There are 2 types of Cardiac Muscle Cells
- Slides: 12
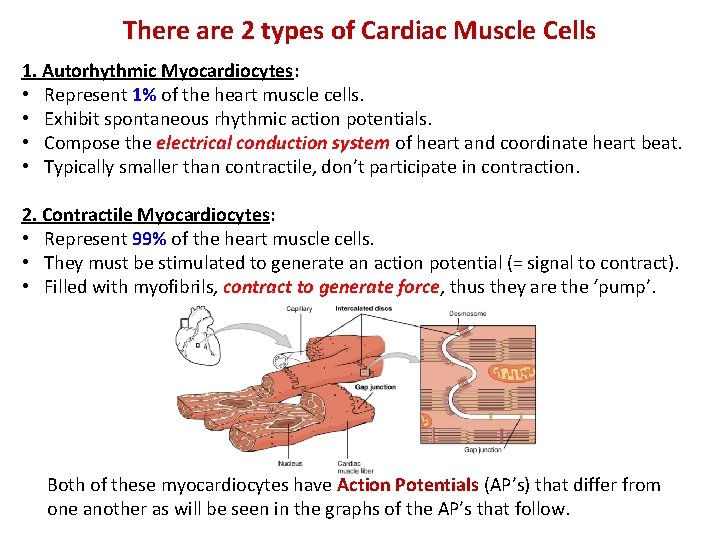
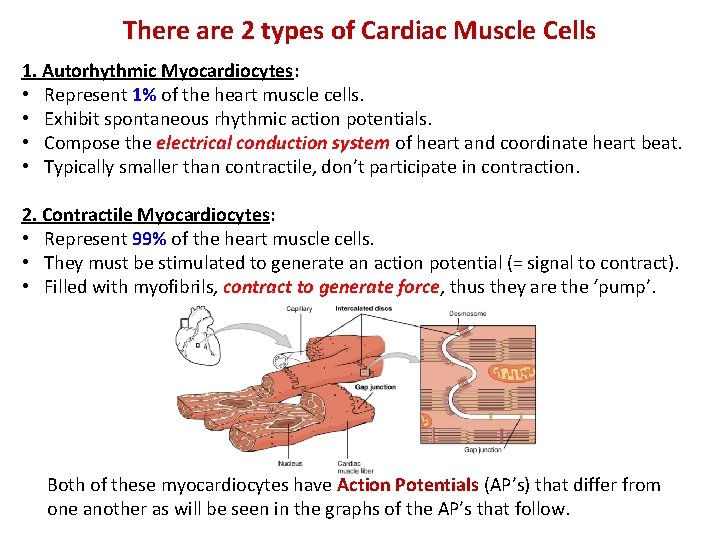
There are 2 types of Cardiac Muscle Cells 1. Autorhythmic Myocardiocytes: • Represent 1% of the heart muscle cells. • Exhibit spontaneous rhythmic action potentials. • Compose the electrical conduction system of heart and coordinate heart beat. • Typically smaller than contractile, don’t participate in contraction. 2. Contractile Myocardiocytes: • Represent 99% of the heart muscle cells. • They must be stimulated to generate an action potential (= signal to contract). • Filled with myofibrils, contract to generate force, thus they are the ‘pump’. Both of these myocardiocytes have Action Potentials (AP’s) that differ from one another as will be seen in the graphs of the AP’s that follow.
