Think Delirium Scottish Delirium Association Pathway Overview Sharing


- Slides: 29
Think Delirium Scottish Delirium Association Pathway Overview & Sharing Good Practice Linda Wolff Mike Hendrix, NHS Forth Valley
Improving detection and Management of delirium in hip fracture Experience in Forth valley orthopoedic unit Linda Wolff Mike Hendrix
Outline • Where are we now? • Where do we want to be? • How are we trying to get there?
Why Bother? • National Priority • Delirium present in up to 60% patients over 65 with hip fracture • 3 rd busiest ortho unit in Scotland • 380 hip fracture patients/ year • Pressure on beds • Staffing challenges
Delirium Outcomes • • • Delirium present in up to 60% patients Length of stay x 3 40% mortality High morbidity Stress
Patients and carers say… • Said he was being difficult • Said she has dementia • • They didn’t explain Took her food away Too much medication I was so worried
Where do we want to be? Reliable recognition and management of delirium in patients with hip fracture
How are we trying to get there? • Steering group • Questionnaires- staff • Patient stories • Identification of delirium • Develop management protocol
Protocol • AMT 10 • CAM • • Medical Pain Management Nursing Discharge
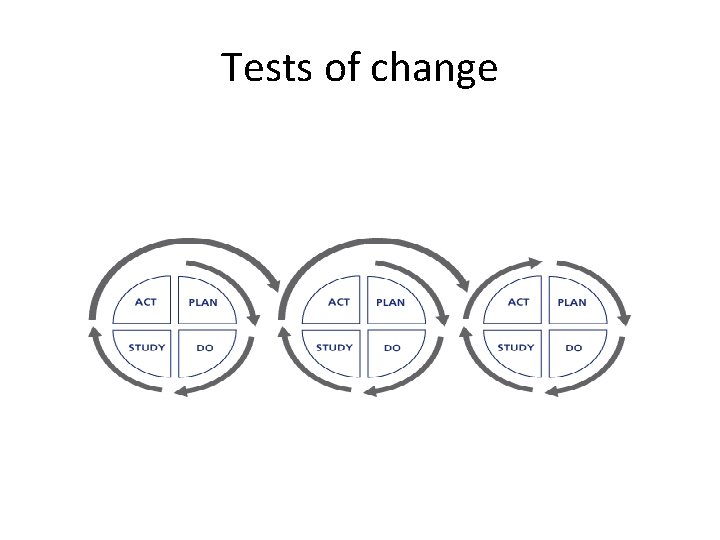
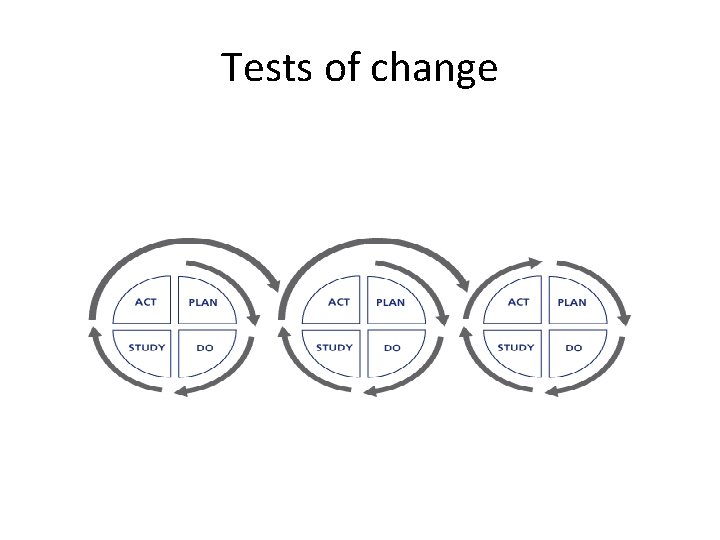
Tests of change
Training • All nursing staff • Hospital Delirium Study Days • Presentations to ortho surgeons


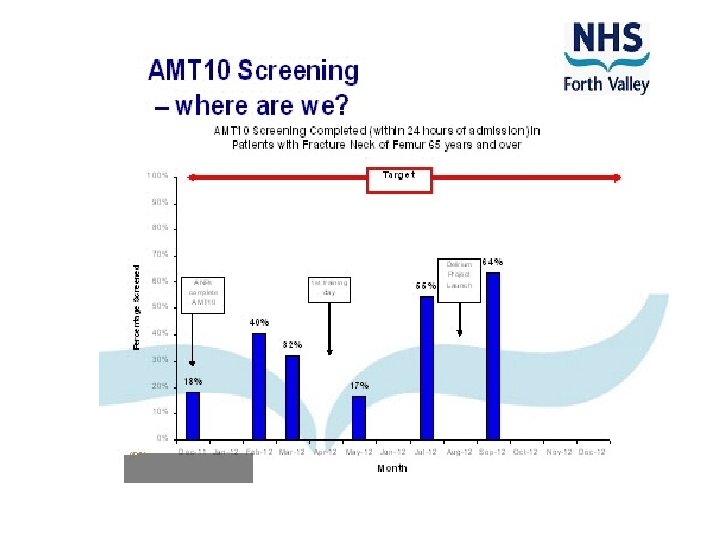
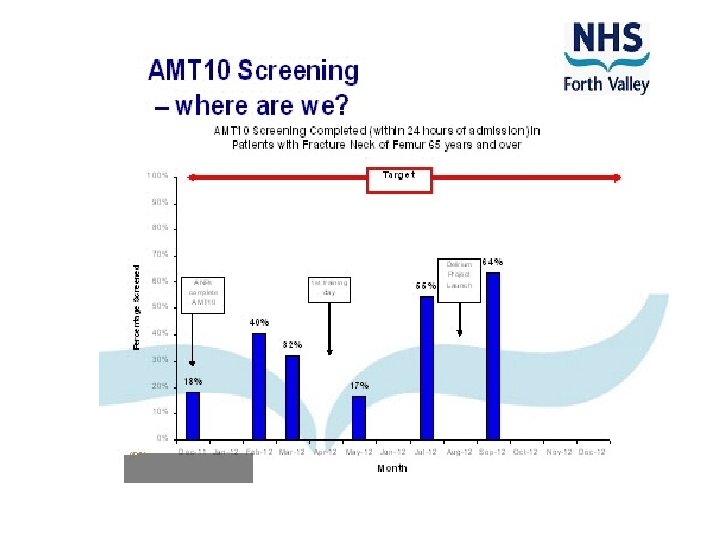
AMT 10 • • • Who will do it ? Junior docs, staff nurse, ANPs Audit Flow chart Screen saver
Think Delirium!
Untreated delirium can increase length of stay up to 3 times
Think Delirium!
Any one of these can cause delirium: • • Infection Fracture Pain Mental stress Constipation Dehydration Low oxygen levels Morphine
How are we doing?
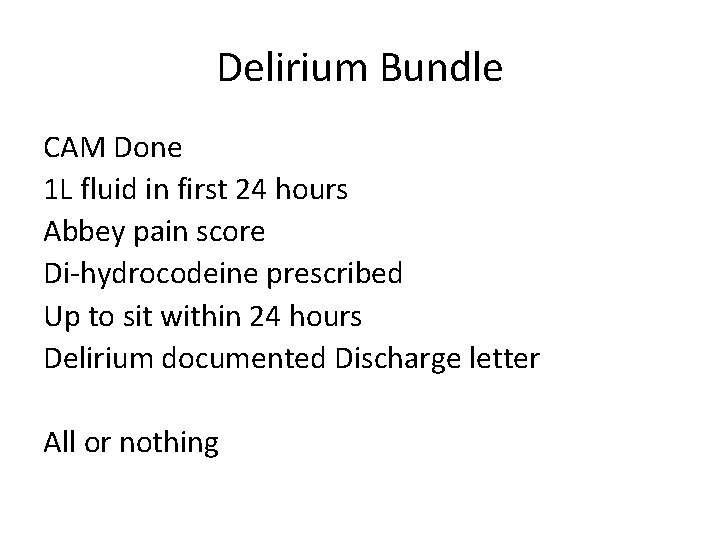
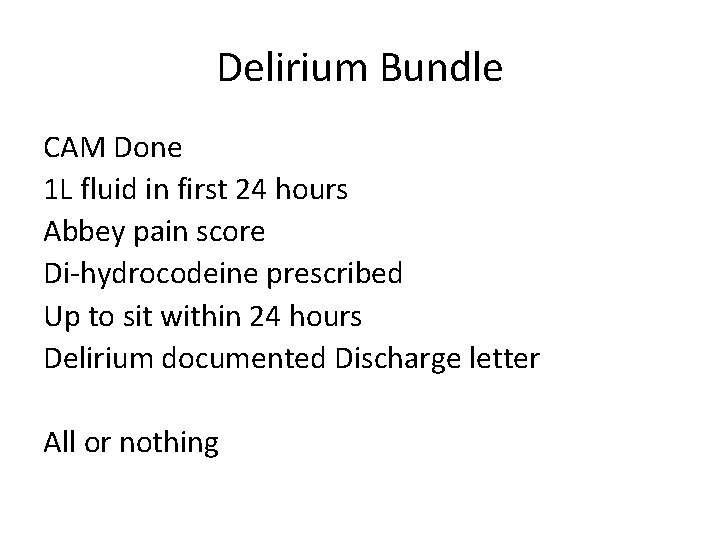
