Thyroid disorders in everyday care Chris Vreeland RN


- Slides: 38
Thyroid disorders in everyday care Chris Vreeland, RN, MSN, NP-c Georgia Mountain Endocrinology, PC
Introduction • One in ten Americans have a thyroid disorder • Body’s response to thyroid disorders is fatigue - most common reason to seek healthcare. • Women particularly affected by thyroid imbalance üWeight üFertility üPregnancy üMenopause üOsteoporosis
Thyroid Hormone Action • Activates nuclear receptors which regulate expression of thyroid hormone-responsive genes: ØFetus & neonate: differentiation of target tissues ØChildhood: differentiation/proliferation ØAdolescent: role in action of sex steroids
Thyroid Hormone Action • Gene expression (continued) All ages: • Regulates energy production • Regulates functional /structural proteins • Regulates action of other hormones - glucocorticoids, mineralocorticoids, growth factors, biologic amines (catecholamines)
Negative Feedback Loop • Thyroid hormone inhibits pituitary secretion of TSH • Hypothalamus plays crucial role • TSH very sensitive indication index of action • TSH & thyroid hormones maintained in a certain relationship • Modified by TBG (thyroxine-binding globulin)
Negative Feedback Loop Hyperthyroidism • Elevated serum thyroid level • Decreased TSH Hypothyroidism • Decreased serum thyroid levels • Increased TSH
Serum Levels of Thyroid Hormones • T 3 regulates peripheral action of hormone • T 3 & T 4 both released from gland • Peripheral conversion of T 4 to T 3 occurs in liver and target tissues • In presence of liver damage, T 3 conversion may be low despite good levels of T 4
TBG Metabolism • T 4 transported to tissue by TBG • High serum TBG (liver damage, pregnancy, OCP’s, HRT) lowers serum concentrations of free T 4 which decreases amount of substrate (T 4) that can be converted to T 3 • Indirect measure of TBG abnormality is T 3 uptake
