The Treatment of Epilepsy A ModernDay Approach Jeffrey


- Slides: 50
The Treatment of Epilepsy: A Modern-Day Approach Jeffrey M. Politsky, MD, FRCP(C) NORHEAST REGIONAL EPILEPSY GROUP
Objectives • Develop a basic understanding of the approach to treatment of epilepsy • Understand the different treatment approaches to the different type of epilepsies
Goals of Epilepsy Therapy • • Long-term seizure control Long-term quality-of-life benefits Safety Assured compliance No interactions with other medications No side-effects or complications There is no single treatment modality that guarantees all of these goals
Epilepsy Treatments • Pharmacologic Therapy – Antiepileptic drugs (AEDs) • Non-pharmacologic Therapy – Diet – Marijuana – Others • Surgical Therapy – Epilepsy surgery
Pharmacologic Treatment • Wide range of anti-seizure drugs to choose from • Can change medications fairly easily • Adjunctive (polypharmacy) often used • Current AEDs have been thoroughly researched • Prescribed for neonates, children, adults, & elderly
AEDs • Usually first-line treatment • Pseudo-rational approach – first choice IS relevant – Anti-seizure drugs can be tailored for type of seizure disorder & in consideration of patient • Controls seizures in two thirds of people with epilepsy – With or without side effects • 1/3 of people with epilepsy have Drug-Resistant “Intractable” Epilepsy
Pharmacologic Treatment • Factors in choosing Treatment – Diagnosis • Syndrome v. s. Localization – Cost – Patient Profile • Wishes, co-morbidity, profession, resources – Drug Profile • Mechanism of action, side effects, quantitation – FDA Approval
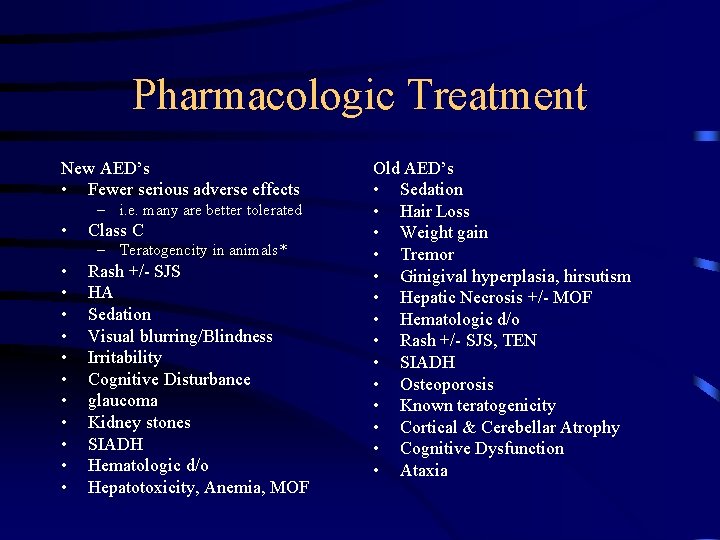
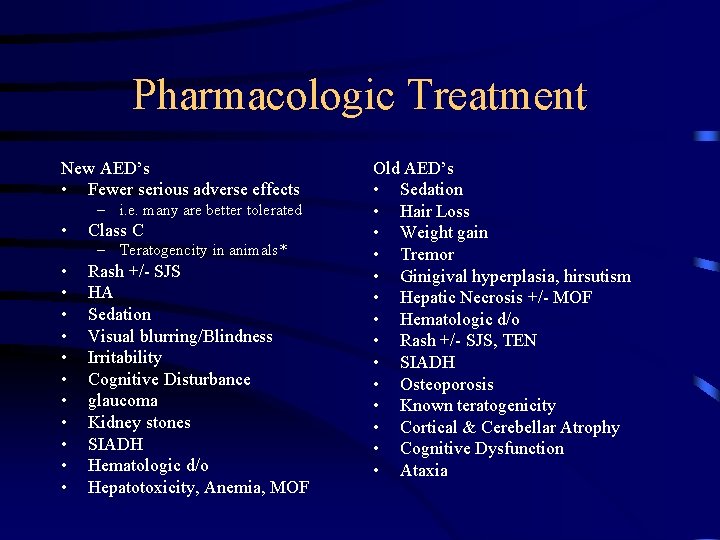
Pharmacologic Treatment New AED’s • Fewer serious adverse effects – i. e. many are better tolerated • Class C – Teratogencity in animals* • • • Rash +/- SJS HA Sedation Visual blurring/Blindness Irritability Cognitive Disturbance glaucoma Kidney stones SIADH Hematologic d/o Hepatotoxicity, Anemia, MOF Old AED’s • Sedation • Hair Loss • Weight gain • Tremor • Ginigival hyperplasia, hirsutism • Hepatic Necrosis +/- MOF • Hematologic d/o • Rash +/- SJS, TEN • SIADH • Osteoporosis • Known teratogenicity • Cortical & Cerebellar Atrophy • Cognitive Dysfunction • Ataxia
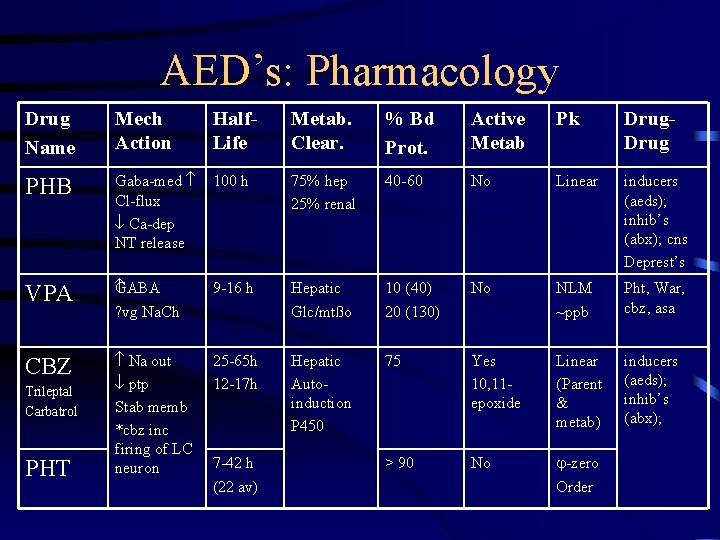
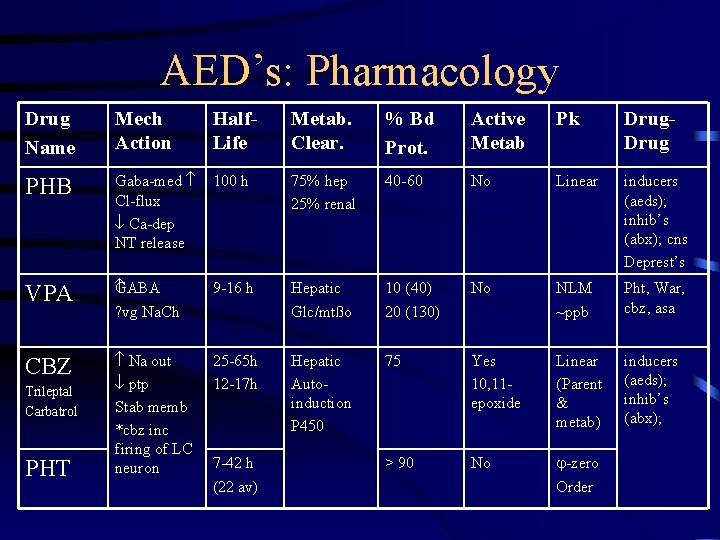
