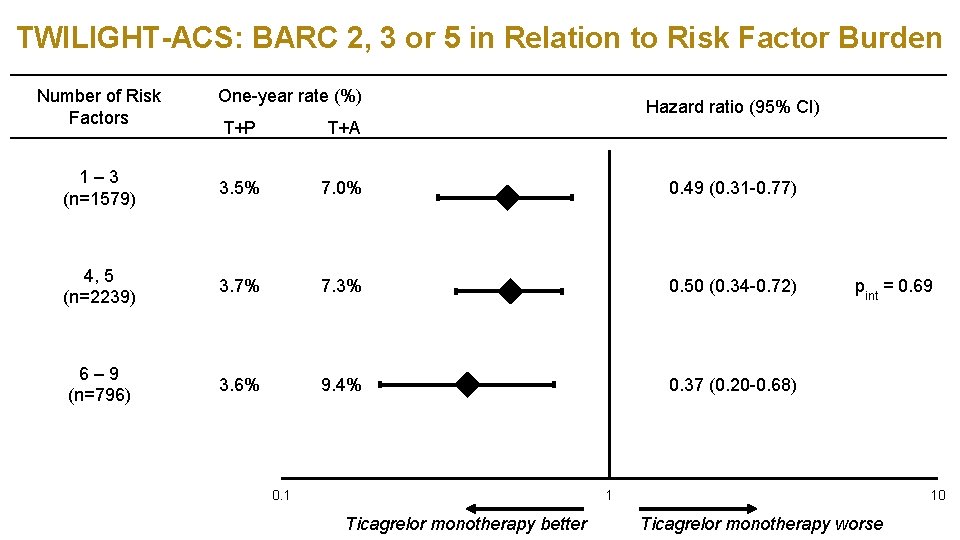
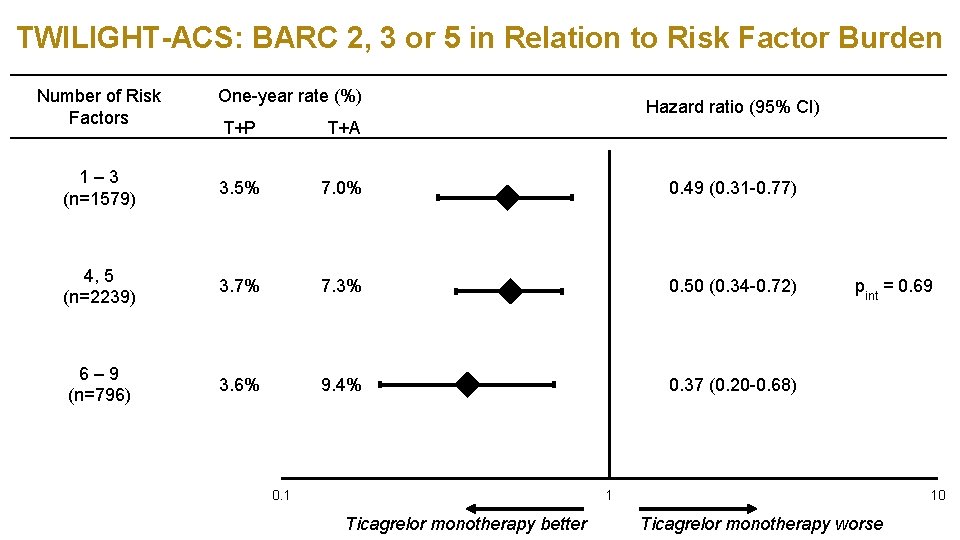
TWILIGHT-ACS: BARC 2, 3 or 5 in Relation to Risk Factor Burden Number of Risk Factors One-year rate (%) Hazard ratio (95% CI) T+P T+A 1– 3 (n=1579) 3. 5% 7. 0% 0. 49 (0. 31 -0. 77) 4, 5 (n=2239) 3. 7% 7. 3% 0. 50 (0. 34 -0. 72) 6– 9 (n=796) 3. 6% 9. 4% 0. 37 (0. 20 -0. 68) pint = 0. 69
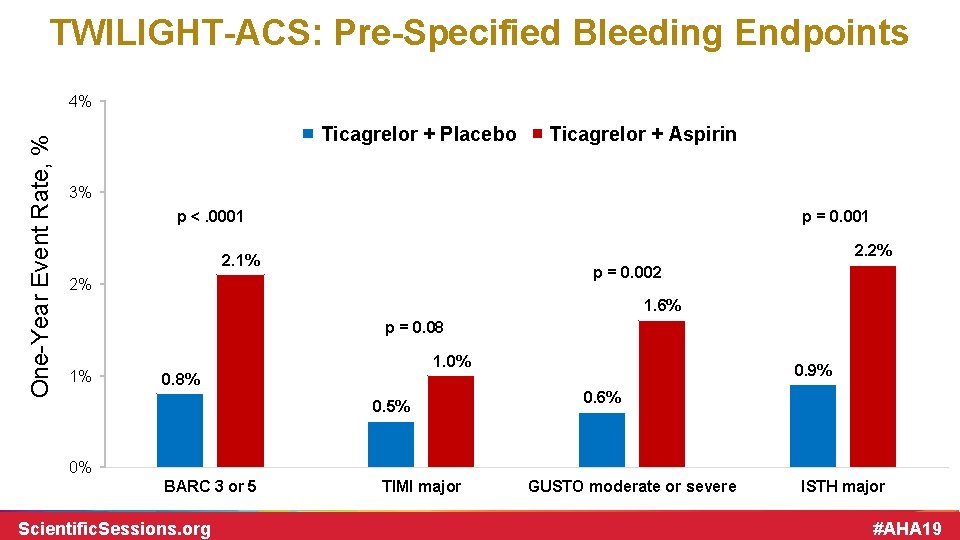
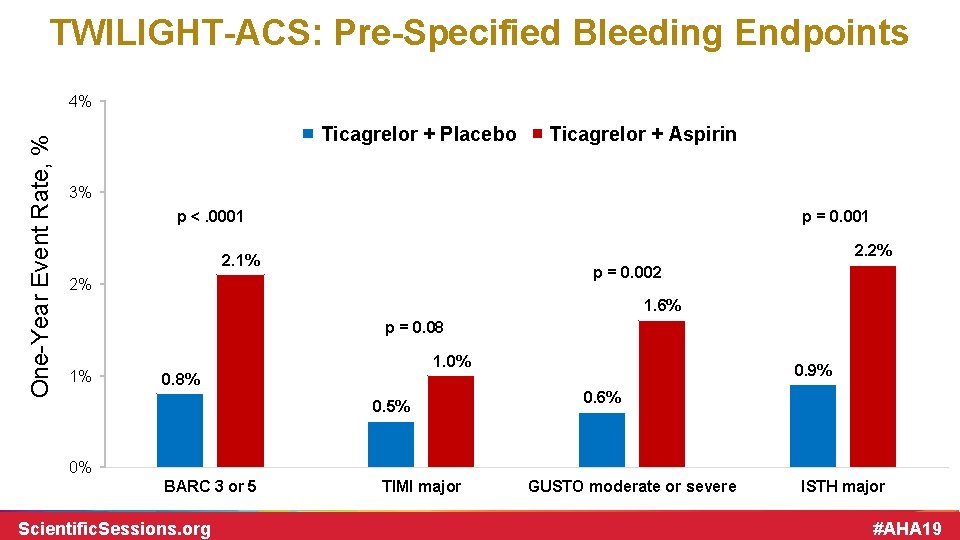
TWILIGHT-ACS: Pre-Specified Bleeding Endpoints One-Year Event Rate, % 4% Ticagrelor + Placebo Ticagrelor + Aspirin 3% p <. 0001 p = 0. 001 2. 