Therapy Modality Continuous Ambulatory Peritoneal Dialysis CAPD Renal
Therapy Modality: Continuous Ambulatory Peritoneal Dialysis (CAPD) Renal Division Baxter Healthcare
CAPD - basic prescription • Manual therapy • Prescription volumes standardised 1, 500 ml, 2000 ml, 2500 ml, 3000 ml solution bags • 6 -8 hour dwell period each night (depends on type of membrane) • 4 -5 day exchanges (with optional night dwell), 7 days a week • 3 -5 hr dwell per day exchange 2 CAPD
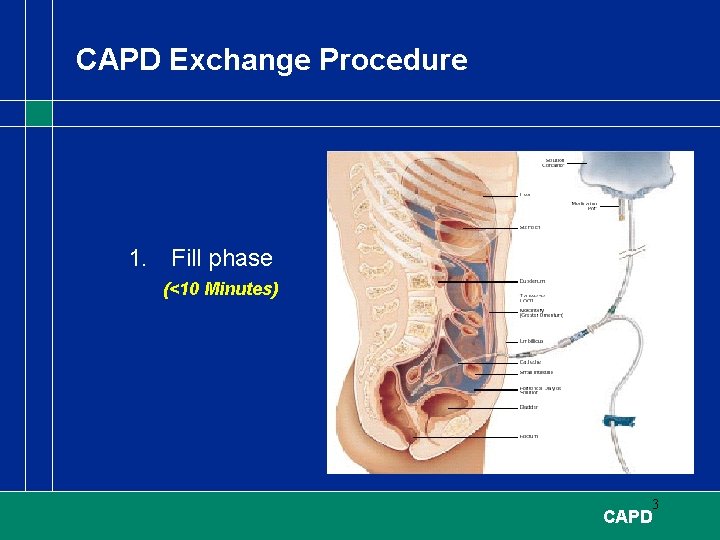
CAPD Exchange Procedure 1. Fill phase (<10 Minutes) 3 CAPD
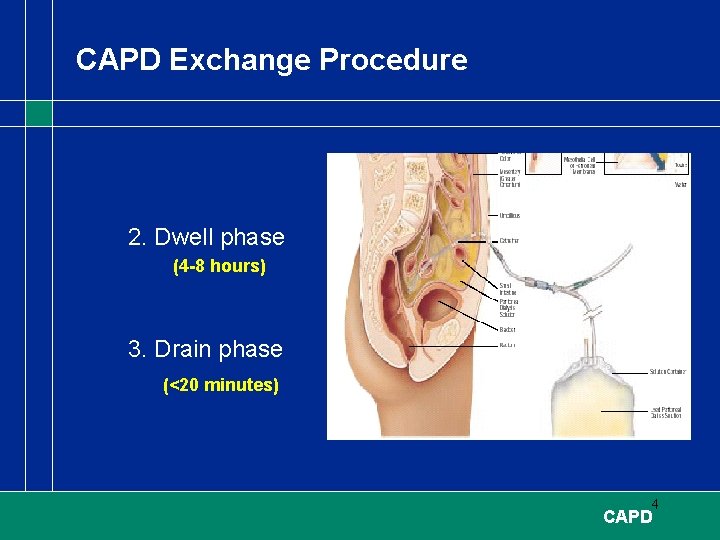
CAPD Exchange Procedure 2. Dwell phase (4 -8 hours) 3. Drain phase (<20 minutes) 4 CAPD
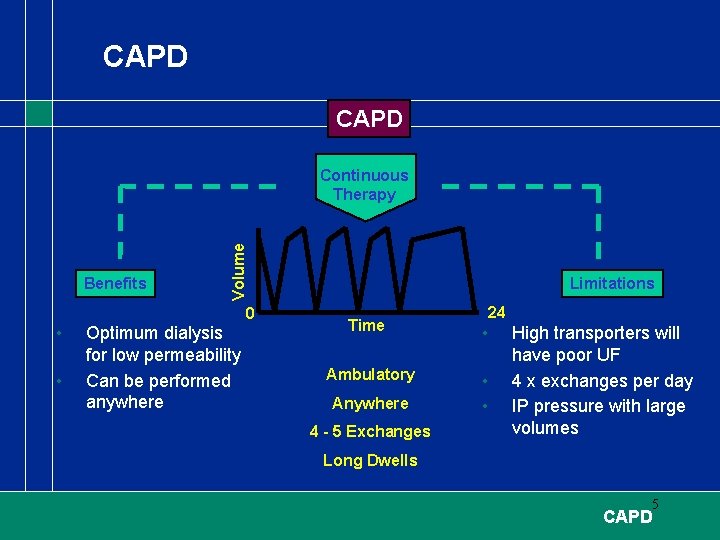
