Therapy Modality Automated Peritoneal Dialysis APD Renal Division
- Slides: 31
Therapy Modality: Automated Peritoneal Dialysis (APD) Renal Division Baxter Healthcare
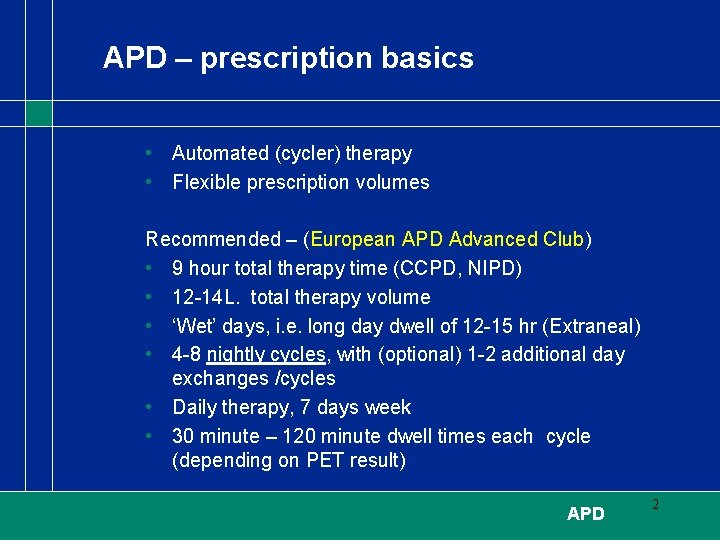
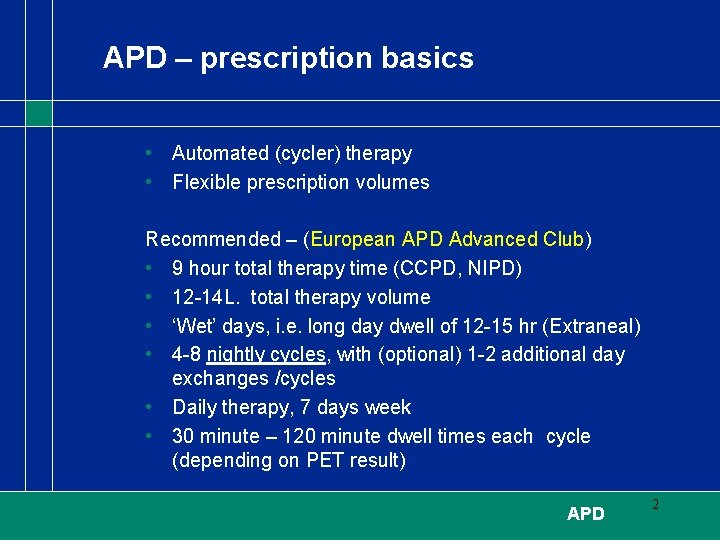
APD – prescription basics • Automated (cycler) therapy • Flexible prescription volumes Recommended – (European APD Advanced Club) • 9 hour total therapy time (CCPD, NIPD) • 12 -14 L. total therapy volume • ‘Wet’ days, i. e. long day dwell of 12 -15 hr (Extraneal) • 4 -8 nightly cycles, with (optional) 1 -2 additional day exchanges /cycles • Daily therapy, 7 days week • 30 minute – 120 minute dwell times each cycle (depending on PET result) APD 2
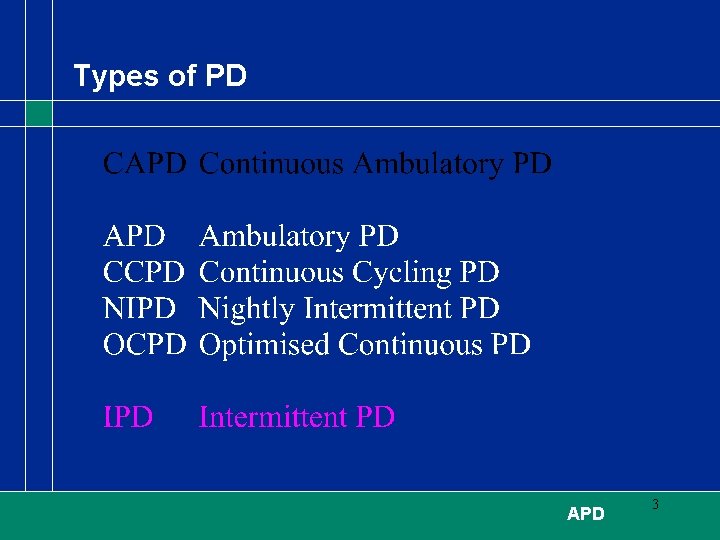
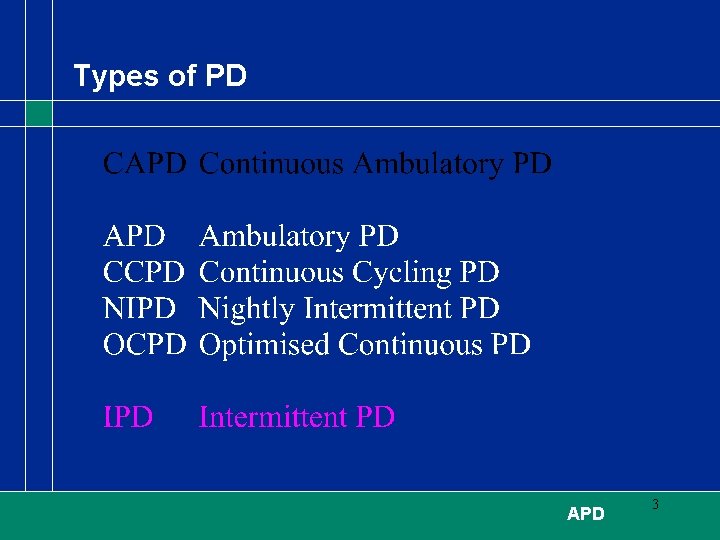
Types of PD APD 3
APD benefits 1. Optimum dialysis for high transporters, large body surface area, and minimal residual renal function 2. Offers potential for better clearances than in CAPD 3. Volumetric control of fill, drain and therapy volume delivery 4. Supine positions at night permit larger fill volumes, a major determinant of treatment adequacy 5. Short dwells may increase ultrafiltration & clearance APD 4
APD benefits 7. Reduced risk of intra-peritoneal pressure complications: hernias, leak, back pain, reduced appetite 8. Reported lower incidence of peritonitis than CAPD 9. Treatment of choice for children – avoids school interruptions and encourages peer integration (“normality”) 10. Daytime freedom and comfort APD 5
APD benefits 11. Employment and school uninterrupted 12. Improved patient compliance 13. Increased patient comfort 14. Possible to monitor patient compliance at home APD 6
Clinical Practice Guidelines of the Canadian Society of Nephrology for treatments of Patients with CRF JASN 10: S 287 -S 321, 1999 ‘A prescription that is compatible with the patient’s preferences and lifestyle is likely to reduce the risk of patient « burnout » and noncompliance’ APD 7
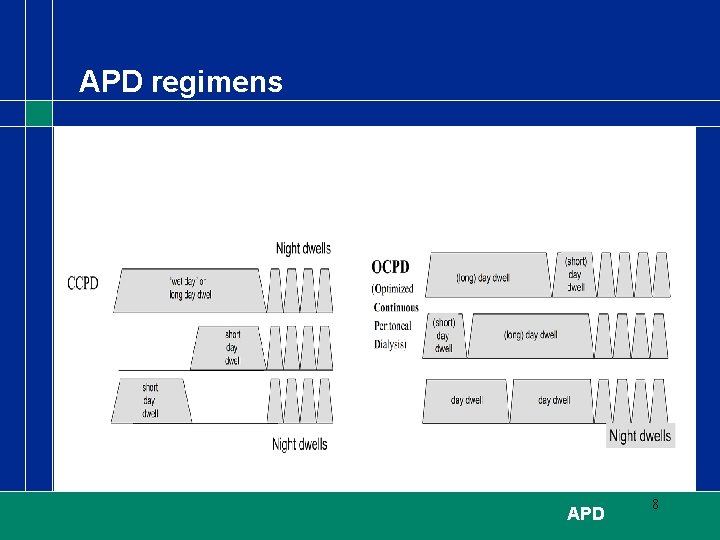
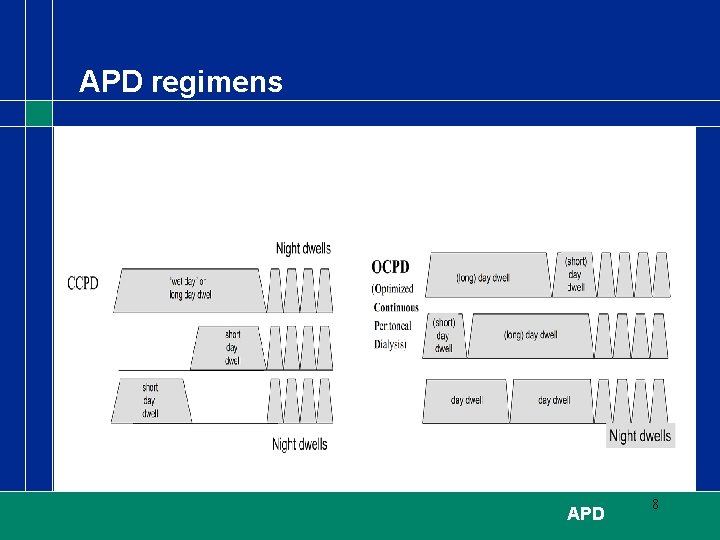
APD regimens APD 8
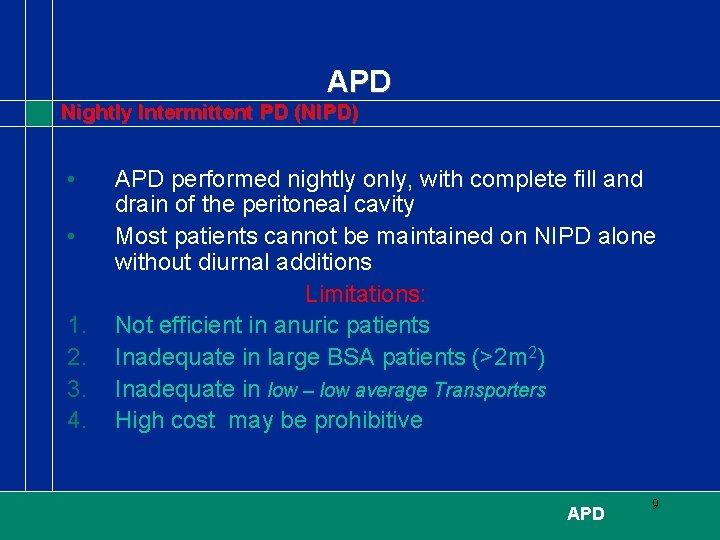
APD Nightly Intermittent PD (NIPD) • • 1. 2. 3. 4. APD performed nightly only, with complete fill and drain of the peritoneal cavity Most patients cannot be maintained on NIPD alone without diurnal additions Limitations: Not efficient in anuric patients Inadequate in large BSA patients (>2 m 2) Inadequate in low – low average Transporters High cost may be prohibitive APD 9
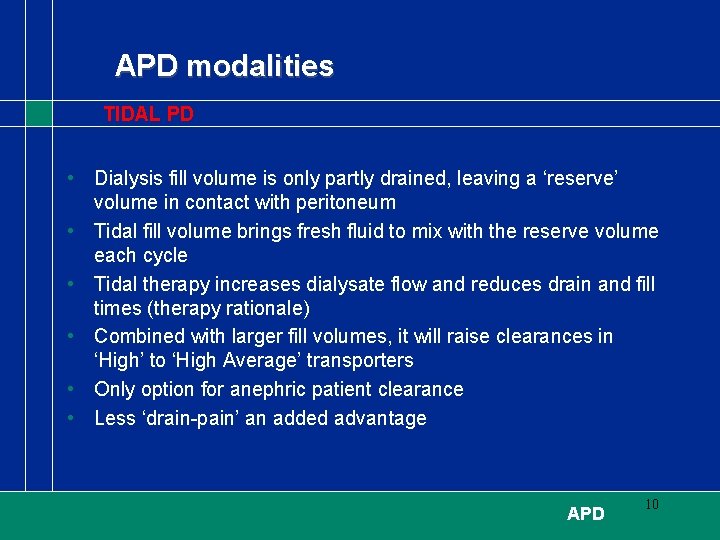
APD modalities TIDAL PD • Dialysis fill volume is only partly drained, leaving a ‘reserve’ volume in contact with peritoneum • Tidal fill volume brings fresh fluid to mix with the reserve volume each cycle • Tidal therapy increases dialysate flow and reduces drain and fill times (therapy rationale) • Combined with larger fill volumes, it will raise clearances in ‘High’ to ‘High Average’ transporters • Only option for anephric patient clearance • Less ‘drain-pain’ an added advantage APD 10
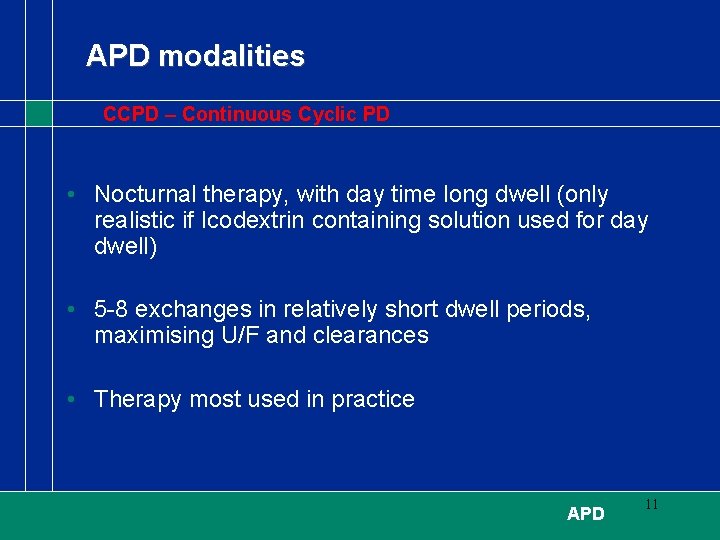
APD modalities CCPD – Continuous Cyclic PD • Nocturnal therapy, with day time long dwell (only realistic if Icodextrin containing solution used for day dwell) • 5 -8 exchanges in relatively short dwell periods, maximising U/F and clearances • Therapy most used in practice APD 11
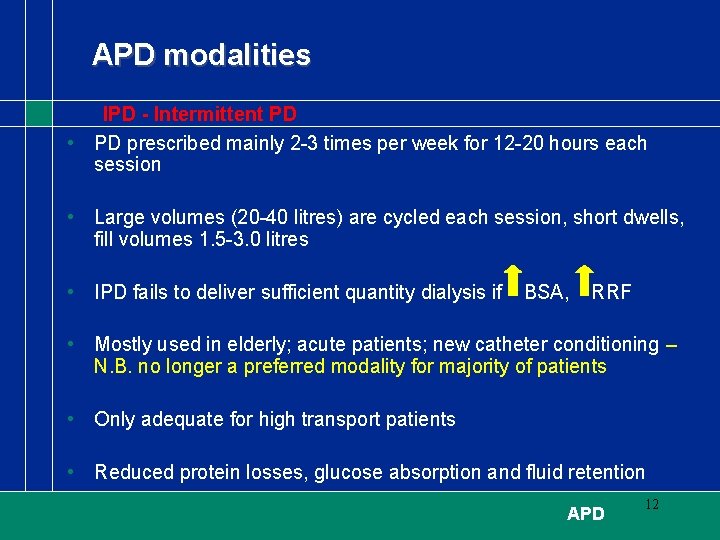
APD modalities IPD - Intermittent PD • PD prescribed mainly 2 -3 times per week for 12 -20 hours each session • Large volumes (20 -40 litres) are cycled each session, short dwells, fill volumes 1. 5 -3. 0 litres • IPD fails to deliver sufficient quantity dialysis if BSA, RRF • Mostly used in elderly; acute patients; new catheter conditioning – N. B. no longer a preferred modality for majority of patients • Only adequate for high transport patients • Reduced protein losses, glucose absorption and fluid retention APD 12
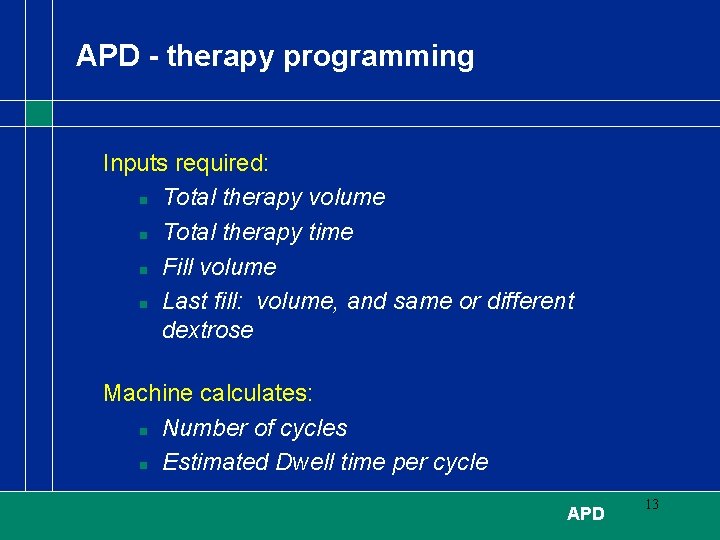
APD - therapy programming Inputs required: n Total therapy volume n Total therapy time n Fill volume n Last fill: volume, and same or different dextrose Machine calculates: n Number of cycles n Estimated Dwell time per cycle APD 13
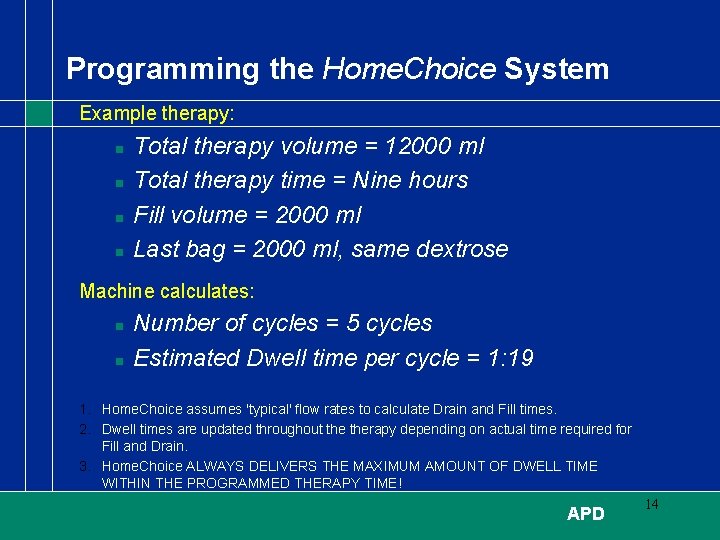
Programming the Home. Choice System Example therapy: n n Total therapy volume = 12000 ml Total therapy time = Nine hours Fill volume = 2000 ml Last bag = 2000 ml, same dextrose Machine calculates: n n Number of cycles = 5 cycles Estimated Dwell time per cycle = 1: 19 1. Home. Choice assumes 'typical' flow rates to calculate Drain and Fill times. 2. Dwell times are updated throughout therapy depending on actual time required for Fill and Drain. 3. Home. Choice ALWAYS DELIVERS THE MAXIMUM AMOUNT OF DWELL TIME WITHIN THE PROGRAMMED THERAPY TIME! APD 14
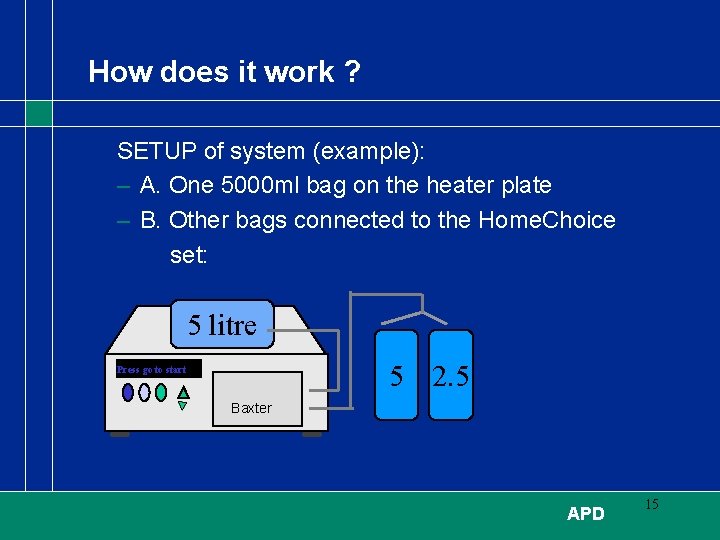
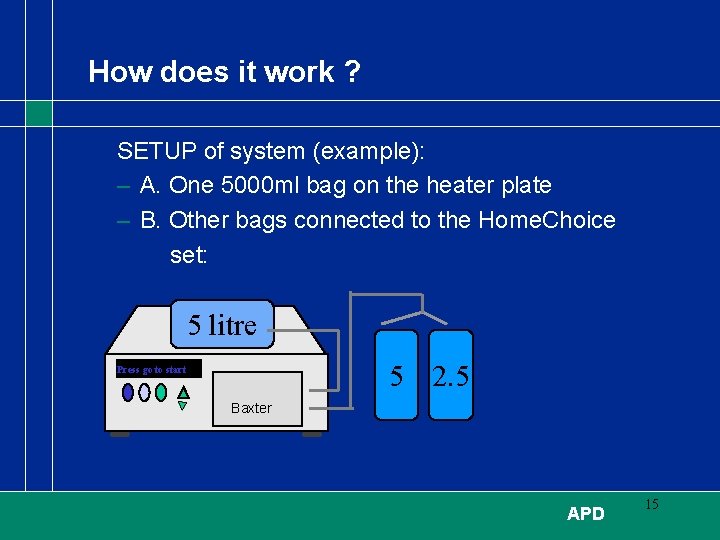
How does it work ? SETUP of system (example): – A. One 5000 ml bag on the heater plate – B. Other bags connected to the Home. Choice set: 5 litre 5 2. 5 Press go to start Baxter APD 15
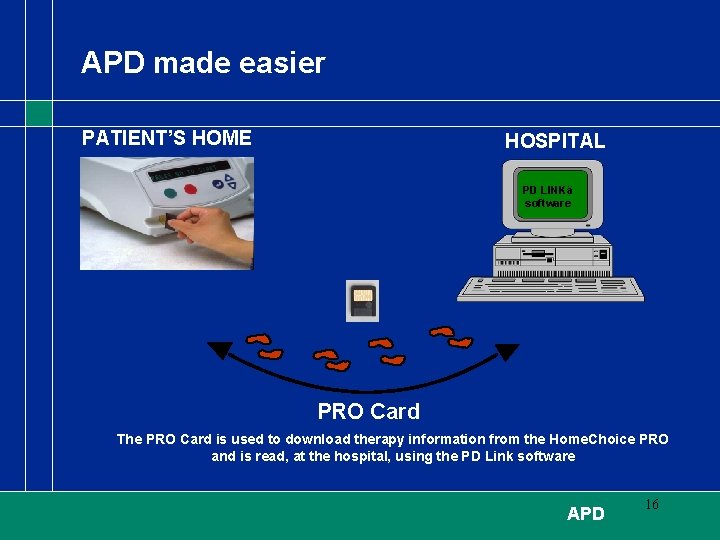
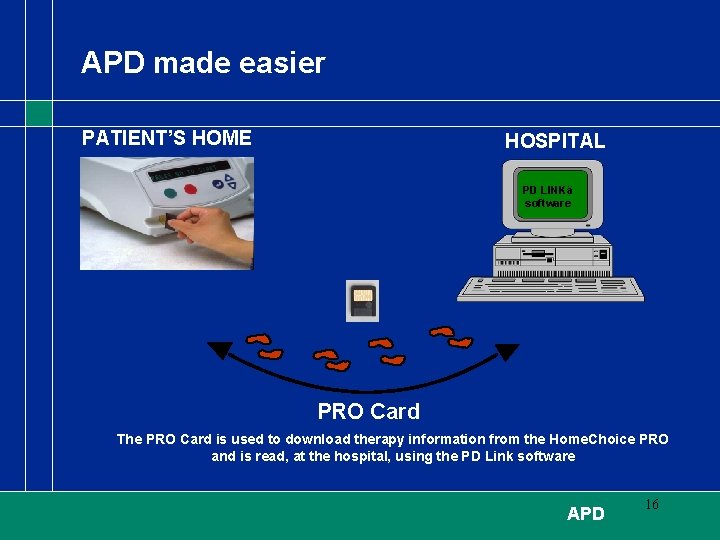
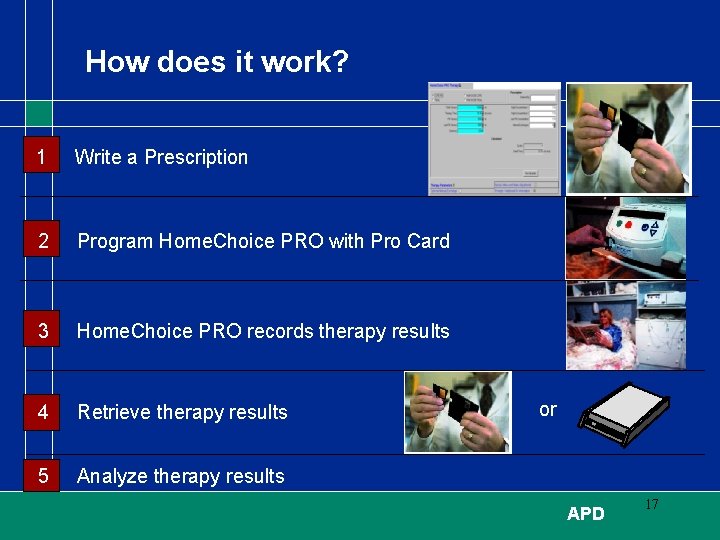
APD made easier PATIENT’S HOME HOSPITAL PD LINKä software PRO Card The PRO Card is used to download therapy information from the Home. Choice PRO and is read, at the hospital, using the PD Link software APD 16
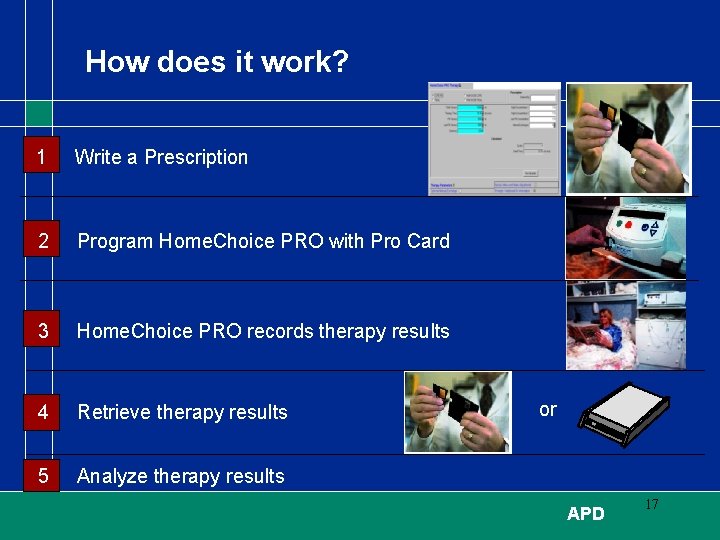
How does it work? 1 Write a Prescription 2 Program Home. Choice PRO with Pro Card 3 Home. Choice PRO records therapy results 4 Retrieve therapy results or 5 Analyze therapy results APD 17
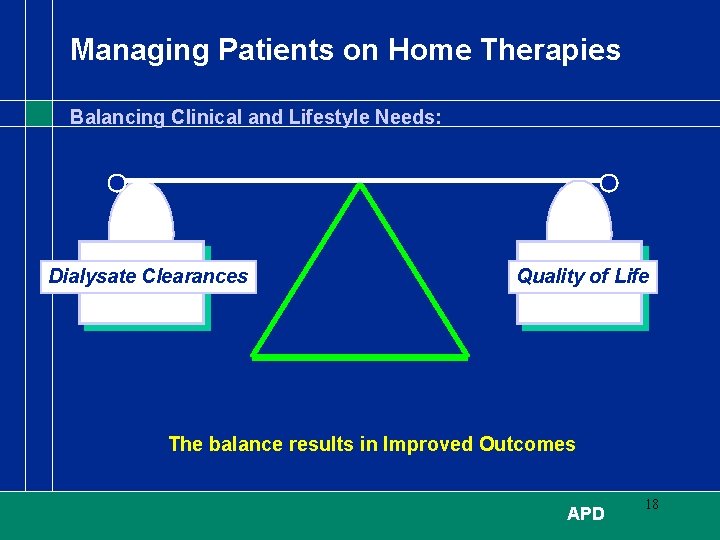
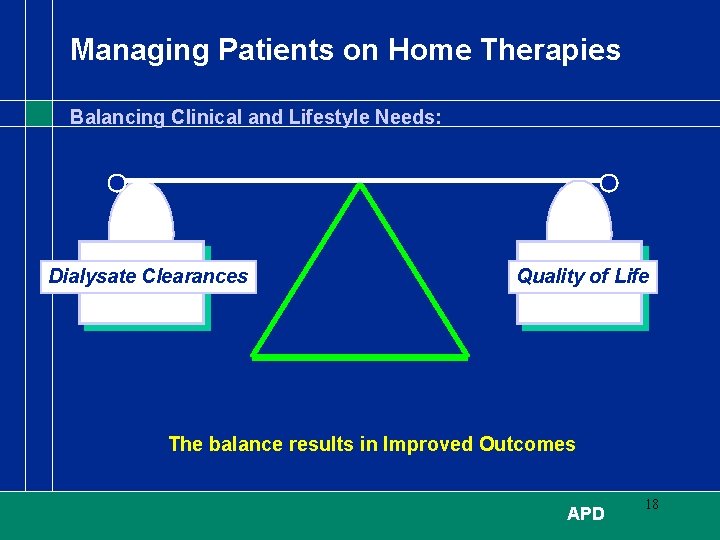
Managing Patients on Home Therapies Balancing Clinical and Lifestyle Needs: Dialysate Clearances Quality of Life The balance results in Improved Outcomes APD 18
Procedural Modifications - to improve UF 1 2 3 4 APD 19
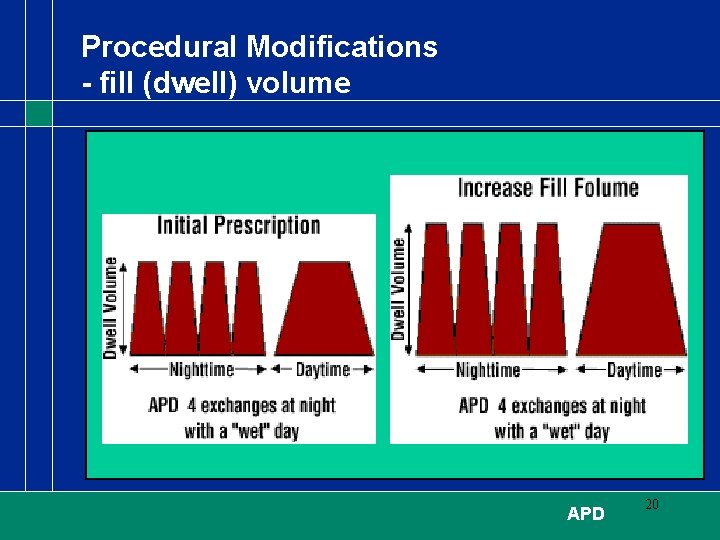
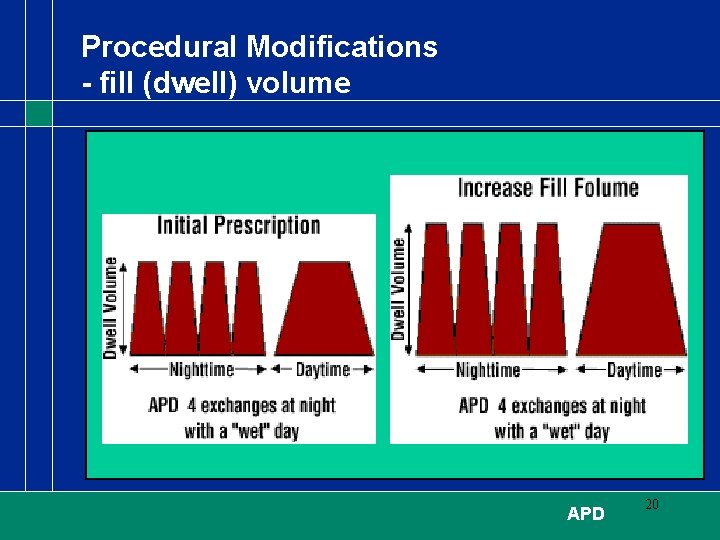
Procedural Modifications - fill (dwell) volume APD 20
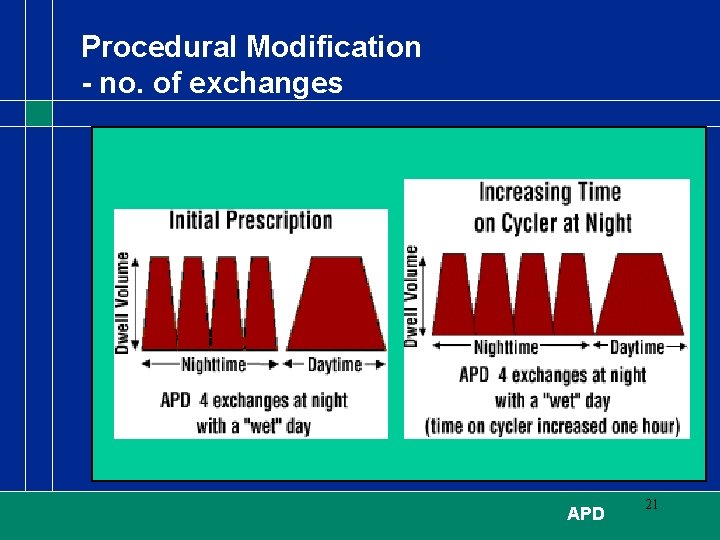
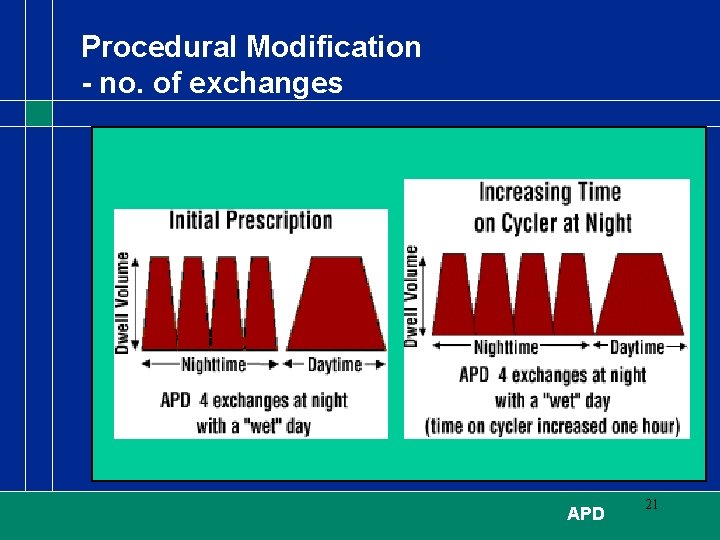
Procedural Modification - no. of exchanges APD 21
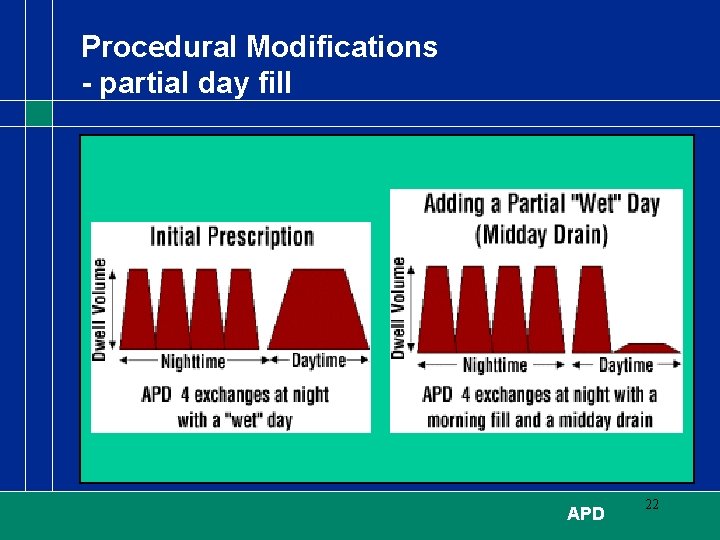
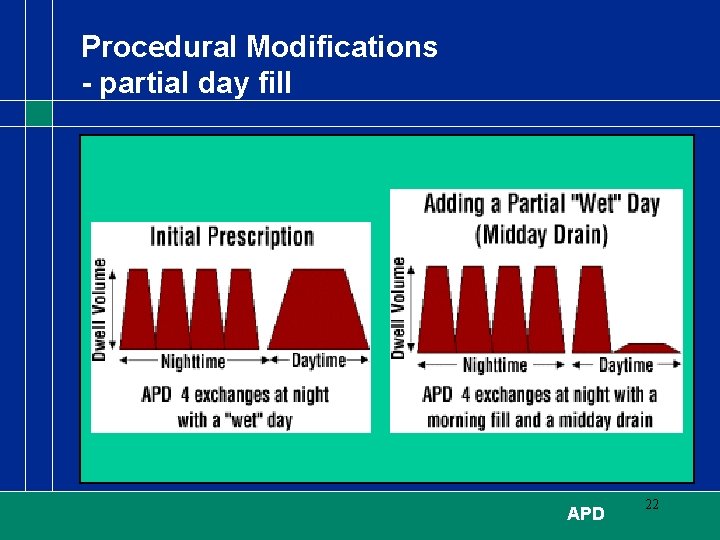
Procedural Modifications - partial day fill APD 22
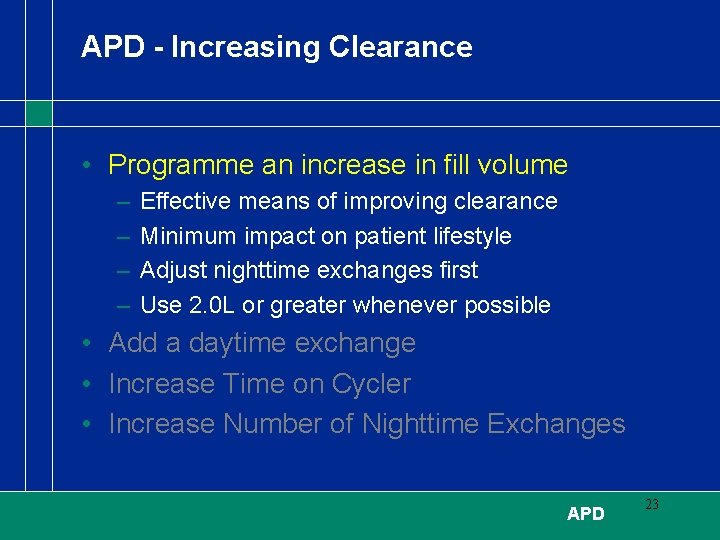
APD - Increasing Clearance • Programme an increase in fill volume – – Effective means of improving clearance Minimum impact on patient lifestyle Adjust nighttime exchanges first Use 2. 0 L or greater whenever possible • Add a daytime exchange • Increase Time on Cycler • Increase Number of Nighttime Exchanges APD 23
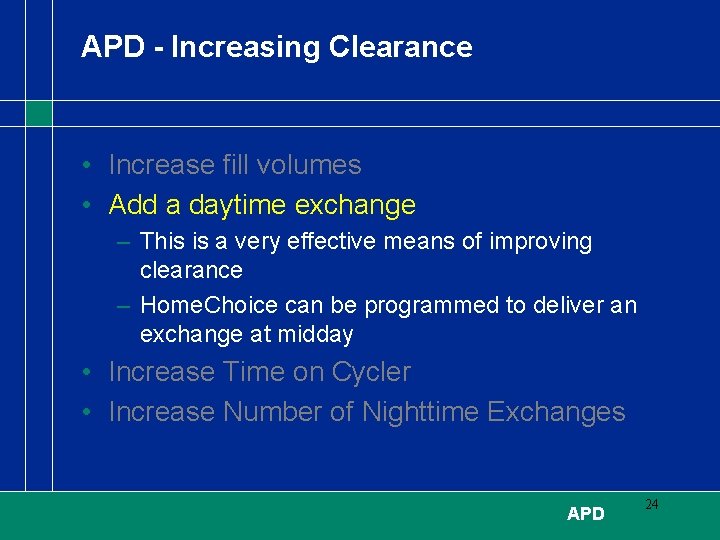
APD - Increasing Clearance • Increase fill volumes • Add a daytime exchange – This is a very effective means of improving clearance – Home. Choice can be programmed to deliver an exchange at midday • Increase Time on Cycler • Increase Number of Nighttime Exchanges APD 24
APD - Increasing Clearance • Increase fill volumes • Add a daytime exchange • Increase Programmed Time on Cycler – Cycler time can be extended to 10 hours – Increasing cycler time with a constant number of exchanges increases dwell time which increases clearance • Increase Number of Night-time Exchanges - May increase clearance, but only if dwell time on cycler is also increased APD 25
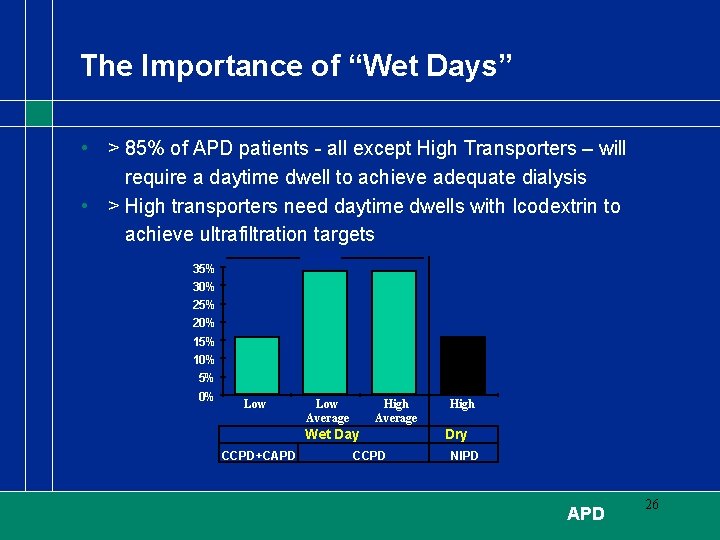
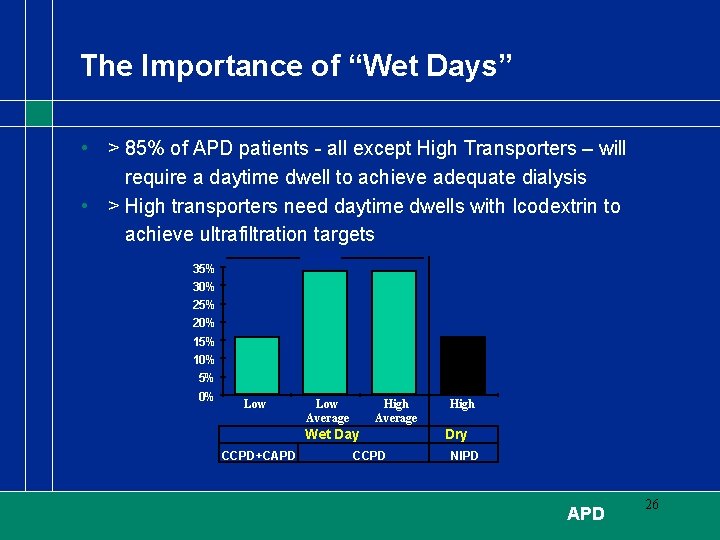
The Importance of “Wet Days” • > 85% of APD patients - all except High Transporters – will require a daytime dwell to achieve adequate dialysis • > High transporters need daytime dwells with Icodextrin to achieve ultrafiltration targets > 85% 30% 25% 20% 15% 10% 5% 0% Low Average High Average Wet Day CCPD+CAPD CCPD High Dry Day NIPD APD 26
Fluid Balance - General Guidelines for APD Evaluation and Management of Ultrafiltration problems in PD, ISPD Recommendations, PDI Vol 20, suppl 4, 2000 • Avoidance of long dwells with low glucose • Use of mid-day drain even when no additional exchange is needed for clearance • “The most frequently ignored principles in PD that lead to UF difficulties are the need to avoid long glucose dwells in high transporters and balancing glucose concentration and dwell time” APD 27
Designing the Optimal APD Therapy Fact: APD utilizes shorter dwell times, relative to CAPD. Therefore, more solution volume is needed to provide adequate clearance Fiction: More total solution volume will always provide better clearance for APD patients The Key to success with APD is a balance of: Solution Volume and Dwell Time Excessive solution volume = too many cycles = wasted time filling and draining = reduced clearances APD 28
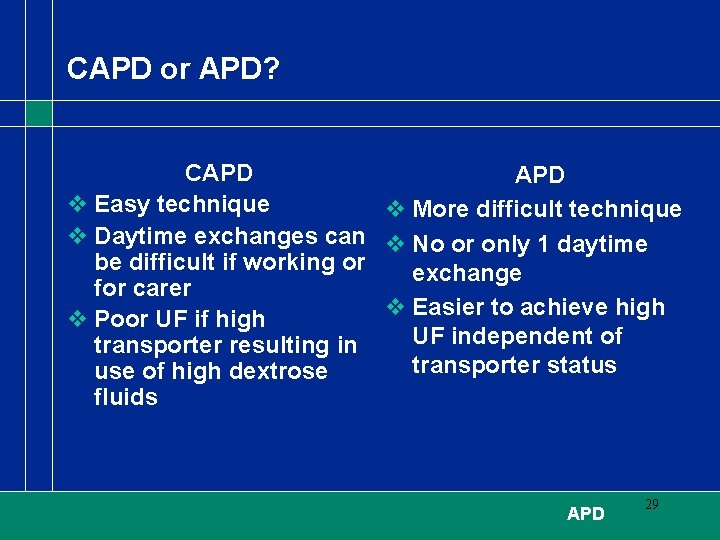
CAPD or APD? CAPD v Easy technique v More difficult technique v Daytime exchanges can v No or only 1 daytime be difficult if working or exchange for carer v Easier to achieve high v Poor UF if high UF independent of transporter resulting in transporter status use of high dextrose fluids APD 29
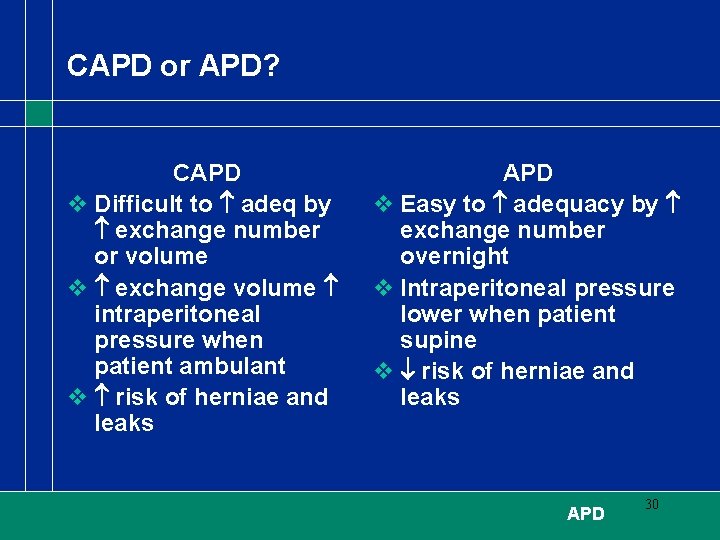
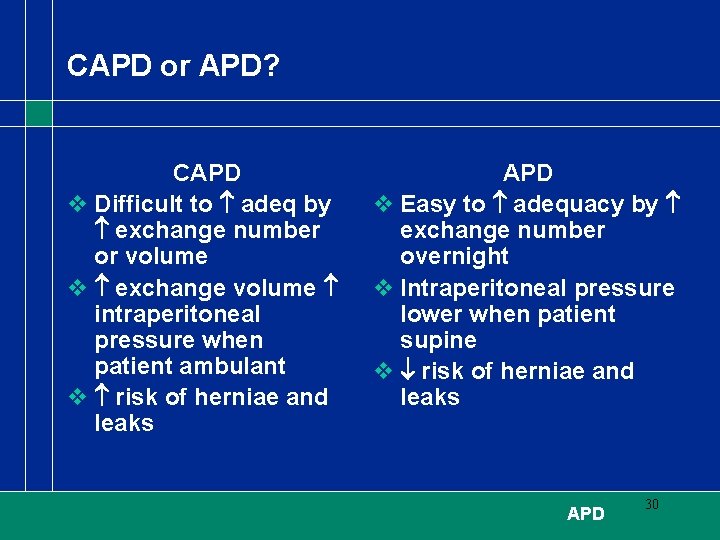
CAPD or APD? CAPD v Difficult to adeq by exchange number or volume v exchange volume intraperitoneal pressure when patient ambulant v risk of herniae and leaks APD v Easy to adequacy by exchange number overnight v Intraperitoneal pressure lower when patient supine v risk of herniae and leaks APD 30
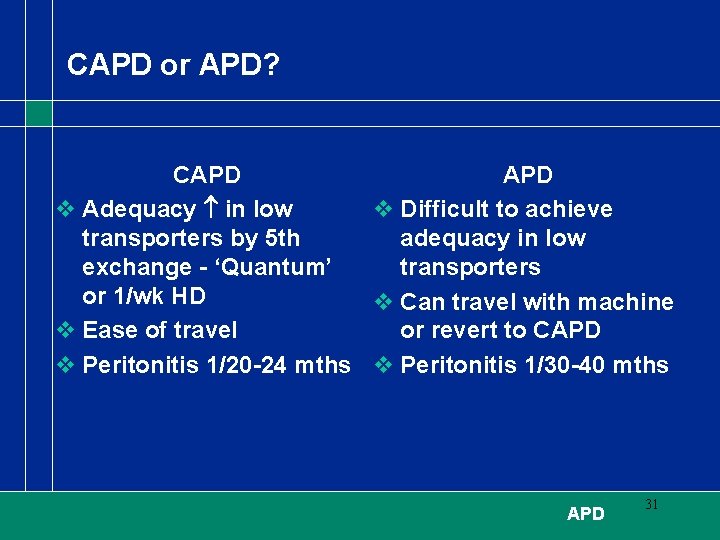
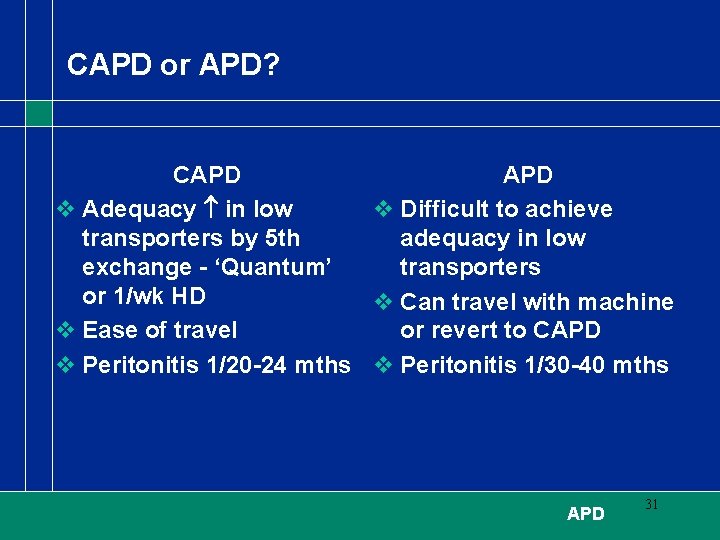
CAPD or APD? CAPD v Adequacy in low v Difficult to achieve transporters by 5 th adequacy in low exchange - ‘Quantum’ transporters or 1/wk HD v Can travel with machine v Ease of travel or revert to CAPD v Peritonitis 1/20 -24 mths v Peritonitis 1/30 -40 mths APD 31