Three Lines of Defense Barriers at body surfaces

Three Lines of Defense • Barriers at body surfaces • Nonspecific responses • Immune responses
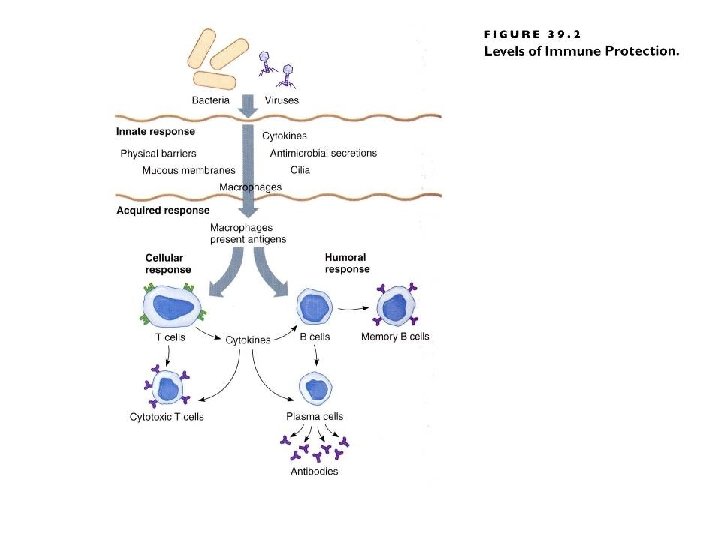
Barriers at Body Surface • Intact skin and mucous membranes • Lysozyme分解酶 • Normal bacterial flora • Flushing effect and low p. H of urine
Nonspecific Responses • Lymph nodes trap and kill pathogens • Natural killer cells attack a range of targets • Inflammation發炎
Acute Inflammation發炎反應 • Nonspecific response to foreign invasion, tissue damage, or both • Destroys invaders, removes debris, and prepares area for healing • Characterized by redness紅, swelling腫, warmth熱, and pain痛
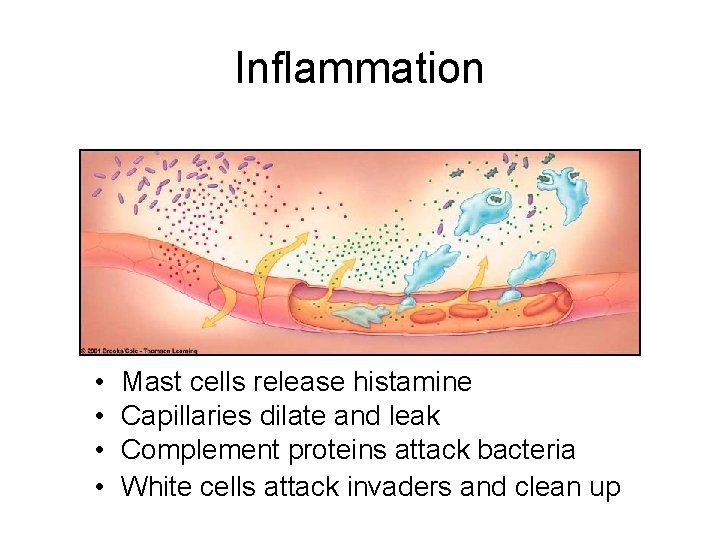
Inflammation • • Mast cells release histamine Capillaries dilate and leak Complement proteins attack bacteria White cells attack invaders and clean up
