The Use of Clinical Case Management to Improve
- Slides: 37
The Use of Clinical Case Management to Improve Outcomes in PCMH-Designated Community Health Centers Brian Reed, MD, Baylor College of Medicine; Linda Keenan MPA, BSN, RN-BC Harris County Hospital District, Houston, TX Join the conversation! Our Twitter hashtag is #CPI 2011.
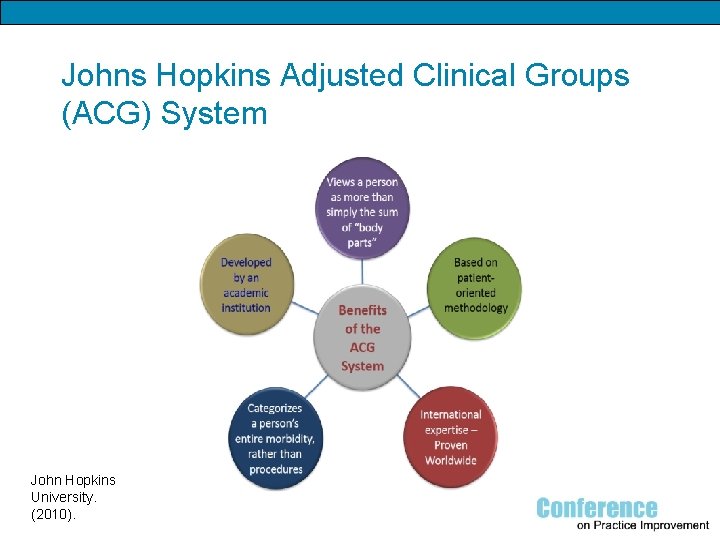
The Use of Clinical Case Management to Improve Outcomes in PCMH-Designated Community Health Centers OBJECTIVES 1. To describe the basic components of the Johns Hopkins Adjusted Clinical Group Case Mix System and how it can be used to predict patients at high risk for utilization of healthcare resources 2. To highlight specific clinical case management interventions that helped to improve patient outcomes 3. To specifically discuss on-going care coordination activities among our patients with poorly controlled diabetes mellitus. 4. To detail clinical outcomes and future goals
Overview • • • Background Johns Hopkins Adjusted Clinical Groups Case management model Case management interventions Clinical outcomes
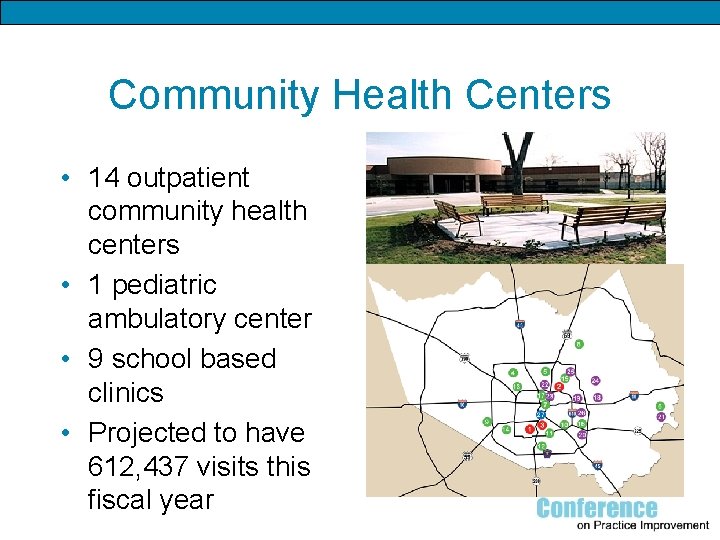