2% 2. 1% p = 0. 002 2% 1. 6% p = 0. 08 1% 1. 0% 0. 9% 0. 8% 0. 5% 0. 6% 0% BARC 3 or 5 Scientific. Sessions. org TIMI major GUSTO moderate or severe ISTH major #AHA 19
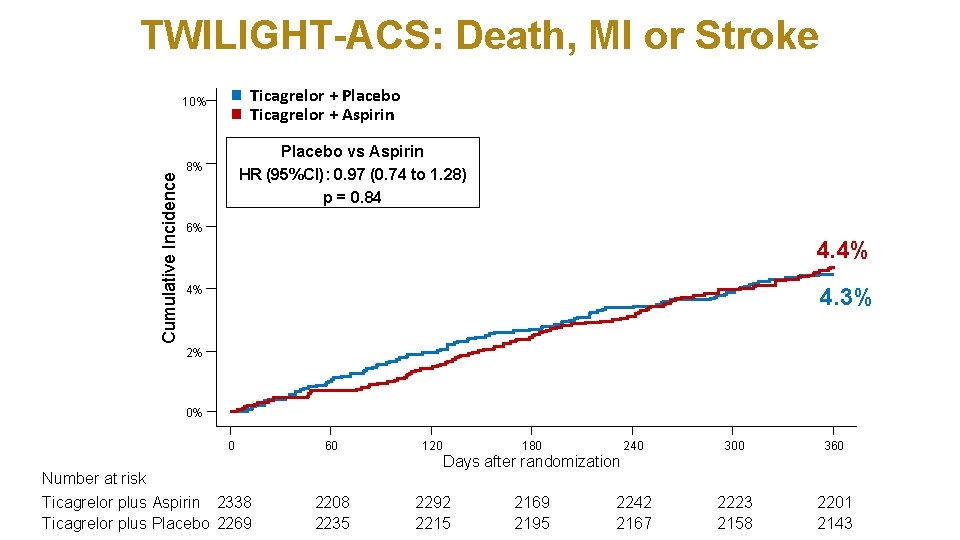
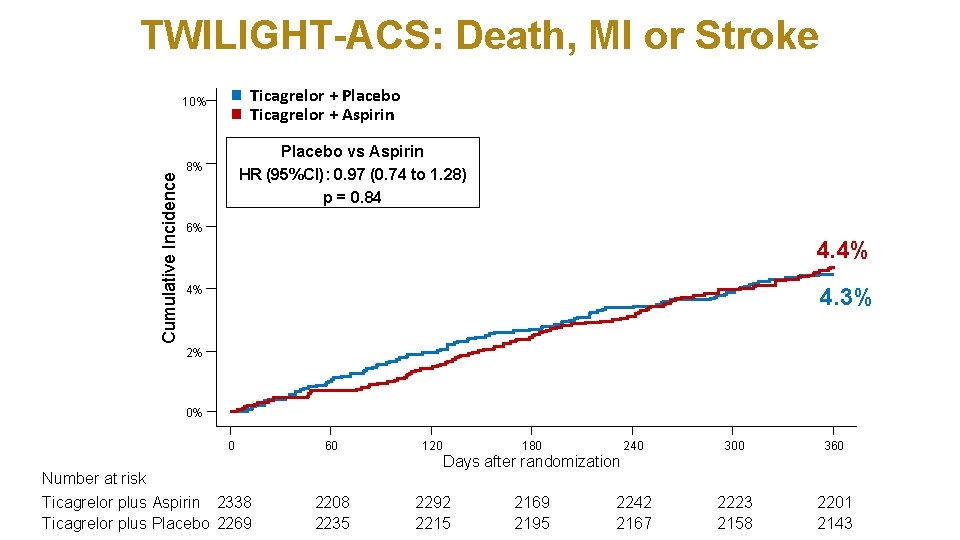
TWILIGHT-ACS: Death, MI or Stroke Ticagrelor + Placebo Ticagrelor + Aspirin Cumulative Incidence 10% Placebo vs Aspirin HR (95%CI): 0. 97 (0. 74 to 1. 28) p = 0. 84 8% 6% 4. 4% 4. 3% 4% 2% 0% 0 60 120 2208 2235 2292 2215 Number at risk Ticagrelor plus Aspirin 2338 Ticagrelor plus Placebo 2269 180 240 300 360 2169 2195 2242 2167 2223 2158 2201 2143 Days after randomization
