Therapy of Type 2 Diabetes Mellitus UPDATE Glycemic
Therapy of Type 2 Diabetes Mellitus: UPDATE Glycemic Goals in the Care of Patients with Type 2 Diabetes- 2013 ADA and AACE Guidelines: Room For Improvement (Be HAPPY/ Avoid Burnout, While Caring for Patients with DM) Stan Schwartz MD, FACP, FACE Affiliate, Main Line Health System Clinical Associate Professor of Medicine, Emeritus, U of Pa. Part 4
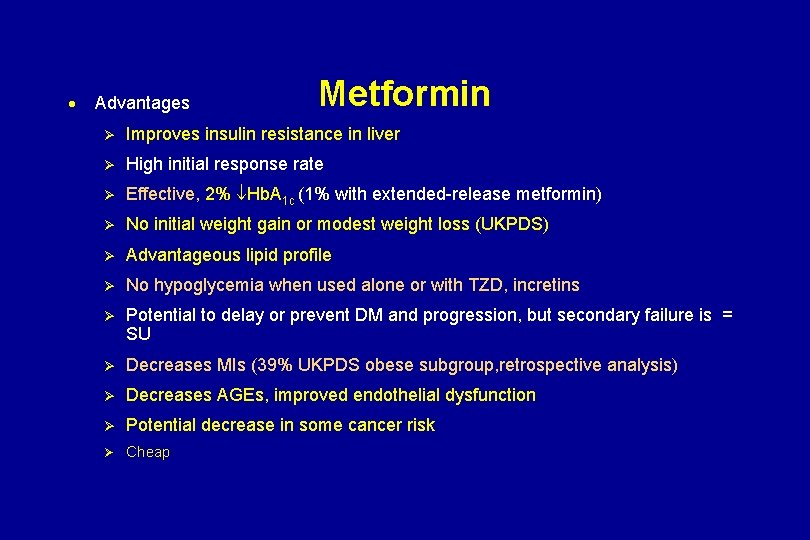
· Advantages Metformin Ø Improves insulin resistance in liver Ø High initial response rate Ø Effective, 2% Hb. A 1 c (1% with extended-release metformin) Ø No initial weight gain or modest weight loss (UKPDS) Ø Advantageous lipid profile Ø No hypoglycemia when used alone or with TZD, incretins Ø Potential to delay or prevent DM and progression, but secondary failure is = SU Ø Decreases MIs (39% UKPDS obese subgroup, retrospective analysis) Ø Decreases AGEs, improved endothelial dysfunction Ø Potential decrease in some cancer risk Ø Cheap
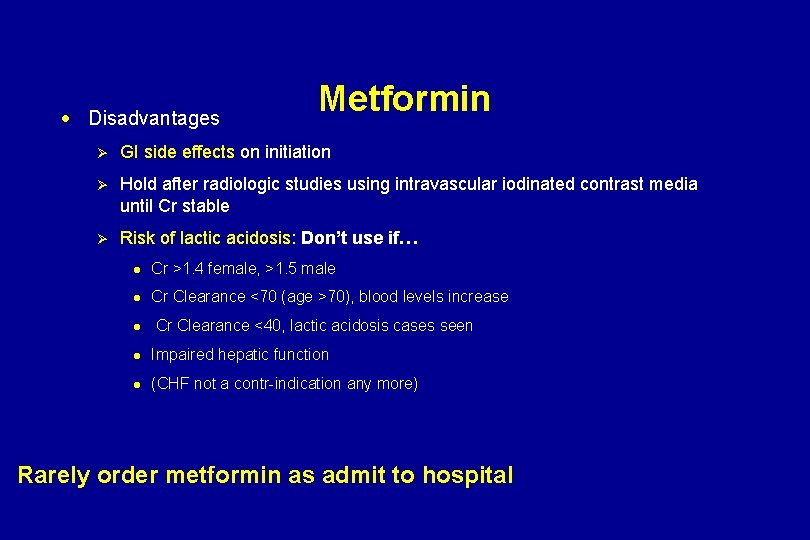
· Disadvantages Metformin Ø GI side effects on initiation Ø Hold after radiologic studies using intravascular iodinated contrast media until Cr stable Ø Risk of lactic acidosis: Don’t use if… l Cr >1. 