Community Health Centers • 14 outpatient community health centers • 1 pediatric ambulatory center • 9 school based clinics • Projected to have 612, 437 visits this fiscal year
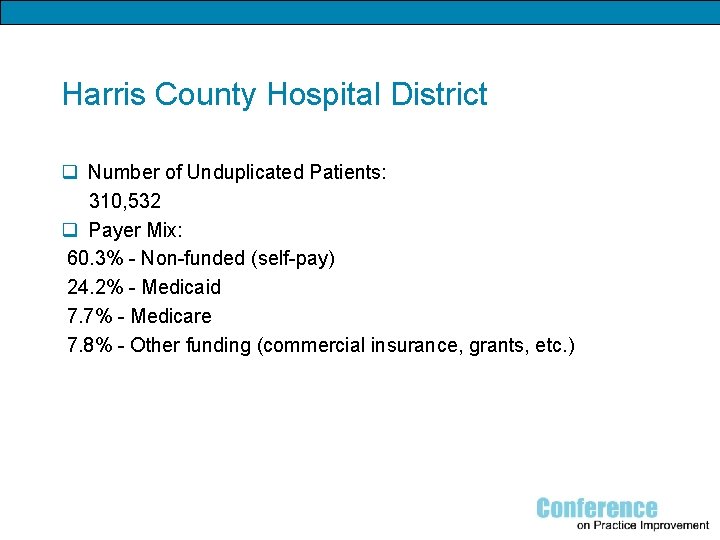
Harris County Hospital District q Number of Unduplicated Patients: 310, 532 q Payer Mix: 60. 3% - Non-funded (self-pay) 24. 2% - Medicaid 7. 7% - Medicare 7. 8% - Other funding (commercial insurance, grants, etc. )
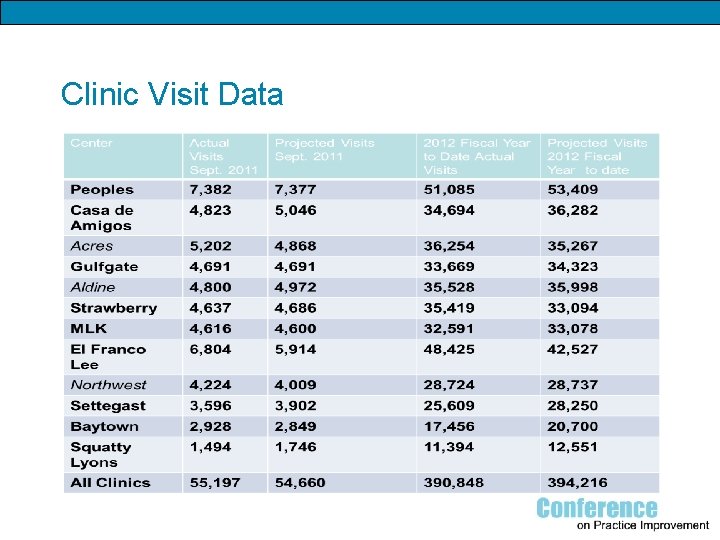
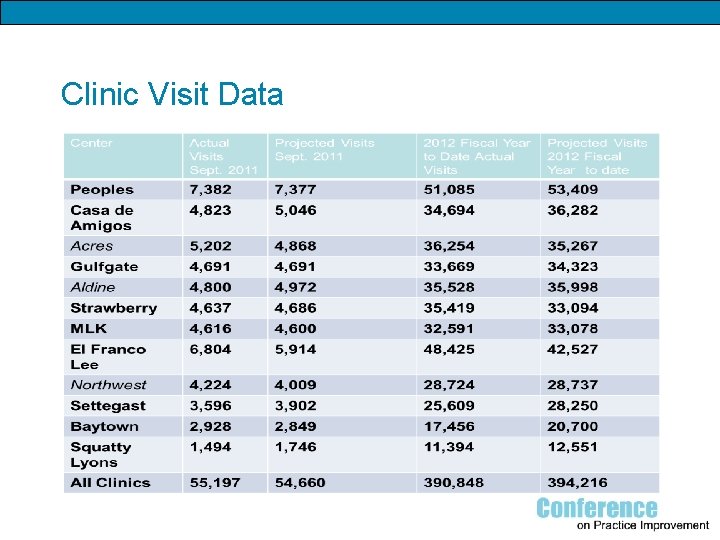
Clinic Visit Data
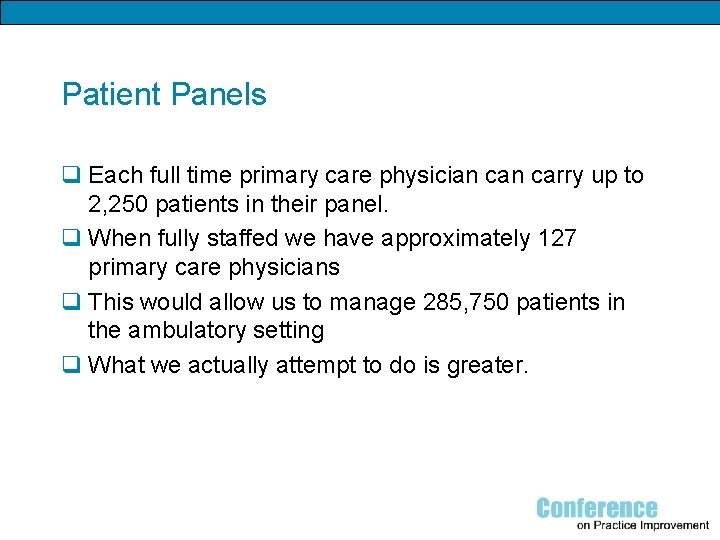
Patient Panels q Each full time primary care physician carry up to 2, 250 patients in their panel. q When fully staffed we have approximately 127 primary care physicians q This would allow us to manage 285, 750 patients in the ambulatory setting q What we actually attempt to do is greater.
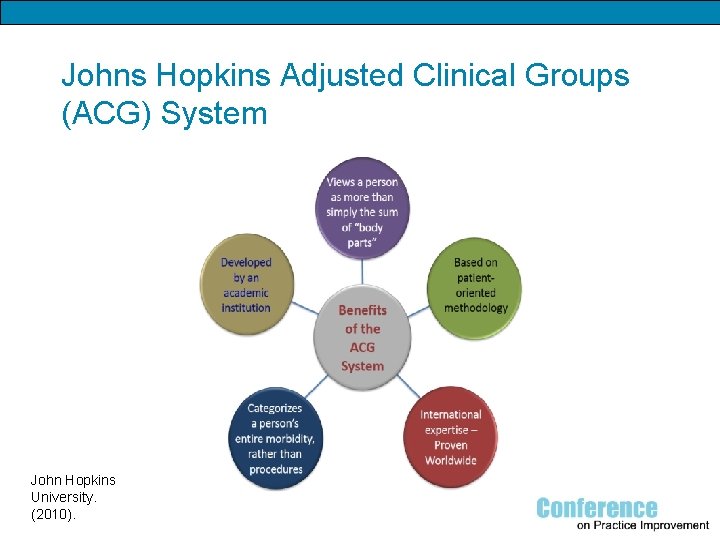
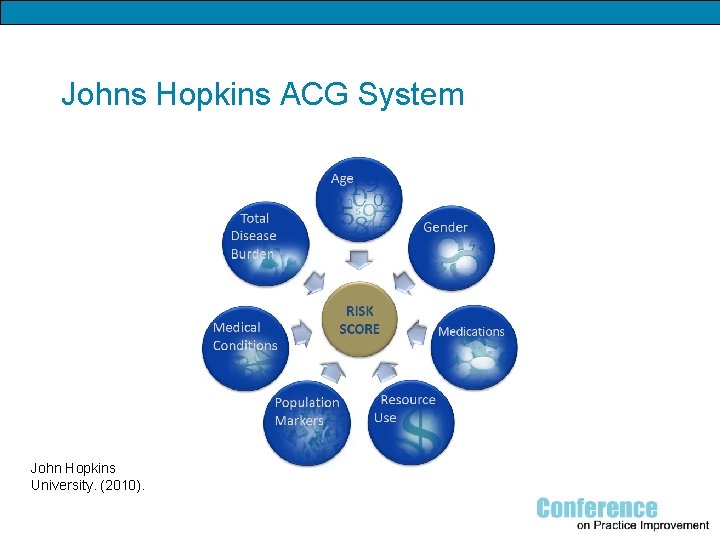
Johns Hopkins Adjusted Clinical Groups (ACG) System John Hopkins University. (2010).
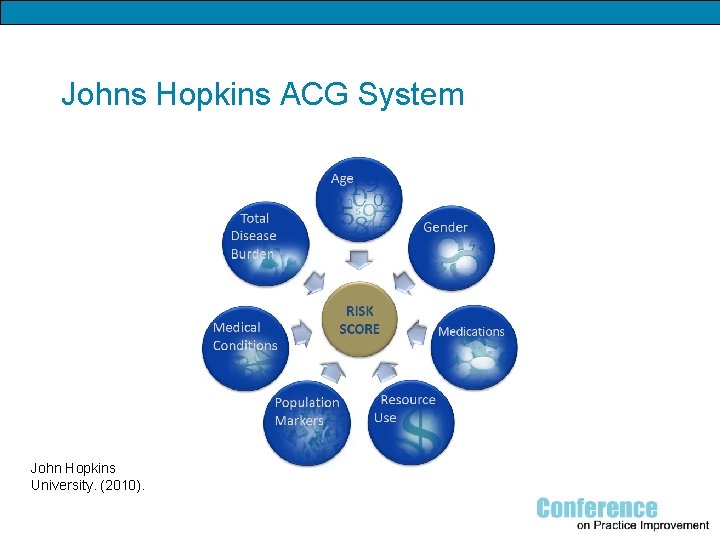
Johns Hopkins ACG System John Hopkins University. (2010).
