Thyroid Gland Part 2 Physiologic Changes in Thyroid
- Slides: 27
Thyroid Gland Part 2
Physiologic Changes in Thyroid Function • Thyroid Function in the Fetus – At birth, there is a sudden marked rise in TSH, in T 4 and in T 3 – These parameters gradually return to normal over the first month of life • Thyroid Function in Pregnancy – There is an increase in urinary iodide clearance; in areas of low dietary iodine intake, this can cause maternal goiter, or when severe, hypothyroidism – During pregnancy, there is a rise in TBG, Consequently, serum total T 4, and to a lesser extent, total T 3 concentrations rise – Rising levels of h. CG, which has weak TSH receptor agonist activity, contributes to minimal thyroid enlargement • peak at approx. 12 weeks resulting in a transient high-normal or even modestly elevated serum free T 4 level and a physiologic suppression of serum TSH Dr. M. Alzaharna (2014) 2
Physiologic Changes in Thyroid Function • Effects of Acute & Chronic illness on Thyroid Function (Euthyroid Sick Syndrome) – Acute or chronic illness has several striking effects on thyroid function – The most common and earliest effect is inhibition of T 4 to T 3 conversion – low serum T 3 levels are typically accompanied by total and free T 4 levels that are normal Dr. M. Alzaharna (2014) 3