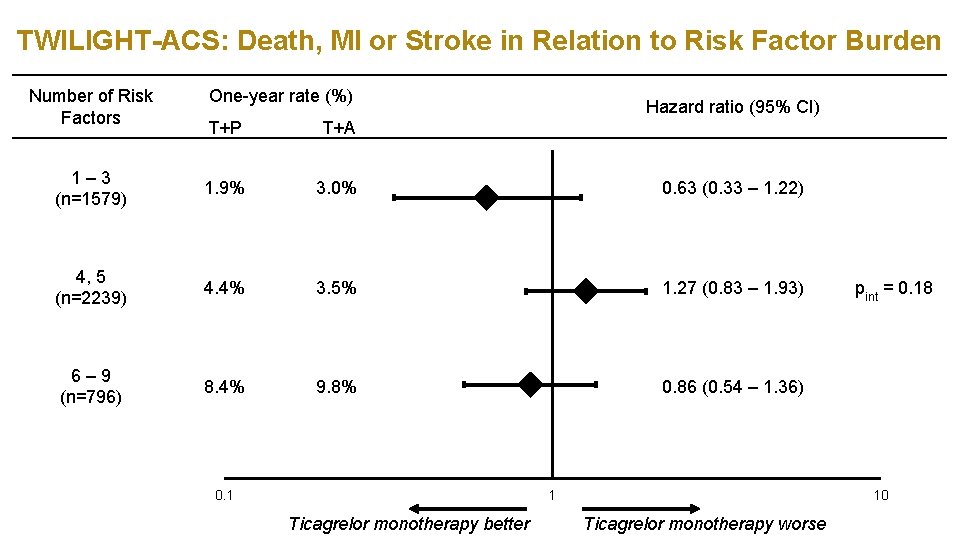
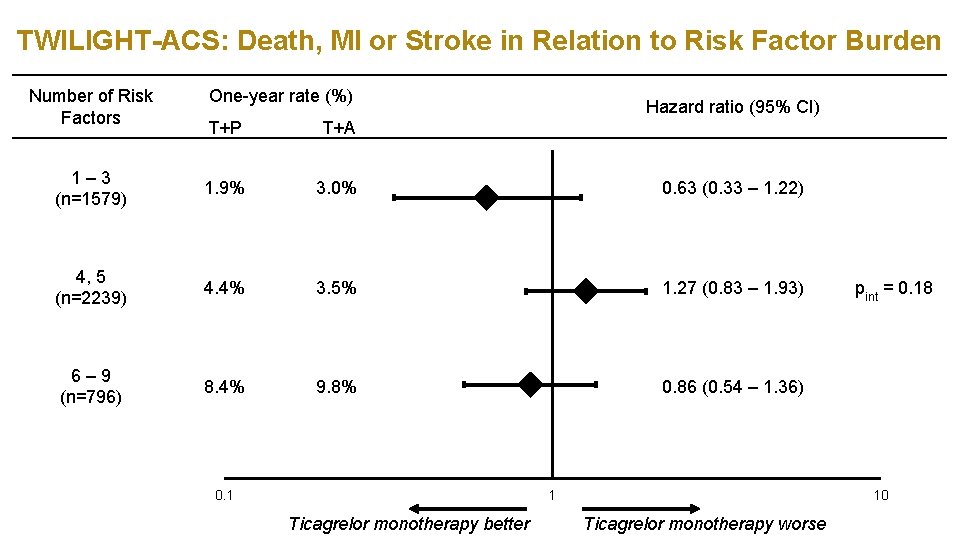
TWILIGHT-ACS: Death, MI or Stroke in Relation to Risk Factor Burden Number of Risk Factors One-year rate (%) Hazard ratio (95% CI) T+P T+A 1– 3 (n=1579) 1. 9% 3. 0% 0. 63 (0. 33 – 1. 22) 4, 5 (n=2239) 4. 4% 3. 5% 1. 27 (0. 83 – 1. 93) 6– 9 (n=796) 8. 4% 9. 8% 0. 86 (0. 54 – 1. 36) 0. 1 1 Ticagrelor monotherapy better pint = 0. 18 10 Ticagrelor monotherapy worse
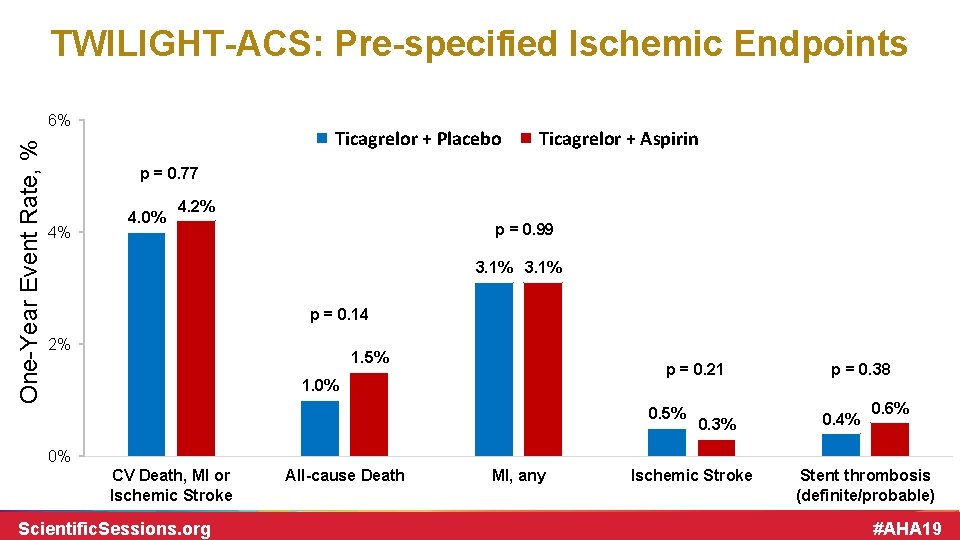
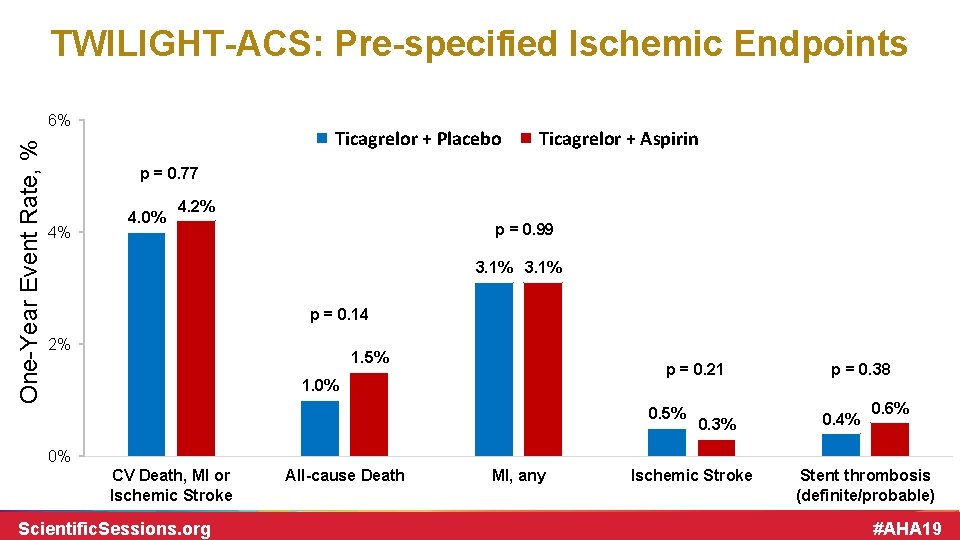
