This Eye Does Not Look Right An Imaging

- Slides: 36
This Eye Does Not Look Right. An Imaging Overview of Common Oculoplastic and Orbital Surgeries. e. Ed. E-109 Farbod Nasseri S. Ali Nabavizadeh PENN RADIOLOGY THE ROOTS OF RADIOLOGICAL Laurie A. Loevner Arastoo Vossough Suyash Mohan EXCELLENCE Neuroradiology Division Department of Radiology University of Pennsylvania
Disclosure statement • Neither the authors nor their immediate family members have a financial relationship with a commercial organization that may have a direct or indirect interest in the content. Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Penn Radiology
Purpose • To present a comprehensive and systematic review of the imaging spectrum of the oculoplastic and orbital surgeries including various types of orbital implants and prostheses. • To review imaging features of potential surgical complications and discuss plausible pitfalls. Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Penn Radiology
Approach • Orbital surgeries Ø Reconstruction, augmentation, decompression Ø Enucleation, evisceration, exenteration • Lacrimal apparatus surgery • Lens surgery & implants • Eyelid surgery • Strabismus surgery • Glaucoma surgery • Retinopexy & scleral buckles • Intraocular injection Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Penn Radiology
Discussion • The development of new surgical techniques, as well as advances in the prostheses offer a wide range of novel alternatives for orbital and oculoplastic surgeries. • Imaging plays a critical role in the postoperative setting, enabling early diagnosis of complications as well as long term follow-up evaluation. • A comprehensive pictorial review of postoperative orbit will be presented. Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Penn Radiology
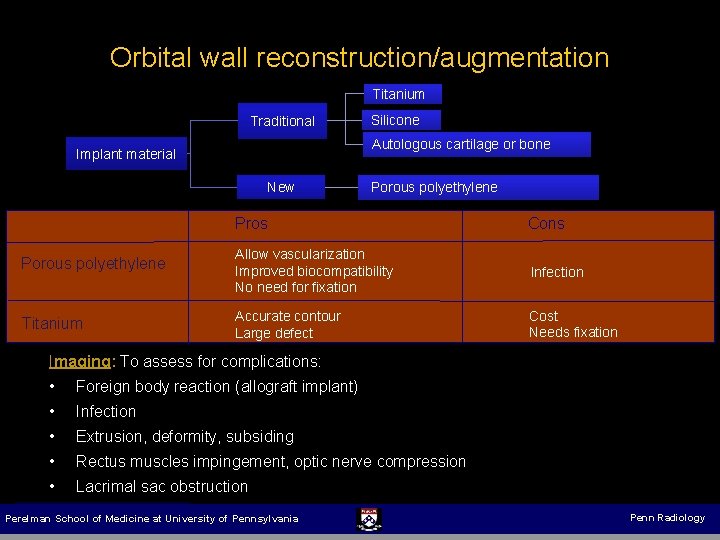
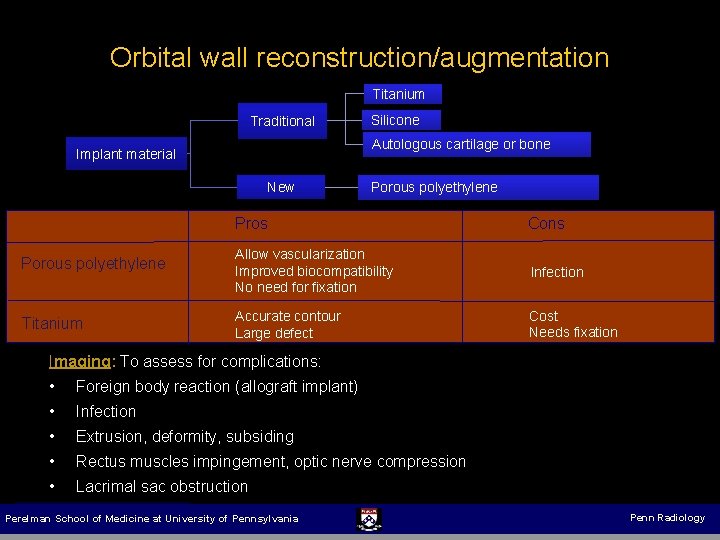
Orbital wall reconstruction/augmentation Titanium Traditional Silicone Autologous cartilage or bone Implant material New Porous polyethylene Pros Porous polyethylene Titanium Cons Allow vascularization Improved biocompatibility No need for fixation Infection Accurate contour Large defect Cost Needs fixation Imaging: To assess for complications: • • Foreign body reaction (allograft implant) • • Extrusion, deformity, subsiding • Lacrimal sac obstruction Infection Rectus muscles impingement, optic nerve compression Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Penn Radiology
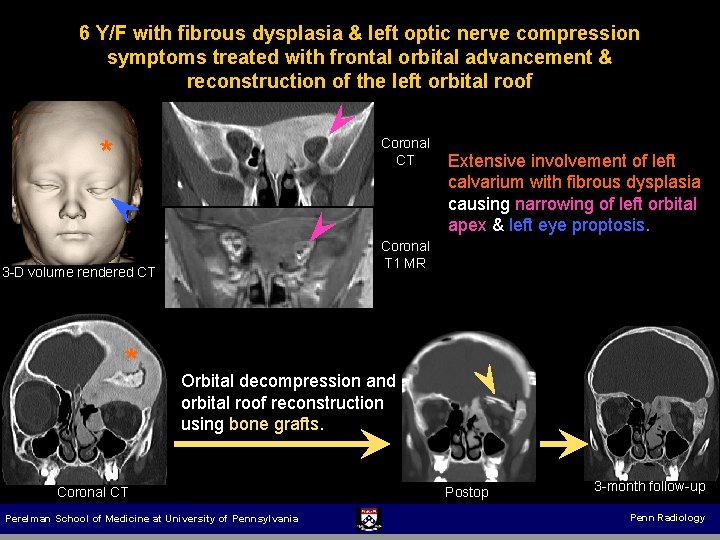
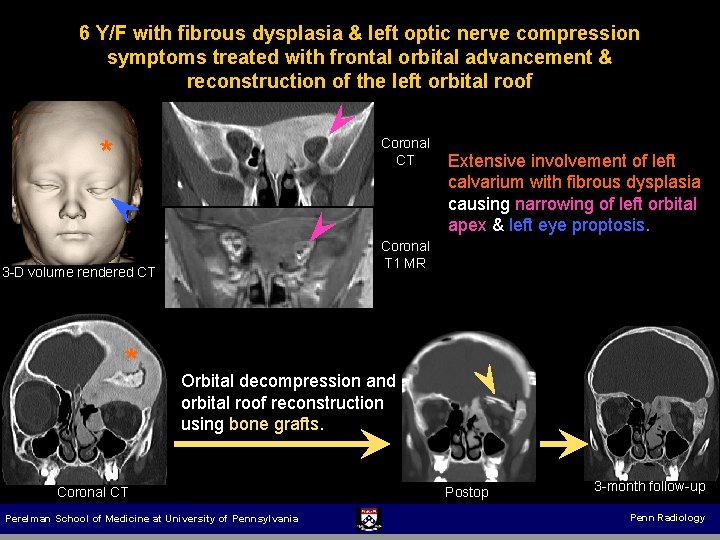