CAPD Benefits • • Volume Continuous Therapy 0 Optimum dialysis for low permeability Can be performed anywhere Limitations 24 Time • Ambulatory • • Anywhere 4 - 5 Exchanges High transporters will have poor UF 4 x exchanges per day IP pressure with large volumes Long Dwells 5 CAPD
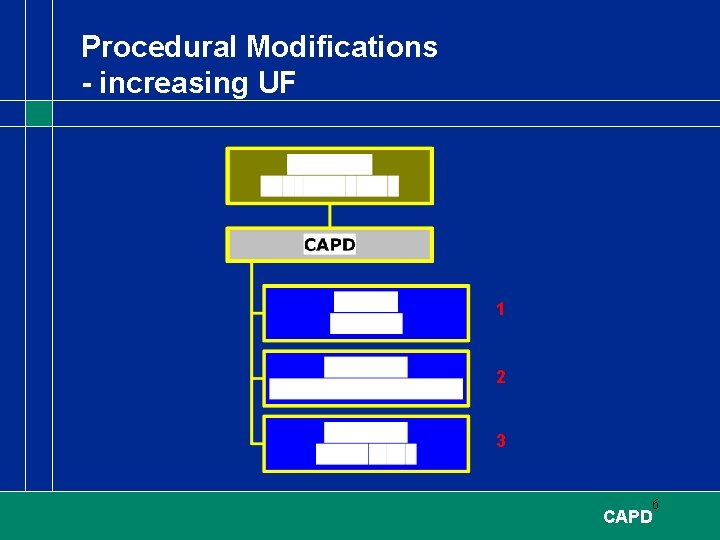
Procedural Modifications - increasing UF 1 2 3 6 CAPD
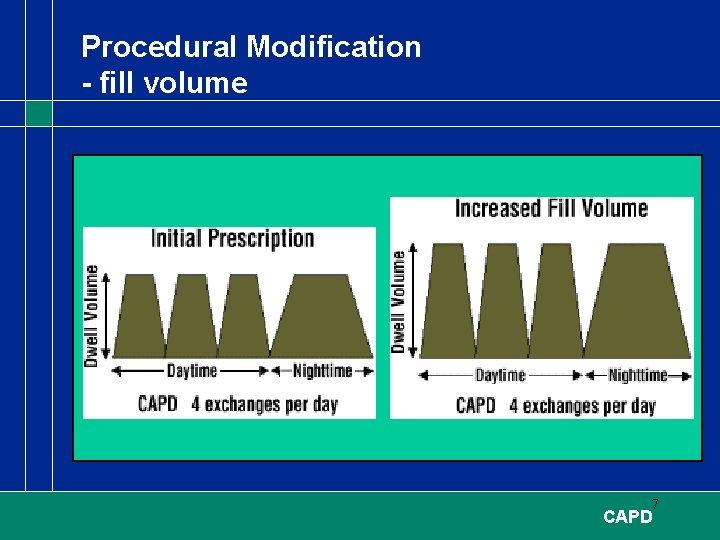
Procedural Modification - fill volume 7 CAPD
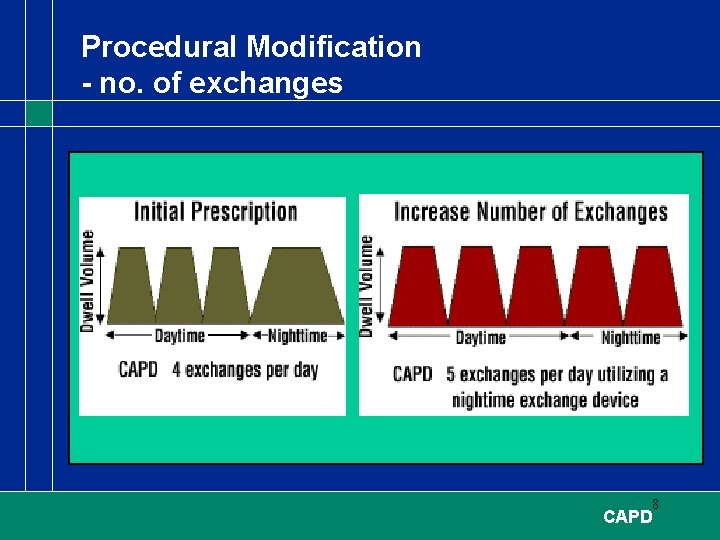
Procedural Modification - no. of exchanges 8 CAPD
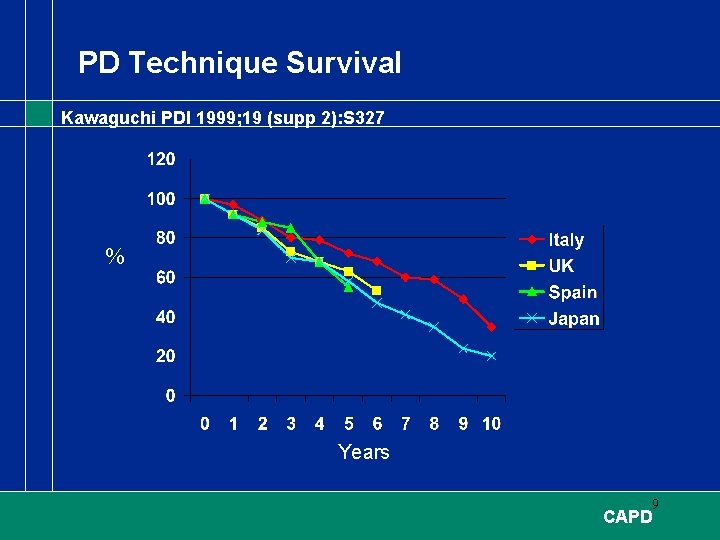
PD Technique Survival Kawaguchi PDI 1999; 19 (supp 2): S 327 % Years 9 CAPD
PD Technique Survival Kawaguchi PDI 1999; 19 (supp 2): S 327 • Reasons for withdrawal - Loss of UF - Inadequate dialysis - Peritonitis - Patient choice/psychological (‘burn-out’) 10 CAPD