Features of Immune System • Immunological specificity(專一性) – B and T cells zero in (瞄準)on certain kinds of pathogens; response is pathogen specific • Immunological memory(記憶性) – Immune system recognizes and reacts swiftly to a pathogen it has “seen”
Key Component of Immune Response • • MHC markers(分子標記) Antigen-presenting cells Helper T cells(幫助型T細胞) Effector cytoxic T cells(細胞 殺手) • Natural killer cells(自然殺手) • B cells
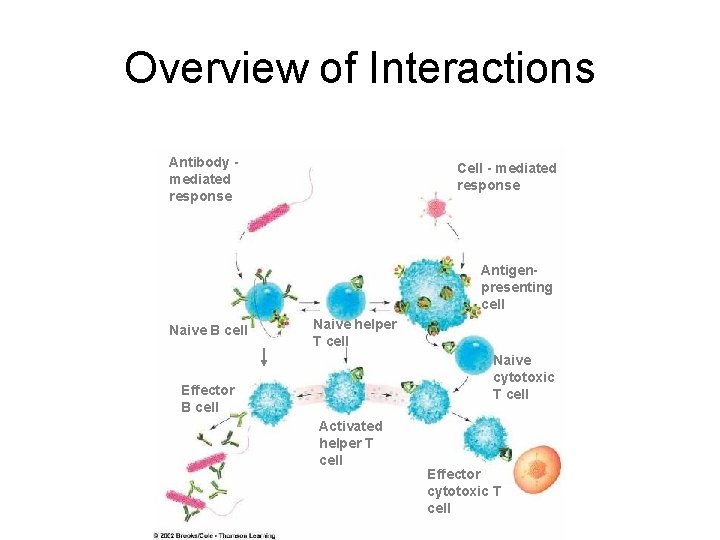
Overview of Interactions Antibody mediated response Cell - mediated response Antigenpresenting cell Naive B cell Naive helper T cell Naive cytotoxic T cell Effector B cell Activated helper T cell Effector cytotoxic T cell
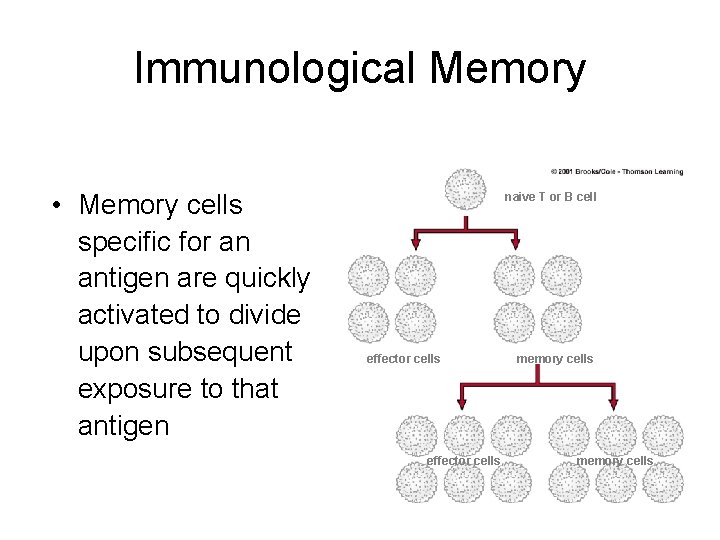
Immunological Memory • Memory cells specific for an antigen are quickly activated to divide upon subsequent exposure to that antigen naive T or B cell effector cells memory cells
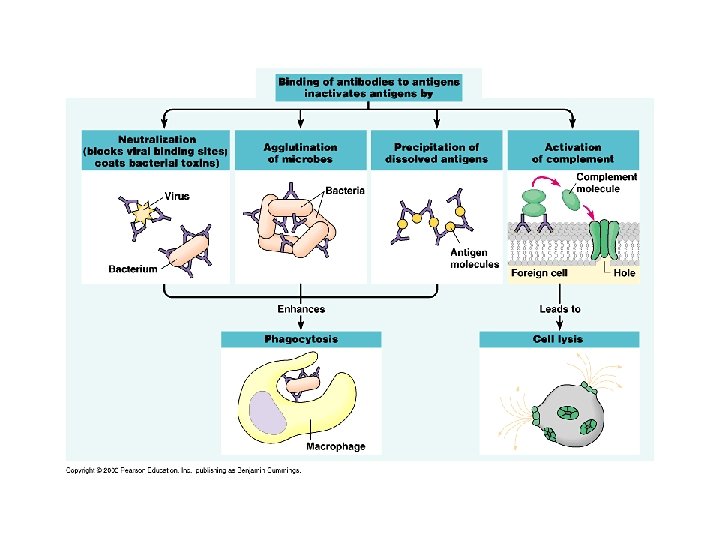
