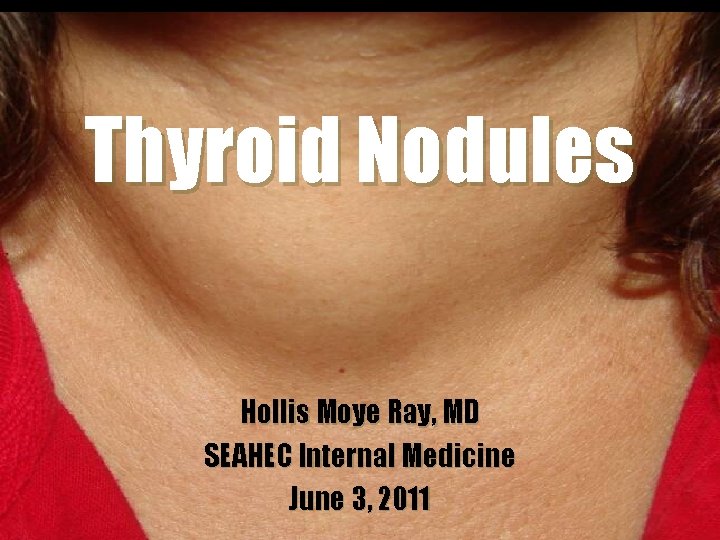
Thyroid Nodules Hollis Moye Ray MD SEAHEC Internal
- Slides: 19
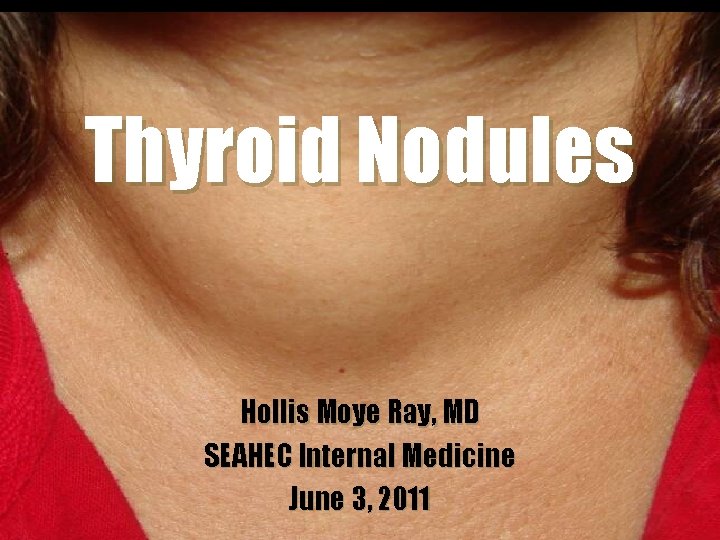
Thyroid Nodules Hollis Moye Ray, MD SEAHEC Internal Medicine June 3, 2011
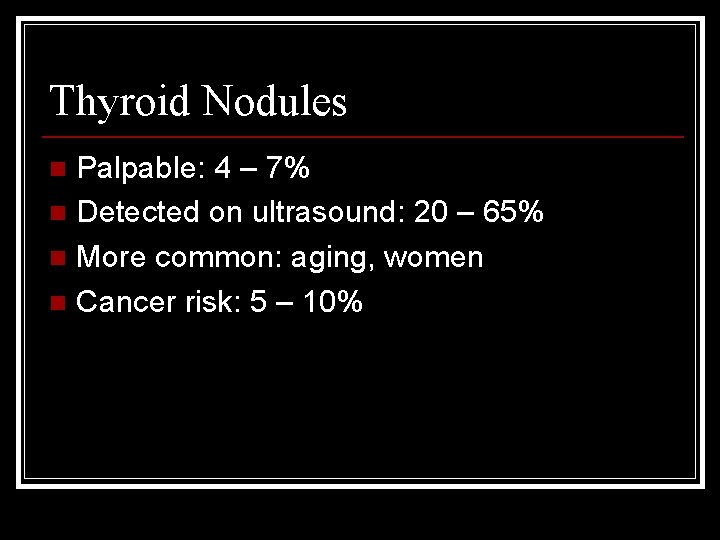
Thyroid Nodules Palpable: 4 – 7% n Detected on ultrasound: 20 – 65% n More common: aging, women n Cancer risk: 5 – 10% n
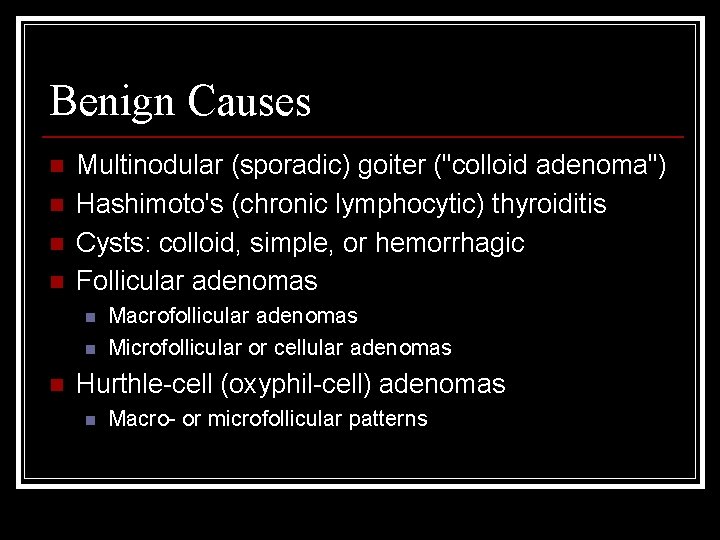
Benign Causes n n Multinodular (sporadic) goiter ("colloid adenoma") Hashimoto's (chronic lymphocytic) thyroiditis Cysts: colloid, simple, or hemorrhagic Follicular adenomas n n n Macrofollicular adenomas Microfollicular or cellular adenomas Hurthle-cell (oxyphil-cell) adenomas n Macro- or microfollicular patterns
