Thyroid Gland Importance In the adult human normal
- Slides: 21
Thyroid Gland
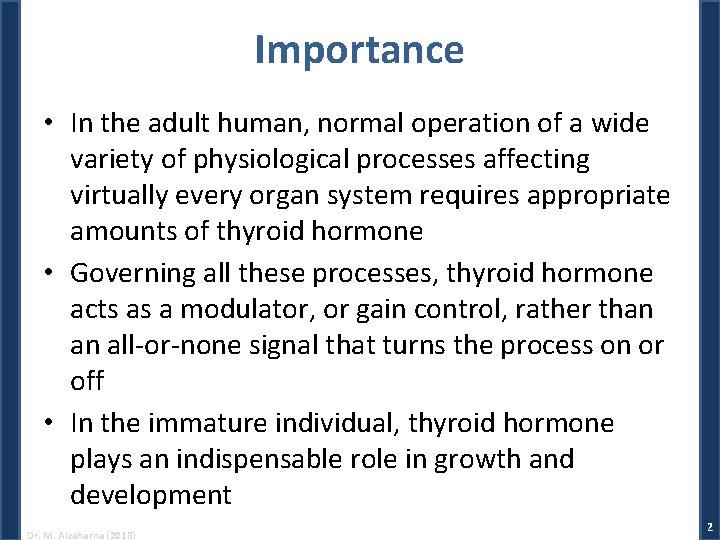
Importance • In the adult human, normal operation of a wide variety of physiological processes affecting virtually every organ system requires appropriate amounts of thyroid hormone • Governing all these processes, thyroid hormone acts as a modulator, or gain control, rather than an all-or-none signal that turns the process on or off • In the immature individual, thyroid hormone plays an indispensable role in growth and development Dr. M. Alzaharna (2018) 2
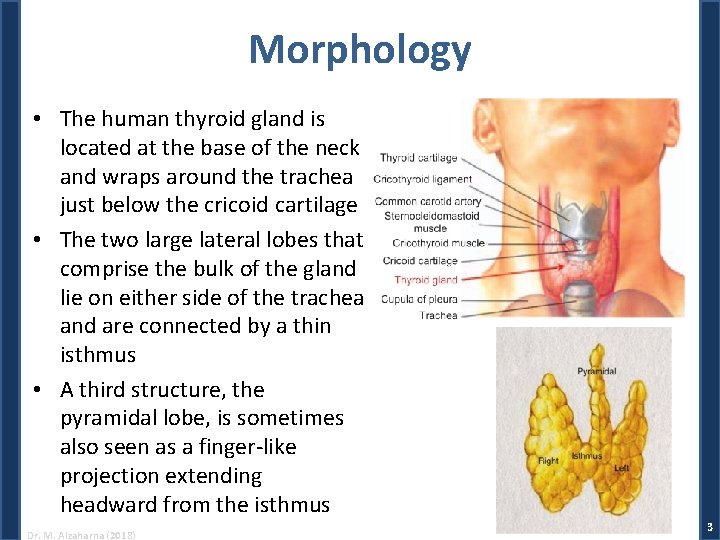
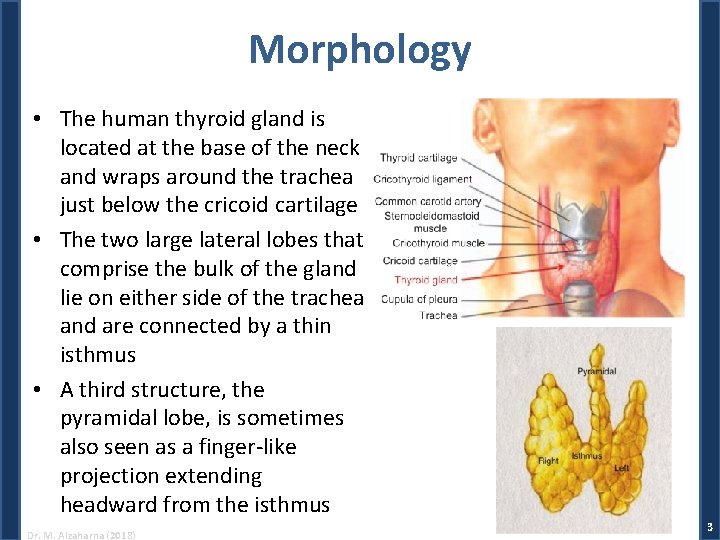
Morphology • The human thyroid gland is located at the base of the neck and wraps around the trachea just below the cricoid cartilage • The two large lateral lobes that comprise the bulk of the gland lie on either side of the trachea and are connected by a thin isthmus • A third structure, the pyramidal lobe, is sometimes also seen as a finger-like projection extending headward from the isthmus Dr. M. Alzaharna (2018) 3
Morphology • The thyroid gland in the normal human being weighs about 20 g but is capable of enormous growth, sometimes achieving a weight of several hundred grams when stimulated intensely over a long period of time • Relative to its weight, the thyroid gland receives a greater flow of blood than most other tissues of the body • The thyroid gland also has an abundant supply of sympathetic and parasympathetic nerves Dr. M. Alzaharna (2018) 4
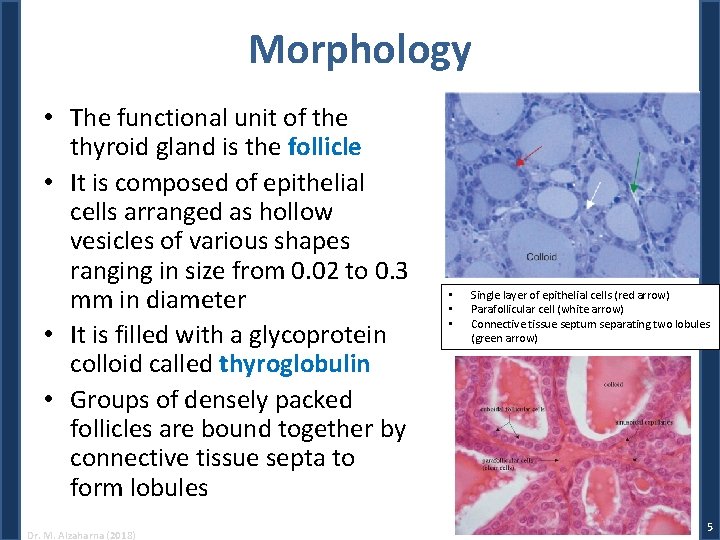
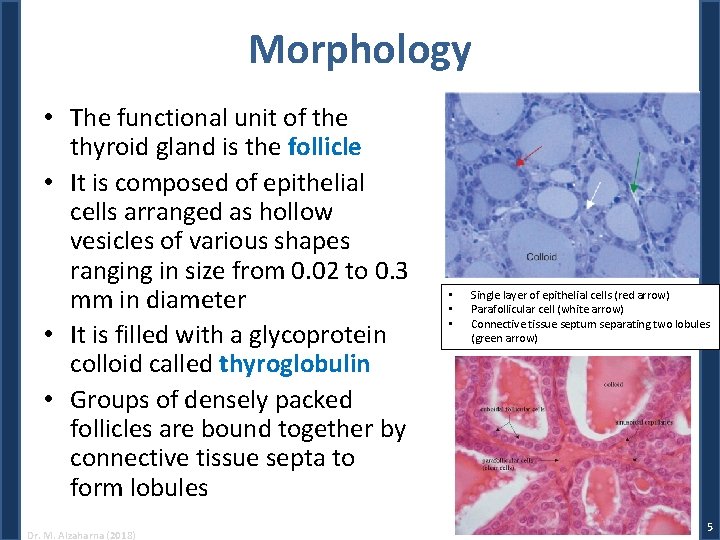
