Thi Qar college of Medicine Family Community medicine









- Slides: 42

Thi. Qar college of Medicine Family & Community medicine dept. 4 th stage by: Dr. Muslim N. Saeed Monday March 18 th , 2019
Care of the Elderly Patient Geriatric medicine is mainly concerned with people over the age of 75, although most ‘geriatric’ patients are much older. Many of these have several complex, interacting medical and psychosocial problems which affect their function and independence.

Geriatric medicine involves dealing with acute illness, chronic disease and rehabilitation, working in multidisciplinary teams in the community and in hospitals, medical education and research.
-Older patients often have comorbidities, “polypharmacy, ” and psychological, social, and functional impairments. -The main goal is to assist elderly persons to maintain function and quality of life.
Age-related differences There are important differences in the physiology and presentation of older people that every clinician needs to know about. 1 -Multiple pathology Older people commonly present with more than one problem, usually with a number of causes. . urinary tract infection, aspirin-induced gastritis and aortic sclerosis. Never stop at a single unifying diagnosis – always consider several.
2 -Atypical presentation Older people commonly present with ‘general deterioration’ or functional decline. Acute disease is often masked but precipitates functional impairment in other areas. Therefore atypical presentations such as falls, confusion or reduced mobility are not social problems – they are medical problems.
3 -Reduced homeostatic reserve Ageing is associated with: -decline in organ function with a reduced ability to compensate. -increase heart rate and cardiac output. -Renal failure due to medications or illness. -electrolyte imbalances. -thermoregulation may also be impaired.
4 -Impaired immunity -Older people do not necessarily have a raised white cell count or a fever with infection , hypothermia may occur instead. -Measuring the serum C-reactive protein can be useful when screening for infection in an older person who is non-specifically unwell.

5 -Some clinical findings are not necessarily pathological Neck stiffness, a positive urine dipstick in women, mild crackles at the bases of the lungs, a slightly reduced Pa. O 2 and reduced skin turgor may be normal findings in older people and do not always indicate disease.
6 -The importance of functional assessment and rehabilitation Older people may take longer to recover from illness (e. g. pneumonia) compared with younger people. 7 -Ethics Geriatric medicine involves balancing the right to gain a high-quality care without age discrimination with avoiding aggressive and futile interventions.
Comprehensive geriatric assessment is the assessment of a patient made by a team which includes a geriatrician or Family Physician. It covers the following areas: • medical diagnoses • review of medicines and concordance with drug therapy • social circumstances • assessment of cognitive function and mood • functional ability (i. e. ability to perform activities of daily living. • environment • economic circumstances.
Rehabilitation is an important aspect of geriatric medicine. Many older patients now have rehabilitation in intermediate care facilities or in their own homes. However, some of these patients undergo rehabilitation without the benefit of a comprehensive geriatric assessment, so that the opportunity for diagnosis, treatment and optimum rehabilitation may be lost.
Geriatric Assessment -medical -Functional -Psychological -social.
Goals of Geriatric Assessment 1. Focus on preventive medicine rather than acute medicine. 2. Focus on improving or maintaining functional ability and not necessarily on a “cure. ” 3. Provide a long-term solution for “difficult to manage” patients with multiple physicians, recurrent emergency department visits, and hospital admissions with poor follow-up. 4. Aid in the diagnosis of health-related problems.
5. Develop plans for treatment and follow-up care. 6. Establish plans for coordination of care. 7. Determine the need and site of long-term care as appropriate. 8. Determine optimal use of health care resources. 9. Prevent readmission into the hospital.
Medical Assessment Includes: -a review of the patient’s medical record -medication history (past and present) -nutritional evaluation. *On average, elderly patients have four to six diagnosable disorders, which may require the use of several medications. *Review of the patient’s medical record should focus on conditions that are more common in the elderly (geriatric syndromes) and in particular their risk factors.
Four shared risk factors identified in elderly: -older age -cognitive impairment -functional impairment -impaired mobility The five most common geriatric syndromes pressure ulcers, incontinence, falls, functional decline, and delirium.
