THIRD EDITION HUMAN PHYSIOLOGY AN INTEGRATED APPROACH Dee
- Slides: 57
THIRD EDITION HUMAN PHYSIOLOGY AN INTEGRATED APPROACH Dee Unglaub Silverthorn, Ph. D. Chapter 16 Blood Power. Point® Lecture Slide Presentation by Dr. Howard D. Booth, Professor of Biology, Eastern Michigan University Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
About this Chapter • Composition of Blood • Plasma make up and roles • Various cell types, origin and roles • Red blood cells, hemoglobin & iron metabolism • How coagulation works Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
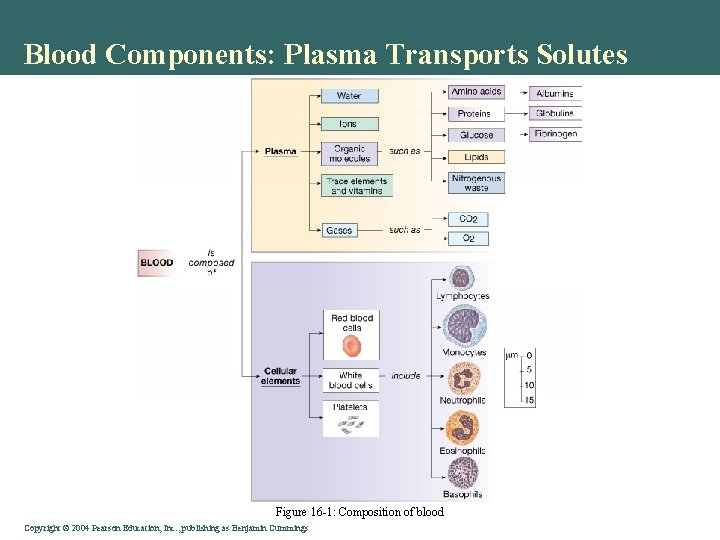
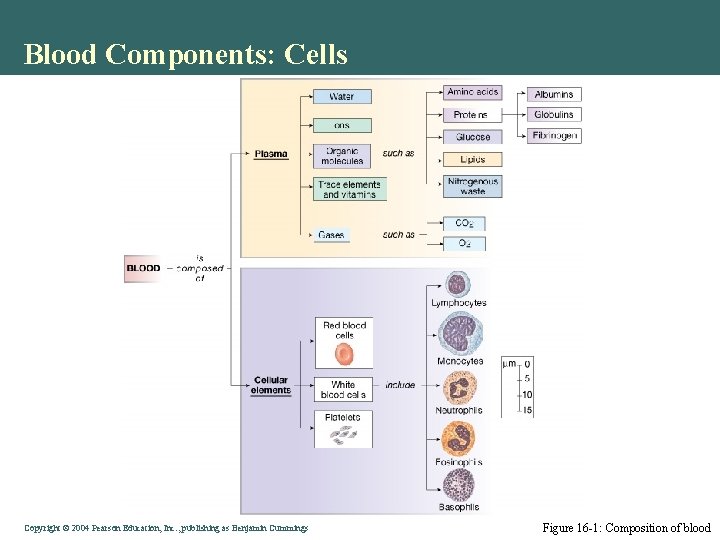
Composition of Blood • 55% of our blood's volume is made up of plasma • Plasma also contains blood clotting factors, sugars, lipids, vitamins, minerals, hormones, enzymes and antibodies • One group detected 490 separate proteins in serum • Serum albumin accounts for ~55% of blood proteins, globulins make up ~38% and fibrinogen comprises ~7% • The remainder of plasma proteins (1%) consists of regulatory proteins such as enzymes, proenzymes and hormones. All blood proteins are synthesized in liver except for the gamma globulins. • Plasma contains many thousands of distinct lipid molecular species that fall into six main categories including fatty acyls, glycerolipids, glycerophospholipids, sphingolipids, sterols, and prenols • The cellular components of blood include red corpuscles (erythrocytes), platelets (thrombocytes), and five types of white corpuscles (leukocytes) Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
Blood Components: Plasma Transports Solutes • Water, ions, trace elements • Gasses: O 2 & CO 2 • Organic Molecules • Glucose • N–wastes • Proteins • Antibodies • Hormones Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
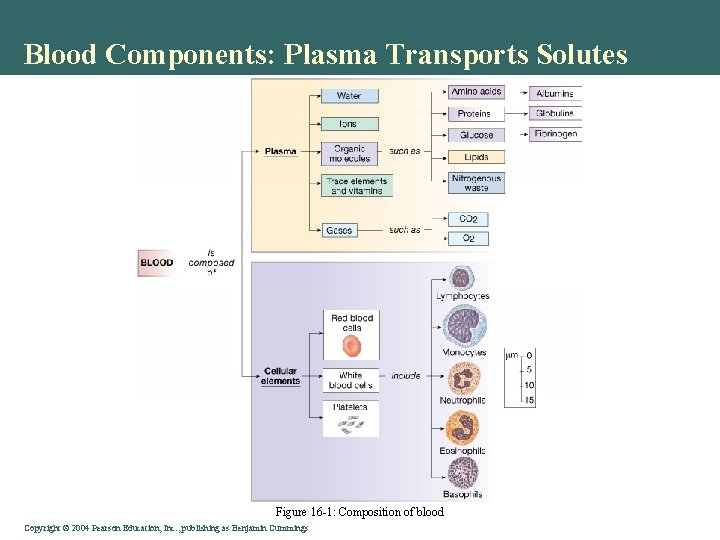
Blood Components: Plasma Transports Solutes Figure 16 -1: Composition of blood Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
