The Urinary System Power Point Lecture Slide Presentation




- Slides: 55

The Urinary System Power. Point® Lecture Slide Presentation by Jerry L. Cook, Sam Houston University ESSENTIALS OF HUMAN ANATOMY & PHYSIOLOGY EIGHTH EDITION ELAINE N. MARIEB adapted by H. Goon May 2010 Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
A) Functions of the Urinary System 1. Elimination of waste products (kidneys filter 200 liters of blood daily) § nitrogenous wastes (urea, uric acid) § toxins § drugs Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings

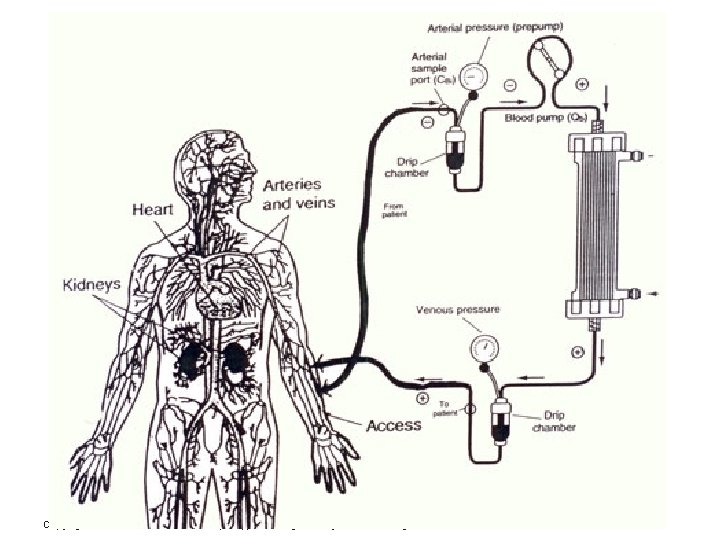
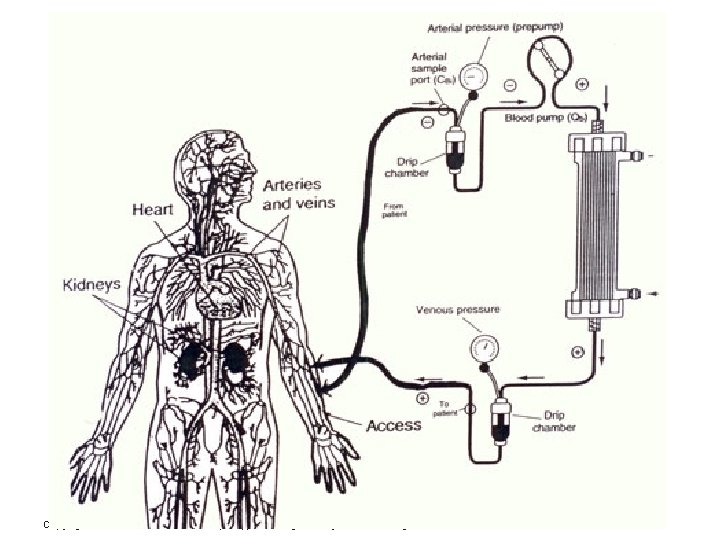
hemodialysis ___________________________________________ Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
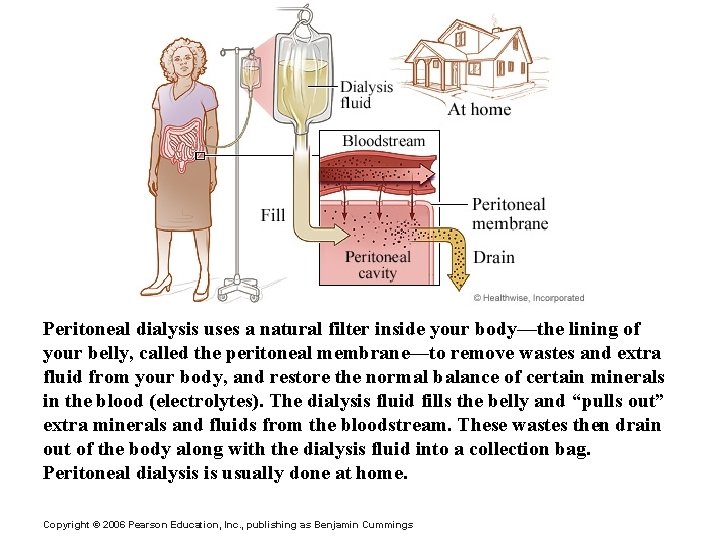
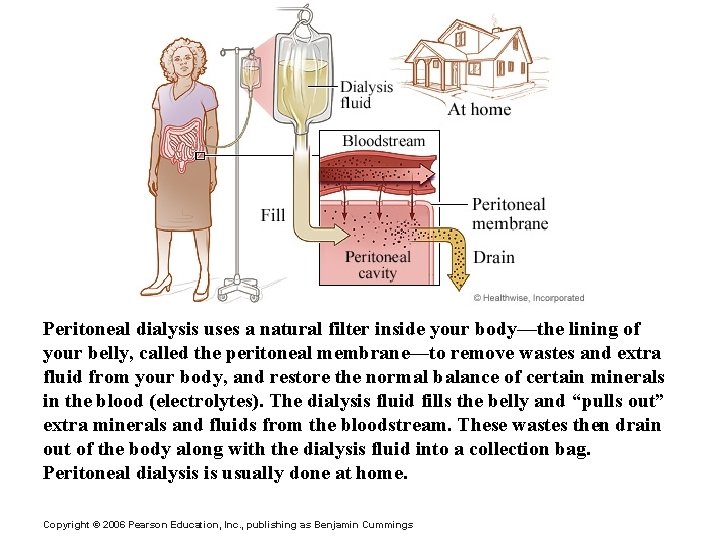
Peritoneal dialysis uses a natural filter inside your body—the lining of your belly, called the peritoneal membrane—to remove wastes and extra fluid from your body, and restore the normal balance of certain minerals in the blood (electrolytes). The dialysis fluid fills the belly and “pulls out” extra minerals and fluids from the bloodstream. These wastes then drain out of the body along with the dialysis fluid into a collection bag. Peritoneal dialysis is usually done at home. Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings

Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
2. Regulate aspects of homeostasis § Water balance § Electrolytes (ions: Na+, K+, Cl-, HCO 3 -) § Acid-base (p. H) balance in the blood Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