AED’s: Pharmacology Drug Name Mech Action Half. Life Metab. Clear. % Bd Prot. Active Metab Pk Drug PHB Gaba-med Cl-flux Ca-dep NT release 100 h 75% hep 25% renal 40 -60 No Linear inducers (aeds); inhib’s (abx); cns Deprest’s VPA ABA G ? vg Na. Ch 9 -16 h Hepatic Glc/mtßo 10 (40) 20 (130) No NLM ~ppb Pht, War, cbz, asa CBZ Na out ptp Stab memb *cbz inc firing of LC neuron 25 -65 h 12 -17 h Hepatic Autoinduction P 450 75 Yes 10, 11 epoxide Linear (Parent & metab) inducers (aeds); inhib’s (abx); > 90 No -zero Order Trileptal Carbatrol PHT 7 -42 h (22 av)
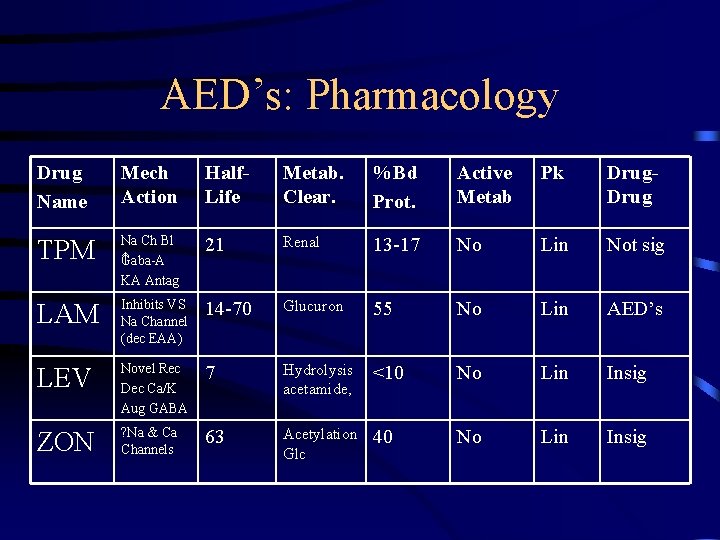
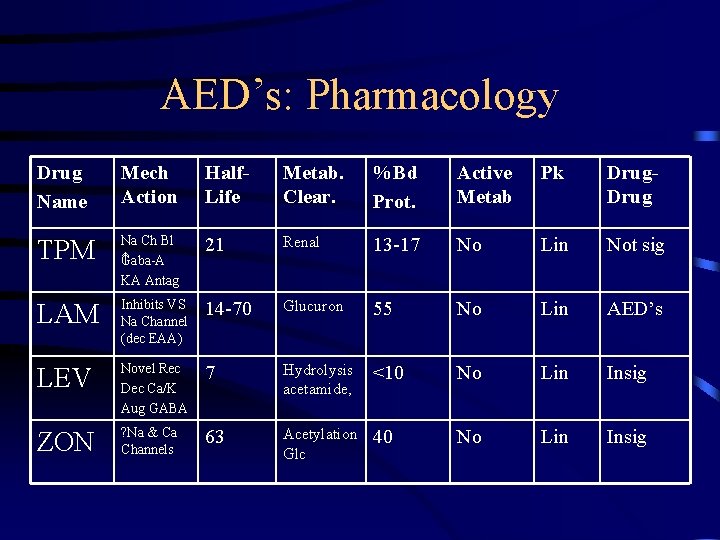
AED’s: Pharmacology Drug Name Mech Action Half. Life Metab. Clear. %Bd Prot. Active Metab Pk Drug TPM Na Ch Bl Gaba-A KA Antag 21 Renal 13 -17 No Lin Not sig LAM Inhibits VS Na Channel (dec EAA) 14 -70 Glucuron 55 No Lin AED’s LEV Novel Rec Dec Ca/K Aug GABA 7 Hydrolysis acetamide, <10 No Lin Insig ZON ? Na & Ca Channels 63 Acetylation Glc 40 No Lin Insig
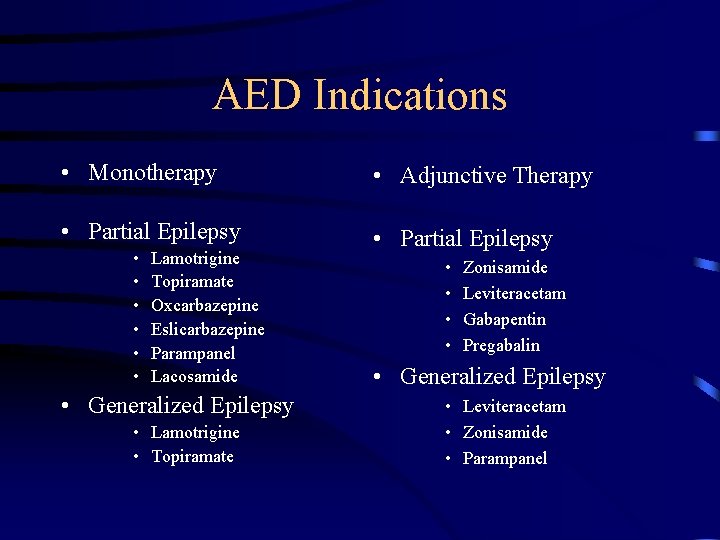
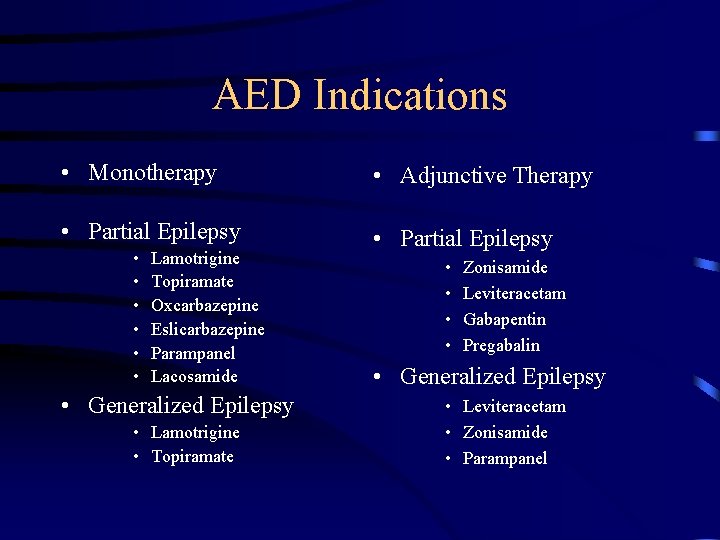
AED Indications • Monotherapy • Adjunctive Therapy • Partial Epilepsy • • • Lamotrigine Topiramate Oxcarbazepine Eslicarbazepine Parampanel Lacosamide • Generalized Epilepsy • Lamotrigine • Topiramate • • Zonisamide Leviteracetam Gabapentin Pregabalin • Generalized Epilepsy • Leviteracetam • Zonisamide • Parampanel
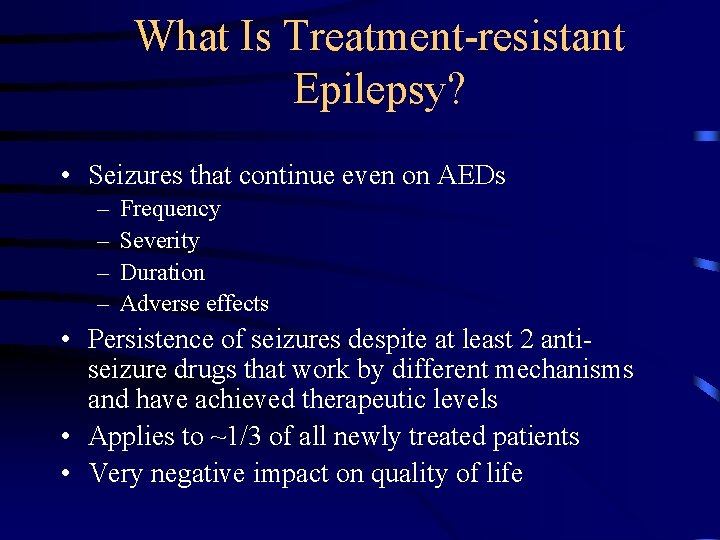
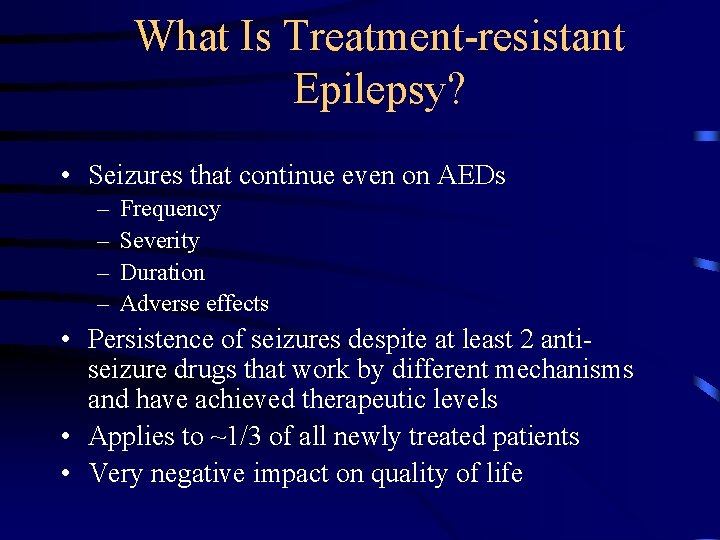
What Is Treatment-resistant Epilepsy? • Seizures that continue even on AEDs – – Frequency Severity Duration Adverse effects • Persistence of seizures despite at least 2 antiseizure drugs that work by different mechanisms and have achieved therapeutic levels • Applies to ~1/3 of all newly treated patients • Very negative impact on quality of life
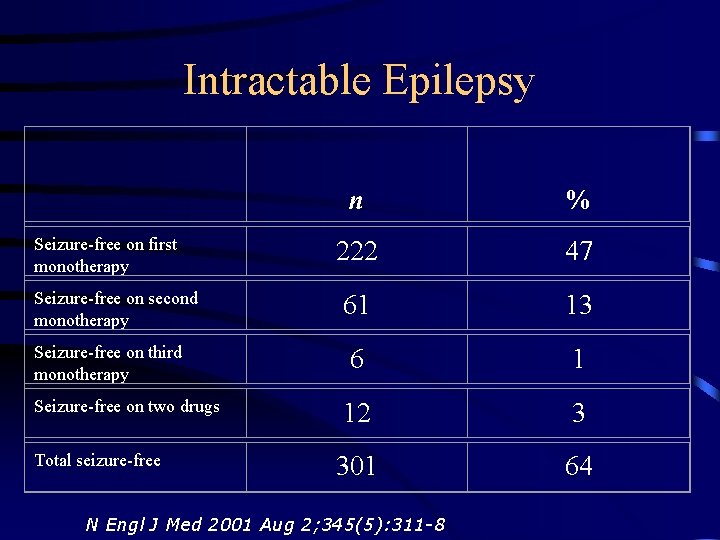
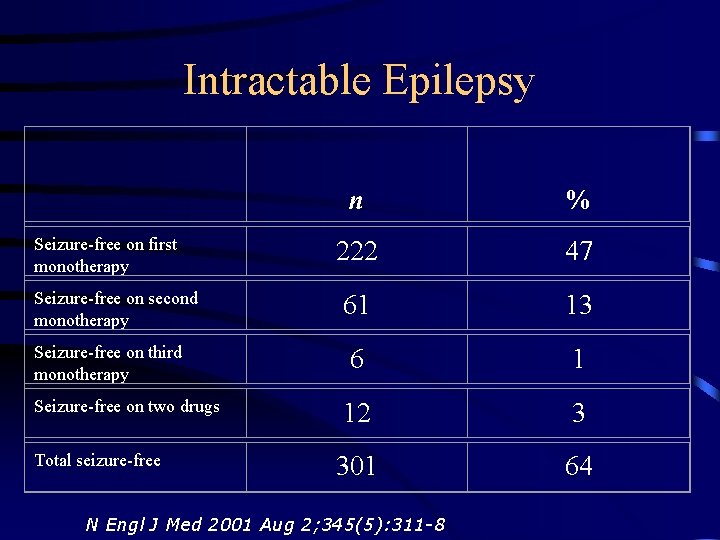
Intractable Epilepsy Seizure-free on first monotherapy Seizure-free on second monotherapy Seizure-free on third monotherapy Seizure-free on two drugs Total seizure-free n % 222 47 61 13 6 1 12 3 301 64 N Engl J Med 2001 Aug 2; 345(5): 311 -8
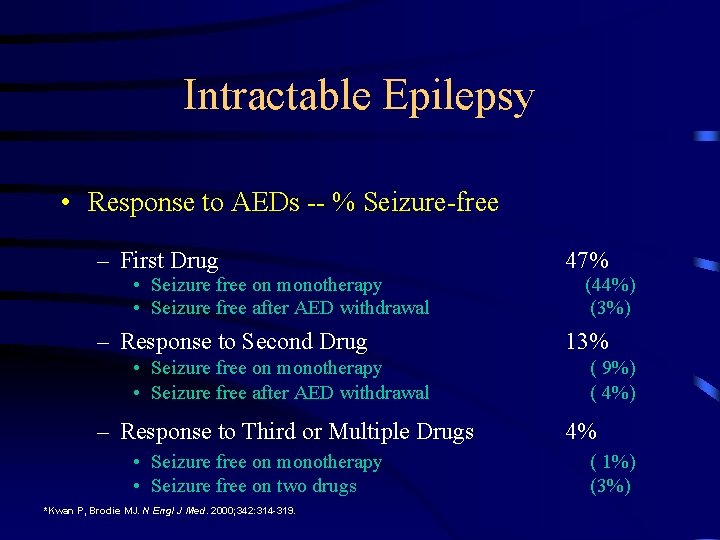
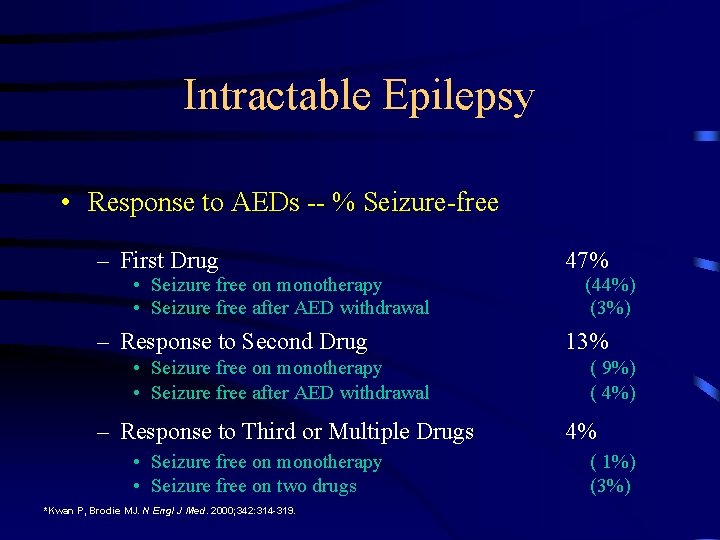
Intractable Epilepsy • Response to AEDs -- % Seizure-free – First Drug 47% – Response to Second Drug 13% • Seizure free on monotherapy • Seizure free after AED withdrawal – Response to Third or Multiple Drugs • Seizure free on monotherapy • Seizure free on two drugs *Kwan P, Brodie MJ. N Engl J Med. 2000; 342: 314 -319. (44%) (3%) ( 9%) ( 4%) 4% ( 1%) (3%)
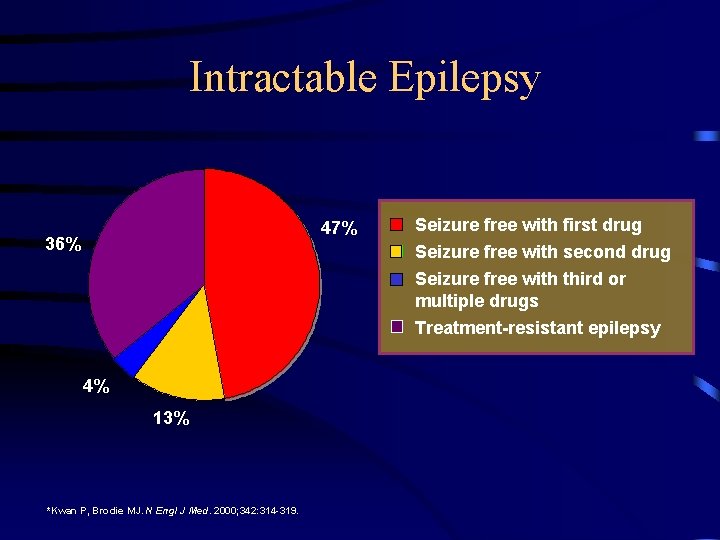
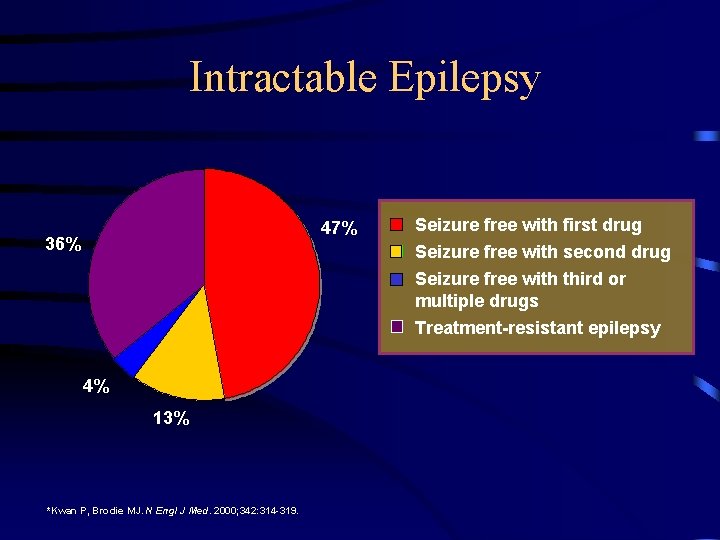
Intractable Epilepsy 47% 36% Seizure free with first drug Seizure free with second drug Seizure free with third or multiple drugs Treatment-resistant epilepsy 4% 13% *Kwan P, Brodie MJ. N Engl J Med. 2000; 342: 314 -319.