Morphology • The functional unit of the thyroid gland is the follicle • It is composed of epithelial cells arranged as hollow vesicles of various shapes ranging in size from 0. 02 to 0. 3 mm in diameter • It is filled with a glycoprotein colloid called thyroglobulin • Groups of densely packed follicles are bound together by connective tissue septa to form lobules Dr. M. Alzaharna (2018) • • • Single layer of epithelial cells (red arrow) Parafollicular cell (white arrow) Connective tissue septum separating two lobules (green arrow) 5
• Secretory cells of the thyroid gland are of two types: – Follicular cells, which produce the classical thyroid hormones, thyroxine and triiodothyronine – Parafollicular, or C cells, are located between the follicles and produce the polypeptide hormone calcitonin Dr. M. Alzaharna (2018) 6
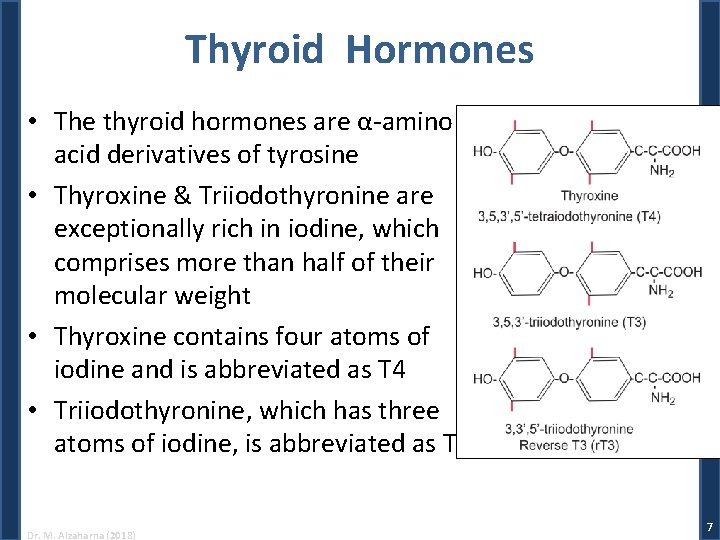
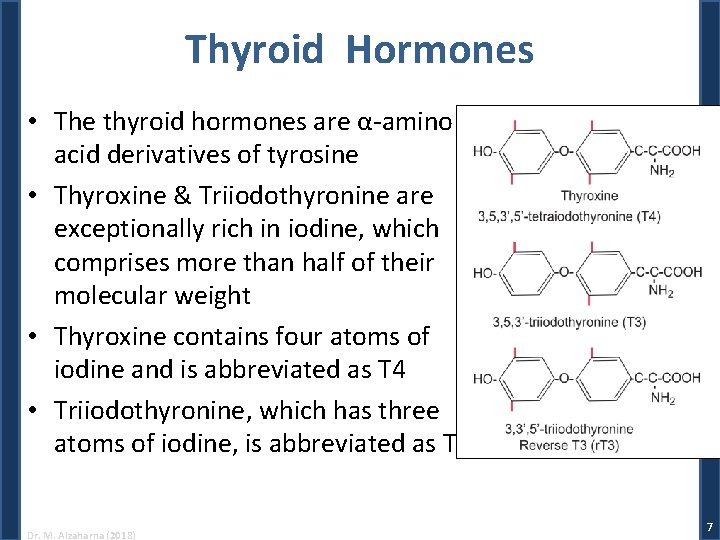
Thyroid Hormones • The thyroid hormones are α-amino acid derivatives of tyrosine • Thyroxine & Triiodothyronine are exceptionally rich in iodine, which comprises more than half of their molecular weight • Thyroxine contains four atoms of iodine and is abbreviated as T 4 • Triiodothyronine, which has three atoms of iodine, is abbreviated as T 3 Dr. M. Alzaharna (2018) 7
Biosynthesis • Several aspects of the production of thyroid hormone are unusual: – Thyroid hormones contain large amounts of iodine • Efficient energy-dependent transport mechanism that allows thyroid cells to take up and concentrate iodide • The thyroid gland is also the principal site of storage of this rare dietary constituent – Thyroid hormones are partially synthesized extracellularly at the luminal surface of follicular cells and stored in an extracellular compartment, the follicular lumen – Thyroglobulin, is released from apical surfaces of follicular cells into the follicular lumen, only to be taken up again by follicular cells and degraded to release T 4 and T 3 from the basal surfaces of follicular cells – Thyroxine, the major secretory product, is not the biologically active form of the hormone, but must be transformed to T 3 at extrathyroidal sites Dr. M. Alzaharna (2018) 8