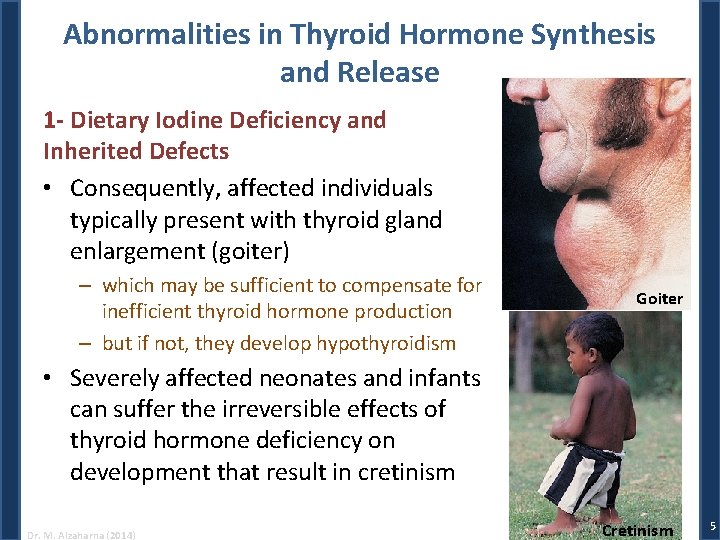
Abnormalities in Thyroid Hormone Synthesis and Release 1 -Dietary Iodine Deficiency and Inherited Defects • A very low iodine diet and inherited defects in genes encoding the proteins required for thyroid hormone biosynthesis (dyshormonogenesis) can both result in insufficient hormone production • The major adaptation to low iodide intake is the preferential synthesis of T 3 rather than T 4 • In response, the hypothalamic-pituitary-thyroid axis responds to thyroid hormone deficiency by increasing TSH secretion Dr. M. Alzaharna (2014) 4
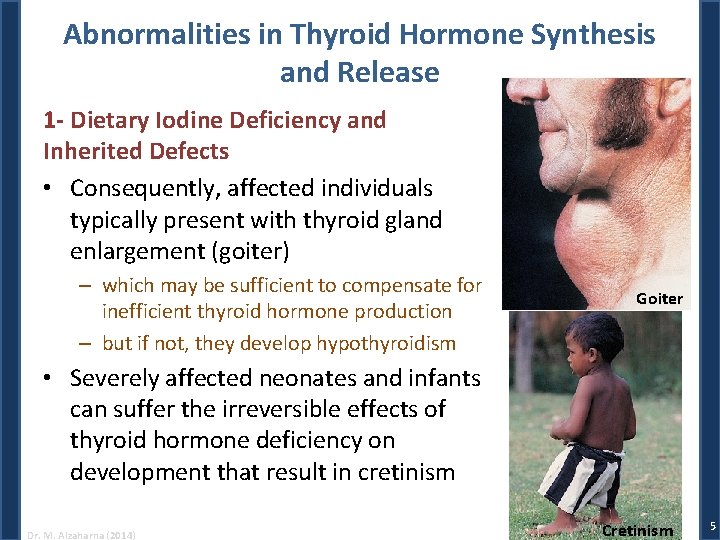
Abnormalities in Thyroid Hormone Synthesis and Release 1 - Dietary Iodine Deficiency and Inherited Defects • Consequently, affected individuals typically present with thyroid gland enlargement (goiter) – which may be sufficient to compensate for inefficient thyroid hormone production – but if not, they develop hypothyroidism Goiter • Severely affected neonates and infants can suffer the irreversible effects of thyroid hormone deficiency on development that result in cretinism Dr. M. Alzaharna (2014) Cretinism 5