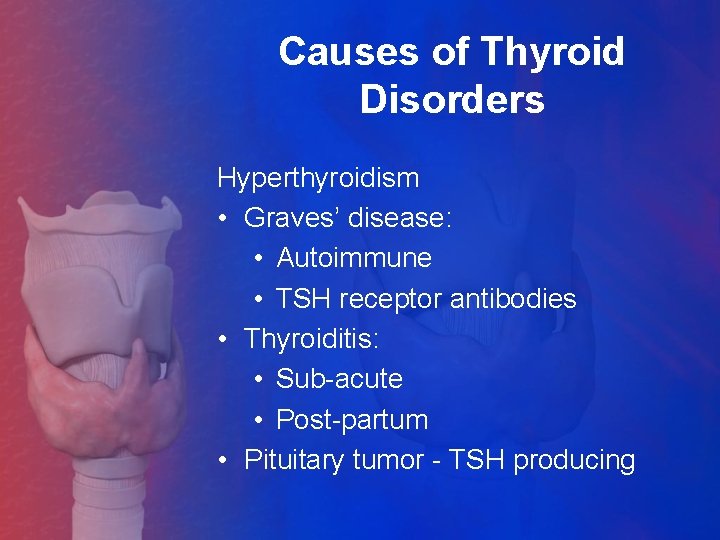
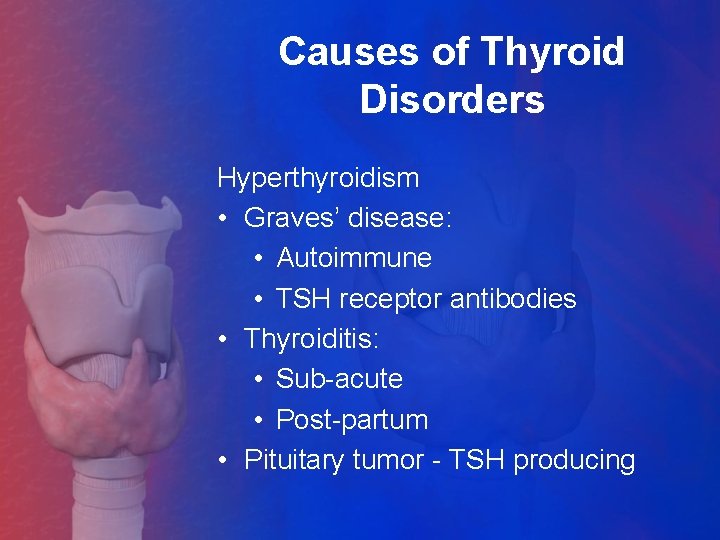
Causes of Thyroid Disorders Hyperthyroidism • Graves’ disease: • Autoimmune • TSH receptor antibodies • Thyroiditis: • Sub-acute • Post-partum • Pituitary tumor - TSH producing
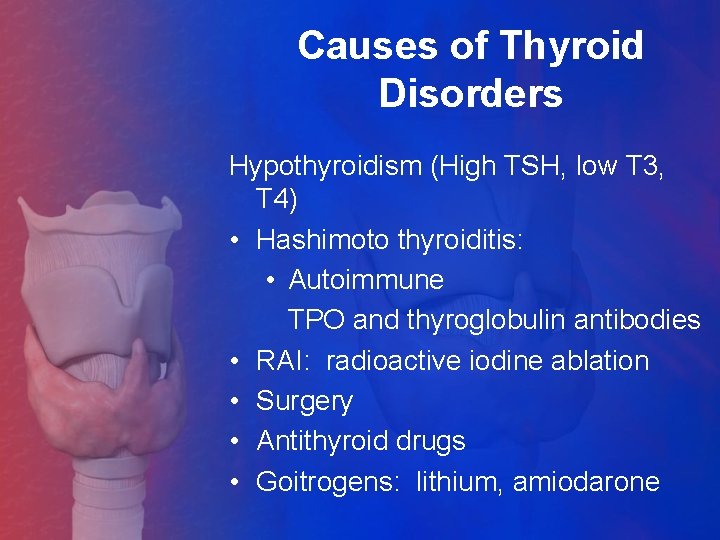
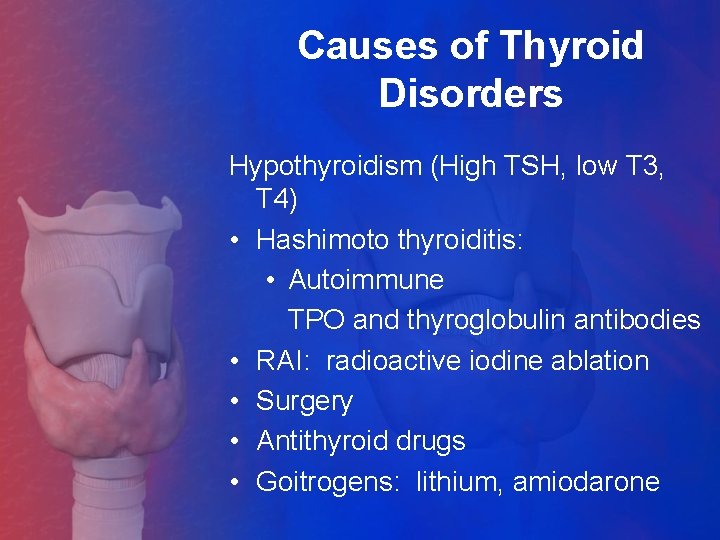
Causes of Thyroid Disorders Hypothyroidism (High TSH, low T 3, T 4) • Hashimoto thyroiditis: • Autoimmune TPO and thyroglobulin antibodies • RAI: radioactive iodine ablation • Surgery • Antithyroid drugs • Goitrogens: lithium, amiodarone
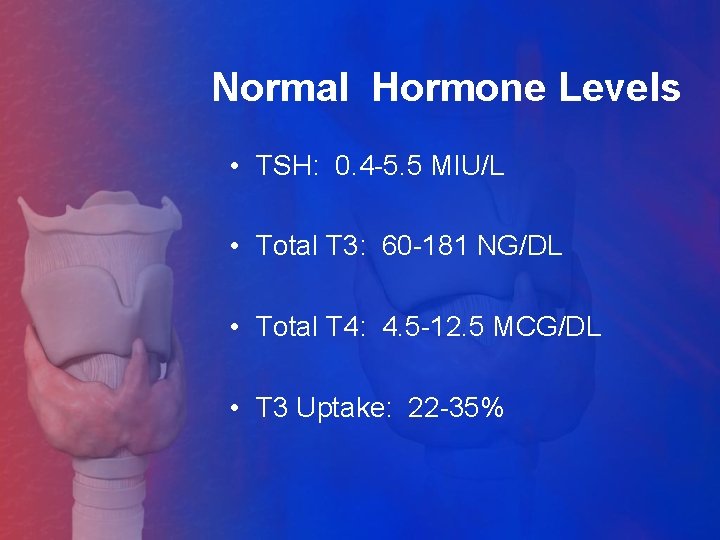
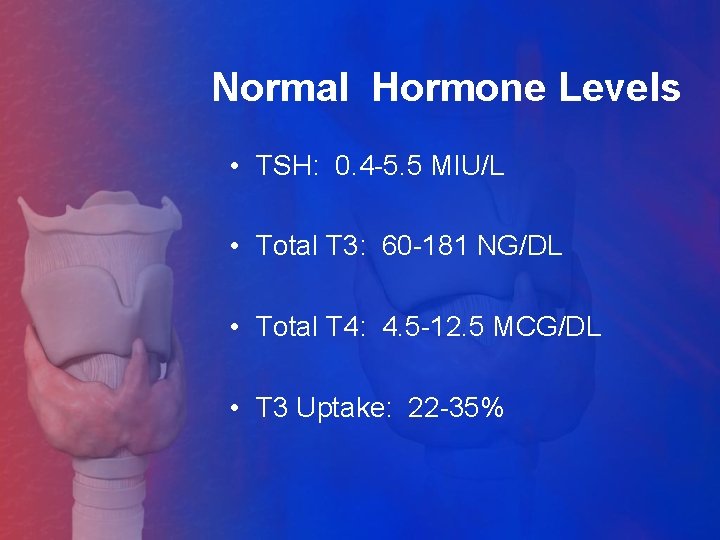
Normal Hormone Levels • TSH: 0. 4 -5. 5 MIU/L • Total T 3: 60 -181 NG/DL • Total T 4: 4. 5 -12. 5 MCG/DL • T 3 Uptake: 22 -35%
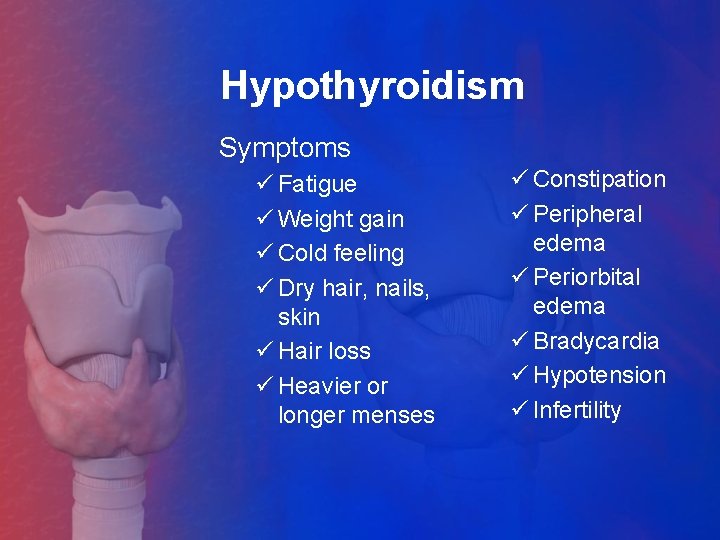
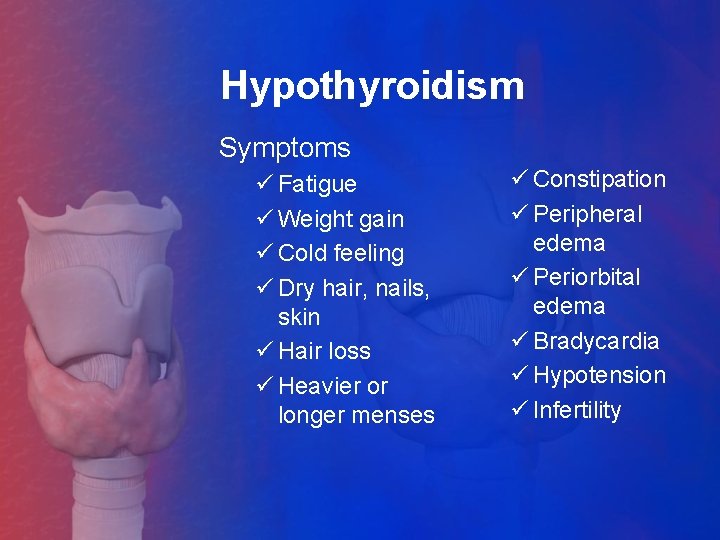
Hypothyroidism Symptoms ü Fatigue ü Weight gain ü Cold feeling ü Dry hair, nails, skin ü Hair loss ü Heavier or longer menses ü Constipation ü Peripheral edema ü Periorbital edema ü Bradycardia ü Hypotension ü Infertility
Hypothyroidism • Treatment: • Hormone replacement (L-T 4) üAbsorbed from small intestine ü 6 -day half-life • Daily dosing: 0. 025 -. 300 mgs • Branded preparations preferred to generic üSynthroid üLevoxyl üTirosint
Hypothyroidism • Treatment üInitial dose: ü 1. 7 mcg per kg üPregnant: may need 1. 8 mcg per kg üElderly: usually start at lower doses, esp. with angina or CAD • Monitoring ü 6 -8 weeks after any dose change üAnnually once stable üEach trimester in pregnancy
Hypothyroidism • Myxedema Coma üEnd stage of uncompensated hypothyroidism üPresents most often in elderly and women in winter months üPresent in respiratory failure, hypotension, bradyarrythmia, along with serious precipitating illness üTreatment is T 4 IV @ 1/10 th dose of oral üICU admit for multi-system failure
