The Urinary System Tubular Reabsorption when water and
The Urinary System

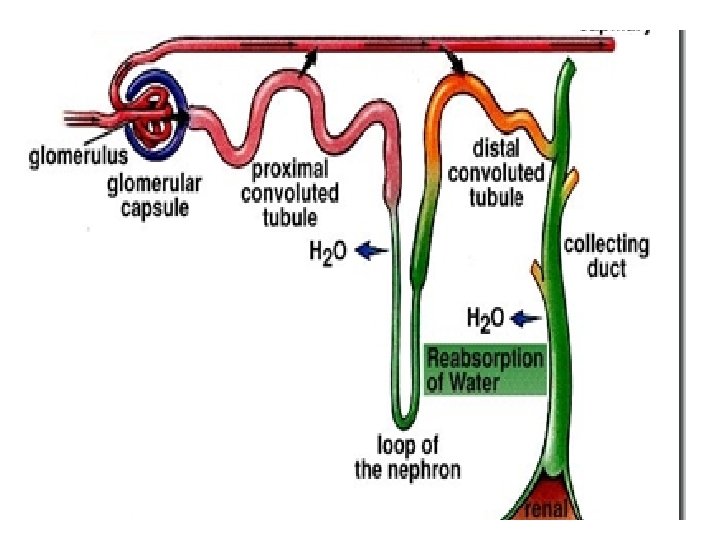
Tubular Reabsorption • when water and nutrients leave tubules by diffusion and are reabsorbed by surrounding tissue – Some nutrients enter the blood supply then return to circulation • Any excess waste and urea are kept within the tubules to be excreted with urine • Compounds reabsorbed – – – – Amino acids Glucose Frutose Na K Ca HCO 3 Cl
The Kidneys
Location and External Anatomy • • Shape/size Behind peritoneum on posterior abdominal T 12 -L 3 Protection=rib cage Renal capsule Renal fascia Hilum Renal sinus
Internal Anatomy • Organized into two regions – Inner Medulla – Outer cortex • Hilus
Blood Supply • Renal artery takes blood to the kidneys – Subdivided into nephrons • Basic units of kidneys
Function of the kidneys • • • Excretion of unwanted substances Maintenance of water balance Regulation of acid-base balance of body fluids Regulation of blood pressure Regulates production of RBC’s
Disease • Polycystic Kidney Disease – Leading cause of renal failure – Inherit condition as an autosomal dominant trait – Enlarged and contain large, fluid filled cysts – Detected using ultra sound – Diagnosed between 30 -50 years old
Ureter • Tube extending from the kidneys to bladder – Extends inferiorly and medially from renal pelvis to renal hilum of each kidney to urinary bladder • Function = carry urine • Transitional epithelium lines both ureters and urinary bladder • Circular smooth muscle in walls of ureters undergo peristaltic contractions which force urine through ureters – Occur every few seconds to once every 2 -3 minutes • Pressure inside of urinary bladder compresses that part of ureter to prevent backflow of urine
Urethra: • Tube extending from bladder to outside of body – Males = conveys sex cells, drains bladder, about 8 inches long – Females = about 1. 5 inches long, only drains bladder • Function = urination/expelling urine from the bladder – Voluntary (External) and Involuntary (Internal) by aid of sphincters • Sphincter = valve that controls flow of urine through urethra • Lined with stratified (or pseudostratified) columnar epithelium • Where urethra exists bladder elastic connective tissue and smooth muscle keep urine from flowing out of bladder until pressure in bladder is great enough to force urine out

Both: • Triangular area wall between 2 ureters posteriorly and urethra anteriorly is called the trigone • Irritation or bacterial infection of urethra can cause urge to urinate even if urinary bladder is empty
Tubular Secretion
Definition • The third major process in urine formation. • It occurs when the nephron cells transport solutes from the blood into the filtrate. • It’s the movement of nonfiltered substances, toxic by-products of metabolism and drugs or molecules not normally produced by the body, from the blood into the filtrate.
• Tubular secretion is the transfer of materials from peritubular capillaries to renal tubular lumen and occurs mainly by active transport • This removes excessive quantities of certain dissolved substances from body also maintains the blood at a normal healthy p. H level. • The substances that are secreted into the tubular fluid for removal from the body include: K+, H+, and NH 4+, creatinine, urea, some hormones, and some drugs.