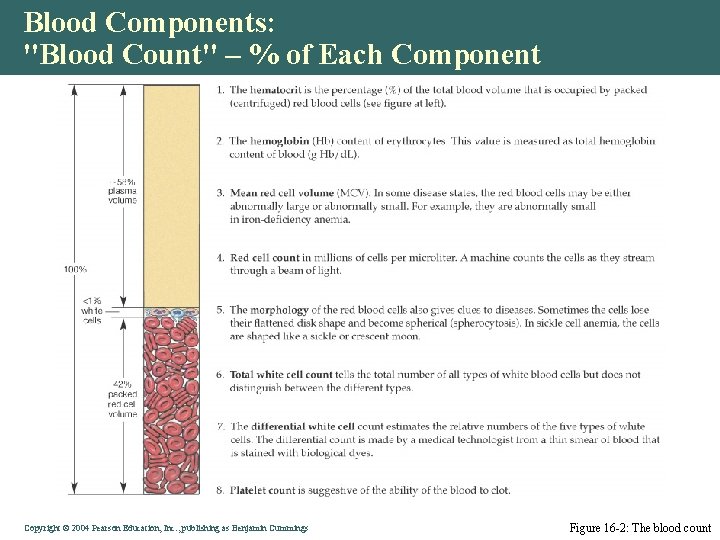
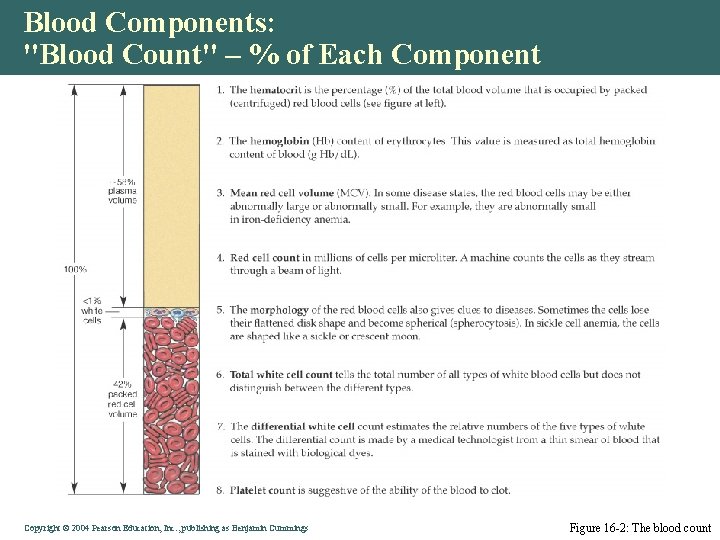
Blood Components: "Blood Count" – % of Each Component Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings Figure 16 -2: The blood count
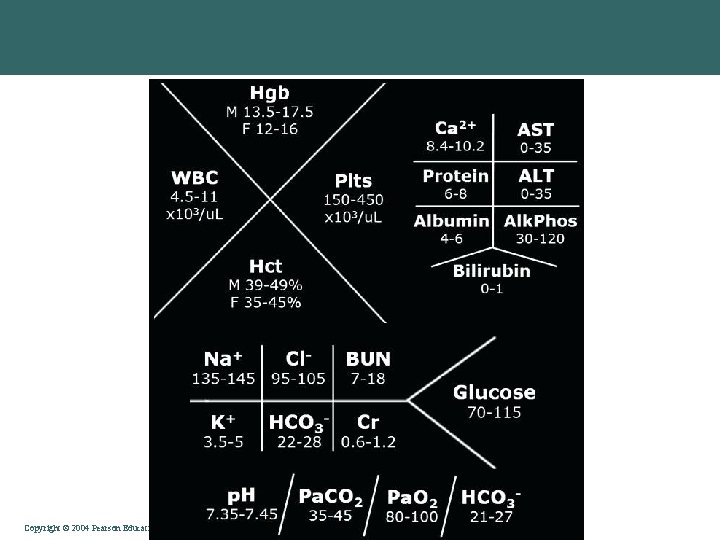
Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
Blood Components: Cells • Erythrocytes • Red Blood Cells (RBC) • O 2 & CO 2 transport • White Blood Cells (WBC) • Immune defense • Phagocytosis • Platelets: clotting Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
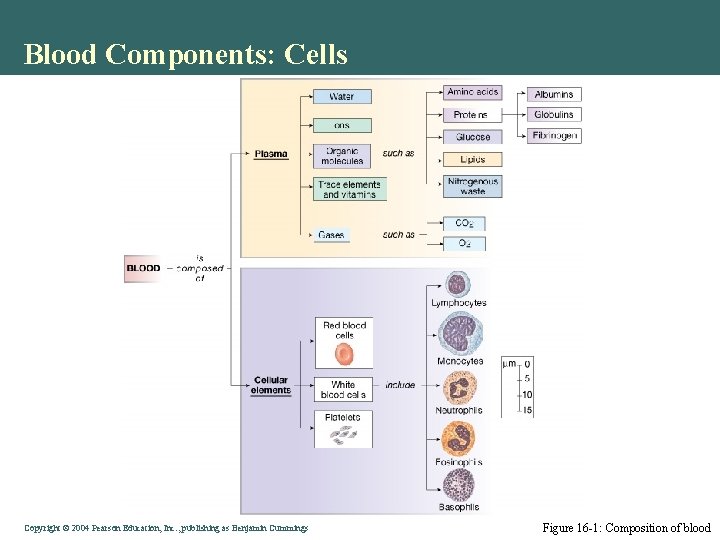
Blood Components: Cells Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings Figure 16 -1: Composition of blood
Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
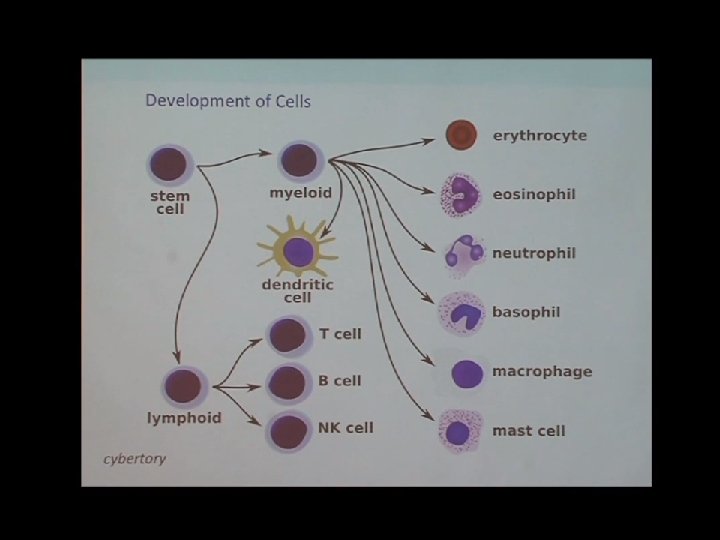
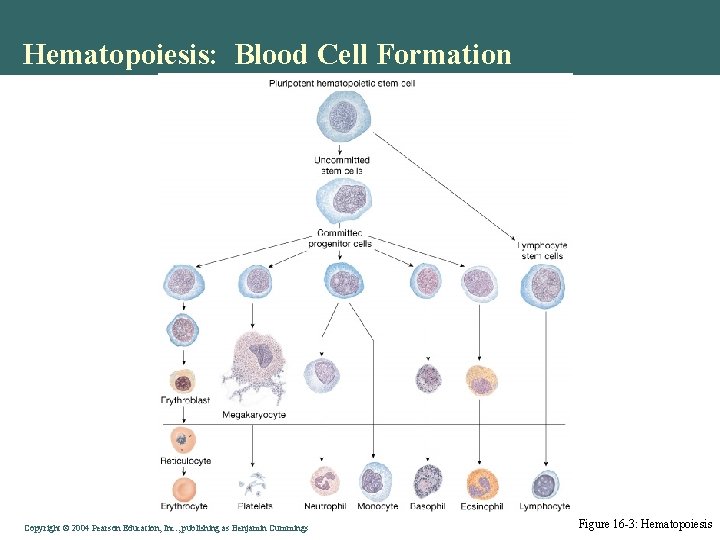
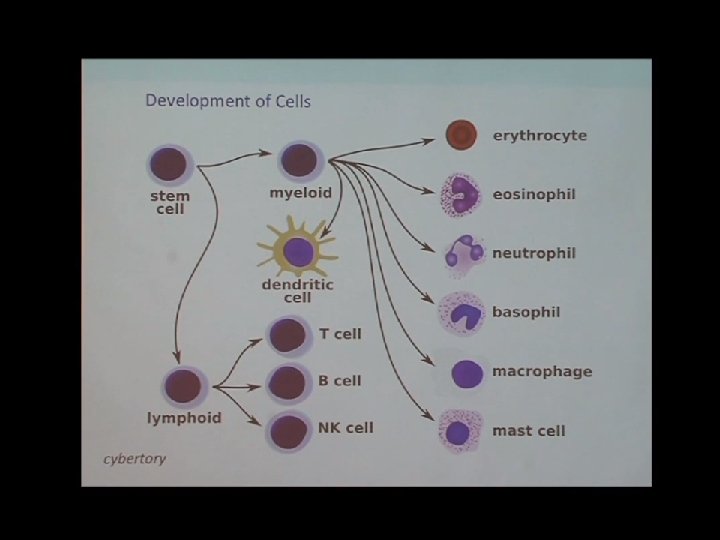
Hematopoiesis: Blood Cell Formation • Mostly in bone marrow from stem cells • Rate regulated by cytokines & growth factors Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
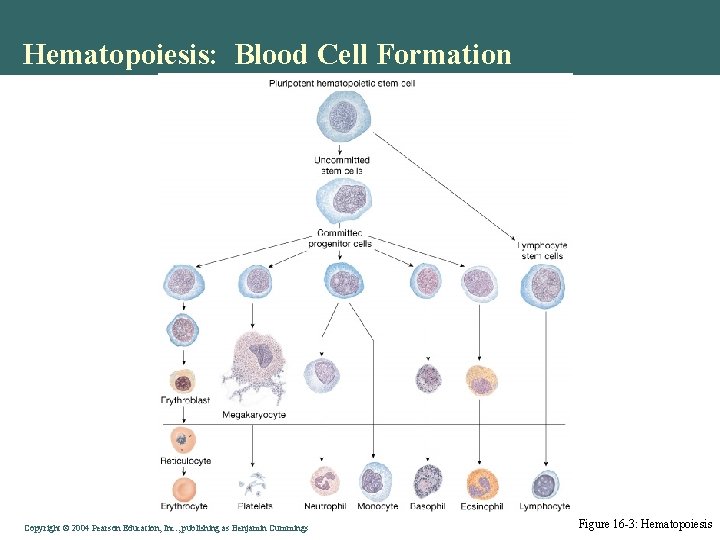
Hematopoiesis: Blood Cell Formation Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings Figure 16 -3: Hematopoiesis
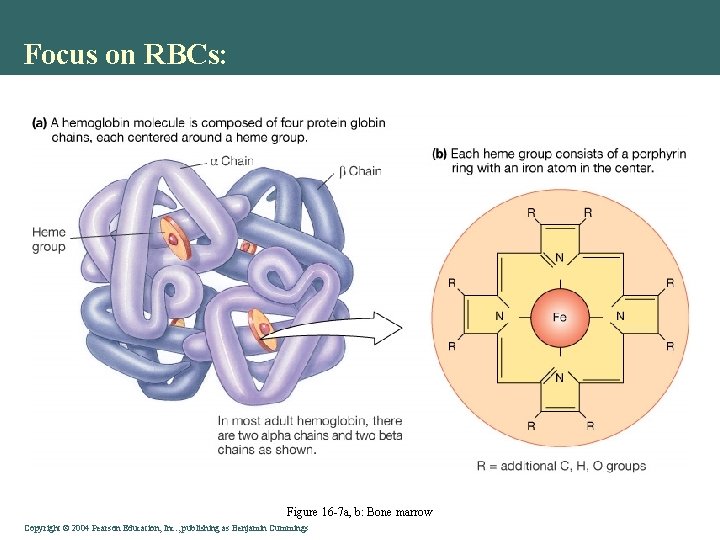
Focus on RBCs: • Lose their nucleus • Cytoskeleton – shape • Hemoglobin • Binds O 2 in heme group • Binds some CO 2 on globulin Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
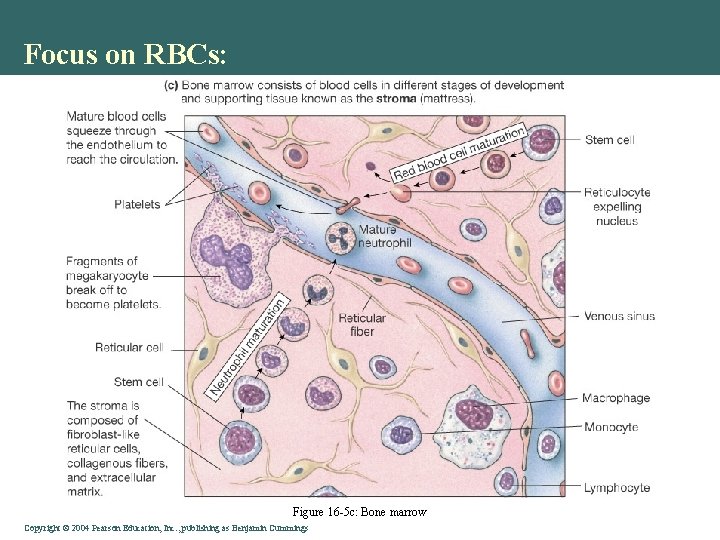
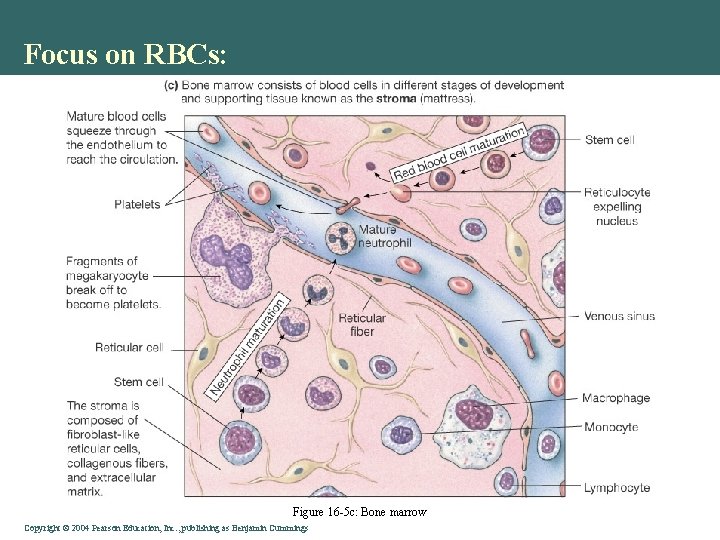
Focus on RBCs: Figure 16 -5 c: Bone marrow Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
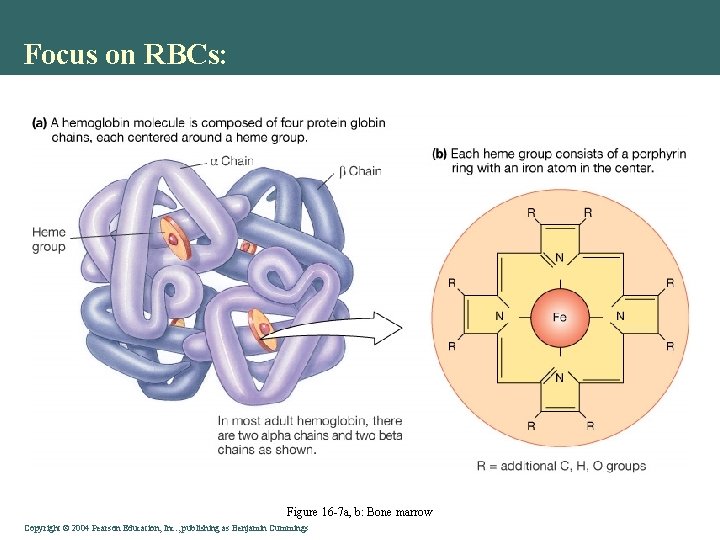
Focus on RBCs: Figure 16 -7 a, b: Bone marrow Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
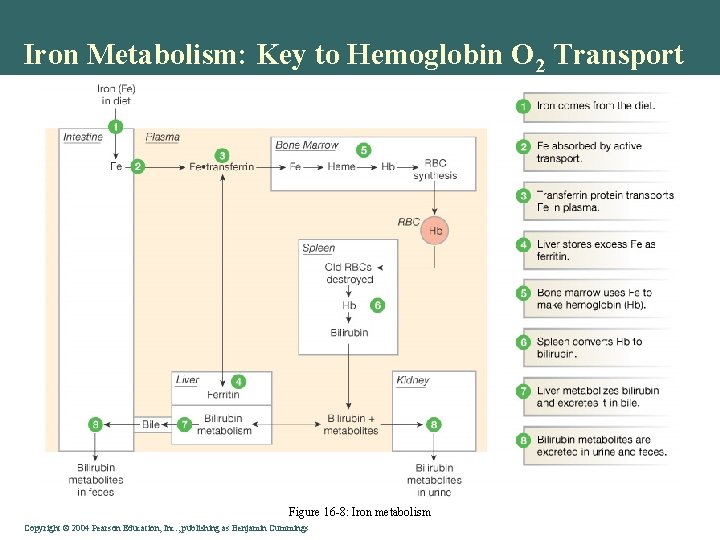
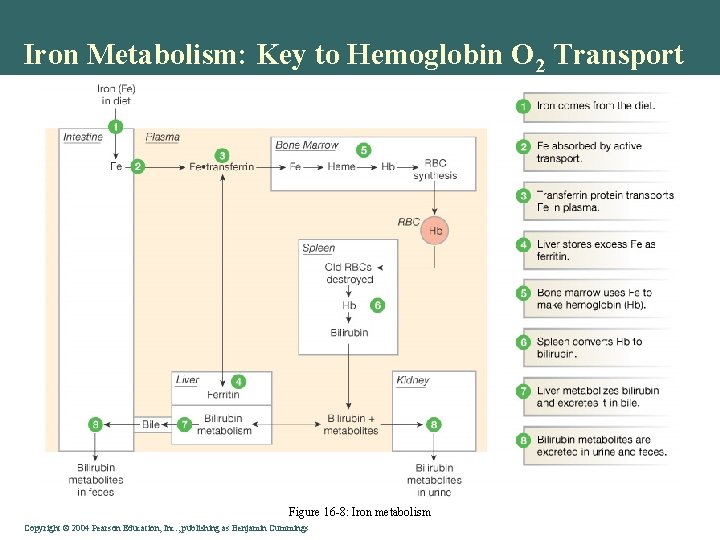