Antibody-Mediated Response 抗體免疫反應 • Carried out by B cells • Targets are intracellular pathogens and toxins • Antibodies bind to target and mark it for destruction by phagocytes吞食 and complement補體
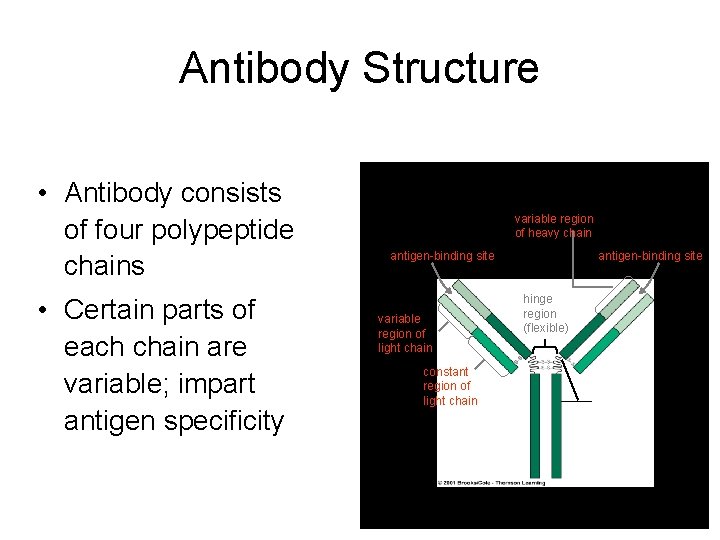
Antibody Structure • Antibody consists of four polypeptide chains • Certain parts of each chain are variable; impart antigen specificity variable region of heavy chain antigen-binding site variable region of light chain constant region of light chain antigen-binding site hinge region (flexible)
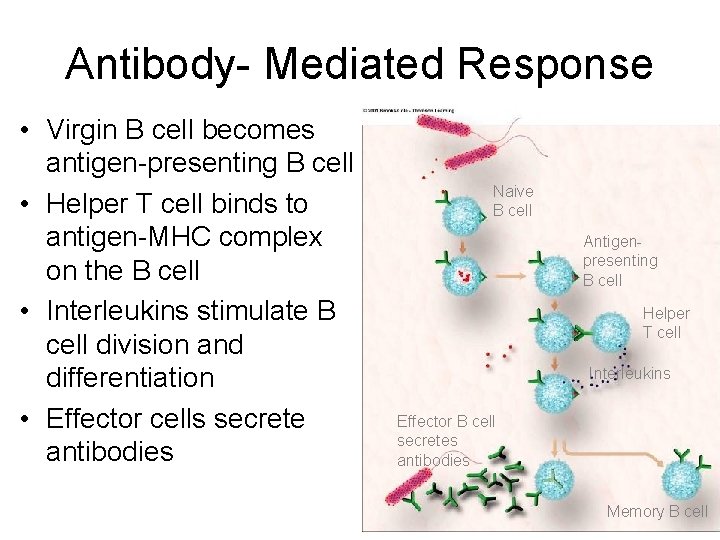
Antibody- Mediated Response • Virgin B cell becomes antigen-presenting B cell • Helper T cell binds to antigen-MHC complex on the B cell • Interleukins stimulate B cell division and differentiation • Effector cells secrete antibodies Naive B cell Antigenpresenting B cell Helper T cell Interleukins Effector B cell secretes antibodies Memory B cell
