The Structure of the NHS A Brief History
The Structure of the NHS
A Brief History n n n The NHS officially came into being on the 5 th July 1948, and was the brainchild of Labour’s Health Secretary Aneurin Bevan. It was designed to provide free comprehensive healthcare for all. The Beverage Report, commissioned by the Labour Party during WWII and published in 1943, had a comprehensive health service as one of its main recommendations, and was hugely popular with the public. Previous to the formation of the NHS, healthcare consisted of a mish-mash of private, municipal, church and charity schemes. This meant that only roughly half the population was covered properly for their healthcare, and it was mostly women and the poorest who were not covered. The plans initially faced opposition from the richer portions of society, and in particular Doctors, who saw the plans as a restriction on their freedoms. However, a generous pay scheme brought them on side. To explain the new service the Government commissioned a series of adverts featuring a character named ‘Charley’. The core principles on which the NHS were founded were; ¨ That it meet the needs of everyone ¨ That it be free at the point of delivery ¨ That it be based on clinical need, not ability to pay Since then, there have been a number of Milestones; ¨ 1952: Introduction of charges for prescriptions – these have since been phased out in Wales and Scotland ¨ 1962: The Hospital plan – Enoch Powell introduces plan to build a hospital for every 125, 000 people. ¨ 1968: First UK Heart Transplant – the operation would not become commonplace for at least a decade. ¨ 1990: NHS and Community Care Act – introduces the ‘internal market’ within the NHS ¨ 2006: Patient Choice – the 2006 Health Act allowed patients to choose which hospital they were treated in
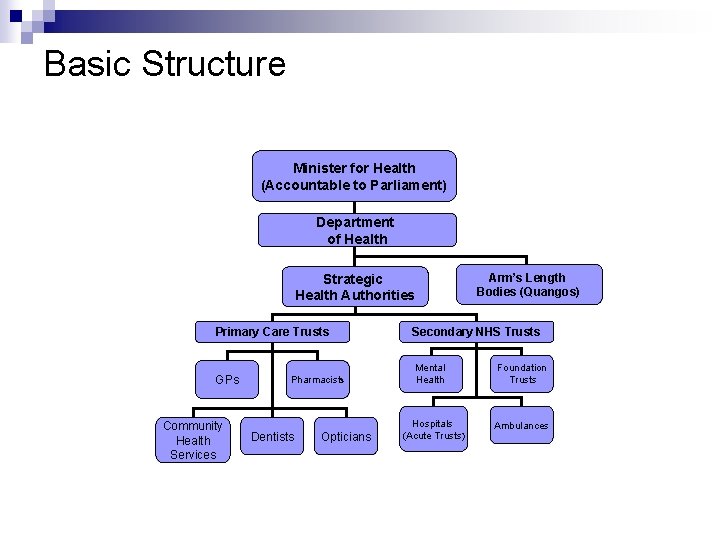
Basic Structure Minister for Health (Accountable to Parliament) Department of Health Strategic Health Authorities Arm’s Length Bodies (Quangos) Primary Care Trusts Secondary NHS Trusts GPs Mental Health Foundation Trusts Hospitals (Acute Trusts) Ambulances Community Health Services Pharmacists Dentists Opticians
Minister for Health and Do. H n n n n Minister: The Secretary of State for Health leads the NHS, working with five other Health Ministers. The combined post of Permanent Secretary/NHS Chief Executive acts as the go between for the Do. H and the Secretary of State. The Secretary of State is accountable to Parliament for the performance of the NHS, and decides how the funds granted by Parliament to the NHS will be spent. Department of Health: The Department of Health is responsible for running the NHS, providing strategic direction, setting standards, investing resources and striving for improvement. The main business of running the NHS is performed by the Do. H Board, which includes the Chief Executive, Directors (Standards and Quality, Delivery, Finance and Investment etc. ) the Chief Medical Officer (Chief medical advisor to the Government) and the Chief Nursing Officer. The CMO and CNO also form part of the seven ‘Heads of profession’, which also include Chief Dental Officer, the Chief Social Services Inspector, the Chief Health Professions Officer, the Chief Pharmaceutical Officer and the Chief Scientist. These people provide expert knowledge in each of their fields. There is also a board of Clinical Directors, who help the Do. H to set the Clinical priorities in a number of areas of expertise, including; Emergency Access, Mental Health, Children’s Services, Heart Disease, Primary Care, Diabetes, Cancer and Older people’s services.