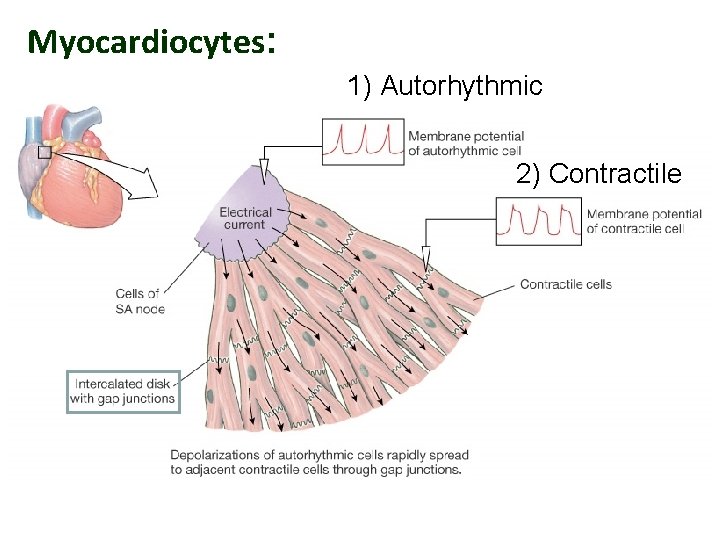
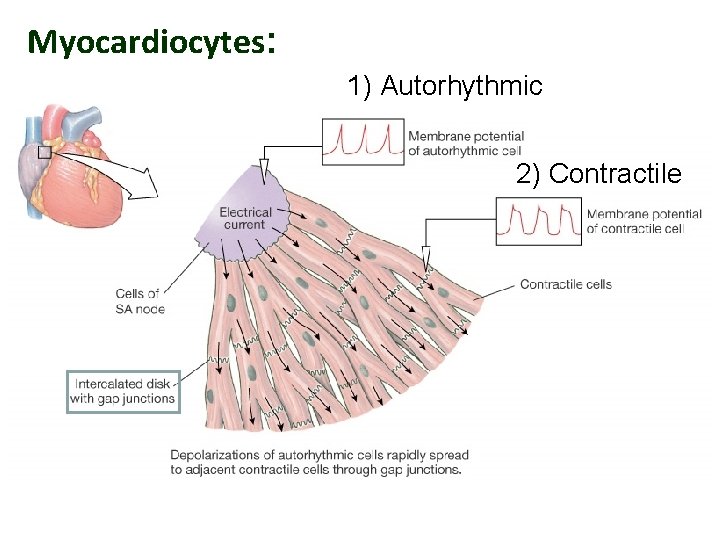
Myocardiocytes: 1) Autorhythmic 2) Contractile
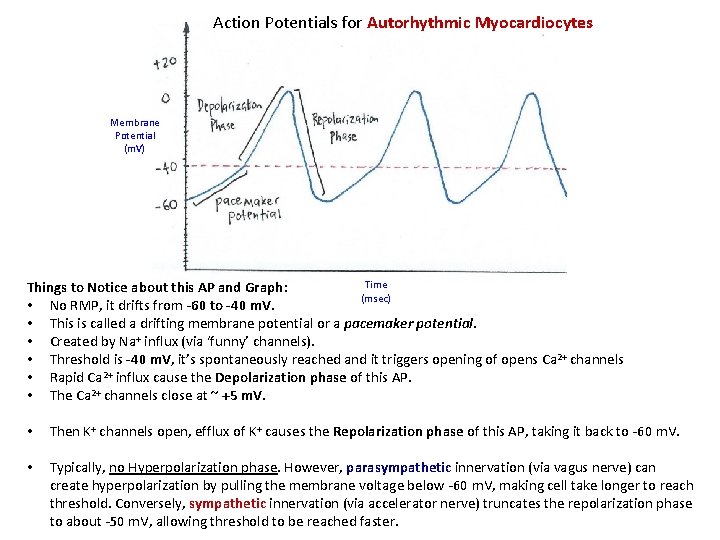
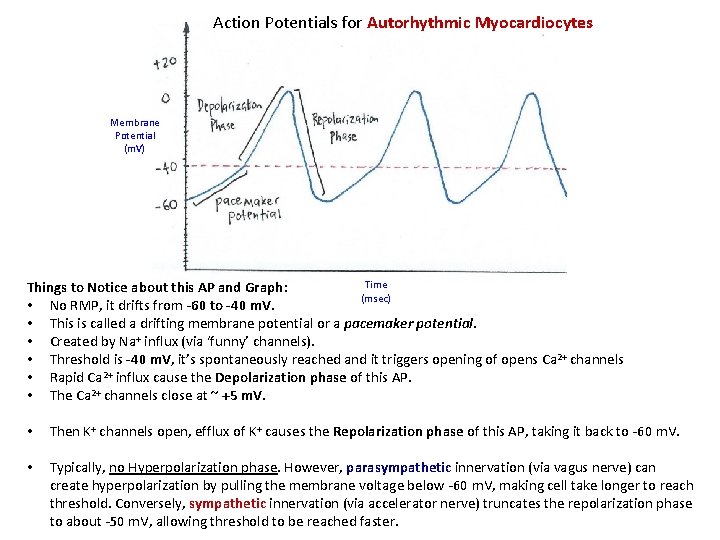
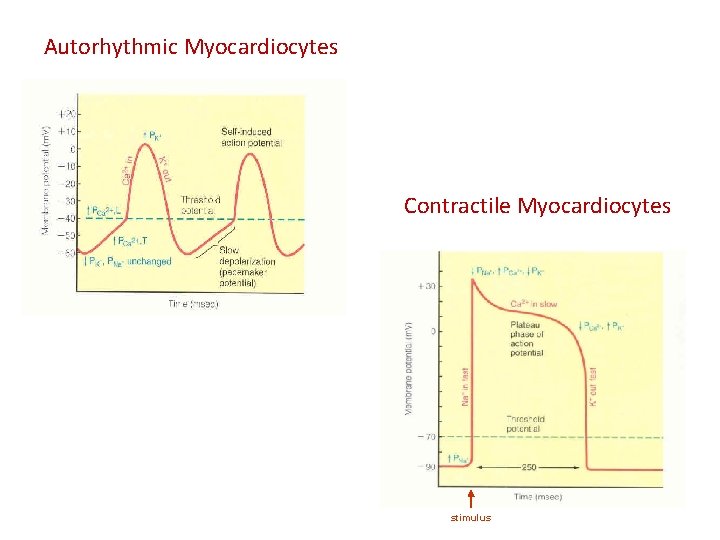
Action Potentials for Autorhythmic Myocardiocytes Membrane Potential (m. V) Time Things to Notice about this AP and Graph: (msec) • No RMP, it drifts from -60 to -40 m. V. • This is called a drifting membrane potential or a pacemaker potential. • Created by Na+ influx (via ‘funny’ channels). • Threshold is -40 m. V, it’s spontaneously reached and it triggers opening of opens Ca 2+ channels • Rapid Ca 2+ influx cause the Depolarization phase of this AP. • The Ca 2+ channels close at ~ +5 m. V. • Then K+ channels open, efflux of K+ causes the Repolarization phase of this AP, taking it back to -60 m. V. • Typically, no Hyperpolarization phase. However, parasympathetic innervation (via vagus nerve) can create hyperpolarization by pulling the membrane voltage below -60 m. V, making cell take longer to reach threshold. Conversely, sympathetic innervation (via accelerator nerve) truncates the repolarization phase to about -50 m. V, allowing threshold to be reached faster.