Urine Concentration Ben Clark and Diana Kiori
Concentration of Urine • • 95% water 5% dissolved solids/gases p. H= 6. 0 Concentration can range from a minimum of 65 to a max of 1200 m. Osm/Kg. This can be done while maintaining the extracellular concentration close to 300 m. Osm/Kg – m. Osm= concentration of interstitial fluid
Urine concentration • Concentration can depend on high amounts of solutes • Regulation of urine concentration can vary due to hormonal changes and within the nervous system • If homeostasis calls for elimination of large volumes of urine, then diluted filtrate will pass the urine into ureters. • Countercurrent mechanism= method for concentrating urine based on movement of ions out of nephrons • Water follows salt, so urine becomes more concentrated and volume will decrease.
Urinary Disorders • • Glomerulonephritis Acute Glomerulonephritis Chronic Glomerulonephritis Pyelonephritis Renal Failure Acute Renal Failure Chronic Renal Failure
The Hilus
Location -a small indentation on the concave medial side of the kidney -where the renal artery and ureter enter and the renal vein and ureter exit (connect to the inside of the kidney)
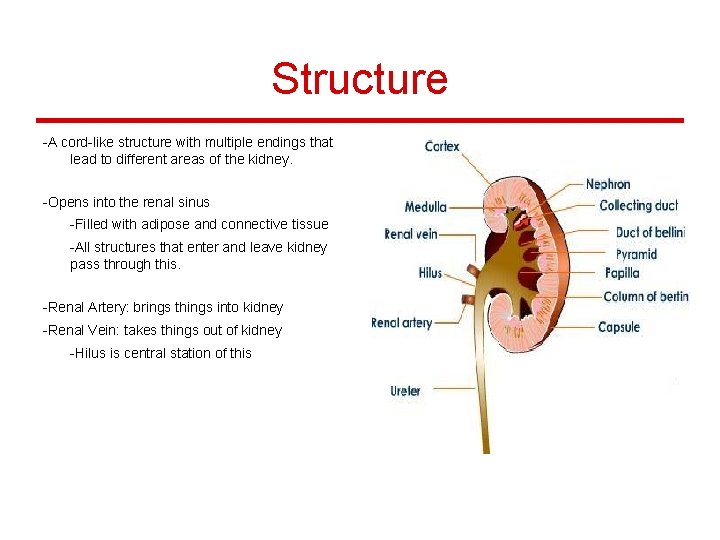
Structure -A cord-like structure with multiple endings that lead to different areas of the kidney. -Opens into the renal sinus -Filled with adipose and connective tissue -All structures that enter and leave kidney pass through this. -Renal Artery: brings things into kidney -Renal Vein: takes things out of kidney -Hilus is central station of this
Function -the renal artery brings the blood with waste in it into the kidney to be filtered -the renal vein takes the filtered blood out to the rest of the body -the ureter is where the waste from the blood goes and where urine begins to form
Possible Problems -Problems with being hit in the kidney: -Hilus (renal artery, vein, and ureter) may become detached in an area -Result: internal bleeding -Bleeding may involve blood with toxins/waste in it -Bleeding may involve blood that has already been filtered -Internal Bleeding may lead to blood poisoning