Abnormalities in Thyroid Hormone Synthesis and Release 2 - Effects of Iodine Excess on Hormone Biosynthesis • Excess iodide actually inhibits three steps in thyroid hormone production: – iodide trapping – thyroglobulin iodination – and thyroid hormone release from the gland • These inhibitory actions are transient, and the normal thyroid gland “escapes” after 10 to 14 days from these effects of excess iodide • These autoregulatory effects of iodide insulate physiologic thyroid function from short term fluctuations in iodine intake • This effect of iodide has been exploited clinically to produce short-term suppression of thyroid hormone secretion Dr. M. Alzaharna (2014) 6
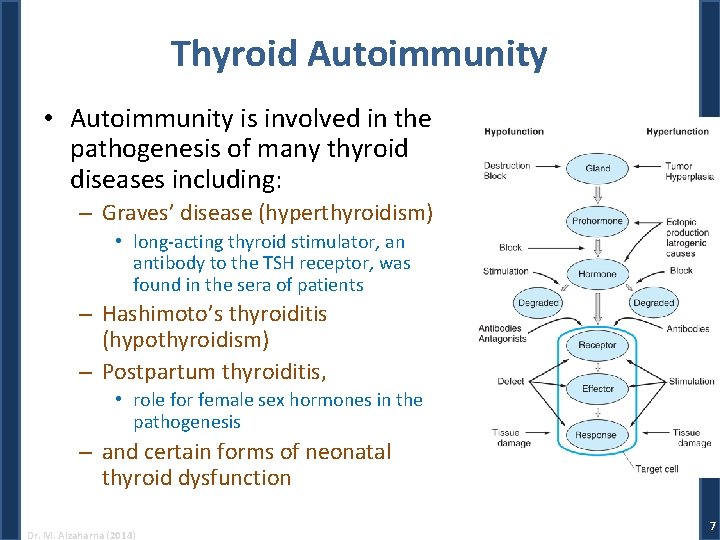
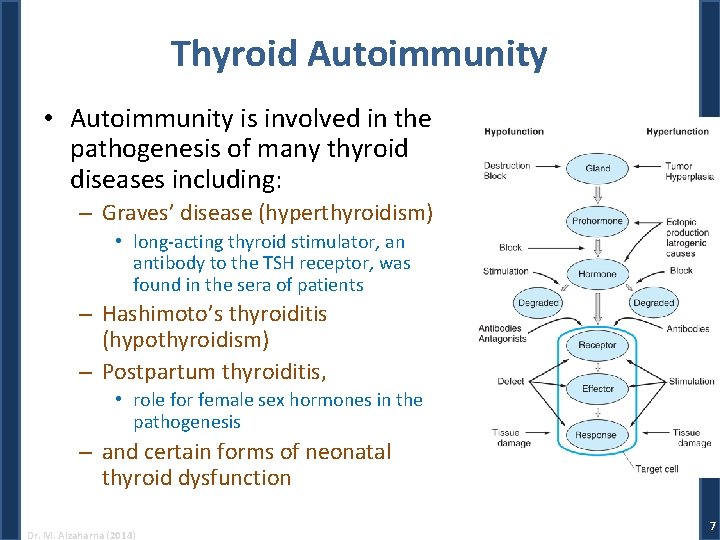
Thyroid Autoimmunity • Autoimmunity is involved in the pathogenesis of many thyroid diseases including: – Graves’ disease (hyperthyroidism) • long-acting thyroid stimulator, an antibody to the TSH receptor, was found in the sera of patients – Hashimoto’s thyroiditis (hypothyroidism) – Postpartum thyroiditis, • role for female sex hormones in the pathogenesis – and certain forms of neonatal thyroid dysfunction Dr. M. Alzaharna (2014) 7
Thyroid Autoimmunity • There are three major thyroidal autoantigens: – Thyroglobulin, – TPO, – and the TSH receptor • Circulating autoantibodies to these antigens are useful markers for thyroid autoimmunity Dr. M. Alzaharna (2014) 8