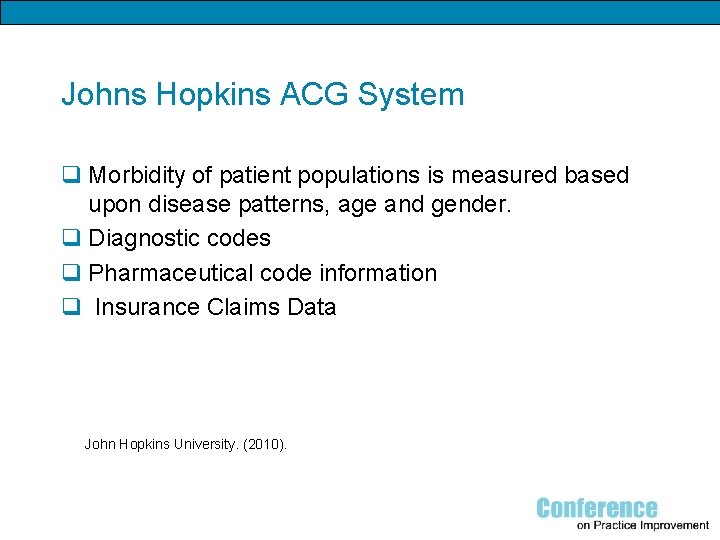
Johns Hopkins ACG System q Morbidity of patient populations is measured based upon disease patterns, age and gender. q Diagnostic codes q Pharmaceutical code information q Insurance Claims Data John Hopkins University. (2010).
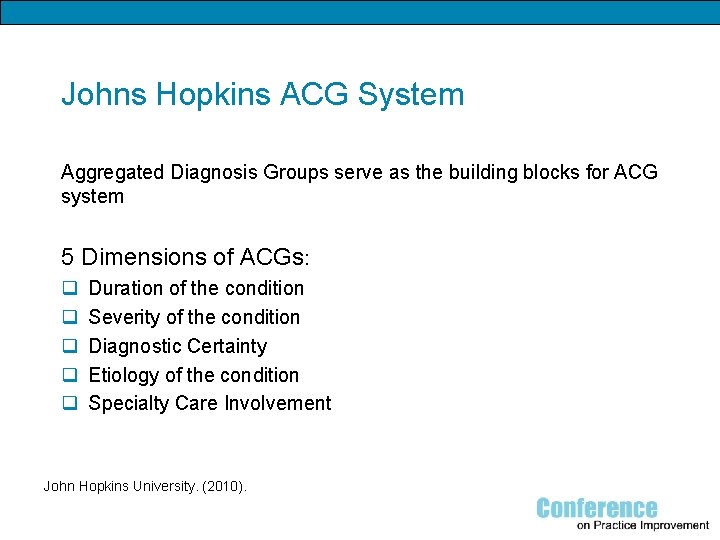
Johns Hopkins ACG System Aggregated Diagnosis Groups serve as the building blocks for ACG system 5 Dimensions of ACGs: q q q Duration of the condition Severity of the condition Diagnostic Certainty Etiology of the condition Specialty Care Involvement John Hopkins University. (2010).
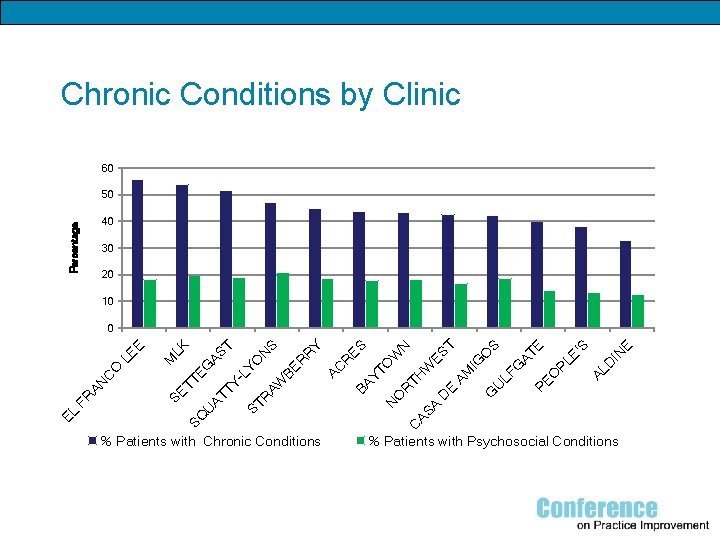
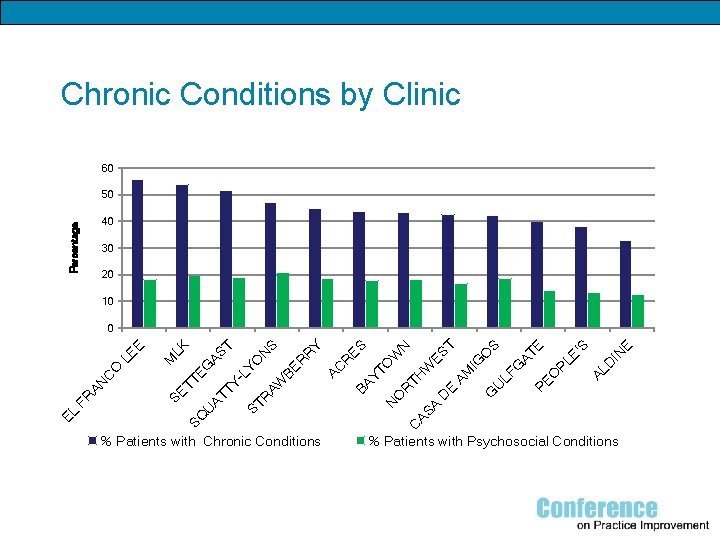
Chronic Conditions by Clinic 60 50 Percentage 40 30 20 10 % Patients with Chronic Conditions E IN AL D PE O PL E' S E AT S LF G U E D G AM W C AS A N O R TH YT BA IG O ES T W O R AC R BE N ES Y R S N R AW YO ST AT TT TY -L EG AS T LK M SE SQ U EL FR AN C O LE E 0 % Patients with Psychosocial Conditions
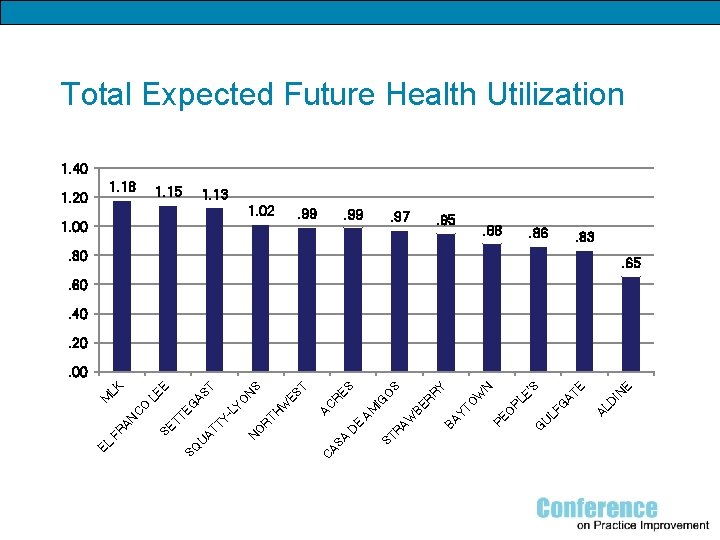
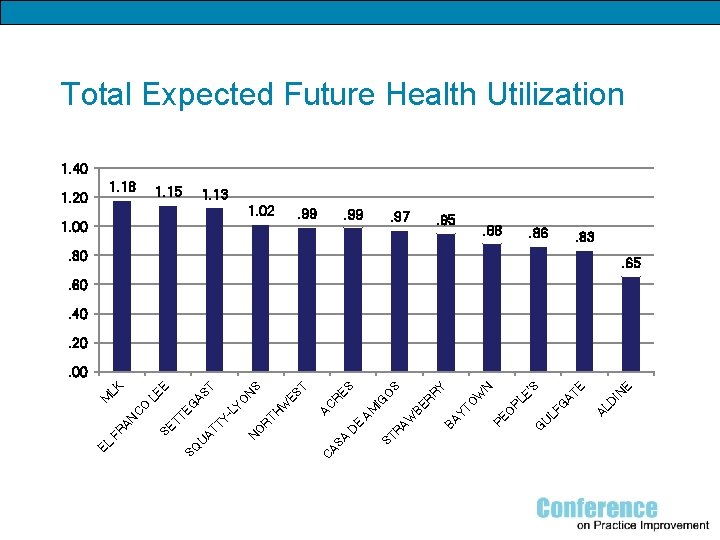
Total Expected Future Health Utilization 1. 40 1. 18 1. 20 1. 15 1. 13 1. 02 . 99 1. 00 . 99 . 97 . 95 . 88 . 86 . 83 . 80 . 65 . 60. 40. 20 G U E IN AL D LF G AT E E' S PE O W O YT PL N Y R BA R AW IG A AS C ST AM E D O N BE R O S ES R AC W R TH -L TY AT ES T S N YO AS T G U SE T TE SQ EL FR AN C O M LE LK E . 00