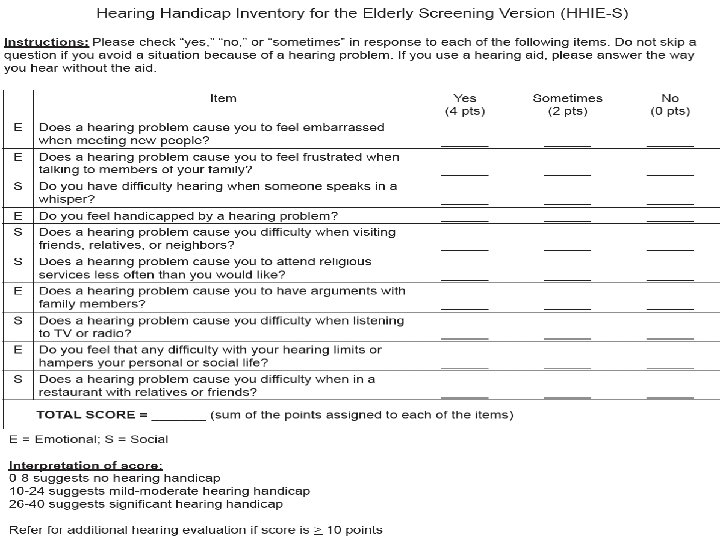
During the medical assessment: -the review of systems should be completed with special emphasis on sensory impairment, dentition, mood, memory, urinary symptoms, falls, nutrition, and pain. -Also recommends routine screening for visual and hearing impairment. -Hearing loss is a prevalent chronic condition, also hypertension and arthritis, and its prevalence and severity increase with age.
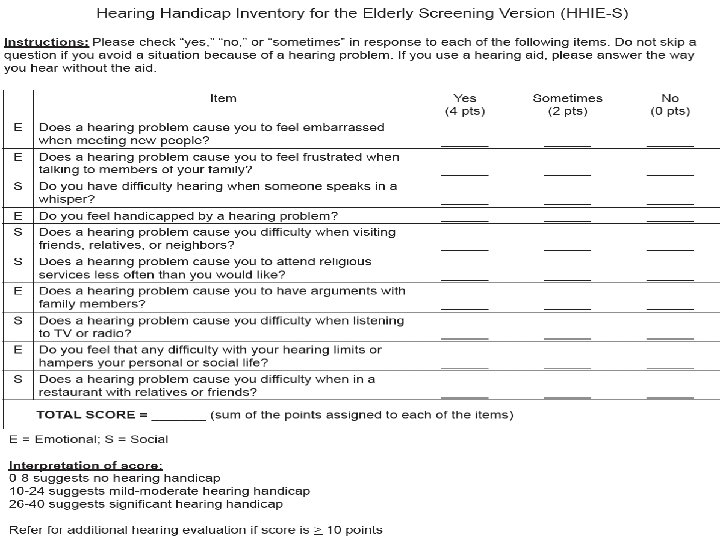
-Audiologic evaluation should be offered to any patient who fails a hearing screening, to assist in determining the need for further testing or management, including hearing aid, medical treatment, or surgical intervention.
Review of the patient’s current medication list, including 1 -over-the-counter (OTC) medications 2 -drug allergies 3 -previous adverse drug reactions *Adverse drug reactions (ADRs, adverse drug events) are a significant public health issue, especially in the elderly population. *Poly-pharmacy is defined as taking more than five medications and is an independent risk factor for both delirium and falls. *All the patient’s prescription medications and supplements seen at the initial visit and periodically thereafter.