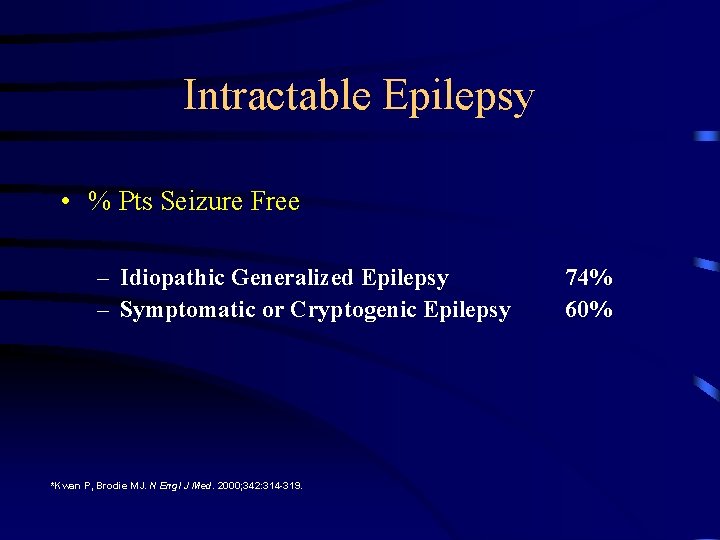
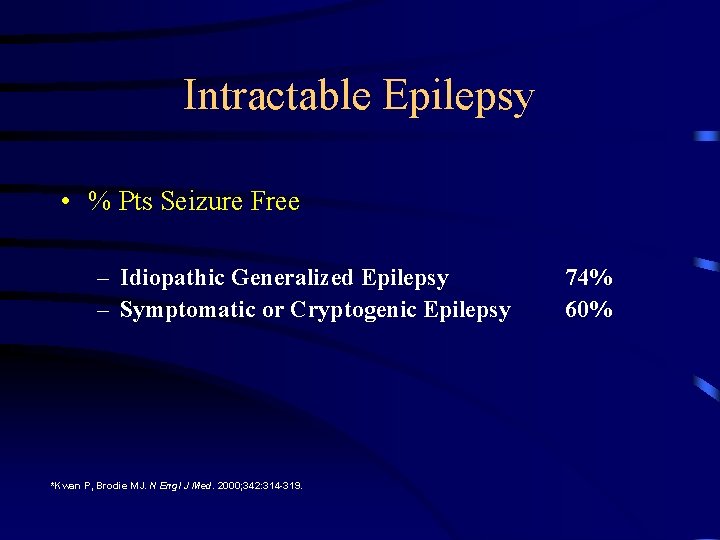
Intractable Epilepsy • % Pts Seizure Free – Idiopathic Generalized Epilepsy – Symptomatic or Cryptogenic Epilepsy *Kwan P, Brodie MJ. N Engl J Med. 2000; 342: 314 -319. 74% 60%
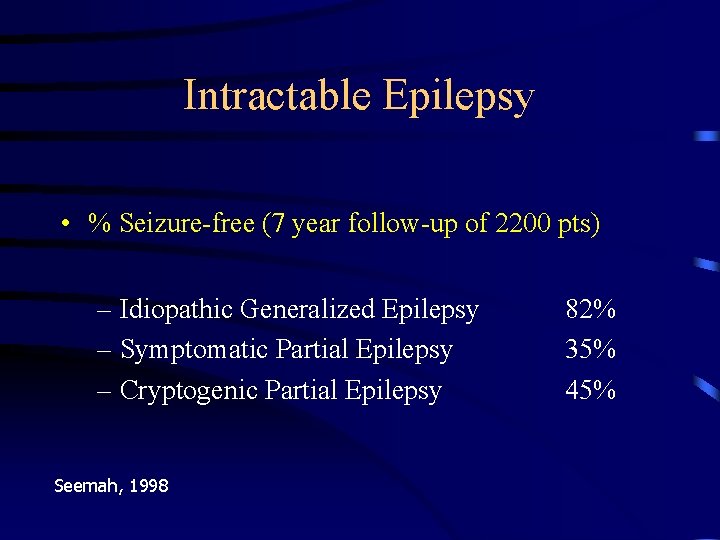
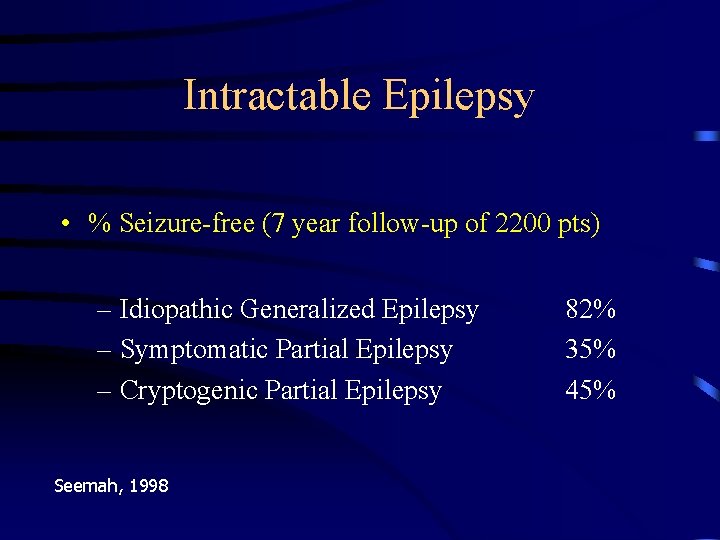
Intractable Epilepsy • % Seizure-free (7 year follow-up of 2200 pts) – Idiopathic Generalized Epilepsy – Symptomatic Partial Epilepsy – Cryptogenic Partial Epilepsy Seemah, 1998 82% 35% 45%
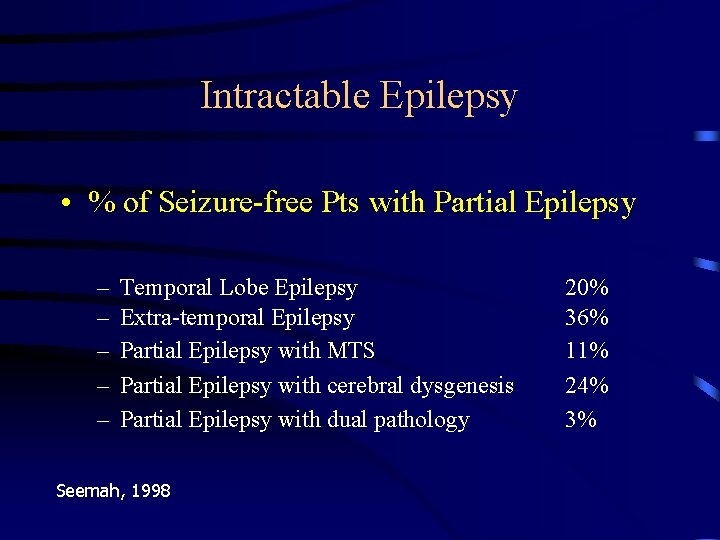
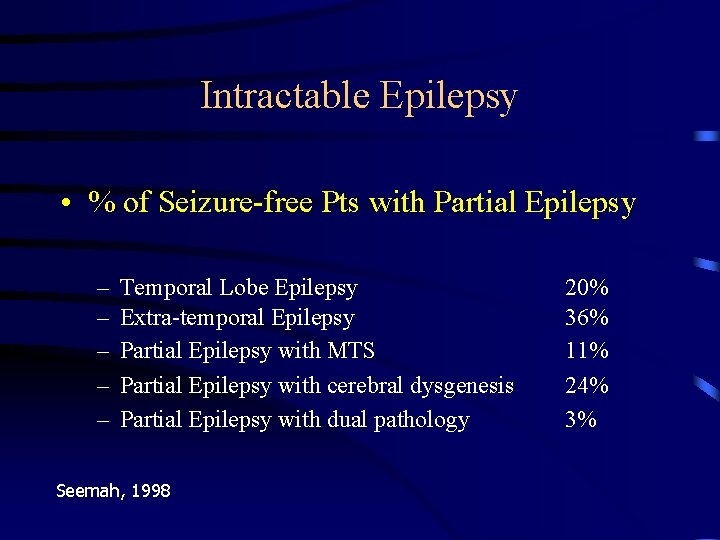
Intractable Epilepsy • % of Seizure-free Pts with Partial Epilepsy – – – Temporal Lobe Epilepsy Extra-temporal Epilepsy Partial Epilepsy with MTS Partial Epilepsy with cerebral dysgenesis Partial Epilepsy with dual pathology Seemah, 1998 20% 36% 11% 24% 3%
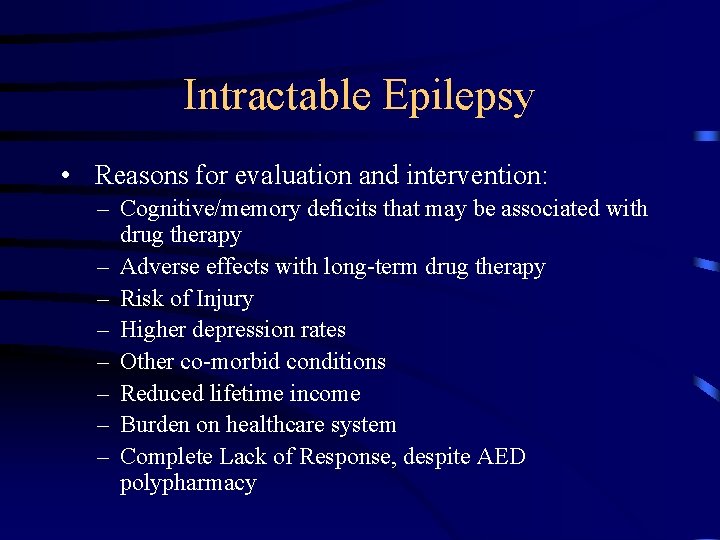
Intractable Epilepsy • Reasons for evaluation and intervention: – Cognitive/memory deficits that may be associated with drug therapy – Adverse effects with long-term drug therapy – Risk of Injury – Higher depression rates – Other co-morbid conditions – Reduced lifetime income – Burden on healthcare system – Complete Lack of Response, despite AED polypharmacy
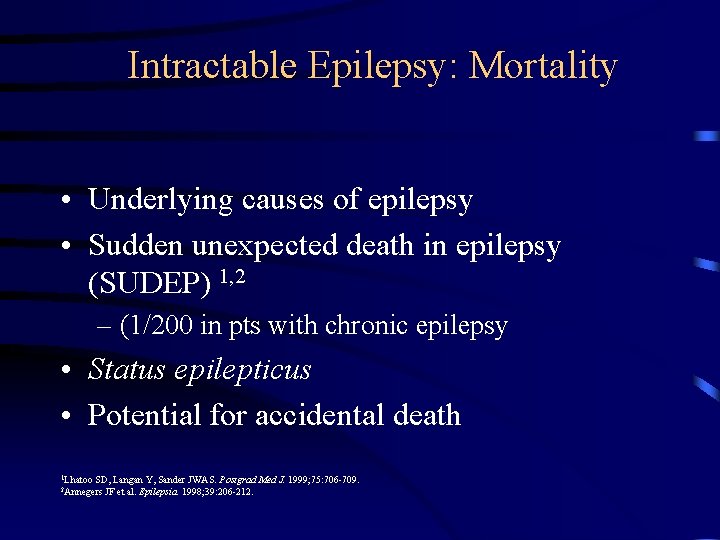
Intractable Epilepsy: Mortality • Underlying causes of epilepsy • Sudden unexpected death in epilepsy (SUDEP) 1, 2 – (1/200 in pts with chronic epilepsy • Status epilepticus • Potential for accidental death 1 Lhatoo SD, Langan Y, Sander JWAS. Postgrad Med J. 1999; 75: 706 -709. JF et al. Epilepsia. 1998; 39: 206 -212. 2 Annegers
Alternative Therapeutic Options • Should be considered early – After 2 to 3 drug “failures” – When there are severe side effects • Early identification of patient enhances seizure control and quality of life • Other options include – Ketogenic Diet – Epilepsy Surgery

Epilepsy Treatments • Pharmacologic Therapy – Antiepileptic drugs (AEDs) • Non-pharmacologic Therapy – Diet – THC – Others • Surgical Therapy – Epilepsy surgery
Ketogenic Diet • Most effective in children – Not typically used in adults • High ratio of fat to protein/carbohydrate • Appears to be effective for most seizure types – More than half of patients experience 50% seizure reduction at 6 months – One out of ten have seizure freedom at 1 year – A 47% continuation rate at 1 year Vining EP et al. Arch Neurol. 1998; 55: 1433 -1437.