6 Y/F with fibrous dysplasia & left optic nerve compression symptoms treated with frontal orbital advancement & reconstruction of the left orbital roof * Coronal CT Coronal T 1 MR 3 -D volume rendered CT * Extensive involvement of left calvarium with fibrous dysplasia causing narrowing of left orbital apex & left eye proptosis. Orbital decompression and orbital roof reconstruction using bone grafts. Coronal CT Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Postop 3 -month follow-up Penn Radiology
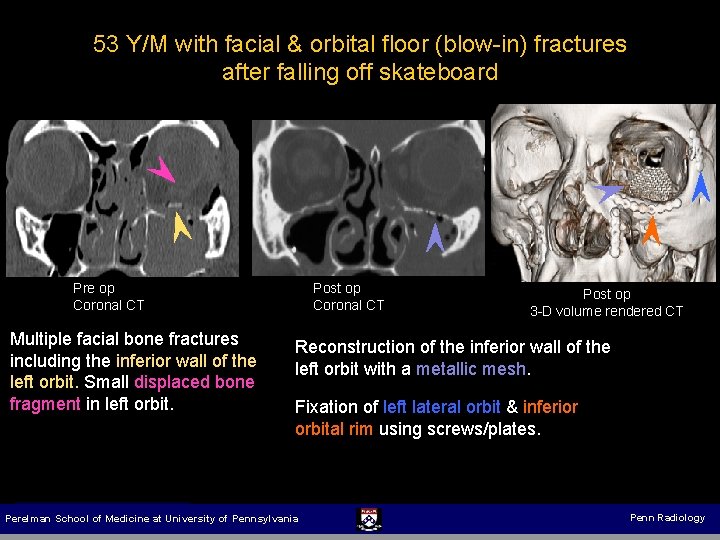
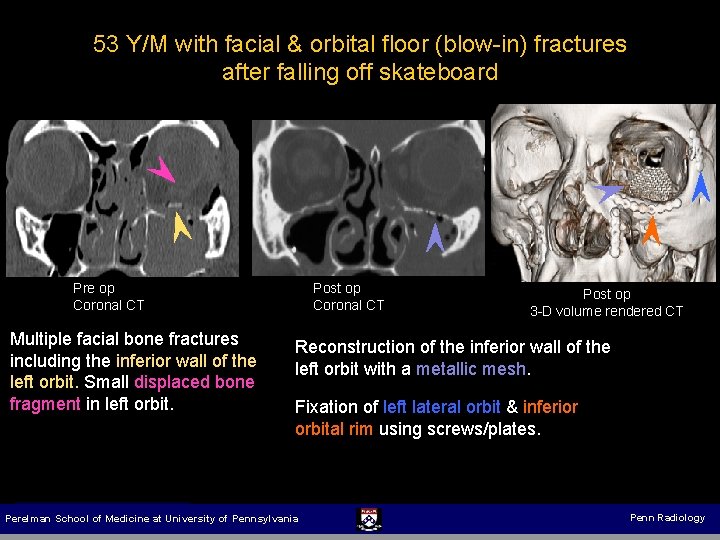
53 Y/M with facial & orbital floor (blow-in) fractures after falling off skateboard Pre op Coronal CT Multiple facial bone fractures including the inferior wall of the left orbit. Small displaced bone fragment in left orbit. Post op Coronal CT Post op 3 -D volume rendered CT Reconstruction of the inferior wall of the left orbit with a metallic mesh. Fixation of left lateral orbit & inferior orbital rim using screws/plates. Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Penn Radiology
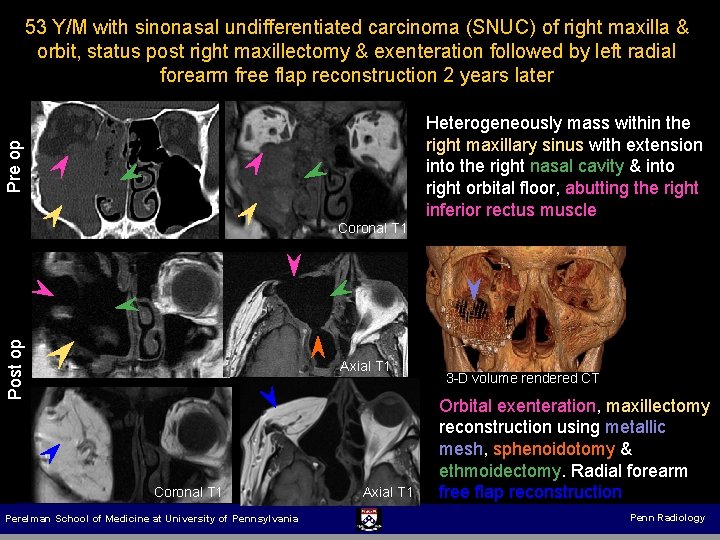
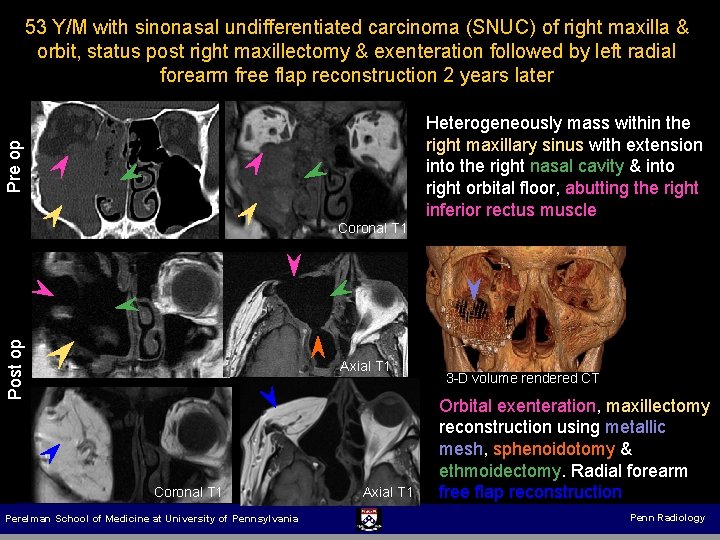
53 Y/M with sinonasal undifferentiated carcinoma (SNUC) of right maxilla & orbit, status post right maxillectomy & exenteration followed by left radial forearm free flap reconstruction 2 years later Pre op Heterogeneously mass within the right maxillary sinus with extension into the right nasal cavity & into right orbital floor, abutting the right inferior rectus muscle Post op Coronal T 1 Axial T 1 Coronal T 1 Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Post op Coronal T 1 Axial T 1 3 -D volume rendered CT Orbital exenteration, maxillectomy reconstruction using metallic mesh, sphenoidotomy & ethmoidectomy. Radial forearm free flap reconstruction Penn Radiology
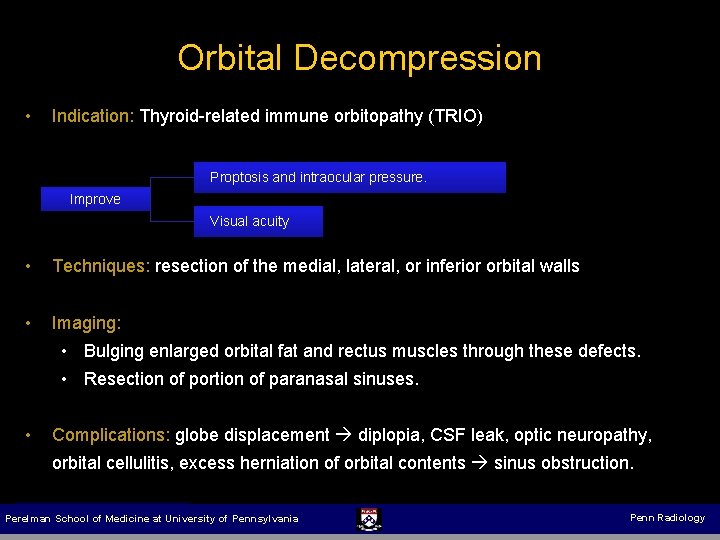
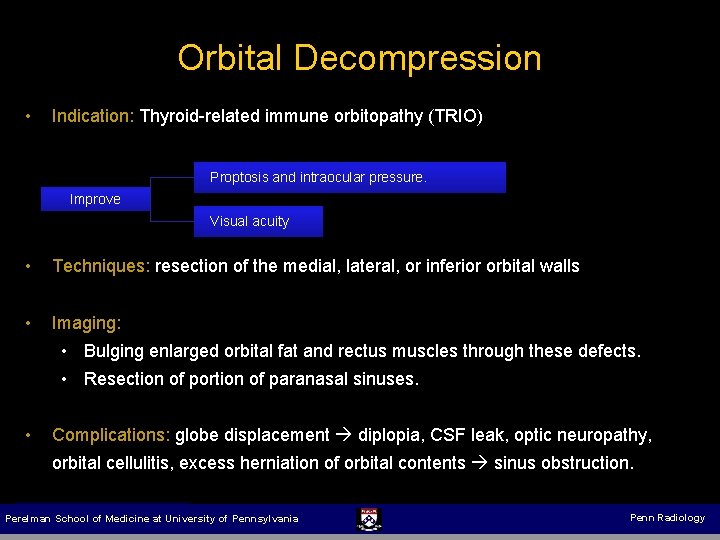
Orbital Decompression • Indication: Thyroid-related immune orbitopathy (TRIO) Proptosis and intraocular pressure. Improve Visual acuity • Techniques: resection of the medial, lateral, or inferior orbital walls • Imaging: • Bulging enlarged orbital fat and rectus muscles through these defects. • Resection of portion of paranasal sinuses. • Complications: globe displacement diplopia, CSF leak, optic neuropathy, orbital cellulitis, excess herniation of orbital contents sinus obstruction. Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Penn Radiology
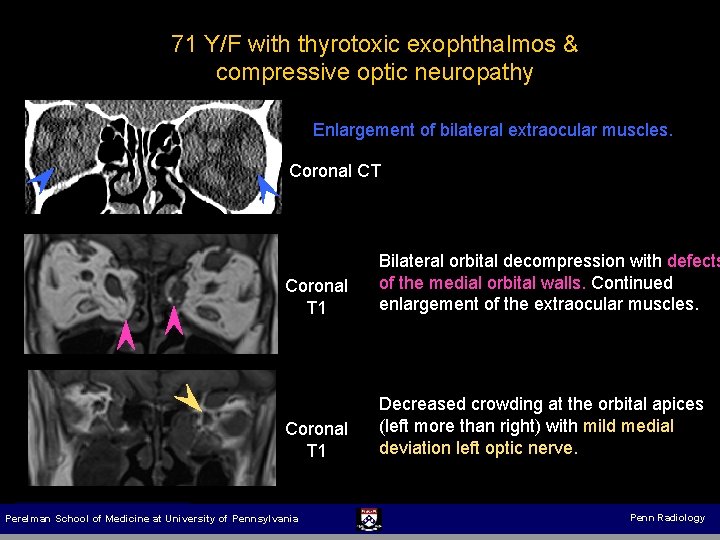
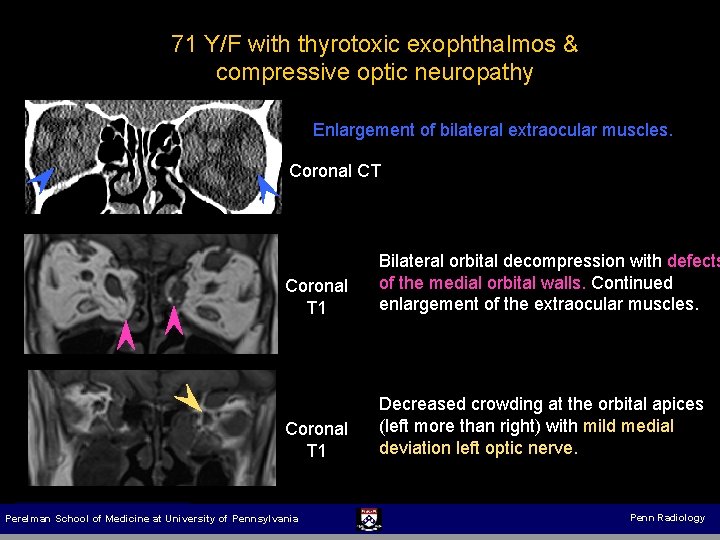