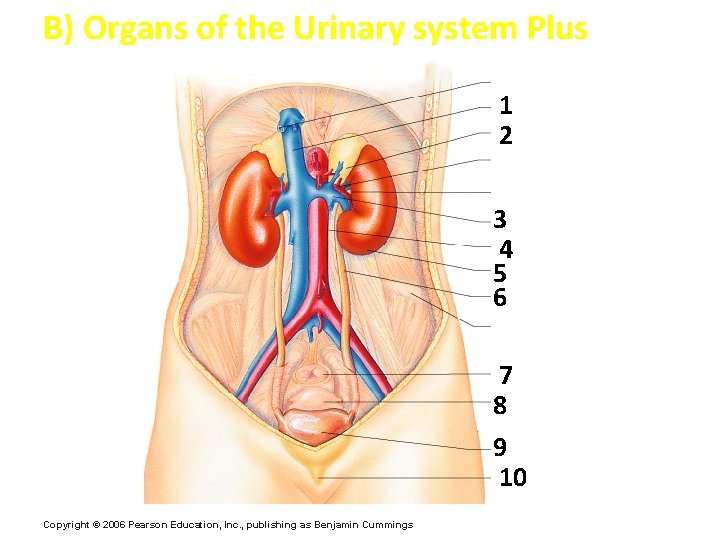
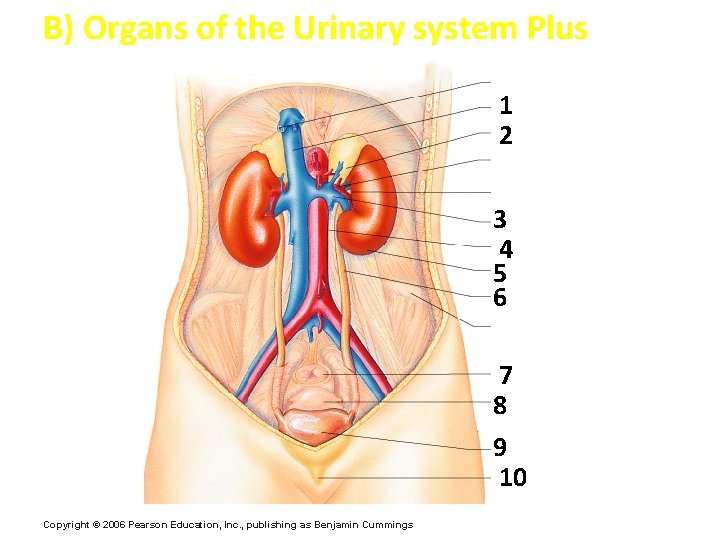
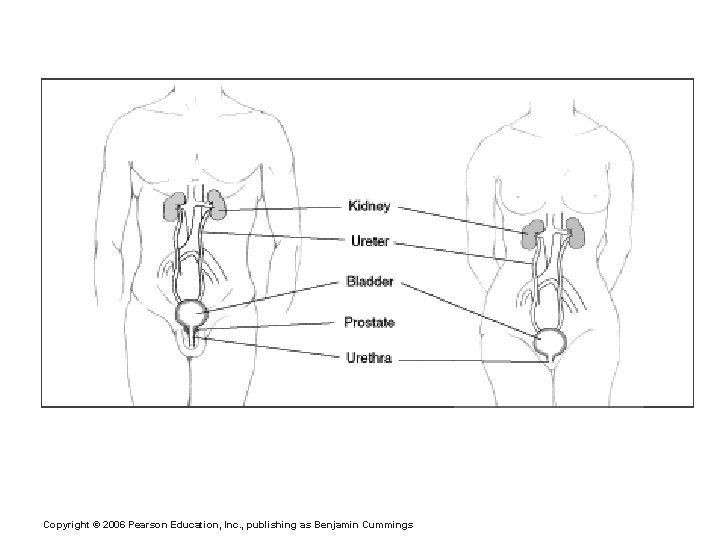
B) Organs of the Urinary system Plus 1 2 3 4 5 6 7 8 9 10 Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
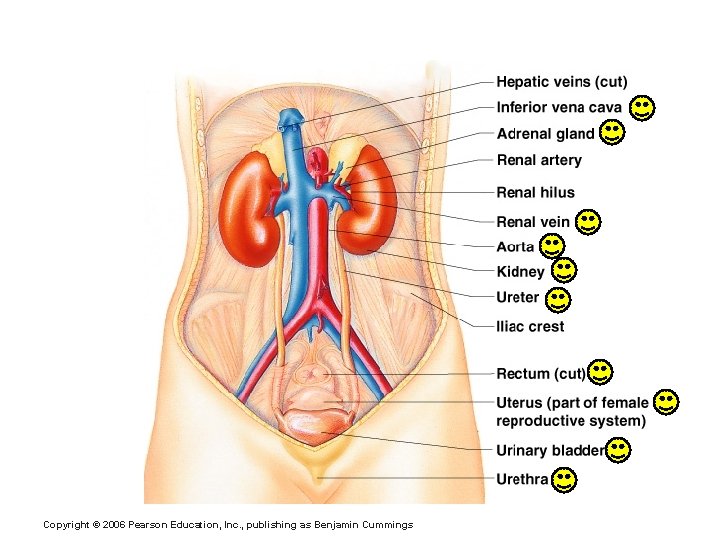
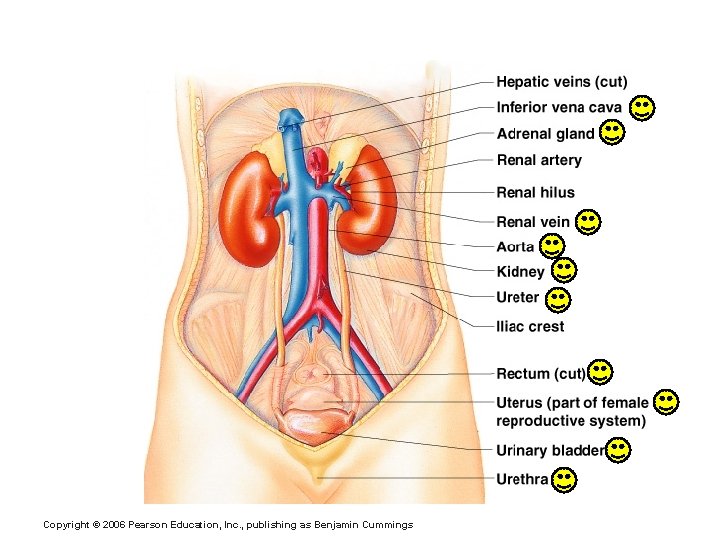
B) Organs of the Urinary system Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
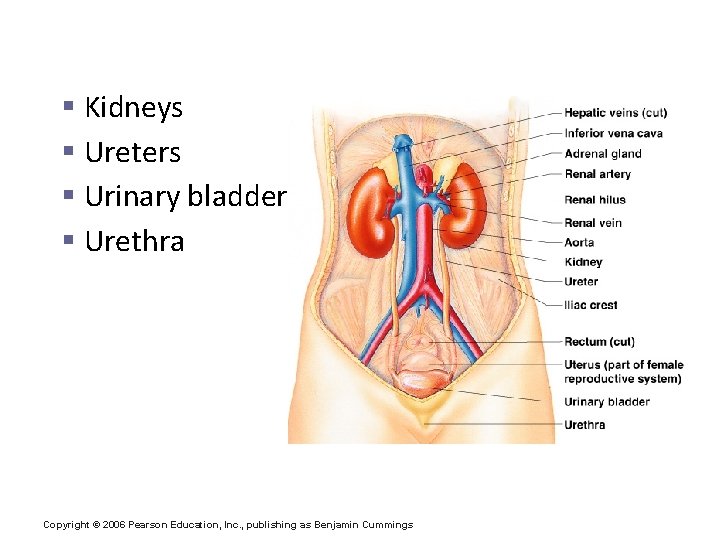
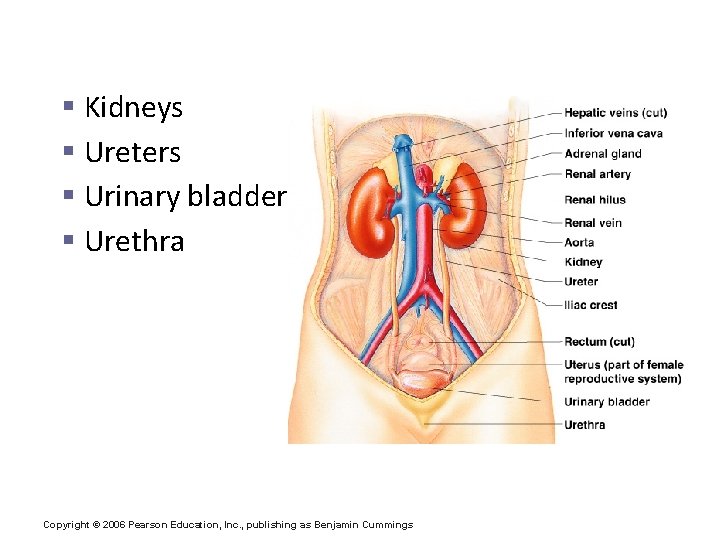
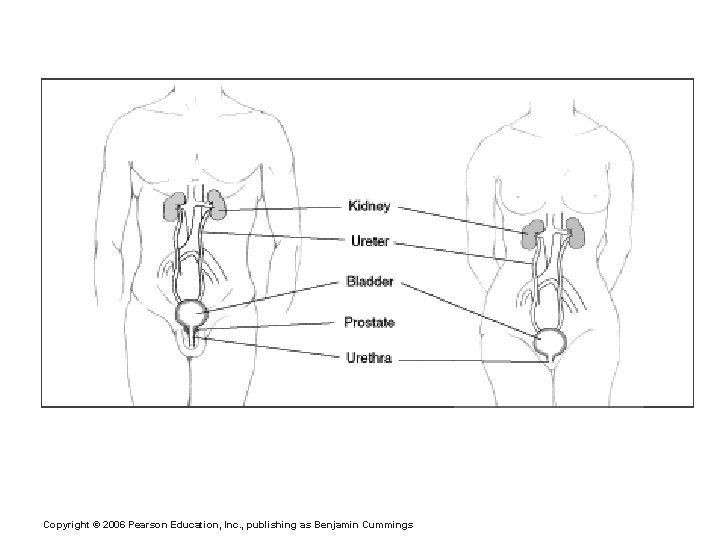
B) Organs of the Urinary system § Kidneys § Ureters § Urinary bladder § Urethra Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
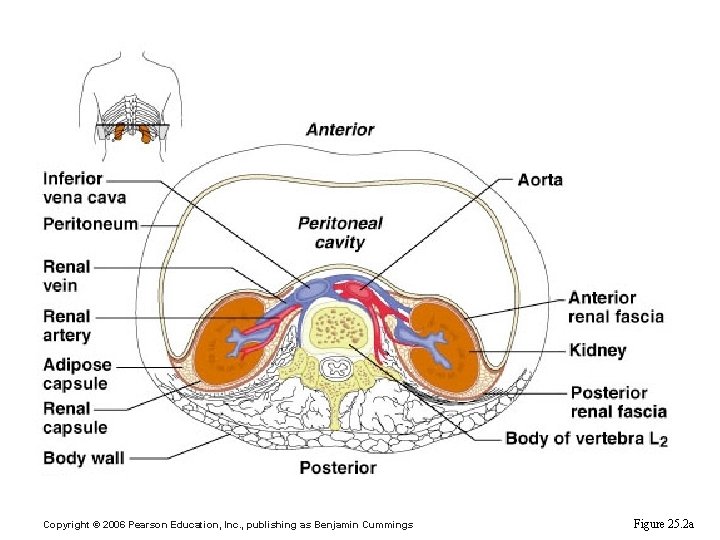
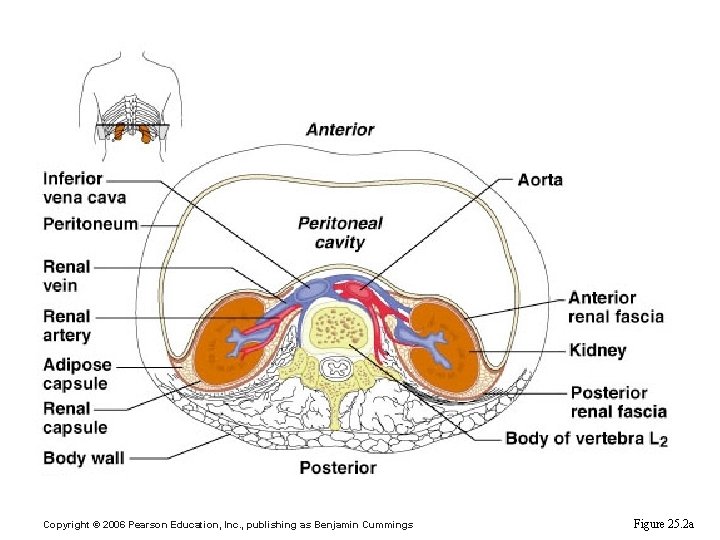
Kidney Location and External Anatomy Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings Figure 25. 2 a
C) Kidneys 1. Location § against the dorsal body wall § at the level of T 12 to L 3 § The right kidney is slightly lower than the left § an adrenal gland is above each kidney Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
2. Coverings of the Kidneys a) Renal capsule § fibrous covering on each kidney b) Adipose capsule § cushions and protects the kidney § keeps the kidney in its correct location Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
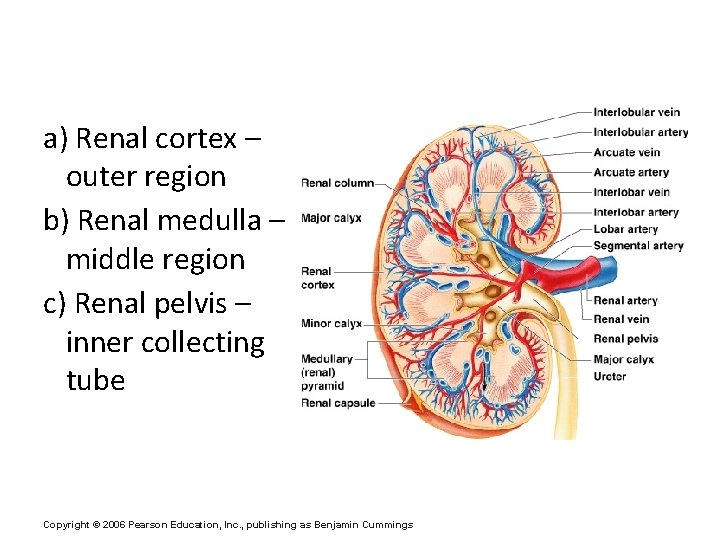
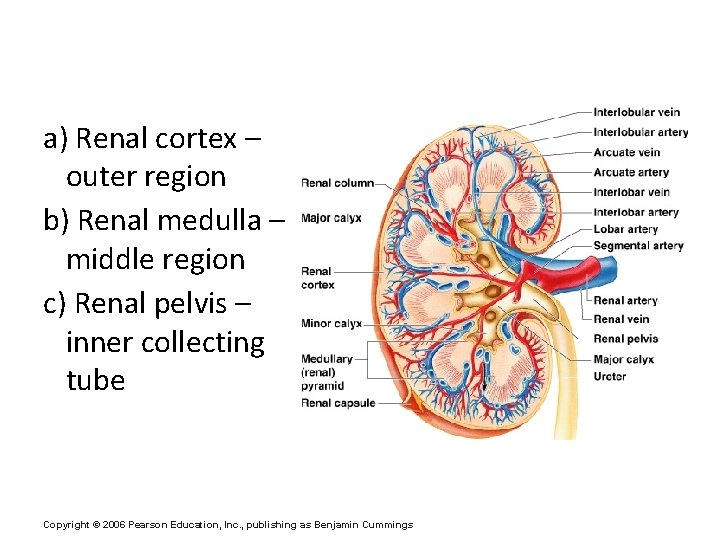
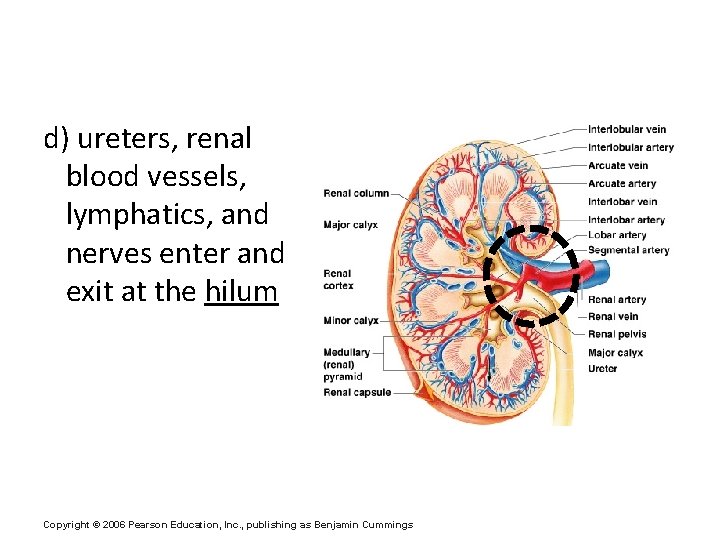
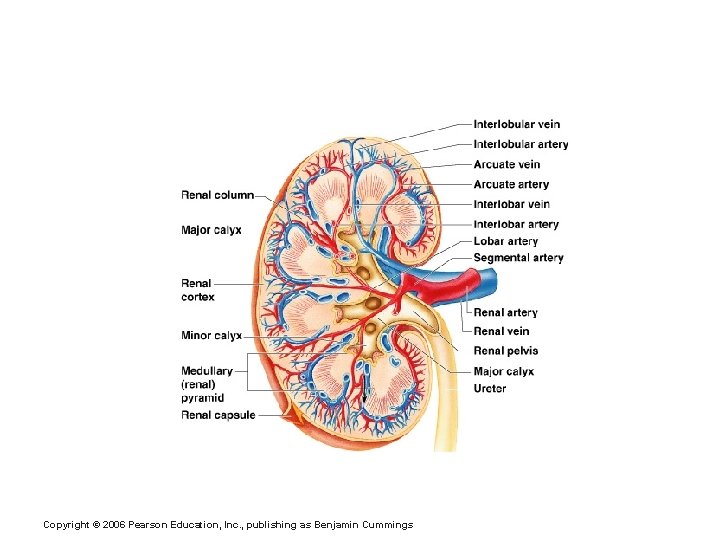