Possible Problems -Renal failure -Could result in the shutting down of renal artery and vein -May not allow anything to pass in or out of the kidney if these aren’t working -Kidney Stones -May pass through hilus in order to get to the ureter -Could possibly result in blocking the hilus -Bacteria may infect the entire area -Accumulation of waste in blood that does not get filtered properly may result in Acute Renal Failure -Result → Catheter (may have to pass through artery/vein in order to reach kidney)
Urinary Bladder The ‘p’ brothers (pun intended)
General information • Hollow, muscular container that lies in the pelvic cavity just posterior to the symphysis pubis. • This container works as a temporary reservoir for urine • In males, it is just anterior to the rectum • In females, it is anterior to the vagina & inferior and anterior to the uterus
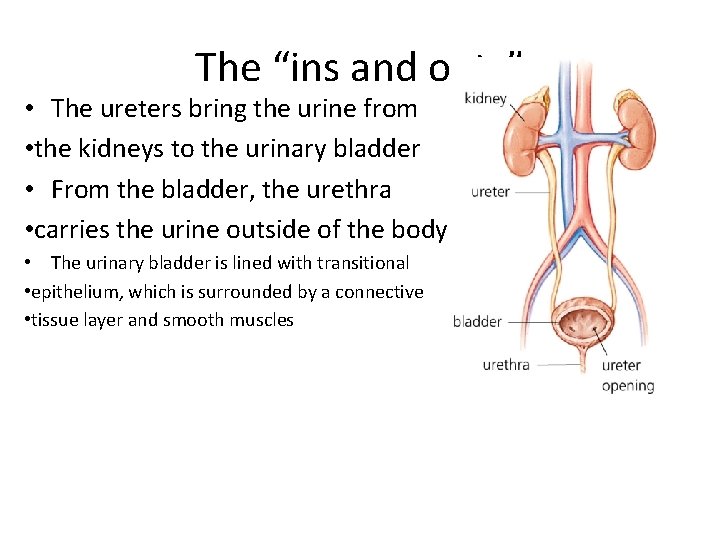
The “ins and outs” • The ureters bring the urine from • the kidneys to the urinary bladder • From the bladder, the urethra • carries the urine outside of the body • The urinary bladder is lined with transitional • epithelium, which is surrounded by a connective • tissue layer and smooth muscles
• • • Complications Cystitis: inflammation of the urinary bladder Tumors Cancer Automatic bladder: no control over the disposal of urine A scenario that can/does happen: there is damage to the sacral region of the spinal cord (nerves) can make the bladder unable to contract on demand
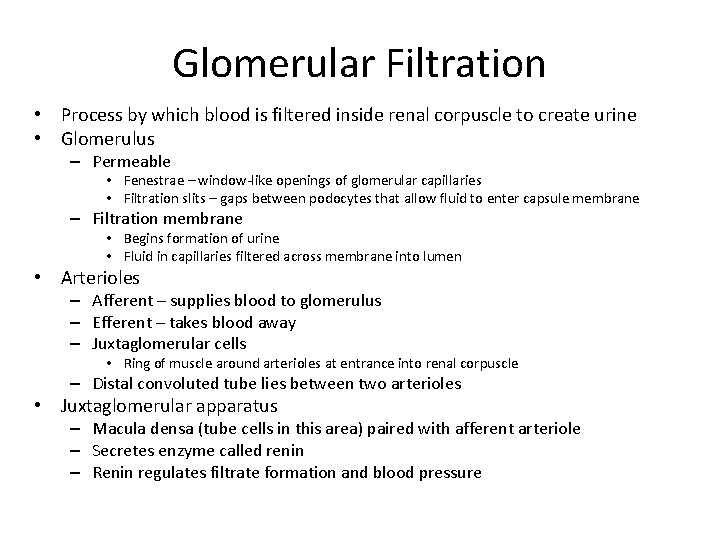
Glomerular Filtration • Process by which blood is filtered inside renal corpuscle to create urine • Glomerulus – Permeable • Fenestrae – window-like openings of glomerular capillaries • Filtration slits – gaps between podocytes that allow fluid to enter capsule membrane – Filtration membrane • Begins formation of urine • Fluid in capillaries filtered across membrane into lumen • Arterioles – Afferent – supplies blood to glomerulus – Efferent – takes blood away – Juxtaglomerular cells • Ring of muscle around arterioles at entrance into renal corpuscle – Distal convoluted tube lies between two arterioles • Juxtaglomerular apparatus – Macula densa (tube cells in this area) paired with afferent arteriole – Secretes enzyme called renin – Renin regulates filtrate formation and blood pressure
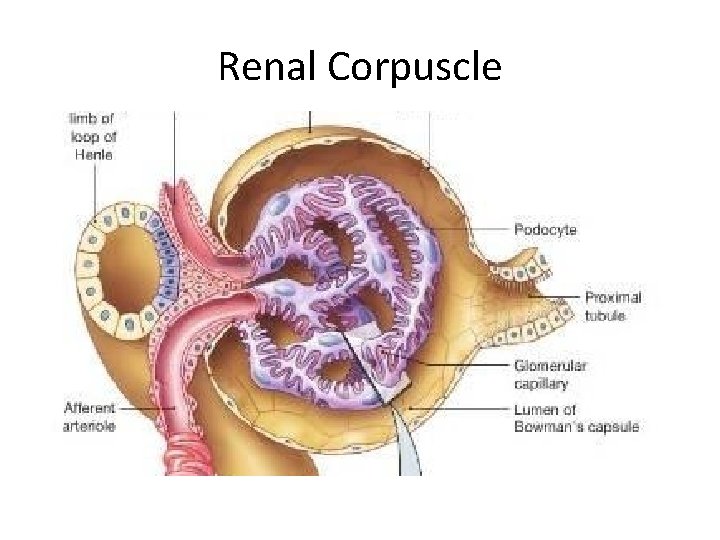
Renal Corpuscle
- Slides: 31