CAPD Outcome - Japan Kawaguchi PDI 1999; 19 (suppl 3): S 9 • • 235 patients analysed between 1980 - 1997 Average survival was 5. 8 years 142 patients changed dialysis therapy Causes - loss of UF (23%) - inadequate dialysis (16%) - peritonitis (14%) • Peritonitis rate was very good - 1 episode/54 patient months 11 CAPD
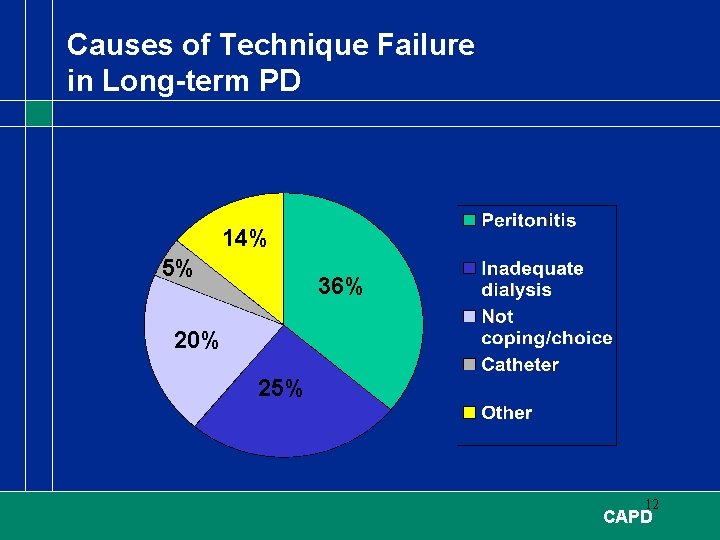
Causes of Technique Failure in Long-term PD 14% 5% 36% 20% 25% 12 CAPD
CAPD Systems AIM: Safety, Simplicity, Comfort & Convenience Requirements: 1. Minimise risk of touch contamination 2. Maximise Flush efficiency 3. Inactivate organisms at patient connector if touch contamination occurred. 4. Proven and reliable connectology 5. Increased inactivation of organisms at the patient connection if a touch contamination occurs 6. Easy to learn and use system for all patients 13 CAPD
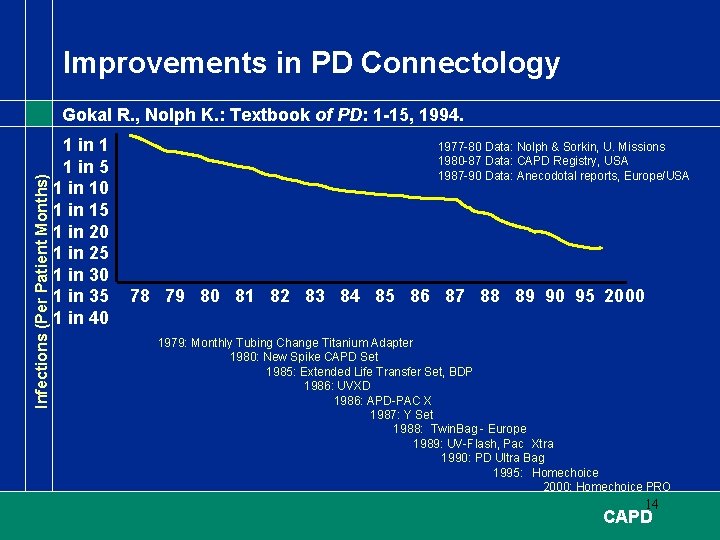