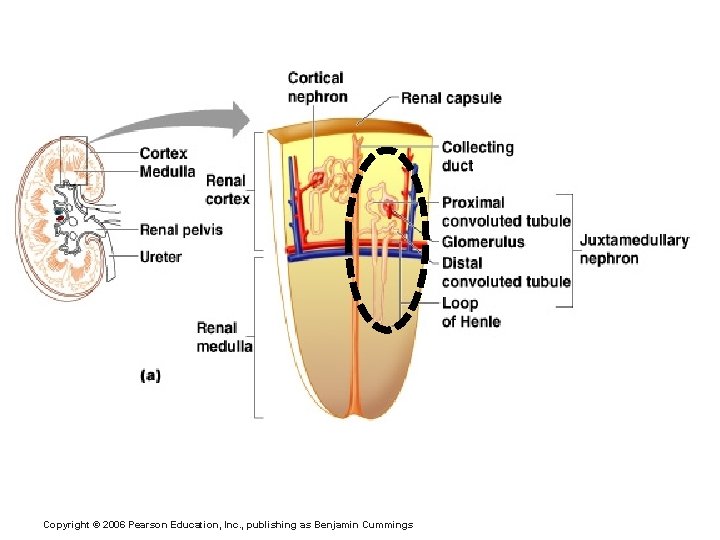
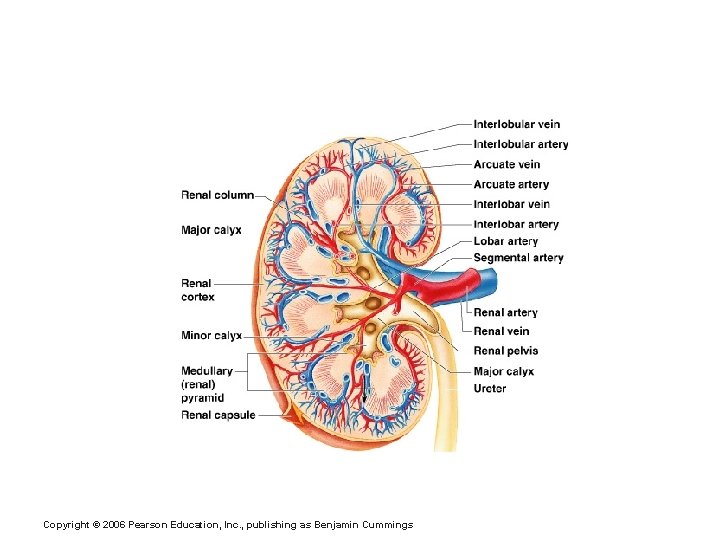
3. Regions of the Kidney a) Renal cortex – outer region b) Renal medulla – middle region c) Renal pelvis – inner collecting tube Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
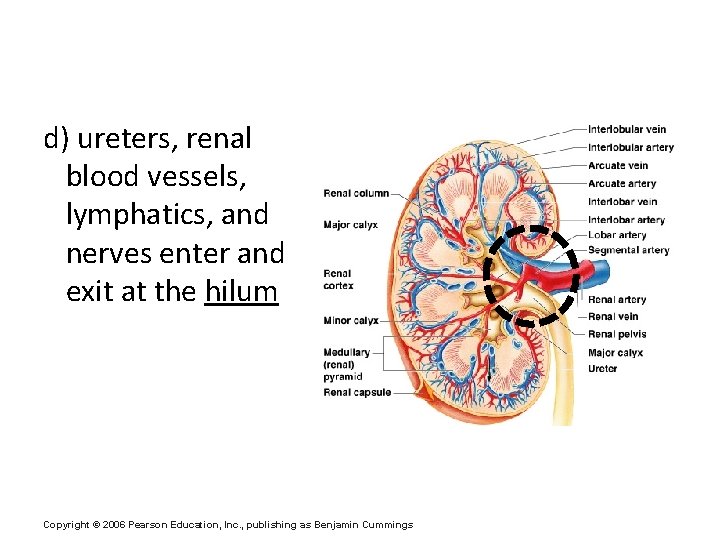
d) ureters, renal blood vessels, lymphatics, and nerves enter and exit at the hilum Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
4. Kidney Structures a) medullary/renal pyramids – triangular regions of tissue in the medulla b) renal columns – extensions of cortex-like material inward in between pyramids c) calyces – cup-shaped branches that funnel urine towards the renal pelvis Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
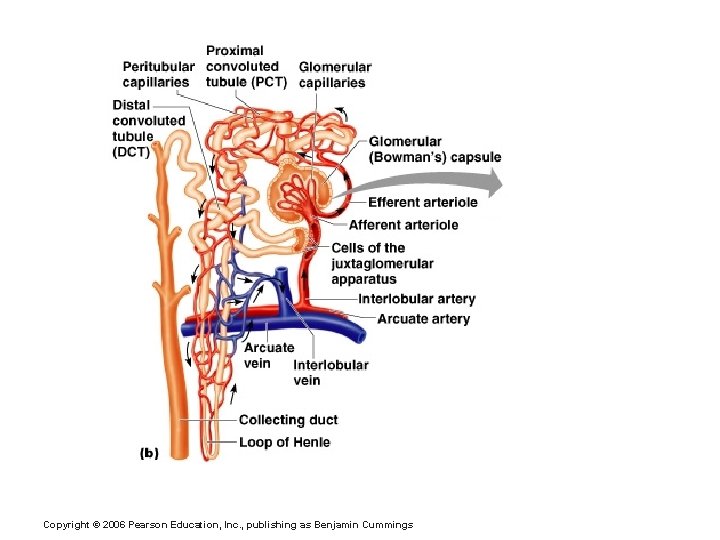
5. Blood Flow in the Kidneys ~ one-fourth (1200 ml) of systemic cardiac output flows through the kidneys each minute Figure 15. 2 c Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
Regions of the Kidney Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
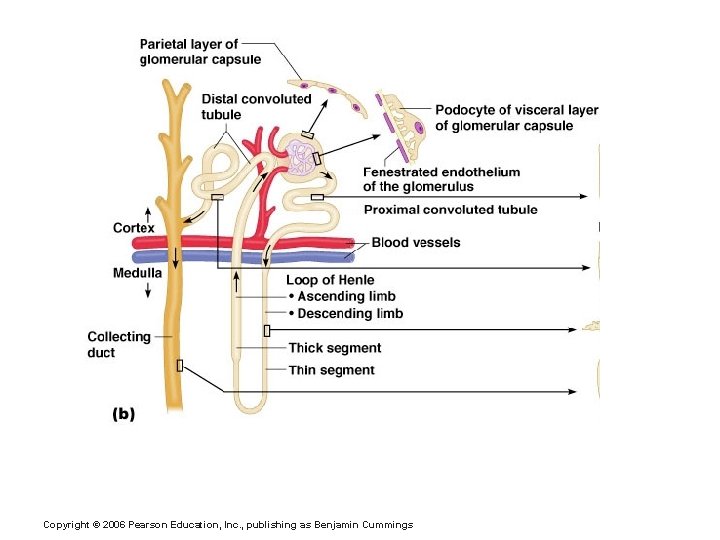
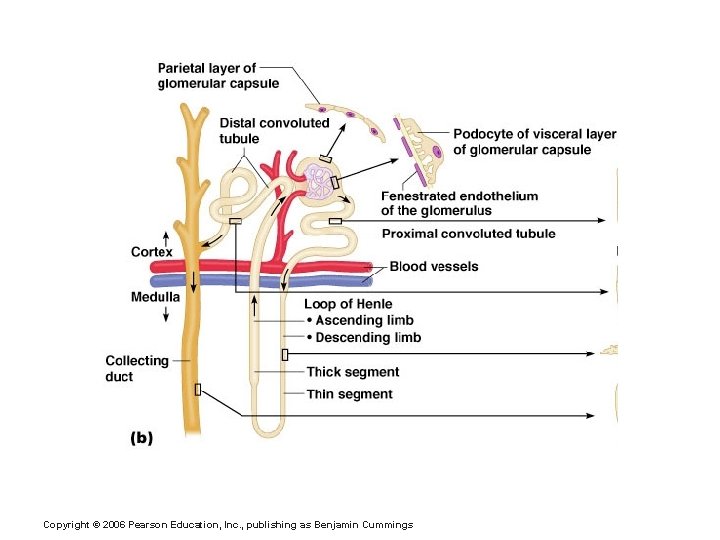
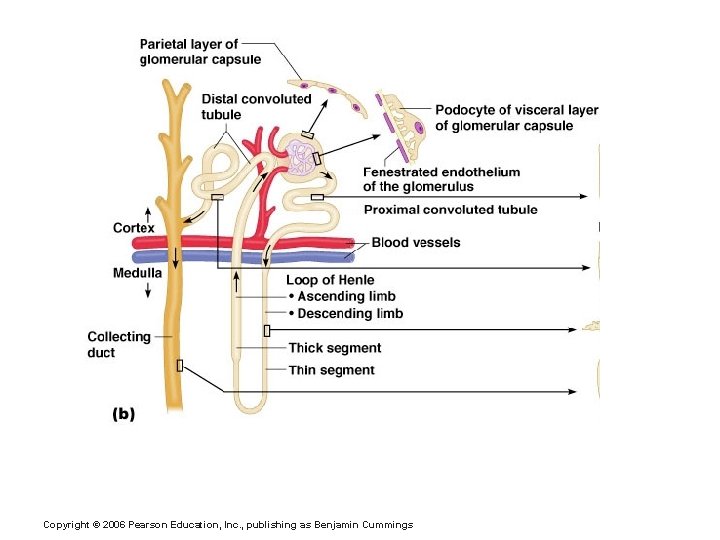
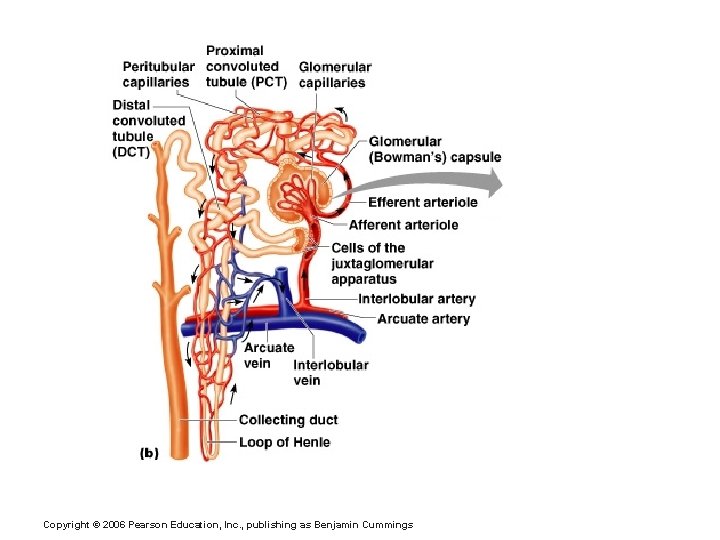
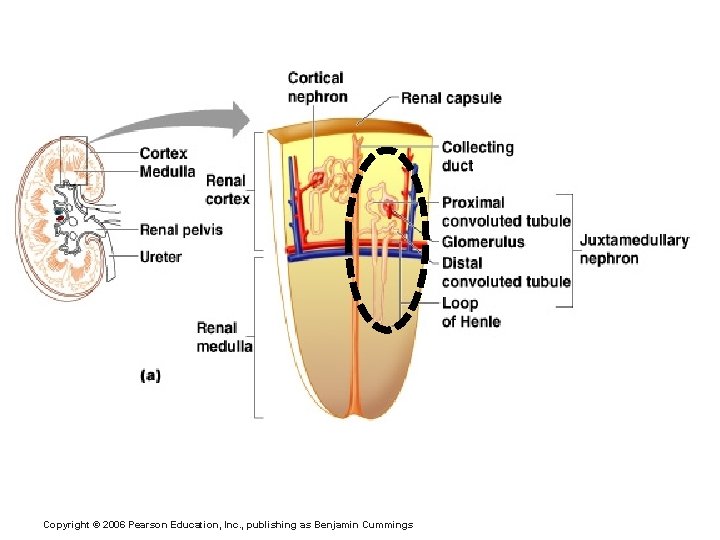
6. Nephrons a) The structural and functional units of the kidneys [1 million per kidney] b) Responsible forming urine c) Main structures of the nephron § renal corpuscle (glomerulus + glomerular capsule) § renal tubule Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