Hypothyroidism Pearls üMost patients reports feeling best with TSH between 1 -2 üIf TSH normal, but patient still not feeling good, think low T 3; may need Cytomel (oral T 3) üDepression very common üInadequate treatment can contribute to infertility üLook for recent onset of symptom with family history of thyroid disease
Hyperthyroidism Symptoms üAnxiety üPalpitations üUnintended weight loss üDecreased or absent menses üOily skin üFine, silky, oily-appearing hair üHeat intolerance üExopthalmos (not all cases) üTachycardia
Hyperthyroidism Treatment • Anti-thyroid drugs ü Methimazole Inhibits thyroid hormone synthesis in the thyroid gland ü PTU Inhibits thyroid hormone synthesis in the thyroid gland & inhibits peripheral conversion of T 4 to T 3
Hyperthyroidism Dosing: • Tapazole: 10 mg BID or TID • PTU: only 50 mg tablets available Usual starting dose: 2 tabs TID; may double dose if necessary • Both very effective at lowering thyroid hormone levels • TSH will stay suppressed several month
Hyperthyroidism Dosing: üMonitor every 4 -6 weeks üWhen TSH rises, may need to add T 4 (thyroid hormone) üWant to leave on ATD’s long enough to allow TSH receptor antibodies to decrease & induce remission; usually 12 -18 months üPlan to withdraw med at 12 -18 months to evaluate remission status
Hyperthyroidism Side effects of anti-thyroid drugs: • Leucocytopenia • Agranulocytosis-most serious • Pernicious anemia • Thrombocytopenia • Hepatic dysfunction • Allergy (discoid rashes) Evaluate with CMP, CBC, & thyroid hormone levels every 4 -6 months
Hyperthyroidism Radioactive Iodine Ablation • Administration of I 131 iodine by mouth • Used after TFT’s normal or if unable to control hyperthyroidism with drugs • Usually destroys gland over 3 -6 months