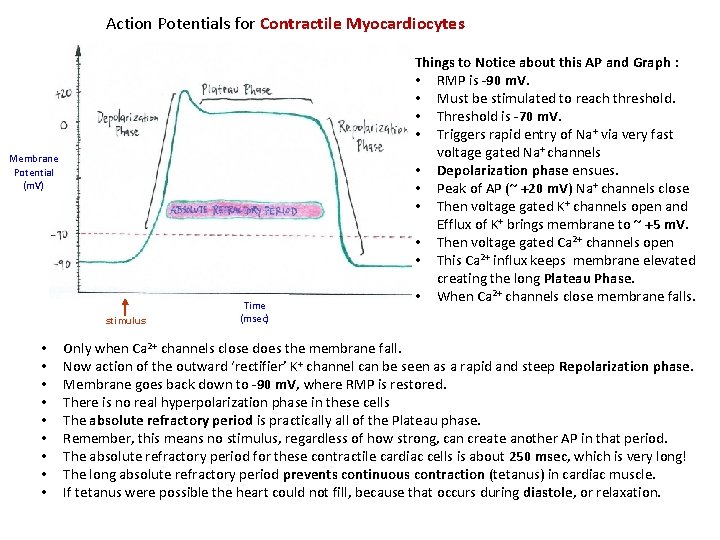
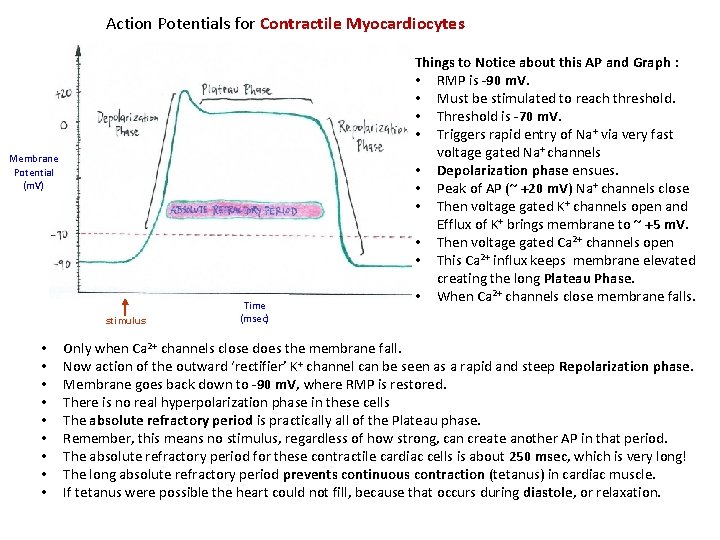
Action Potentials for Contractile Myocardiocytes Membrane Potential (m. V) stimulus • • • Time (msec) Things to Notice about this AP and Graph : • RMP is -90 m. V. • Must be stimulated to reach threshold. • Threshold is -70 m. V. • Triggers rapid entry of Na+ via very fast voltage gated Na+ channels • Depolarization phase ensues. • Peak of AP (~ +20 m. V) Na+ channels close • Then voltage gated K+ channels open and Efflux of K+ brings membrane to ~ +5 m. V. • Then voltage gated Ca 2+ channels open • This Ca 2+ influx keeps membrane elevated creating the long Plateau Phase. • When Ca 2+ channels close membrane falls. Only when Ca 2+ channels close does the membrane fall. Now action of the outward ‘rectifier’ K+ channel can be seen as a rapid and steep Repolarization phase. Membrane goes back down to -90 m. V, where RMP is restored. There is no real hyperpolarization phase in these cells The absolute refractory period is practically all of the Plateau phase. Remember, this means no stimulus, regardless of how strong, can create another AP in that period. The absolute refractory period for these contractile cardiac cells is about 250 msec, which is very long! The long absolute refractory period prevents continuous contraction (tetanus) in cardiac muscle. If tetanus were possible the heart could not fill, because that occurs during diastole, or relaxation.