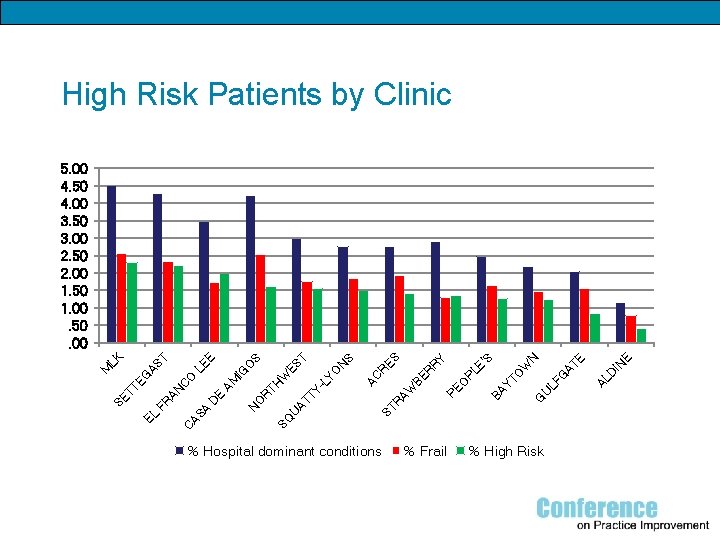
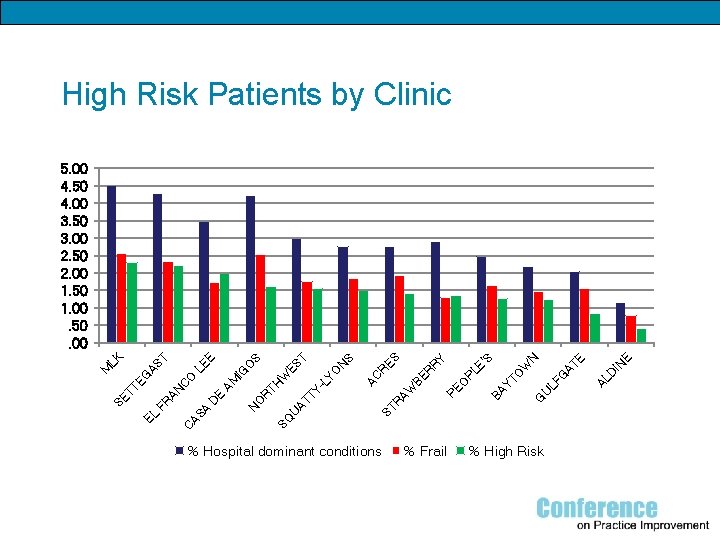
High Risk Patients by Clinic % Hospital dominant conditions % Frail % High Risk E IN AL D AT E G LF U G YT O W N E' S PL BA AW R PE O BE R R Y ES R ST U AT T Y- TH SQ R O N AC N S W LY O O IG AM E D A AS C ES T S E LE C AN FR EL SE T TE O G M AS T LK 5. 00 4. 50 4. 00 3. 50 3. 00 2. 50 2. 00 1. 50 1. 00. 50. 00
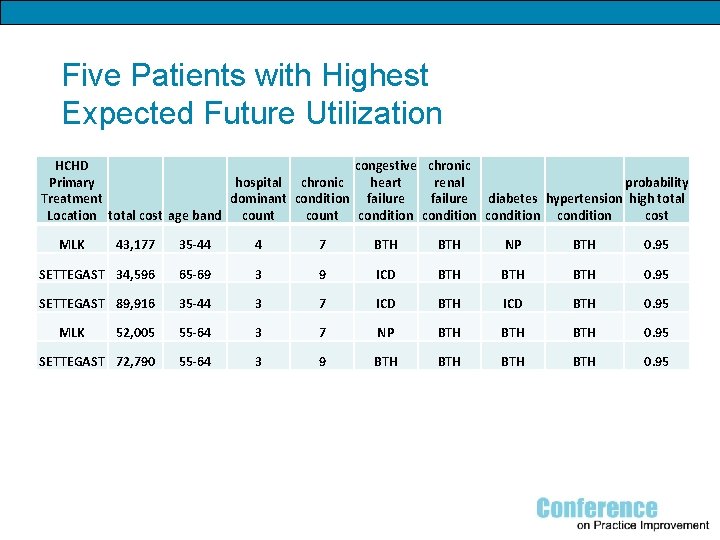
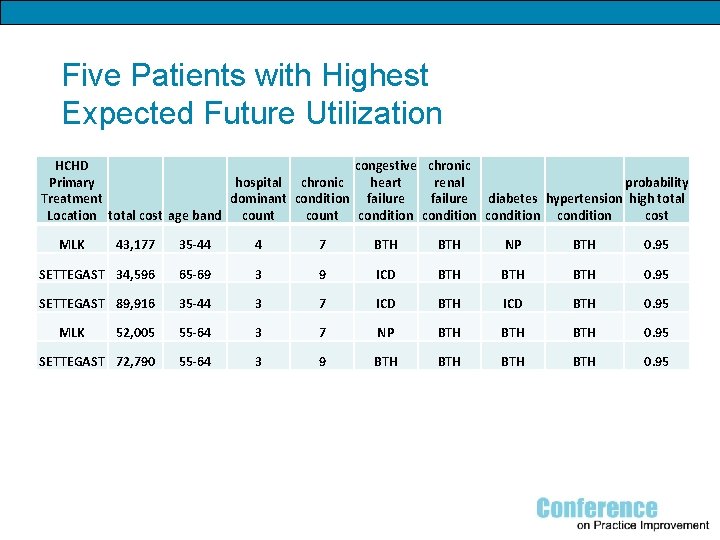
Five Patients with Highest Expected Future Utilization HCHD congestive chronic Primary hospital chronic heart renal probability Treatment failure diabetes hypertension high total dominant condition failure Location total cost age band count condition cost MLK 43, 177 35 -44 4 7 BTH NP BTH 0. 95 SETTEGAST 34, 596 65 -69 3 9 ICD BTH BTH 0. 95 SETTEGAST 89, 916 35 -44 3 7 ICD BTH 0. 95 52, 005 55 -64 3 7 NP BTH BTH 0. 95 SETTEGAST 72, 790 55 -64 3 9 BTH BTH 0. 95 MLK
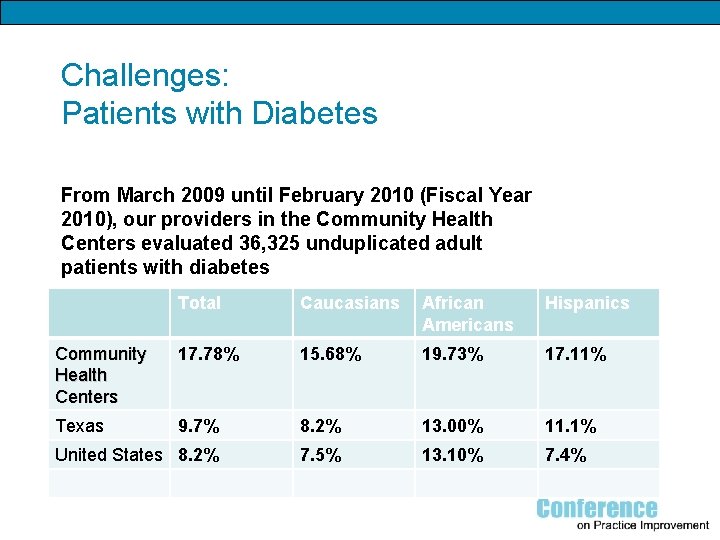
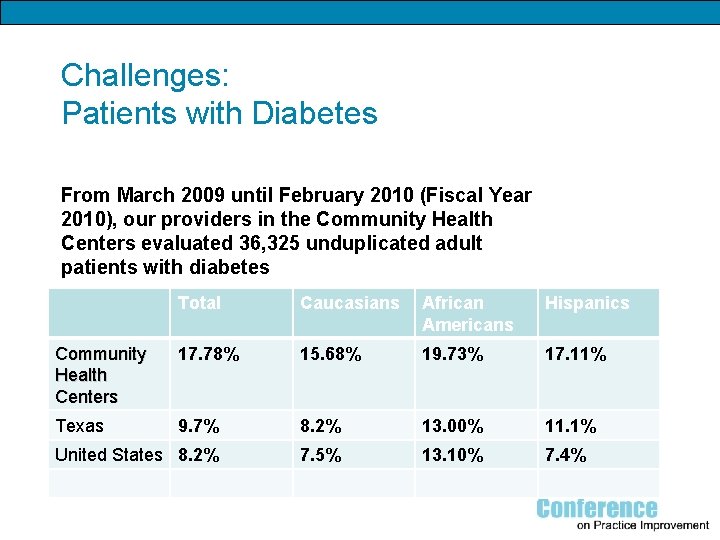