Hyperthyroidism Radioactive Iodine Ablation • Induces permanent hypothyroidism • May cause post-treatment thyroid storm (rare) • May cause aggravation of Graves’ eye disease • Pregnancy should be prevented within 6 months after treatment
Hyperthyroidism Surgery • When disease state or gland size can’t be controlled with drugs • When gland causing obstructive signs üDifficulty breathing either supine or upright -Evaluated by PA & LAT CXR üDifficulty swallowing food -Evaluated by barium swallow
Hyperthyroidism • Thyroid Storm • Most often with Graves’ disease • Levels same as with Graves’ • Cardinal signs: Temperature 102 to 1050 Profuse sweating Marked tachycardia (120 -140 pulse rate or higher) Atrial fibrillation • Usually induced by concurrent infection or surgery on hyperactive gland
Hyperthyroidism Thyroid storm • Treatment üPTU orally or by NG tube üTapazole not favored because it does not inhibit peripheral conversion of T 4 to T 3 üBeta blockade, PO or IV üSupportive therapy for fever, dehydration üPerhaps iodine solution or corticosteroids
Hyperthyroidism Graves’ Eye Disease: • Caused by antibody effect on orbital tissue • Symptoms include: üEdema üInflammation üHypertrophy of extra ocular muscles & orbital fat • Exopthalmos upper & lower lid retraction, strabismus, herniated orbital fat
Hyperthyroidism Graves’ Eye Disease: • Should be stabilized for 6 months prior to any other treatment modality • Exception is optic neuropathy caused by strangulation of optic nerve • Extent of protrusion measured by increase in distance between lateral orbital rim and anterior aspect of eye
Thyroid Nodules • May be a single nodule or larger of multiple nodules • 95% benign • More common in women • More likely malignant in men • Increase in size while on T 4 therapy worrisome for malignancy