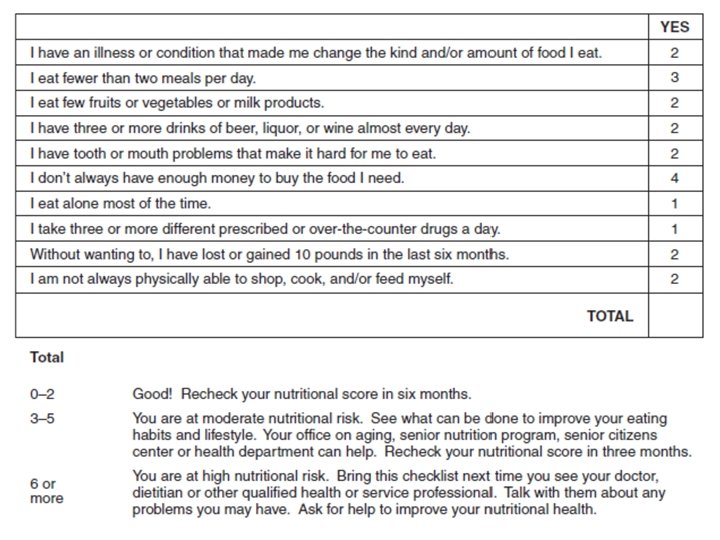
Nutritional evaluation is an integral part of the geriatric assessment. The type, quantity, and frequency of food eaten should be determined. Malnutrition and under nutrition can lead to health problems that include delayed healing and longer hospital stays. A reliable marker of nutritional problems is weight loss, specifically, more than 5% in the past month and 10% or greater weight loss in the last 6 months.
Clinicians should ask about any special diets (e. g. , low carbohydrate, vegetarian, low salt) or self prescribed “fad” diets. Additional questioning should include weight loss and change of fit in clothing; amount of money spent on food; and accessibility of grocers with a variety of fresh foods.
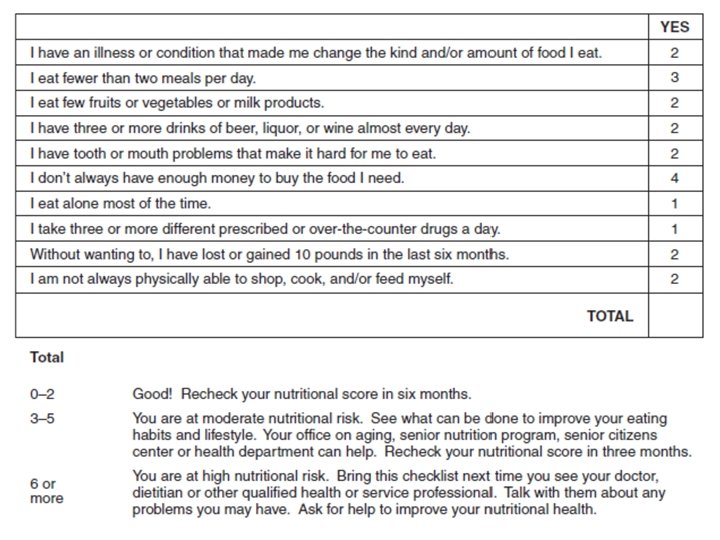
The ability to chew and swallow should also be evaluated. It may be impaired by xerostomia (dryness of mouth), which is common in elderly persons.
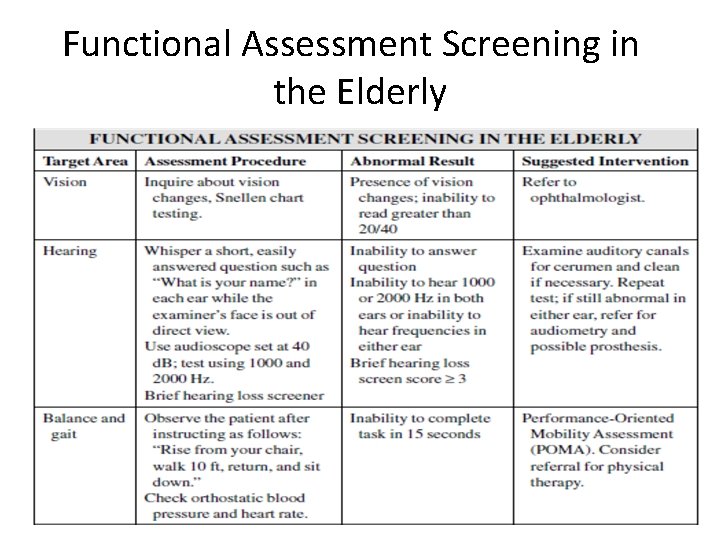
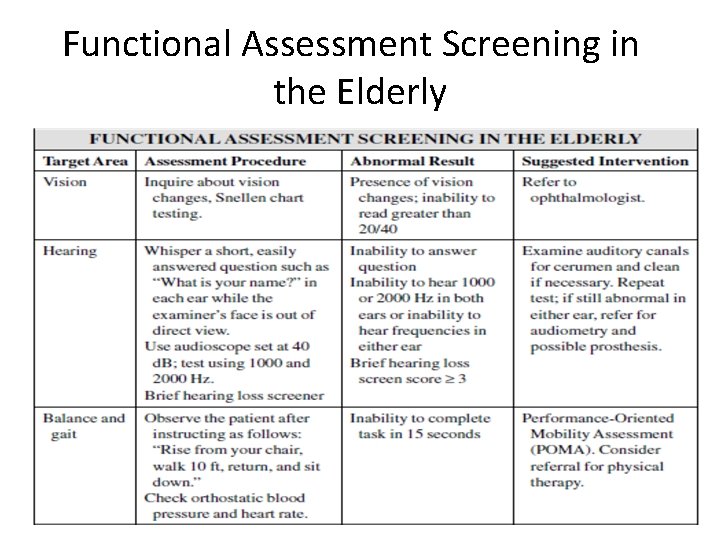
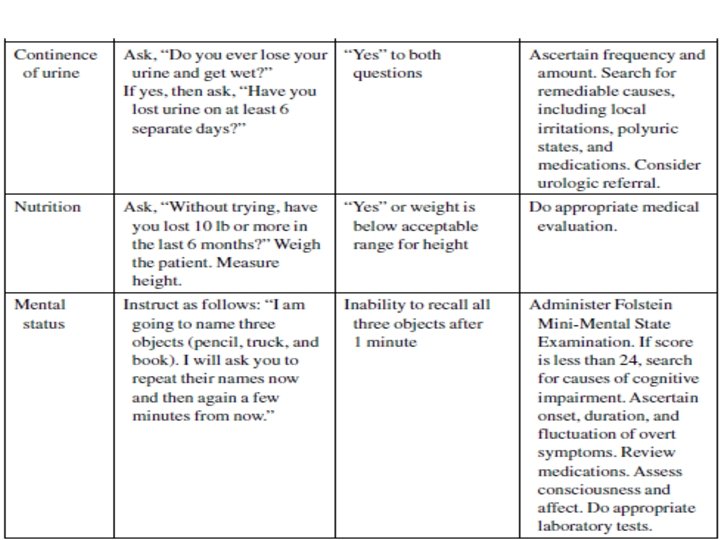