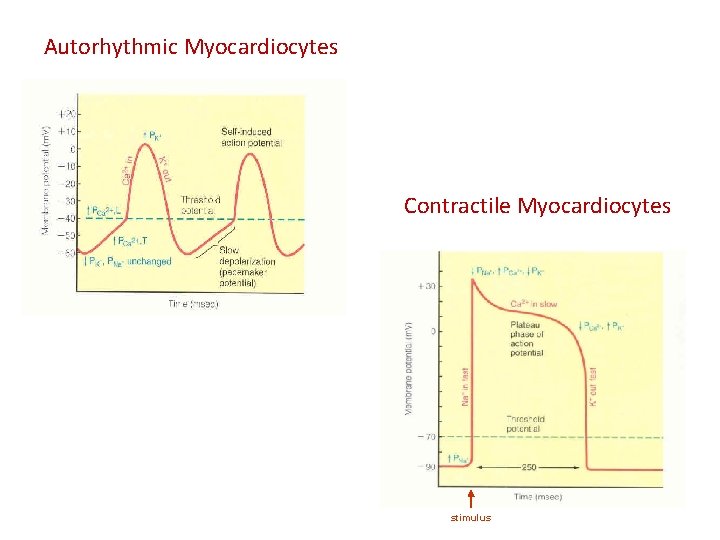
Autorhythmic Myocardiocytes Contractile Myocardiocytes stimulus
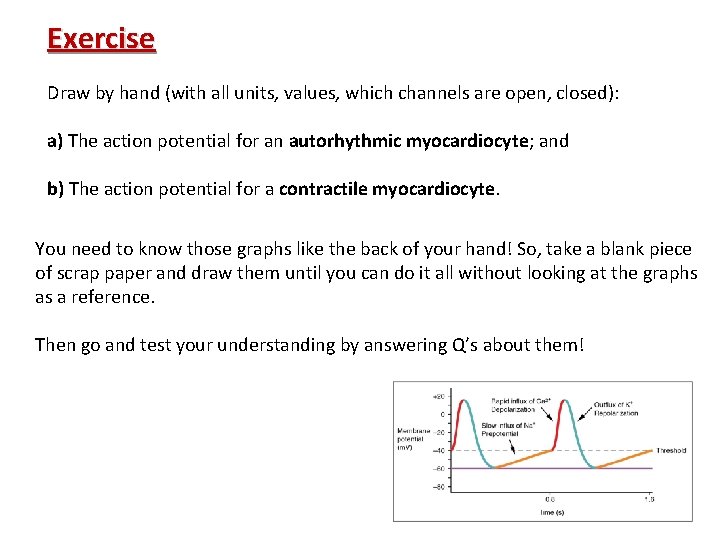
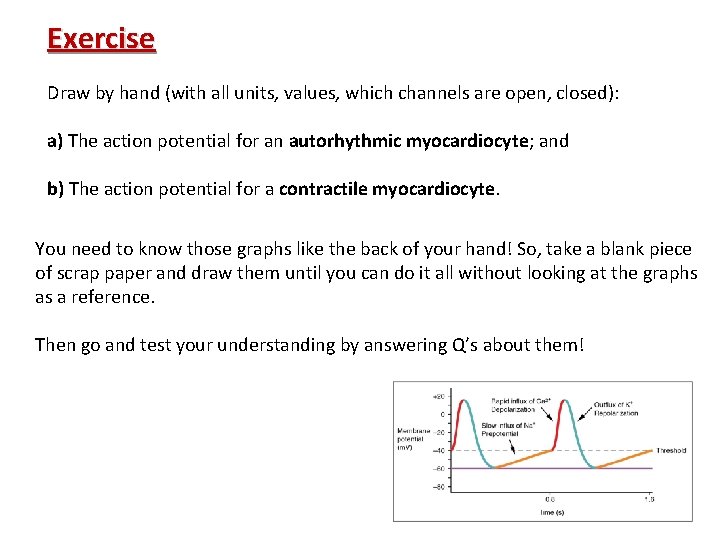
Exercise Draw by hand (with all units, values, which channels are open, closed): a) The action potential for an autorhythmic myocardiocyte; and b) The action potential for a contractile myocardiocyte. You need to know those graphs like the back of your hand! So, take a blank piece of scrap paper and draw them until you can do it all without looking at the graphs as a reference. Then go and test your understanding by answering Q’s about them!
