THE URINARY SYSTEM FUNCTIONS OF THE URINARY SYSTEM

- Slides: 19
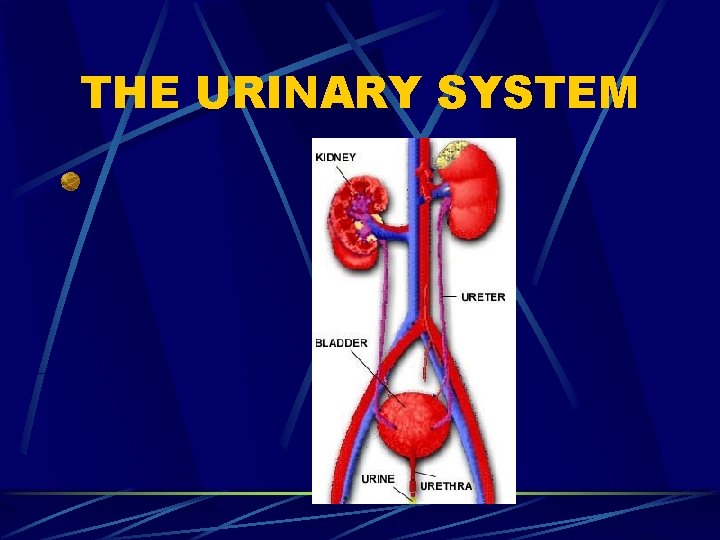
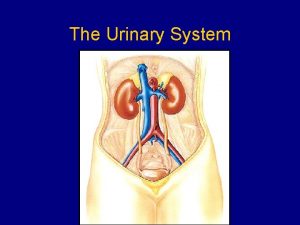
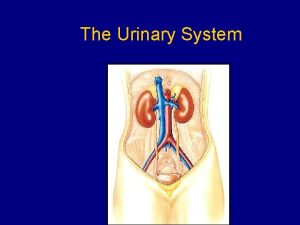
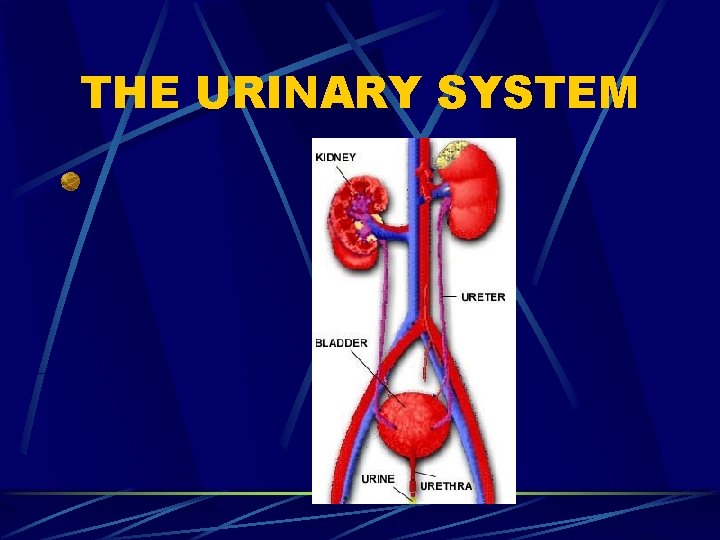
THE URINARY SYSTEM
FUNCTIONS OF THE URINARY SYSTEM 1. Excretion – removing nitrogenous wastes, certain salts, and excess water from blood 2. Maintain acid-base balance 