TWILIGHT-ACS: Pre-specified Ischemic Endpoints One-Year Event Rate, % 6% Ticagrelor + Placebo Ticagrelor + Aspirin p = 0. 77 4% 4. 0% 4. 2% p = 0. 99 3. 1% p = 0. 14 2% 1. 5% p = 0. 21 1. 0% 0. 5% 0. 3% p = 0. 38 0. 4% 0. 6% 0% CV Death, MI or Ischemic Stroke Scientific. Sessions. org All-cause Death MI, any Ischemic Stroke Stent thrombosis (definite/probable) #AHA 19
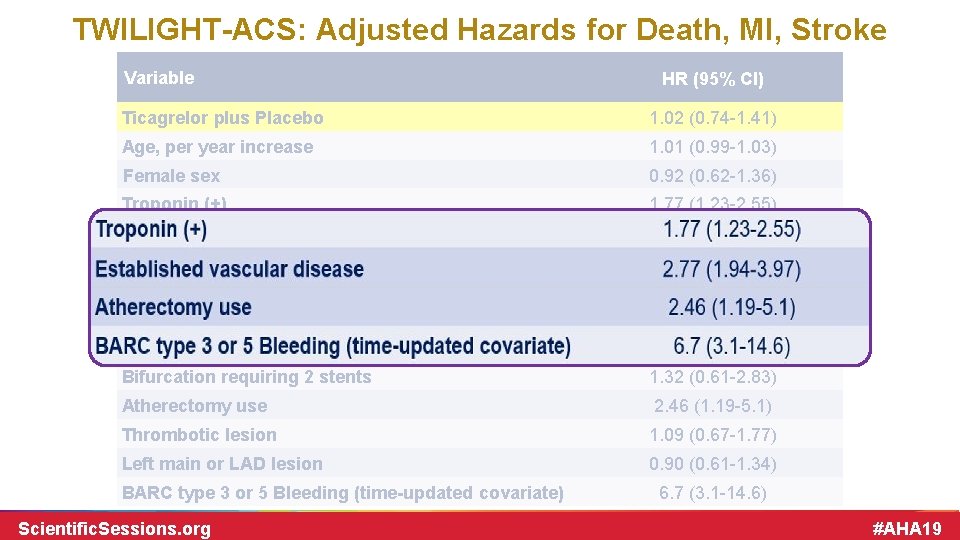
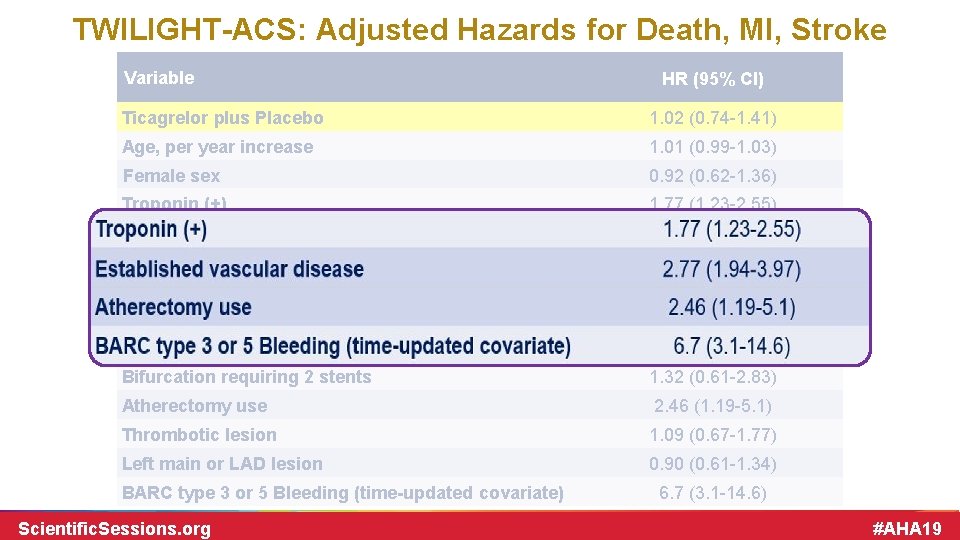
TWILIGHT-ACS: Adjusted Hazards for Death, MI, Stroke Variable HR (95% CI) Ticagrelor plus Placebo 1. 02 (0. 74 -1. 41) Age, per year increase 1. 01 (0. 99 -1. 