Iron Metabolism: Key to Hemoglobin O 2 Transport Figure 16 -8: Iron metabolism Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
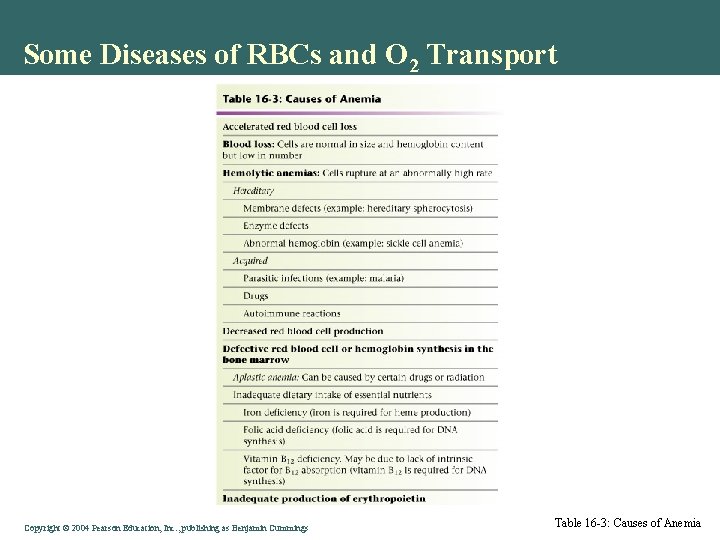
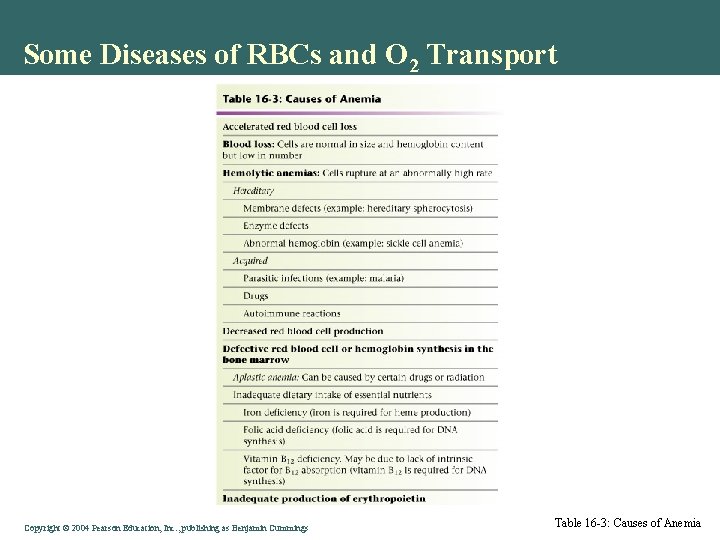
Some Diseases of RBCs and O 2 Transport Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings Table 16 -3: Causes of Anemia
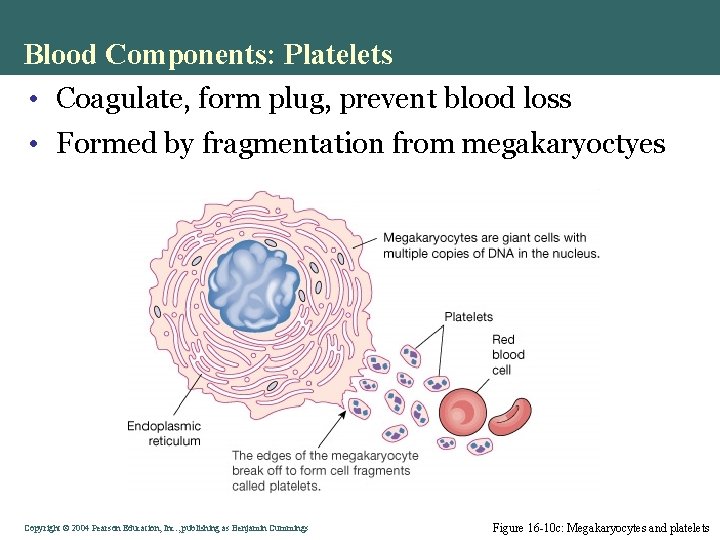
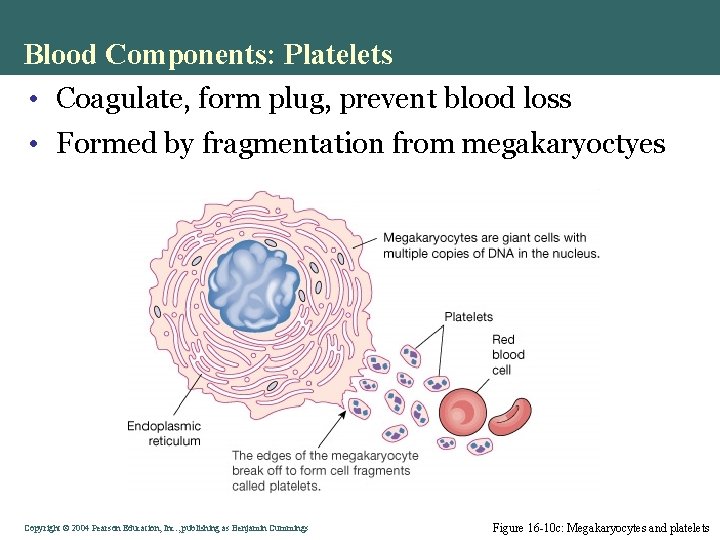
Blood Components: Platelets • Coagulate, form plug, prevent blood loss • Formed by fragmentation from megakaryoctyes Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings Figure 16 -10 c: Megakaryocytes and platelets
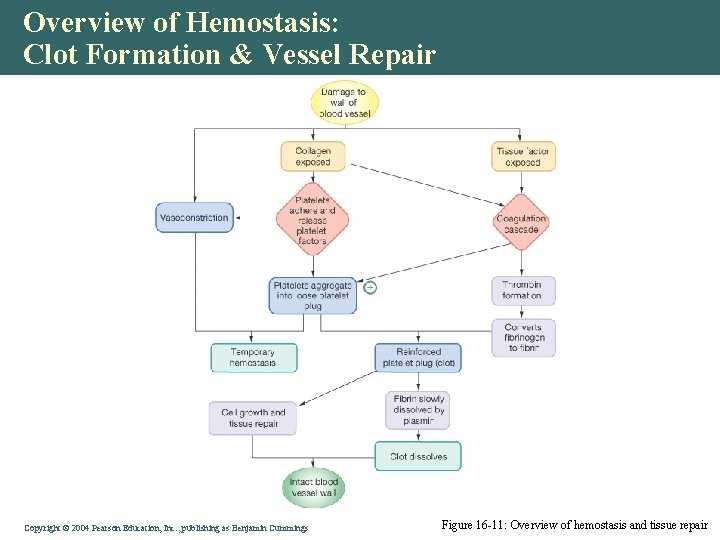
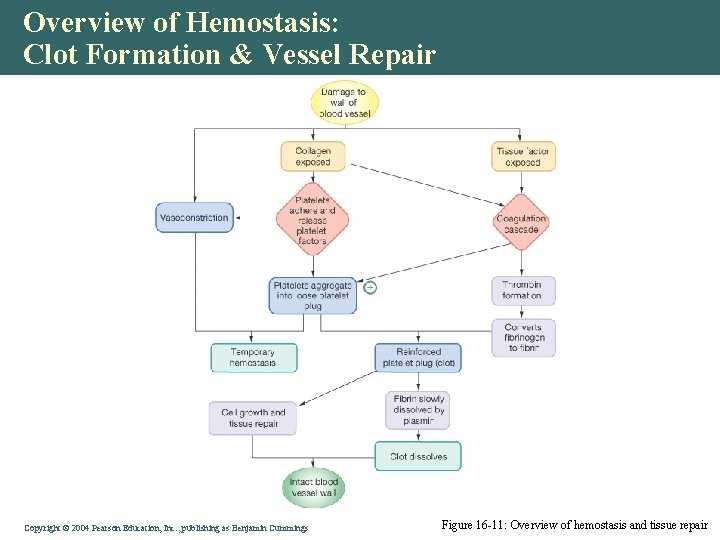
Overview of Hemostasis: Clot Formation & Vessel Repair Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings Figure 16 -11: Overview of hemostasis and tissue repair
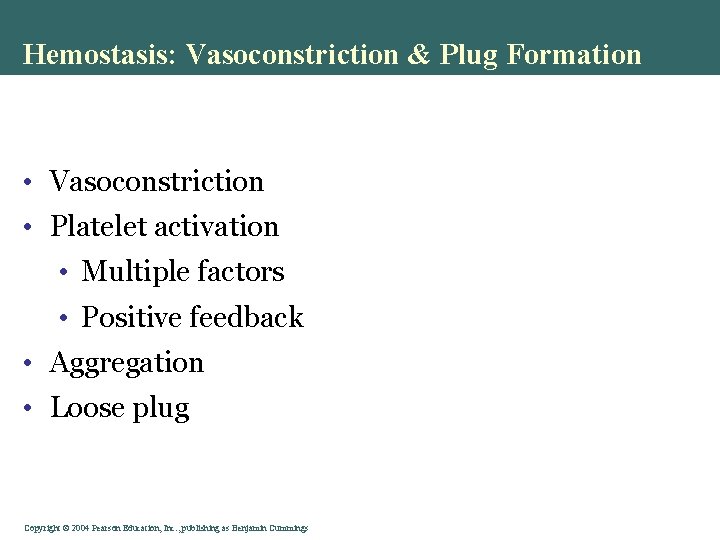
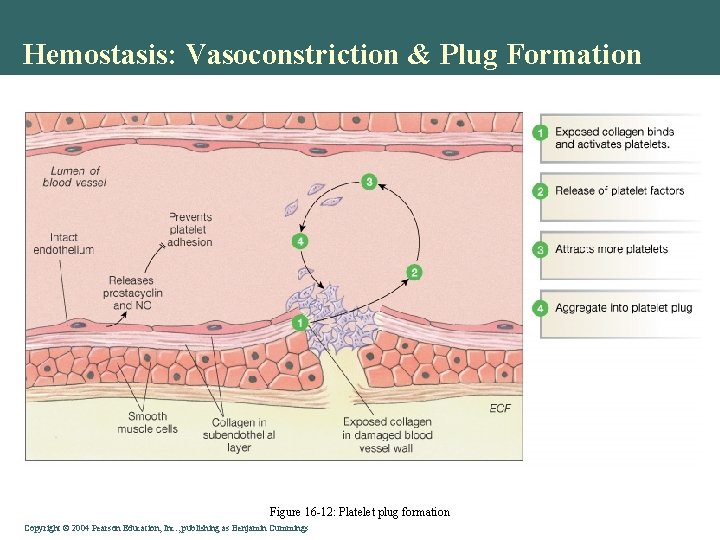
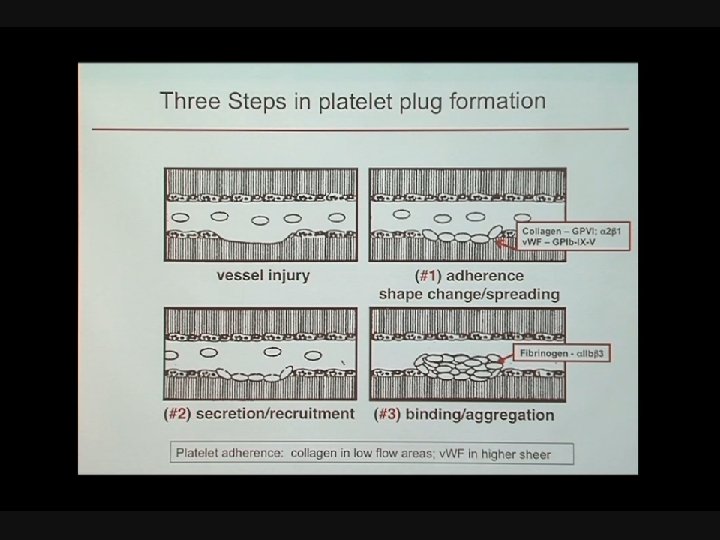
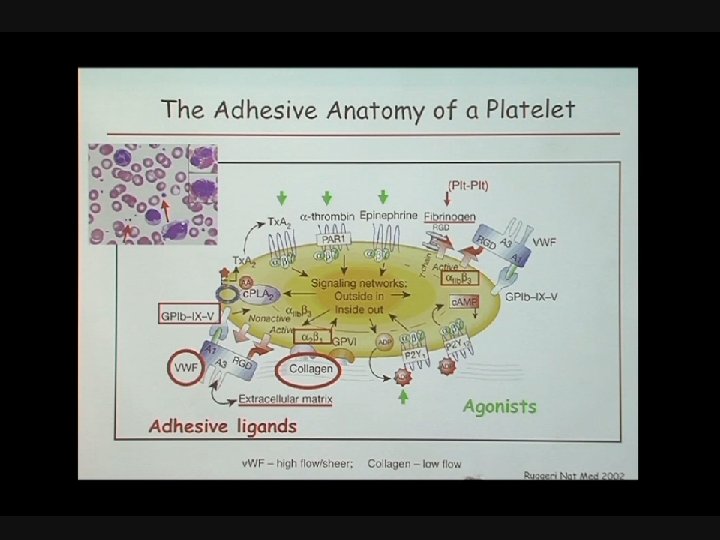
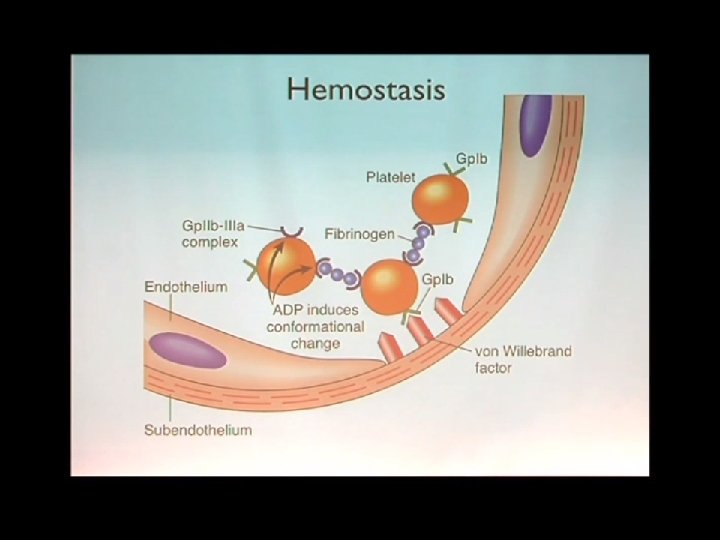
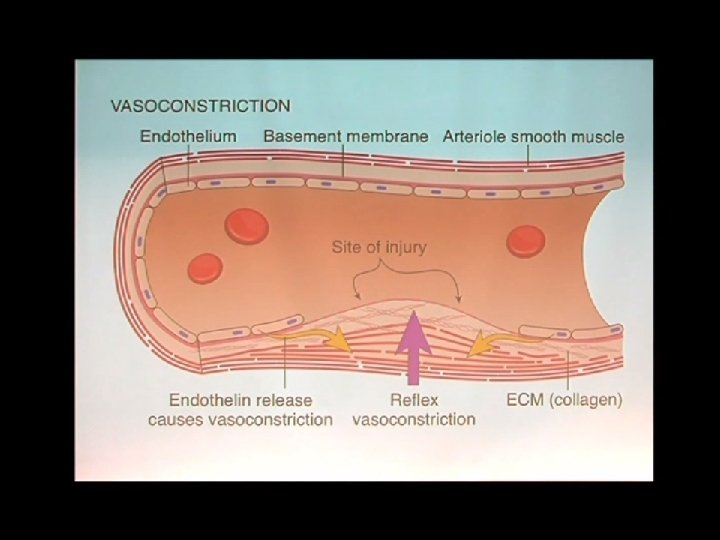
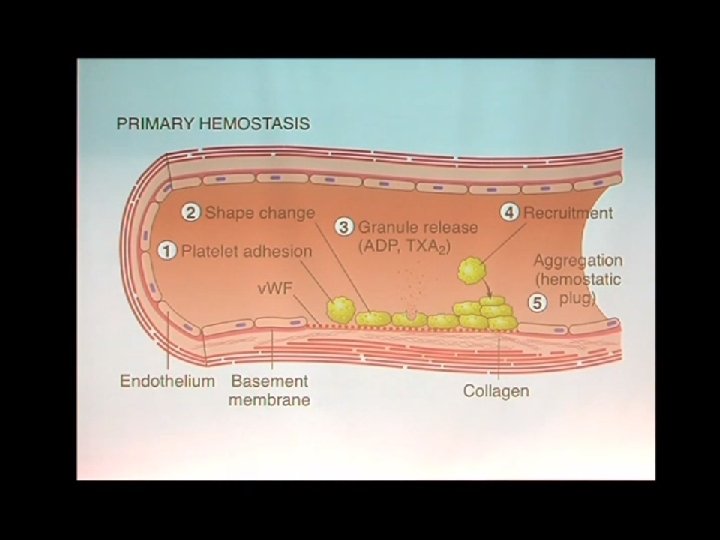
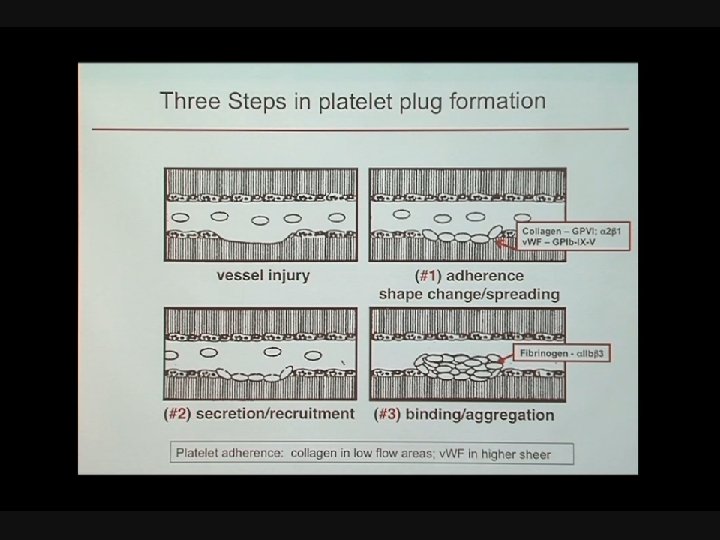
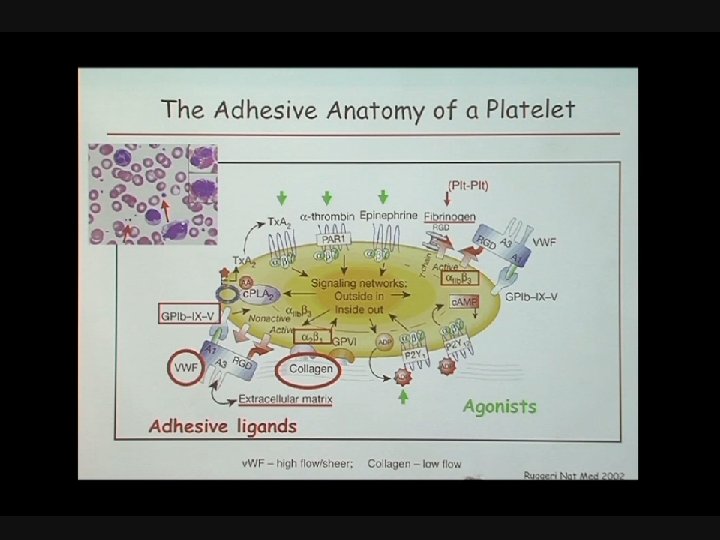
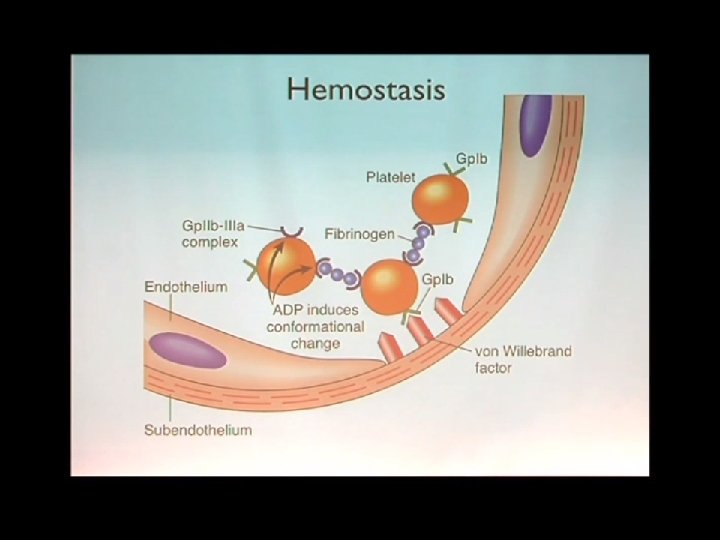
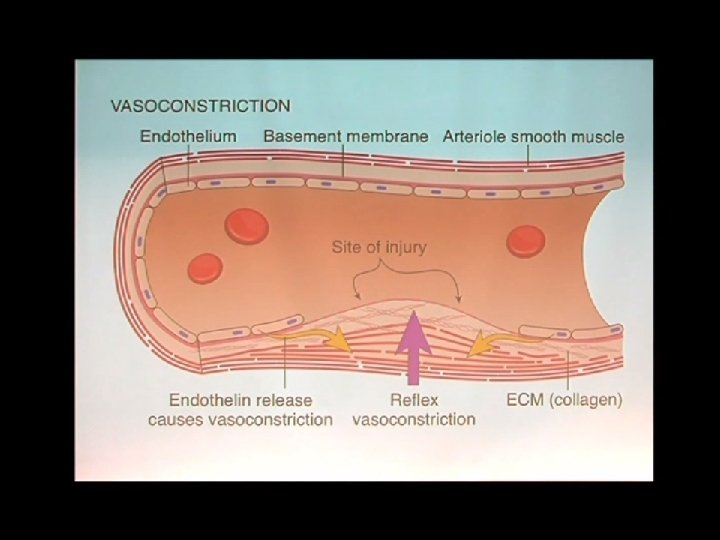
Hemostasis: Vasoconstriction & Plug Formation • Vasoconstriction • Platelet activation • Multiple factors • Positive feedback • Aggregation • Loose plug Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
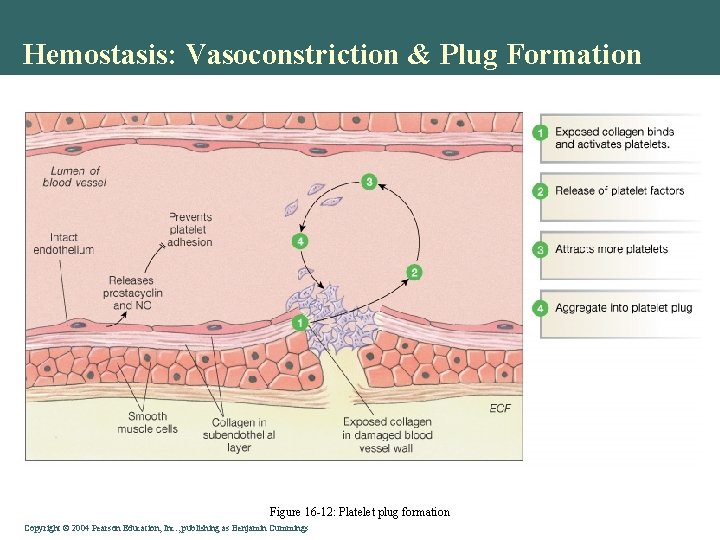
Hemostasis: Vasoconstriction & Plug Formation Figure 16 -12: Platelet plug formation Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
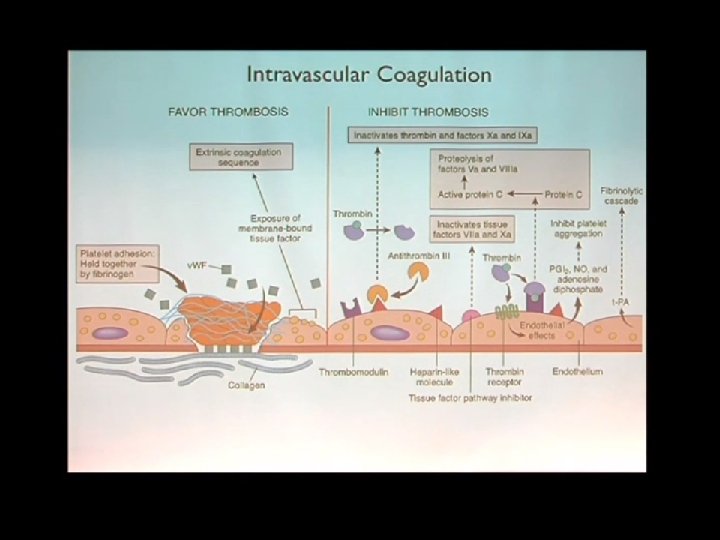
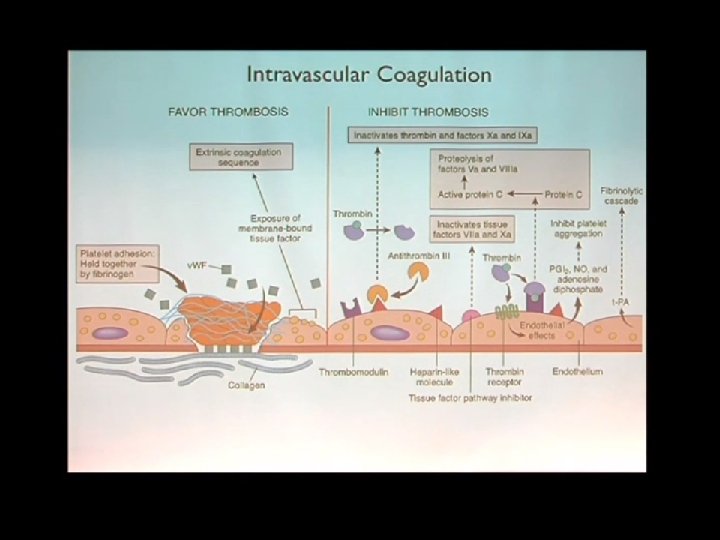
Hemostasis involves the interaction of: • Vascular Endothelium • Platelets • Coagulation Factors and • Fibrinolytic Proteins 23 Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