Disorders of The Thyroid • Patients with thyroid disease usually complain of one or more of the following: – Hypothyroidism, symptoms of thyroid hormone deficiency – Hyperthyroidism, symptoms of thyroid hormone excess – Thyroid enlargement which may be • diffuse or nodular; Dr. M. Alzaharna (2014) 9
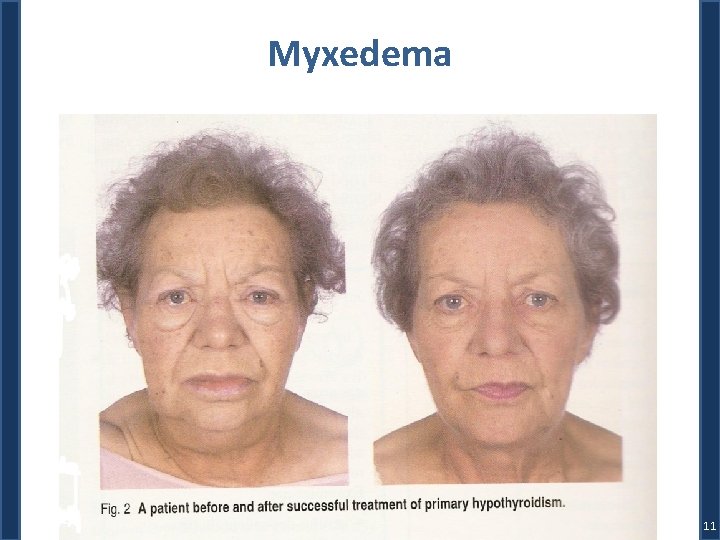
Hypothyroidism • Hypothyroidism is a clinical syndrome resulting from a deficiency of thyroid hormones, which in turn results in a generalized slowing down of metabolic processes – Hypothyroidism in infants and children results in: • marked slowing of growth and development, • with serious permanent consequences, including mental retardation, when it occurs in infancy – Hypothyroidism with onset in adulthood causes: • generalized decrease in metabolism, • diminished oxygen consumption, • and deposition of glycosaminoglycans in intracellular spaces, particularly in skin and muscle, producing in extreme cases the clinical picture of myxedema • The symptoms and signs of hypothyroidism in adults are reversible with therapy Dr. M. Alzaharna (2014) 10
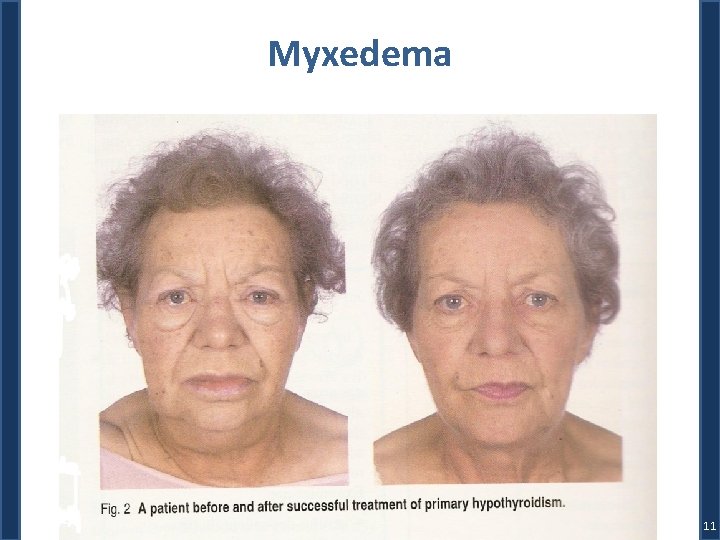
Myxedema 11