71 Y/F with thyrotoxic exophthalmos & compressive optic neuropathy Enlargement of bilateral extraocular muscles. Coronal CT Coronal T 1 Bilateral orbital decompression with defects of the medial orbital walls. Continued enlargement of the extraocular muscles. Coronal T 1 Decreased crowding at the orbital apices (left more than right) with mild medial deviation left optic nerve. Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Penn Radiology

Orbital Enucleation / Evisceration: removal of globe contents, preserving the sclera & extraocular muscles. Enucleation: removal of globe contents entirely, preserving the extraocular muscles. Intraocular malignancies Indication Irreparable globe rupture Prevention of sympathetic ophthalmia Globe implants: provide orbital volume for cosmesis following enucleation. Cover shell / eye prosthesis (anterior) Implant Components Orbital implant (posterior) Materials: metallic (old), hydroxyapatite, solid silicone, & Medpor (new). www. oasa. org. za Pitfall: Diffuse linear enhancement surrounding the implant (no clinical significance). Complications: rotation, infection, inflammation, & exposure. Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Penn Radiology
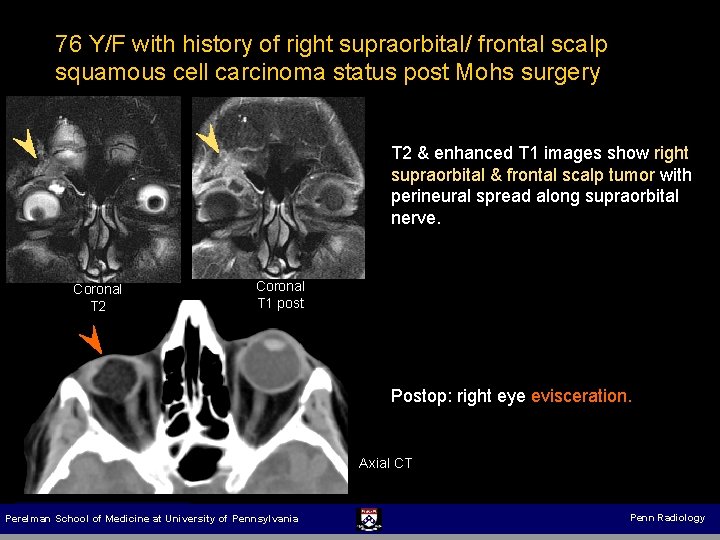
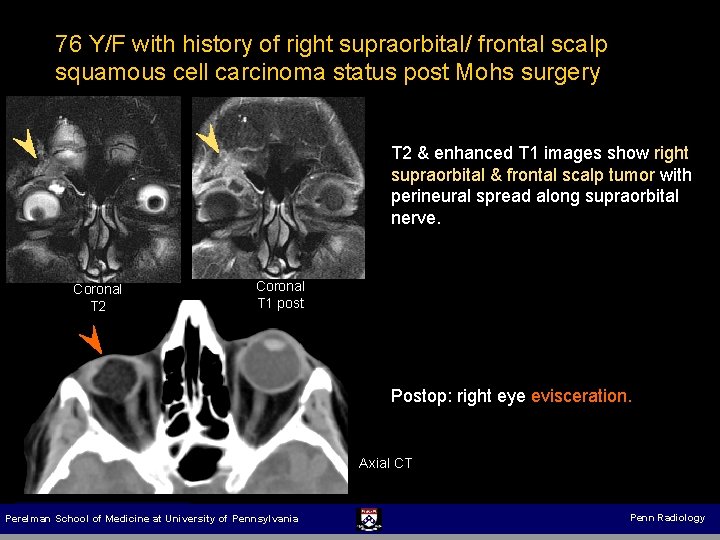
76 Y/F with history of right supraorbital/ frontal scalp squamous cell carcinoma status post Mohs surgery T 2 & enhanced T 1 images show right supraorbital & frontal scalp tumor with perineural spread along supraorbital nerve. Coronal T 2 Coronal T 1 post Postop: right eye evisceration. Axial CT Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Penn Radiology
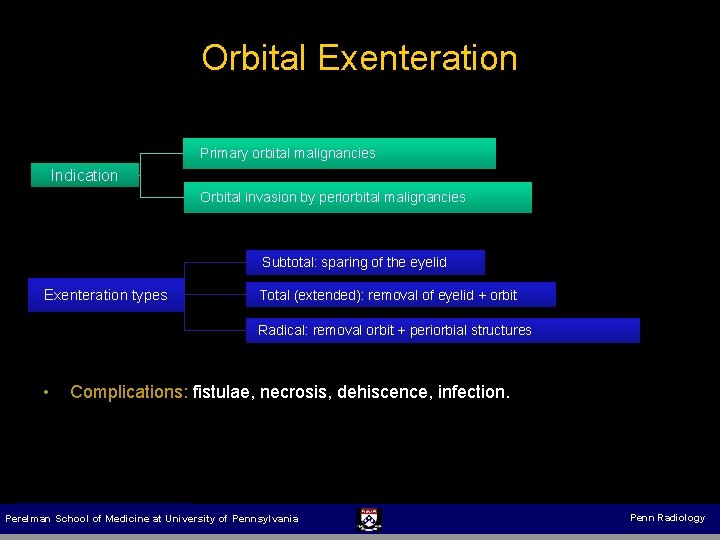
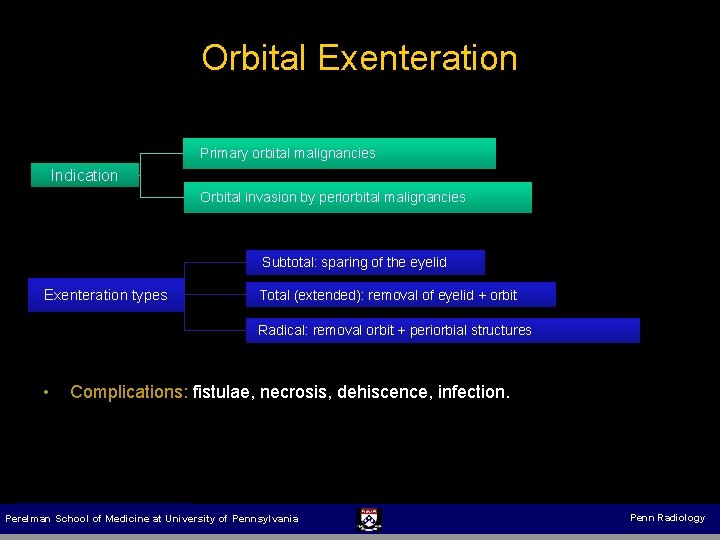
Orbital Exenteration Primary orbital malignancies Indication Orbital invasion by periorbital malignancies Subtotal: sparing of the eyelid Exenteration types Total (extended): removal of eyelid + orbit Radical: removal orbit + periorbial structures • Complications: fistulae, necrosis, dehiscence, infection. Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Penn Radiology
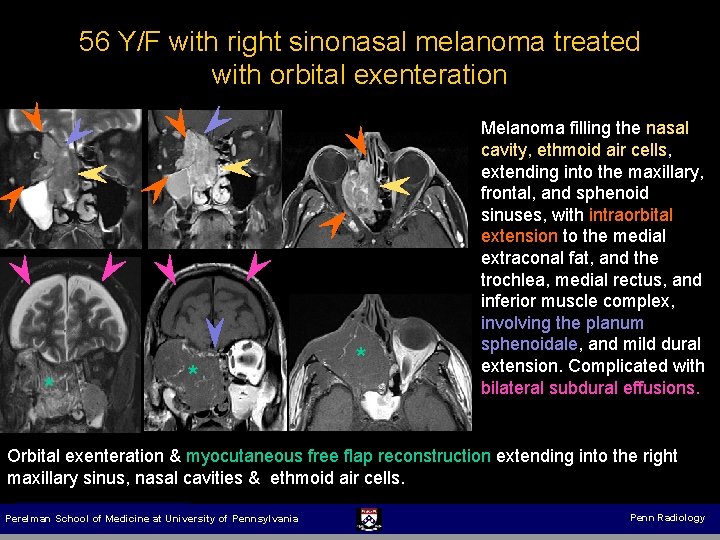
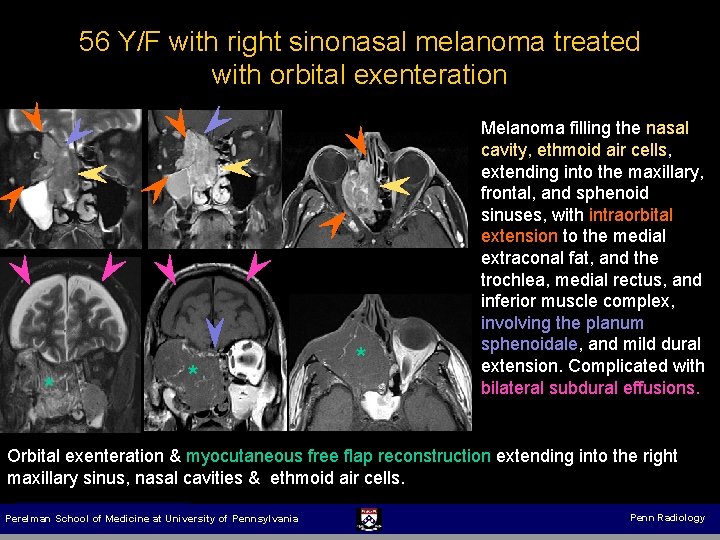
56 Y/F with right sinonasal melanoma treated with orbital exenteration * * * Melanoma filling the nasal cavity, ethmoid air cells, extending into the maxillary, frontal, and sphenoid sinuses, with intraorbital extension to the medial extraconal fat, and the trochlea, medial rectus, and inferior muscle complex, involving the planum sphenoidale, and mild dural extension. Complicated with bilateral subdural effusions. Orbital exenteration & myocutaneous free flap reconstruction extending into the right maxillary sinus, nasal cavities & ethmoid air cells. Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Penn Radiology