Thyroid Nodules • Note size, consistency and mobility on physical exam • Evaluate for tracheal deviation or esophageal obstruction • Usually TSH suppressed, T 3 and T 4 levels normal • Antibodies may be present, but more likely they are not • Ultrasound best way to diagnose
Thyroid Nodules Treatment • Multinodular gland without dominant nodule: T 4 to shrink if TSH not suppressed • Single nodule 1 cm or greater: fine needle aspiration biopsy • Enlarging nodule despite “good” dose of T 4 or indeterminate or malignant result from FNA indicates need for surgery
Thyroiditis • Most common cause: chronic autoimmune thyroiditis or postpartum thyroiditis • Next is sub acute thyroiditis • More rare: acute suppurative thyroiditis
Thyroiditis Post-partum thyroiditis • May occur anytime in the first year, but most common in first 3 months • Usually have hyperthyroid symptoms first, followed by hypothyroid findings • Gland usually enlarged • Will not have other markers for inflammation: fever, tenderness, high sed rate
Thyroiditis Post-partum thyroiditis • Usually spontaneously resolve • May need temporary medication support for symptoms üBeta blockers for tachycardia üTranquilizers for anxiety üT 4 for hypothyroidism • Can progress to permanent hypothyroidism
Thyroiditis Sub acute • Usually follows viral illness • Gland is swollen, tender • Sed rate elevated >50 mm/hour • May have fever, even fairly mild • Leucocytosis • Follows usual pattern of transient hyperthyroidism, then hypothyroidism, then euthyroid
Thyroiditis Sub acute • Treatment: üSymptomatic üNSAIDS for pain, fever üPrednisone for severe pain unrelieved by above üBeta blockers for hyper phase üThyroid replacement for hypo phase üResolve spontaneously

Questions?

Thank you!