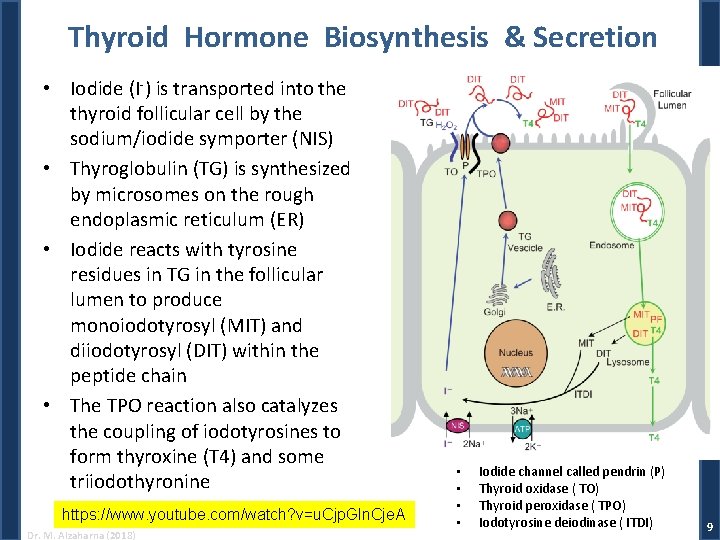
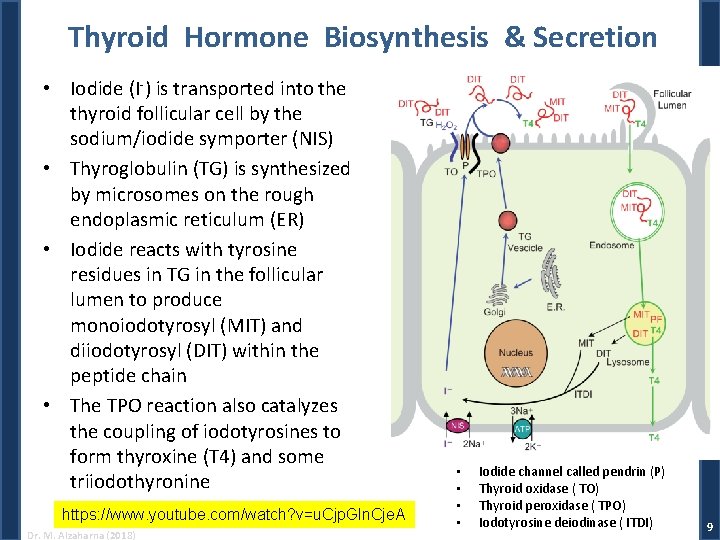
Thyroid Hormone Biosynthesis & Secretion • Iodide (I-) is transported into the thyroid follicular cell by the sodium/iodide symporter (NIS) • Thyroglobulin (TG) is synthesized by microsomes on the rough endoplasmic reticulum (ER) • Iodide reacts with tyrosine residues in TG in the follicular lumen to produce monoiodotyrosyl (MIT) and diiodotyrosyl (DIT) within the peptide chain • The TPO reaction also catalyzes the coupling of iodotyrosines to form thyroxine (T 4) and some triiodothyronine https: //www. youtube. com/watch? v=u. Cjp. Gln. Cje. A Dr. M. Alzaharna (2018) • • Iodide channel called pendrin (P) Thyroid oxidase ( TO) Thyroid peroxidase ( TPO) Iodotyrosine deiodinase ( ITDI) 9
Hormone Storage • The thyroid is unique among endocrine glands in that it stores its product extracellularly as large precursor molecules in follicular lumens • In the normal individual, approximately 30% of the mass of the thyroid gland is thyroglobulin, which corresponds to about two to three months supply of hormone Dr. M. Alzaharna (2018) 10
Control of Thyroid Function • The principal regulator of thyroid function is the thyroid-stimulating hormone (TSH), which is secreted by thyrotropes in the pituitary gland • Binding of TSH to the G-protein coupled receptor results in its activation and production of c-AMP • Each step of hormone biosynthesis, storage, and secretion appears to be directly stimulated by a c. AMP-dependent process • This lead finally to phosphorylation of proteins including transcription factors and protein production • TSH also increases blood flow to the thyroid Dr. M. Alzaharna (2018) 11