3. Secrete waste products in the form of urine Eliminate urine from blodder
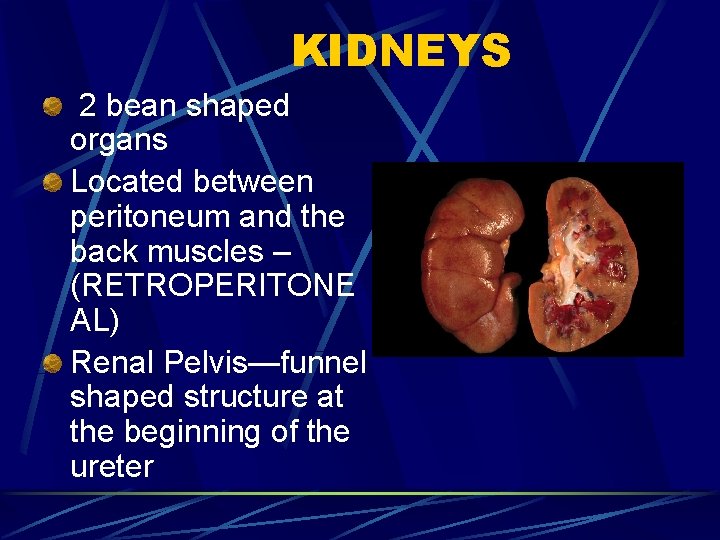
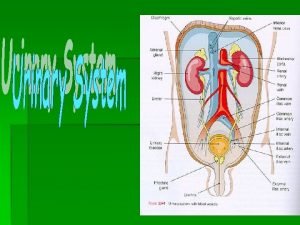
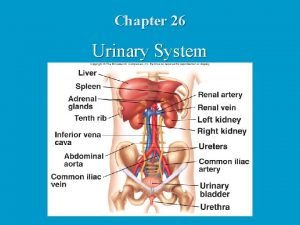
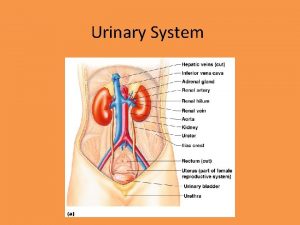
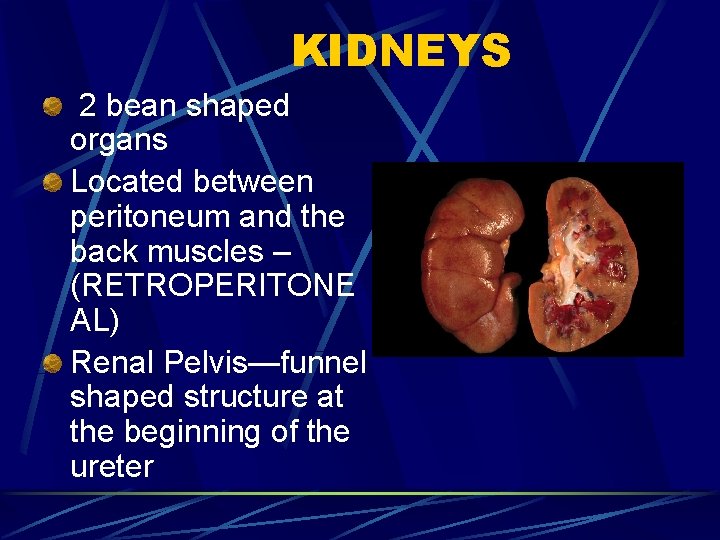
KIDNEYS 2 bean shaped organs Located between peritoneum and the back muscles – (RETROPERITONE AL) Renal Pelvis—funnel shaped structure at the beginning of the ureter