Challenges: Patients with Diabetes From March 2009 until February 2010 (Fiscal Year 2010), our providers in the Community Health Centers evaluated 36, 325 unduplicated adult patients with diabetes Total Caucasians African Americans Hispanics Community Health Centers 17. 78% 15. 68% 19. 73% 17. 11% Texas 9. 7% 8. 2% 13. 00% 11. 1% United States 8. 2% 7. 5% 13. 10% 7. 4%
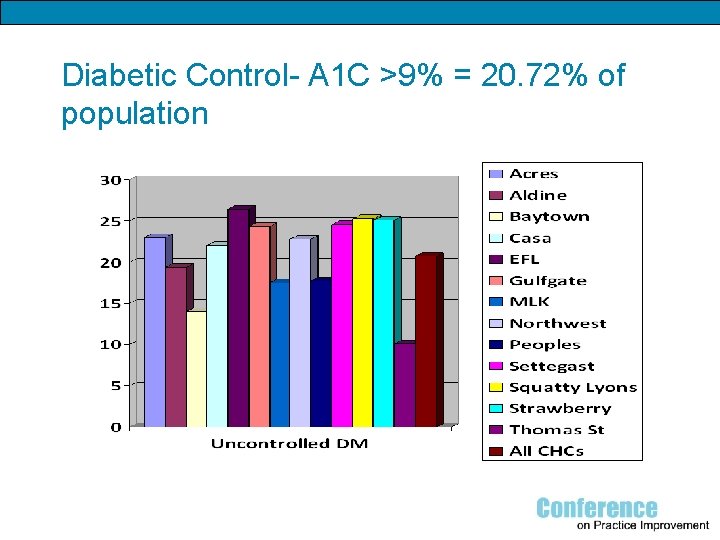
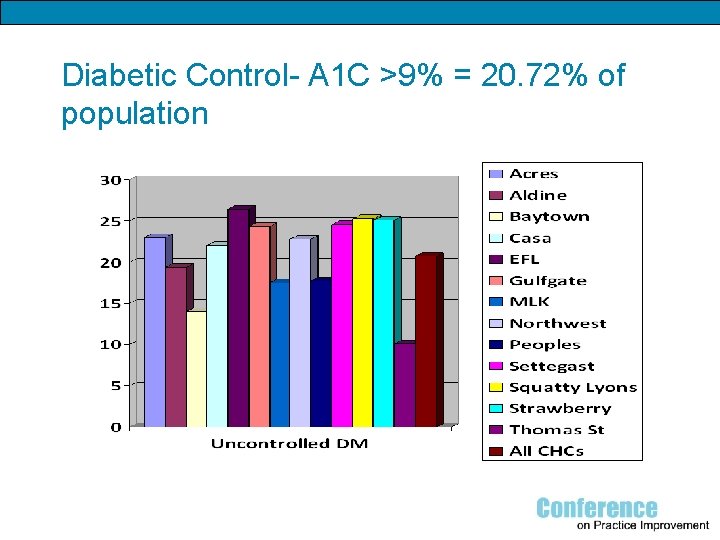
Diabetic Control- A 1 C >9% = 20. 72% of population
Care Teams: The Foundation of Our Medical Home
Care Teams § § § Physician Case Management Dietician RN/LVN Behavioral Therapy Clinical Pharmacist
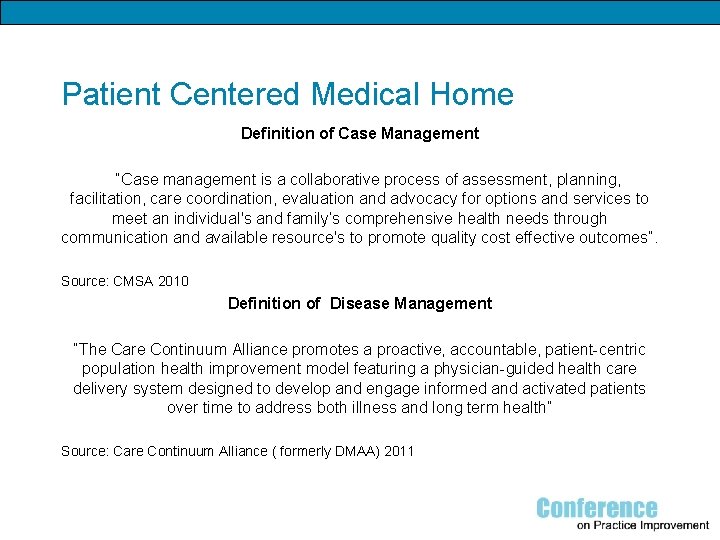
Patient Centered Medical Home Definition of Case Management “Case management is a collaborative process of assessment, planning, facilitation, care coordination, evaluation and advocacy for options and services to meet an individual's and family’s comprehensive health needs through communication and available resource's to promote quality cost effective outcomes”. Source: CMSA 2010 Definition of Disease Management “The Care Continuum Alliance promotes a proactive, accountable, patient-centric population health improvement model featuring a physician-guided health care delivery system designed to develop and engage informed and activated patients over time to address both illness and long term health” Source: Care Continuum Alliance ( formerly DMAA) 2011