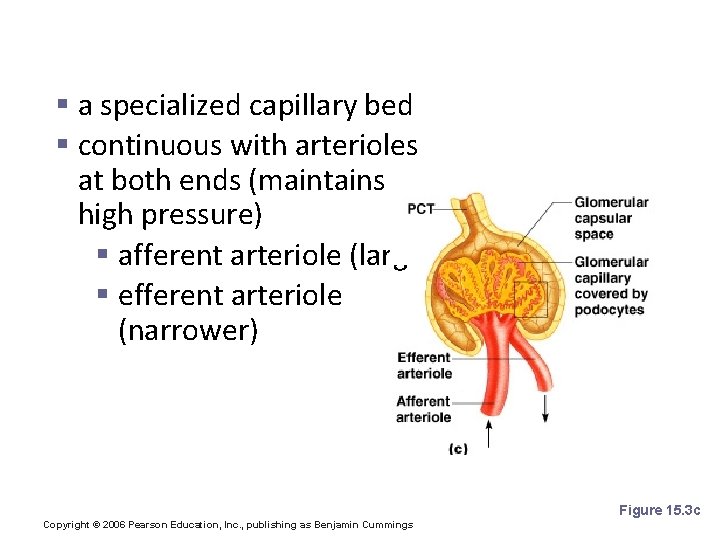
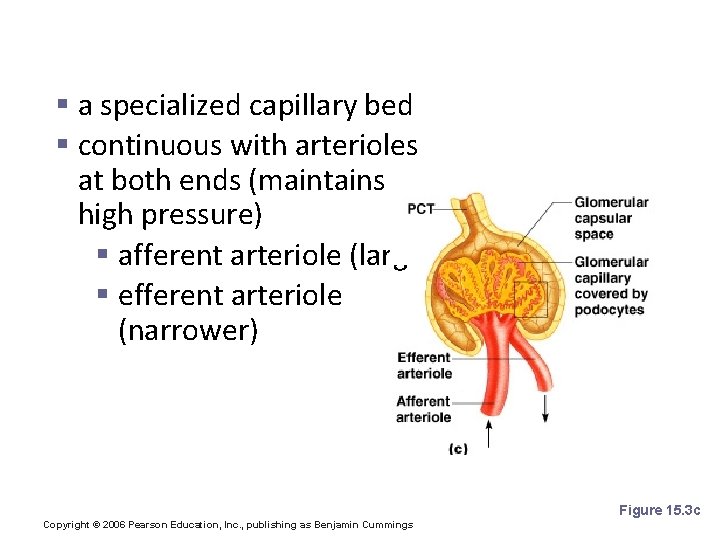
d) glomerulus § a specialized capillary bed § continuous with arterioles at both ends (maintains high pressure) § afferent arteriole (large) § efferent arteriole (narrower) Figure 15. 3 c Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
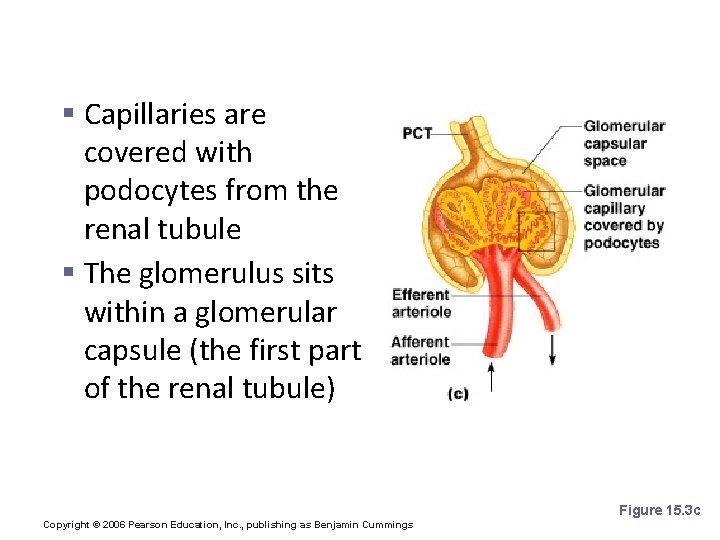
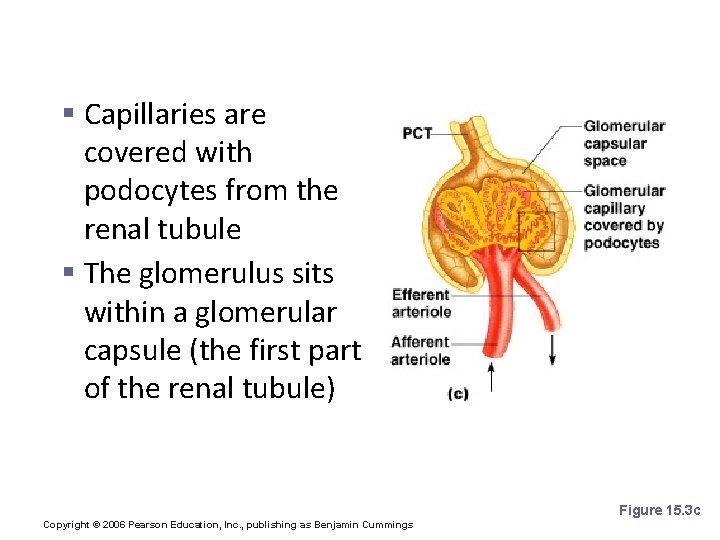
§ Capillaries are covered with podocytes from the renal tubule § The glomerulus sits within a glomerular capsule (the first part of the renal tubule) Figure 15. 3 c Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
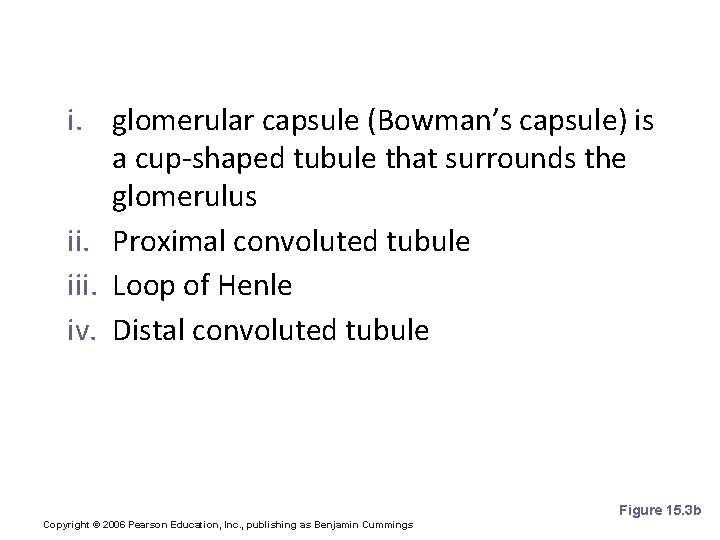
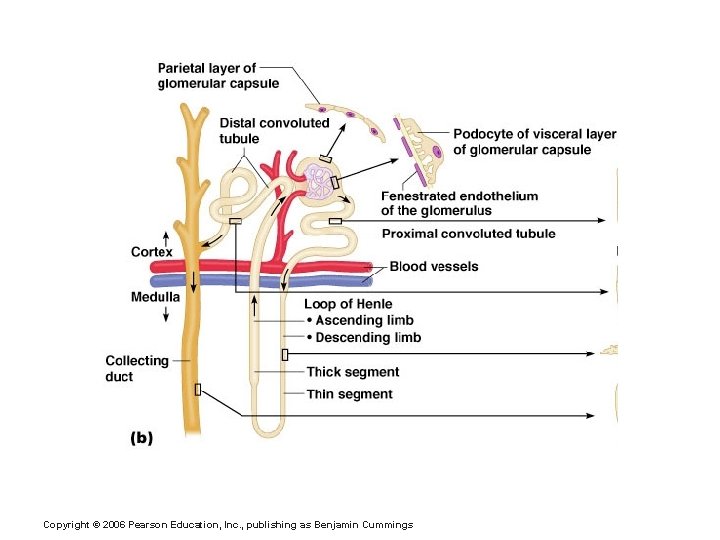
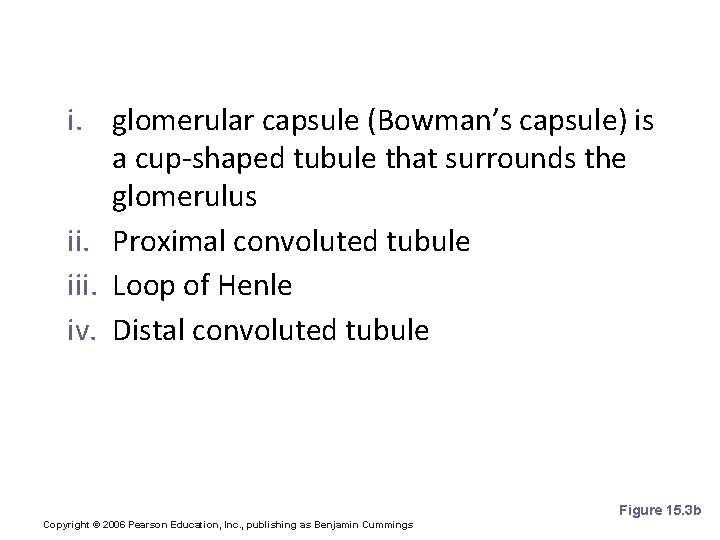
e) renal tubule i. glomerular capsule (Bowman’s capsule) is a cup-shaped tubule that surrounds the glomerulus ii. Proximal convoluted tubule iii. Loop of Henle iv. Distal convoluted tubule Figure 15. 3 b Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
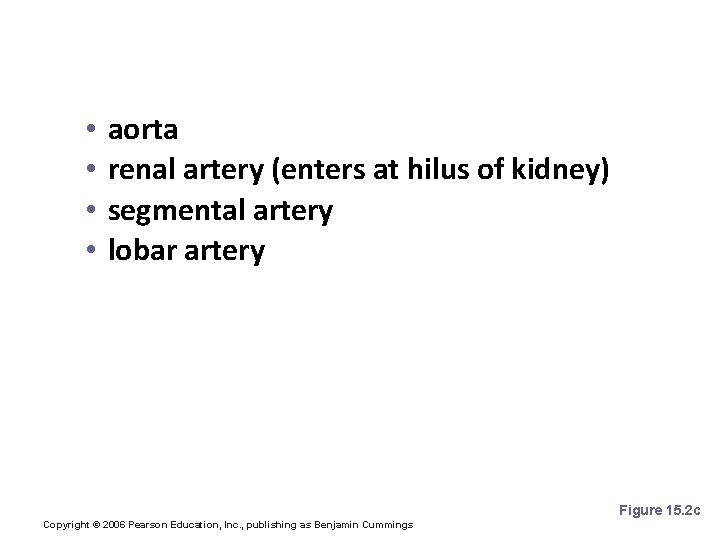
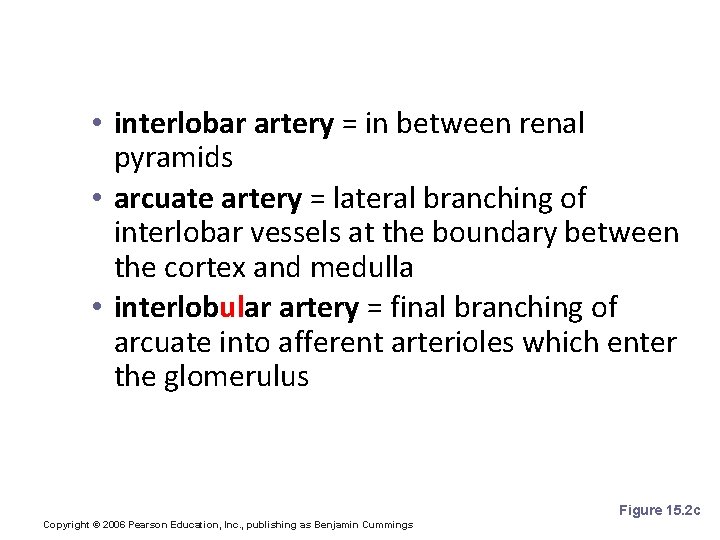
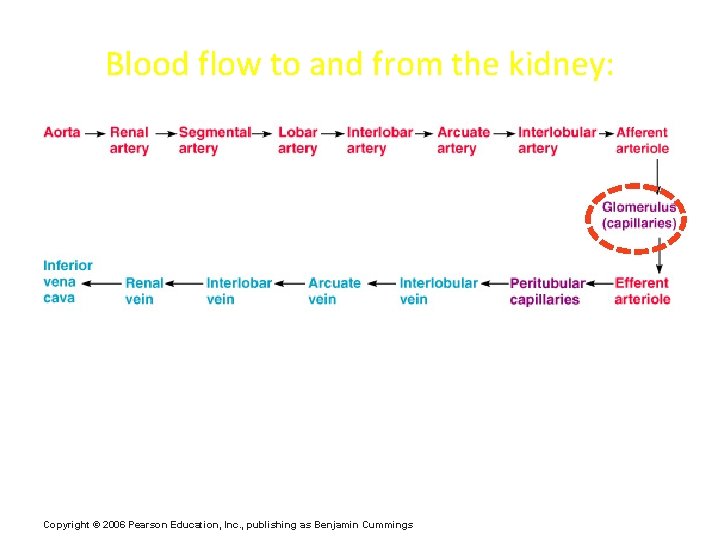
7. Blood Supply to Kidneys/Nephrons • • aorta renal artery (enters at hilus of kidney) segmental artery lobar artery Figure 15. 2 c Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
• interlobar artery = in between renal pyramids • arcuate artery = lateral branching of interlobar vessels at the boundary between the cortex and medulla • interlobular artery = final branching of arcuate into afferent arterioles which enter the glomerulus Figure 15. 2 c Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