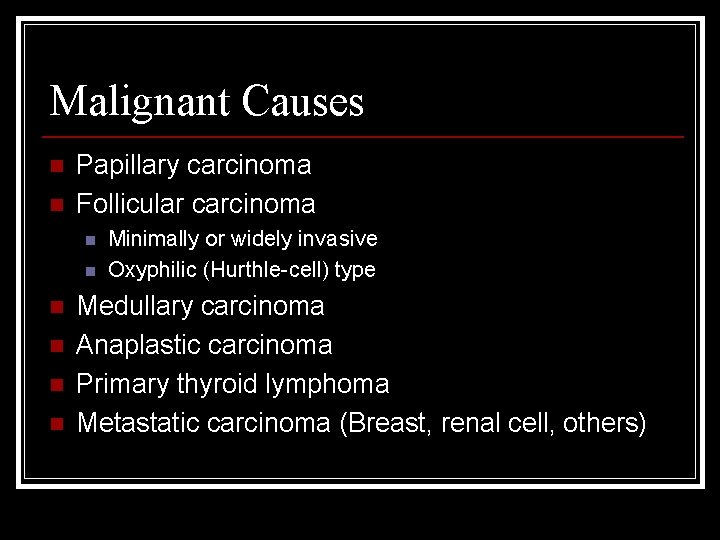
Malignant Causes n n Papillary carcinoma Follicular carcinoma n n n Minimally or widely invasive Oxyphilic (Hurthle-cell) type Medullary carcinoma Anaplastic carcinoma Primary thyroid lymphoma Metastatic carcinoma (Breast, renal cell, others)
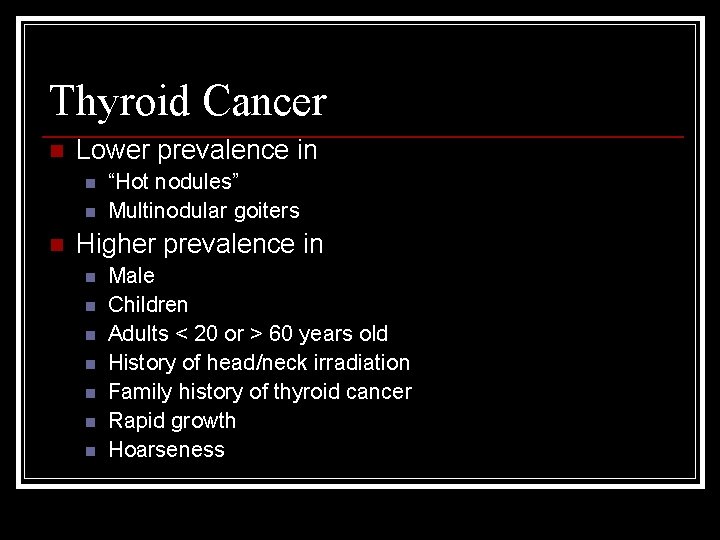
Thyroid Cancer n Lower prevalence in n “Hot nodules” Multinodular goiters Higher prevalence in n n n Male Children Adults < 20 or > 60 years old History of head/neck irradiation Family history of thyroid cancer Rapid growth Hoarseness
Evaluation n History n n n Rapid growth? Family history? Irradiation? Cancer syndromes? Physical Examination n n Fixed, hard mass Vocal cord paralysis Cervical lymphadenopathy Obstructive symptoms