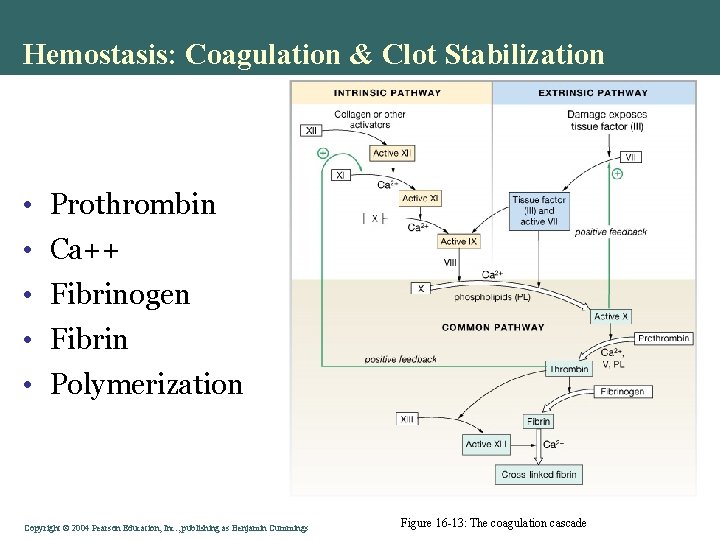
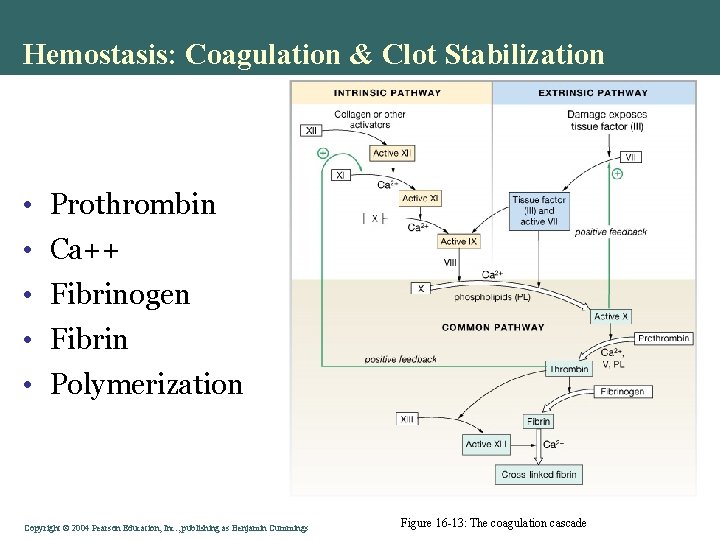
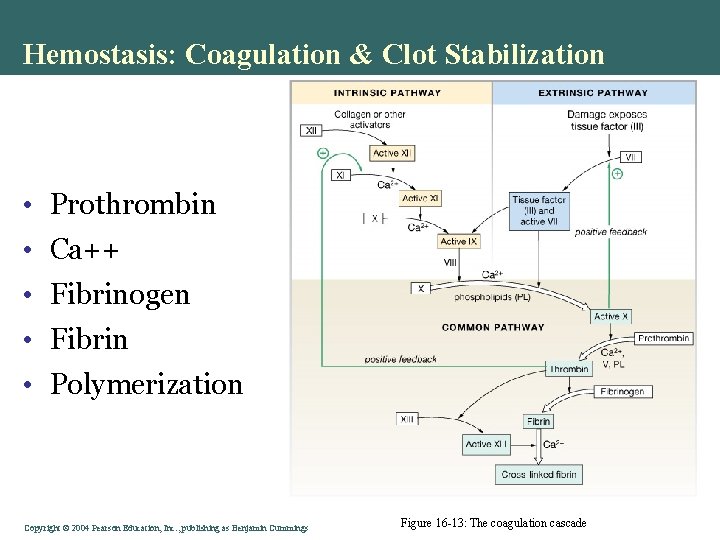
Hemostasis: Coagulation & Clot Stabilization • Prothrombin • Ca++ • Fibrinogen • Fibrin • Polymerization Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings Figure 16 -13: The coagulation cascade
Hemostasis has 2 main functions: 1. Induce a rapid & localized hemostatic plug at the site of vascular injury (clot formation) 2. Maintain Blood in a fluid, clot-free state after the injury is healed (clot dissolution) 25 Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
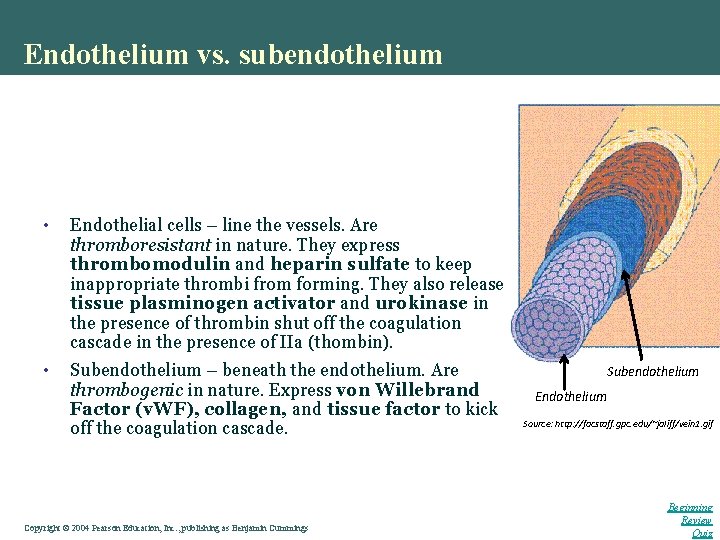
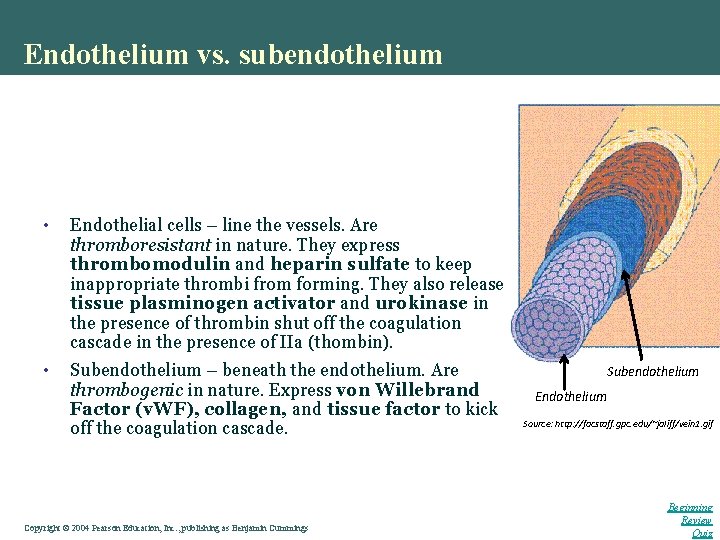
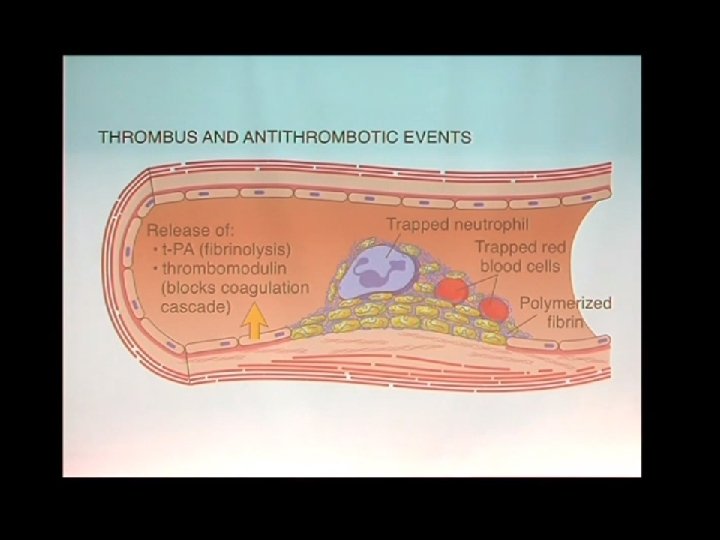
Endothelium vs. subendothelium • Endothelial cells – line the vessels. Are thromboresistant in nature. They express thrombomodulin and heparin sulfate to keep inappropriate thrombi from forming. They also release tissue plasminogen activator and urokinase in the presence of thrombin shut off the coagulation cascade in the presence of IIa (thombin). • Subendothelium – beneath the endothelium. Are thrombogenic in nature. Express von Willebrand Factor (v. WF), collagen, and tissue factor to kick off the coagulation cascade. Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings Subendothelium Endothelium Source: http: //facstaff. gpc. edu/~jaliff/vein 1. gif Beginning Review Quiz
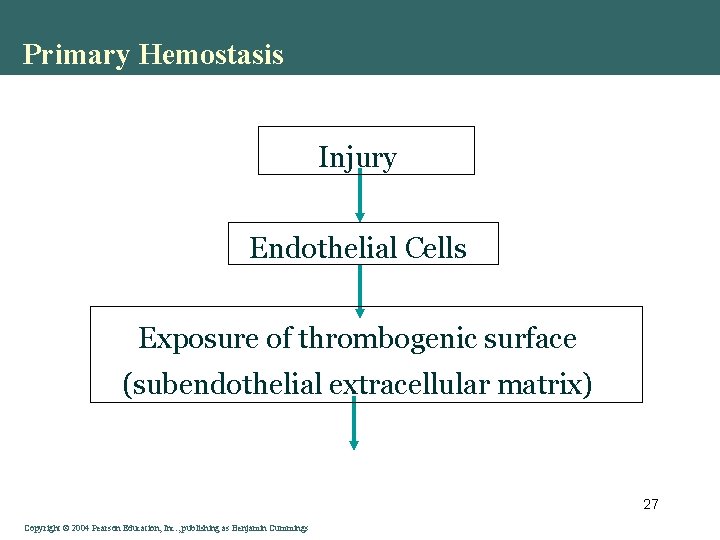
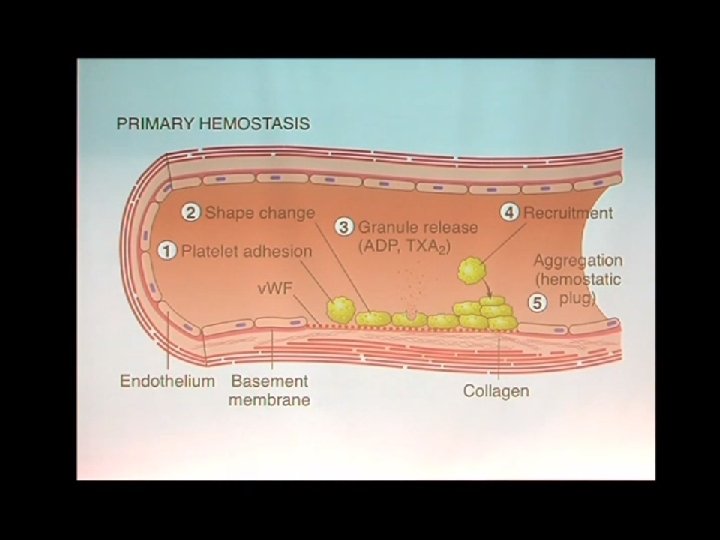
Primary Hemostasis Injury Endothelial Cells Exposure of thrombogenic surface (subendothelial extracellular matrix) 27 Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
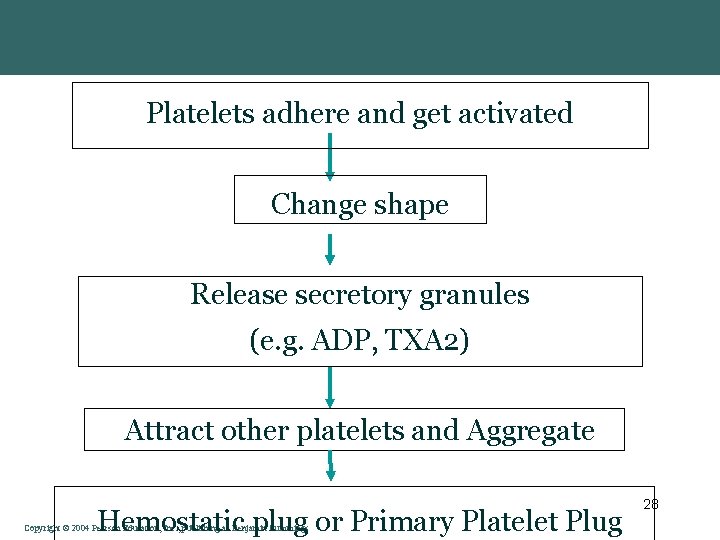
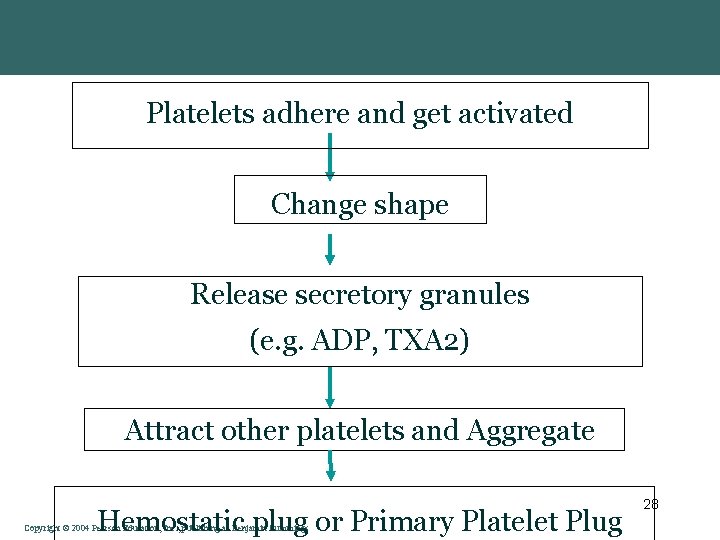
Platelets adhere and get activated Change shape Release secretory granules (e. g. ADP, TXA 2) Attract other platelets and Aggregate Hemostatic plug or Primary Platelet Plug Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings 28
Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
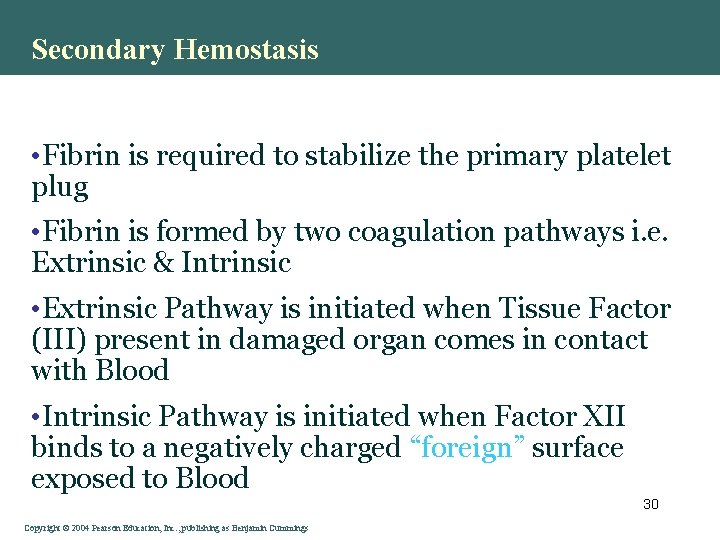
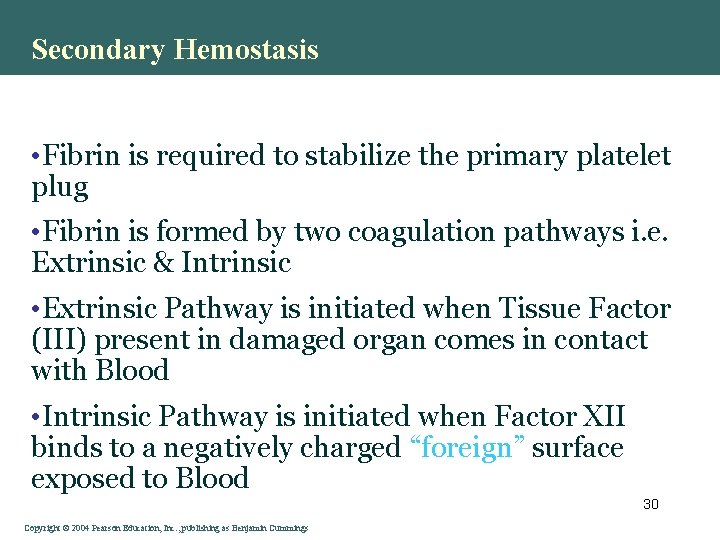
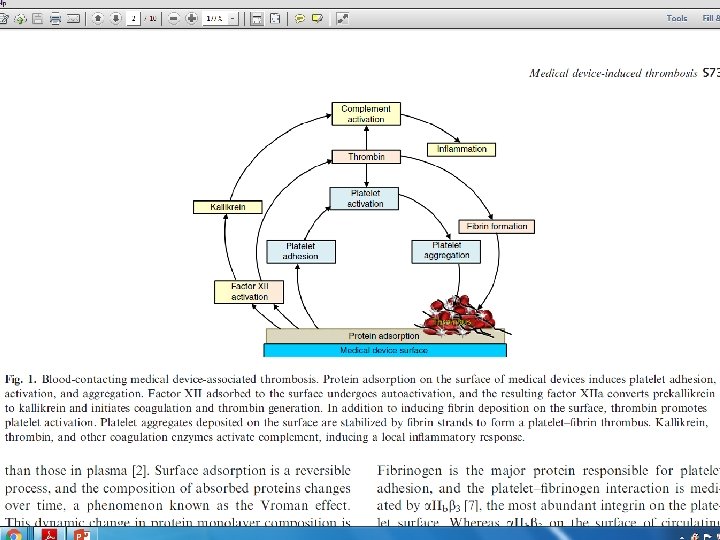
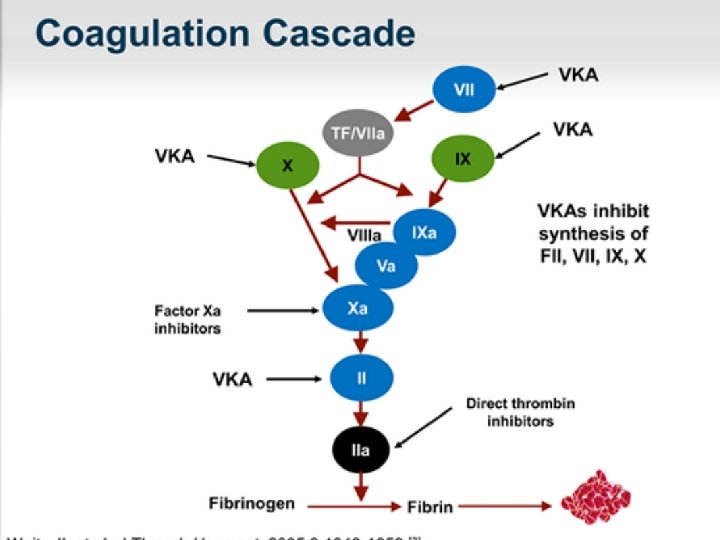
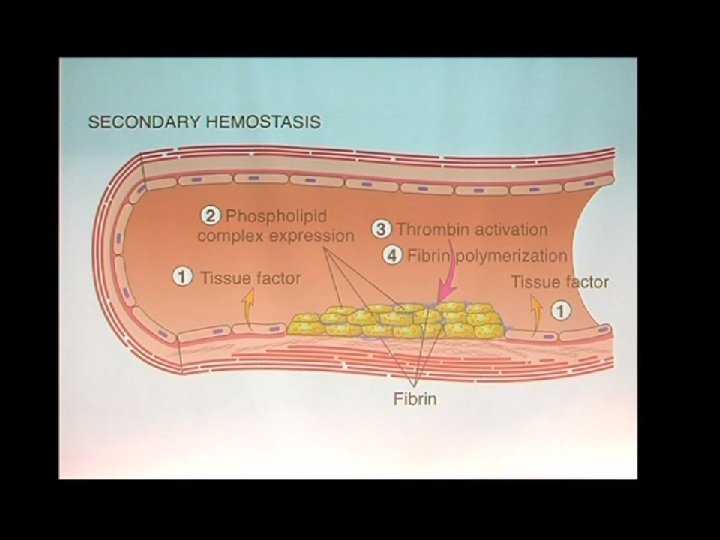
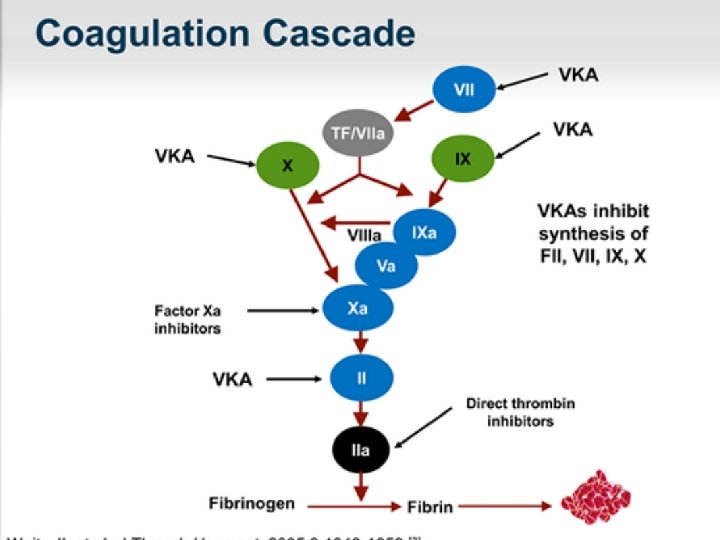
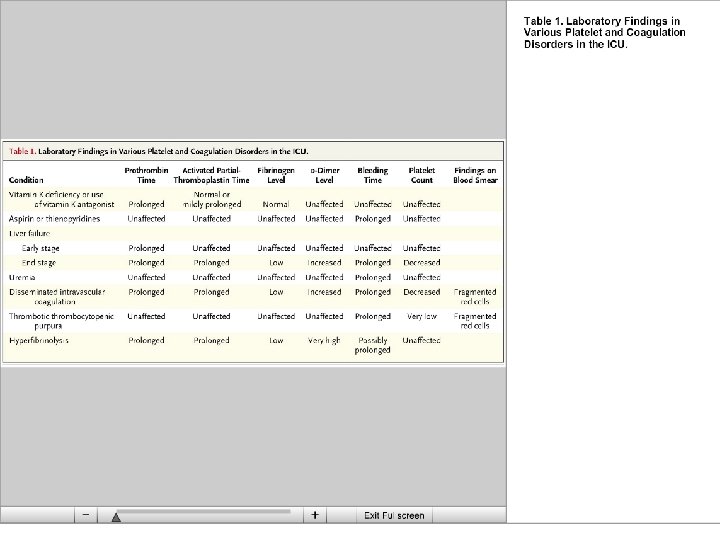
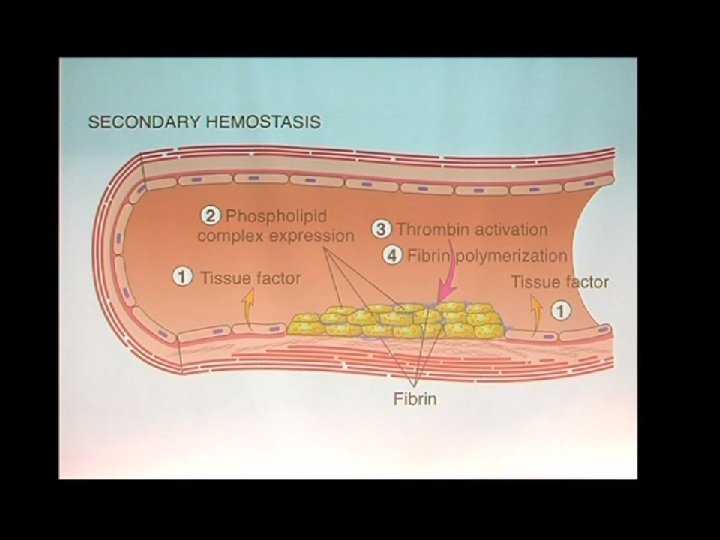
Secondary Hemostasis • Fibrin is required to stabilize the primary platelet plug • Fibrin is formed by two coagulation pathways i. e. Extrinsic & Intrinsic • Extrinsic Pathway is initiated when Tissue Factor (III) present in damaged organ comes in contact with Blood • Intrinsic Pathway is initiated when Factor XII binds to a negatively charged “foreign” surface exposed to Blood 30 Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
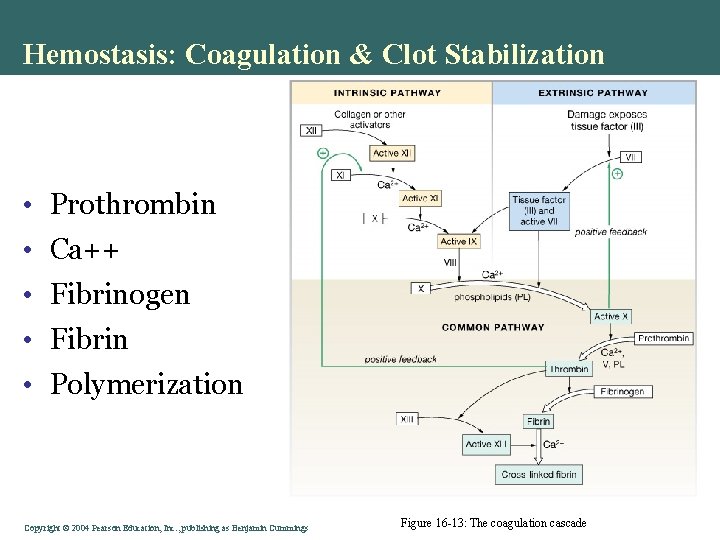
Hemostasis: Coagulation & Clot Stabilization • Prothrombin • Ca++ • Fibrinogen • Fibrin • Polymerization Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings Figure 16 -13: The coagulation cascade
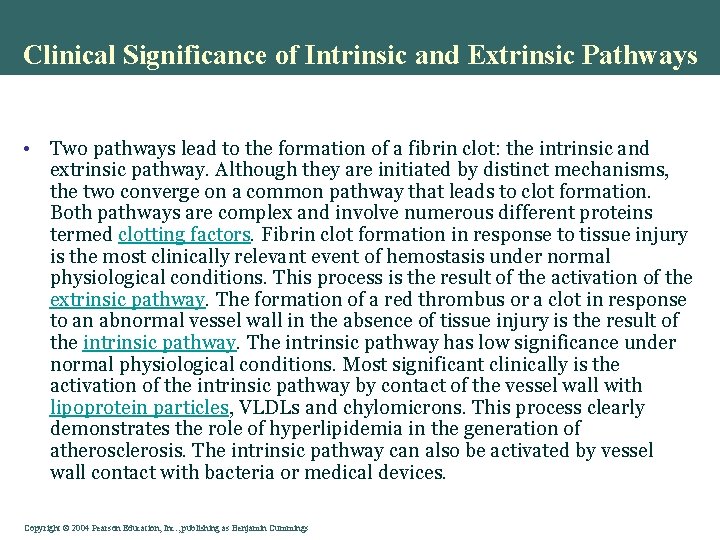
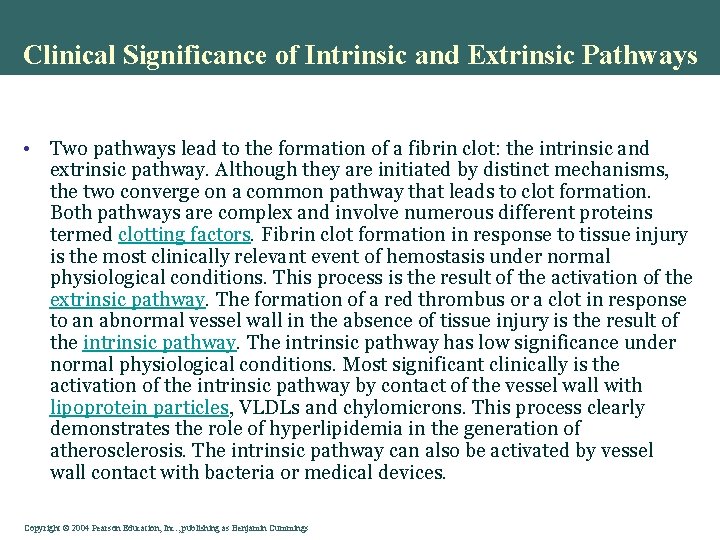
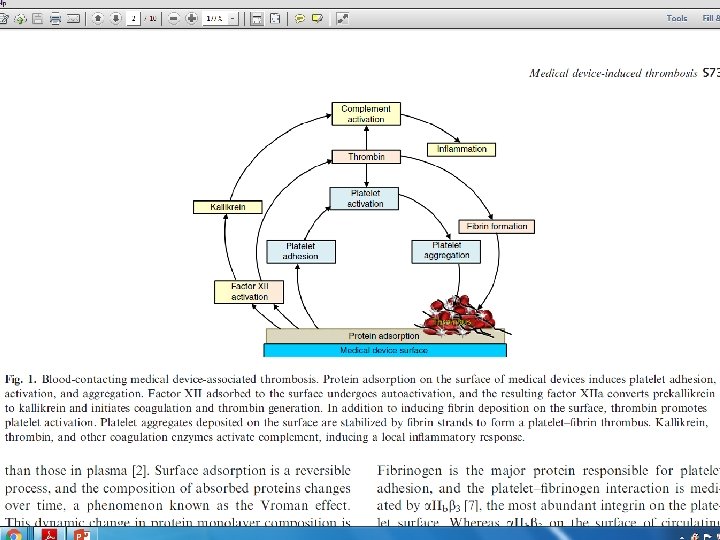
Clinical Significance of Intrinsic and Extrinsic Pathways • Two pathways lead to the formation of a fibrin clot: the intrinsic and extrinsic pathway. Although they are initiated by distinct mechanisms, the two converge on a common pathway that leads to clot formation. Both pathways are complex and involve numerous different proteins termed clotting factors. Fibrin clot formation in response to tissue injury is the most clinically relevant event of hemostasis under normal physiological conditions. This process is the result of the activation of the extrinsic pathway. The formation of a red thrombus or a clot in response to an abnormal vessel wall in the absence of tissue injury is the result