Other symptoms of Hypothyroidism • Cardiovascular signs – Bradycardia • Pulmonary function – shallow, slow respirations • Renal function – impaired with decreased glomerular filtration rate • Neuromuscular system – Muscle weakness • Central nervous system – fatigue, lethargy and inability to concentrate Dr. M. Alzaharna (2014) 12
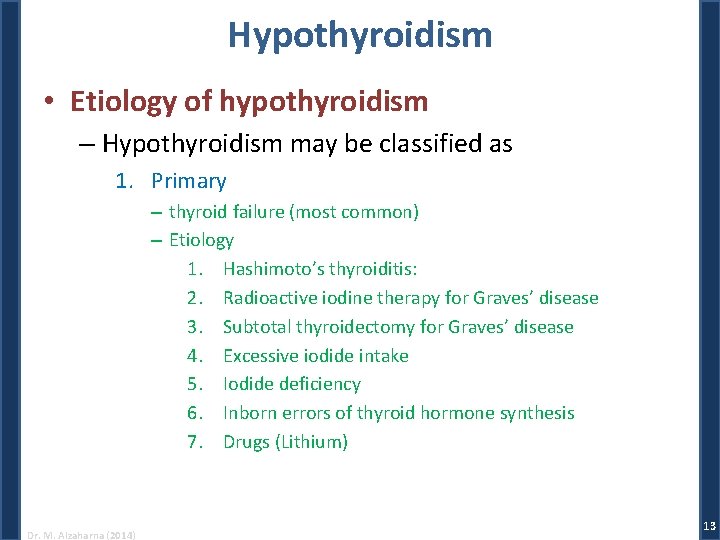
Hypothyroidism • Etiology of hypothyroidism – Hypothyroidism may be classified as 1. Primary – thyroid failure (most common) – Etiology 1. Hashimoto’s thyroiditis: 2. Radioactive iodine therapy for Graves’ disease 3. Subtotal thyroidectomy for Graves’ disease 4. Excessive iodide intake 5. Iodide deficiency 6. Inborn errors of thyroid hormone synthesis 7. Drugs (Lithium) Dr. M. Alzaharna (2014) 13
2. Secondary – due to pituitary TSH deficiency 3. Tertiary – due to hypothalamic deficiency of TRH 4. Peripheral resistance to the action of thyroid hormones Dr. M. Alzaharna (2014) 14
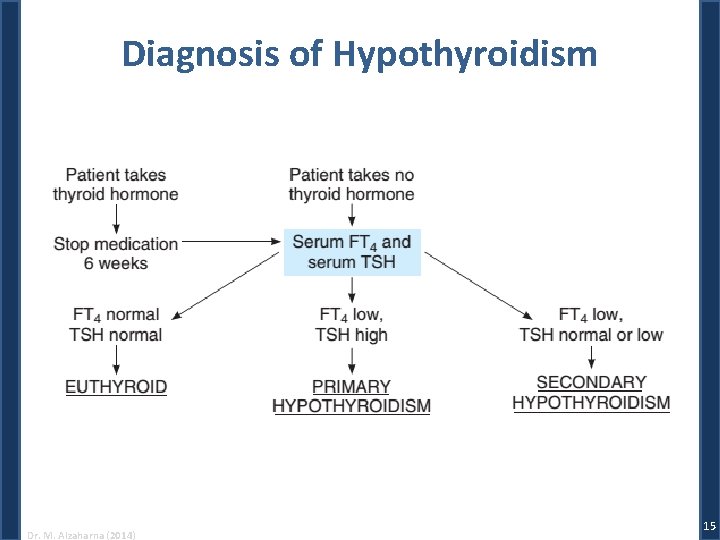
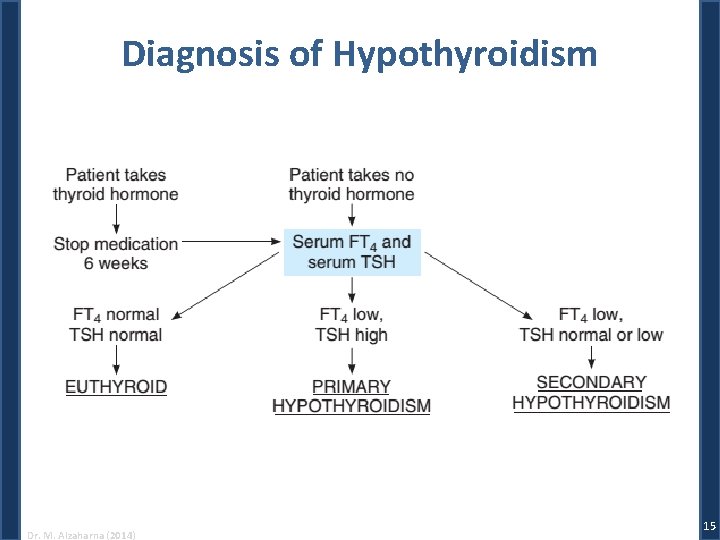
Diagnosis of Hypothyroidism Dr. M. Alzaharna (2014) 15
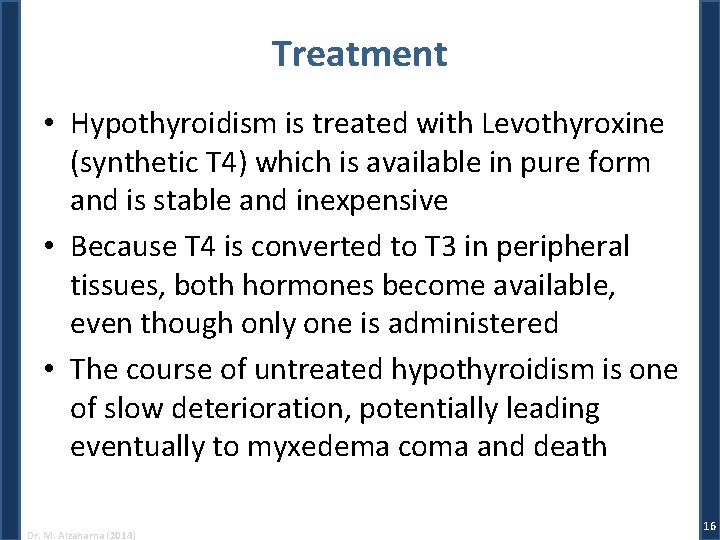