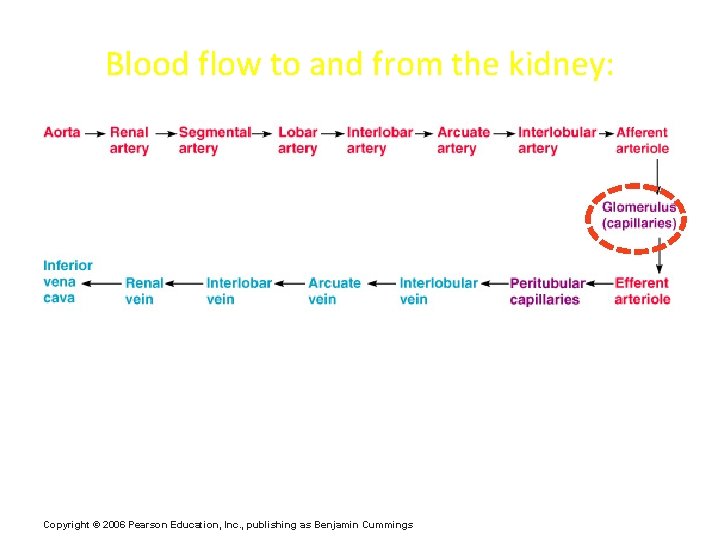
Blood flow to and from the kidney: Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
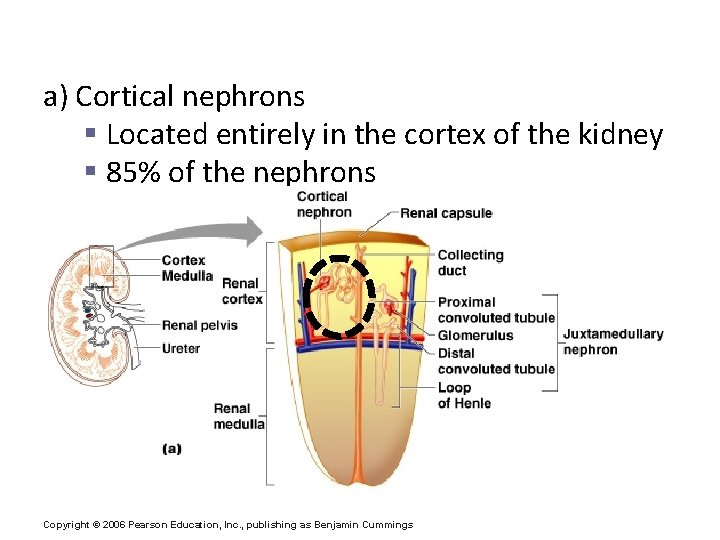
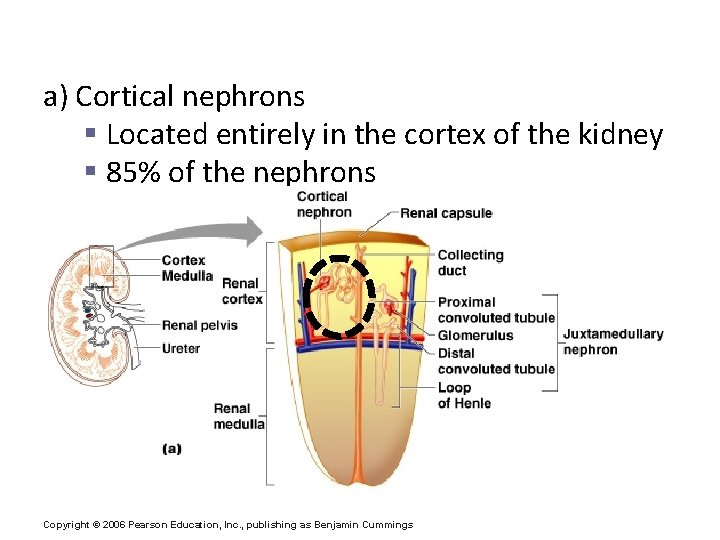
8. Types of Nephrons a) Cortical nephrons § Located entirely in the cortex of the kidney § 85% of the nephrons Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
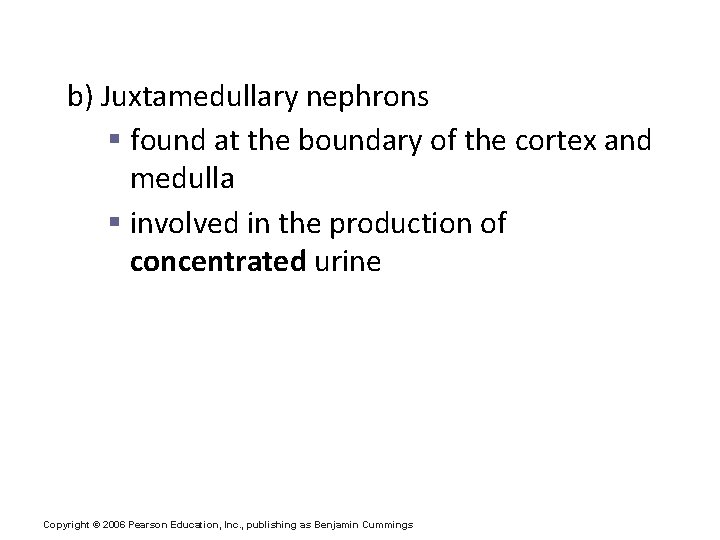
b) Juxtamedullary nephrons § found at the boundary of the cortex and medulla § involved in the production of concentrated urine Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
9. Peritubular Capillaries § network of capillaries surrounding the renal tubule; formed by the branching of the efferent arteriole § normal, low pressure capillaries § attach to a venule § reabsorb (reclaim) some substances from renal tubule Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
? ? ? The kidneys remove 180 liters of filtrate from the blood per day. How much urine do you actually eliminate per day? Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
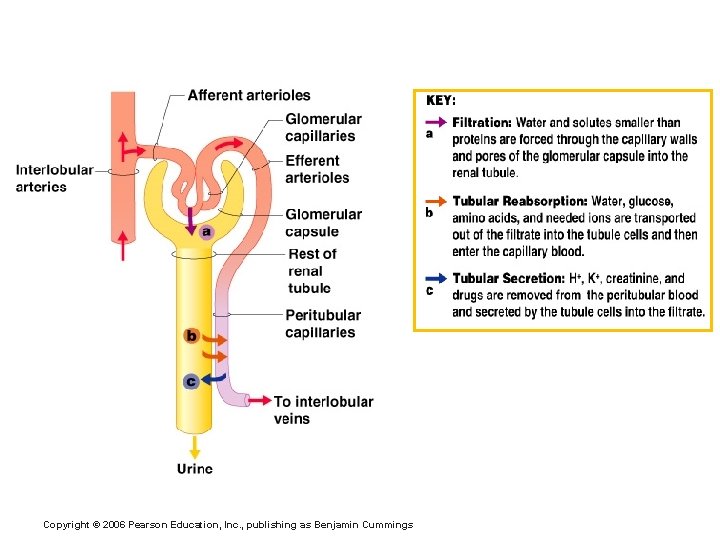
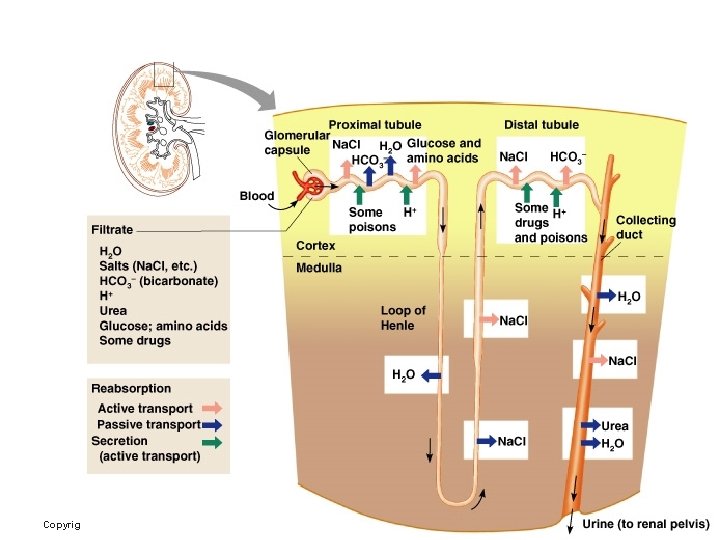
D) Urine Formation Processes glomerular filtration - tubular reabsorption + tubular secretion urine Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
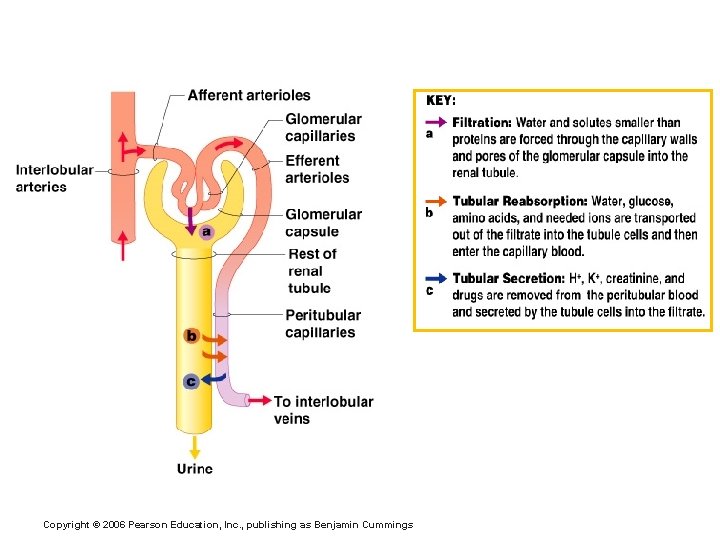