Ketogenic Diet • Possible Adverse Effects – – – – Constipation & vomiting Lethargy Kidney stones Excess acid accumulation Severe dehydration Behavioral changes Increased risk of infections • Other Disadvantages – Initiation of diet usually requires hospitalization – Food must be carefully weighted and measured – Poor compliance rate

Epilepsy Treatments • Pharmacologic Therapy – Antiepileptic drugs (AEDs) • Non-pharmacologic Therapy – Ketogenic diet • Surgical Therapy – Epilepsy surgery
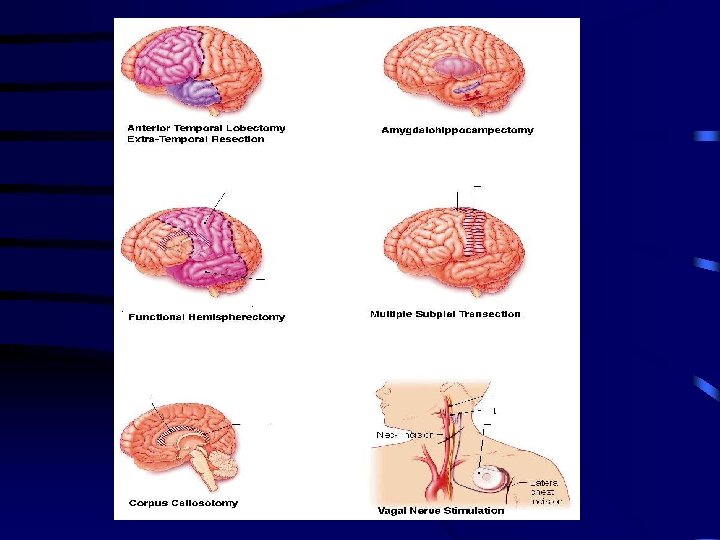
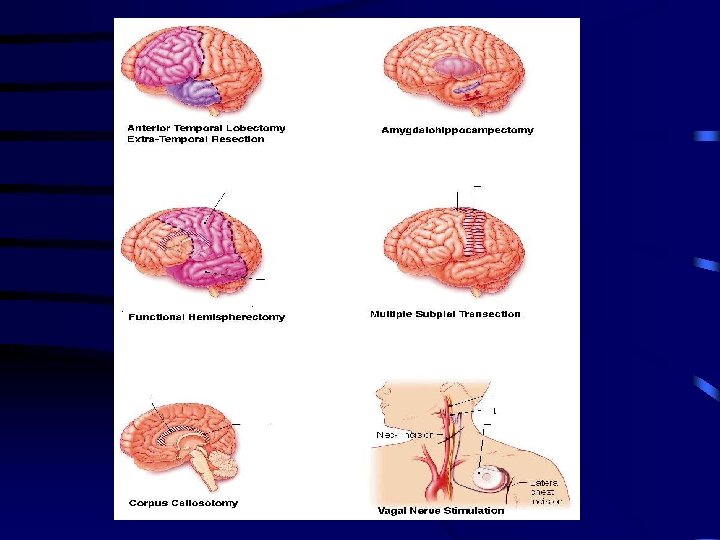
Epilepsy Surgery • Minimally Invasive Surgery – Vagus Nerve Stimulation (VNS Therapy. TM) • Moderately Invasive Surgery – Investigational Devices: Neuropace Responsive Neurostimulator (RNSTM); Medtronic Deep Brain Stimulator (DBSTM) • Maximally Invasive Surgery – Cortical Resection – Hemispherectomy/Hemispherotomy – Corpus Callosotomy
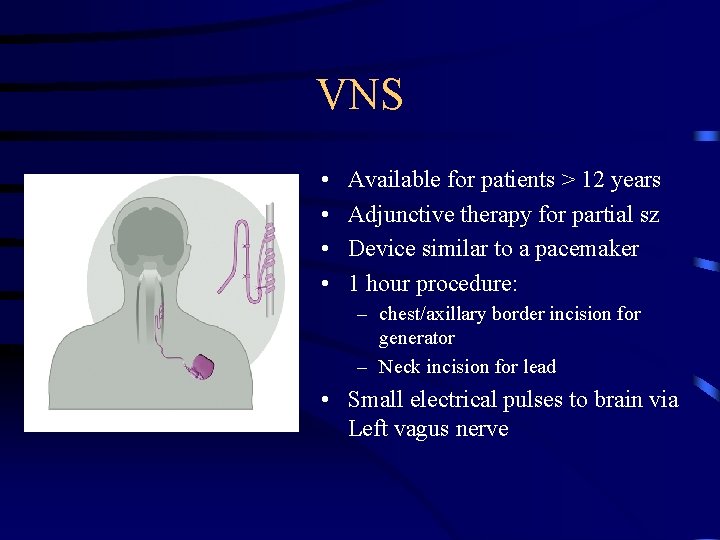
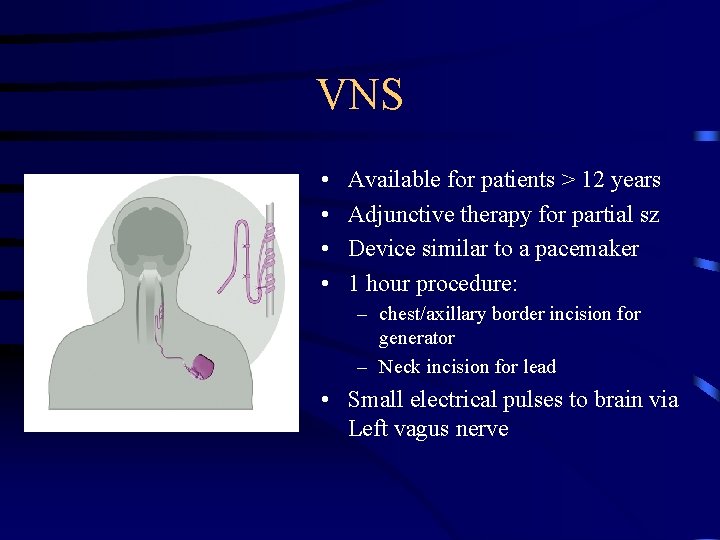
VNS • • Available for patients > 12 years Adjunctive therapy for partial sz Device similar to a pacemaker 1 hour procedure: – chest/axillary border incision for generator – Neck incision for lead • Small electrical pulses to brain via Left vagus nerve
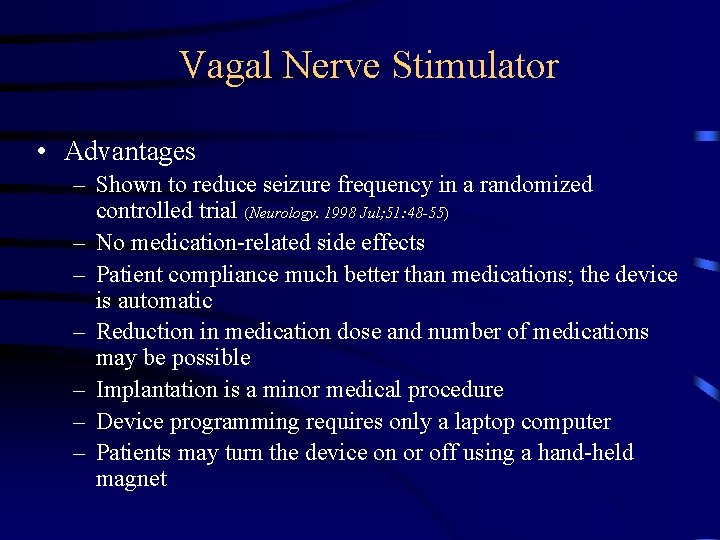
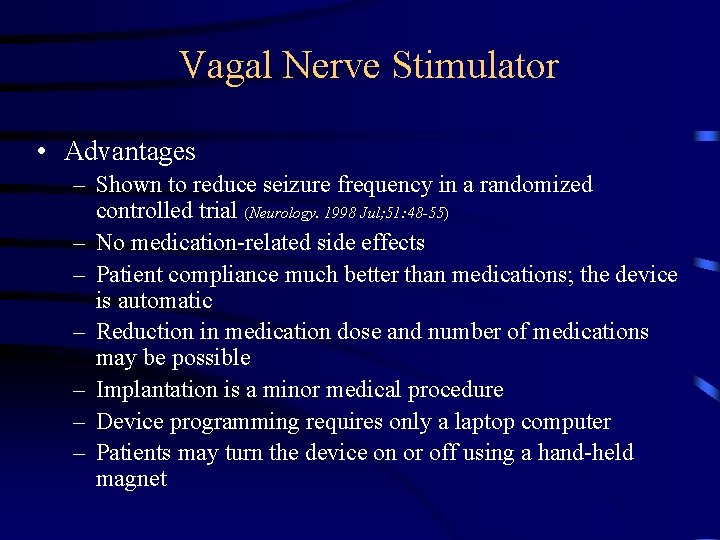
Vagal Nerve Stimulator • Advantages – Shown to reduce seizure frequency in a randomized controlled trial (Neurology. 1998 Jul; 51: 48 -55) – No medication-related side effects – Patient compliance much better than medications; the device is automatic – Reduction in medication dose and number of medications may be possible – Implantation is a minor medical procedure – Device programming requires only a laptop computer – Patients may turn the device on or off using a hand-held magnet
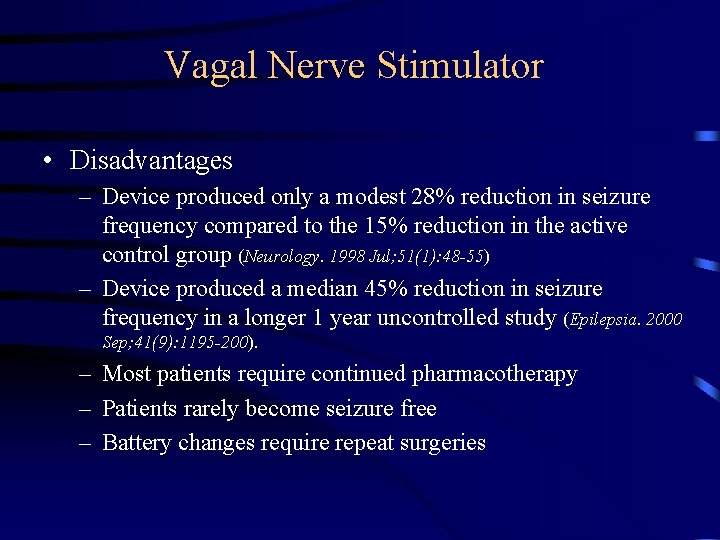
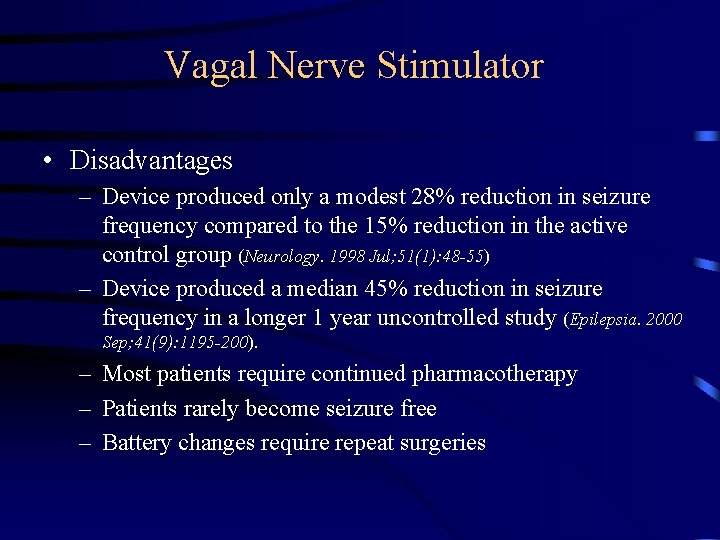