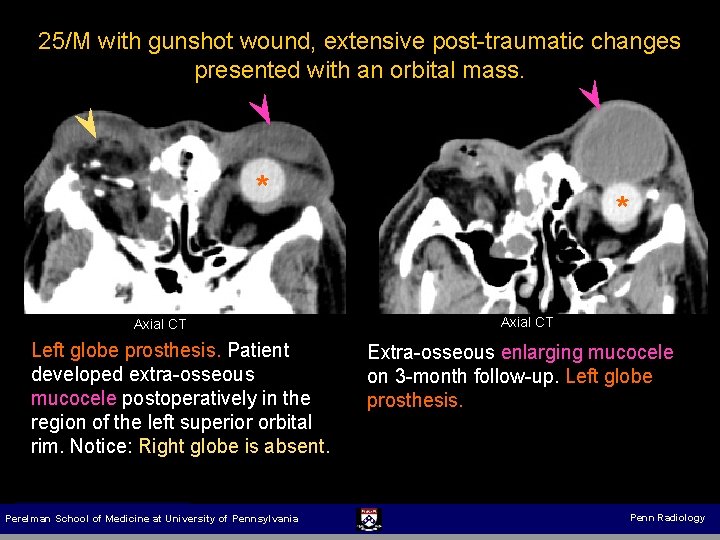
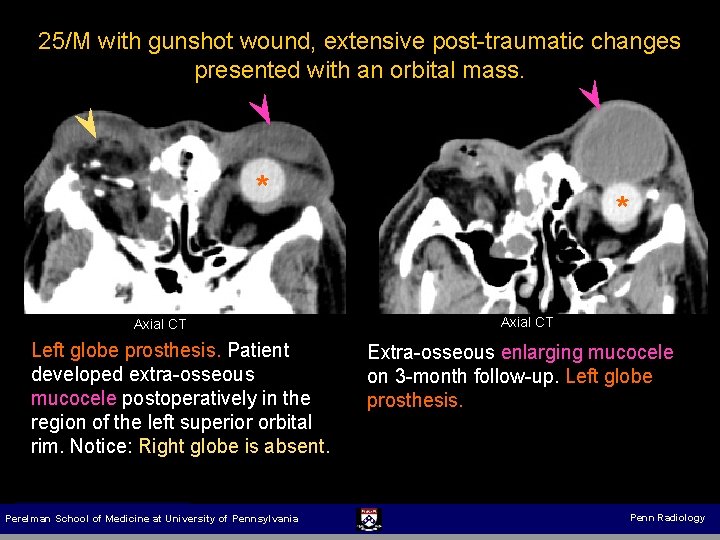
25/M with gunshot wound, extensive post-traumatic changes presented with an orbital mass. * Axial CT Left globe prosthesis. Patient developed extra-osseous mucocele postoperatively in the region of the left superior orbital rim. Notice: Right globe is absent. Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania * Axial CT Extra-osseous enlarging mucocele on 3 -month follow-up. Left globe prosthesis. Penn Radiology
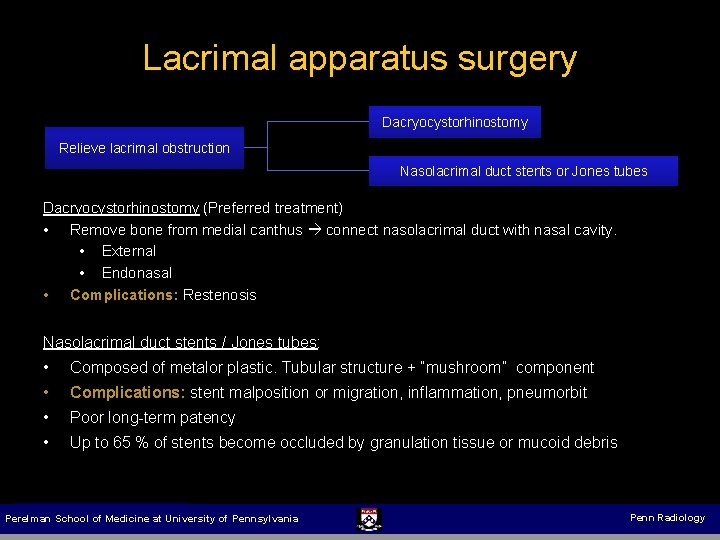
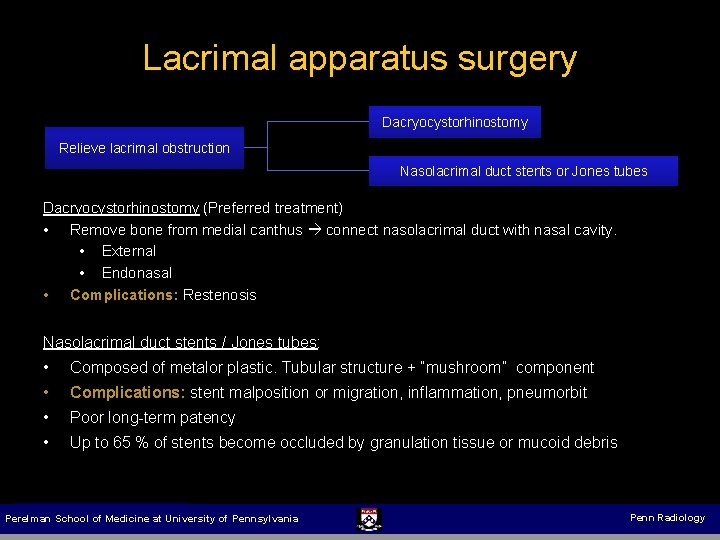
Lacrimal apparatus surgery Dacryocystorhinostomy Relieve lacrimal obstruction Nasolacrimal duct stents or Jones tubes Dacryocystorhinostomy (Preferred treatment) • Remove bone from medial canthus connect nasolacrimal duct with nasal cavity. • External • Endonasal • Complications: Restenosis Nasolacrimal duct stents / Jones tubes: • • Composed of metalor plastic. Tubular structure + “mushroom” component • • Poor long-term patency Complications: stent malposition or migration, inflammation, pneumorbit Up to 65 % of stents become occluded by granulation tissue or mucoid debris Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Penn Radiology
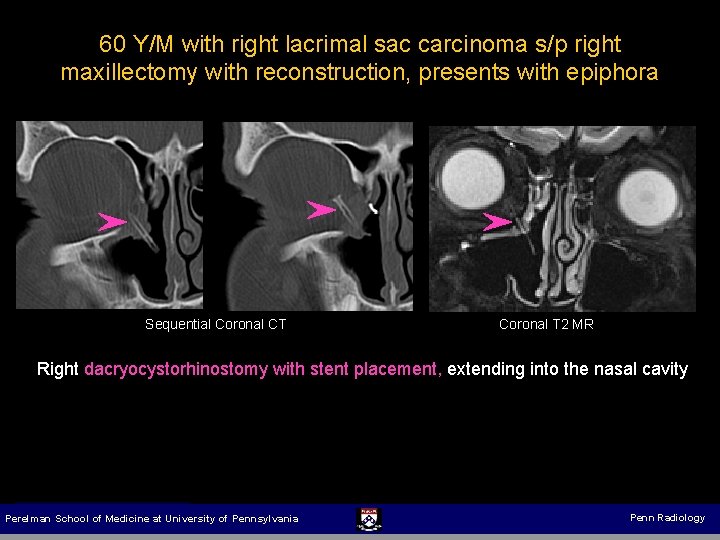
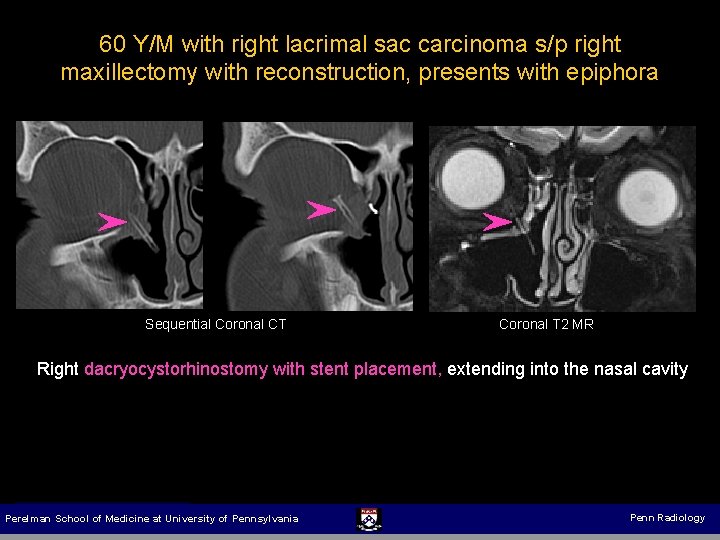
60 Y/M with right lacrimal sac carcinoma s/p right maxillectomy with reconstruction, presents with epiphora Sequential Coronal CT Coronal T 2 MR Right dacryocystorhinostomy with stent placement, extending into the nasal cavity Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Penn Radiology
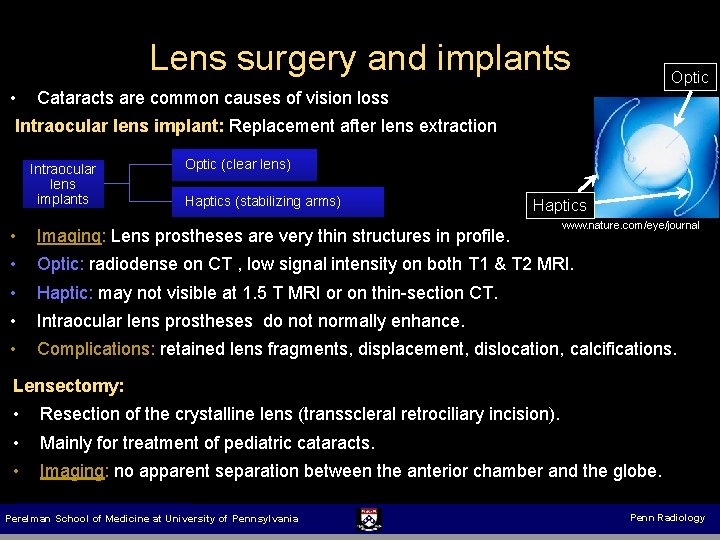
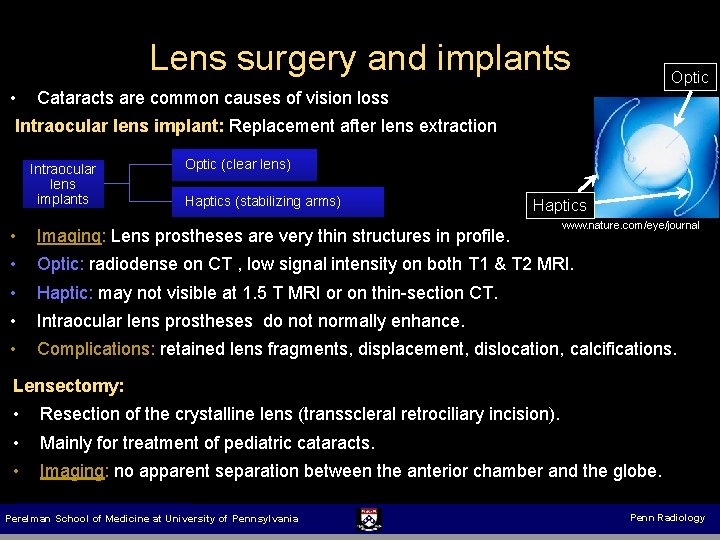
Lens surgery and implants Optic • Cataracts are common causes of vision loss Intraocular lens implant: Replacement after lens extraction Intraocular lens implants Optic (clear lens) Haptics (stabilizing arms) Haptics www. nature. com/eye/journal • • Imaging: Lens prostheses are very thin structures in profile. • • Haptic: may not visible at 1. 5 T MRI or on thin-section CT. • Complications: retained lens fragments, displacement, dislocation, calcifications. Optic: radiodense on CT , low signal intensity on both T 1 & T 2 MRI. Intraocular lens prostheses do not normally enhance. Lensectomy: • • Resection of the crystalline lens (transscleral retrociliary incision). • Imaging: no apparent separation between the anterior chamber and the globe. Mainly for treatment of pediatric cataracts. Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Penn Radiology
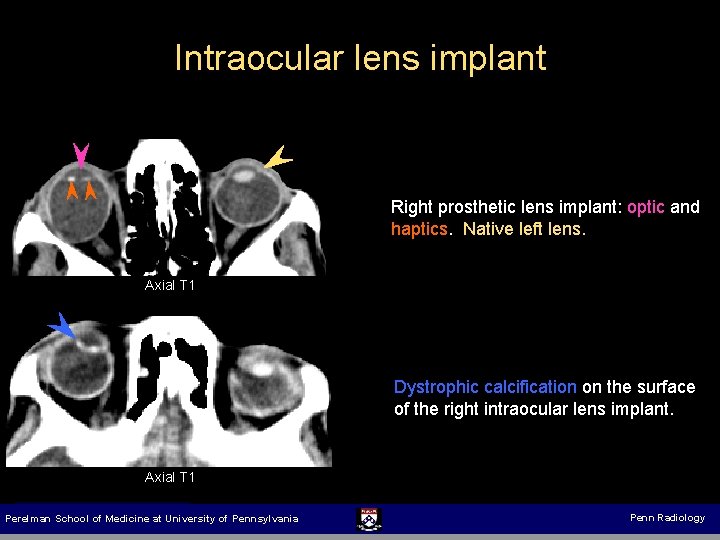