5 Classes of Immunoglobulins • Ig. M are secreted first; trigger complement reactions, agglutination • Ig. D function is not understood • Ig. G activates complement; can cross placenta • Ig. A associates with mucus-coated surfaces • Ig. E triggers inflammation
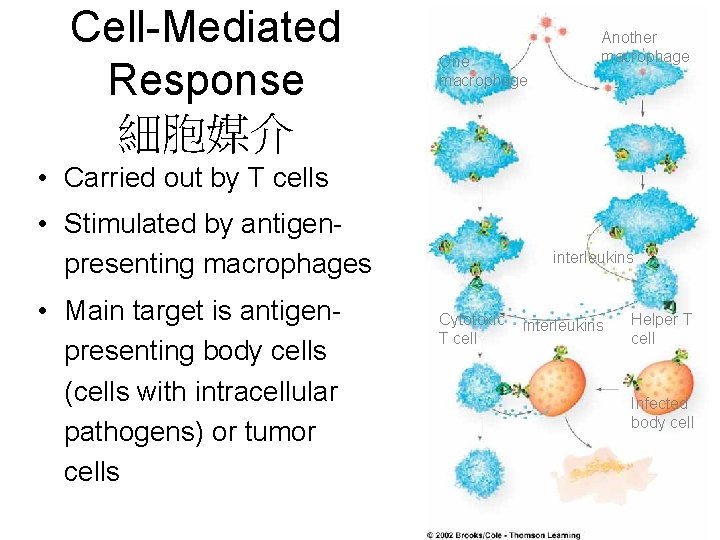
Cell-Mediated Response 細胞媒介 One macrophage Another macrophage • Carried out by T cells • Stimulated by antigenpresenting macrophages • Main target is antigenpresenting body cells (cells with intracellular pathogens) or tumor cells interleukins Cytotoxic T cell interleukins Helper T cell Infected body cell
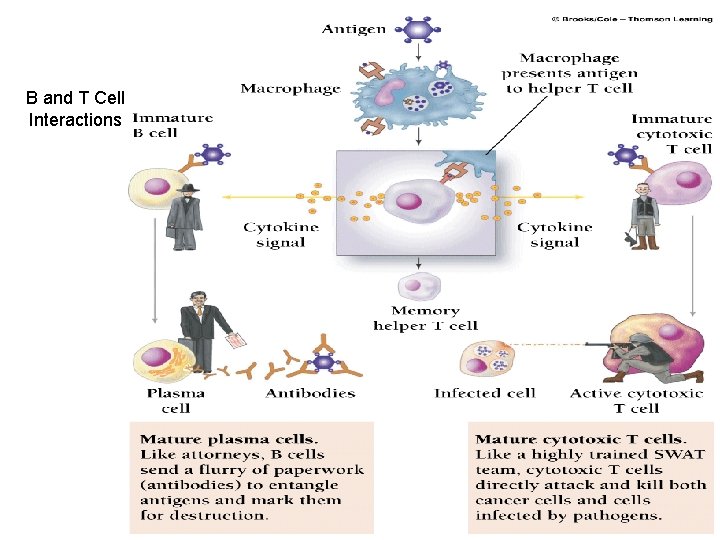
B and T Cell Interactions
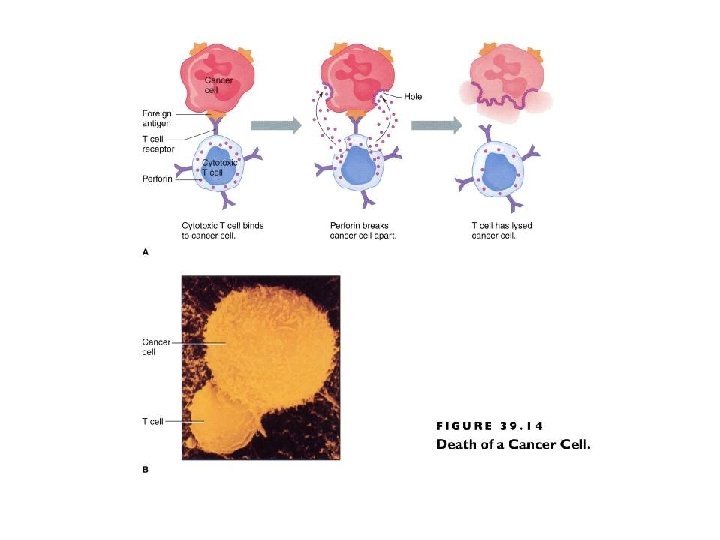
Types of T Cells • Helper T (TH) cells release cytokines to stimulate B cells to make antibodies and present antigens • Cytotoxic T cells (Tc) kill cells by poking holes in membrane or triggering cell suicide (apoptosis)
