THE SKELETAL SYSTEM PART 1 BONES Chapter 6
THE SKELETAL SYSTEM PART 1: BONES Chapter 6
Bone �a connective tissue � 18% of weight of human body �Skeletal System includes bones & cartilage �Part 1: Bone �Part 2: Axial Skeleton �Part 3: Appendicular Skeleton �Part 4: Joints
FUNCTIONS SUPPORT � skeleton serves as structural framework by supporting soft tissues & providing attachments for tendons of muscle 1. 2. PROTECTION �Protects most important soft tissue organs from injury
FUNCTIONS 3. MOVEMENT �Skeletal muscles attach to bones, when the muscle contract the bones move 4. MINERAL HOMEOSTASIS �Bone stores calcium, phosphorus which both help make bone strong �If body needs these minerals bone releases them
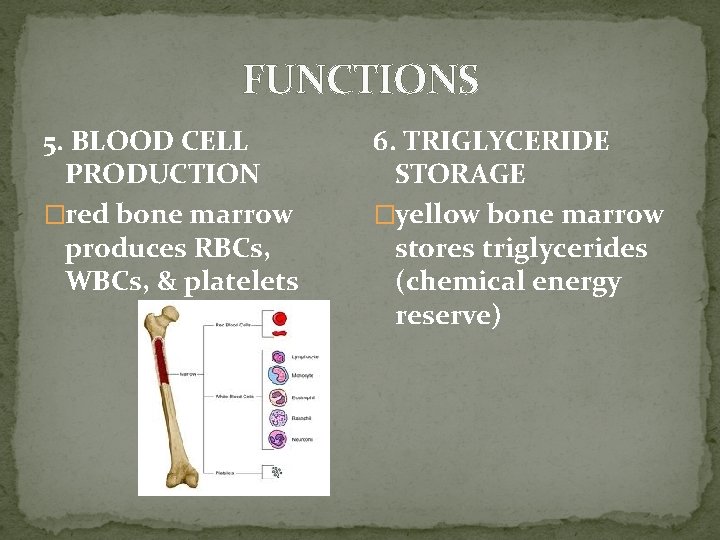