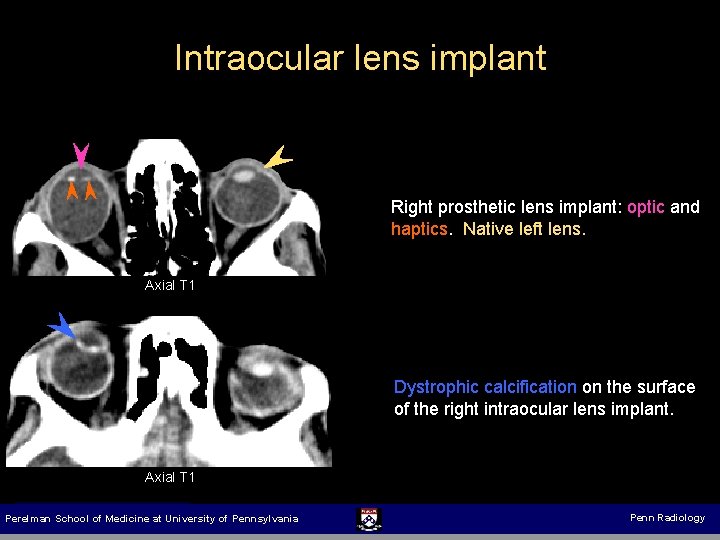
Intraocular lens implant Right prosthetic lens implant: optic and haptics. Native left lens. Axial T 1 Dystrophic calcification on the surface of the right intraocular lens implant. Axial T 1 Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Penn Radiology
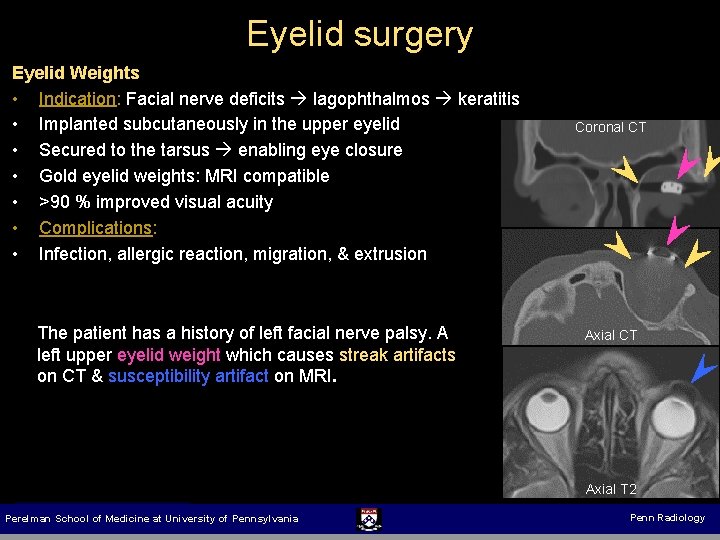
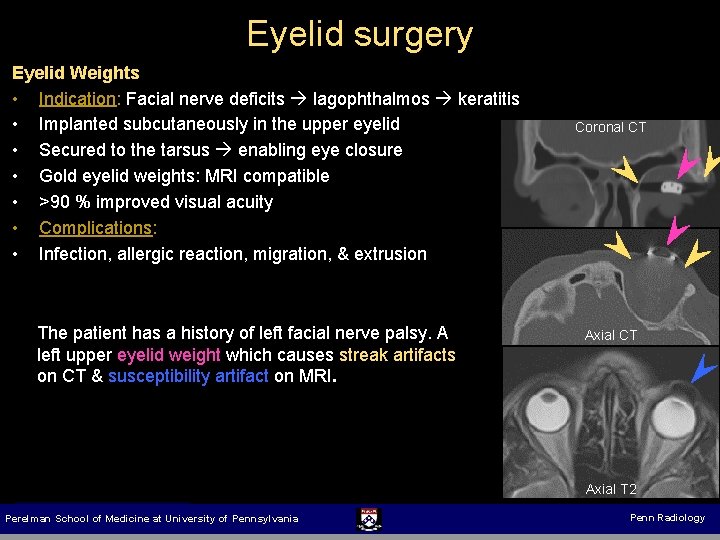
Eyelid surgery Eyelid Weights • Indication: Facial nerve deficits lagophthalmos keratitis • Implanted subcutaneously in the upper eyelid • Secured to the tarsus enabling eye closure • Gold eyelid weights: MRI compatible • >90 % improved visual acuity • Complications: • Infection, allergic reaction, migration, & extrusion The patient has a history of left facial nerve palsy. A left upper eyelid weight which causes streak artifacts on CT & susceptibility artifact on MRI. Coronal CT Axial T 2 Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Penn Radiology
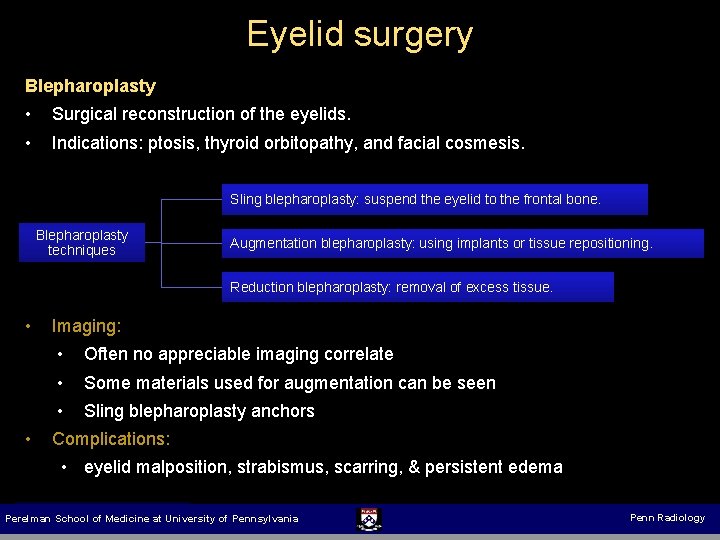
Eyelid surgery Blepharoplasty • • Surgical reconstruction of the eyelids. Indications: ptosis, thyroid orbitopathy, and facial cosmesis. Sling blepharoplasty: suspend the eyelid to the frontal bone. Blepharoplasty techniques Augmentation blepharoplasty: using implants or tissue repositioning. Reduction blepharoplasty: removal of excess tissue. • Imaging: • • • Often no appreciable imaging correlate Some materials used for augmentation can be seen • Sling blepharoplasty anchors Complications: • eyelid malposition, strabismus, scarring, & persistent edema Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Penn Radiology
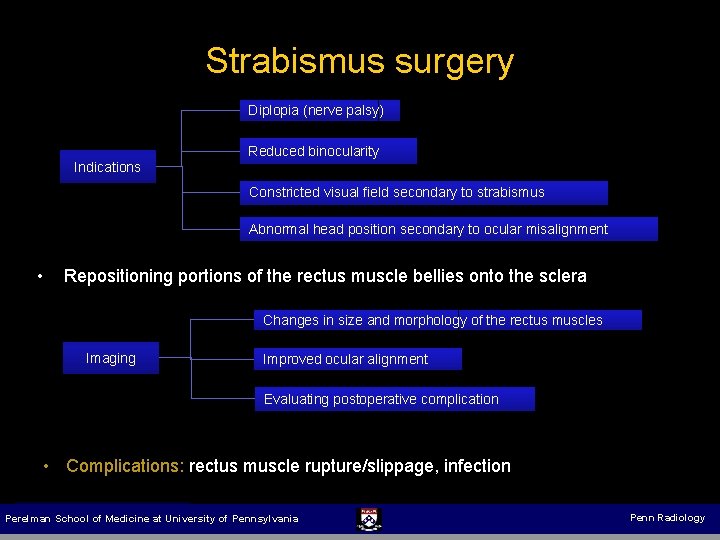
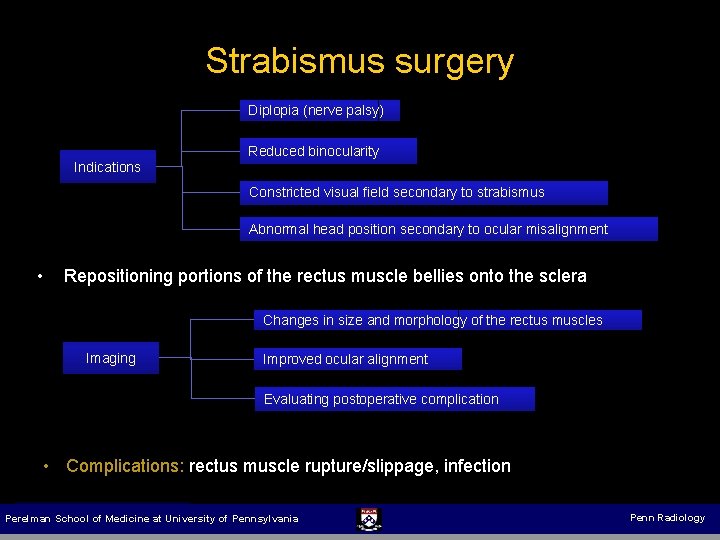
Strabismus surgery Diplopia (nerve palsy) Reduced binocularity Indications Constricted visual field secondary to strabismus Abnormal head position secondary to ocular misalignment • Repositioning portions of the rectus muscle bellies onto the sclera Changes in size and morphology of the rectus muscles Imaging Improved ocular alignment Evaluating postoperative complication • Complications: Complications rectus muscle rupture/slippage, infection Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Penn Radiology
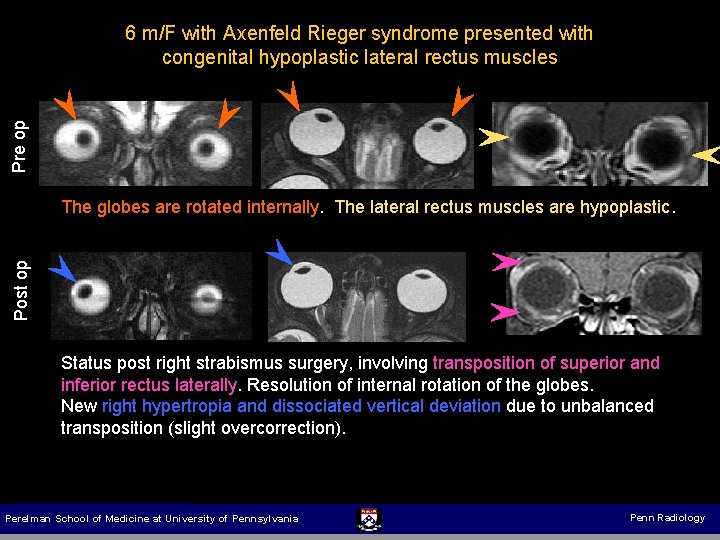
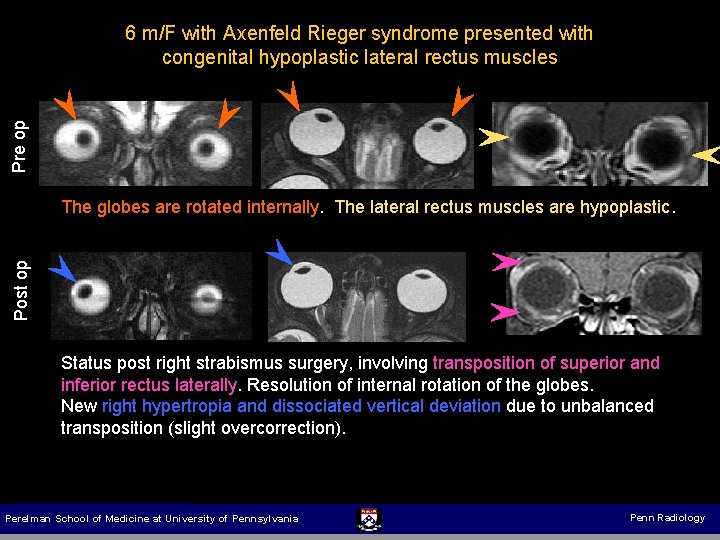
Pre op 6 m/F with Axenfeld Rieger syndrome presented with congenital hypoplastic lateral rectus muscles Post op The globes are rotated internally. The lateral rectus muscles are hypoplastic. Status post right strabismus surgery, involving transposition of superior and inferior rectus laterally. Resolution of internal rotation of the globes. New right hypertropia and dissociated vertical deviation due to unbalanced transposition (slight overcorrection). Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Penn Radiology