Improvements in PD Connectology Infections (Per Patient Months) Gokal R. , Nolph K. : Textbook of PD: 1 -15, 1994. 1 in 1 1 in 5 1 in 10 1 in 15 1 in 20 1 in 25 1 in 30 1 in 35 1 in 40 1977 -80 Data: Nolph & Sorkin, U. Missions 1980 -87 Data: CAPD Registry, USA 1987 -90 Data: Anecodotal reports, Europe/USA 78 79 80 81 82 83 84 85 86 87 88 89 90 95 2000 1979: Monthly Tubing Change Titanium Adapter 1980: New Spike CAPD Set 1985: Extended Life Transfer Set, BDP 1986: UVXD 1986: APD-PAC X 1987: Y Set 1988: Twin. Bag - Europe 1989: UV-Flash, Pac Xtra 1990: PD Ultra Bag 1995: Homechoice 2000: Homechoice PRO 14 CAPD
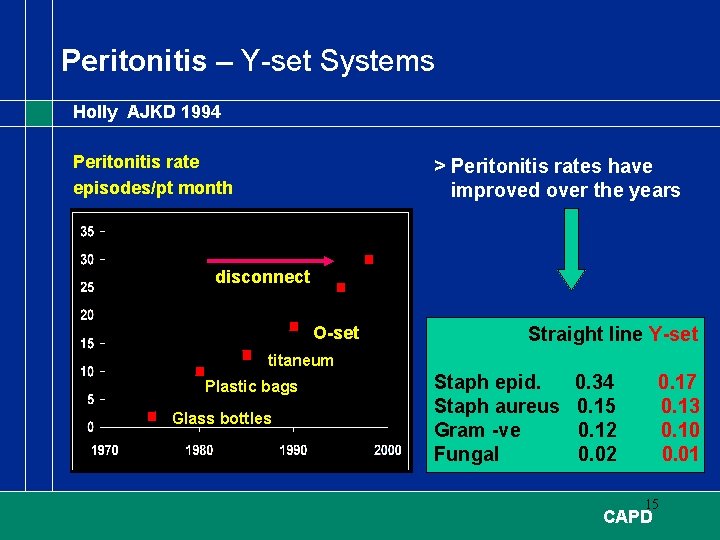
Peritonitis – Y-set Systems Holly AJKD 1994 Peritonitis rate episodes/pt month > Peritonitis rates have improved over the years disconnect O-set Straight line Y-set titaneum Plastic bags Glass bottles Staph epid. Staph aureus Gram -ve Fungal 0. 34 0. 15 0. 12 0. 02 0. 17 0. 13 0. 10 0. 01 15 CAPD