Treatment • Hypothyroidism is treated with Levothyroxine (synthetic T 4) which is available in pure form and is stable and inexpensive • Because T 4 is converted to T 3 in peripheral tissues, both hormones become available, even though only one is administered • The course of untreated hypothyroidism is one of slow deterioration, potentially leading eventually to myxedema coma and death Dr. M. Alzaharna (2014) 16
Hyperthyroidism & Thyrotoxicosis • Hyperthyroidism is a condition in which the thyroid gland produces and secretes excessive amounts of thyroid hormones • Thyrotoxicosis is the clinical syndrome that results when tissues are exposed to high levels of circulating thyroid hormones • It results in a generalized acceleration of metabolic processes • In most instances, thyrotoxicosis is due to hyperactivity of the thyroid gland, or hyperthyroidism Dr. M. Alzaharna (2014) 17
Symptoms of Hyperthyroidism • Cardiovascular signs – Tachycardia • Neuromuscular system – Tremor • Neurological – Anxiety Dr. M. Alzaharna (2014) 18
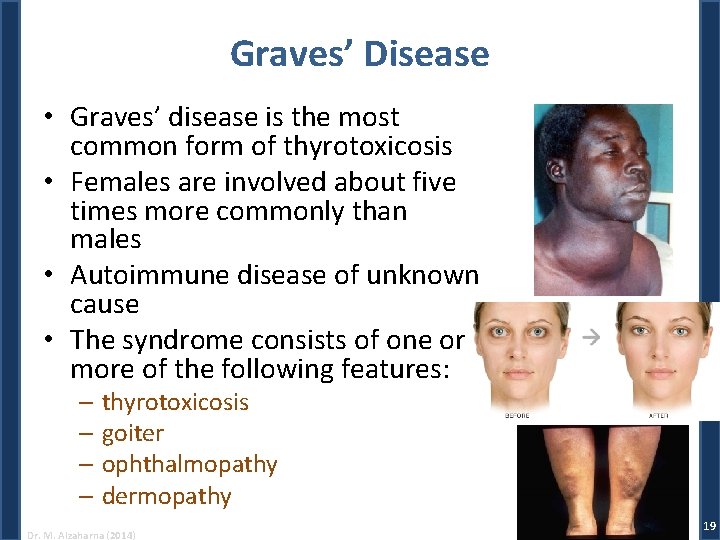
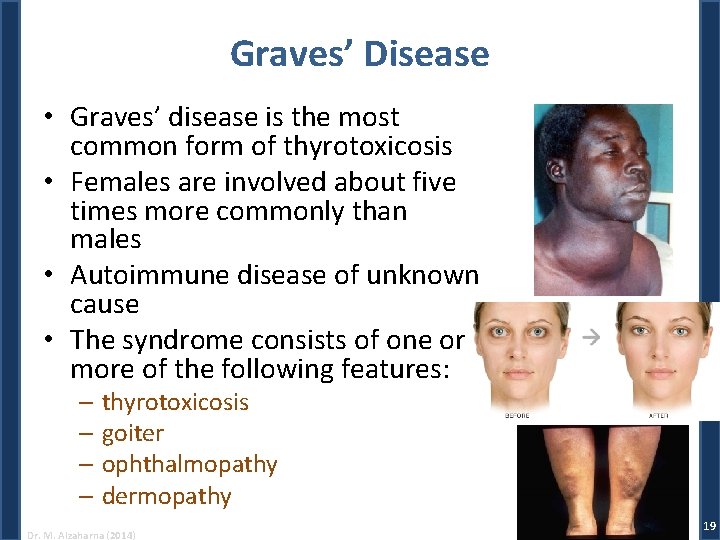
Graves’ Disease • Graves’ disease is the most common form of thyrotoxicosis • Females are involved about five times more commonly than males • Autoimmune disease of unknown cause • The syndrome consists of one or more of the following features: – thyrotoxicosis – goiter – ophthalmopathy – dermopathy Dr. M. Alzaharna (2014) 19