Vagal Nerve Stimulator • Disadvantages – Device produced only a modest 28% reduction in seizure frequency compared to the 15% reduction in the active control group (Neurology. 1998 Jul; 51(1): 48 -55) – Device produced a median 45% reduction in seizure frequency in a longer 1 year uncontrolled study (Epilepsia. 2000 Sep; 41(9): 1195 -200). – Most patients require continued pharmacotherapy – Patients rarely become seizure free – Battery changes require repeat surgeries
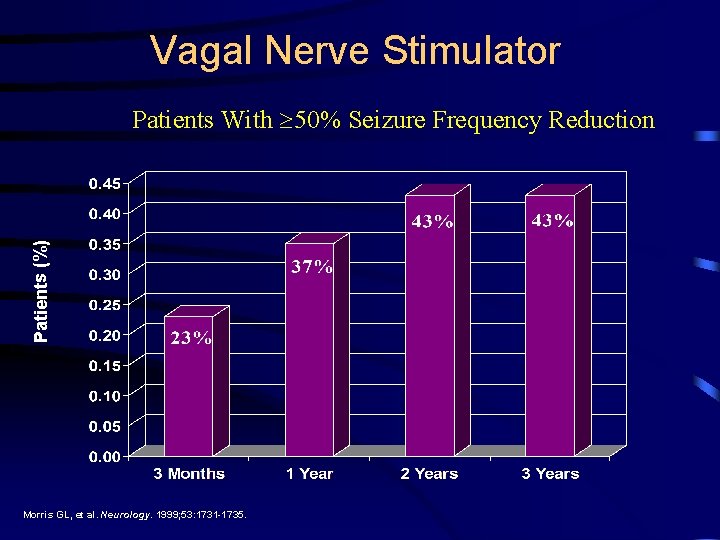
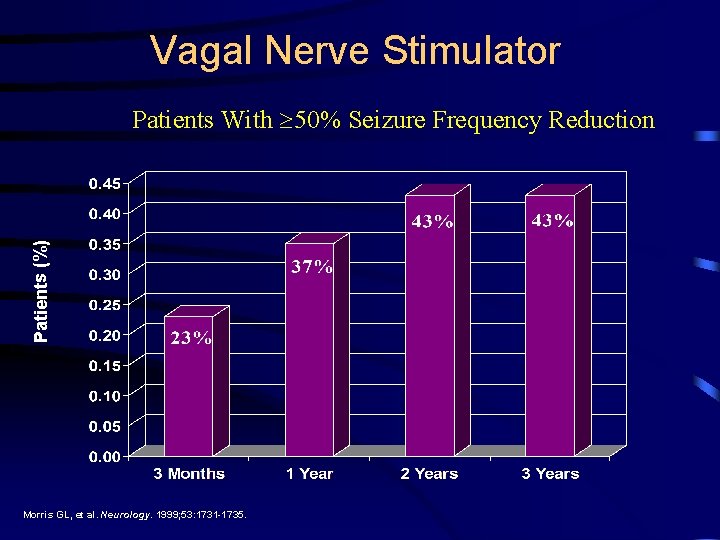
Vagal Nerve Stimulator Patients (%) Patients With 50% Seizure Frequency Reduction Morris GL, et al. Neurology. 1999; 53: 1731 -1735.
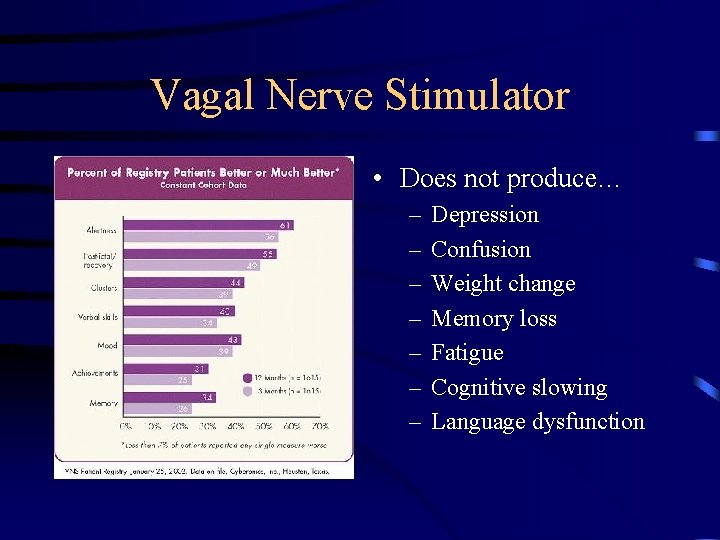
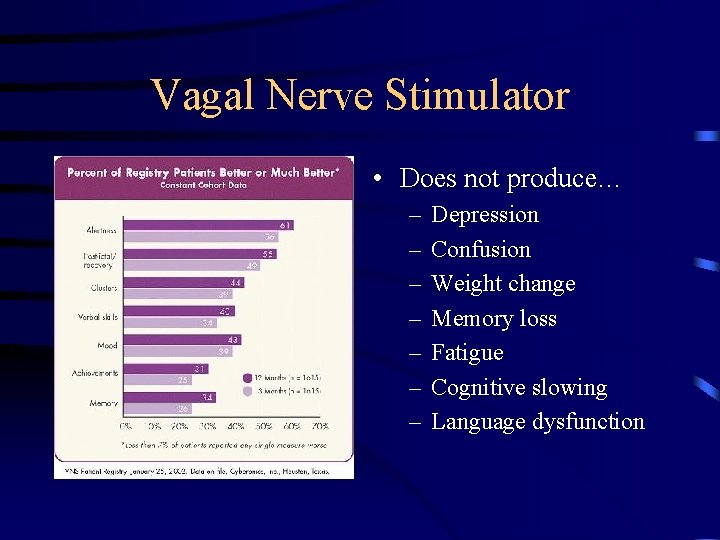
Vagal Nerve Stimulator • Does not produce… – – – – Depression Confusion Weight change Memory loss Fatigue Cognitive slowing Language dysfunction
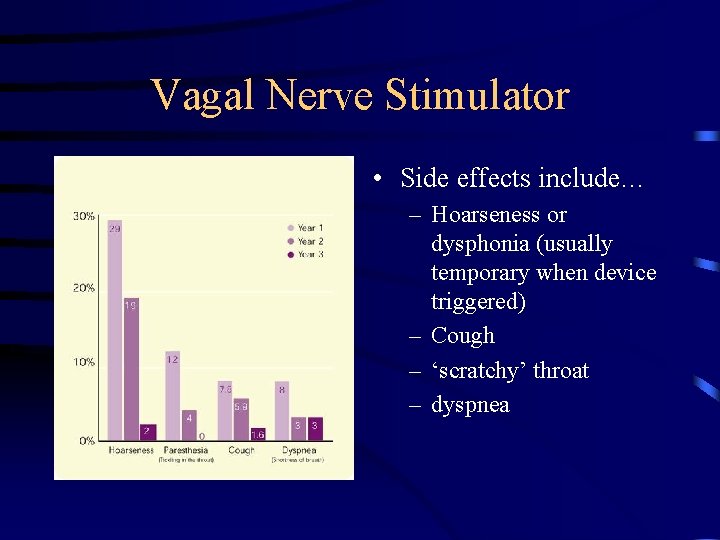
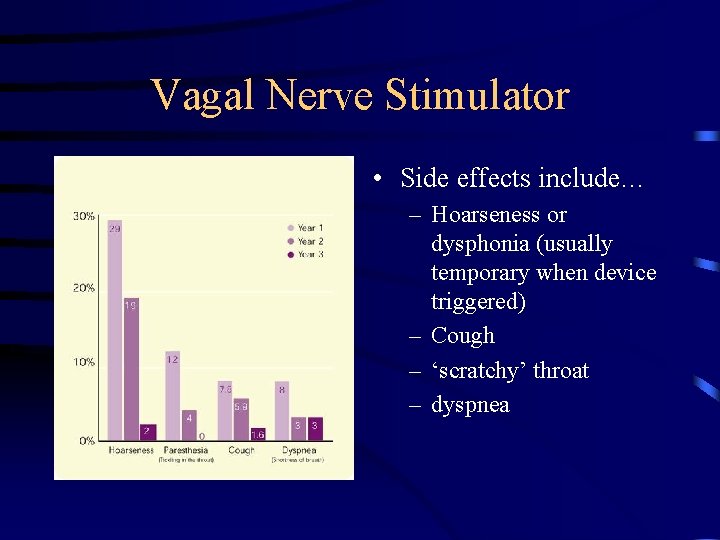
Vagal Nerve Stimulator • Side effects include… – Hoarseness or dysphonia (usually temporary when device triggered) – Cough – ‘scratchy’ throat – dyspnea
Epilepsy Surgery • Minimally Invasive Surgery – Vagus Nerve Stimulation Therapy (VNS Therapy. TM) • Moderately Invasive Surgery – Investigational Devices: Neuropace Responsive Neurostimulator (RNSTM); Medtronic Deep Brain Stimulator (DBSTM) • Maximally Invasive Surgery – Cortical Resection – Corpus Callosotomy – Hemispherotomy
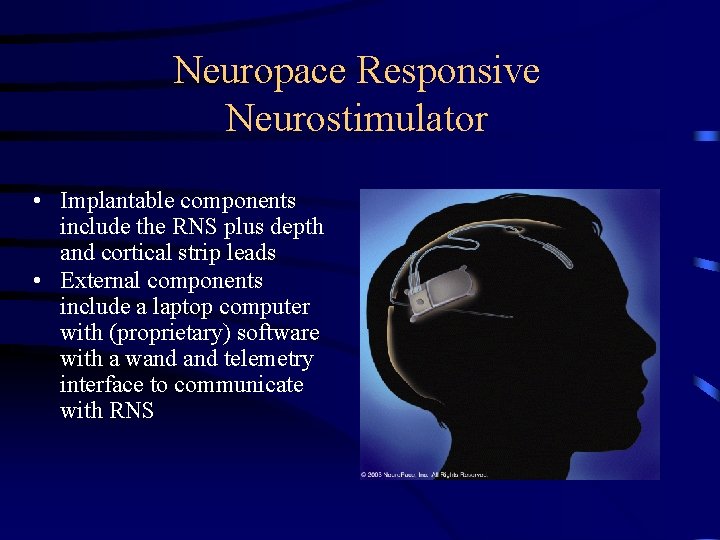
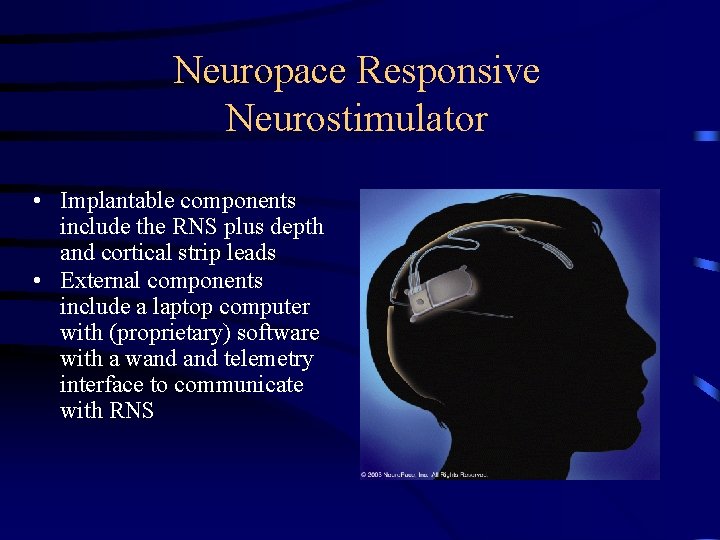
Neuropace Responsive Neurostimulator • Implantable components include the RNS plus depth and cortical strip leads • External components include a laptop computer with (proprietary) software with a wand telemetry interface to communicate with RNS
Epilepsy Surgery • Minimally Invasive Surgery – Vagus Nerve Stimulation Therapy (VNS Therapy. TM) • Moderately Invasive Surgery – Investigational Devices: Neuropace Responsive Neurostimulator (RNSTM); Medtronic Deep Brain Stimulator (DBSTM) • Maximally Invasive Surgery – Cortical Resection – Corpus Callosotomy – Hemispherotomy