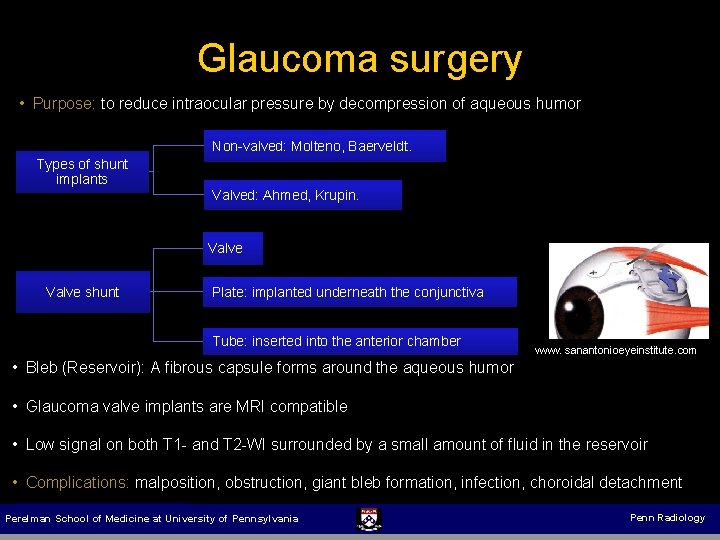
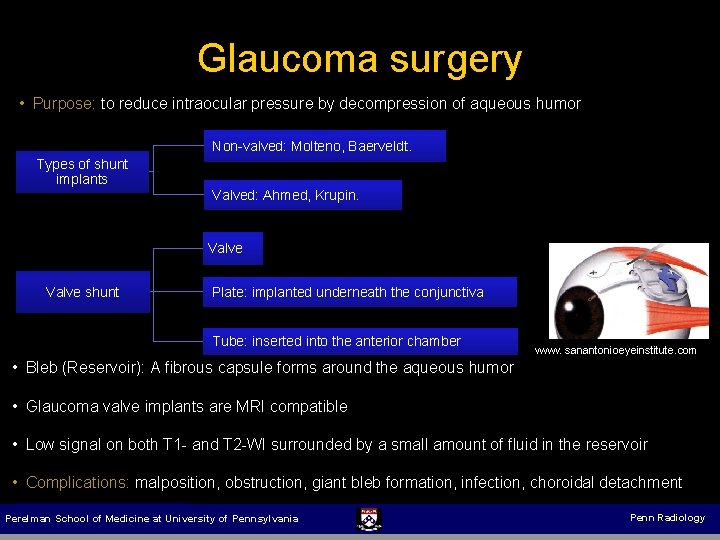
Glaucoma surgery • Purpose: to reduce intraocular pressure by decompression of aqueous humor Non-valved: Molteno, Baerveldt. Types of shunt implants Valved: Ahmed, Krupin. Valve shunt Plate: implanted underneath the conjunctiva Tube: inserted into the anterior chamber www. sanantonioeyeinstitute. com • Bleb (Reservoir): A fibrous capsule forms around the aqueous humor • Glaucoma valve implants are MRI compatible • Low signal on both T 1 - and T 2 -WI surrounded by a small amount of fluid in the reservoir • Complications: malposition, obstruction, giant bleb formation, infection, choroidal detachment Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Penn Radiology
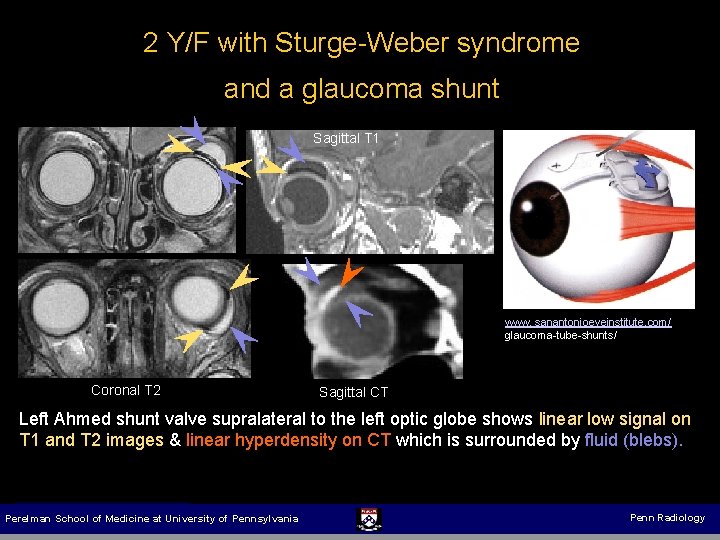
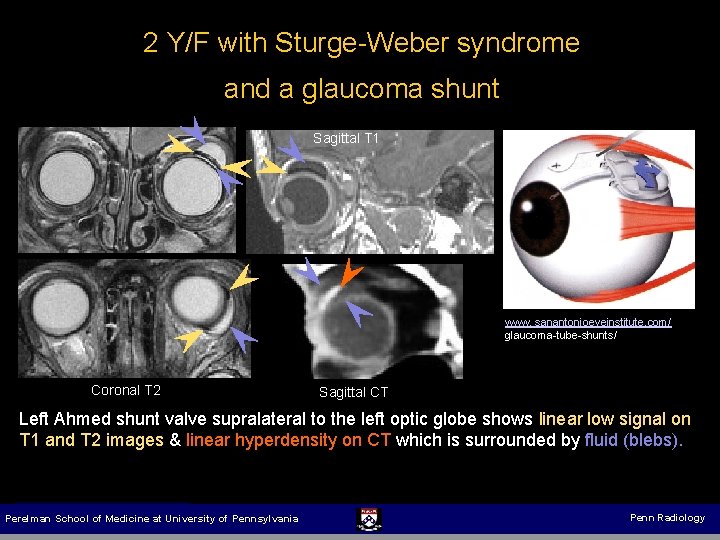
2 Y/F with Sturge-Weber syndrome and a glaucoma shunt Sagittal T 1 www. sanantonioeyeinstitute. com/ glaucoma-tube-shunts/ Coronal T 2 Sagittal CT Left Ahmed shunt valve supralateral to the left optic globe shows linear low signal on T 1 and T 2 images & linear hyperdensity on CT which is surrounded by fluid (blebs). Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Penn Radiology
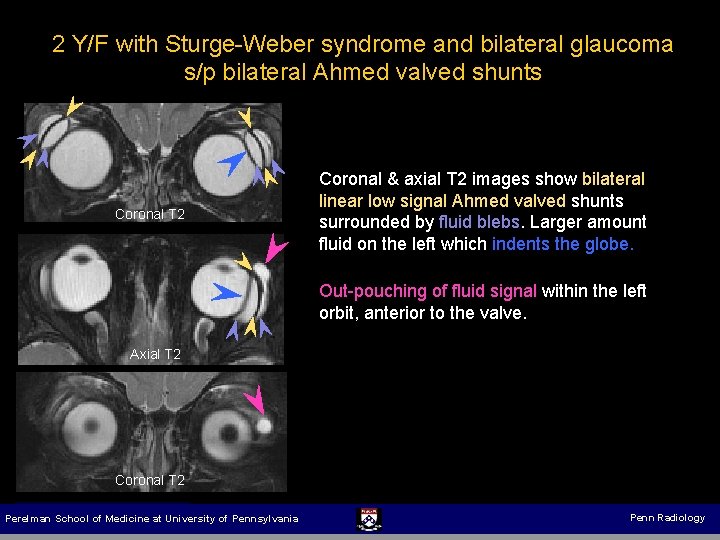
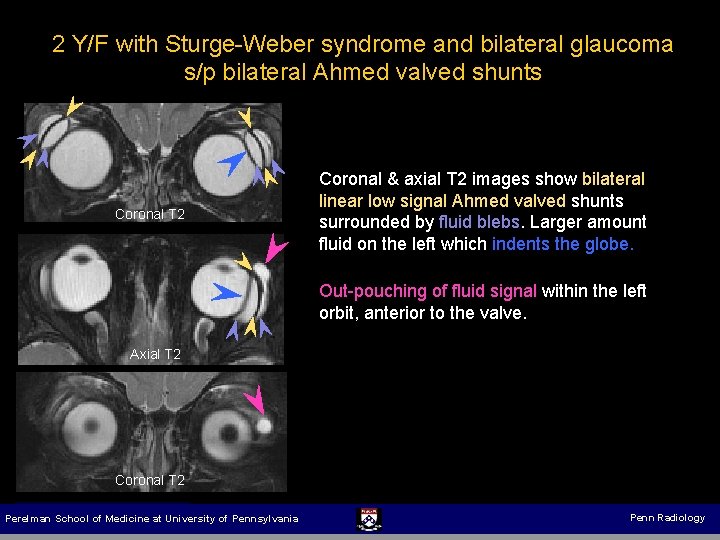
2 Y/F with Sturge-Weber syndrome and bilateral glaucoma s/p bilateral Ahmed valved shunts Coronal T 2 Coronal & axial T 2 images show bilateral linear low signal Ahmed valved shunts surrounded by fluid blebs. Larger amount fluid on the left which indents the globe. Out-pouching of fluid signal within the left orbit, anterior to the valve. Axial T 2 Coronal T 2 Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Penn Radiology
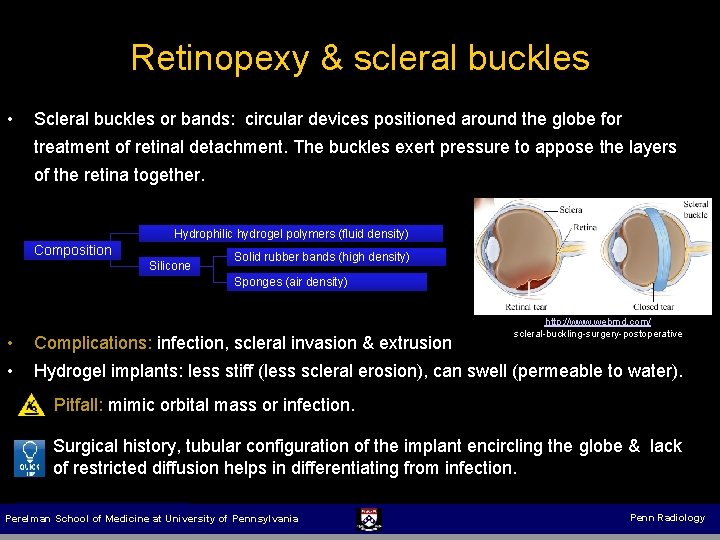
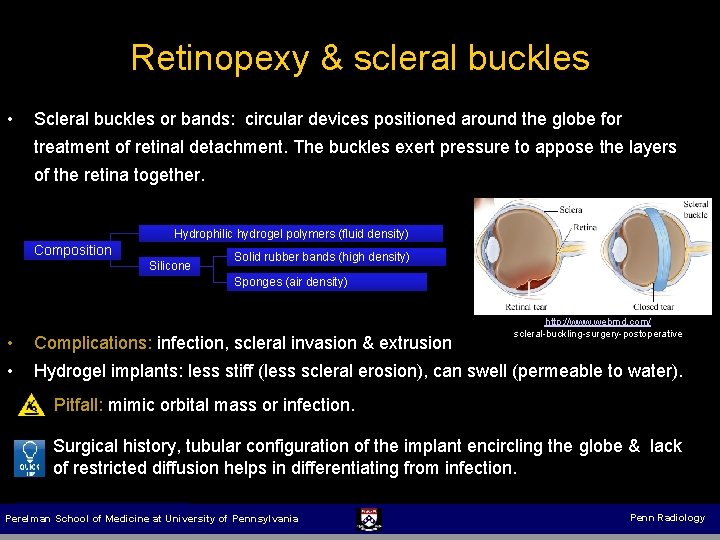
Retinopexy & scleral buckles • Scleral buckles or bands: circular devices positioned around the globe for treatment of retinal detachment. The buckles exert pressure to appose the layers of the retina together. Hydrophilic hydrogel polymers (fluid density) Composition Silicone Solid rubber bands (high density) Sponges (air density) • • Complications: infection, scleral invasion & extrusion http: //www. webmd. com/ scleral-buckling-surgery-postoperative Hydrogel implants: less stiff (less scleral erosion), can swell (permeable to water). Pitfall: mimic orbital mass or infection. Surgical history, tubular configuration of the implant encircling the globe & lack of restricted diffusion helps in differentiating from infection. Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Penn Radiology
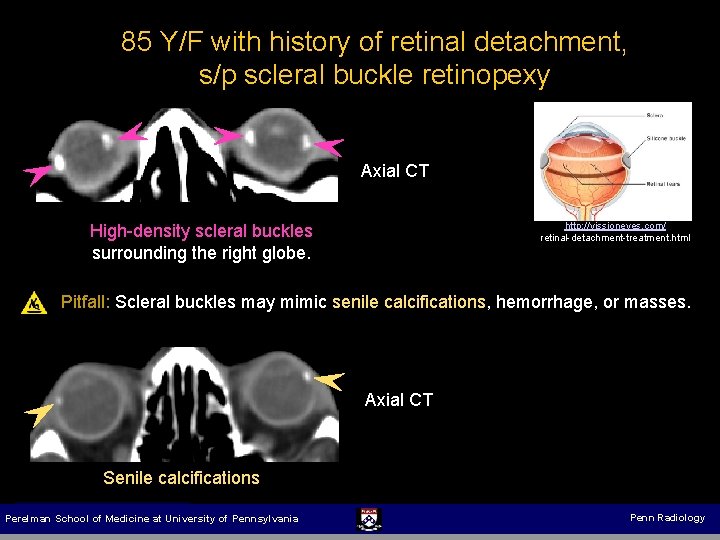
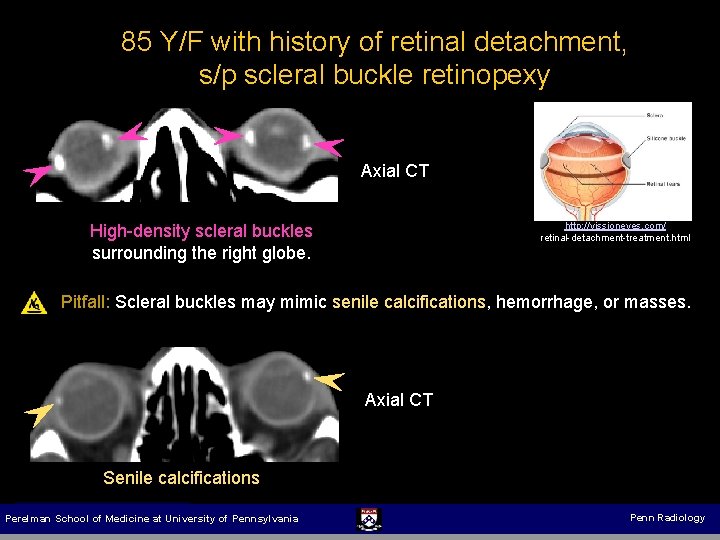
85 Y/F with history of retinal detachment, s/p scleral buckle retinopexy Axial CT http: //vissioneyes. com/ retinal-detachment-treatment. html High-density scleral buckles surrounding the right globe. Pitfall: Scleral buckles may mimic senile calcifications, hemorrhage, or masses. Axial CT Senile calcifications Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Penn Radiology
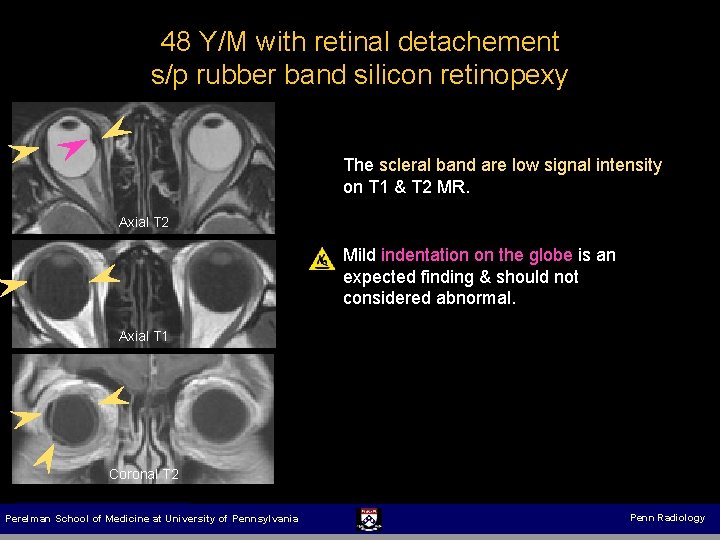
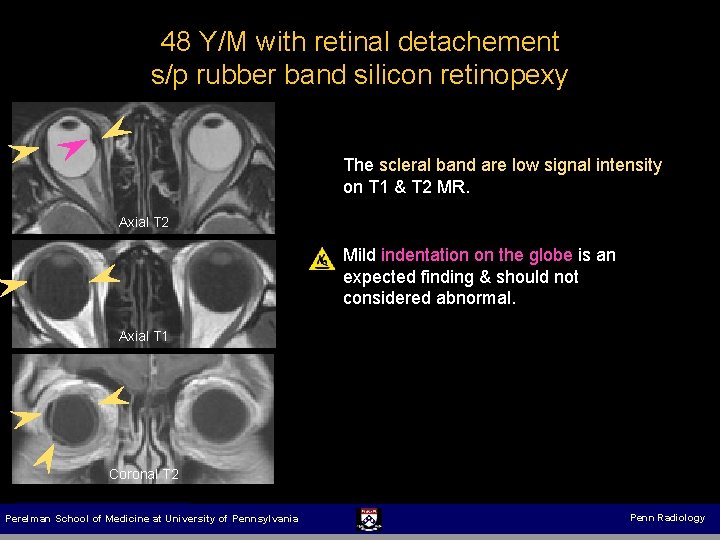
48 Y/M with retinal detachement s/p rubber band silicon retinopexy The scleral band are low signal intensity on T 1 & T 2 MR. Axial T 2 Mild indentation on the globe is an expected finding & should not considered abnormal. Axial T 1 Coronal T 2 Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Penn Radiology
Intraocular injections Indication: To tamponade the retina following retinal detachment until chorioretinal adhesions form. Pneumatic Retinopexy (Intraocular gas injection): (Effective up to 80 %) • • To restore intraocular volume during scleral banding • Imaging: Air lucency is present antidependently in the vitreous body, creating an air-fluid A variety of gases: air, hexafluoride, & perfluoropropane level • Complications: secondary glaucoma, gas migration, vitreous hemorrhage, endophthalmitis & proliferative vitreoretinopathy Intraocular Silicone Injection: • The silicone oil used for tamponade is usually removed after 8 weeks, but may remain permanently, depending on the risk of recurrent detachment • • Imaging: On CT, silicone oil is hyperdense & globular, measuring up to 120 HU Complications: choroidal detachment, scarring, cataracts, & optic nerve atrophy Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Penn Radiology
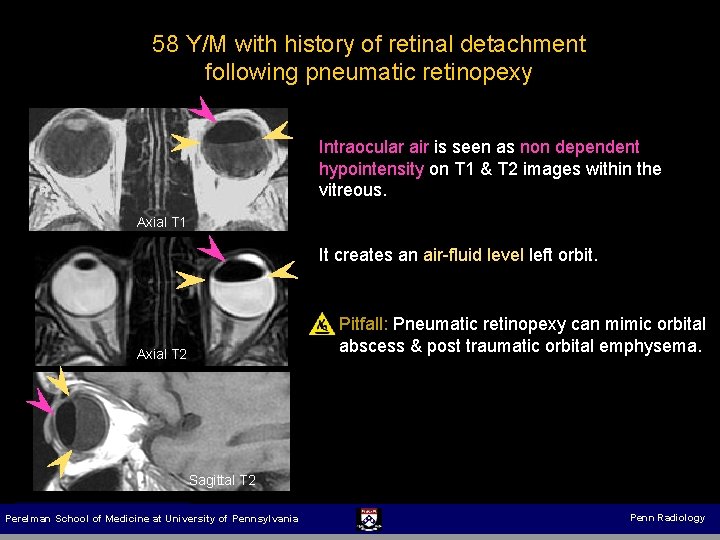
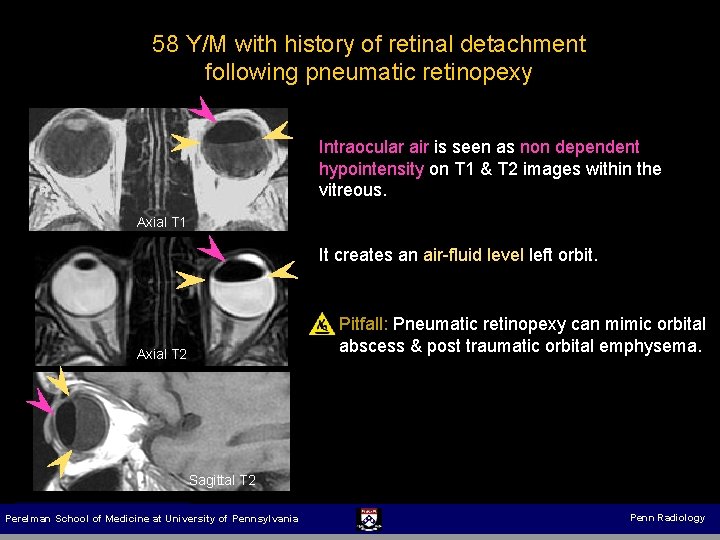
58 Y/M with history of retinal detachment following pneumatic retinopexy Intraocular air is seen as non dependent hypointensity on T 1 & T 2 images within the vitreous. Axial T 1 It creates an air-fluid level left orbit. Pitfall: Pneumatic retinopexy can mimic orbital abscess & post traumatic orbital emphysema. Axial T 2 Sagittal T 2 Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Penn Radiology
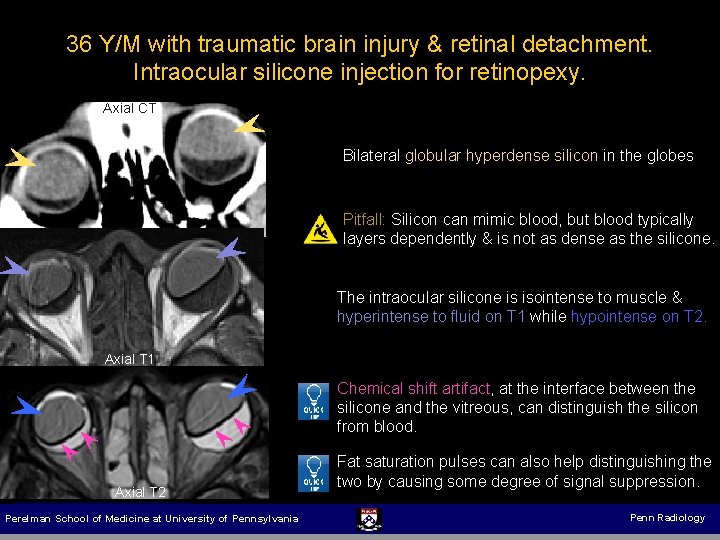
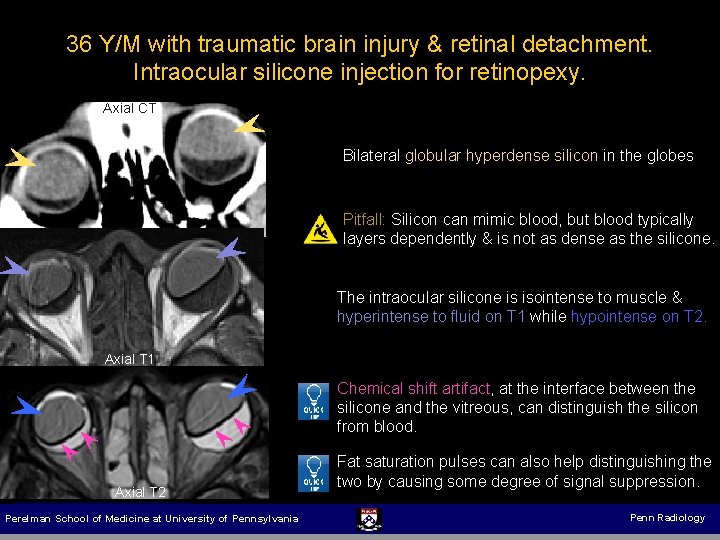