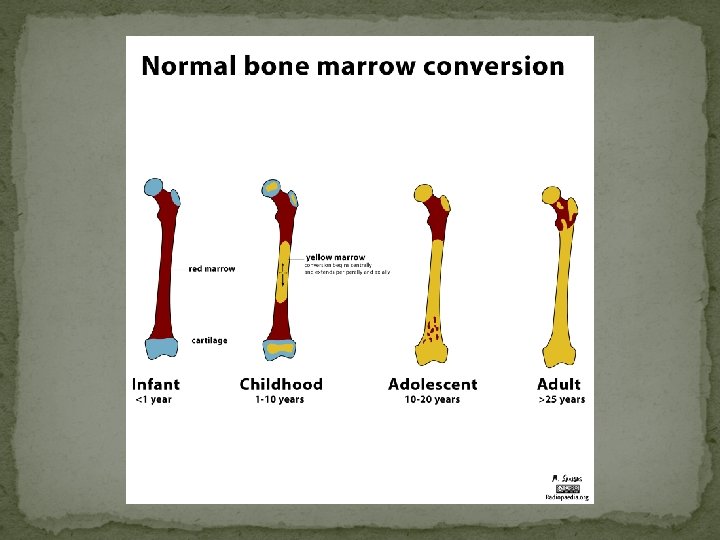
FUNCTIONS 5. BLOOD CELL PRODUCTION �red bone marrow produces RBCs, WBCs, & platelets 6. TRIGLYCERIDE STORAGE �yellow bone marrow stores triglycerides (chemical energy reserve)
Classification of the Skeletal System Axial Skeleton �skull �vertebral column �rib cage �hyoid Appendicular Skeleton �Bones that make up the limbs and their girdles (bones that hold limbs to trunk)
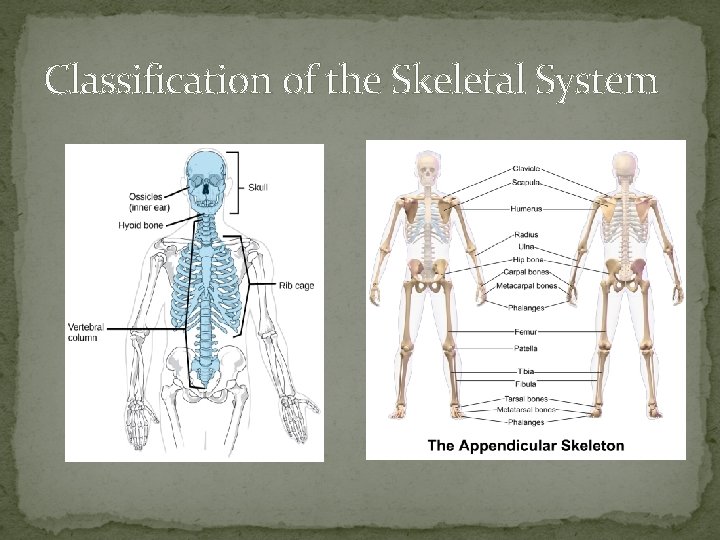
Classification of the Skeletal System
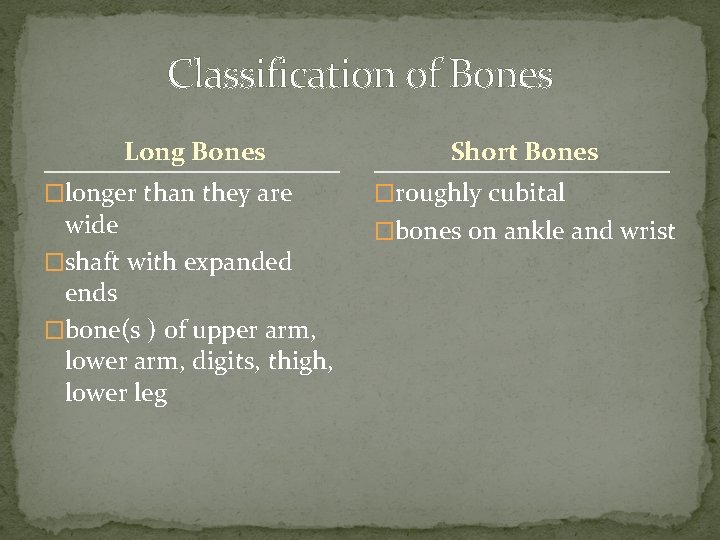
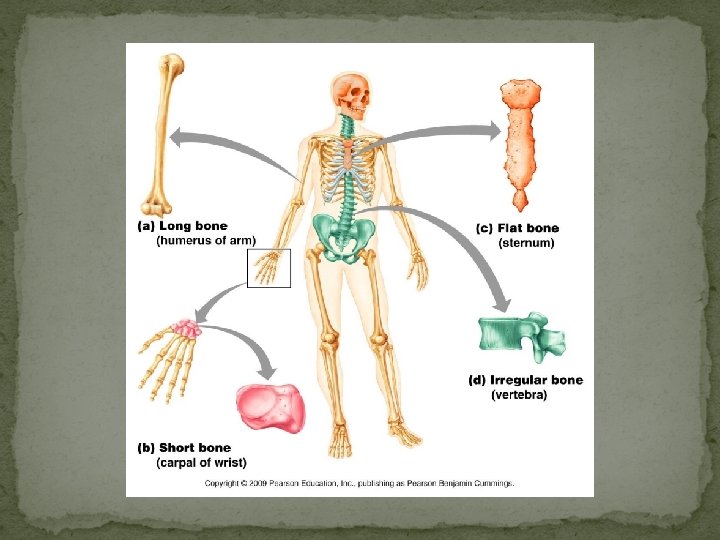
Classification of Bones Long Bones �longer than they are wide �shaft with expanded ends �bone(s ) of upper arm, lower arm, digits, thigh, lower leg Short Bones �roughly cubital �bones on ankle and wrist