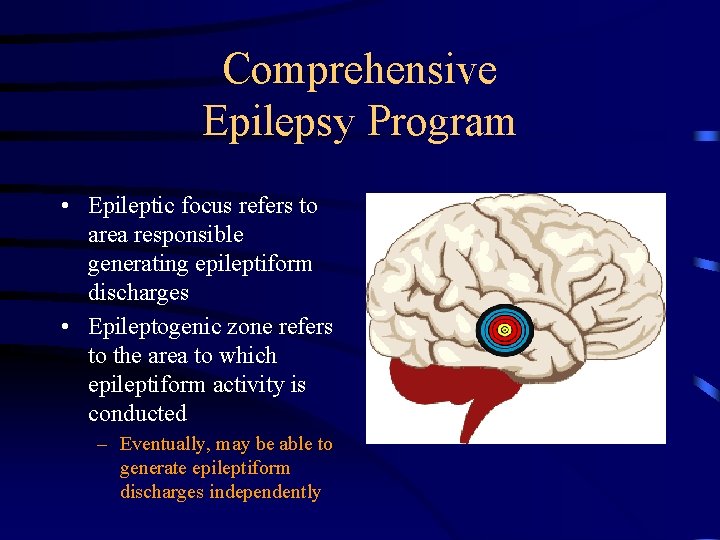
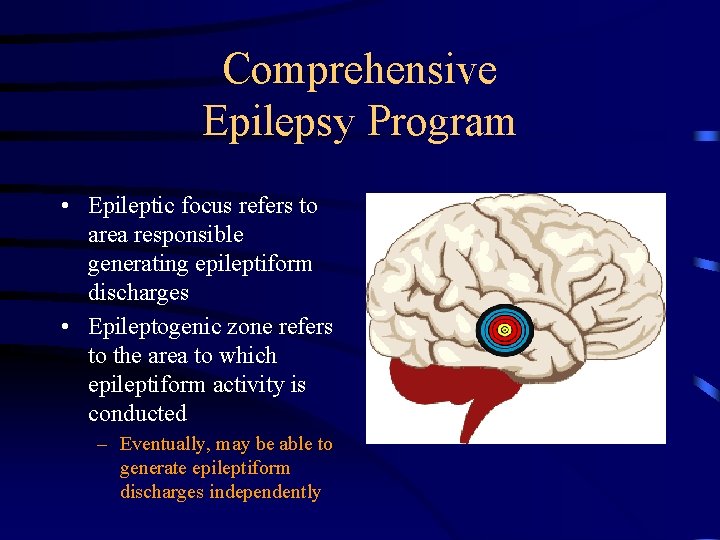
Comprehensive Epilepsy Program • Epileptic focus refers to area responsible generating epileptiform discharges • Epileptogenic zone refers to the area to which epileptiform activity is conducted – Eventually, may be able to generate epileptiform discharges independently
Comprehensive Epilepsy Program • Epilepsy Surgery • Approximately 1/3 to ½ of intractable epilepsy surgery patients are good surgical candidates • Various pathologic circumstances can result in seizures: – – – – brain tumors vascular malformation Hemorrhages Strokes Abscesses Trauma (bullet and missile-type wounds, blunt trauma) Scarring/Gliosis (mesial temporal sclerosis, previous stroke or surgery or hemorrhage, for e. g) – Abnormally formed brain tissue (cerebral dysgenesis)
Epilepsy Surgery Procedures • • Anterior Temporal Resections Extra. Temporal Resections Callosotomies Hemispherectomies Vagal Nerve Stimulation Depth Electrodes Subdural Electrodes
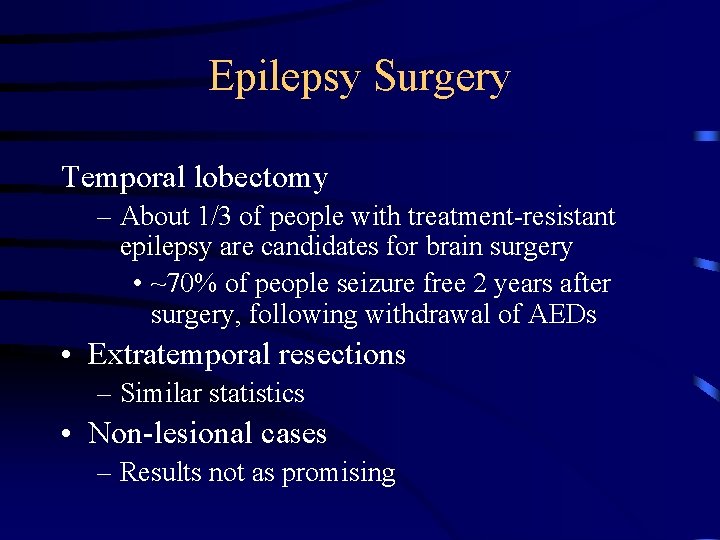
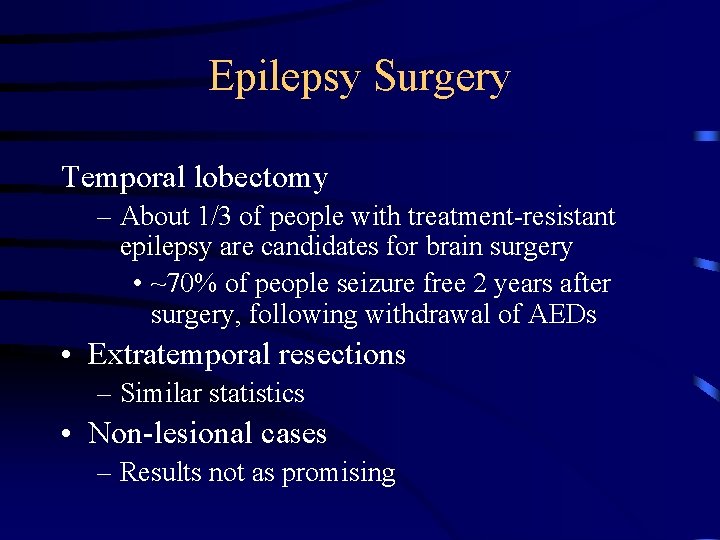
Epilepsy Surgery Temporal lobectomy – About 1/3 of people with treatment-resistant epilepsy are candidates for brain surgery • ~70% of people seizure free 2 years after surgery, following withdrawal of AEDs • Extratemporal resections – Similar statistics • Non-lesional cases – Results not as promising
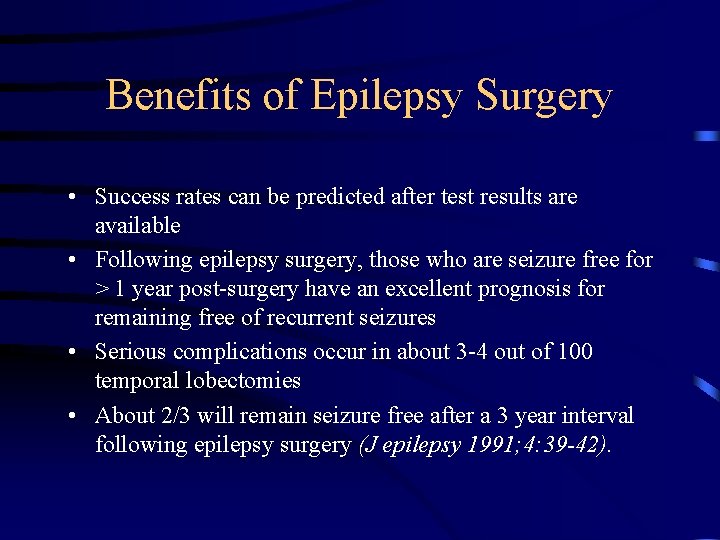
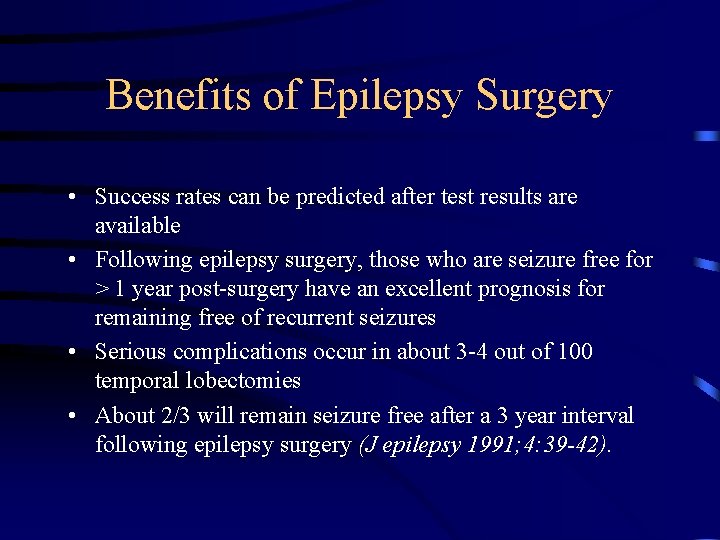
Benefits of Epilepsy Surgery • Success rates can be predicted after test results are available • Following epilepsy surgery, those who are seizure free for > 1 year post-surgery have an excellent prognosis for remaining free of recurrent seizures • Serious complications occur in about 3 -4 out of 100 temporal lobectomies • About 2/3 will remain seizure free after a 3 year interval following epilepsy surgery (J epilepsy 1991; 4: 39 -42).