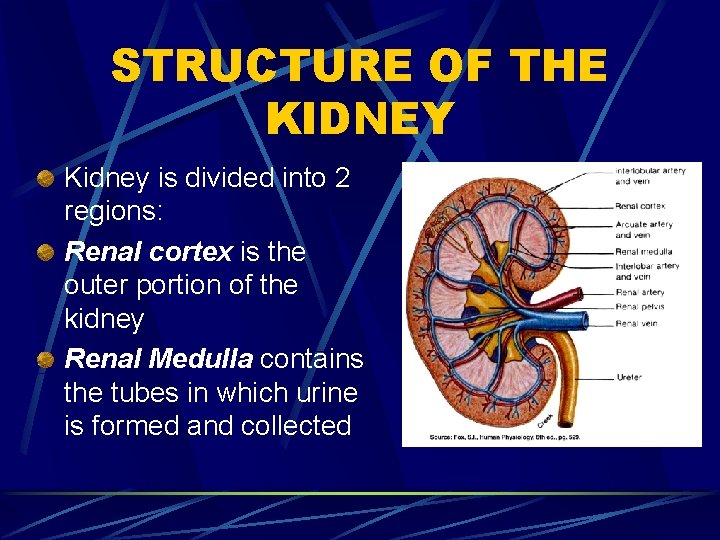
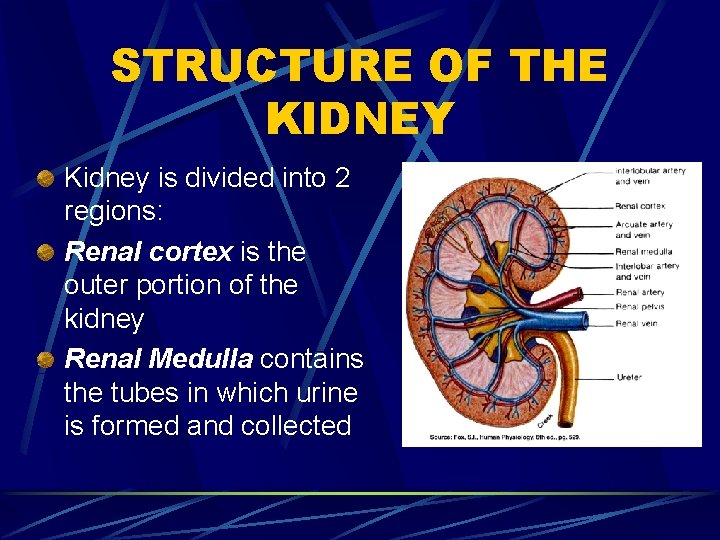
STRUCTURE OF THE KIDNEY Kidney is divided into 2 regions: Renal cortex is the outer portion of the kidney Renal Medulla contains the tubes in which urine is formed and collected
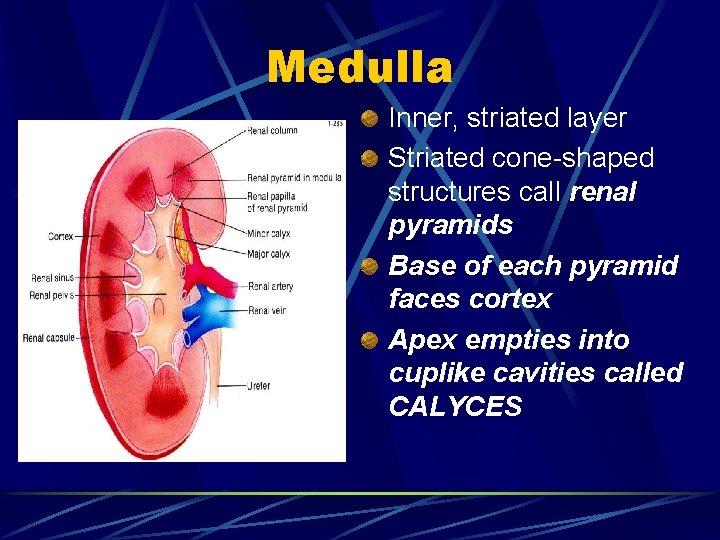
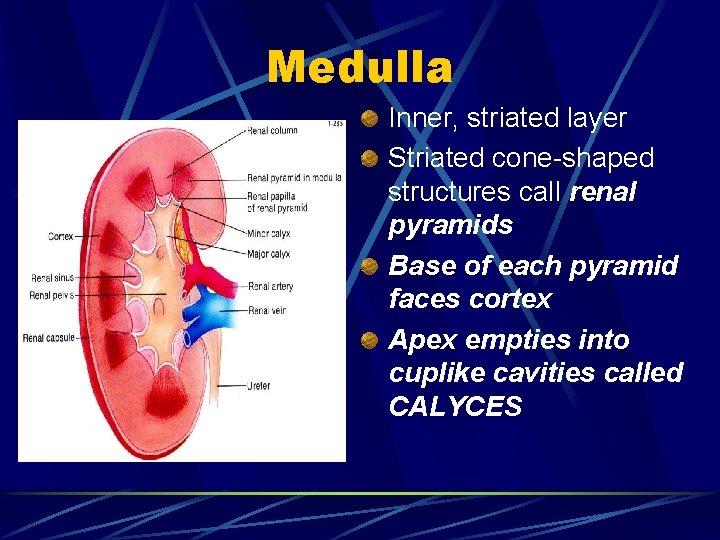