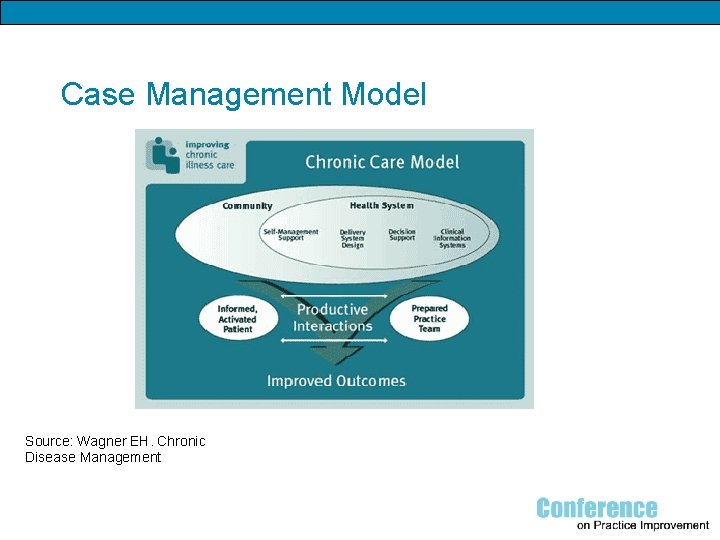
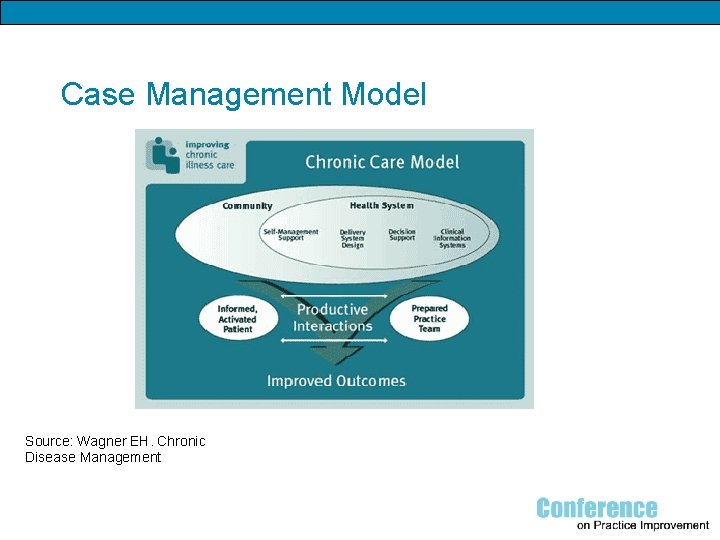
Case Management Model Source: Wagner EH. Chronic Disease Management
Scope of Medical Home Case Management q Dyad Model- experienced RN and Social worker q Motivational interviewing- holistic, comprehensive patient assessment q Open access – when the patient needs us at their convenience q Telephonic monitoring q Risk assessment- drives interventions and level of monitoring q Patient–Centric, Medical Home philosophy q Incorporates wellness, prevention and self management of disease
Case Management Design q Opt-Out design q Promotes engagement q Increases positive enrollment q Consent required q Enrolled patients are “flagged” in the Electronic Medical Record
Evidence Based practice (EBP) ü Research based case management interventions ü Standardization of EBP documentation template ü Motivational Interviewing ü Self-management ü Teach Back
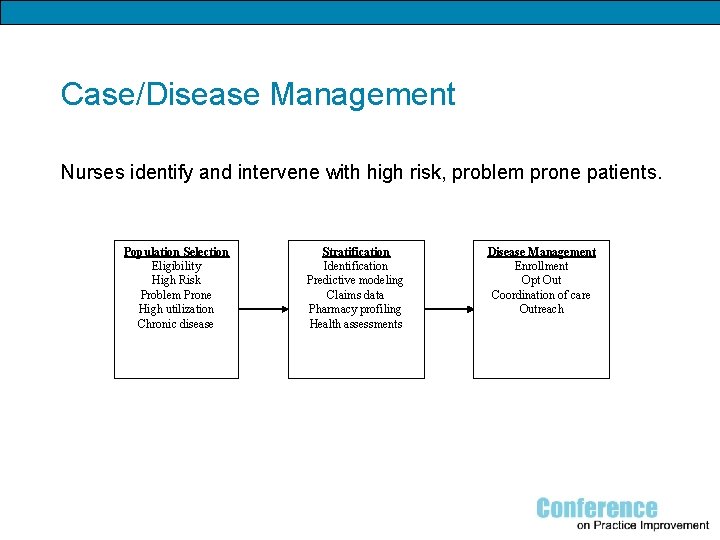
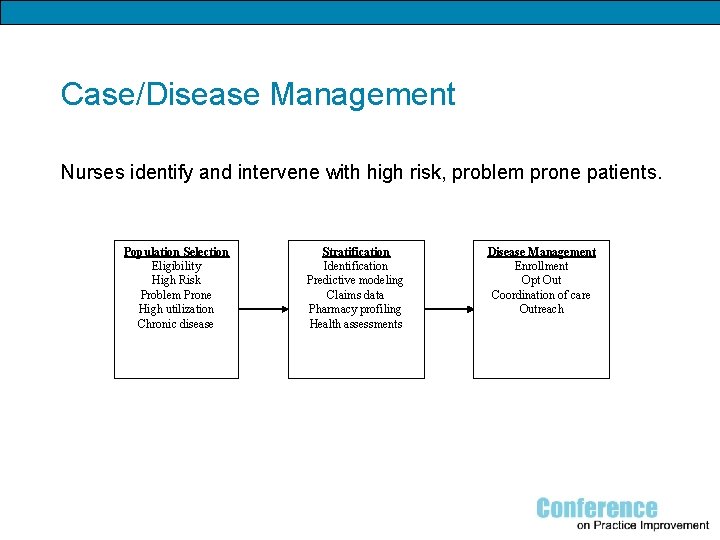
Case/Disease Management Nurses identify and intervene with high risk, problem prone patients. Population Selection Eligibility High Risk Problem Prone High utilization Chronic disease Stratification Identification Predictive modeling Claims data Pharmacy profiling Health assessments Disease Management Enrollment Opt Out Coordination of care Outreach