of the intrinsic pathway. The intrinsic pathway has low significance under normal physiological conditions. Most significant clinically is the activation of the intrinsic pathway by contact of the vessel wall with lipoprotein particles, VLDLs and chylomicrons. This process clearly demonstrates the role of hyperlipidemia in the generation of atherosclerosis. The intrinsic pathway can also be activated by vessel wall contact with bacteria or medical devices. Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
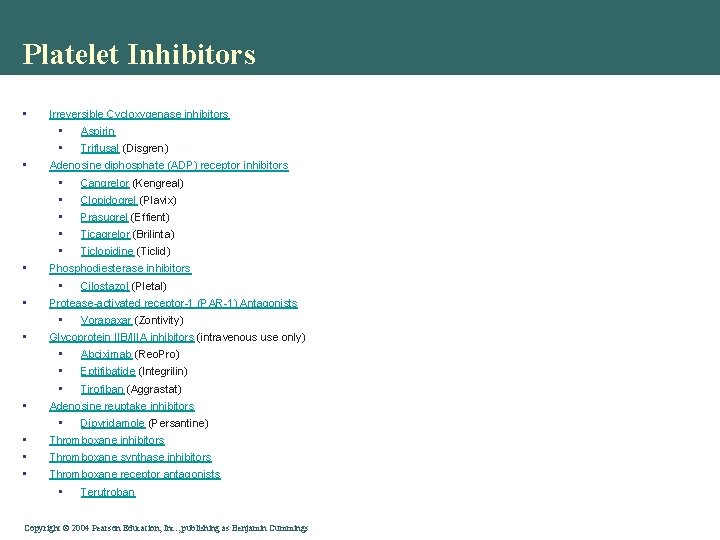
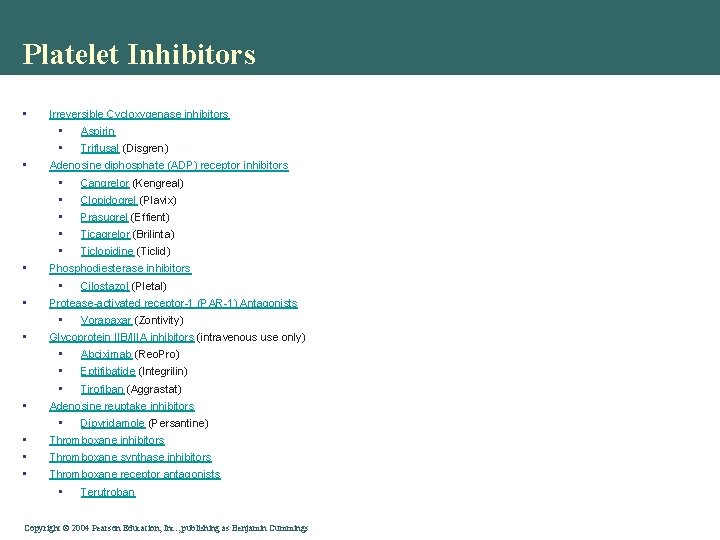
Platelet Inhibitors • • • Irreversible Cycloxygenase inhibitors • Aspirin • Triflusal (Disgren) Adenosine diphosphate (ADP) receptor inhibitors • Cangrelor (Kengreal) • Clopidogrel (Plavix) • Prasugrel (Effient) • Ticagrelor (Brilinta) • Ticlopidine (Ticlid) Phosphodiesterase inhibitors • Cilostazol (Pletal) Protease-activated receptor-1 (PAR-1) Antagonists • Vorapaxar (Zontivity) Glycoprotein IIB/IIIA inhibitors (intravenous use only) • Abciximab (Reo. Pro) • Eptifibatide (Integrilin) • Tirofiban (Aggrastat) Adenosine reuptake inhibitors • Dipyridamole (Persantine) Thromboxane inhibitors Thromboxane synthase inhibitors Thromboxane receptor antagonists • Terutroban Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
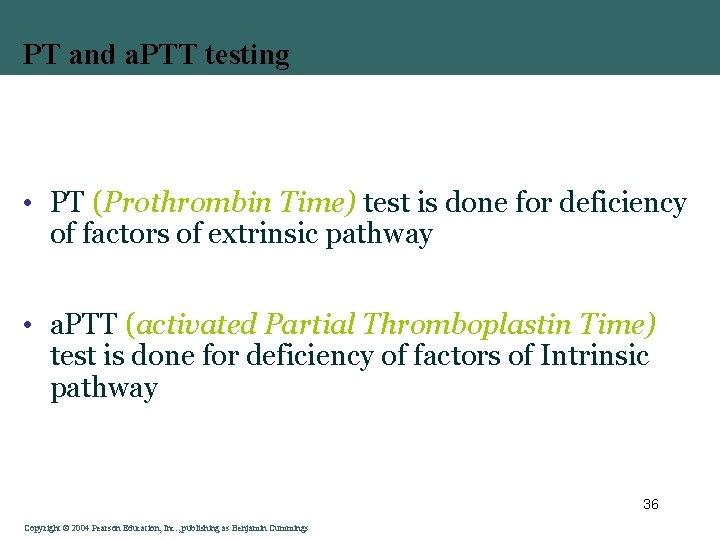
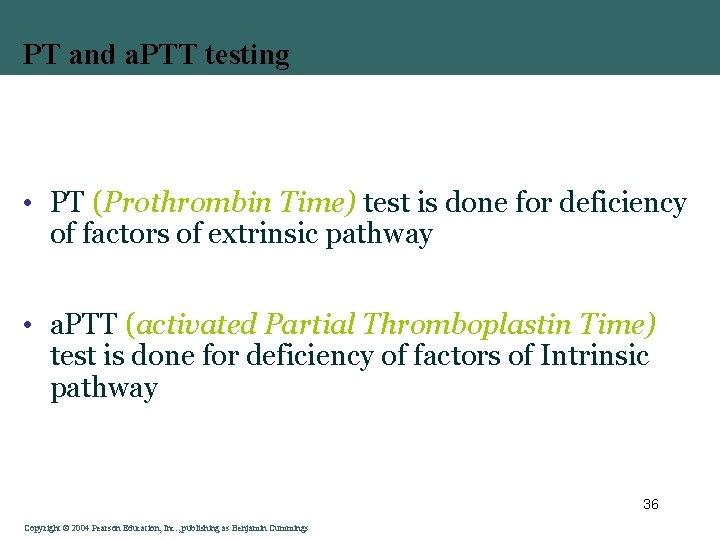
PT and a. PTT testing • PT (Prothrombin Time) test is done for deficiency of factors of extrinsic pathway • a. PTT (activated Partial Thromboplastin Time) test is done for deficiency of factors of Intrinsic pathway 36 Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
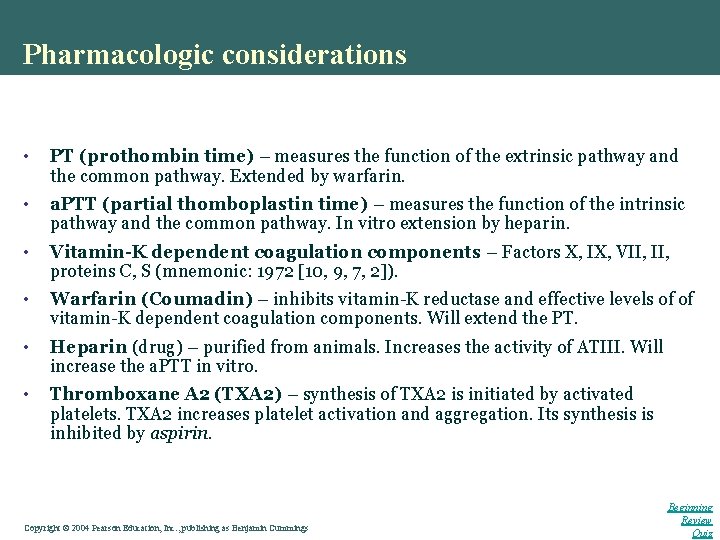
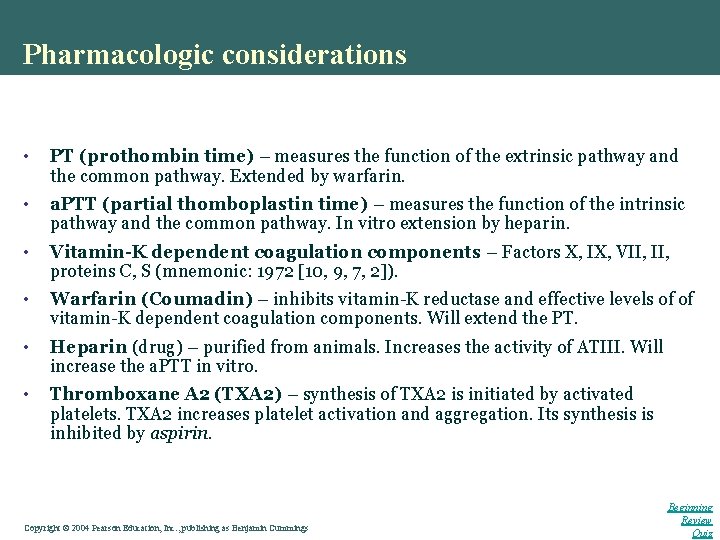
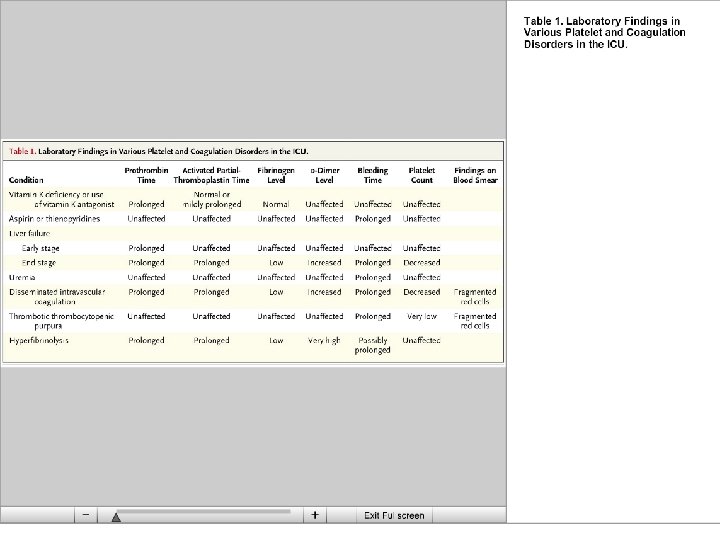
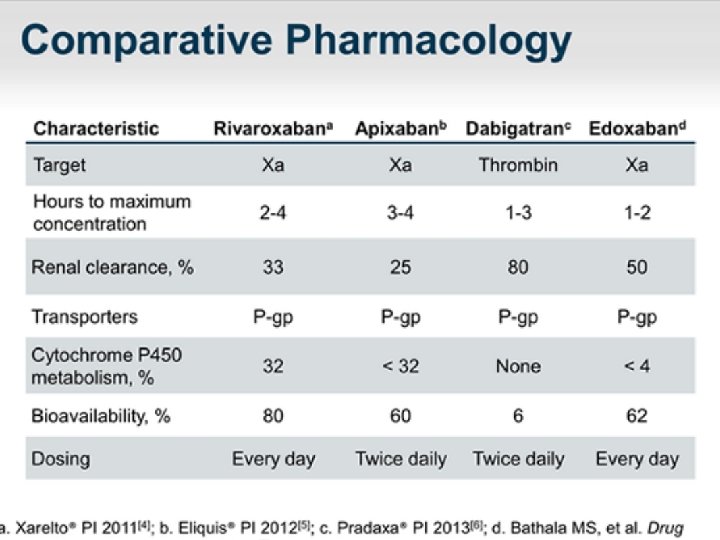