Dr. Carlo Urbani • Doctors Without Borders working in Hanoi, Vietnam • The first people alters WHO about the dangers of the SARS (severe acute respiratory syndrome; atypical pneumonia) epidemic • 10% mortality
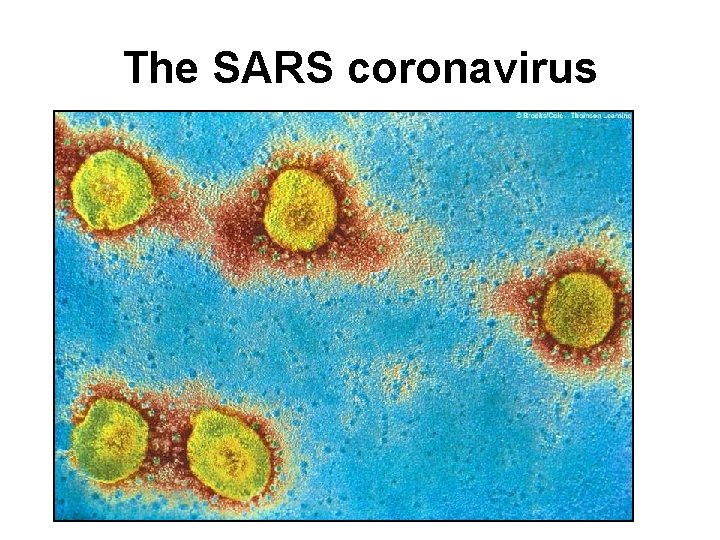
The SARS coronavirus
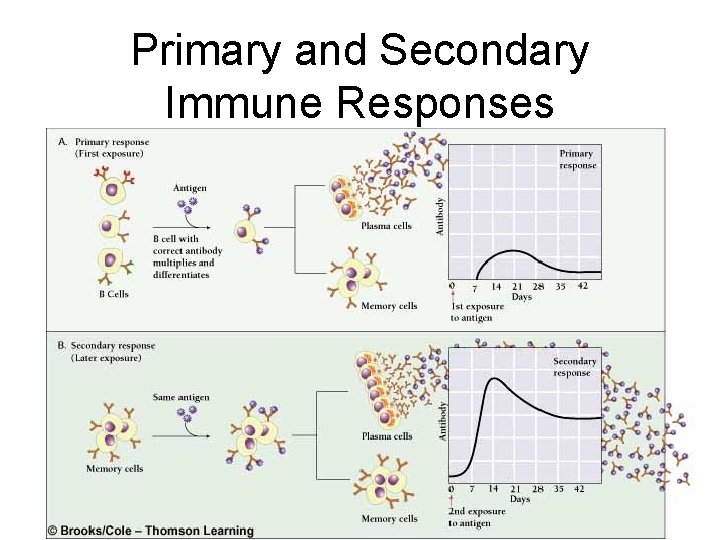
Primary and Secondary Immune Responses
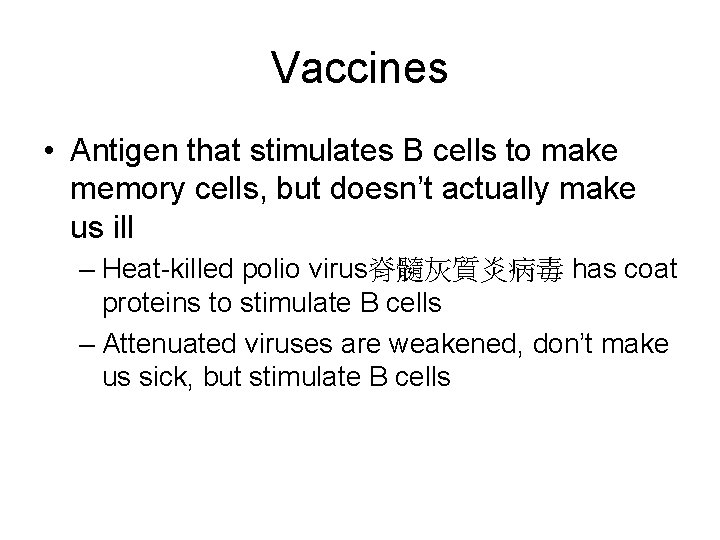
Vaccines • Antigen that stimulates B cells to make memory cells, but doesn’t actually make us ill – Heat-killed polio virus脊髓灰質炎病毒 has coat proteins to stimulate B cells – Attenuated viruses are weakened, don’t make us sick, but stimulate B cells
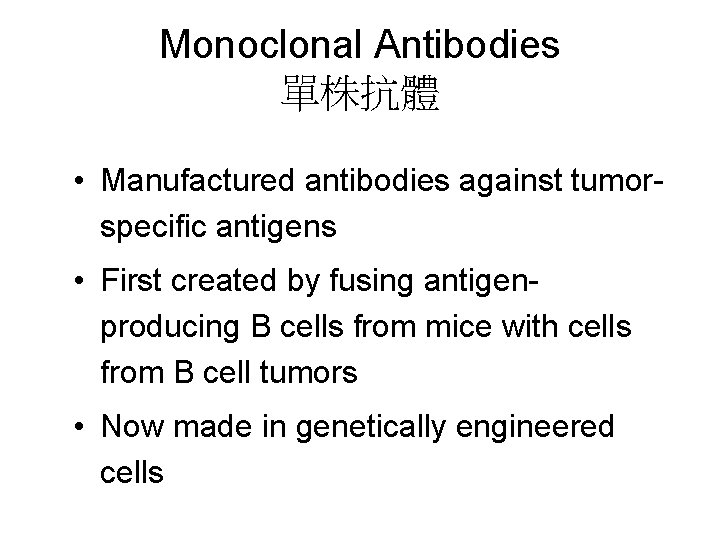
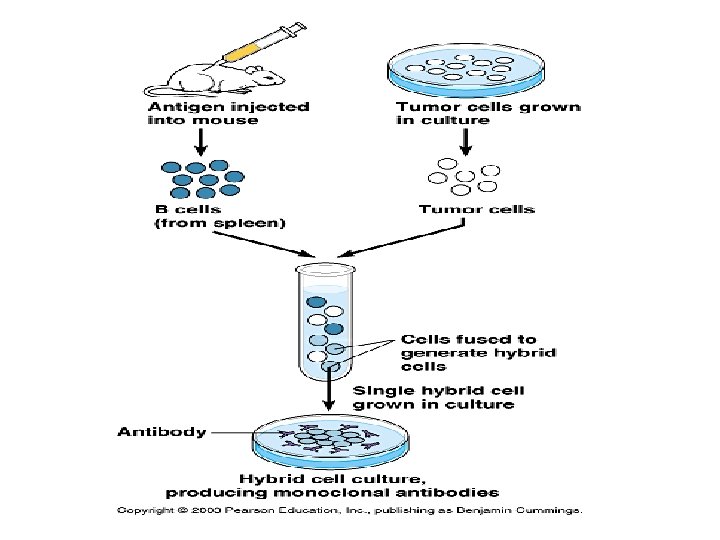
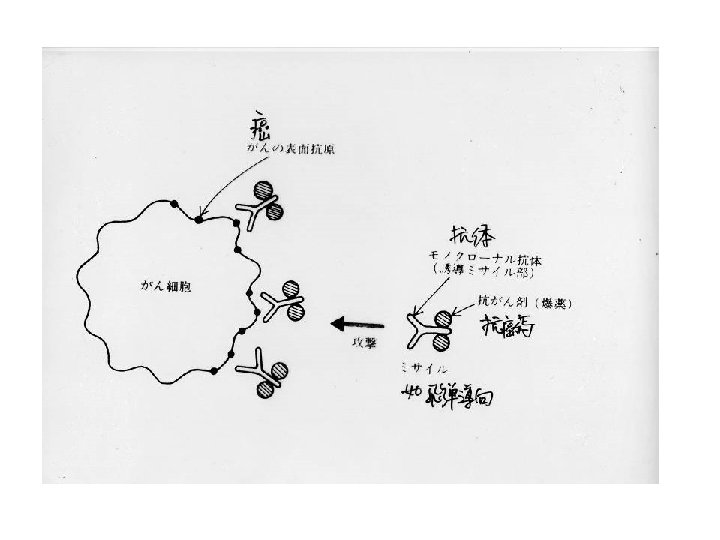
Monoclonal Antibodies 單株抗體 • Manufactured antibodies against tumorspecific antigens • First created by fusing antigenproducing B cells from mice with cells from B cell tumors • Now made in genetically engineered cells