Evaluation n TSH n n n Low Thyroid scintigraphy Not low US to select for FNA biopsy; evaluate for hypothyroidism Ultrasound n n High risk of cancer: hypoechoic, microcalcifications, increased central vascularity, irregular margins, taller than wide, documented enlargement, size >3 cm Low risk of cancer: hyperechoic, peripheral vascularity, pure cyst, comet-tail shadowing
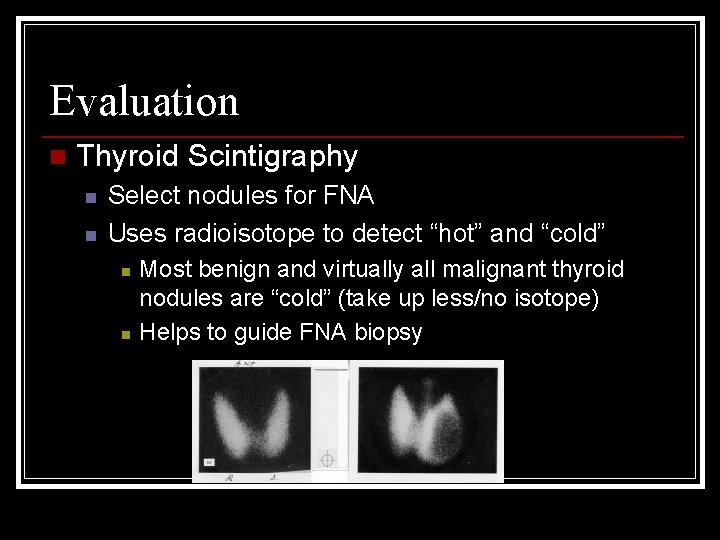
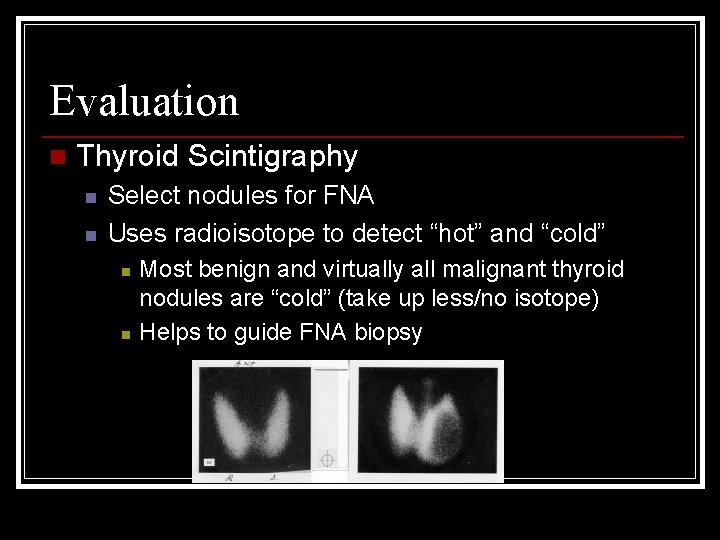
Evaluation n Thyroid Scintigraphy n n Select nodules for FNA Uses radioisotope to detect “hot” and “cold” n n Most benign and virtually all malignant thyroid nodules are “cold” (take up less/no isotope) Helps to guide FNA biopsy