Medulla Inner, striated layer Striated cone-shaped structures call renal pyramids Base of each pyramid faces cortex Apex empties into cuplike cavities called CALYCES
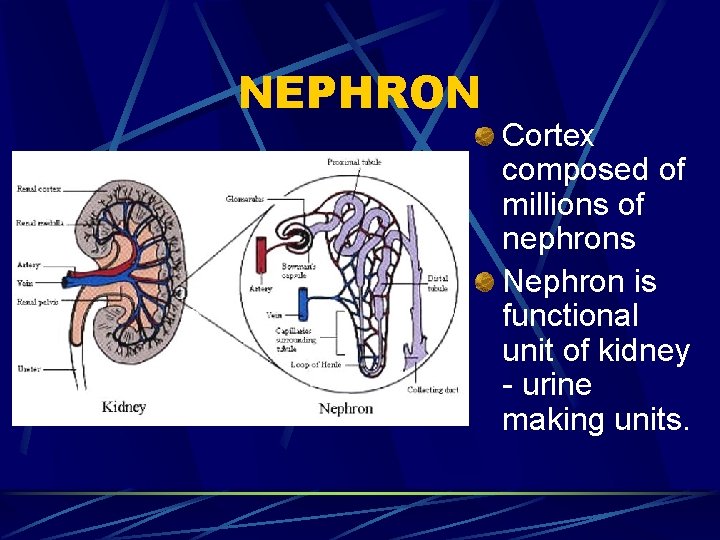
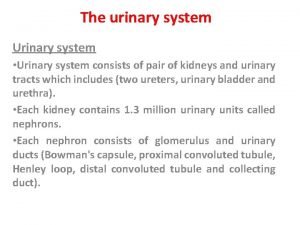
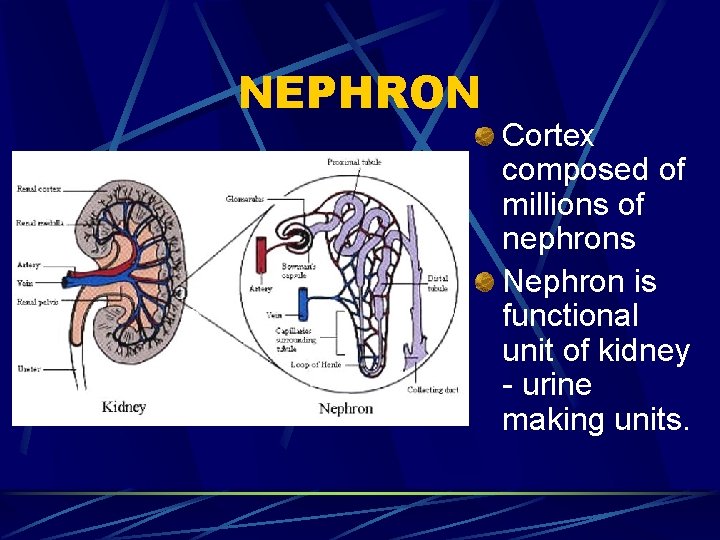
NEPHRON Cortex composed of millions of nephrons Nephron is functional unit of kidney - urine making units.