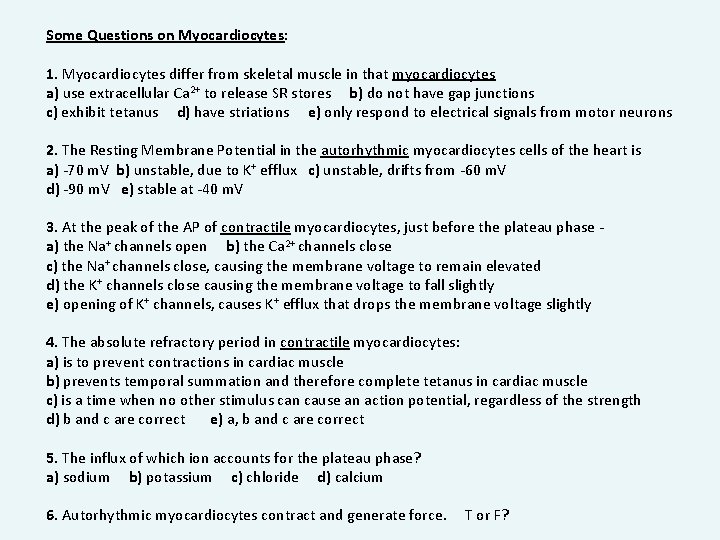
Some Questions on Myocardiocytes: 1. Myocardiocytes differ from skeletal muscle in that myocardiocytes a) use extracellular Ca 2+ to release SR stores b) do not have gap junctions c) exhibit tetanus d) have striations e) only respond to electrical signals from motor neurons 2. The Resting Membrane Potential in the autorhythmic myocardiocytes cells of the heart is a) -70 m. V b) unstable, due to K+ efflux c) unstable, drifts from -60 m. V d) -90 m. V e) stable at -40 m. V 3. At the peak of the AP of contractile myocardiocytes, just before the plateau phase a) the Na+ channels open b) the Ca 2+ channels close c) the Na+ channels close, causing the membrane voltage to remain elevated d) the K+ channels close causing the membrane voltage to fall slightly e) opening of K+ channels, causes K+ efflux that drops the membrane voltage slightly 4. The absolute refractory period in contractile myocardiocytes: a) is to prevent contractions in cardiac muscle b) prevents temporal summation and therefore complete tetanus in cardiac muscle c) is a time when no other stimulus can cause an action potential, regardless of the strength d) b and c are correct e) a, b and c are correct 5. The influx of which ion accounts for the plateau phase? a) sodium b) potassium c) chloride d) calcium 6. Autorhythmic myocardiocytes contract and generate force. T or F?
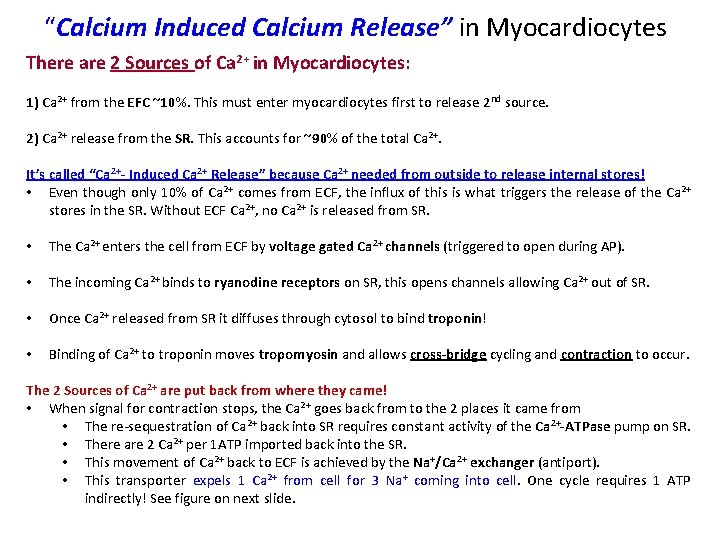
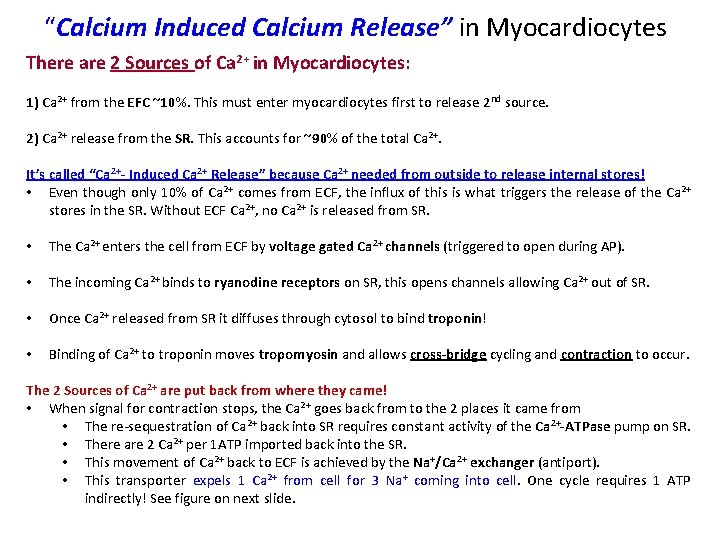