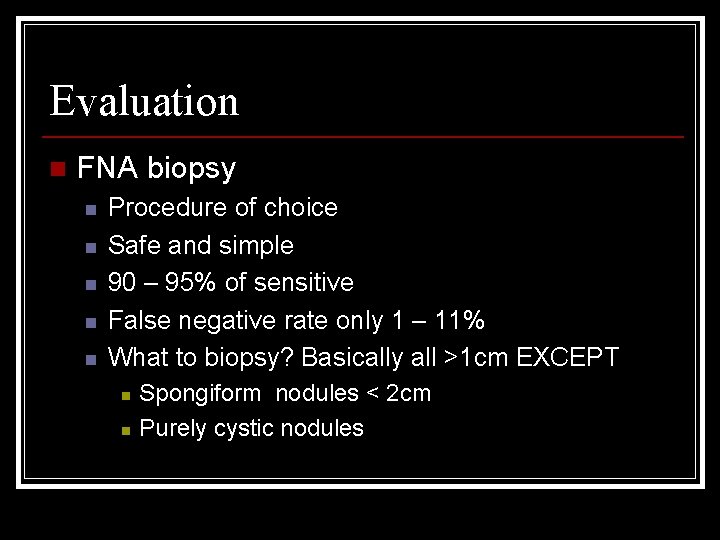
Evaluation n FNA biopsy n n n Procedure of choice Safe and simple 90 – 95% of sensitive False negative rate only 1 – 11% What to biopsy? Basically all >1 cm EXCEPT n n Spongiform nodules < 2 cm Purely cystic nodules
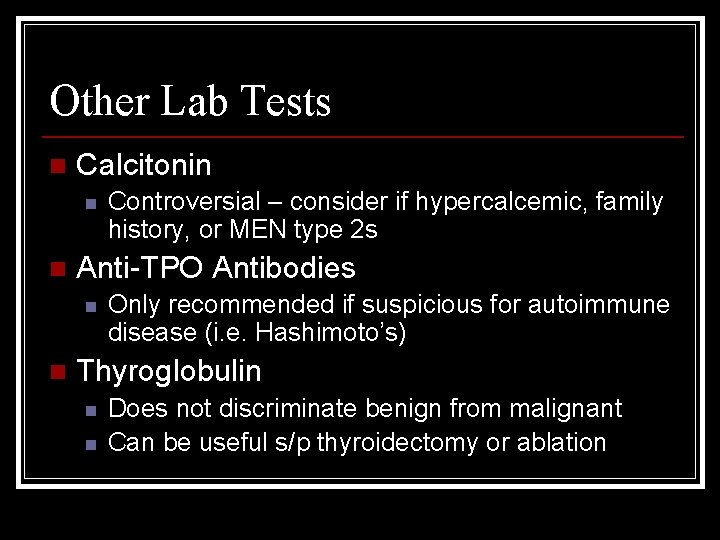
Other Lab Tests n Calcitonin n n Anti-TPO Antibodies n n Controversial – consider if hypercalcemic, family history, or MEN type 2 s Only recommended if suspicious for autoimmune disease (i. e. Hashimoto’s) Thyroglobulin n n Does not discriminate benign from malignant Can be useful s/p thyroidectomy or ablation
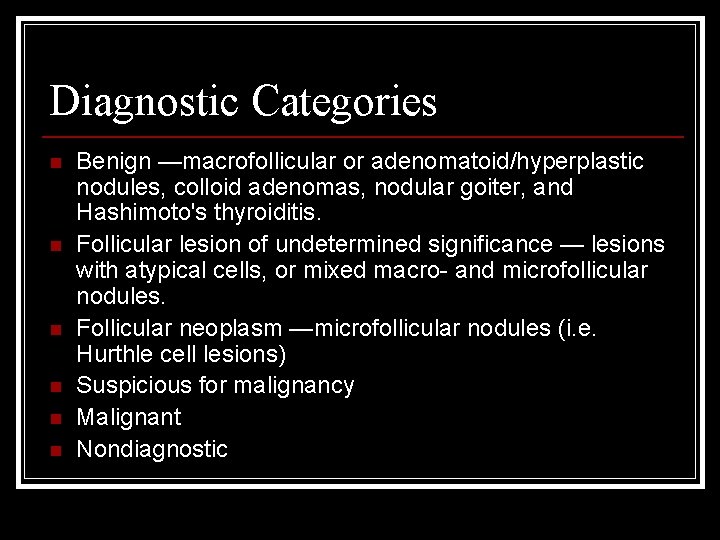