1. Filtration § The fenestrated glomerular endothelium allows water and solutes (filtrate) to easily pass from the blood in the glomerulus into the glomerular capsule § Nonselective passive process § Water and solutes are forced through capillary walls b/c glomerular blood pressure is high, which causes a high net filtration pressure Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
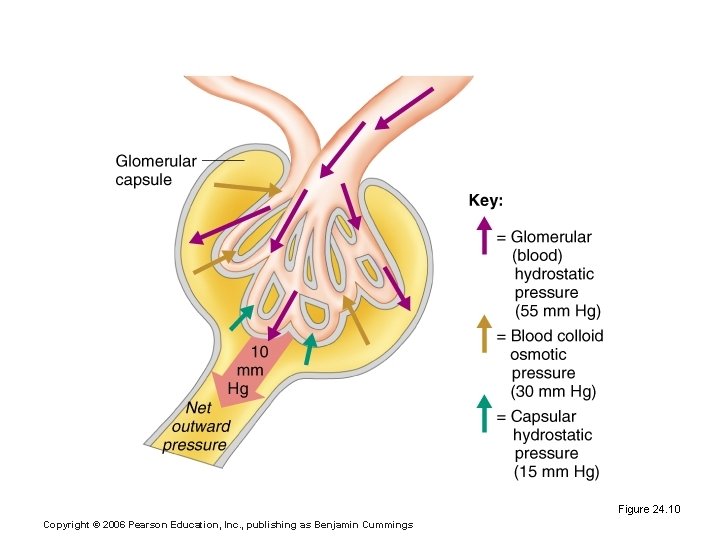
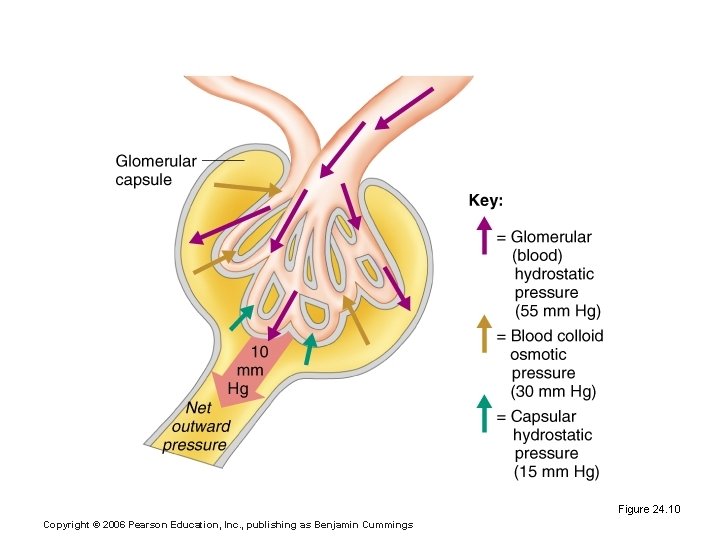
Glomerular Filtration Rate (GFR) Figure 24. 10 Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
§ Plasma proteins are not filtered due to large size § GFR (glomerular filtration rate)= total amount of filtrate formed per minute by the kidneys [180 L/day] Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
2. Tubular Reabsorption a) occurs as the peritubular capillaries reabsorb several materials [NOTE: back into bloodstream] § some water § glucose § amino acids § ions b) most reabsorption is via active transport, and occurs in the proximal convoluted tubule (PCT) Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
c) materials NOT reabsorbed: nitrogenous waste products Ø urea Ø uric acid Ø creatinine § excess water § Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
3. Tubular Secretion – reabsorption in “reverse” Some materials move from the peritubular capillaries back into the filtrate (urine) forming in the renal tubules: § hydrogen and potassium ions § creatinine § drugs Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
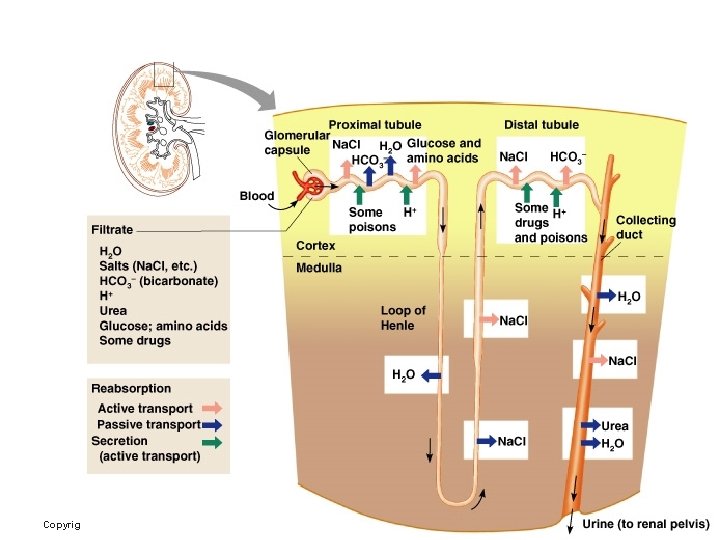
Formation of Urine Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
E) Hormonal control of urine formation 1. ADH (anti-diuretic hormone) § from pituitary gland § causes reabsorption of water (so urine contains less water) in DCT & collecting duct 2. aldosterone § from adrenal gland § causes Na+ reabsorption in DCT & collecting duct (e. g. water retention triggered by low blood volume or low blood pressure) Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
e. g. Alcohol and urine production • ADH acts on the kidney to reabsorb water back into bloodstream (makes urine more concentrated) • Alcohol inhibits the pituitary secretion of anti-diuretic hormone (ADH), which then causes ADH levels to drop. Ø Therefore, the kidneys don't reabsorb as much water and the kidneys produce a higher volume of URINE (more diluted). Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
F) Characteristics of Urine for Medical Diagnosis v somewhat yellow color due to the pigment urochrome (from the destruction of hemoglobin) and solutes v sterile v slightly aromatic v normal p. H ~ 6 v specific gravity of 1. 001 to 1. 035 Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
G) Ureters § a pair of slender tubes that transport urine from the kidney to the bladder § Continuous with the renal pelvis § Enter the posterior aspect of the bladder § peristalsis aids gravity in urine transport Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
H) Urinary bladder § muscular, hollow organ § stores up to 600 m. L of urine (~ 2 cups) Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
I) Urethra § short tube that transports urine out of the bladder Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
J) Micturition (urinary reflex) § stretch receptors are stimulated when the bladder fills with 150 m. L, then 300 m. L of urine; capacity of 600 m. L § The muscles controlling micturition are controlled by the autonomic and somatic nervous systems. § During the storage phase the internal urethral sphincter remains tense and the detrusor muscle (in walls of the bladder) is relaxed. Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
§ During micturition, parasympathetic stimulation causes the detrusor muscle to contract and the internal urethral sphincter to relax. § The external urethral sphincter (skeletal muscle) is under somatic control and is consciously relaxed during micturition. e. g. potty training! Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
Review: Micturition = urination reflex (Fill in the blanks!) v at 300 m. L, stretch receptors in the bladder wall are triggered v parasympathetic impulses trigger: § contraction of the detrusor muscle layer § relaxation of the internal urethral sphincter muscle § relaxation of the external urethral sphincter (skeletal muscle) Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings

Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings
? ? Regulation of Glomerular Filtration § Three mechanisms control the GFR § Renal autoregulation (intrinsic system) § Neural controls § The renin-angiotensin system (hormonal mechanism) Copyright © 2006 Pearson Education, Inc. , publishing as Benjamin Cummings