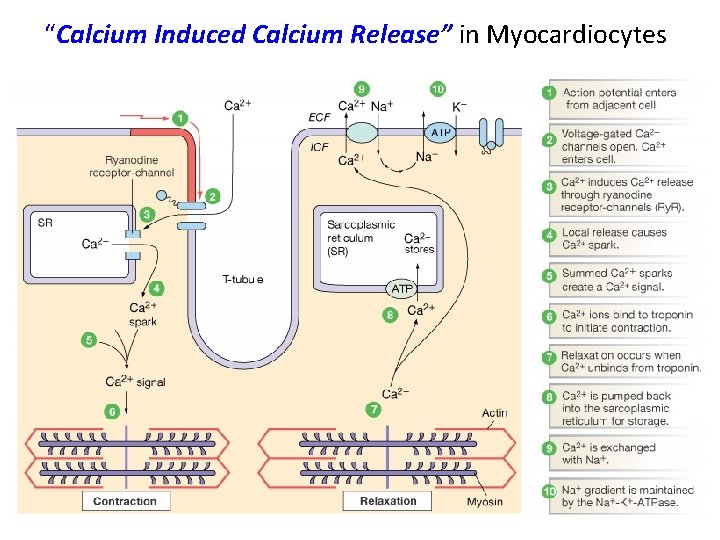
“Calcium Induced Calcium Release” in Myocardiocytes There are 2 Sources of Ca 2+ in Myocardiocytes: 1) Ca 2+ from the EFC ~10%. This must enter myocardiocytes first to release 2 nd source. 2) Ca 2+ release from the SR. This accounts for ~90% of the total Ca 2+. It’s called “Ca 2+- Induced Ca 2+ Release” because Ca 2+ needed from outside to release internal stores! • Even though only 10% of Ca 2+ comes from ECF, the influx of this is what triggers the release of the Ca 2+ stores in the SR. Without ECF Ca 2+, no Ca 2+ is released from SR. • The Ca 2+ enters the cell from ECF by voltage gated Ca 2+ channels (triggered to open during AP). • The incoming Ca 2+ binds to ryanodine receptors on SR, this opens channels allowing Ca 2+ out of SR. • Once Ca 2+ released from SR it diffuses through cytosol to bind troponin! • Binding of Ca 2+ to troponin moves tropomyosin and allows cross-bridge cycling and contraction to occur. The 2 Sources of Ca 2+ are put back from where they came! • When signal for contraction stops, the Ca 2+ goes back from to the 2 places it came from • The re-sequestration of Ca 2+ back into SR requires constant activity of the Ca 2+-ATPase pump on SR. • There are 2 Ca 2+ per 1 ATP imported back into the SR. • This movement of Ca 2+ back to ECF is achieved by the Na+/Ca 2+ exchanger (antiport). • This transporter expels 1 Ca 2+ from cell for 3 Na+ coming into cell. One cycle requires 1 ATP indirectly! See figure on next slide.