Diagnostic Categories n n n Benign —macrofollicular or adenomatoid/hyperplastic nodules, colloid adenomas, nodular goiter, and Hashimoto's thyroiditis. Follicular lesion of undetermined significance — lesions with atypical cells, or mixed macro- and microfollicular nodules. Follicular neoplasm —microfollicular nodules (i. e. Hurthle cell lesions) Suspicious for malignancy Malignant Nondiagnostic
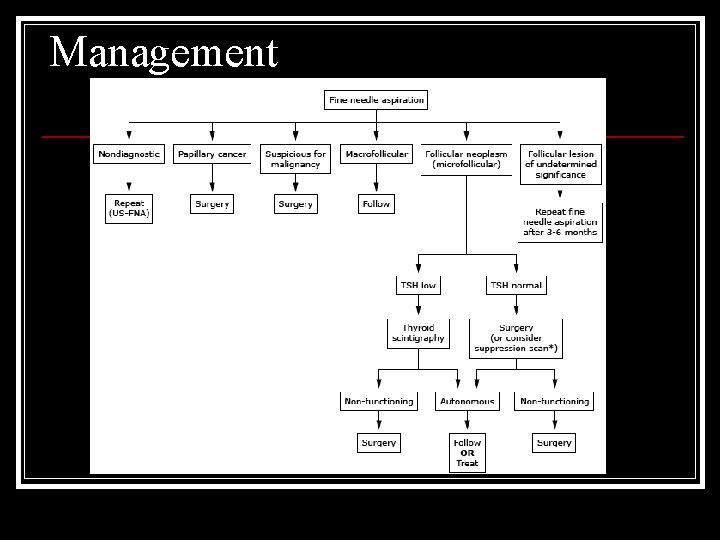
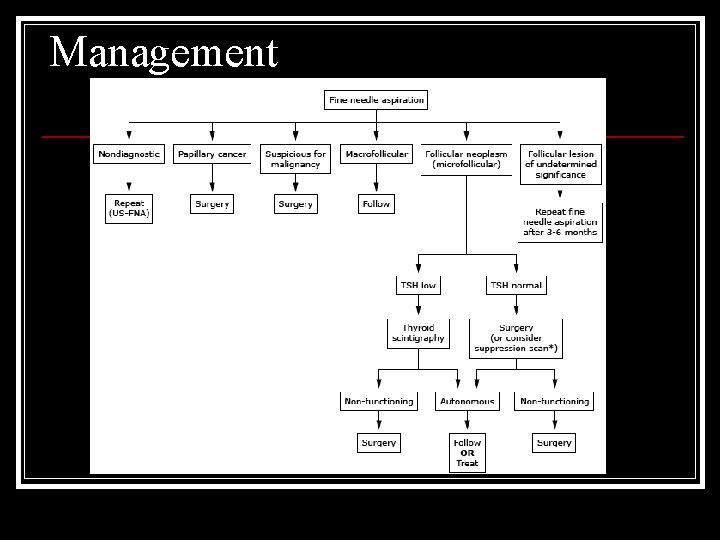
Management
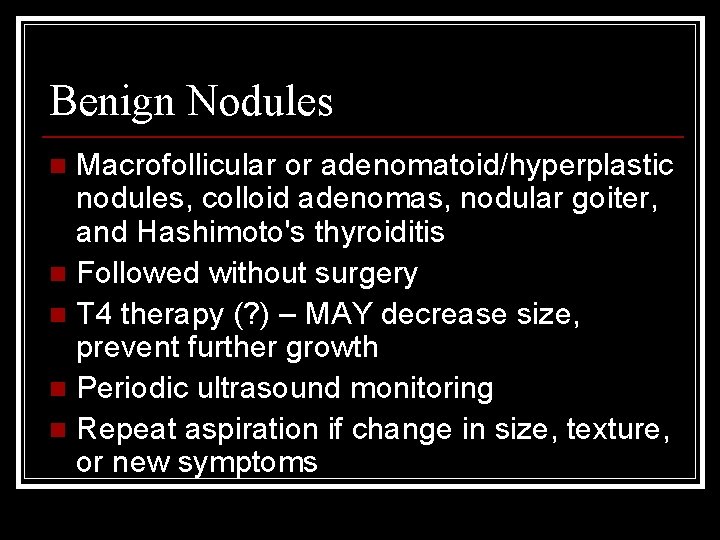
Benign Nodules Macrofollicular or adenomatoid/hyperplastic nodules, colloid adenomas, nodular goiter, and Hashimoto's thyroiditis n Followed without surgery n T 4 therapy (? ) – MAY decrease size, prevent further growth n Periodic ultrasound monitoring n Repeat aspiration if change in size, texture, or new symptoms n