Treatment of Graves’ Disease • Although autoimmune mechanisms are responsible for the syndrome of Graves’ disease, management has been largely directed toward controlling the hyperthyroidism • Three good methods are available: – Antithyroid Drug therapy • inhibiting TPO-mediated iodination of thyroglobulin – Surgery • Partial or total thyroidectomy – and radioactive iodine therapy (131 I) • destroys thyroid cells Dr. M. Alzaharna (2014) 20
Other Forms of Thyrotoxicosis Toxic Adenoma • A functioning adenoma hypersecreting T 3 and T 4 causes hyperthyroidism • These lesions start out as a small autonomously functioning nodule that slowly increases in size to produce excessive quantities of thyroid hormones • This gradually suppresses endogenous TSH secretion, which results in reduced function of the contralateral lobe of the gland Dr. M. Alzaharna (2014) 21
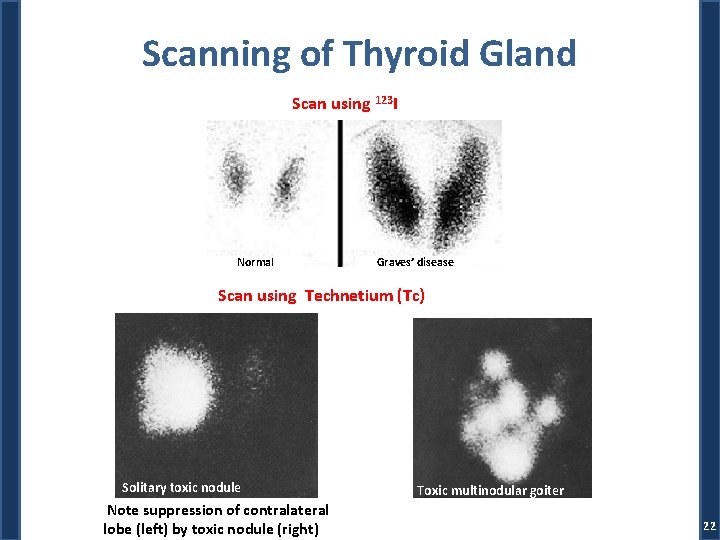
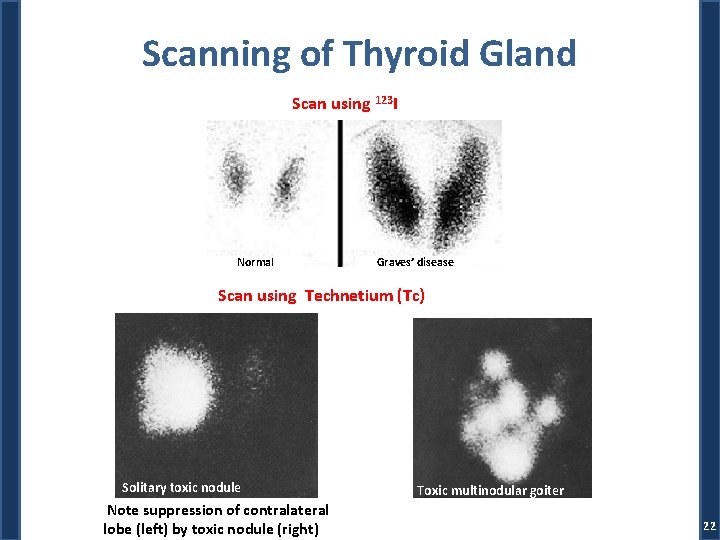
Scanning of Thyroid Gland Scan using 123 I Normal Graves’ disease Scan using Technetium (Tc) Solitary toxic nodule Note suppression of contralateral lobe (left) by toxic nodule (right) Toxic multinodular goiter 22
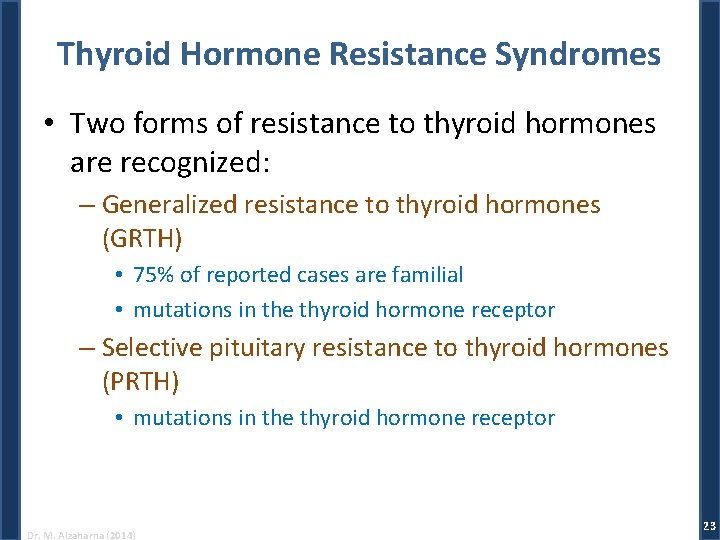
Thyroid Hormone Resistance Syndromes • Two forms of resistance to thyroid hormones are recognized: – Generalized resistance to thyroid hormones (GRTH) • 75% of reported cases are familial • mutations in the thyroid hormone receptor – Selective pituitary resistance to thyroid hormones (PRTH) • mutations in the thyroid hormone receptor Dr. M. Alzaharna (2014) 23
Nontoxic Goiter • Nontoxic goiter is not associated with hyperthyroidism • Can be diffuse or nodular • May result from TSH stimulation due to inadequate thyroid hormone synthesis • Worldwide, iodine deficiency remains the most common cause of nontoxic goiter Dr. M. Alzaharna (2014) 24
Thyroiditis • Subacute Thyroiditis – is an acute inflammatory disorder of the thyroid gland most likely due to viral infection • Chronic Thyroiditis – Hashimoto’s thyroiditis Dr. M. Alzaharna (2014) 25
Thyroid Nodules & Thyroid Cancer • Thyroid nodules are common – Benign Thyroid Nodules • But thyroid cancer is a relatively rare condition – Follicular carcinoma – Medullary carcinoma • disease of the C cells (parafollicular cells) Dr. M. Alzaharna (2014) 26
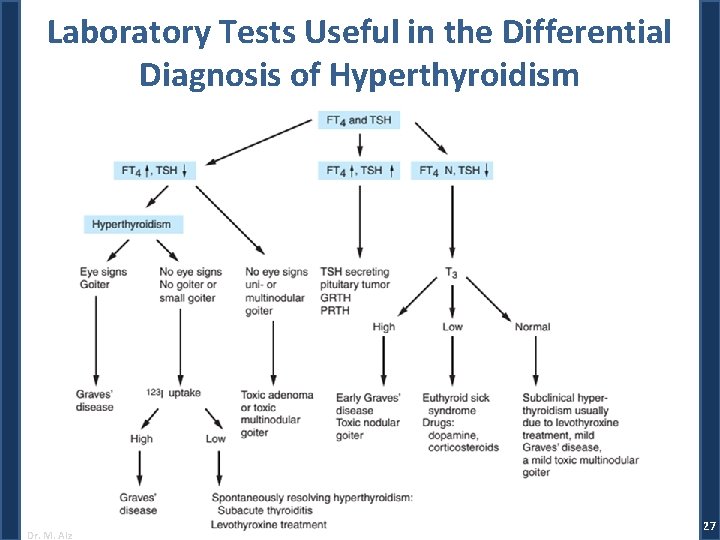
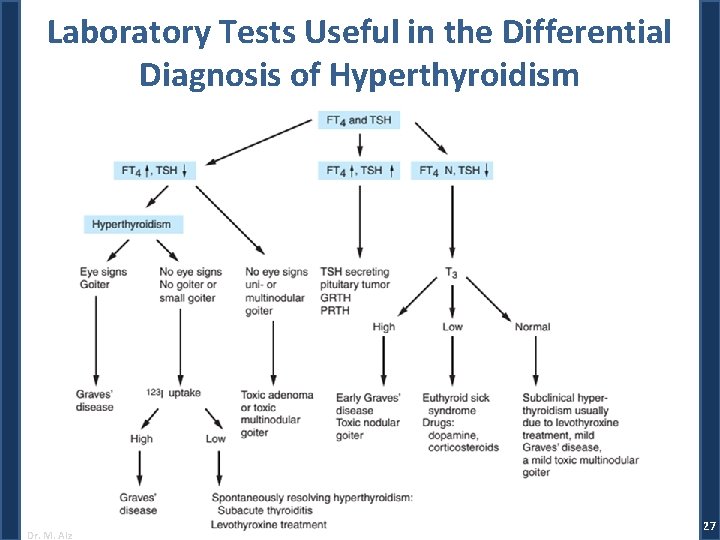
Laboratory Tests Useful in the Differential Diagnosis of Hyperthyroidism Dr. M. Alzaharna (2014) 27