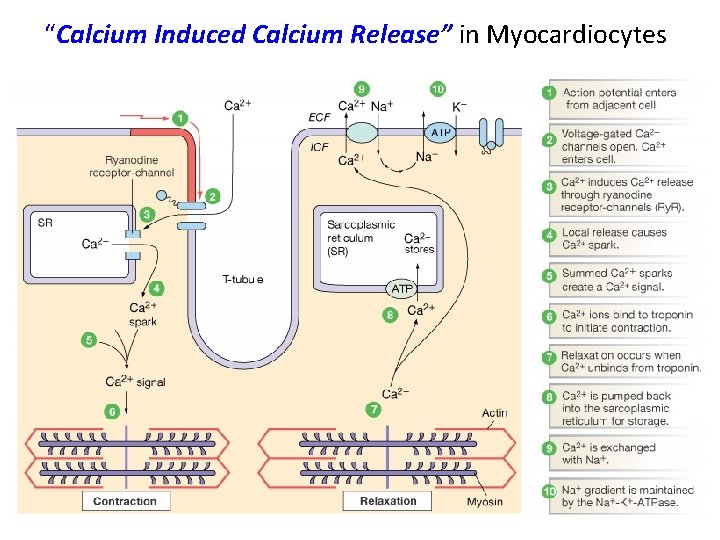
“Calcium Induced Calcium Release” in Myocardiocytes
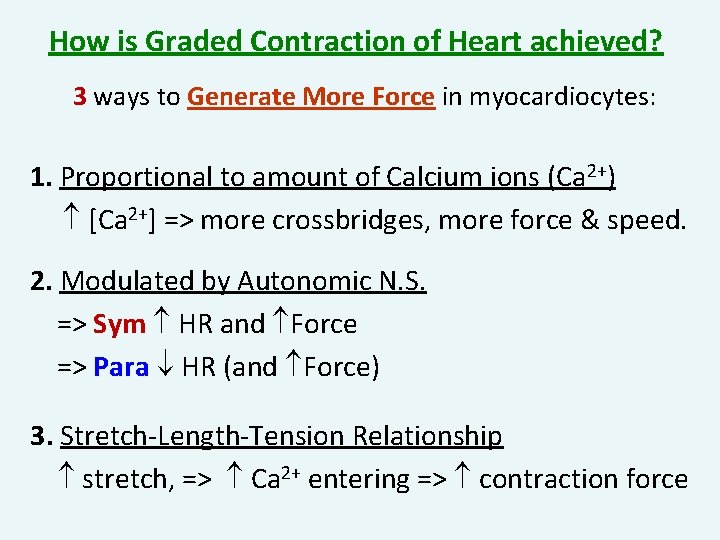
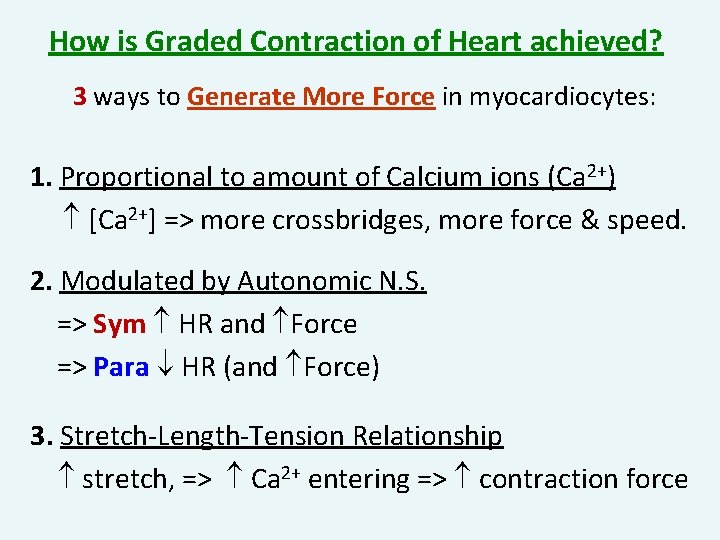
How is Graded Contraction of Heart achieved? 3 ways to Generate More Force in myocardiocytes: 1. Proportional to amount of Calcium ions (Ca 2+) [Ca 2+] => more crossbridges, more force & speed. 2. Modulated by Autonomic N. S. => Sym HR and Force => Para HR (and Force) 3. Stretch-Length-Tension Relationship stretch, => Ca 2+ entering => contraction force