Pharmacologic considerations • PT (prothombin time) – measures the function of the extrinsic pathway and the common pathway. Extended by warfarin. • a. PTT (partial thomboplastin time) – measures the function of the intrinsic pathway and the common pathway. In vitro extension by heparin. • Vitamin-K dependent coagulation components – Factors X, IX, VII, proteins C, S (mnemonic: 1972 [10, 9, 7, 2]). • Warfarin (Coumadin) – inhibits vitamin-K reductase and effective levels of of vitamin-K dependent coagulation components. Will extend the PT. • Heparin (drug) – purified from animals. Increases the activity of ATIII. Will increase the a. PTT in vitro. • Thromboxane A 2 (TXA 2) – synthesis of TXA 2 is initiated by activated platelets. TXA 2 increases platelet activation and aggregation. Its synthesis is inhibited by aspirin. Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings Beginning Review Quiz
Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
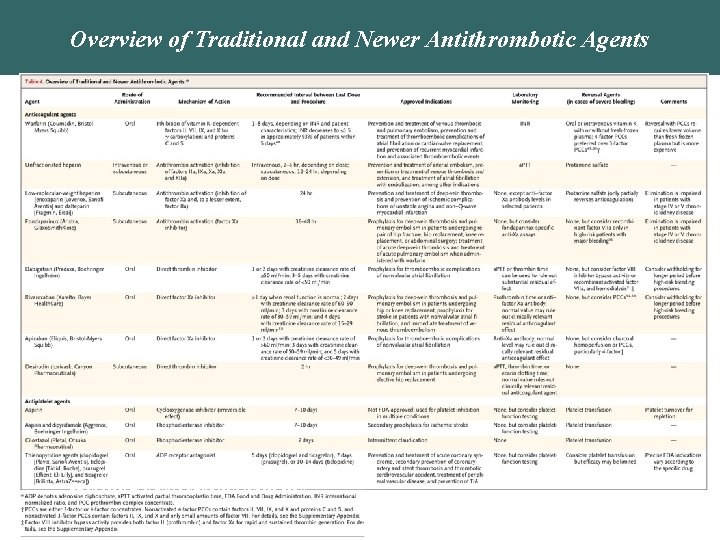
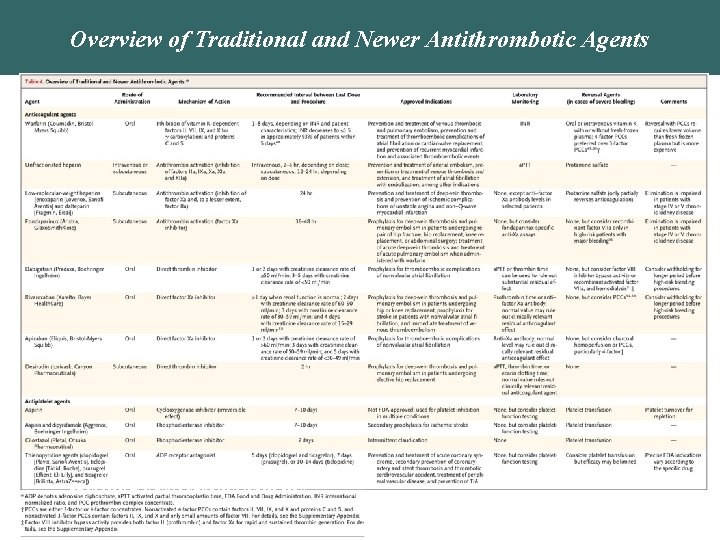
Overview of Traditional and Newer Antithrombotic Agents Baron TH et al. N Engl J Med 2013; 368: 2113 -2124. Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
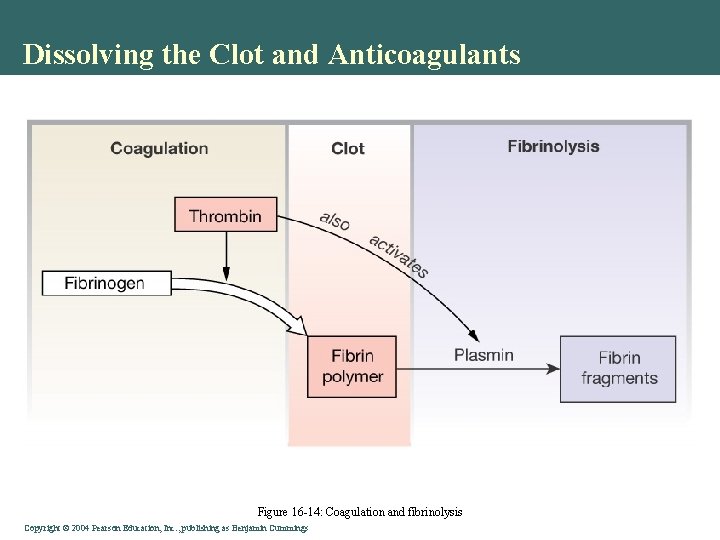
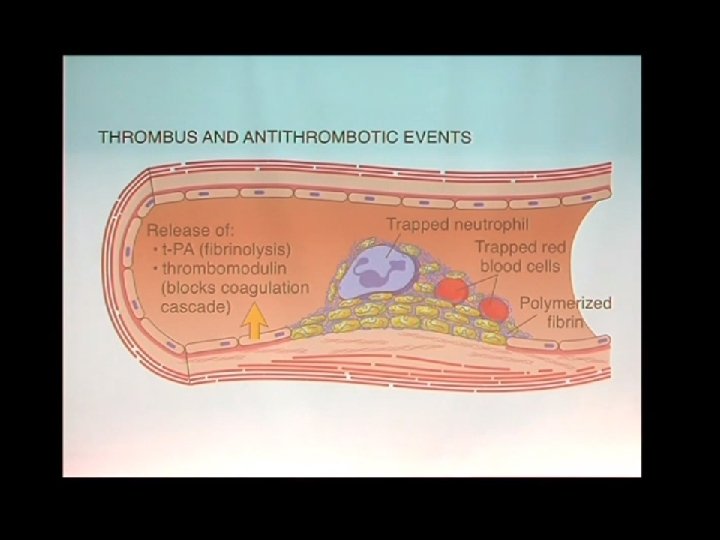
Dissolving the Clot and Anticoagulants • Bleeding stopped • Vessel repair • Plasmin • Fibrinolysis • Clot dissolved Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
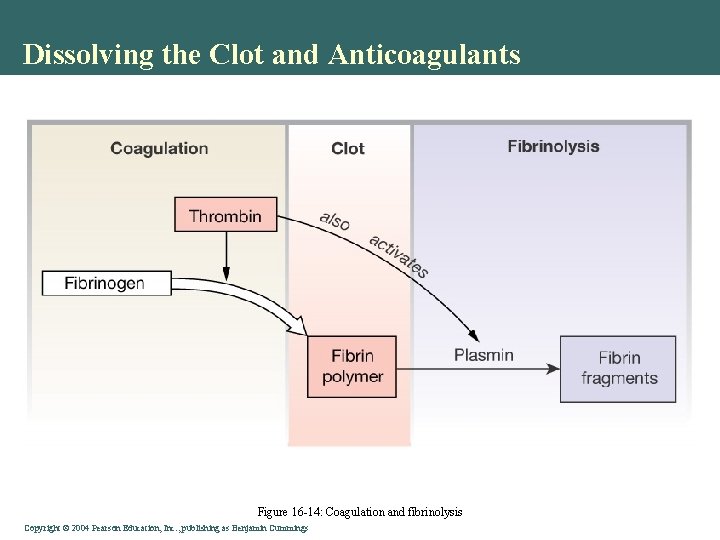
Dissolving the Clot and Anticoagulants Figure 16 -14: Coagulation and fibrinolysis Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
Fibrinolysis • As soon as the injury is healed clot dissolution starts, to restore the normal flow of Blood • Plasminogen is converted to the active form Plasmin by 2 distinct Plasminogen Activators (PAs): • tissue plasminogen activator (t-PA) from injured endothelial cells • Urokinase from Kidney endothelial cells and plasma 50 Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