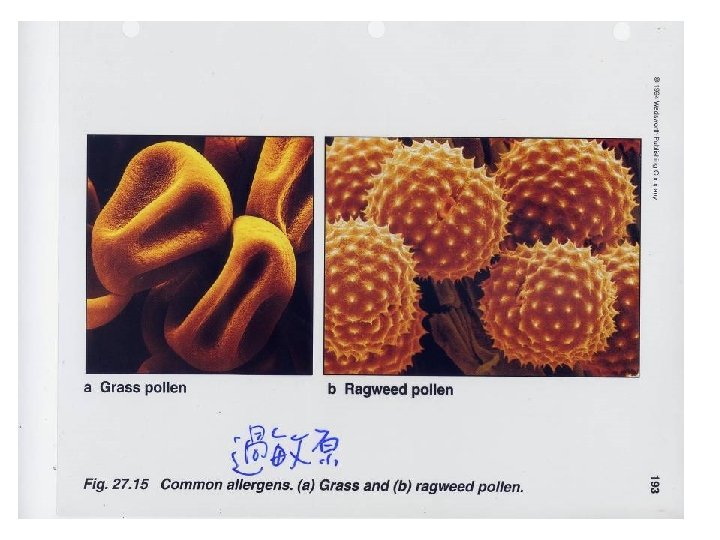
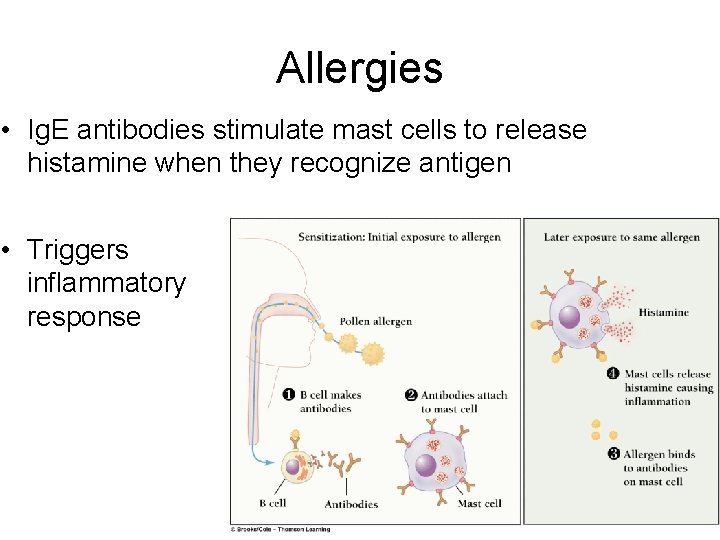
Allergies • Ig. E antibodies stimulate mast cells to release histamine when they recognize antigen • Triggers inflammatory response
Autoimmune Disorders 1. Immune system makes antibodies against self antigens 2. Grave’s disease 甲狀腺素過 多 • Myasthenia gravis 肌肉無力 • Rheumatoid arthritis 類風濕 性關節炎
AIDS • Combination of disorders that follows infection with HIV • Includes – Yeast (Candida) infections – Pneumocystis pneumonia – Karposi’s sarcoma
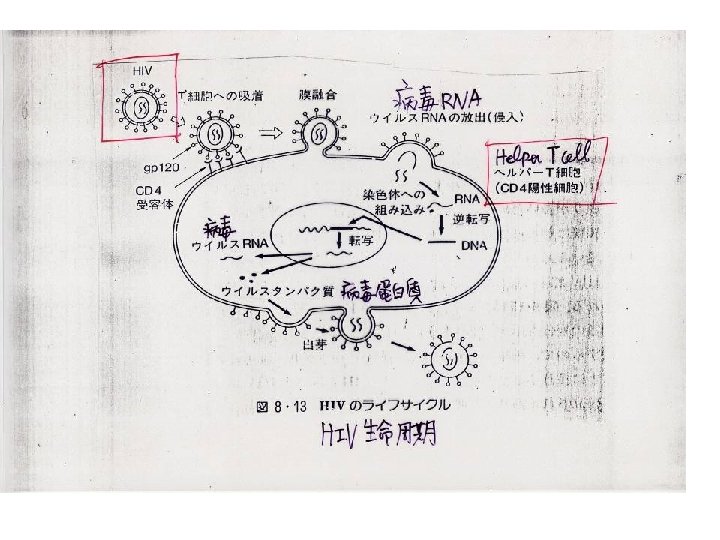
HIV Replication (1) • RNA retrovirus • A protein (gp 120) at virus surface binds to host cells with CD 4 receptors • These receptors occur on helper T cells • Once bound, RNA and viral enzymes enter the host cell