Functional Assessment Screening in the Elderly
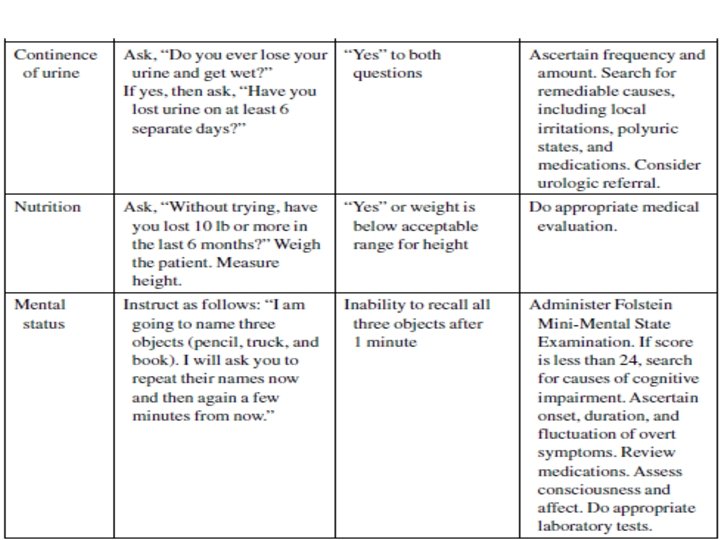



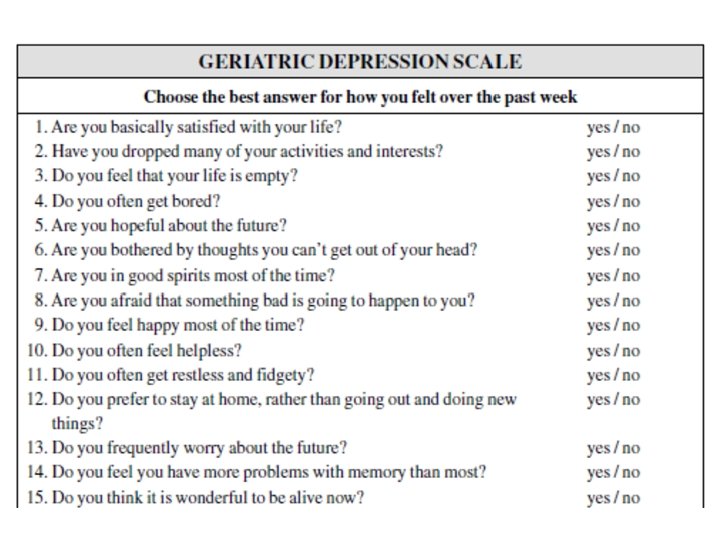
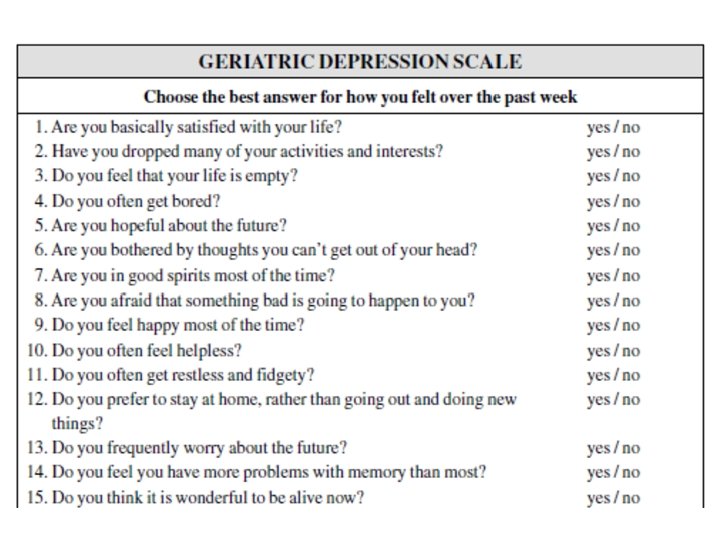
Psychological Assessment The psychological assessment screens for cognitive impairment and depression, two conditions that significantly impact both the patient and the family. -Mini-Mental State Examination, is best for identifying patients with moderate or severe dementia. -Depression assessed by Geriatric Depression Scale (GDS). -Depression Screen (“Do you often feel sad or depressed? ”) is a validated one-item GDS screening tool.


Social Assessment -It is important to assess the patient’s living situation and social support when performing a geriatric assessment. -The living situation should be evaluated for potential hazards. -The social assessment also includes questions about financial issues and caregiver concerns.
Pressure Ulcers • Preventive measures can reduce the incidence of pressure ulcers in elderly patients. • Classification is only one aspect of wound assessment. • Assessment of pressure ulcers includes identification of risk factors. • Pain assessment is an essential component of management. • Risk factor modification is the key to management of pressure ulcers.
Risk Factors for Pressure Sore 1 - Extrinsic Factors Pressure Shear Friction Moisture 2 - Intrinsic Factors Age Impaired mobility Malnutrition Sensory impairment
KEY TREATMENT -Assess all support surfaces and patient factors for increased pressure and modify appropriately. -Assess and manage the patient’s nutritional status. -Assess all patients for pain related to the pressure ulcer or its treatment.
Rational Drug Prescribing for Elderly Patients -Medications should be adjusted for the individual patient’s renal function. -Medication lists of elderly patients should be periodically reviewed, focusing on indications and side effects. -One drug should not be used to treat the side effects of another medication. -Pharmacists’ recommendations should be incorporated in a rational drug-prescribing plan.