03) Female sex 0. 92 (0. 62 -1. 36) Troponin (+) 1. 77 (1. 23 -2. 55) Established vascular disease 2. 77 (1. 94 -3. 97) Diabetes Mellitus 1. 38 (0. 99 -1. 93) Chronic Kidney Disease 1. 35 (0. 88 -2. 06) Multivessel CAD 1. 25 (0. 86 -1. 82) Lesion requiring stent length > 30 mm 1. 30 (0. 94 -1. 81) Bifurcation requiring 2 stents 1. 32 (0. 61 -2. 83) Atherectomy use 2. 46 (1. 19 -5. 1) Thrombotic lesion 1. 09 (0. 67 -1. 77) Left main or LAD lesion 0. 90 (0. 61 -1. 34) BARC type 3 or 5 Bleeding (time-updated covariate) Scientific. Sessions. org 6. 7 (3. 1 -14. 6) #AHA 19
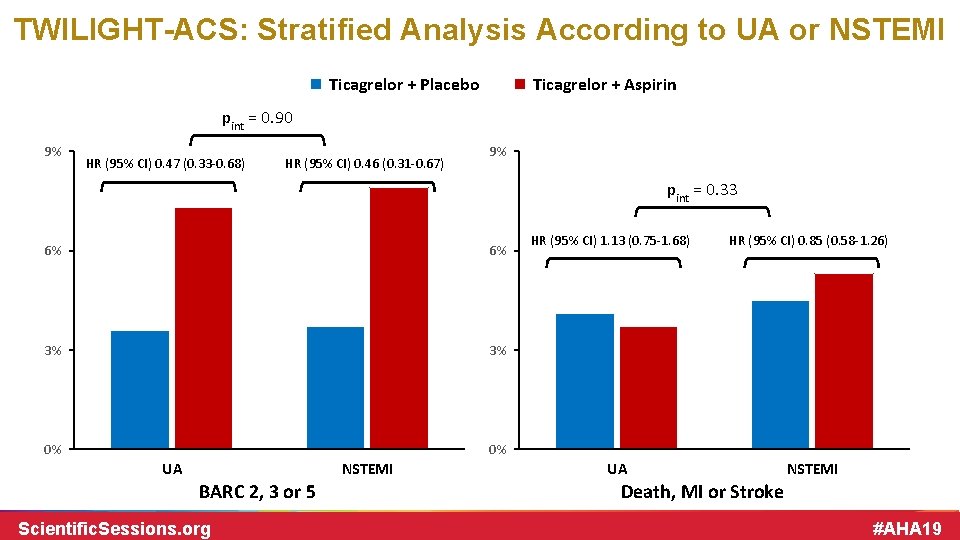
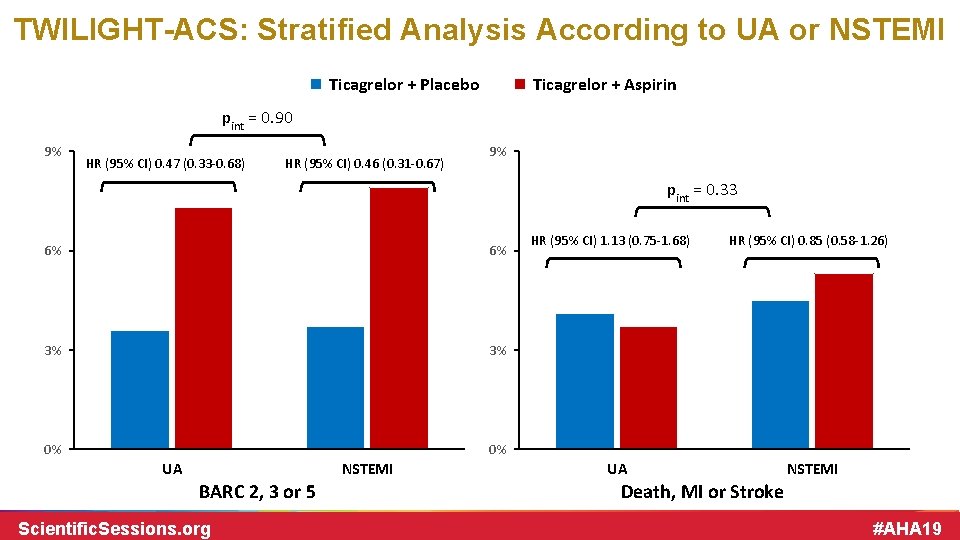
TWILIGHT-ACS: Stratified Analysis According to UA or NSTEMI Ticagrelor + Placebo Ticagrelor + Aspirin pint = 0. 90 9% HR (95% CI) 0. 47 (0. 33 -0. 68) HR (95% CI) 0. 46 (0. 31 -0. 67) 9% pint = 0. 33 6% 6% 3% 3% 0% 0% UA NSTEMI BARC 2, 3 or 5 Scientific. Sessions. org HR (95% CI) 1. 13 (0. 75 -1. 68) HR (95% CI) 0. 85 (0. 58 -1. 26) UA NSTEMI Death, MI or Stroke #AHA 19
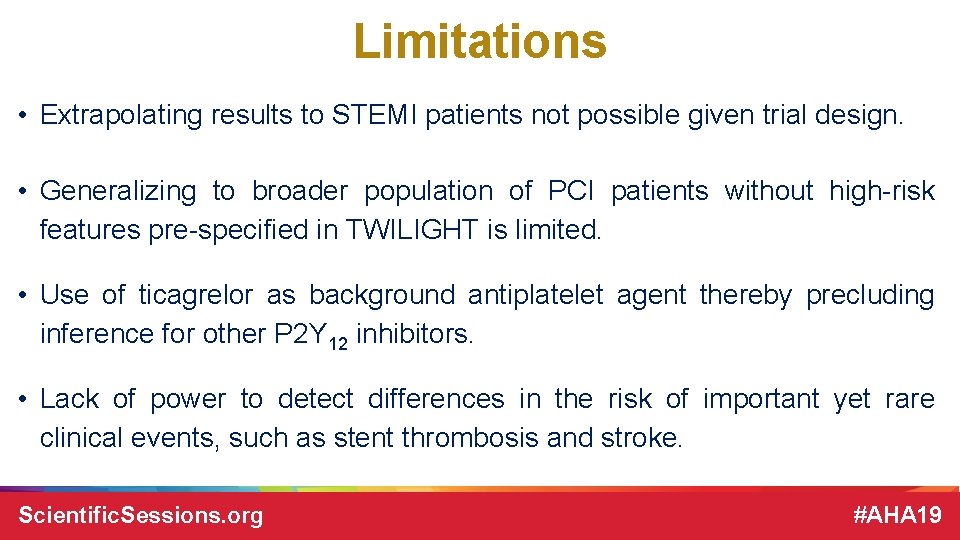
Limitations • Extrapolating results to STEMI patients not possible given trial design. • Generalizing to broader population of PCI patients without high-risk features pre-specified in TWILIGHT is limited. • Use of ticagrelor as background antiplatelet agent thereby precluding inference for other P 2 Y 12 inhibitors. • Lack of power to detect differences in the risk of important yet rare clinical events, such as stent thrombosis and stroke. Scientific. Sessions. org #AHA 19
Conclusions • Among patients with NSTE-ACS undergoing PCI with DES and who have completed a 3 -month course of DAPT with ticagrelor plus aspirin, continued treatment with ticagrelor alone significantly lowers clinically relevant and major bleeding without increasing risk for ischemic events over one year. • The effect of ticagrelor monotherapy with respect to bleeding and ischemic events is uniform across different levels of risk. • Results are unchanged for patients presenting with UA or NSTEMI. • Overall findings are concordant with the results of the primary trial. Scientific. Sessions. org #AHA 19

Acknowledgement We thank all country leaders, investigators, coordinators and study participants who made TWILIGHT possible! Scientific. Sessions. org #AHA 19

Thank you! Scientific. Sessions. org #AHA 19