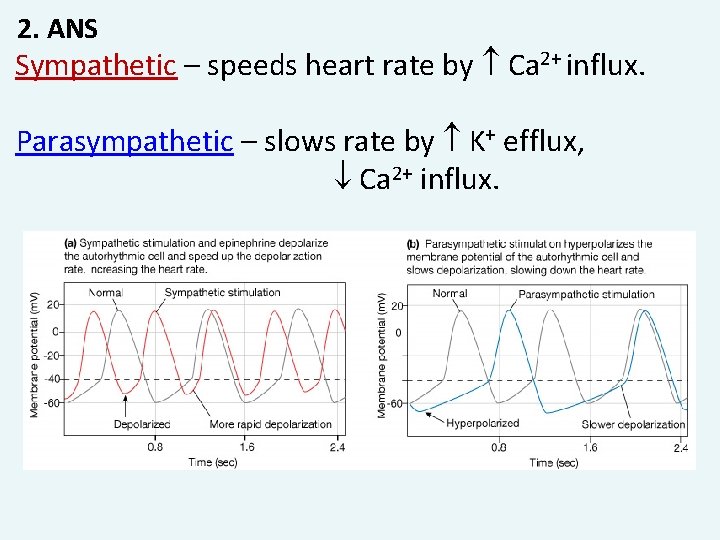
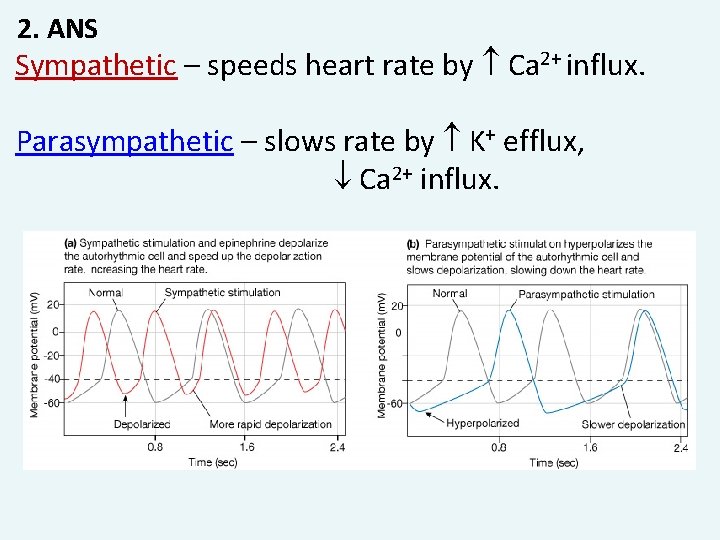
2. ANS Sympathetic – speeds heart rate by Ca 2+ influx. Parasympathetic – slows rate by K+ efflux, Ca 2+ influx.
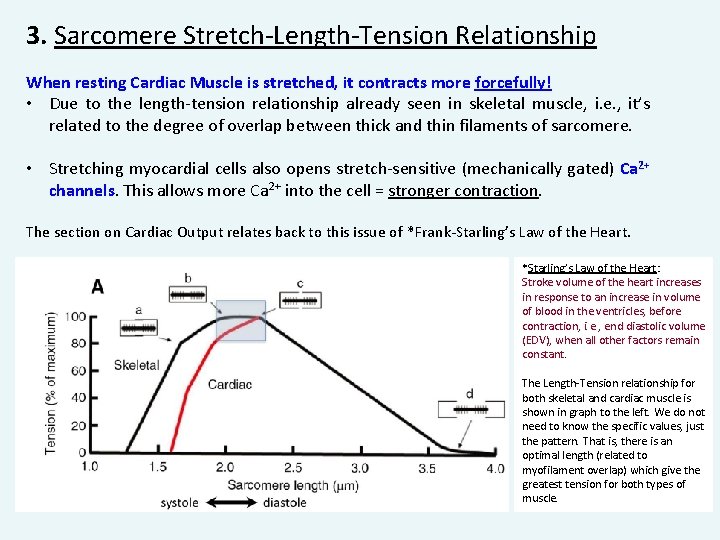
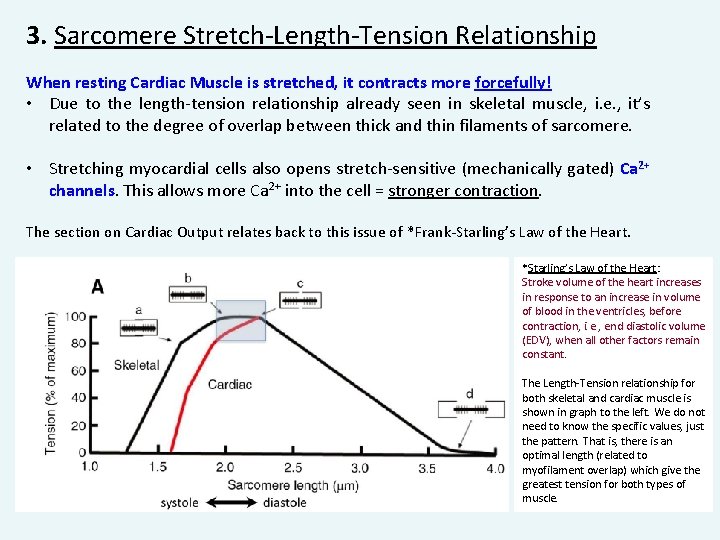
3. Sarcomere Stretch-Length-Tension Relationship When resting Cardiac Muscle is stretched, it contracts more forcefully! • Due to the length-tension relationship already seen in skeletal muscle, i. e. , it’s related to the degree of overlap between thick and thin filaments of sarcomere. • Stretching myocardial cells also opens stretch-sensitive (mechanically gated) Ca 2+ channels. This allows more Ca 2+ into the cell = stronger contraction. The section on Cardiac Output relates back to this issue of *Frank-Starling’s Law of the Heart. *Starling’s Law of the Heart: Stroke volume of the heart increases in response to an increase in volume of blood in the ventricles, before contraction, i. e. , end diastolic volume (EDV), when all other factors remain constant. The Length-Tension relationship for both skeletal and cardiac muscle is shown in graph to the left. We do not need to know the specific values, just the pattern. That is, there is an optimal length (related to myofilament overlap) which give the greatest tension for both types of muscle.