HIV Replication (2) • Viral RNA is reverse transcribed to DNA • HIV DNA is called provirus; it inserts into host DNA • The host cell makes copies of viral DNA and viral proteins that assemble to form new virus particles
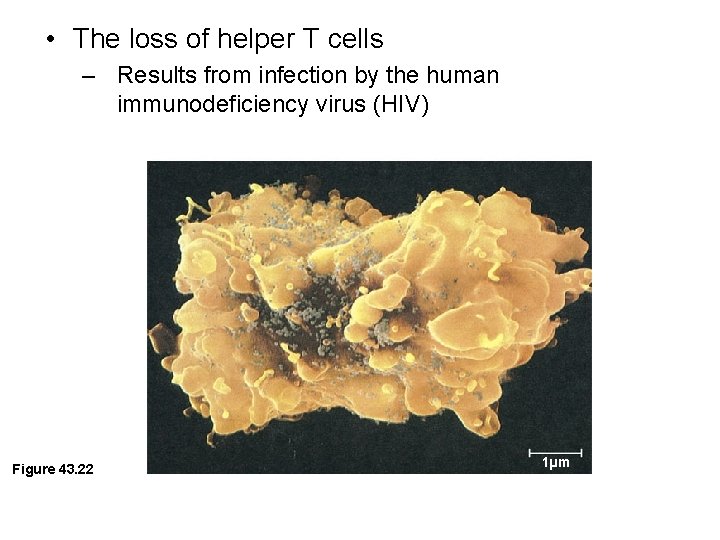
• The loss of helper T cells – Results from infection by the human immunodeficiency virus (HIV) Figure 43. 22 1µm
T Cell Decline • Release of new viral particles kills the host T cell • The body is constantly making new T cells, but cannot outpace the rate of destruction • As infection proceeds, T cell numbers inevitably decline
Effect of T Cell Decline • CD 4 helper T cells play a vital role in immune function • They are required for both cell-mediated antibody-mediated immunity • Infected individual becomes vulnerable to other infections, which eventually result in death
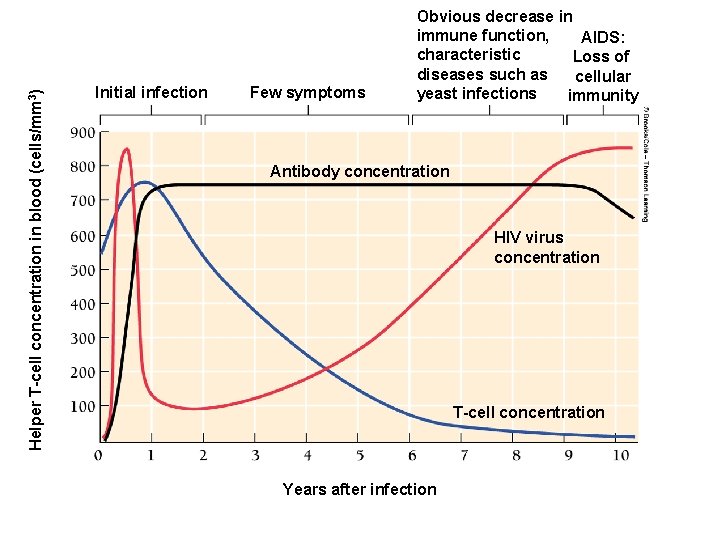
Helper T-cell concentration in blood (cells/mm 3) Initial infection Few symptoms Obvious decrease in immune function, AIDS: characteristic Loss of diseases such as cellular yeast infections immunity Antibody concentration HIV virus concentration T-cell concentration Years after infection
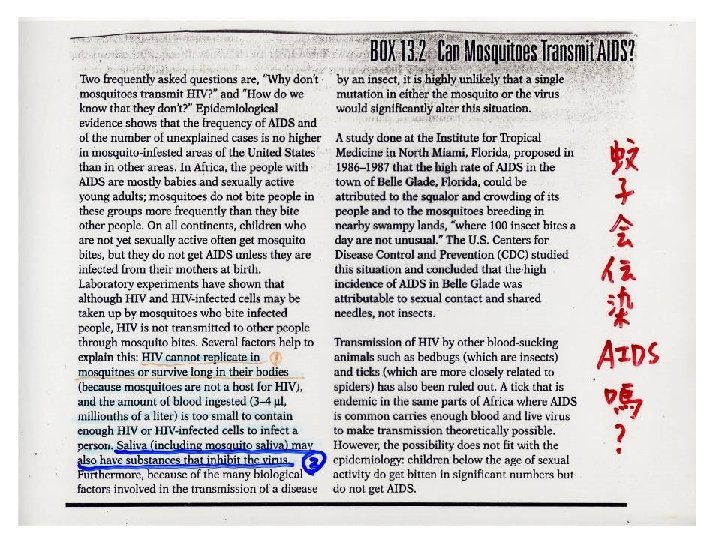
Transmission of HIV • HIV does not live long outside human body • Most often spread by exchange of bodily fluids with an infected person • In the U. S. , anal intercourse and needle sharing are main modes of transmission
Transmission of HIV • Less commonly transmitted by vaginal intercourse and oral sex • Can travel from mothers to offspring during pregnancy, birth, or breast-feeding • Not known to be transmitted by food, air, water, casual contact, or insect bites
Treatment • No cure • Once HIV genes are incorporated, no way to get them out • AZT, and other drugs slow the course of the disease and increase life span • Researchers continue to develop drugs and to work toward an AIDS vaccine
- Slides: 55