Pharmacokinetic Changes in Older Persons -Absorption generally does not change. -Longer half-life of lipophilic drugs. -Increased amount of water soluble and free (active) drug. -Decreased excretion.
Principles of Rational Drug Prescribing for Elderly patients 1. Periodically update and review the medication list. 2. Work with the community pharmacist. 3. Educate the patient about the medication. 4. Consider an adverse drug event (ADE) as a cause of any new patient symptom. 5. Simplify the medication regimen. 6. Start one medication at a time, at lowest possible dose.
Urinary Incontinence defined as involuntary leakage of urine. • Incontinence is a common medical problem in the elderly population, affecting up to 30% of women and 15% of men. • Older women are more likely to have urge and stress incontinence, and older men are more likely to experience overflow and urge incontinence. • Acute episodes of incontinence are more likely the result of underlying medical conditions (e. g. , infection, hyperglycemia) or new medications (e. g. , diuretics).

• History, physical examination, urinalysis, and postvoid residual assessment are the key elements in categorization of incontinence. • Treatment options for incontinence include behavior modification, pelvic floor exercises, pharmacologic agents, vaginal pessaries, and surgical procedures. • Systemic hormone replacement therapy may exacerbate incontinence.
END
 Types of family in community medicine
Types of family in community medicine Principles of primary health care
Principles of primary health care Duke family medicine and community health
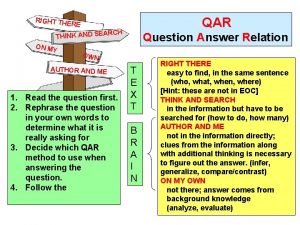
Duke family medicine and community health What are right there questions
What are right there questions Right there questions
Right there questions Qar examples
Qar examples Qar test
Qar test Qış baba şeiri
Qış baba şeiri Qar visuals
Qar visuals Qar visuals
Qar visuals Tế bào thụ cảm thị giác
Tế bào thụ cảm thị giác Một học sinh cận thị có các điểm cc cv
Một học sinh cận thị có các điểm cc cv Bé thì chăn nghé chăn trâu
Bé thì chăn nghé chăn trâu Bớt đầu thì bé nhất nhà
Bớt đầu thì bé nhất nhà Mode địa chỉ tức thì là mode
Mode địa chỉ tức thì là mode Nguyễn thị cẩm châu
Nguyễn thị cẩm châu Các kiểu bố trí thí nghiệm
Các kiểu bố trí thí nghiệm Riskman incident reporting
Riskman incident reporting Creative thi
Creative thi đặc tuyến bjt
đặc tuyến bjt Thuy ha
Thuy ha Pham thi thanh thao
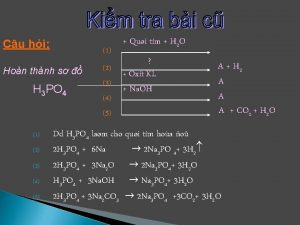
Pham thi thanh thao Thí nghiệm nhận biết ion photphat
Thí nghiệm nhận biết ion photphat đồ thị phụ tải
đồ thị phụ tải Nguyễn thị diễm my
Nguyễn thị diễm my Thực hành một số thí nghiệm về enzim
Thực hành một số thí nghiệm về enzim Dinh thi lan
Dinh thi lan Weak forms in sentences examples
Weak forms in sentences examples Lan nguyen thi
Lan nguyen thi Phan thị nga
Phan thị nga Trình bày diễn biến
Trình bày diễn biến Tran thi gung
Tran thi gung Cont'd pronunciation
Cont'd pronunciation Thí nghiệm phát hiện virus của ivanopxki
Thí nghiệm phát hiện virus của ivanopxki What is he doing
What is he doing đồ thị hàm arctan
đồ thị hàm arctan Lạy chúa này con xin đến để thực thi ý ngài
Lạy chúa này con xin đến để thực thi ý ngài Le thi kim thoa
Le thi kim thoa Lead time in community medicine
Lead time in community medicine Lead time in community medicine
Lead time in community medicine Minus desk in community medicine
Minus desk in community medicine Introduction to community medicine
Introduction to community medicine Concepts of health and disease
Concepts of health and disease