Case Management Interventions q q q q q Motivational interviewing Holistic assessment- bio-psychosocial Education- patient and family Risk assessment and stratification Utilization monitoring- real time Pre-visit chart review- pre-visit planning Multidisciplinary referral and collaboration Community referrals DME, Home Health, IV therapy coordination Transition from acute care
Detailed Risk Interventions ü Scorecards for patient education and PCMH now include interventions and utilization data trending outcome of intervention ü Transition of Care across the continuum ü High risk problem prone patients with diabetes are seen and/or contacted within 48 hrs of discharge by an educator/diabetes staff
Strategies for Controlling Diabetes q Patient advocacy- self-management q Evidence based practice documentation q Clinical reminders-foot and retinal exam, labs q Identification of patients with A 1 C >9 ( lab reports) q Telephonic monitoring q Provision of tools and equipment q Education by case manager, educator, pharmacist q Classes q 1: 1 q Physician group visits
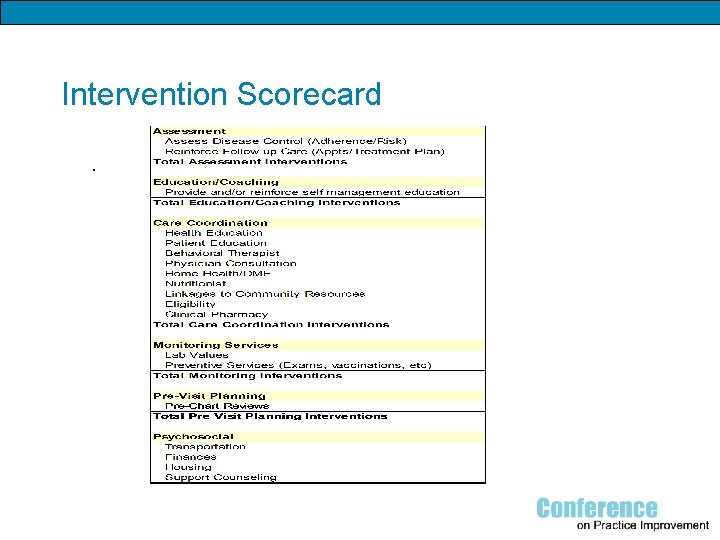
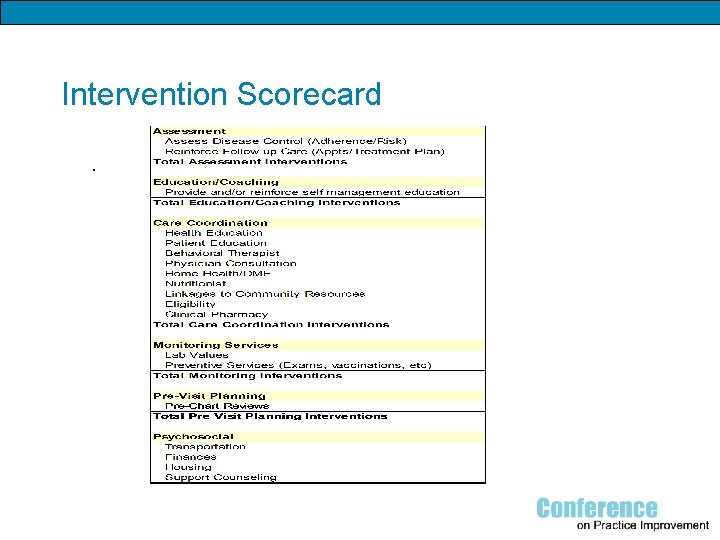
Intervention Scorecard.