Thyroid Hormones in Blood • More than 99. 8% of thyroid hormone circulating in blood is bound firmly to three plasma proteins: – thyroxine-binding globulin (TBG), • 70% of the total protein-bound hormone – transthyretin (TTR), – and albumin • Less than 1% of hormone present in free solution is in equilibrium with bound hormone and is the only hormone that can escape from capillaries to produce biological activity Dr. M. Alzaharna (2018) 12
Metabolism of Thyroid Hormones • Because T 4 is bound much more tightly by plasma proteins than T 3, a greater fraction of T 3 is free to diffuse out of the vascular compartment and into cells where it can produce its biological effects or be degraded • Although the main secretory product of the thyroid gland the major form of thyroid hormone present in the circulating plasma reservoir is T 4, it is primarily T 3 and not T 4 that binds to thyroid hormone receptors • T 4 can be considered to be a prohormone that serves as the precursor for extrathyroidal formation of T 3 (Iodotyrosine deiodinase ) Dr. M. Alzaharna (2018) 13
Physiological Effects of Thyroid Hormones • Growth and maturation – Skeletal system – Central nervous system • normal development of the brain • Metabolism – Oxidative metabolism and thermogenesis – Carbohydrate metabolism • increases glucose absorption from the digestive tract, glycogenolysis and gluconeogenesis • and glucose oxidation in liver, fat, and muscle cells Dr. M. Alzaharna (2018) 14