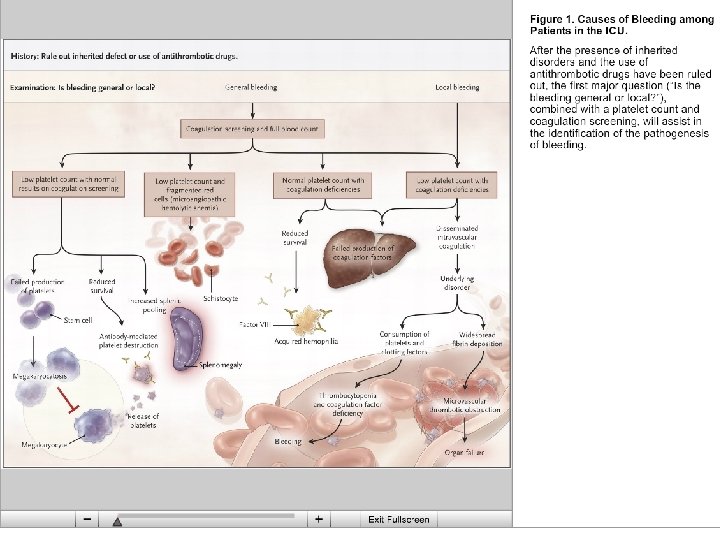
Coagulation and Disease • Hemophilia • Cardiovascular Diseases • Key problem – clots block undamaged blood vessels • Anticoagulants prevent coagulation • Keep platelets from adhering • Prevent fibrin coagulation • "Clot Busters": Prevent further clotting • Speed fibrinolysis • Limit tissue damage (heart, brain…) Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
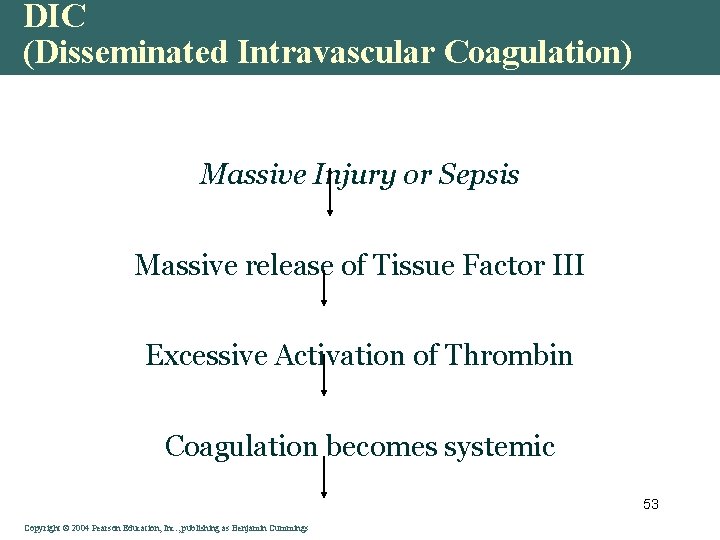
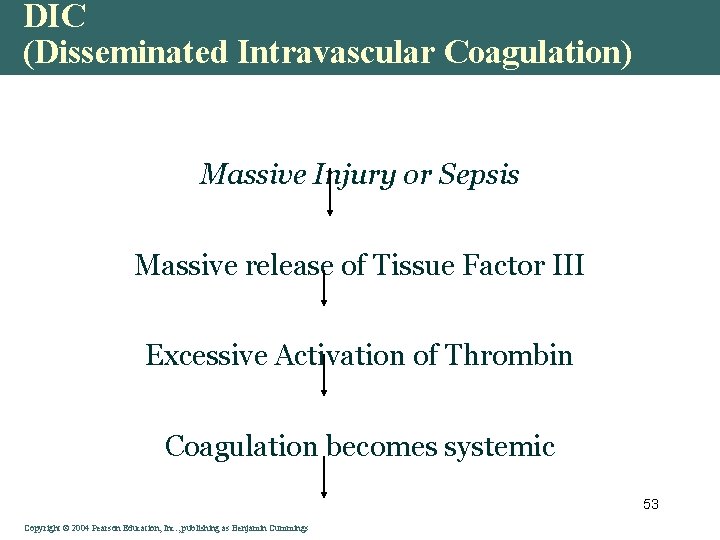
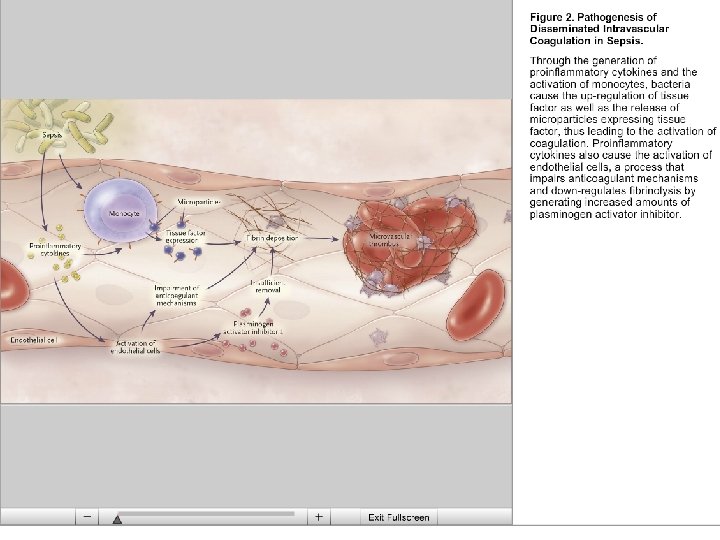
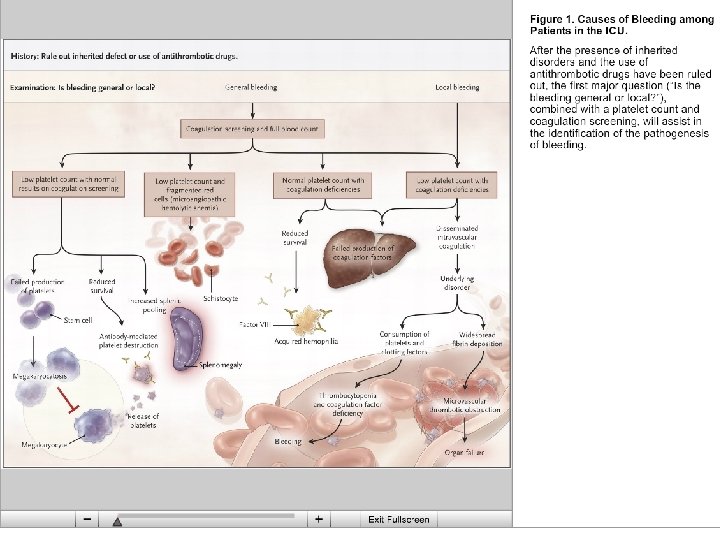
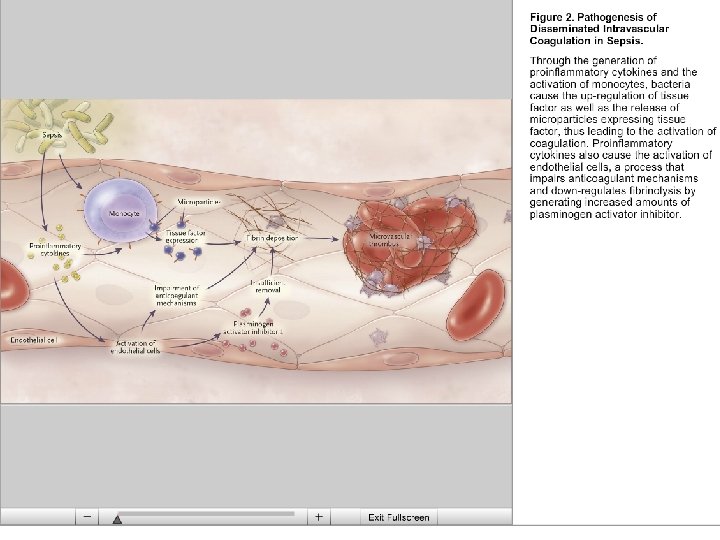
DIC (Disseminated Intravascular Coagulation) Massive Injury or Sepsis Massive release of Tissue Factor III Excessive Activation of Thrombin Coagulation becomes systemic 53 Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
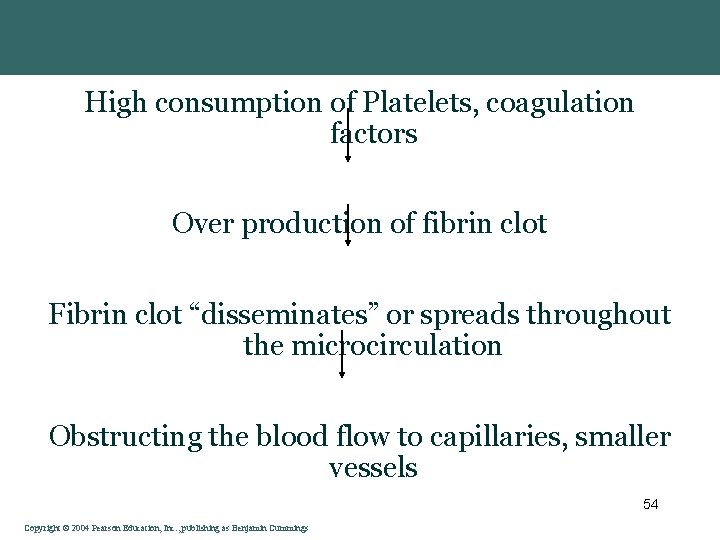
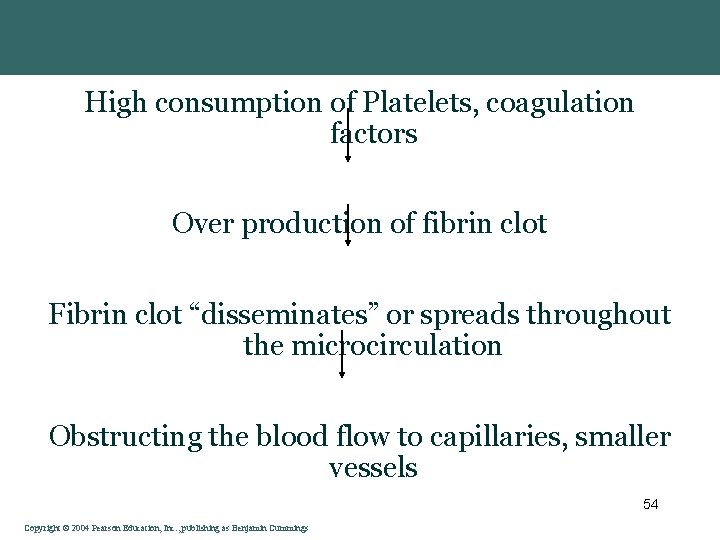
High consumption of Platelets, coagulation factors Over production of fibrin clot Fibrin clot “disseminates” or spreads throughout the microcirculation Obstructing the blood flow to capillaries, smaller vessels 54 Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
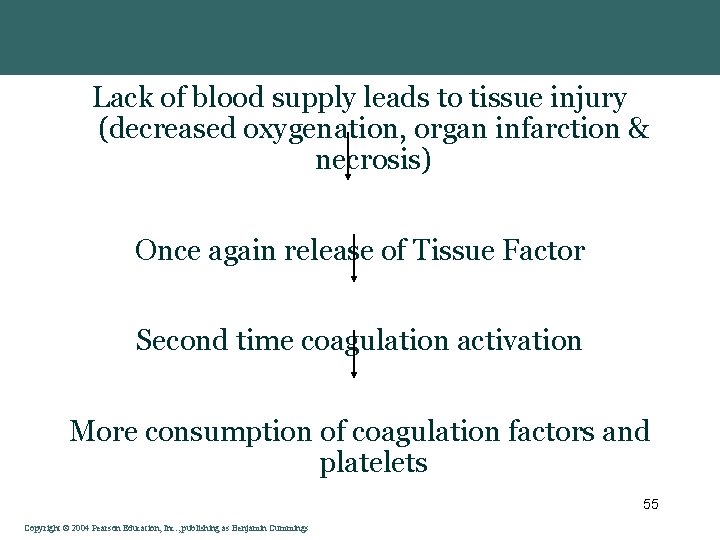
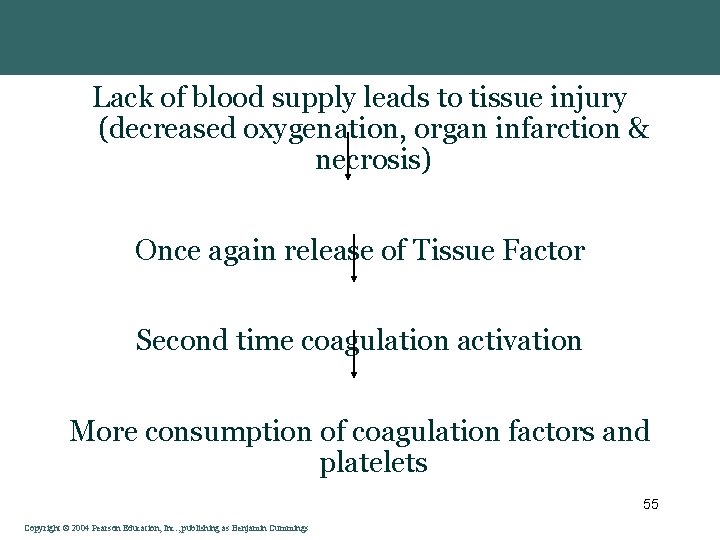
Lack of blood supply leads to tissue injury (decreased oxygenation, organ infarction & necrosis) Once again release of Tissue Factor Second time coagulation activation More consumption of coagulation factors and platelets 55 Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings
Summary • Blood is about 50% plasma, water solvent & solutes: ions, elements, gases, proteins, wastes & nutrients • White blood cells function in internal defense • Iron in hemoglobin is key to RBC transport of O 2 • Platelet activation initiates clot formation • Clotting prevents blood loss but is a problem in cardiovascular disease Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings