The Victorian Dysphagia Screening Model This model has

- Slides: 63
The Victorian Dysphagia Screening Model This model has been endorsed by: Victorian Stroke Clinical Network
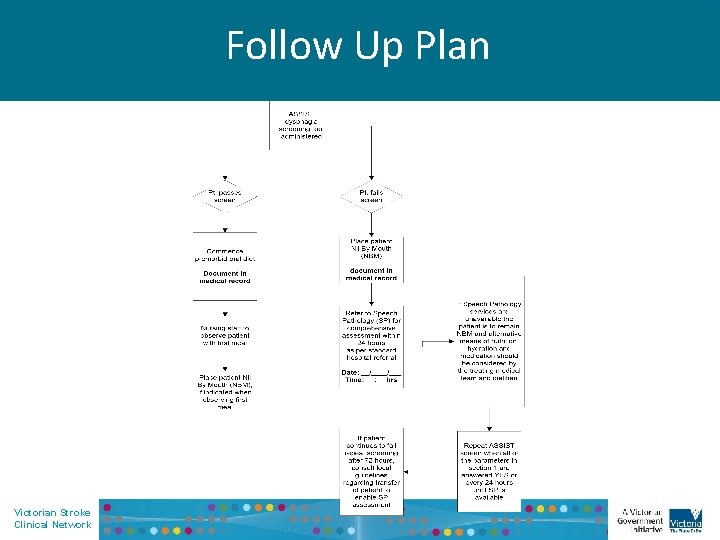
Objectives At the conclusion of this presentation and subsequent reflection you should be able to: • Outline the history of the Victorian Dysphagia Screening Project • Describe the components of normal swallow • Discuss the elements of the ASSIST dysphagia assessment tool • Follow the follow up plan recommendations Victorian Stroke Clinical Network
The Victorian Stroke Clinical Network (VSCN) Background • Stroke Care Strategy for Victoria released Sept. 2007 (Stroke Week) • 28 Recommendations • Establishment of the Victorian Stroke Clinical Network (VSCN) in October 2007 to oversee the implementation of the strategy • In 2008 the Victorian Dysphagia Screening Project (VDSP) commenced with the aim to develop a state wide consistent model for dysphagia screening. Victorian Stroke Clinical Network
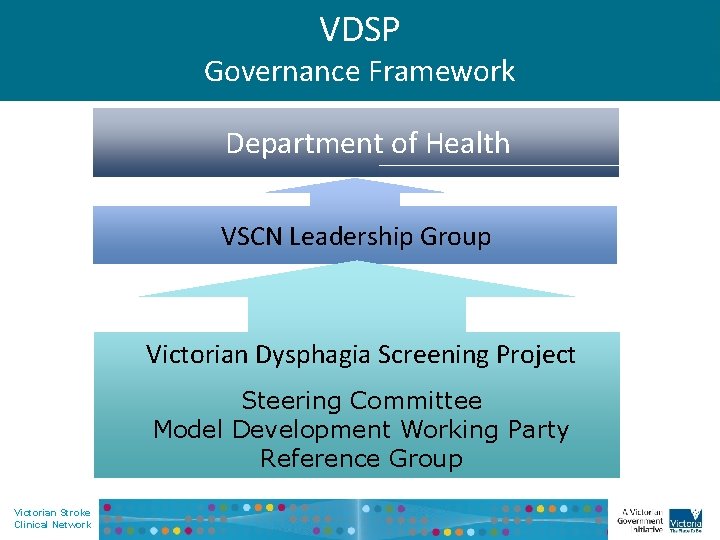
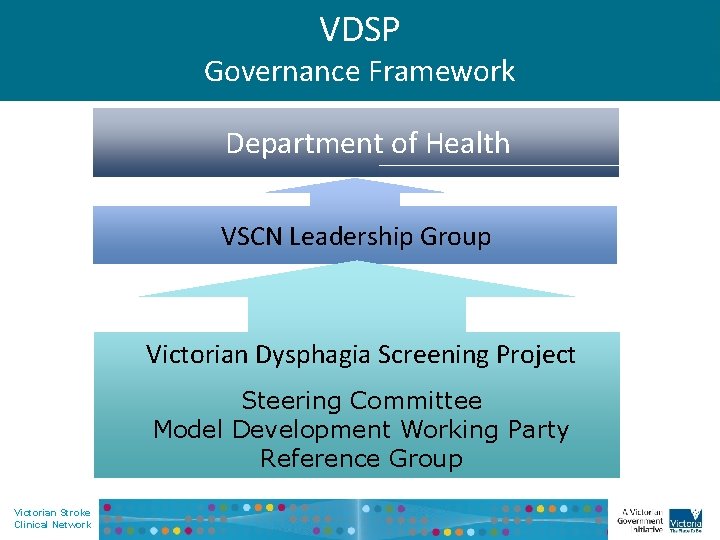
VDSP Governance Framework Department of Health VSCN Leadership Group Victorian Dysphagia Screening Project Steering Committee Model Development Working Party Reference Group Victorian Stroke Clinical Network
2010 National Stroke Foundation Clinical Guidelines 1 6. 2. 1 Dysphagia a). Patient’s should be screened for swallowing deficits before being given food, drink or oral medications. Personnel specifically trained in swallowing screening using a validated tool should undertake screening. b). Swallowing should be screened for as soon as possible but at least within 24 hours of admission. Victorian Stroke Clinical Network
Impact of Dysphagia • • Aspiration Pneumonia 2, 3, 4, 11 Malnutrition 2, 3, 4 Dehydration 2, 3, 4 Increased length of stay 2, 3, 4, 12 Increased Mortality 2, 3, 4 Increased Disability 2, 3, 4 Institutional Care at Discharge 2, 3, 4 Victorian Stroke Clinical Network
Incidence of Dysphagia • 80% incidence of dysphagia in the first two days • 50 -80% incidence of dysphagia at one week 5, 6 7, 8 • 64% incidence at first ten days • Dysphagia persists in up to 11% of patients at six month follow up 7, 8 9 Victorian Stroke Clinical Network
Current Evidence Base • Validity data supports use of dysphagia screening • Formal dysphagia screening programs reduces: - the incidence of aspiration pneumonia, - length of hospital stay and - time spent without nutrition for stroke patients 14, 15, 16 Victorian Stroke Clinical Network
Dysphagia Victorian Stroke Clinical Network
What is Dysphagia? Dysphagia is a disorder or a symptom that can be caused by structural, physiological and /or neurological impairments affecting the preparatory, oral, pharyngeal, and/or oesophageal stages 19 It describes any difficulty moving food from the mouth to the stomach 17 Victorian Stroke Clinical Network
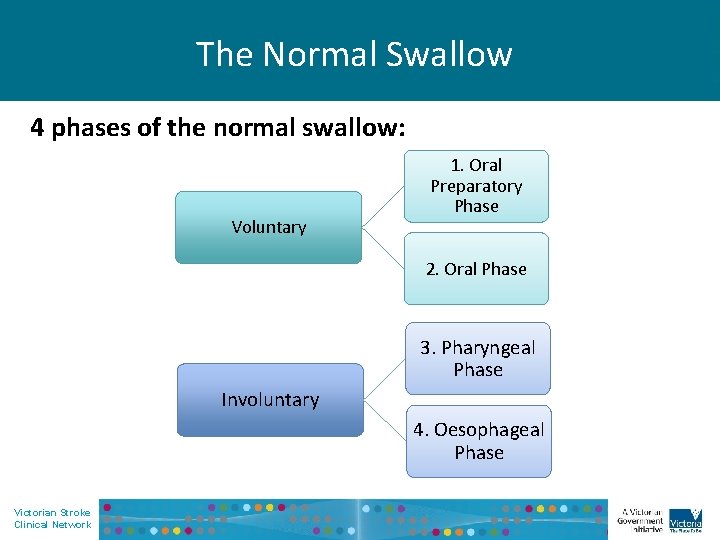
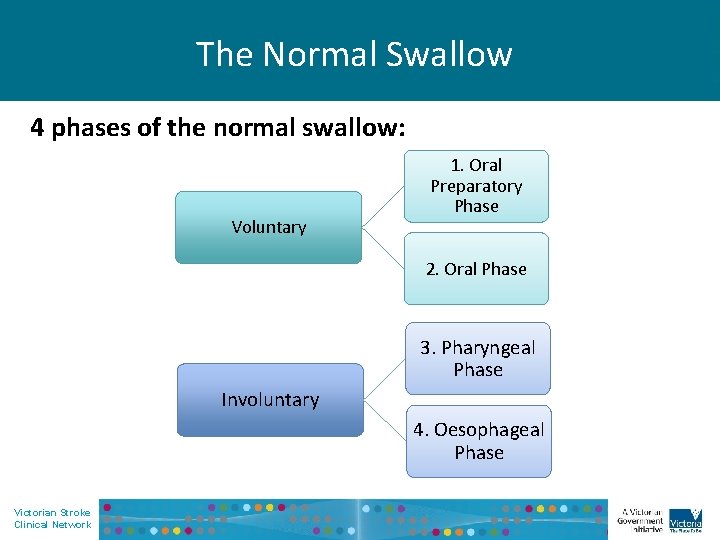
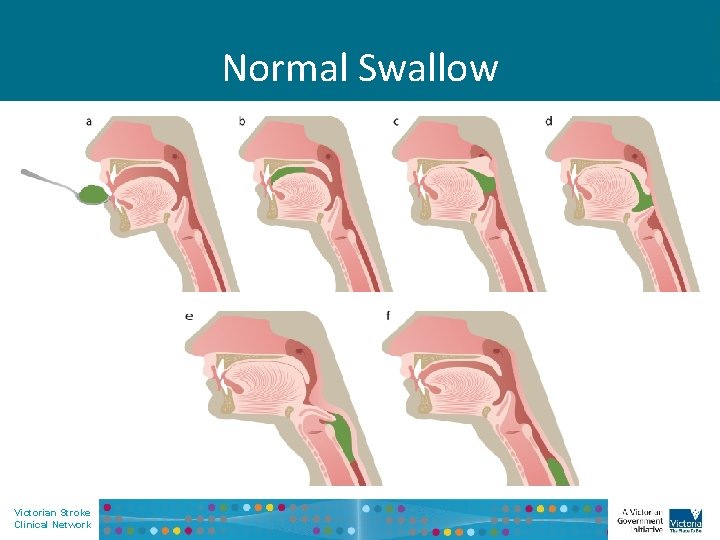
The Normal Swallow 4 phases of the normal swallow: Voluntary 1. Oral Preparatory Phase 2. Oral Phase 3. Pharyngeal Phase Involuntary 4. Oesophageal Phase Victorian Stroke Clinical Network
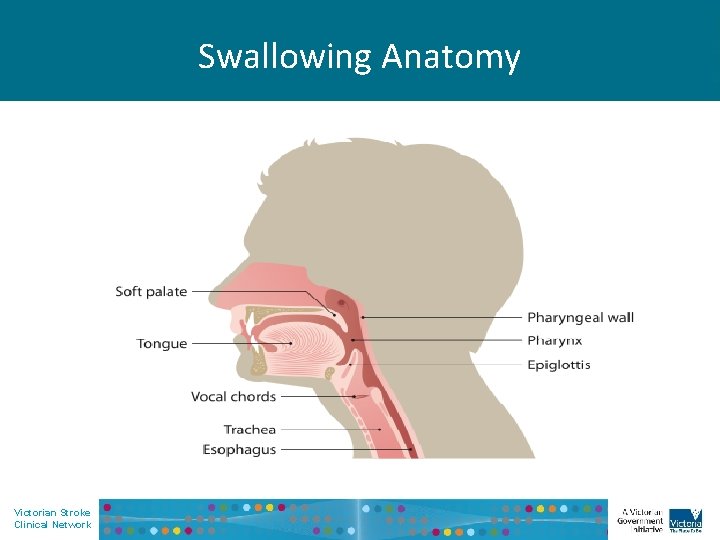
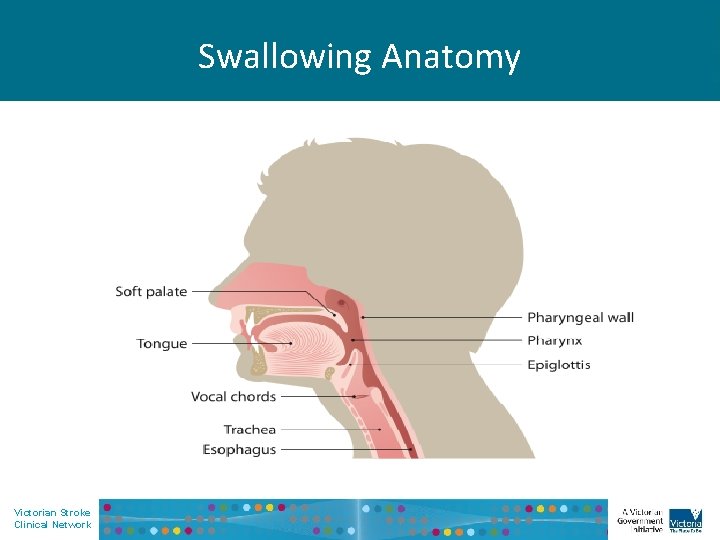
Swallowing Anatomy • Insert images Victorian Stroke Clinical Network
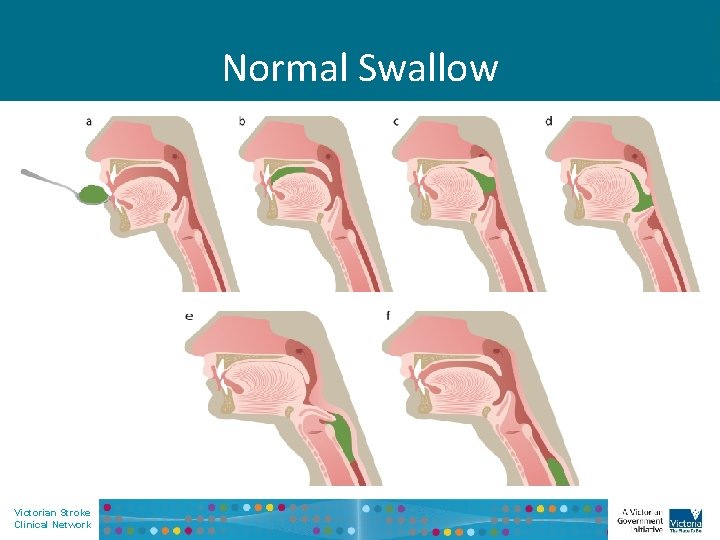
Normal Swallow Victorian Stroke Clinical Network
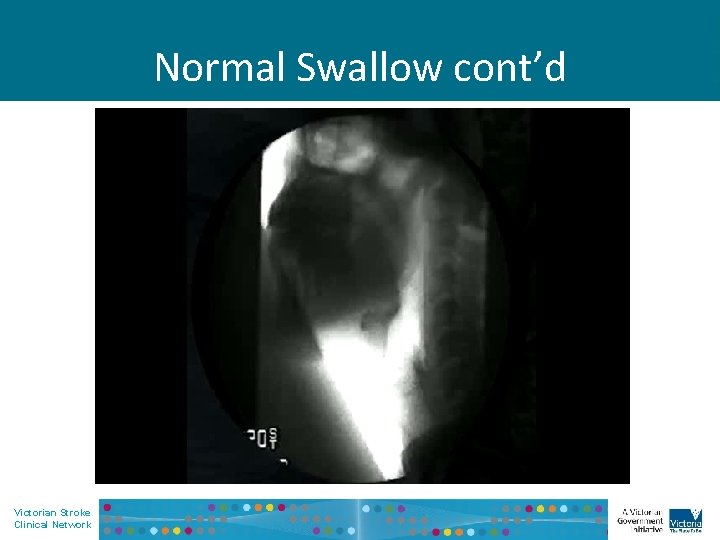
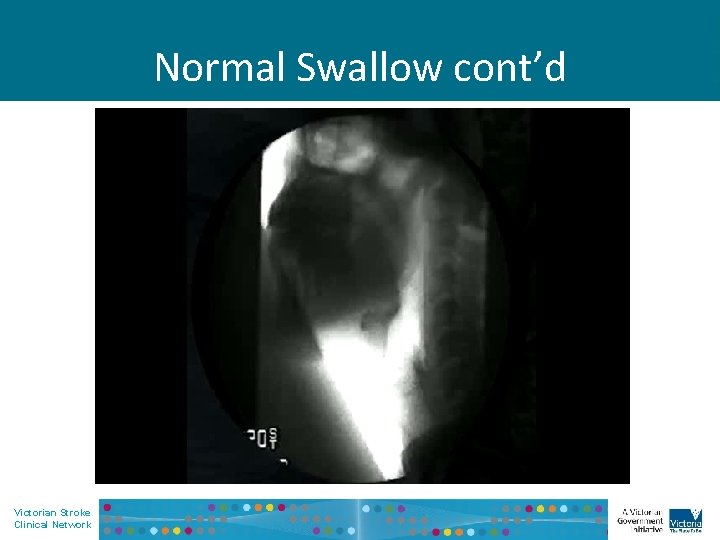
Normal Swallow cont’d Victorian Stroke Clinical Network
1. Oral Preparatory Phase • • Prepares the mouth for the bolus and fluid The larynx and pharynx are relaxed Airway is open Requires senses of taste, temperature and touch formation of a bolus to the right size and consistency 17 Victorian Stroke Clinical Network
2. Oral Phase Voluntary Phase • Begins with placement of food in the mouth • Lips/Cheeks seal – Food is chewed, mixed with saliva and gathered to form the bolus. • Soft palate rests against back of tongue. • The larynx and pharynx are at rest and the airway is open. Victorian Stroke Clinical Network
2. Oral Phase Voluntary phase • Initiated when the tongue begins to move the bolus towards the pharynx • Once the bolus reaches the pharynx the oral stage of the swallow is terminated. Victorian Stroke Clinical Network
3. Pharyngeal Phase Involuntary Phase • Begins with triggering of the swallow reflex - Breathing suspended - Soft palate meets pharyngeal wall - Larynx elevates and airway seals - Bolus squeezed through oropharynx - Upper oesophageal sphincter opens to allow food into oesophagus Victorian Stroke Clinical Network
4. Oesophageal Phase Involuntary Phase • Closure of upper oesophageal sphincter to prevent regurgitation • The hyoid bone is released and moves back to its resting position. The individual breaths out • Food moves down toward stomach Victorian Stroke Clinical Network
Oral Dysphagia • • • Reduced awareness of the bolus Lip weakness Slow and laboured chewing Poor bolus control and formation Oral residue Victorian Stroke Clinical Network
Impaired Swallow • A number of functions can become impaired at the oral stage of the swallow including: • Reduced awareness of the bolus • Lip weakness • Slow and labored chewing • Poor bolus control and formation • Oral residue • The presence of one or most of these impairments can have a significant impact on the patients health and ability to swallow safely. Victorian Stroke Clinical Network
Pharyngeal Dysphagia • • • Delayed or absent swallow reflex Premature spillage into pharynx Penetration into the larynx Pharyngeal pooling Reduced laryngeal excursion Victorian Stroke Clinical Network
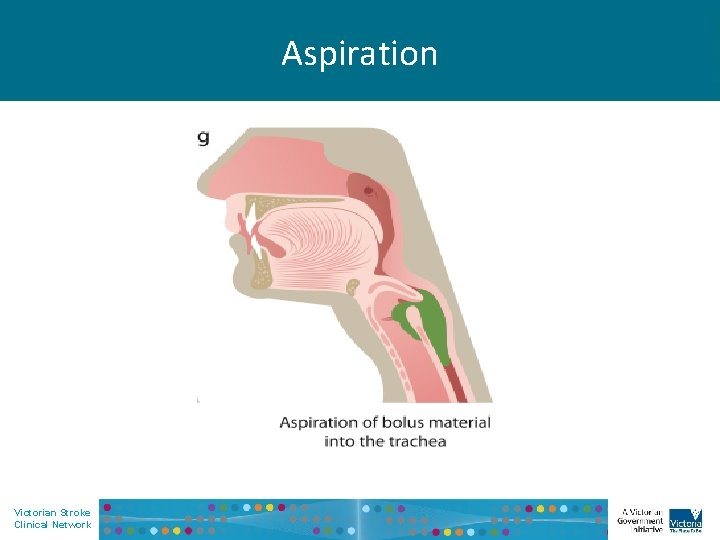
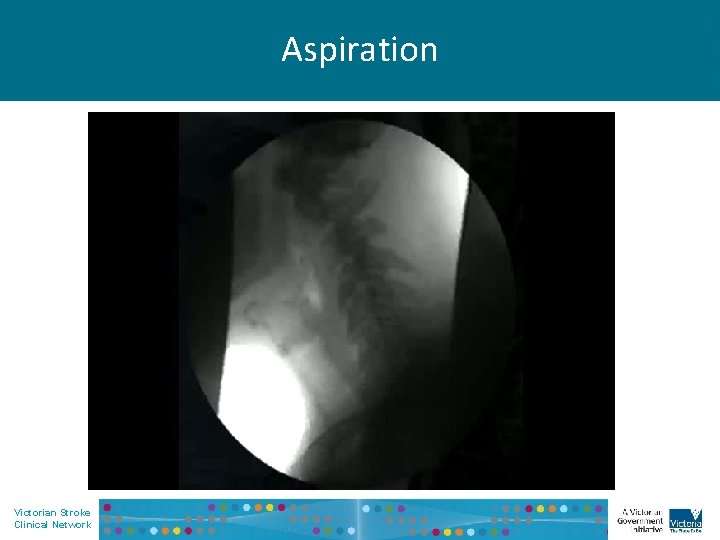
Aspiration • Aspiration refers to the passing of food or fluid below the level of the vocal folds toward the lungs • Commonly occurs from impairment in the swallow function • Aspiration can be overt or silent • May result in aspiration pneumonia Victorian Stroke Clinical Network
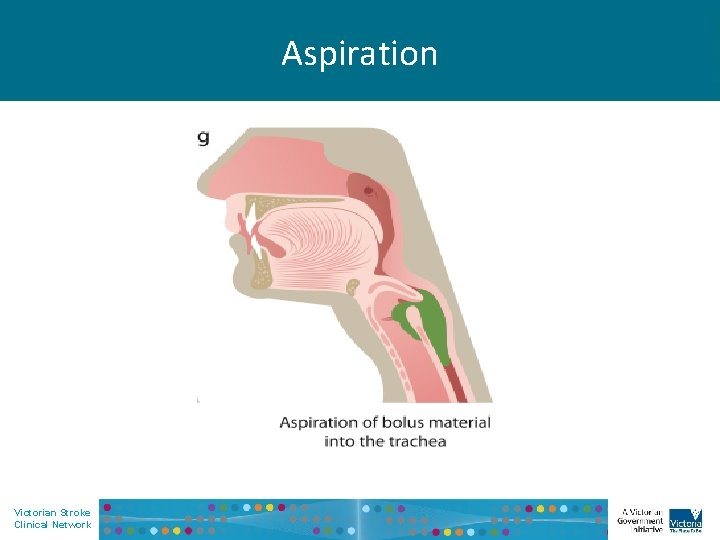
Aspiration Victorian Stroke Clinical Network
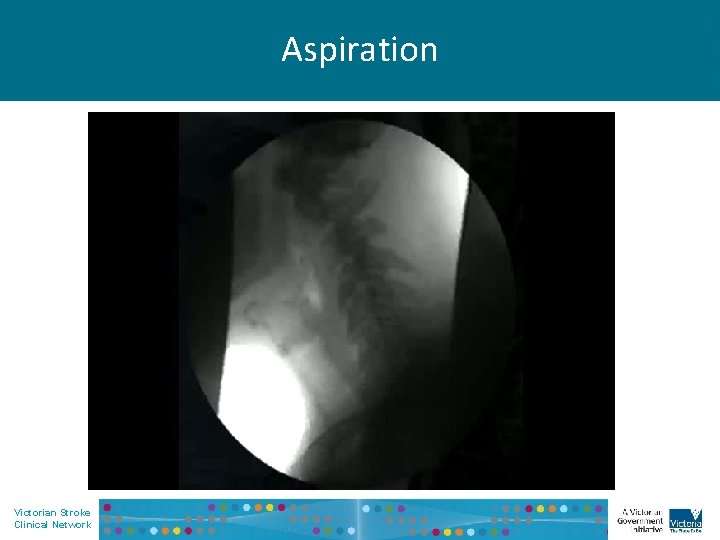
Aspiration Victorian Stroke Clinical Network
Oesophageal Dysphagia • Patients with oesophageal dysphagia may report food “sticking” at level of sternum, and or regurgitation. • May be better able to manage fluids than solids • May require gastroenterology review Victorian Stroke Clinical Network
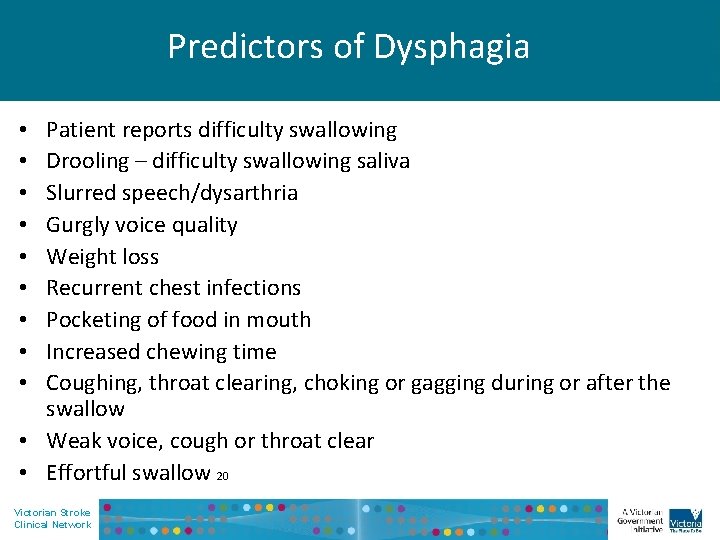
Predictors of Dysphagia Patient reports difficulty swallowing Drooling – difficulty swallowing saliva Slurred speech/dysarthria Gurgly voice quality Weight loss Recurrent chest infections Pocketing of food in mouth Increased chewing time Coughing, throat clearing, choking or gagging during or after the swallow • Weak voice, cough or throat clear • Effortful swallow 20 • • • Victorian Stroke Clinical Network
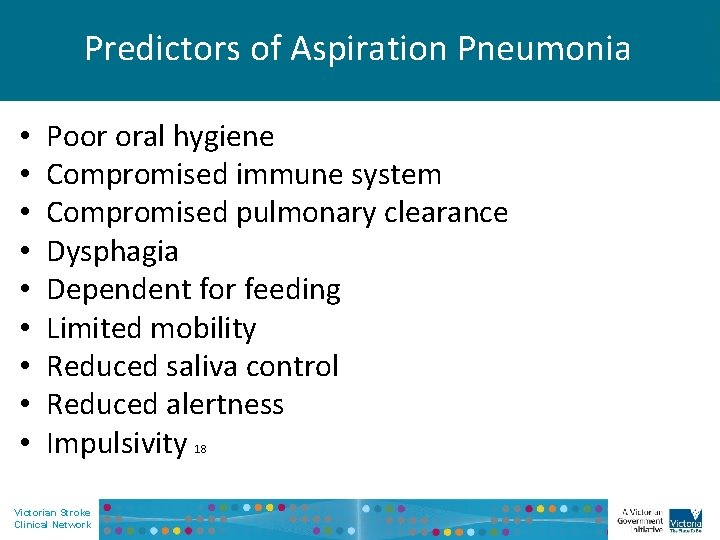
Predictors of Aspiration Pneumonia • • • Poor oral hygiene Compromised immune system Compromised pulmonary clearance Dysphagia Dependent for feeding Limited mobility Reduced saliva control Reduced alertness Impulsivity Victorian Stroke Clinical Network 18
The Victorian Dysphagia Screening Model (VDSM) Victorian Stroke Clinical Network
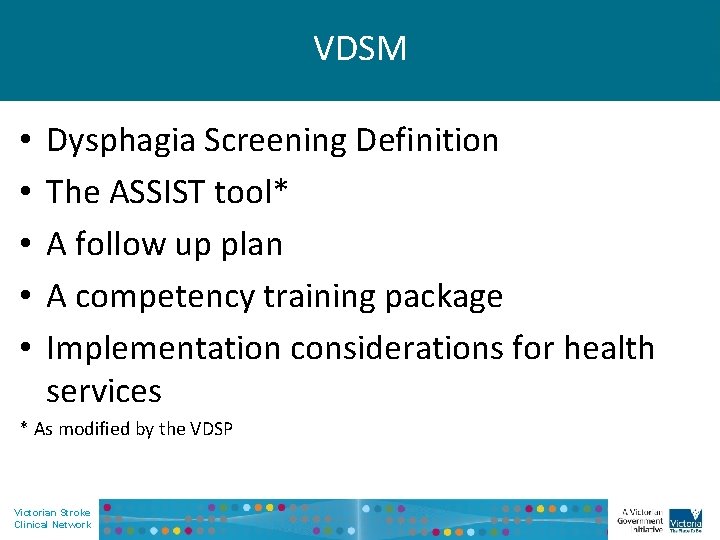
VDSM • • • Dysphagia Screening Definition The ASSIST tool* A follow up plan A competency training package Implementation considerations for health services * As modified by the VDSP Victorian Stroke Clinical Network
VDSM Dysphagia Screening Definition Dysphagia Screening is a non-invasive procedure, designed to detect the clinical indication of dysphagia/swallow impairment, by specifically trained personnel. The screen should result in a pass / fail outcome Victorian Stroke Clinical Network
What are competency standards? • Competency standards define the requirements for effective workplace performance in a discrete area of work, work function, activity or process. Victorian Stroke Clinical Network
VDSM Competency Requirements Successful completion of training requires the following: 1. Completion of pre-training questionnaire 2. Attendance at a training session 3. Successful completion of three swallow screens, supervised by trained personnel using the competency tool 4. Successful completion of post-training written assessment Victorian Stroke Clinical Network

Development of ASSIST • Originally developed by Working Party of Managers of the Greater Metropolitan Speech Pathology Services in NSW Health. Endorsed in April 2004 by the Speech Pathology Advisors Group and GMCT Stroke Co-ordinating Committee • Based on current evidence – not formally validated • Adapted for VDSM and endorsed by Speech Pathology Australia, the Dietitians Association of Australia, College of Emergency Nursing Australasia and the Australasian Neurosciences Nursing Association Victorian Stroke Clinical Network
Victorian Stroke Clinical Network
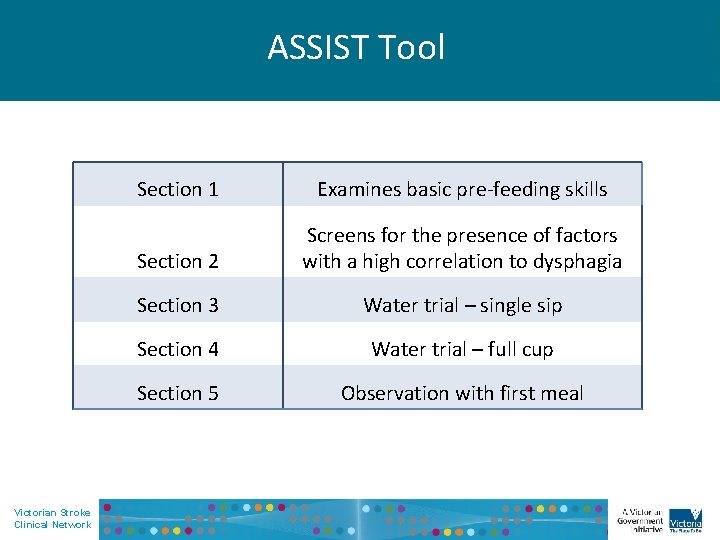
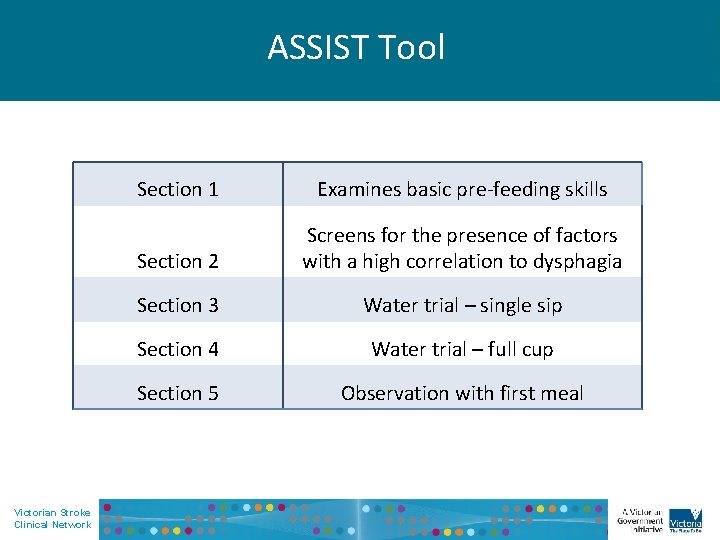
ASSIST Tool Victorian Stroke Clinical Network Section 1 Examines basic pre-feeding skills Section 2 Screens for the presence of factors with a high correlation to dysphagia Section 3 Water trial – single sip Section 4 Water trial – full cup Section 5 Observation with first meal
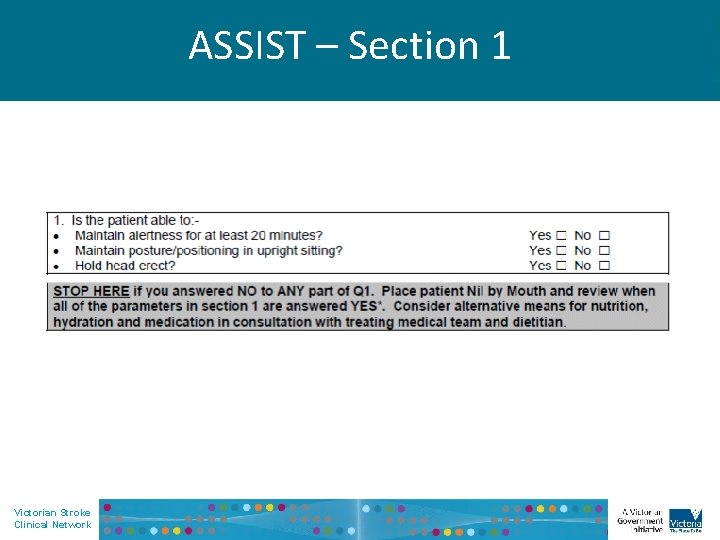
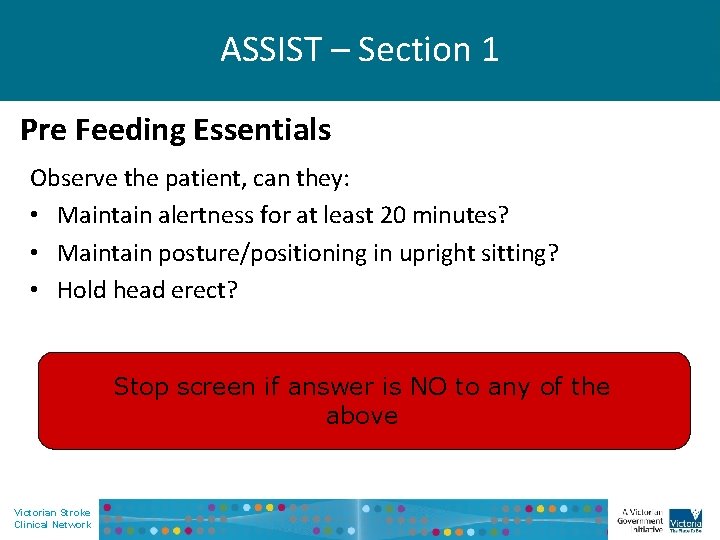
ASSIST – Section 1 Victorian Stroke Clinical Network
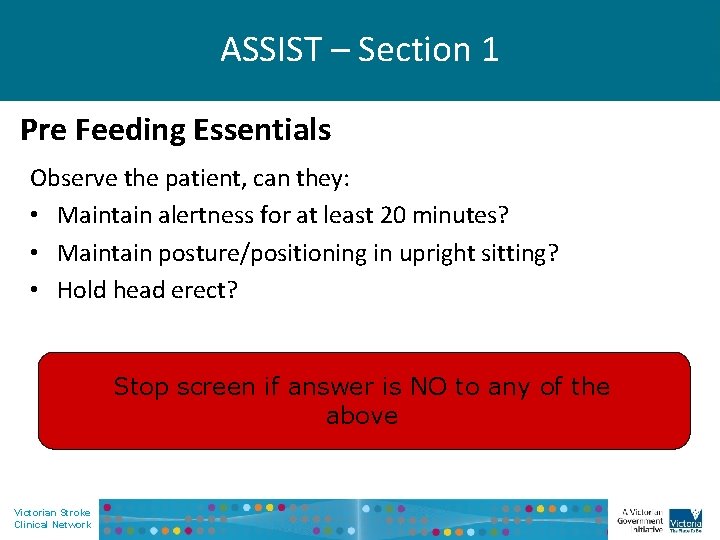
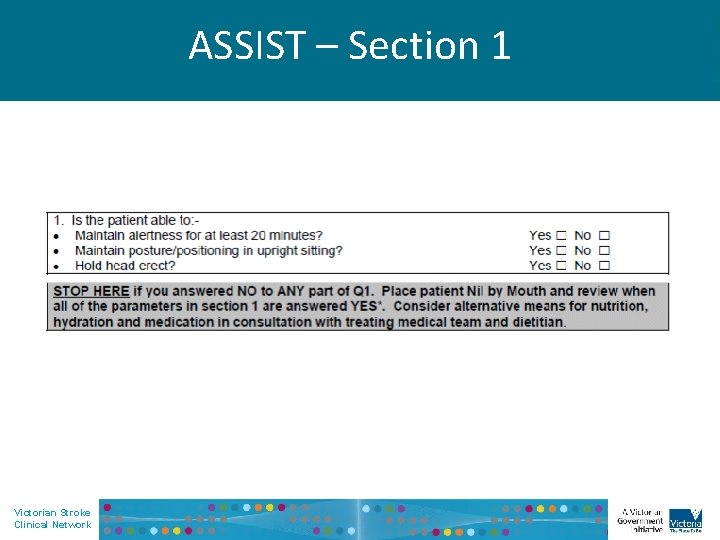
ASSIST – Section 1 Pre Feeding Essentials Observe the patient, can they: • Maintain alertness for at least 20 minutes? • Maintain posture/positioning in upright sitting? • Hold head erect? Stop screen if answer is NO to any of the above Victorian Stroke Clinical Network
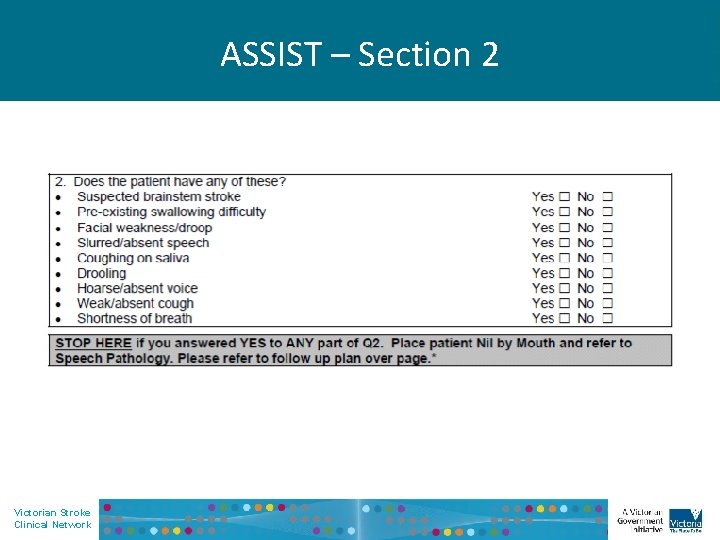
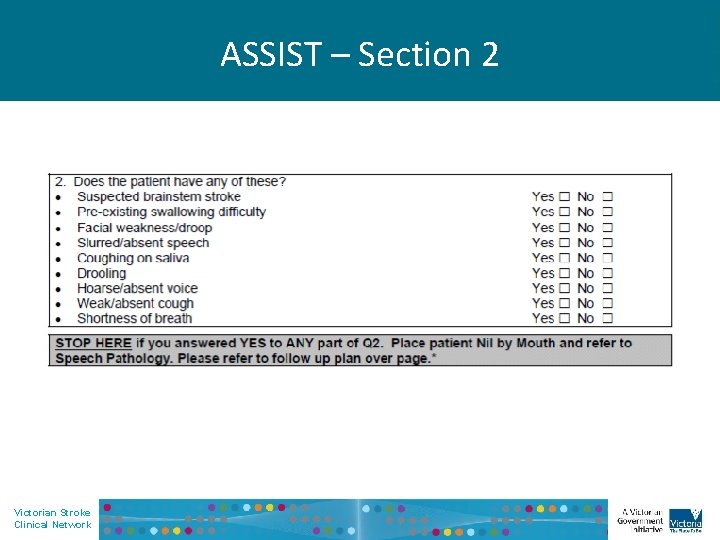
ASSIST – Section 2 Victorian Stroke Clinical Network
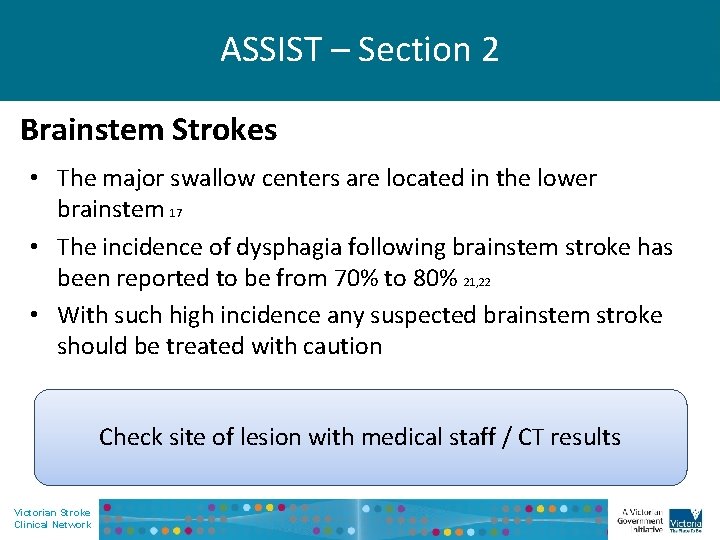
ASSIST – Section 2 Brainstem Strokes • The major swallow centers are located in the lower brainstem 17 • The incidence of dysphagia following brainstem stroke has been reported to be from 70% to 80% 21, 22 • With such high incidence any suspected brainstem stroke should be treated with caution Check site of lesion with medical staff / CT results Victorian Stroke Clinical Network
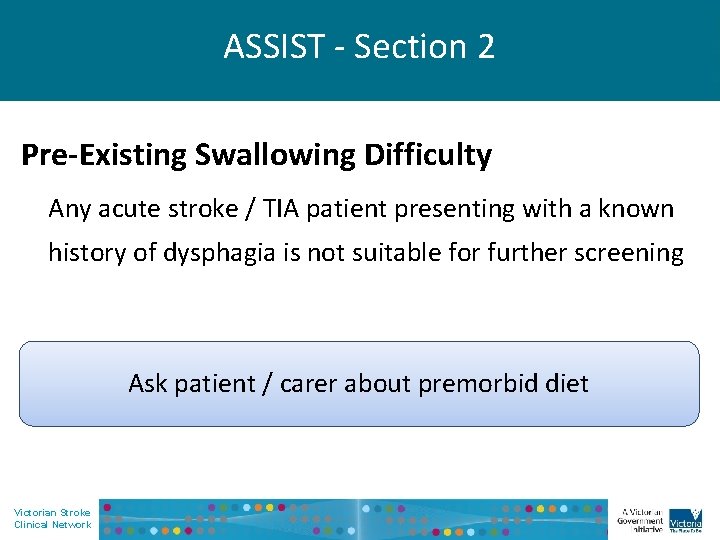
ASSIST - Section 2 Pre-Existing Swallowing Difficulty Any acute stroke / TIA patient presenting with a known history of dysphagia is not suitable for further screening Ask patient / carer about premorbid diet Victorian Stroke Clinical Network
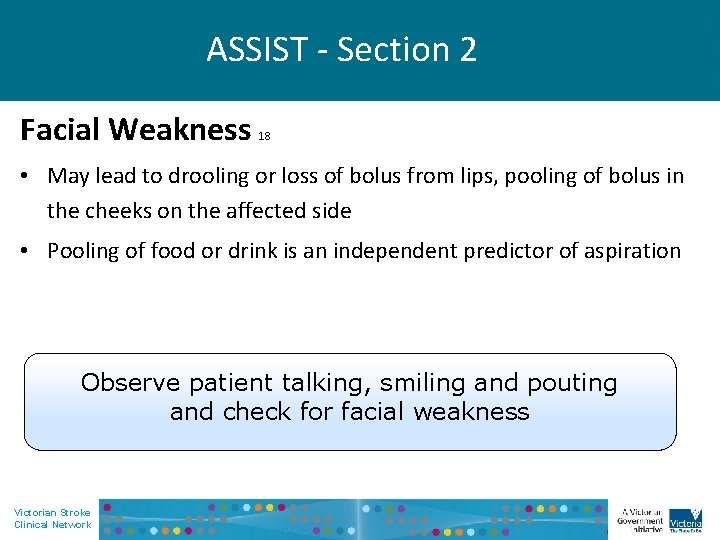
ASSIST - Section 2 Facial Weakness 18 • May lead to drooling or loss of bolus from lips, pooling of bolus in the cheeks on the affected side • Pooling of food or drink is an independent predictor of aspiration Observe patient talking, smiling and pouting and check for facial weakness Victorian Stroke Clinical Network
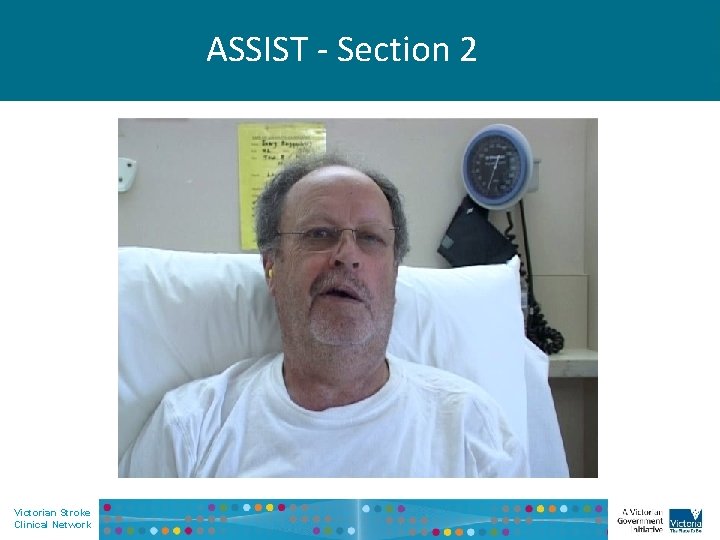
ASSIST - Section 2 Victorian Stroke Clinical Network
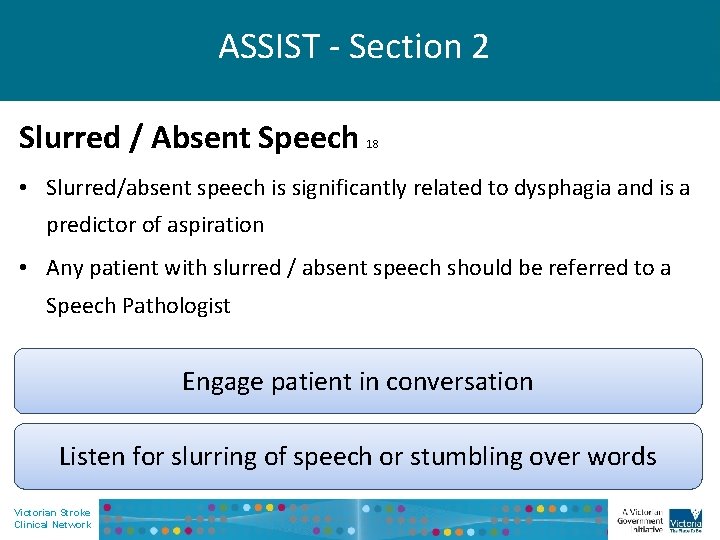
ASSIST - Section 2 Slurred / Absent Speech 18 • Slurred/absent speech is significantly related to dysphagia and is a predictor of aspiration • Any patient with slurred / absent speech should be referred to a Speech Pathologist Engage patient in conversation Listen for slurring of speech or stumbling over words Victorian Stroke Clinical Network
ASSIST - Section 2 Victorian Stroke Clinical Network
ASSIST - Section 2 Coughing on Saliva/Drooling 18 • There is a significant relationship between difficulty managing saliva and swallowing problems • Coughing on saliva or drooling is a predictor of aspiration Is the patient coughing at rest? Does the patient have a wet voice quality? Is the patient drooling? Victorian Stroke Clinical Network
ASSIST - Section 2 Hoarse/Absent Voice 18 • Any change in vocal quality may indicate a risk of aspiration • May be characterised by impairment to pitch, loudness, quality • Listen for the following voice qualities: Hoarse Breathy Harsh Victorian Stroke Clinical Network
ASSIST - Section 2 Victorian Stroke Clinical Network
ASSIST - Section 2 Weak/Absent Cough 18 • Weak or absent cough is a predictor of aspiration Ask the patient to cough: Are they able to generate a cough? How strong does it sound? Victorian Stroke Clinical Network
ASSIST - Section 2 Shortness of breath 18 • Shortness of breath may lead to in coordination of the breathswallow cycle, placing the patient at increased risk of aspiration Observe for the following and place patient NBM if present: Difficult, laboured or uncomfortable breathing 23 Victorian Stroke Clinical Network
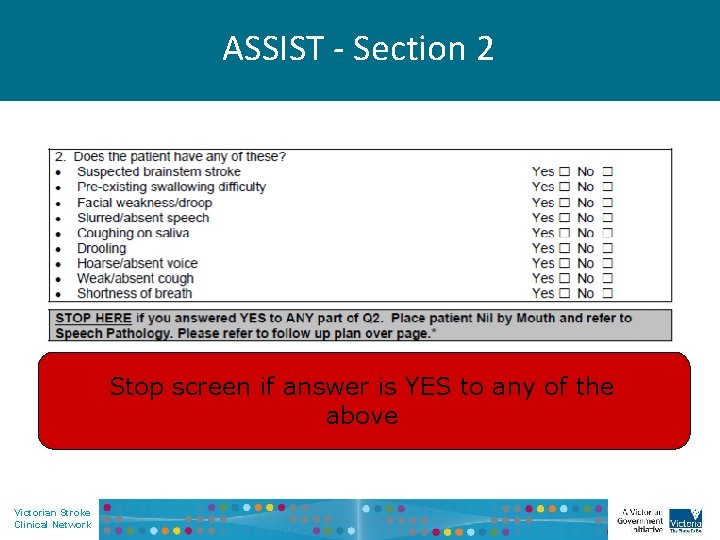
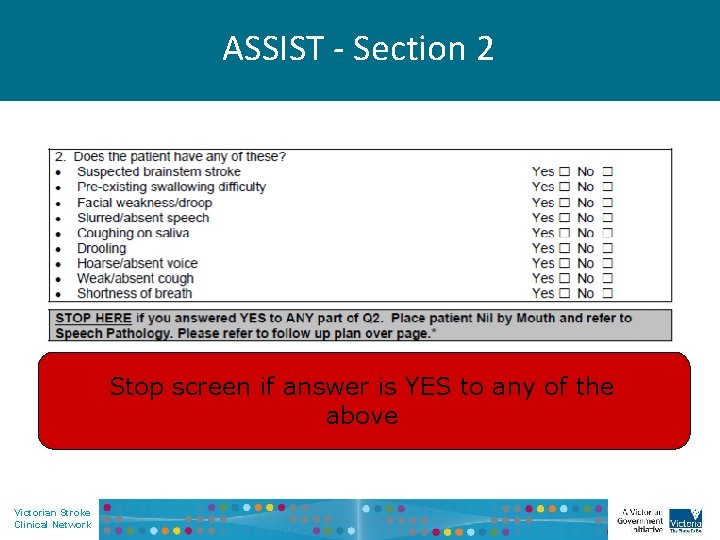
ASSIST - Section 2 Stop screen if answer is YES to any of the above Victorian Stroke Clinical Network
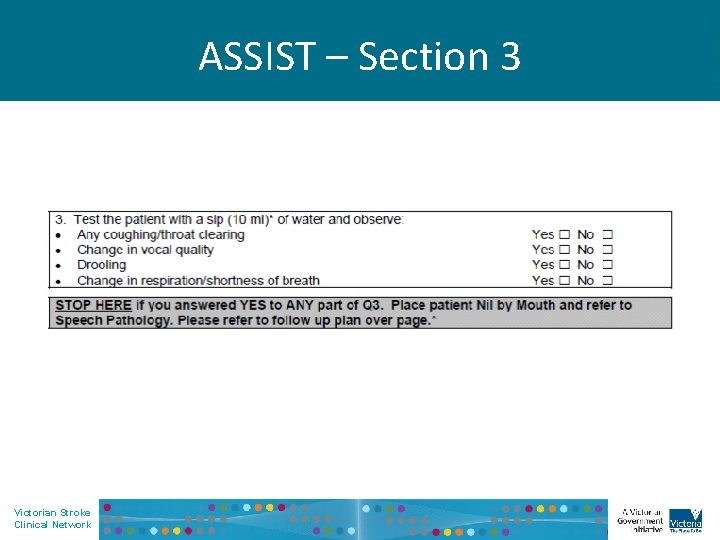
ASSIST – Section 3 Victorian Stroke Clinical Network
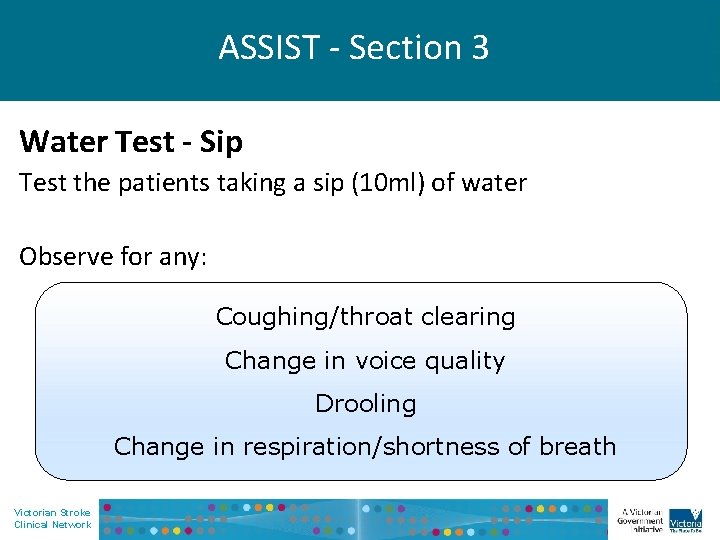
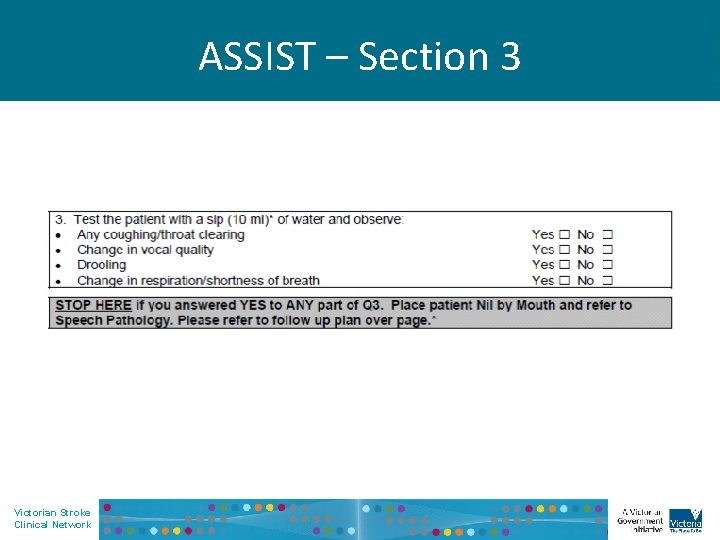
ASSIST - Section 3 Water Test - Sip Test the patients taking a sip (10 ml) of water Observe for any: Coughing/throat clearing Change in voice quality Drooling Change in respiration/shortness of breath Victorian Stroke Clinical Network
ASSIST - Section 3 Victorian Stroke Clinical Network
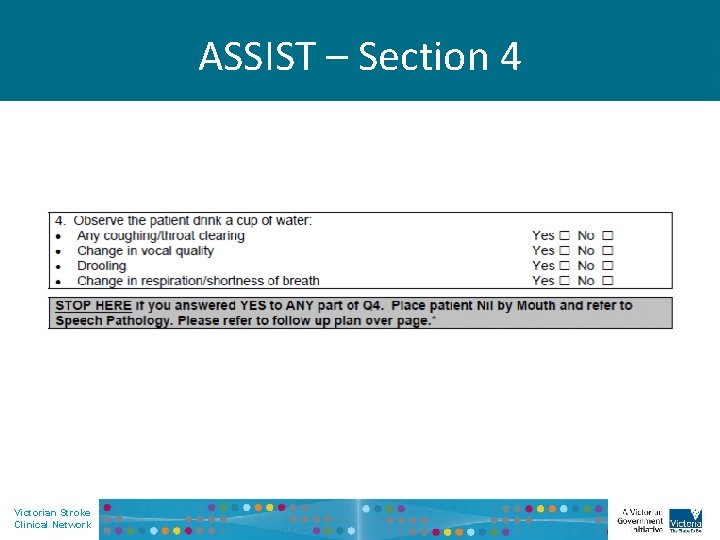
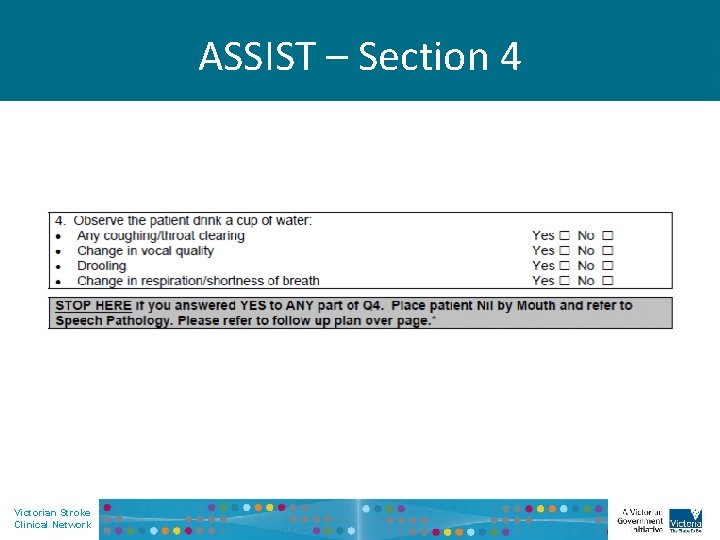
ASSIST – Section 4 Victorian Stroke Clinical Network
ASSIST - Section 4 Water Test - Cup • Observe patient drinking a cup of water (provide assistance if required) Observe for: Coughing/throat clearing Change in voice quality Drooling Change in respiration/shortness of breath Victorian Stroke Clinical Network
ASSIST - Section 4 Victorian Stroke Clinical Network
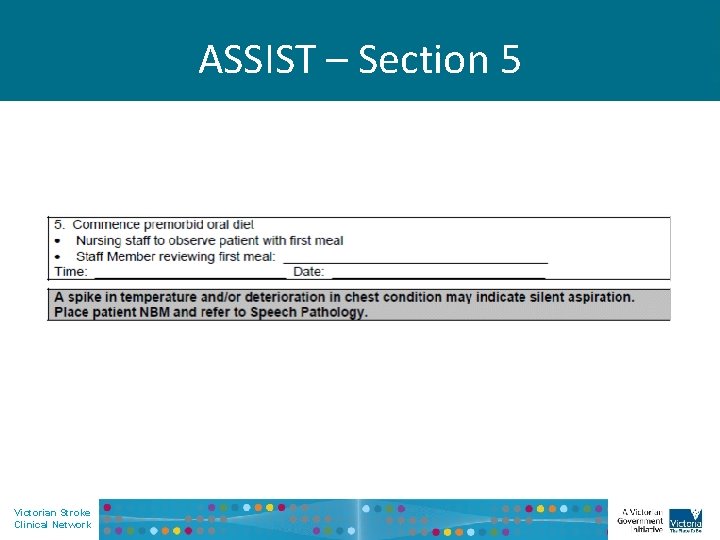
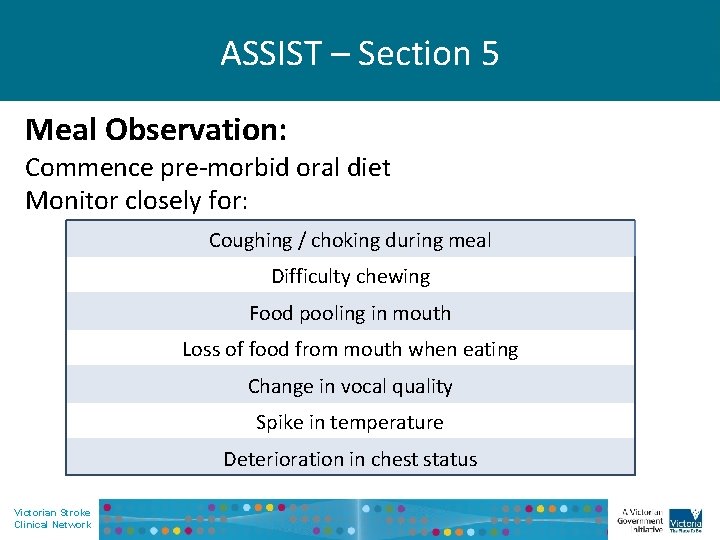
ASSIST – Section 5 Victorian Stroke Clinical Network
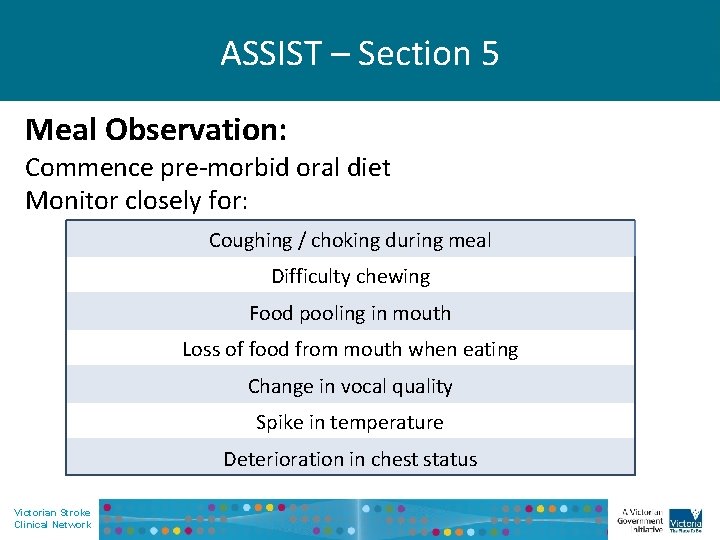
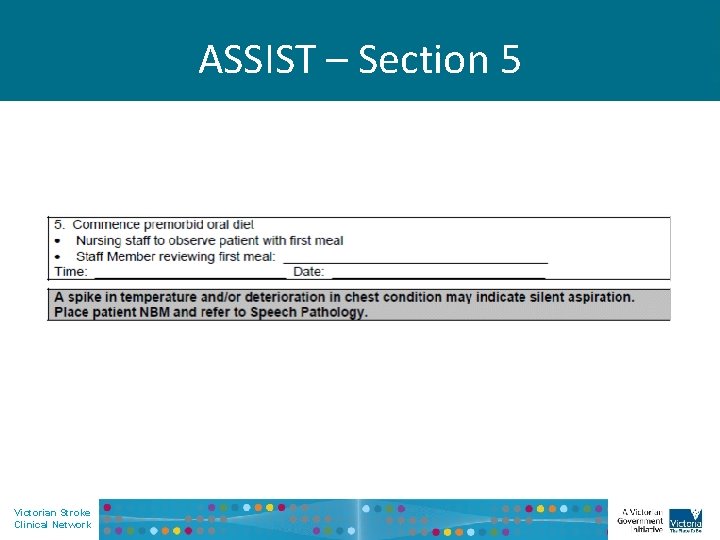
ASSIST – Section 5 Meal Observation: Commence pre-morbid oral diet Monitor closely for: Coughing / choking during meal Difficulty chewing Food pooling in mouth Loss of food from mouth when eating Change in vocal quality Spike in temperature Deterioration in chest status Victorian Stroke Clinical Network
Victorian Stroke Clinical Network
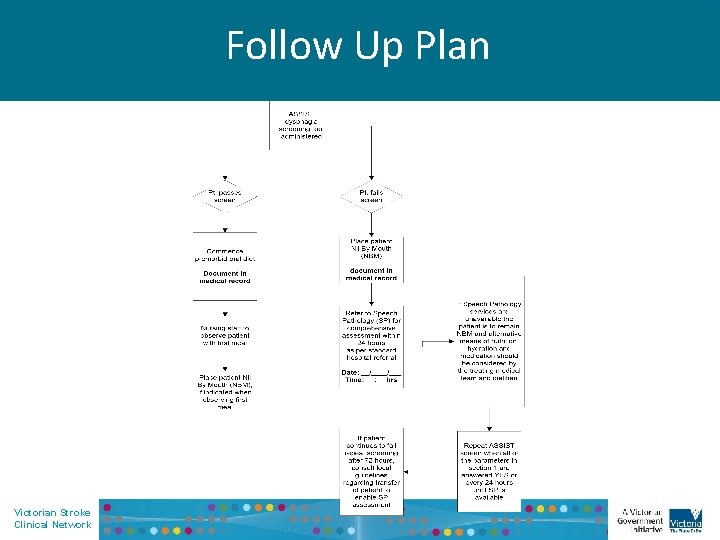
Follow Up Plan Victorian Stroke Clinical Network
References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. Clinical Guidelines for Stroke Management: National Stroke Foundation; 2010 Webster JD, R. Aspiration pnuemonitis: a serious problem. Geriatrics 1977; 32: 42 – 47. Kirch CS. A. Aspiration pneumonia-medical management. Otolaryngology 1988; 21: 677 – 687 Wiles CM. Neurogenic Dysphagia – editorial. Journal Neurology Neurosurgery and Psychiatry. 1991; 54: 1037 – 1039. Daniels SK, Brailey K, Priestly DH, Herrington LR, Weisberg LA, Foundas AL. Aspiration in patients with acute stroke. Archives of Physical Medicine and Rehabilitation. 1998; 79 (1): 14 -9. Langdon PDE. Management of Dysphagia in Australian Stroke Units. Internal Medicine Journal. 2008; 38 (4). Perry L & Love C. Screening for Dysphagia and Aspiration in Acute Stroke: A Systematic Review. Dysphagia 2001; 16: 7 – 18. Langdon, C, Lee, H & Binns, C. Dysphagia in Acute Ischaemic Stroke: Severity, Recovery and Relationship to Stroke Subtype. Journal of Clinical Neuroscience. 2007; 14: 630 – 634. Smithard DG, O’Neill PA, England RE, Park CL, Wyatt R, Martin DF, et al. The natural history of dysphagia following a stroke. Dysphagia 1997; 12 (4): 188 – 93. Clinical Guidelines for Acute Stroke Management: National Stroke Foundation; 2008 Suiter DM, & Leder SB. Clinical Utility of the 3 -ounce water swallow test. Dysphagia 2008; 23 (3): 244 – 50. Martino RP, G. & Diamant, N. Screening for Oropharyngeal Dysphagia in Stroke: Insufficient Evidence for Guidelines. Dysphagia 2000; 15: 19 – 30. Ramsey, DJ, Smithard, DG, Kalra L. Early Assessments of Dysphagia and Aspiration Risk in Acute Stroke Patients. Stroke 2003; 34 (5): 1252 – 7. Odderson IR, Keaton JC, Mc. Kenna BS. Swallow Management in Patients on an Acute Stroke Pathway: Quality is Cost Effective. Archives of Physical Medicine and Rehabilitation. 1995; 76 (12): 1130 -3 Hinchey JA, Shephard T, Furie K, Smith D, Wang D, Tonn S. Formal Dysphagia Screening Protocols Prevent Pneumonia. Stroke 2005; 36 (9): 1972 – 6. Victorian Stroke Clinical Network
References (continue) 16. 17. 18. 19. 20. 21. 22. 23. Perry, L & Mc. Laren, S. Nutritional Support in Acute Stroke: The Impact of Evidence-Based Guidelines. 2003 22 (3): 283 – 293. Logemann JA. Evaluation and Treatment of Swallowing Disorders: pro-ed; 1998. Langmore S, Terpenning M, Schork A, Chen Y, Murray J, Lopatin D & Lesche W. Predictors of aspiration pneumonia: how important is dysphagia. Dysphagia 1998; 13(2) Speech Pathology Australia Position Paper. Dysphagia: General (2004) Daniels SK, Ballo LA, Mahoney MC, Foundas AL. Clinical predictors of dysphagia and aspiration risk: outcome measures in acute stroke patients. Arch Phys Med Rehabilitation 2000; 81(8) Meng NH, Wang TG, Lien IN. Dysphagia in patients with brainstem stroke: incidence and outcome. American Journal of Physical Medicine and Rehabilitation 2000, 79(2), pp 170 -175 Horner J, Buoyer FG, Alberts MJ, et al. Dysphagia following brainstem stroke: clinical correlates and outcome. Arch Neurol 1991, 48, 1170 -3. American Thoracic Society. (1999) Dyspnea: Mechanisms, Assessment, and management: A consenusstatement. American Journal of Respiratory and critical care Medicine. Vol 15. pp 321 -340 Victorian Stroke Clinical Network