Parts of a Nephron Bowman’s Capsule Glomerulus Proximal Convoluted Tubule Loop of Henle Distal convoluted tubule Collecting tubule
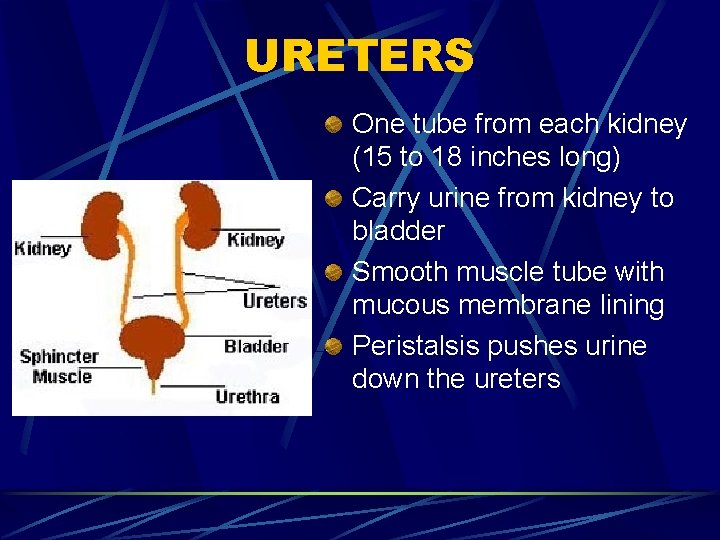
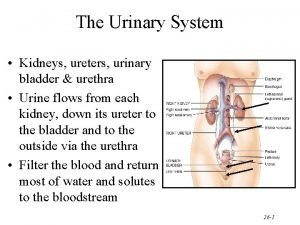
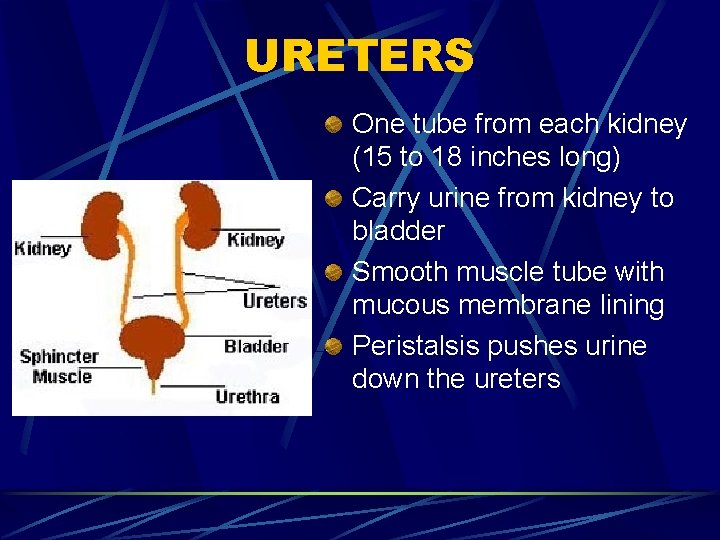
URETERS One tube from each kidney (15 to 18 inches long) Carry urine from kidney to bladder Smooth muscle tube with mucous membrane lining Peristalsis pushes urine down the ureters

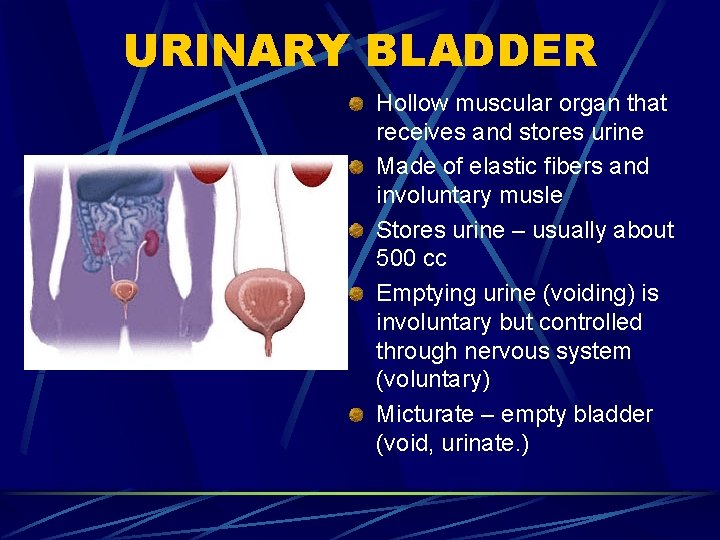
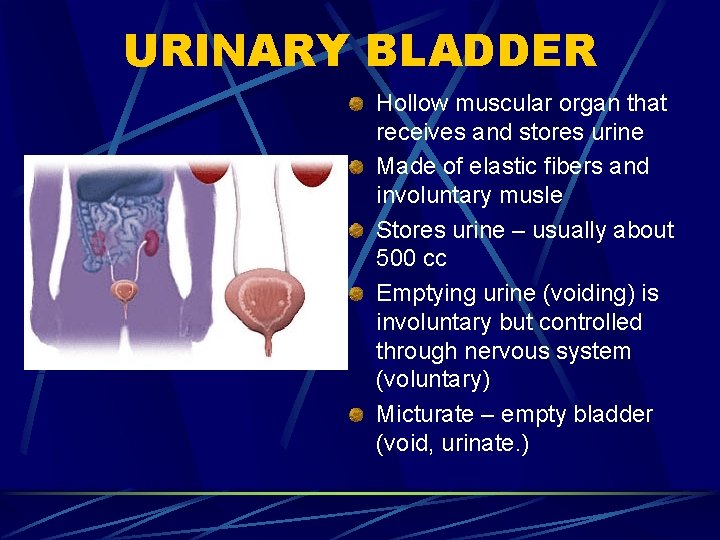
URINARY BLADDER Hollow muscular organ that receives and stores urine Made of elastic fibers and involuntary musle Stores urine – usually about 500 cc Emptying urine (voiding) is involuntary but controlled through nervous system (voluntary) Micturate – empty bladder (void, urinate. )
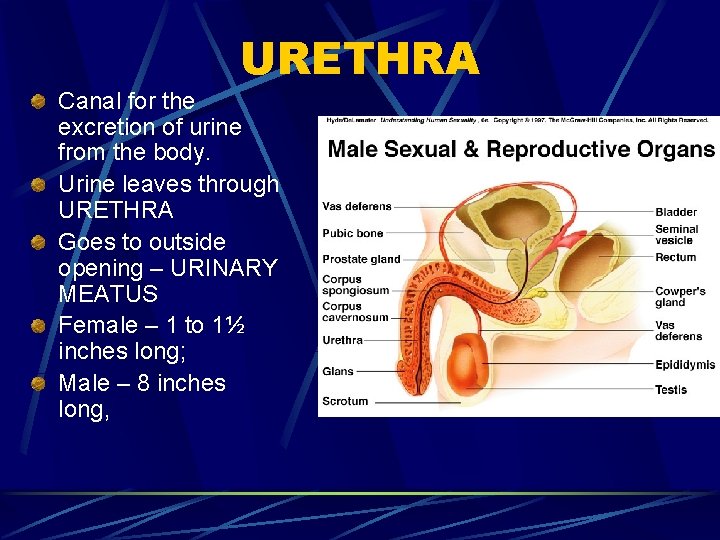
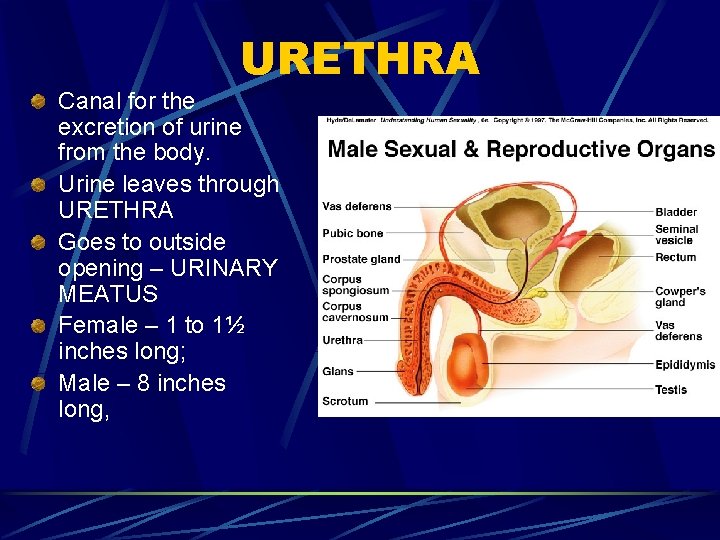
URETHRA Canal for the excretion of urine from the body. Urine leaves through URETHRA Goes to outside opening – URINARY MEATUS Female – 1 to 1½ inches long; Male – 8 inches long,
URINE FORMATION IN THE NEPRON 1 – Filtration 2 – Reabsorption 3 - Secretion