Delirium Bundle CAM Done 1 L fluid in first 24 hours Abbey pain score Di-hydrocodeine prescribed Up to sit within 24 hours Delirium documented Discharge letter All or nothing
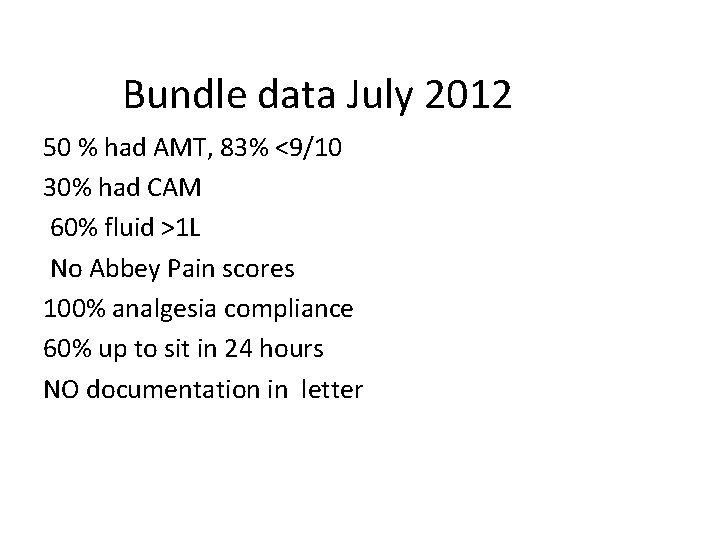
Bundle data July 2012 50 % had AMT, 83% <9/10 30% had CAM 60% fluid >1 L No Abbey Pain scores 100% analgesia compliance 60% up to sit in 24 hours NO documentation in letter
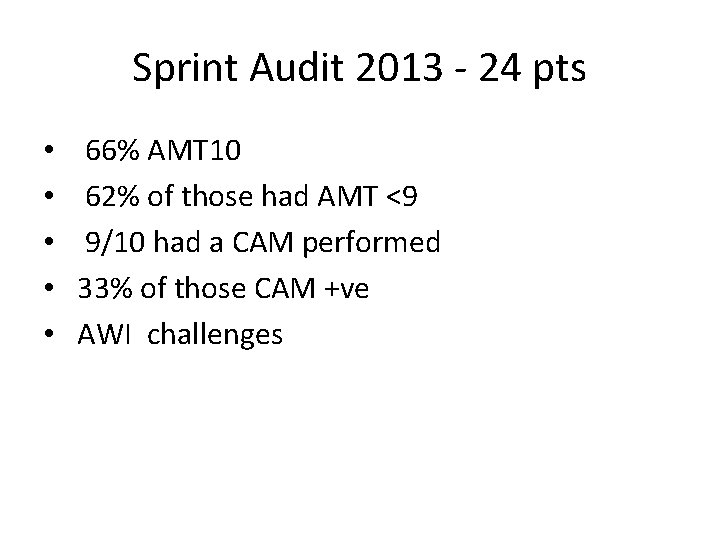
Sprint Audit 2013 - 24 pts • • • 66% AMT 10 62% of those had AMT <9 9/10 had a CAM performed 33% of those CAM +ve AWI challenges
Successes • • Improved cognitive assessment Improved staff knowledge More consistent pain management Increased documentation of delirium Introduction of butterfly scheme Carer’s letter to CE Mike feel free to add…
Challenges • • • Cognitive assessment / detection Delirium Bundle just starting AWI irregularities Engage all medical staff Evaluation LOS, complaints, questionnaires, discharge documentation