Physiological Effects of Thyroid Hormones – Lipid metabolism • The primary determinant of lipogenesis is not T 3 – Nitrogen metabolism • Cardiovascular system – Cardiac output is increased in hyperthyroidism and decreased in thyroid deficiency • Autonomic nervous system – Thyroid hormones increase the abundance of receptors for epinephrine and norepinephrine in the myocardium and some other tissues Dr. M. Alzaharna (2018) 15
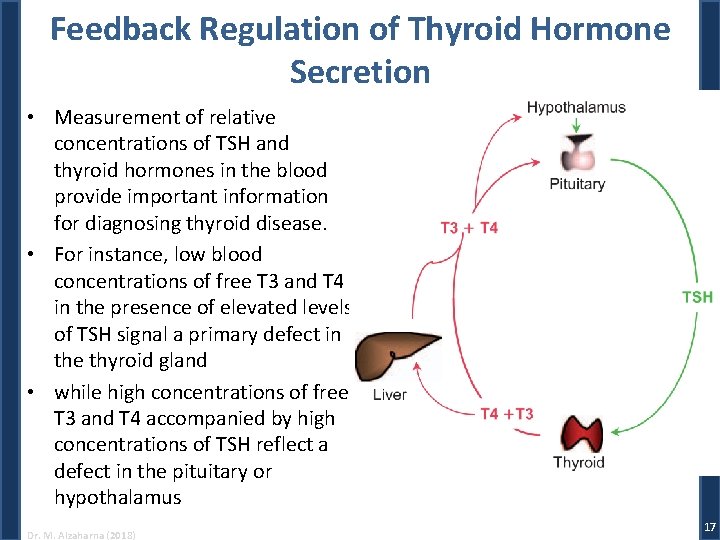
Regulation of Thyroid Hormone Secretion • Secretion of thyroid hormones depends on stimulation of thyroid follicular cells by TSH – TSH absence: quiescent and atrophy of thyroid cells – administration of TSH increases both synthesis and secretion of T 4 and T 3 • TSH bears primary responsibility for integrating thyroid function with bodily needs • Secretion of TSH by the pituitary gland is governed by: – positive input from the hypothalamus by way of thyrotropin releasing hormone (TRH) – and negative input from the thyroid gland by way of T 3 and T 4 Dr. M. Alzaharna (2018) 16
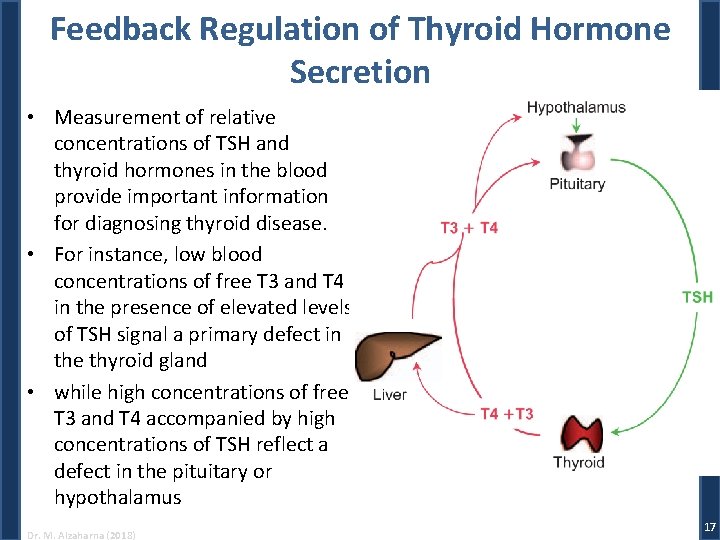
Feedback Regulation of Thyroid Hormone Secretion • Measurement of relative concentrations of TSH and thyroid hormones in the blood provide important information for diagnosing thyroid disease. • For instance, low blood concentrations of free T 3 and T 4 in the presence of elevated levels of TSH signal a primary defect in the thyroid gland • while high concentrations of free T 3 and T 4 accompanied by high concentrations of TSH reflect a defect in the pituitary or hypothalamus Dr. M. Alzaharna (2018) 17
Mechanism of Thyroid Hormone Action • As must already be obvious, virtually all cells appear to require optimal amounts of thyroid hormone for normal operation • The thyroid hormones exert their actions through two general mechanisms: – genomic actions effected through T 3 interactions with its nuclear receptors, regulating gene activity; – and nongenomic actions mediated by T 3 and T 4 interactions with certain enzymes, glucose transporters, and mitochondrial proteins Dr. M. Alzaharna (2018) 18