4 female, >1. 5 male l Cr Clearance <70 (age >70), blood levels increase l Cr Clearance <40, lactic acidosis cases seen l Impaired hepatic function l (CHF not a contr-indication any more) Rarely order metformin as admit to hospital
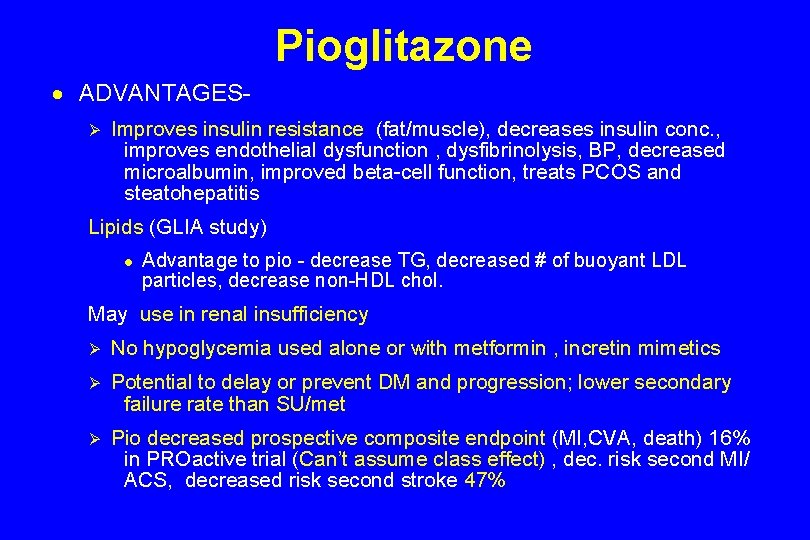
Pioglitazone · ADVANTAGESØ Improves insulin resistance (fat/muscle), decreases insulin conc. , improves endothelial dysfunction , dysfibrinolysis, BP, decreased microalbumin, improved beta-cell function, treats PCOS and steatohepatitis Lipids (GLIA study) l Advantage to pio - decrease TG, decreased # of buoyant LDL particles, decrease non-HDL chol. May use in renal insufficiency Ø No hypoglycemia used alone or with metformin , incretin mimetics Ø Potential to delay or prevent DM and progression; lower secondary failure rate than SU/met Ø Pio decreased prospective composite endpoint (MI, CVA, death) 16% in PROactive trial (Can’t assume class effect) , dec. risk second MI/ ACS, decreased risk second stroke 47%
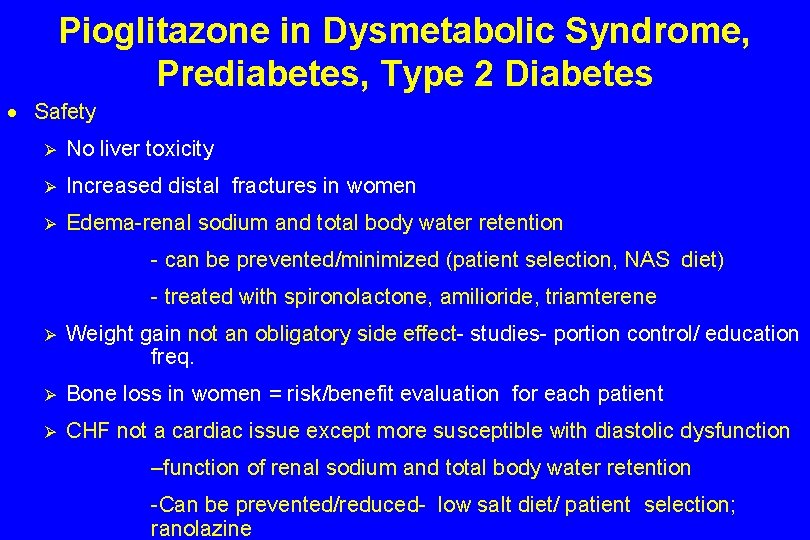
Pioglitazone in Dysmetabolic Syndrome, Prediabetes, Type 2 Diabetes · Safety Ø No liver toxicity Ø Increased distal fractures in women Ø Edema-renal sodium and total body water retention - can be