Classification of Bones Flat Bones �thin, flat bones with bit of a curve �sternum �scapula �ribs �most skull bones Irregular Bones �do not fit into other categories �vertebrae �hip bones
Classification of Bone Tissue �Compact Bone � outside layer of all bones �Spongy Bone � inside certain bones
TYPES of BONE: COMPACT BONE �has few spaces �strongest form of bone �beneath periosteum of all bone �provides protection & support and resists stresses produced by weight & movement
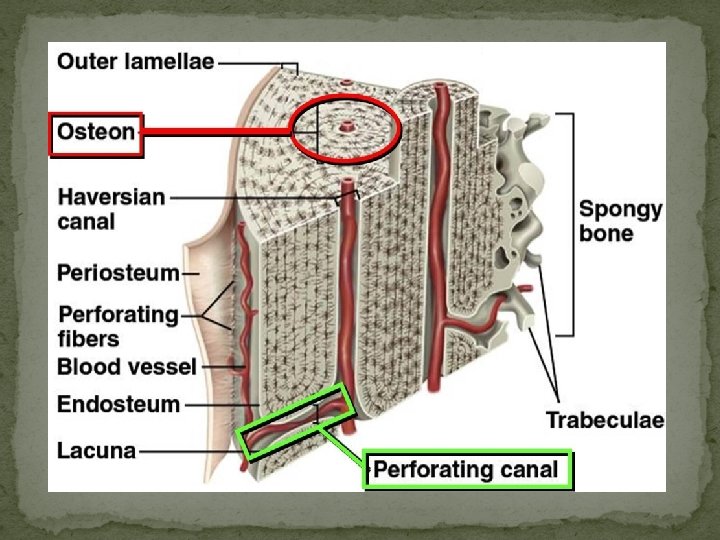
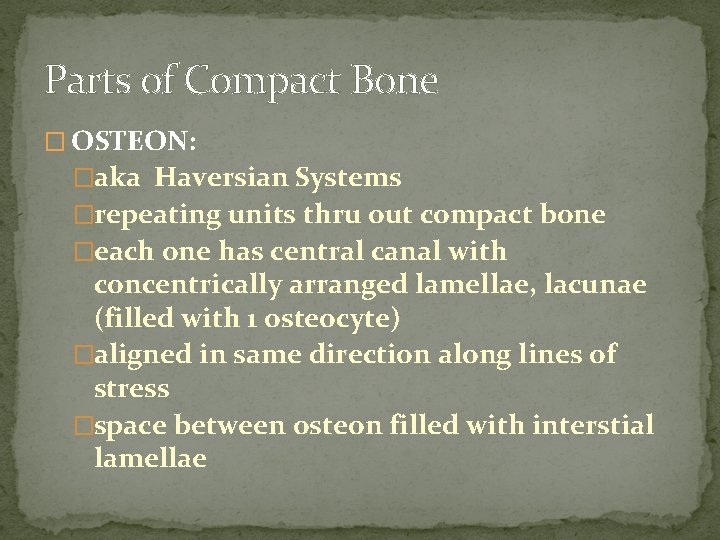
Parts of Compact Bone � OSTEON: �aka Haversian Systems �repeating units thru out compact bone �each one has central canal with concentrically arranged lamellae, lacunae (filled with 1 osteocyte) �aligned in same direction along lines of stress �space between osteon filled with interstial lamellae
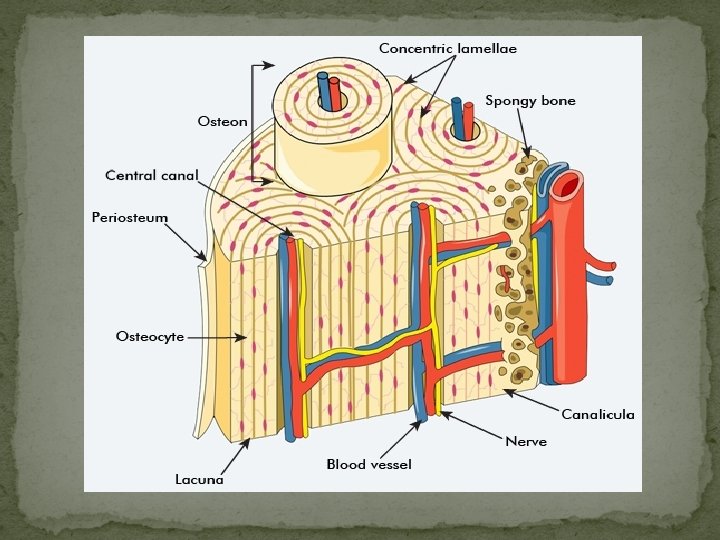
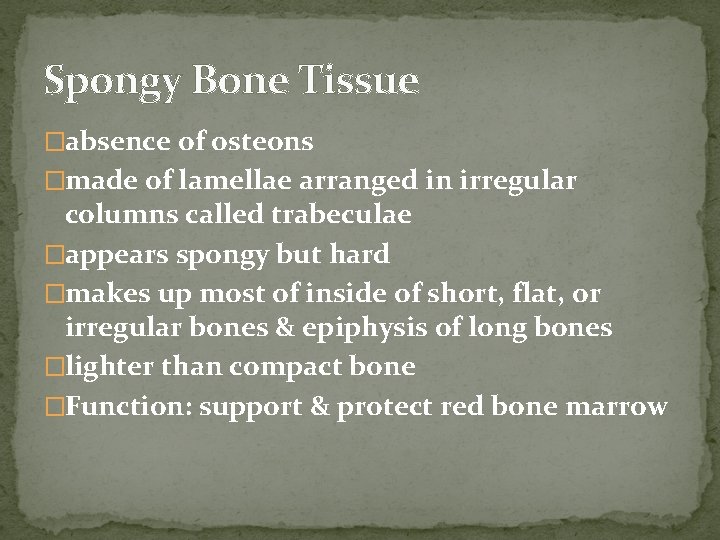
Spongy Bone Tissue �absence of osteons �made of lamellae arranged in irregular columns called trabeculae �appears spongy but hard �makes up most of inside of short, flat, or irregular bones & epiphysis of long bones �lighter than compact bone �Function: support & protect red bone marrow
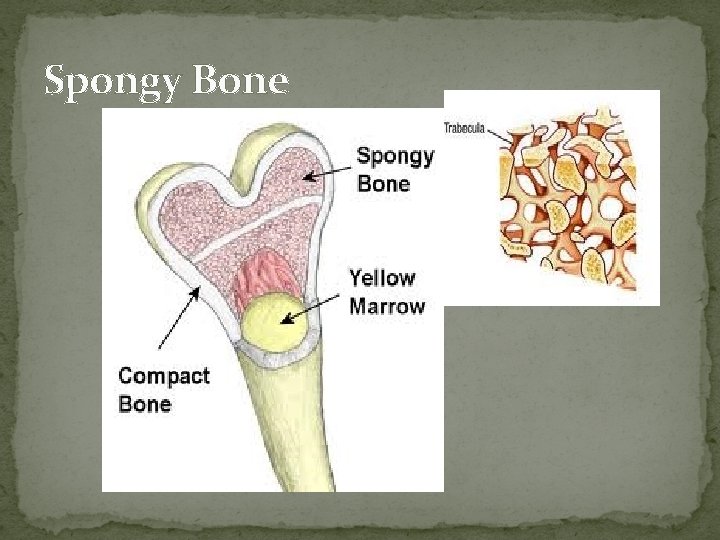
Spongy Bone
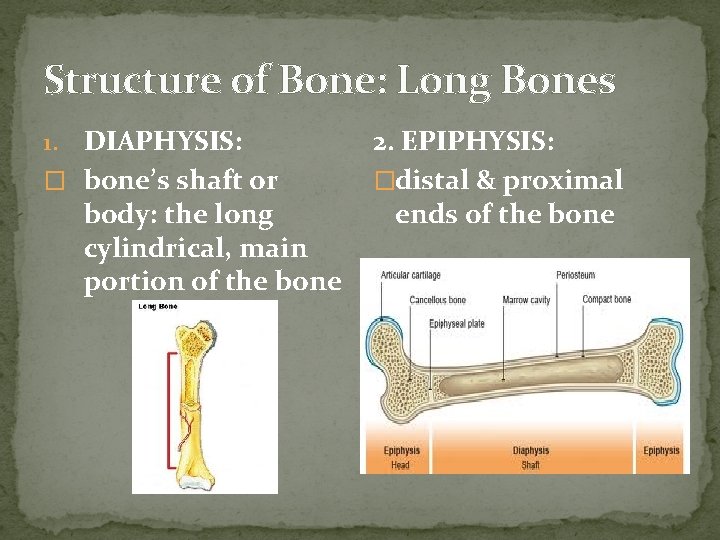
Structure of Bone: Long Bones DIAPHYSIS: � bone’s shaft or body: the long cylindrical, main portion of the bone 1. 2. EPIPHYSIS: �distal & proximal ends of the bone