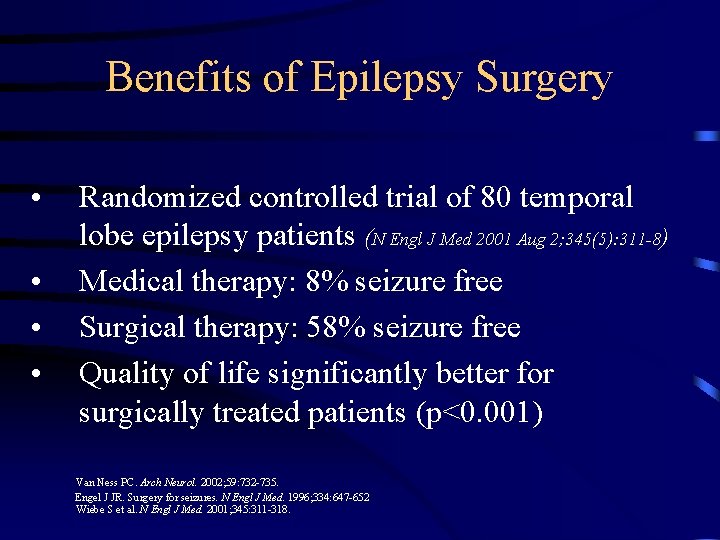
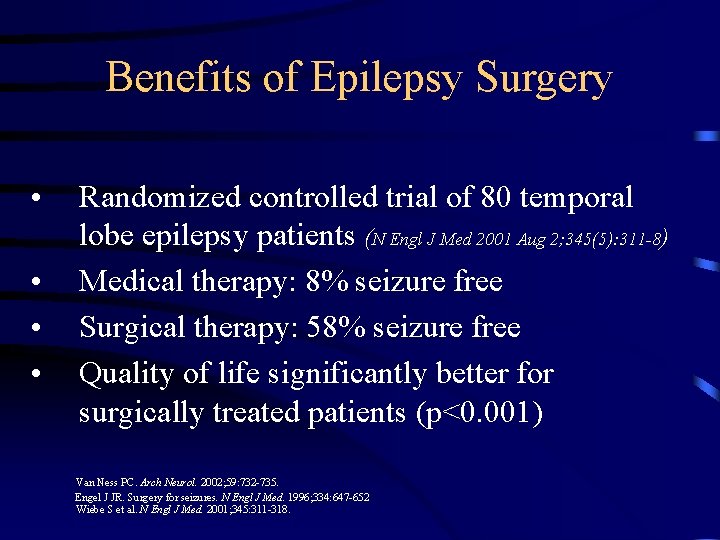
Benefits of Epilepsy Surgery • • Randomized controlled trial of 80 temporal lobe epilepsy patients (N Engl J Med 2001 Aug 2; 345(5): 311 -8) Medical therapy: 8% seizure free Surgical therapy: 58% seizure free Quality of life significantly better for surgically treated patients (p<0. 001) Van Ness PC. Arch Neurol. 2002; 59: 732 -735. Engel J JR. Surgery for seizures. N Engl J Med. 1996; 334: 647 -652 Wiebe S et al. N Engl J Med. 2001; 345: 311 -318.
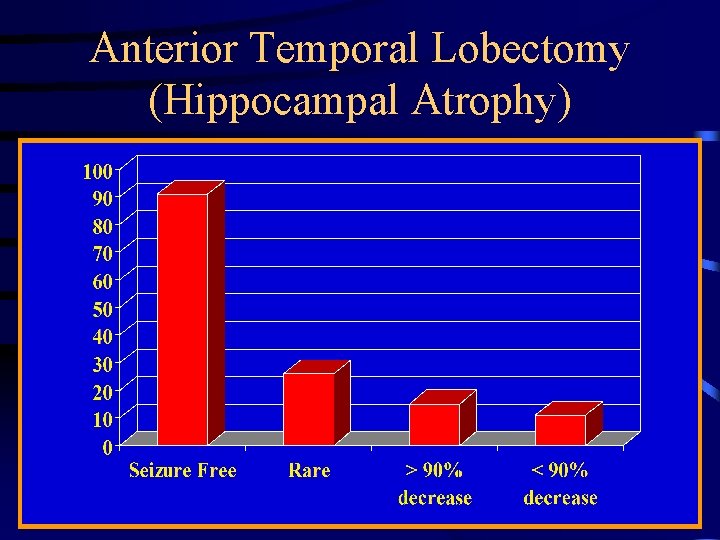
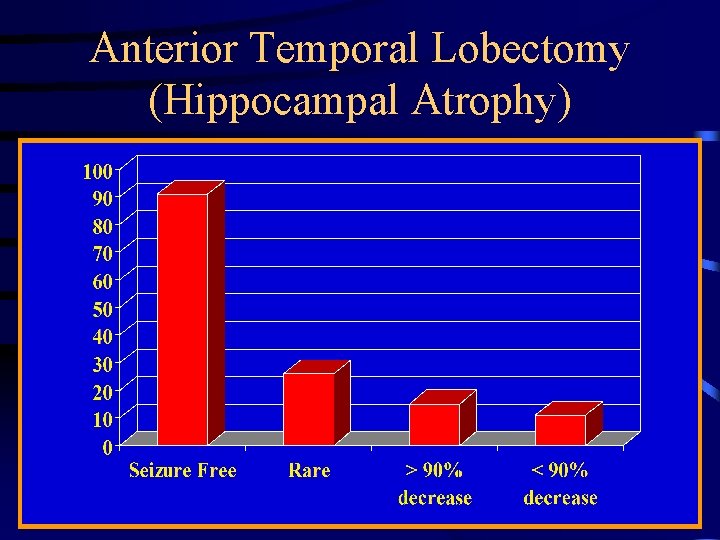
Anterior Temporal Lobectomy (Hippocampal Atrophy)
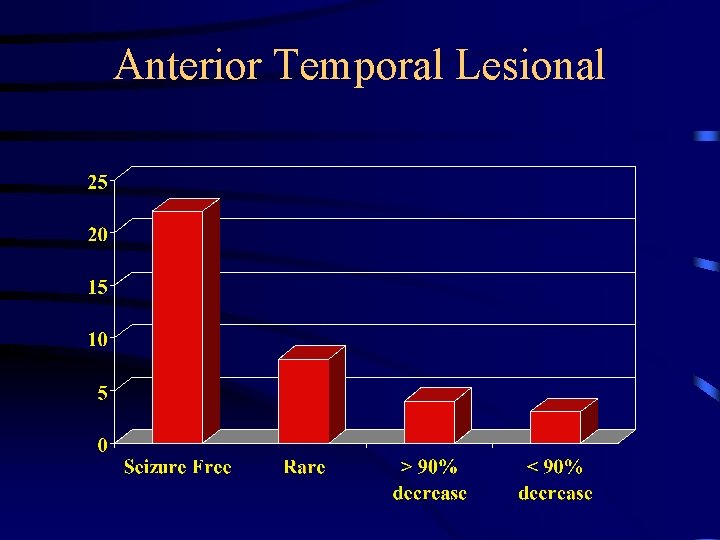
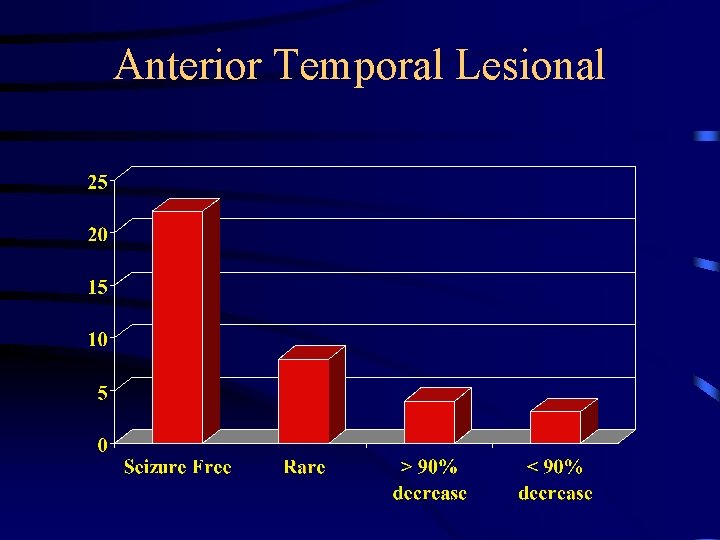
Anterior Temporal Lesional
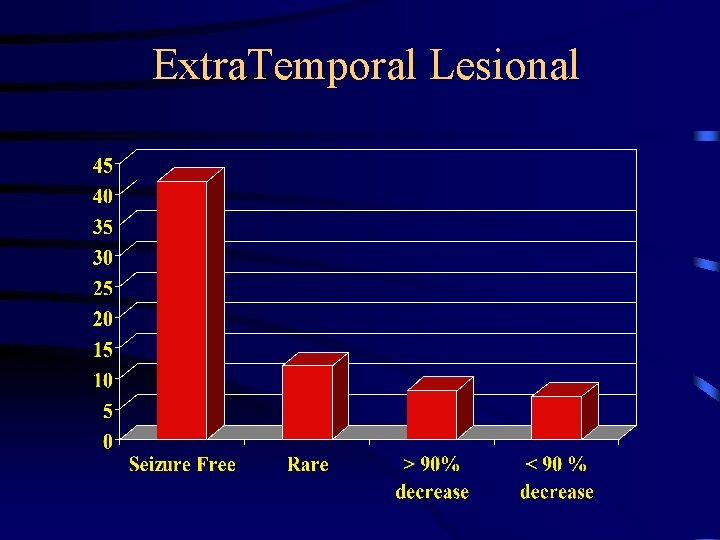
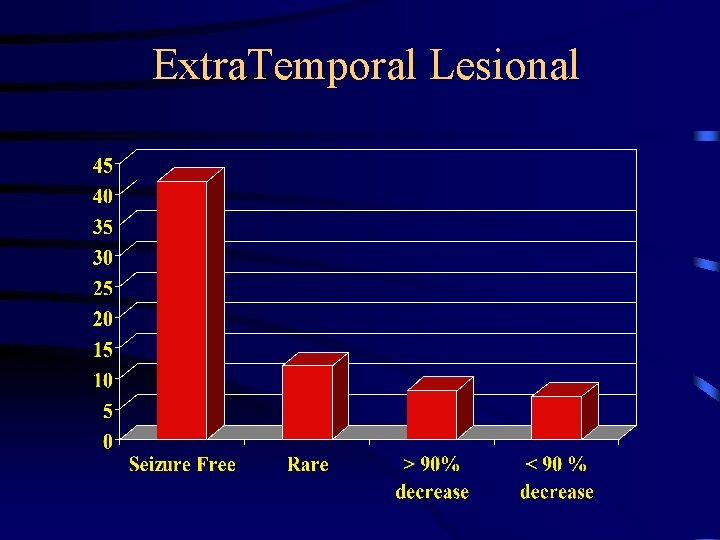
Extra. Temporal Lesional
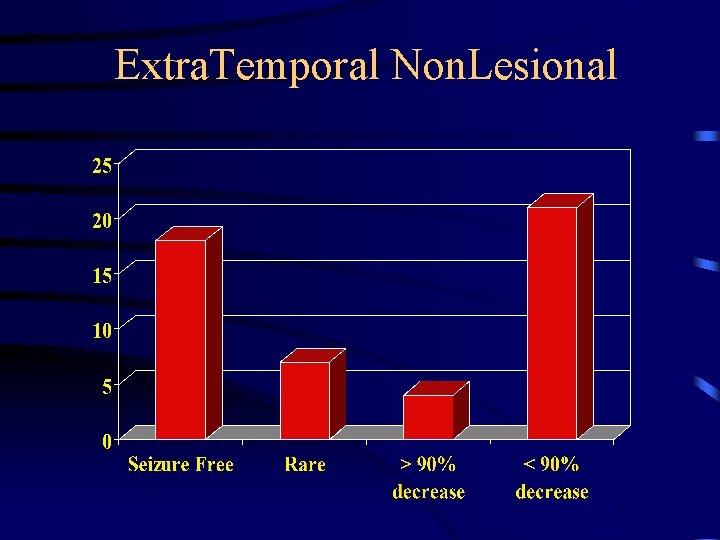
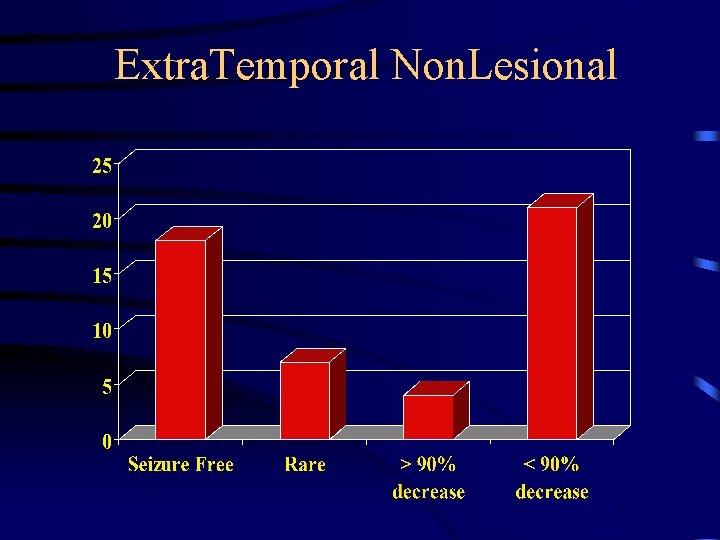
Extra. Temporal Non. Lesional
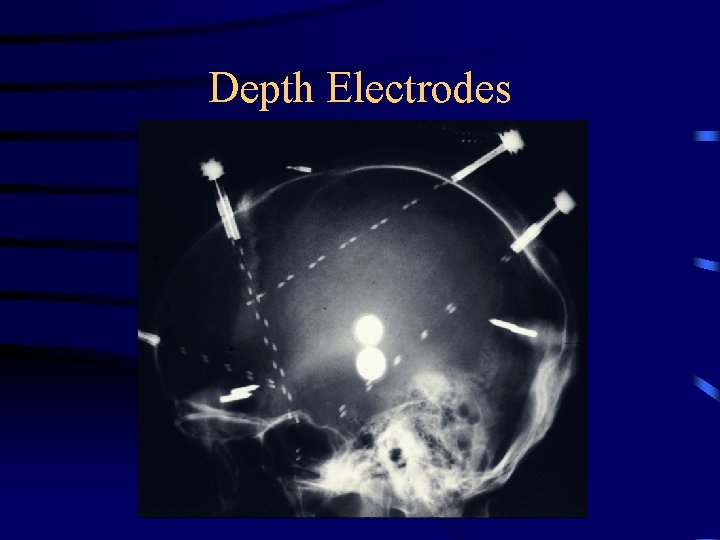
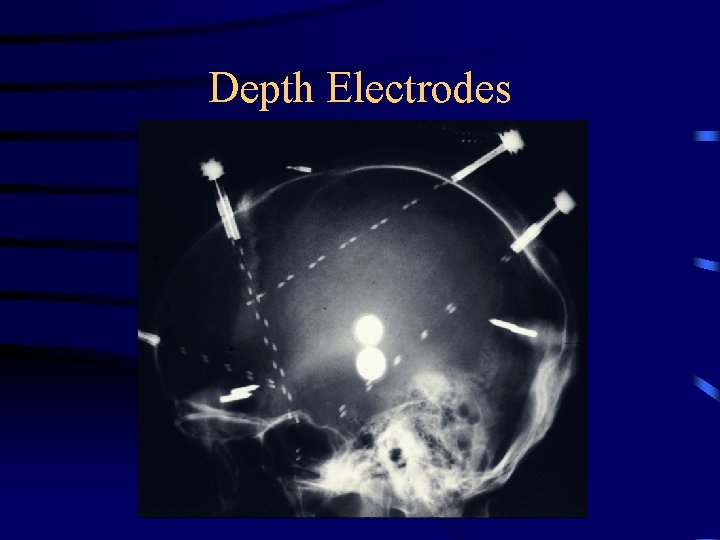
Depth Electrodes
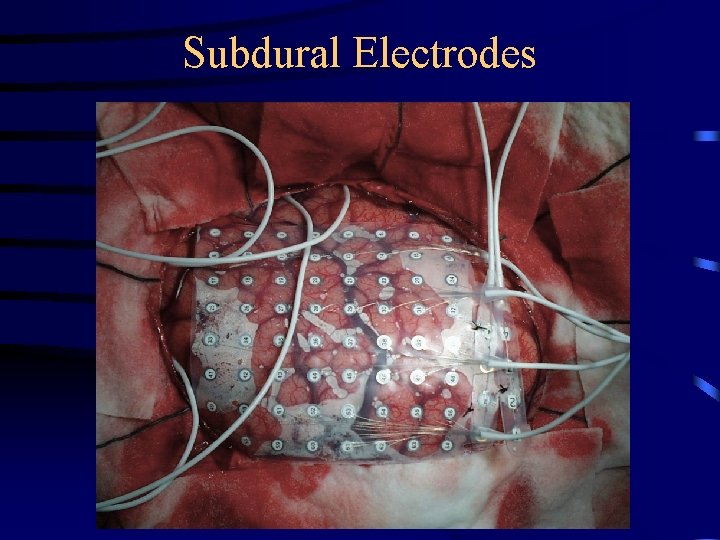
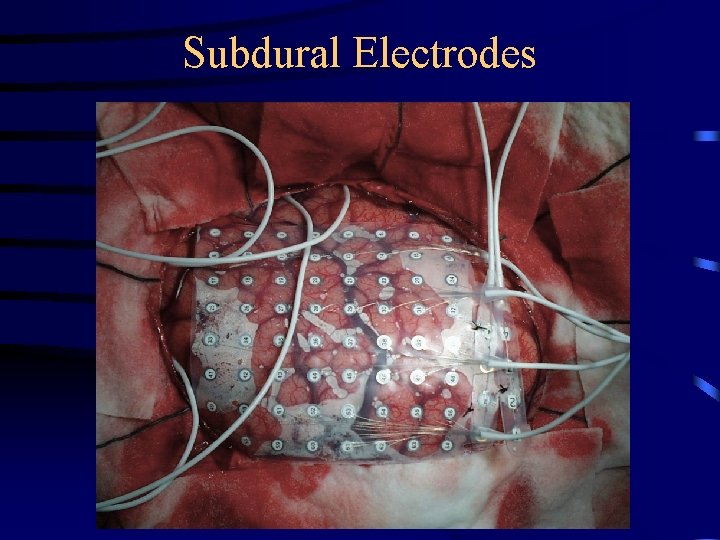
Subdural Electrodes
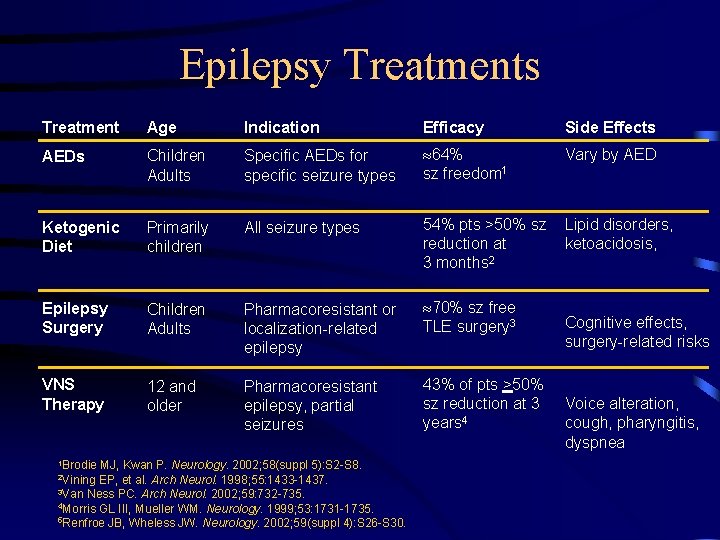
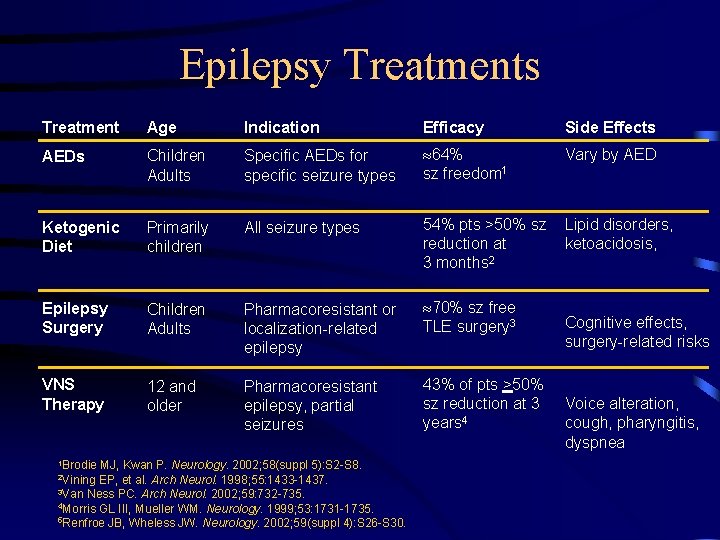