36 Y/M with traumatic brain injury & retinal detachment. Intraocular silicone injection for retinopexy. Axial CT Bilateral globular hyperdense silicon in the globes Pitfall: Silicon can mimic blood, but blood typically layers dependently & is not as dense as the silicone. The intraocular silicone is isointense to muscle & hyperintense to fluid on T 1 while hypointense on T 2. Axial T 1 Chemical shift artifact, at the interface between the silicone and the vitreous, can distinguish the silicon from blood. Axial T 2 Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Fat saturation pulses can also help distinguishing the two by causing some degree of signal suppression. Penn Radiology
Conclusion Familiarity with imaging findings of the wide-ranging spectrum of postoperative changes are crucial to differentiate expected postoperative findings from complications. Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Penn Radiology
Thank you for reviewing our exhibit v Farbodnasserimd@gmail. com v Suyash. mohan@uphs. upenn. edu Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Penn Radiology
Selected References 1. Jordan DR, St Onge P, Anderson RL, Patrinely JR, Nerad JA (1992) Complications associated with alloplastic implants used in orbital fracture repair. Ophthalmology 99(10): 1600– 1608 2. Leong SC, White PS (2010) Outcomes following surgical decompression for dysthyroid orbitopathy (Graves’disease). Curr Opin Otolaryngol Head Neck Surg 18(1): 37– 43 3. Christmas NJ, Gordon CD, Murray TG, Tse D, Johnson T, Garonzik S, O’Brien JM (1998) Intraorbital implants after enucleation and their complications: a 10 -year review. Arch Ophthalmol 116(9): 1199– 1203 4. Tyers AG (2006) Orbital exenteration for invasive skin tumours. Eye (Lond) 20(10): 1165– 1170 5. Nishida Y, Inatomi A, Aoki Y, Hayashi O, Iwami T, Oda S, Nakamura J, Kani K (2003) A muscle transposition procedure for abducens palsy, in which the halves of the vertical rectus muscle bellies are sutured onto the sclera. Jpn J Ophthalmol 47(3): 281– 286 6. Freedman J (2010) What is new after 40 years of glaucoma implants. J Glaucoma 19(8): 504– 508 7. Chan CK, Lin SG, Nuthi AS, Salib DM (2008) Pneumatic retinopexy for the repair of retinal detachments: a comprehensive review (1986– 2007). Surv Ophthalmol 53(5): 443– 8 8. Mathews VP, Elster AD, Barker PB, Buff BL, Haller JA, Greven CM (1994) Intraocular silicone oil: in vitro and in vivo MR and CT characteristics. AJNR 15: 343– 347 9. Kartush JM, Linstrom CJ, Mc. Cann PM, Graham MD (1990) Early gold weight eyelid implantation for facial paralysis. Otolaryngol Head Neck Surg 103(6): 1016– 1023 Baltimore, Maryland Perelman School of Medicine at University of Pennsylvania Penn Radiology