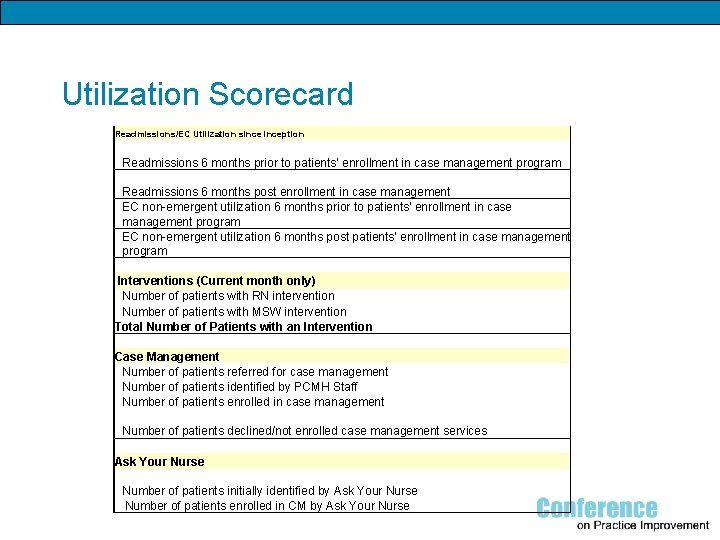
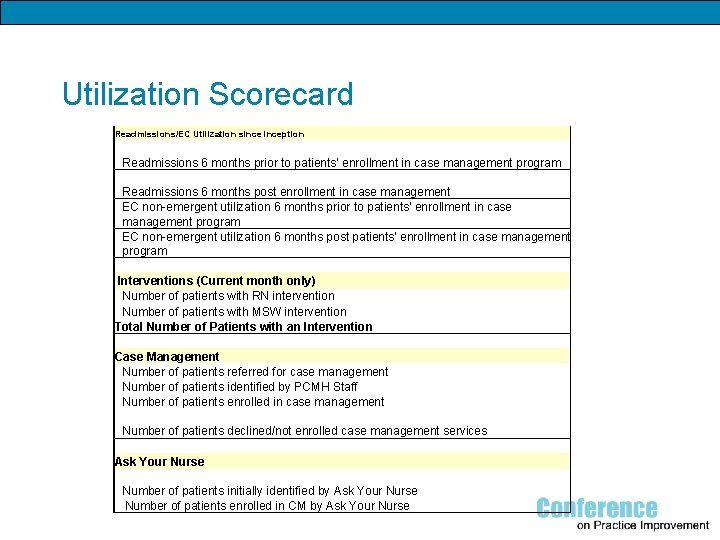
Utilization Scorecard Readmissions/EC Utilization sinception Readmissions 6 months prior to patients' enrollment in case management program Readmissions 6 months post enrollment in case management EC non-emergent utilization 6 months prior to patients' enrollment in case management program EC non-emergent utilization 6 months post patients' enrollment in case management program Interventions (Current month only) Number of patients with RN intervention Number of patients with MSW intervention Total Number of Patients with an Intervention Case Management Number of patients referred for case management Number of patients identified by PCMH Staff Number of patients enrolled in case management Number of patients declined/not enrolled case management services Ask Your Nurse Number of patients initially identified by Ask Your Nurse Number of patients enrolled in CM by Ask Your Nurse
Health Promotion and Wellness q Health Fairs q Diabetes Prevention Program q American Diabetes Association recognition q Smoking cessation q Coaching q Weight management
Noteworthy outcomes 900 patients enrolled in ongoing case management program ü 2 clinics have an average A 1 C decrease of 3% over 3 months for > 36 patients ü No shows for physician diabetes group visits < 2% versus overall 15% ü Readmissions and EC visits decreased by 25% in 9 months ü Real time utilization of patients by clinic visible in EMR
Outcomes Reporting q q Community Health Center Medical Executive Committee Performance Improvement Quality Resource Council Utilization Review Committee
Expected Return on Investment/Benefits HCHD Ø Ø Ø Ø Ø Improve Quality of care Reduce costs Reduce avoidable hospitalizations and EC visits Position HCHD for future healthcare reform and enhanced reimbursement Increase funded patient volume and attract interest from health plans Align clinical and administrative efforts and strengthen organizational matrix Alignment of performance improvement efforts Optimize “meaningful use” of Epic and other information systems Increase patient satisfaction by providing patient-centered care and open access Coordination of care using a team approach to care delivery- optimal scope of practice Ø National recognition for HCHD, BCM, and UTHSC-H
Next steps q Remote in-home monitoring for blood glucose, BP, oxygen saturation, delivered to case manager’s desk top q Congestive Heart Failure monitoring- in home scales q Optimization EMR for end user reporting q Focus on ambulatory care sensitive conditions- CHF, DM, HTN, Asthma
The Use of Clinical Case Management to Improve Outcomes in PCMH-designated Community Health Centers Questions?
References Care Continuum Alliance (2011) available from http: //carecontinuum. org/ CMSA (2010) Standards of Practice for Case Management. Available from http: //www. cmsa. org John Hopkins University. (2010). The John Hopkins ACG System. Available at http: //www. acg. jhsph. org/index. php? option=com_content&view=article&id=46&Itemi d=366 Wagner EH. (1998) Chronic disease management: What will it take to improve care for chronic illness? Effective Clinical Practice. 1(1): 2 -4. Wagner, EH et al (1996) available from http: //www. rwjf. org/files/research/021011. policysynthesis. mentalhealth. report. pdf