prevented/minimized (patient selection, NAS diet) - treated with spironolactone, amilioride, triamterene Ø Weight gain not an obligatory side effect- studies- portion control/ education freq. Ø Bone loss in women = risk/benefit evaluation for each patient Ø CHF not a cardiac issue except more susceptible with diastolic dysfunction –function of renal sodium and total body water retention -Can be prevented/reduced- low salt diet/ patient selection; ranolazine
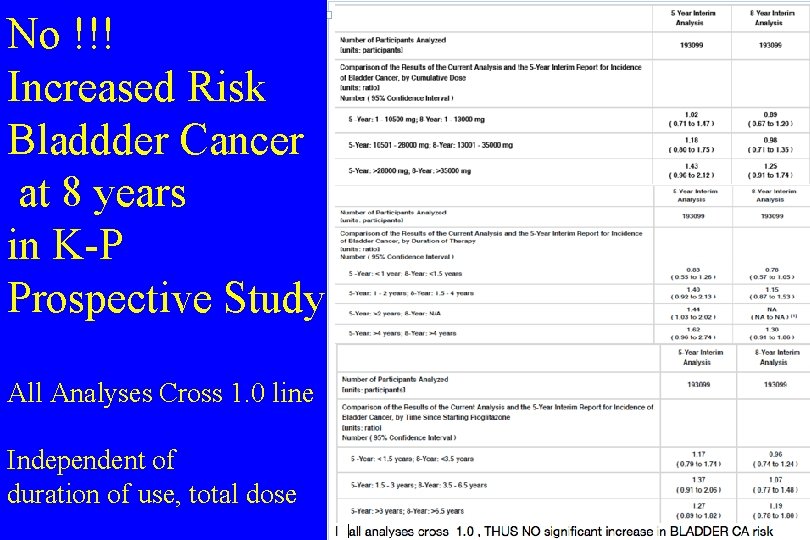
No !!! Increased Risk Bladdder Cancer at 8 years in K-P Prospective Study All Analyses Cross 1. 0 line Independent of duration of use, total dose
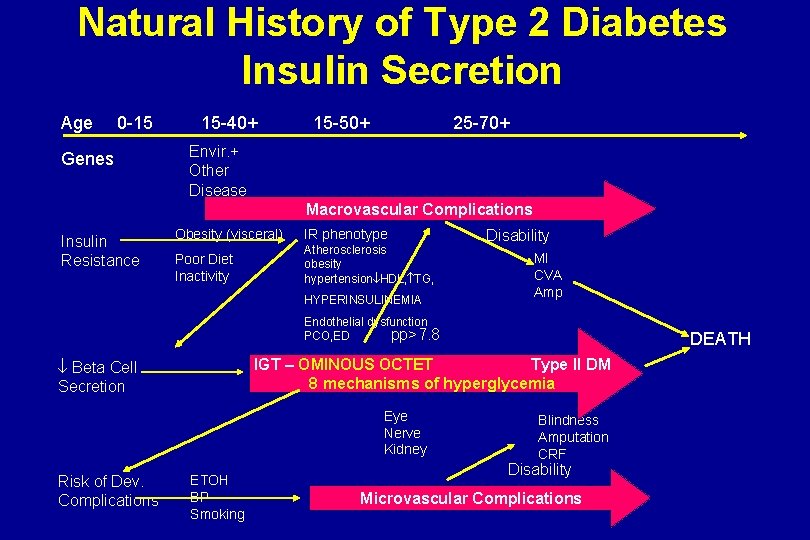
Natural History of Type 2 Diabetes Insulin Secretion Age 0 -15 Genes 15 -40+ 15 -50+ 25 -70+ Envir. + Other Disease Macrovascular Complications Insulin Resistance Obesity (visceral) IR phenotype Poor Diet Inactivity Atherosclerosis obesity hypertension HDL, TG, HYPERINSULINEMIA Disability MI CVA Amp Endothelial dysfunction pp>7. 8 PCO, ED IGT – OMINOUS OCTET Type II DM 8 mechanisms of hyperglycemia Beta Cell Secretion Eye Nerve Kidney Risk of Dev. Complications DEATH ETOH BP Smoking Blindness Amputation CRF Disability Microvascular Complications