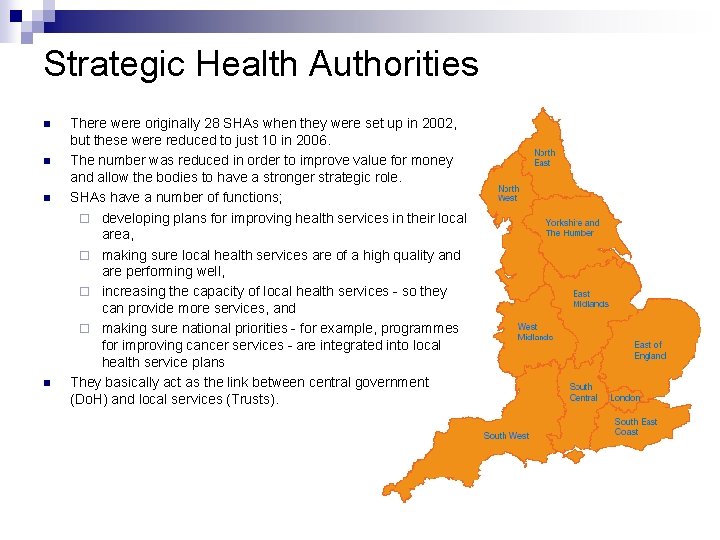
Strategic Health Authorities n n There were originally 28 SHAs when they were set up in 2002, but these were reduced to just 10 in 2006. The number was reduced in order to improve value for money and allow the bodies to have a stronger strategic role. SHAs have a number of functions; ¨ developing plans for improving health services in their local area, ¨ making sure local health services are of a high quality and are performing well, ¨ increasing the capacity of local health services - so they can provide more services, and ¨ making sure national priorities - for example, programmes for improving cancer services - are integrated into local health service plans They basically act as the link between central government (Do. H) and local services (Trusts).
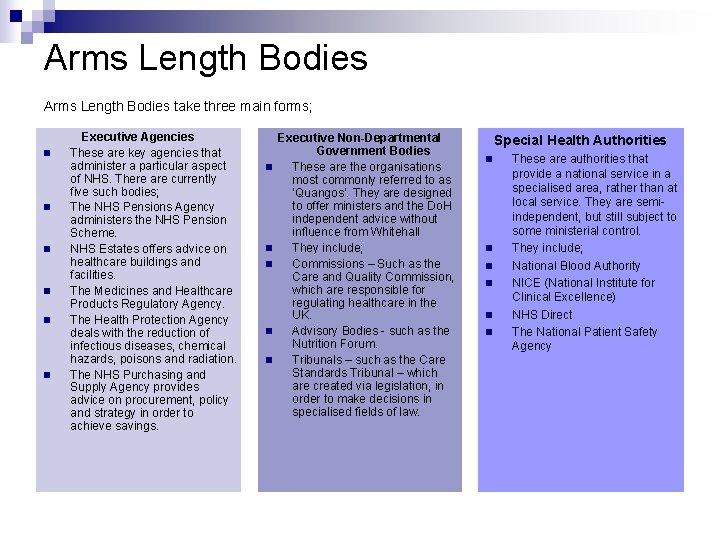
Arms Length Bodies take three main forms; n n n Executive Agencies These are key agencies that administer a particular aspect of NHS. There are currently five such bodies; The NHS Pensions Agency administers the NHS Pension Scheme. NHS Estates offers advice on healthcare buildings and facilities. The Medicines and Healthcare Products Regulatory Agency. The Health Protection Agency deals with the reduction of infectious diseases, chemical hazards, poisons and radiation. The NHS Purchasing and Supply Agency provides advice on procurement, policy and strategy in order to achieve savings. n n n Executive Non-Departmental Government Bodies These are the organisations most commonly referred to as ‘Quangos’. They are designed to offer ministers and the Do. H independent advice without influence from Whitehall They include; Commissions – Such as the Care and Quality Commission, which are responsible for regulating healthcare in the UK. Advisory Bodies - such as the Nutrition Forum. Tribunals – such as the Care Standards Tribunal – which are created via legislation, in order to make decisions in specialised fields of law. Special Health Authorities n n n These are authorities that provide a national service in a specialised area, rather than at local service. They are semiindependent, but still subject to some ministerial control. They include; National Blood Authority NICE (National Institute for Clinical Excellence) NHS Direct The National Patient Safety Agency
Primary Care Trusts n n n Primary Care Trusts are directly responsible for the provision of all primary care at a local level – the first place you would go with a health problem. This may be the GP, NHS direct phone line, the Dentist or a drop in centre. These are all managed by the local PCT, of which there are 152 currently in England. PCTs will work with local agencies and authorities in order to deliver the full range of primary care. PCTs control around 80% of the entire NHS budget, and use this not only to provide primary care, but also fund the Hospitals, Ambulances and other secondary NHS trusts through ‘service level agreements’. These work on a ‘payment by results’ basis, with the PCT deciding funding levels to these trusts according to their performance against predetermined targets. Essentially then, PCTs are responsible for the provision of all local health services, both in terms of primary care and secondary care provided by semi-independent secondary trusts. They ensure that they wok together well, and specific local needs are met. They also work with local agencies – such as social care – and local government authorities to further ensure all elements of local care met. PCTs vary in size significantly. They may cover just a city and its surrounding area (for example Peterborough PCT, which covers 156, 000 people) to whole counties (such as Norfolk PCT, which covers over 700, 000 people).