FILTRATION First step in urine formation Blood from renal artery enters glomerulus High blood pressure in glomerulus forces fluid (FILTRATE) to filter into Bowman’s capsule Filtrate does not contain plasma proteins or RBCs – they’re too big Bowman’s capsule filters out 125 cc of fluid/min – 7500 cc/hr As filtrate continues through nephron, 90% of water is reabsorbed
REABSORPTION Water and useful substances are reabsorbed If blood levels of certain substances are high (glucose, amino acids, vitamins, sodium) then those substances will not be reabsorbed
SECRETION Opposite of reabsorption – (moves substances out of the blood into the urine) Secretion transports substances from blood into collecting tubules Substances include creatinine, hydrogen ions, potassium ions, and some drugs Electrolytes are selectively secreted to maintain acid-base balance
URINARY OUTPUT Average urine output = 1500 ml/day Anuria – absence of urine Oliguria – scanty amounts of urine Polyuria – an unusually large amount of urine Nocturia – frequent urination at night
Control of Urinary Secretion Chemical Control Nervous Control
Chemical Control Reabsorption of water in distal convoluted tubule controlled by ADH (antidiuretic hormone) Secretion and regulation of ADH controlled by hypothalmus Diuretics inhibit reabsorption of water
Nervous Control Direct control through nerve impulses on kidney blood vessels Indirect control through stimulation of endocrine glands
 Lymphatic system organs and functions
Lymphatic system organs and functions Urinary system introduction
Urinary system introduction The urinary system chapter 15
The urinary system chapter 15 Pyelonephritis medical terminology
Pyelonephritis medical terminology Interesting facts about the urinary system
Interesting facts about the urinary system Allantoic stalk fetal pig
Allantoic stalk fetal pig Chapter 30 the urinary system workbook answers
Chapter 30 the urinary system workbook answers Chapter 15 the urinary system figure 15-3
Chapter 15 the urinary system figure 15-3 Chapter 20 urinary/excretory system
Chapter 20 urinary/excretory system Urinary system model
Urinary system model Urinary system model
Urinary system model Optic lobes
Optic lobes Urinary system powerpoint
Urinary system powerpoint Proximal convoluted tubule histology
Proximal convoluted tubule histology Functions of adh
Functions of adh Ureter diameter
Ureter diameter Normal constituents of urine
Normal constituents of urine Spill of dye
Spill of dye Defination of urine
Defination of urine Urinary system label
Urinary system label