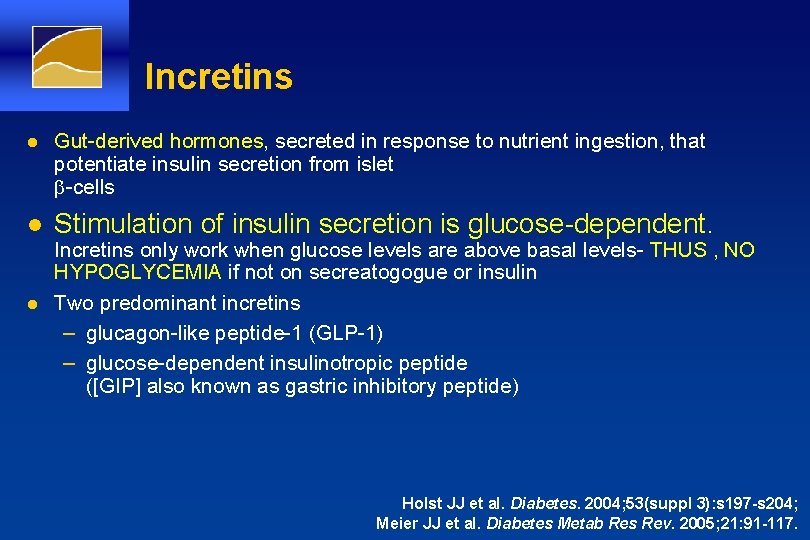
Incretins l Gut-derived hormones, secreted in response to nutrient ingestion, that potentiate insulin secretion from islet b-cells l Stimulation of insulin secretion is glucose-dependent. l Incretins only work when glucose levels are above basal levels- THUS , NO HYPOGLYCEMIA if not on secreatogogue or insulin Two predominant incretins – glucagon-like peptide-1 (GLP-1) – glucose-dependent insulinotropic peptide ([GIP] also known as gastric inhibitory peptide) Holst JJ et al. Diabetes. 2004; 53(suppl 3): s 197 -s 204; Meier JJ et al. Diabetes Metab Res Rev. 2005; 21: 91 -117.
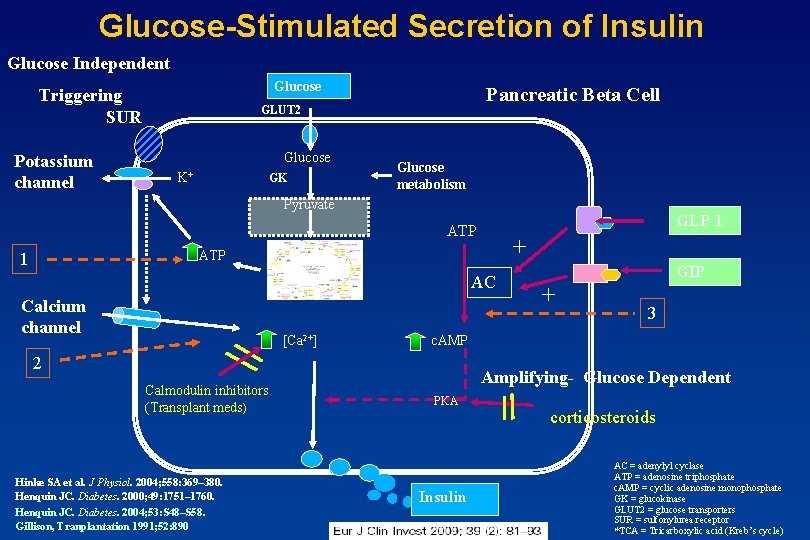
Glucose-Stimulated Secretion of Insulin Glucose Independent Glucose Triggering SUR Potassium channel Pancreatic Beta Cell GLUT 2 Glucose K+ GK Glucose metabolism Pyruvate GLP-1 ATP 1 Calcium channel TCA Cycle* [Ca 2+] AC Hinke SA et al. J Physiol. 2004; 558: 369– 380. Henquin JC. Diabetes. 2000; 49: 1751– 1760. Henquin JC. Diabetes. 2004; 53: S 48–S 58. Gillison, Tranplantation 1991; 52: 890 GIP + 3 c. AMP 2 Calmodulin inhibitors (Transplant meds) + Amplifying- Glucose Dependent PKA Insulin corticosteroids AC = adenylyl cyclase ATP = adenosine triphosphate c. AMP = cyclic adenosine monophosphate GK = glucokinase GLUT 2 = glucose transporters SUR = sulfonylurea receptor *TCA = Tricarboxylic acid (Kreb’s cycle)
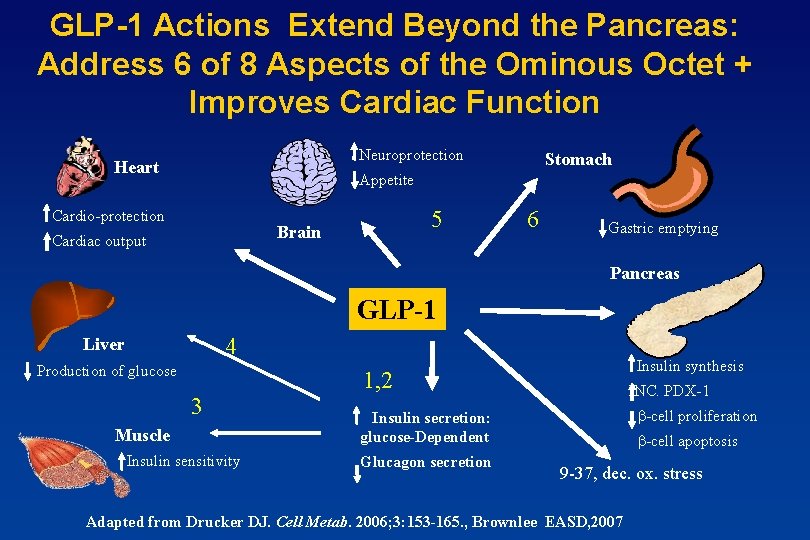
GLP-1 Actions Extend Beyond the Pancreas: Address 6 of 8 Aspects of the Ominous Octet + Improves Cardiac Function Neuroprotection Heart Stomach Appetite Cardio-protection 5 Brain Cardiac output 6 Gastric emptying Pancreas GLP-1 4 Liver Production of glucose 3 Muscle Insulin sensitivity Insulin synthesis 1, 2 INC. PDX-1 b-cell proliferation Insulin secretion: glucose-Dependent Glucagon secretion b-cell apoptosis 9 -37, dec. ox. stress Adapted from Drucker DJ. Cell Metab. 2006; 3: 153 -165. , Brownlee EASD, 2007
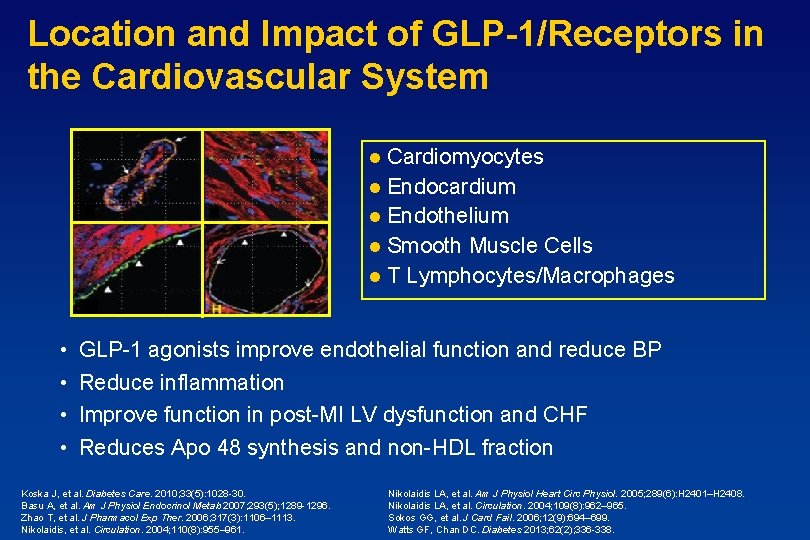
Location and Impact of GLP-1/Receptors in the Cardiovascular System Cardiomyocytes l Endocardium l Endothelium l Smooth Muscle Cells l T Lymphocytes/Macrophages l • • GLP-1 agonists improve endothelial function and reduce BP Reduce inflammation Improve function in post-MI LV dysfunction and CHF Reduces Apo 48 synthesis and non-HDL fraction Koska J, et al. Diabetes Care. 2010; 33(5): 1028 -30. Basu A, et al. Am J Physiol Endocrinol Metab 2007; 293(5); 1289 -1296. Zhao T, et al. J Pharmacol Exp Ther. 2006; 317(3): 1106– 1113. Nikolaidis, et al. Circulation. 2004; 110(8): 955– 961. Nikolaidis LA, et al. Am J Physiol Heart Circ Physiol. 2005; 289(6): H 2401–H 2408. Nikolaidis LA, et al. Circulation. 2004; 109(8): 962– 965. Sokos GG, et al. J Card Fail. 2006; 12(9): 694– 699. Watts GF, Chan DC. Diabetes 2013; 62(2); 336 -338.
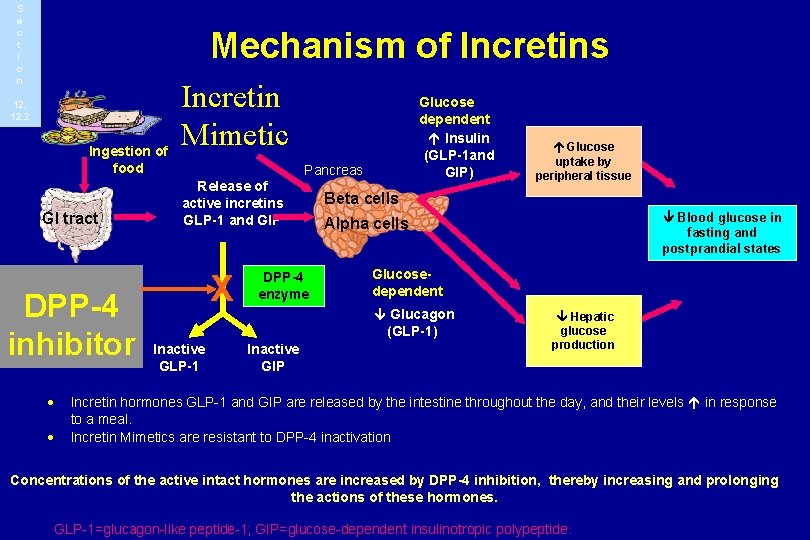
S e c t i o n Mechanism of Incretins 12, 12. 2 Ingestion of food GI tract DPP-4 inhibitor · · Incretin Mimetic Glucose dependent Insulin (GLP-1 and GIP) Pancreas Release of active incretins GLP-1 and GIP X Inactive GLP-1 DPP-4 enzyme Beta cells Blood glucose in fasting and postprandial states Alpha cells Glucosedependent Glucagon (GLP-1) Inactive GIP Glucose uptake by peripheral tissue Hepatic glucose production Incretin hormones GLP-1 and GIP are released by the intestine throughout the day, and their levels in response to a meal. Incretin Mimetics are resistant to DPP-4 inactivation Concentrations of the active intact hormones are increased by DPP-4 inhibition, thereby increasing and prolonging the actions of these hormones. GLP-1=glucagon-like peptide-1; GIP=glucose-dependent insulinotropic polypeptide.
- Slides: 13