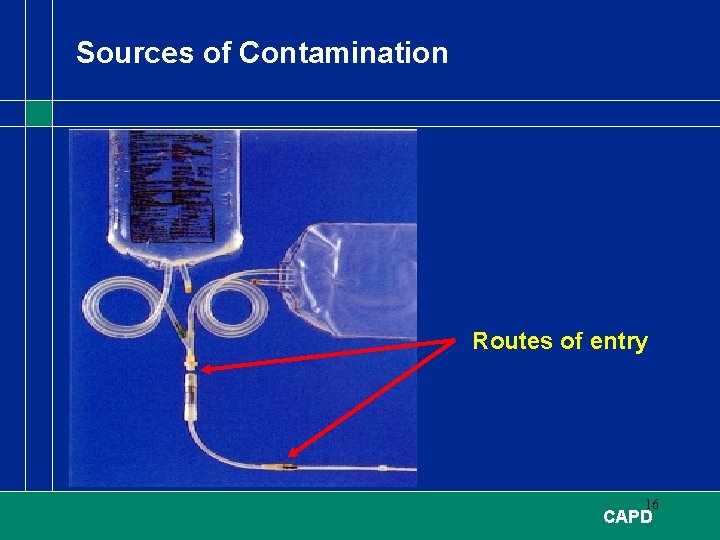
Sources of Contamination Routes of entry 16 CAPD
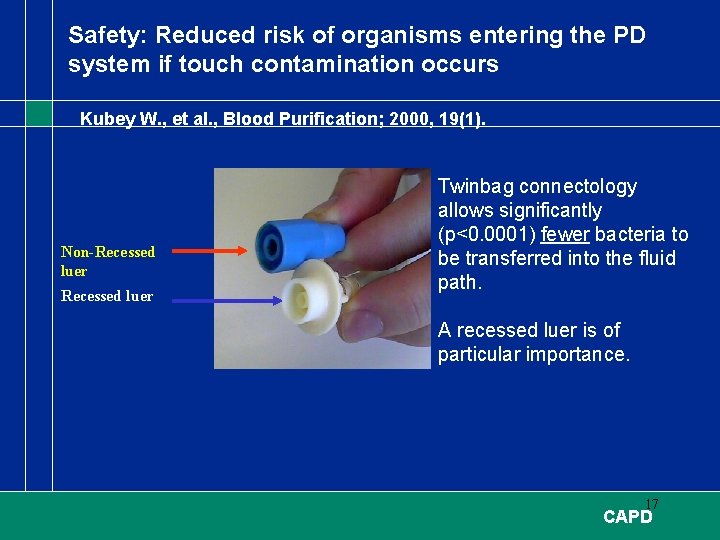
Safety: Reduced risk of organisms entering the PD system if touch contamination occurs Kubey W. , et al. , Blood Purification; 2000, 19(1). Non-Recessed luer Twinbag connectology allows significantly (p<0. 0001) fewer bacteria to be transferred into the fluid path. A recessed luer is of particular importance. 17 CAPD
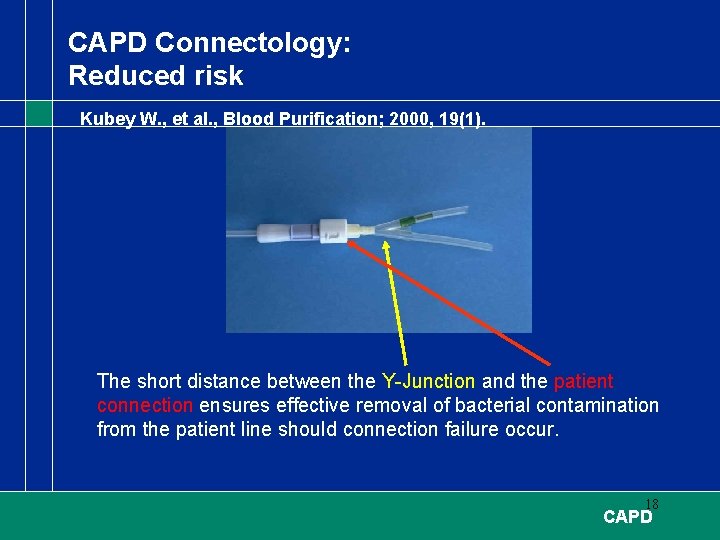
CAPD Connectology: Reduced risk Kubey W. , et al. , Blood Purification; 2000, 19(1). The short distance between the Y-Junction and the patient connection ensures effective removal of bacterial contamination from the patient line should connection failure occur. 18 CAPD
- Slides: 18