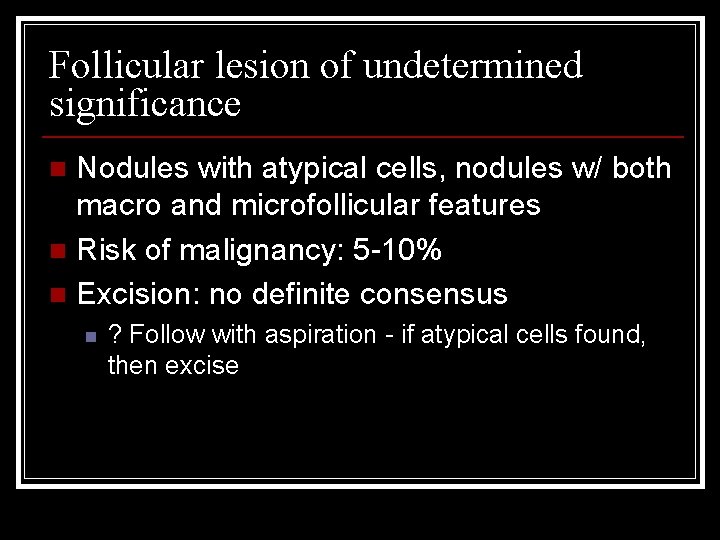
Follicular lesion of undetermined significance Nodules with atypical cells, nodules w/ both macro and microfollicular features n Risk of malignancy: 5 -10% n Excision: no definite consensus n n ? Follow with aspiration - if atypical cells found, then excise
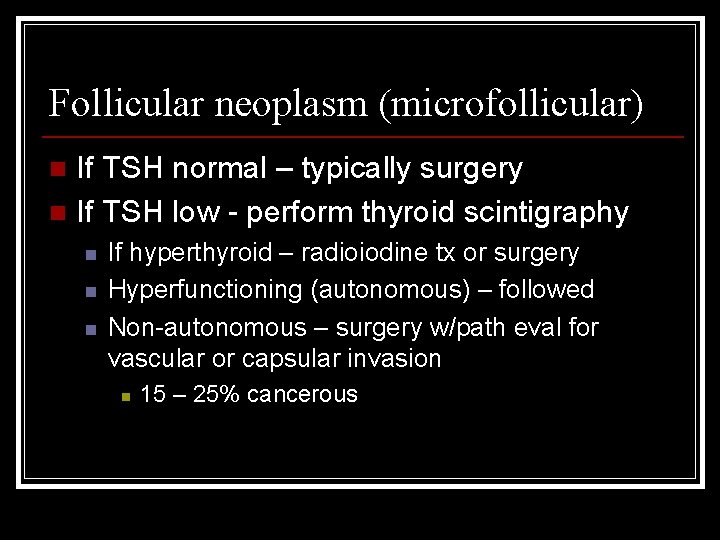
Follicular neoplasm (microfollicular) If TSH normal – typically surgery n If TSH low - perform thyroid scintigraphy n n If hyperthyroid – radioiodine tx or surgery Hyperfunctioning (autonomous) – followed Non-autonomous – surgery w/path eval for vascular or capsular invasion n 15 – 25% cancerous
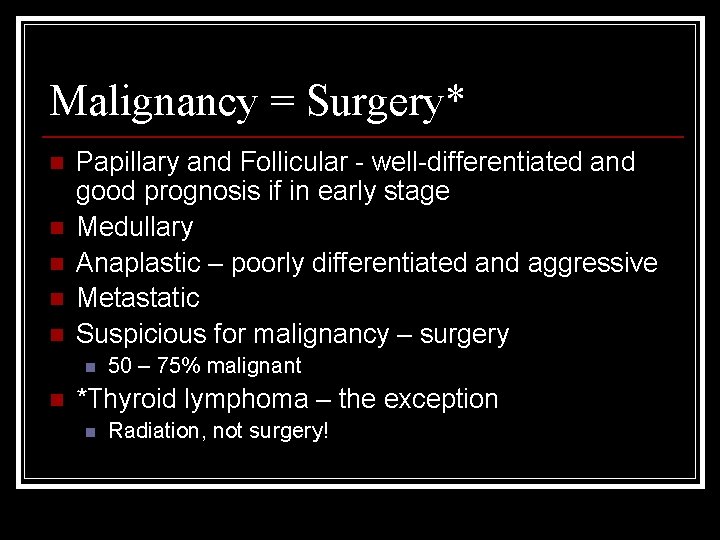
Malignancy = Surgery* n n n Papillary and Follicular - well-differentiated and good prognosis if in early stage Medullary Anaplastic – poorly differentiated and aggressive Metastatic Suspicious for malignancy – surgery n n 50 – 75% malignant *Thyroid lymphoma – the exception n Radiation, not surgery!
Management of other path findings Nondiagnostic FNA – repeat under US n Cystic thyroid nodules – followed or excised for therapeutic reasons if recurrent n Ablation – benign, autonomous, or cystic n n n Inject ethanol or other sclerosing agent Controversial (complications, prolonged pain)
References MKSAP 15: Endocrinology and Metabolism n Harrison’s Internal Medicine n Up. To. Date: Thyroid Nodules n
THE END