• Thyroid hormone receptors are members of the nuclear receptor superfamily of transcription factors and bind T 3 about ten times more avidly than T 4 • Unlike most other nuclear receptors, thyroid hormone receptors bind to specific nucleotide sequences (thyroid response elements or TREs) in the genes they regulate whether or not the hormone is present • They may bind as monomers, but more typically as homodimers composed of two thyroid hormone receptors or as heterodimers with other nuclear receptor family members Dr. M. Alzaharna (2018) 19
Mechanism of Thyroid Hormone Action • In the absence of T 3, the unoccupied receptor, in conjunction with a corepressor protein complex inhibits T 3 -dependent gene expression by maintaining the DNA in a tightly coiled configuration – This bars access of transcription activators or RNA polymerase • Upon binding T 3, the configuration of the receptor is modified in a way that causes it to release the corepressor and bind instead to a coactivator Dr. M. Alzaharna (2018) 20
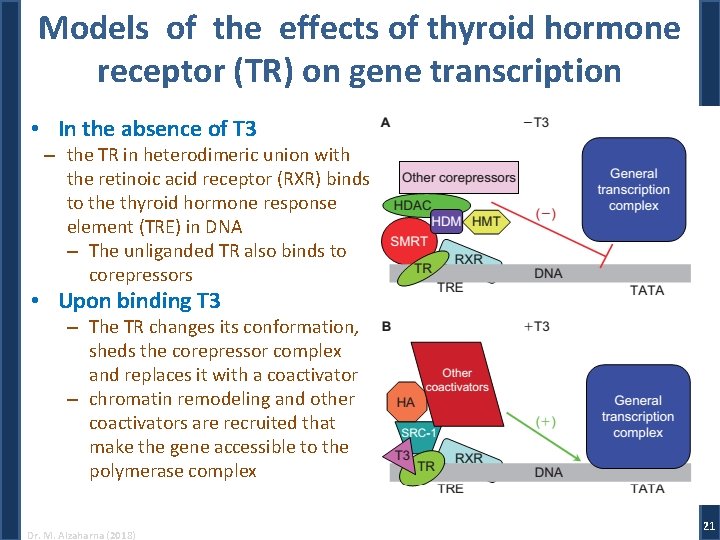
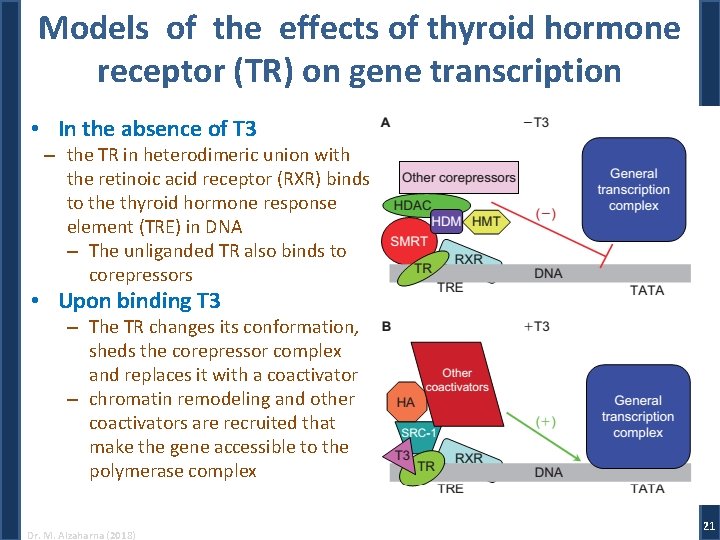
Models of the effects of thyroid hormone receptor (TR) on gene transcription • In the absence of T 3 – the TR in heterodimeric union with the retinoic acid receptor (RXR) binds to the thyroid hormone response element (TRE) in DNA – The unliganded TR also binds to corepressors • Upon binding T 3 – The TR changes its conformation, sheds the corepressor complex and replaces it with a coactivator – chromatin remodeling and other coactivators are recruited that make the gene accessible to the polymerase complex Dr. M. Alzaharna (2018) 21