Epilepsy Treatments Treatment Age Indication Efficacy Side Effects AEDs Children Adults Specific AEDs for specific seizure types 64% sz freedom 1 Vary by AED Ketogenic Diet Primarily children All seizure types 54% pts >50% sz reduction at 3 months 2 Lipid disorders, ketoacidosis, Epilepsy Surgery Children Adults Pharmacoresistant or localization-related epilepsy 70% sz free TLE surgery 3 VNS Therapy 12 and older Pharmacoresistant epilepsy, partial seizures 43% of pts >50% sz reduction at 3 years 4 1 Brodie MJ, Kwan P. Neurology. 2002; 58(suppl 5): S 2 -S 8. EP, et al. Arch Neurol. 1998; 55: 1433 -1437. 3 Van Ness PC. Arch Neurol. 2002; 59: 732 -735. 4 Morris GL III, Mueller WM. Neurology. 1999; 53: 1731 -1735. 5 Renfroe JB, Wheless JW. Neurology. 2002; 59(suppl 4): S 26 -S 30. 2 Vining Cognitive effects, surgery-related risks Voice alteration, cough, pharyngitis, dyspnea
Summary - Objectives • Understand terminology specific to seizures & epilepsy – – Distinguish partial onset from generalized seizures Simple v. Complex Secondarily v. Primary Differentiate clinical from syndromic epilepsies • Appreciate variability of seizure disorders wrt clinical appearance and cause • Understand the diagnostic approach to seizure disorders – not all seizures represent epilepsy; not all spells are seizures • Develop a basic understanding of the approach to treatment of epilepsy