Secondary NHS Trusts n Aside from Primary Care Trusts, there are semi-independent NHS trusts that cover secondary care provision; n Acute Trusts; These are the trusts that manage hospitals. They may cover just one large hospital or a small number of hospitals, but normally have a ‘main’ hospital as their focus. They are responsible for medical and surgical care for the local population, which can include home visits or small clinics as well as hospital care. Acute trusts employ the vast majority of NHS staff. Some are teaching trusts, and others are regional or national centres for specialised care. Foundation Trusts; These are the more independent form of Hospital trust than an Acute trust, and are managed by local managers, staff and members of the public. They are still a part of the NHS and party to its inspection regime, and recently added powers in the Health Bill 2009 will give the Health minister greater powers to intervene when they begin to fail. Mental Health Trusts; There are 60 mental health trusts serving England, which are responsible for providing for their areas mental health needs. Treatment may come through a primary care outlet, but can involved more specialist care that might include counselling and other psychological therapies, community and family support – this is provided by the Mental Health Trust. Ambulance Trusts; There are 12 Ambulance trusts covering England. They provide emergency access to healthcare for patients, categorised into either A, B or C class emergencies, with A as the most serious and lifethreatening. They provide rapid response vehicles and paramedics that can treat at the scene, as well as general transportation for treatment (but only in some areas) Care Trusts; These are a relatively new form of trust, and there aren’t many in existence yet. They are designed as a link for community social care and community healthcare, when it is believed that a closer relationship between the two is needed. n n
Costs and Funding n n n The NHS cost the government £ 92. 5 Billion in the year 2008/9. Most of this is funding, as mentioned before, goes directly to the PCTs, who decide how the money is to be spent. The PCTs receive a budget from the Department of Health on a formula basis relating to population and specific local needs. PCTs are expected to ‘break even’, i. e. not go into deficit, but this has proved near impossible for some trusts, and there are those that consistently overspend. Almost all of the NHS’s money is derived from the UK taxpayers, and presents the single largest cost on the Government Budget. There have been commitments from both main parties to continue at present funding levels past 2011, and this has been a cause of concern as many analysts have shown them to be unsustainable without either cuts made elsewhere in the public sector, or an increase in tax rates.
Regulation n n The NHS is regulated by the Care and Quality Commission, or CQC. It took over the role of the Healthcare Commission in early 2009. This body is responsible for healthcare and adult services provision, both public and private. It makes sure that essential common quality standards are being met where care is provided, from hospitals to private care homes, and works towards their improvement By law all NHS providers such as hospitals and ambulance services must register with CQC from April 1 2009, to show they are protecting people from the risk of infection. The registration system applies to NHS provider trusts (acute, ambulance, mental health and primary care) and the NHS Blood and Transplant Authority. CQC has a wide range of enforcement powers, such as fines and public warnings, and has flexibility about how and when to use them. It can apply specific conditions in response to serious risks. For example, it can demand that a hospital ward or service is closed until the provider meets safety requirements or is suspended. Or, it can take a service off the register if absolutely necessary Example: Late last year (October) The CQC has recently released its latest reports into the UK’s NHS Trusts, and found that 1 in 8 is not meeting minimum standards, and ‘urgently need to improve the standard of care that they provide’ The CQC has rated trusts on a wide range of issues, such as patient satisfaction, cleanliness, training and so forth. While there has been little improvement amongst the worst performing trusts, a majority of trusts are now rated ‘Good’ or ‘Excellent’. This is an improvement on previous all previous years of the reports. As for the failing trusts; The CQC said it intended to work closely with these 47 trusts to sort out their problems ahead of April next year Link: http: //news. bbc. co. uk/1/hi/health/8307300. stm
The Health Act 2009 n n n This law covers a variety of improvements across the NHS, the most significant of which will be the formal duty for Health Services to have regard to the NHS Constitution, first published in January 2009. It will also introduce; Direct payments for health services, giving patients greater control over the services they receive; Quality accounts, made available to patients, medics and managers; Toughens provisions to prevent the damaging effects of smoking to children and young people – with particular regard to advertising and vending machines Greater powers for the Local Government Ombudsman to deal with complaints with regard to adult social care. Awards for innovation in health care provision Link: Health Act 2009
- Slides: 11