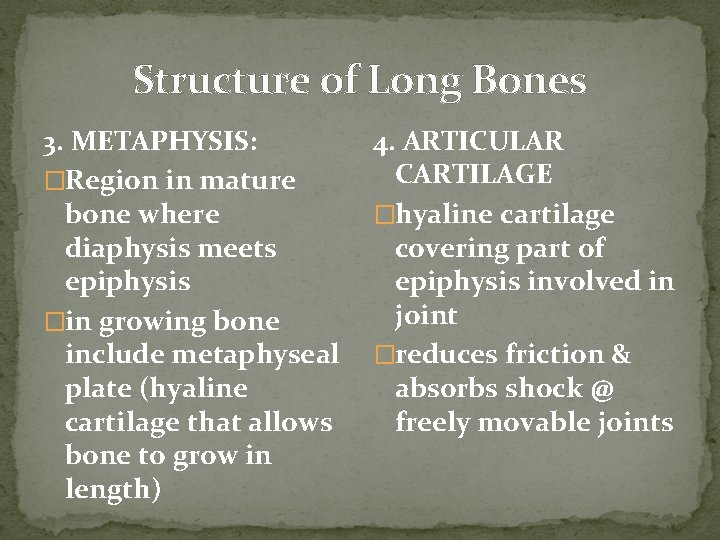
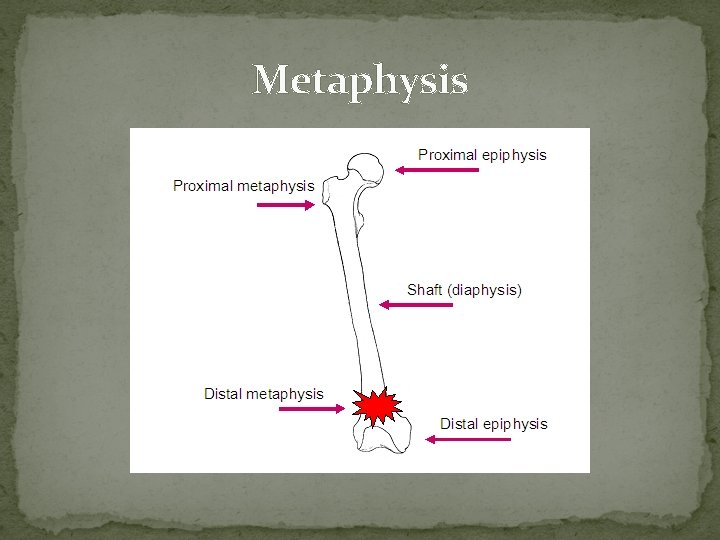
Structure of Long Bones 3. METAPHYSIS: �Region in mature bone where diaphysis meets epiphysis �in growing bone include metaphyseal plate (hyaline cartilage that allows bone to grow in length) 4. ARTICULAR CARTILAGE �hyaline cartilage covering part of epiphysis involved in joint �reduces friction & absorbs shock @ freely movable joints
Metaphysis
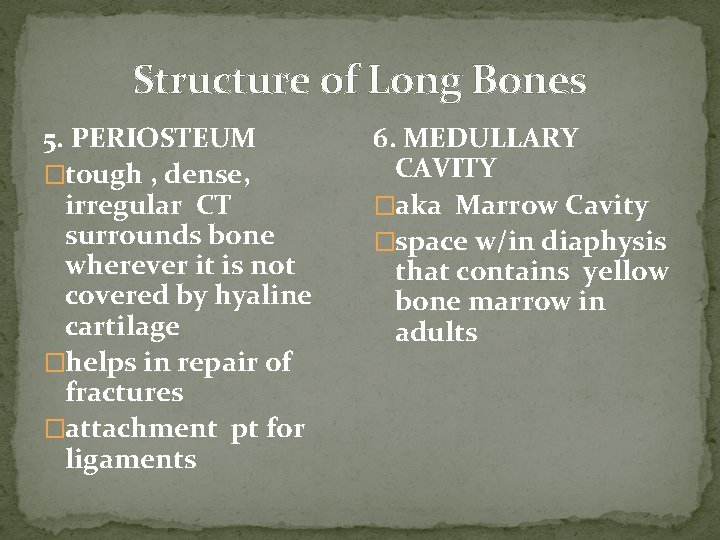
Structure of Long Bones 5. PERIOSTEUM �tough , dense, irregular CT surrounds bone wherever it is not covered by hyaline cartilage �helps in repair of fractures �attachment pt for ligaments 6. MEDULLARY CAVITY �aka Marrow Cavity �space w/in diaphysis that contains yellow bone marrow in adults
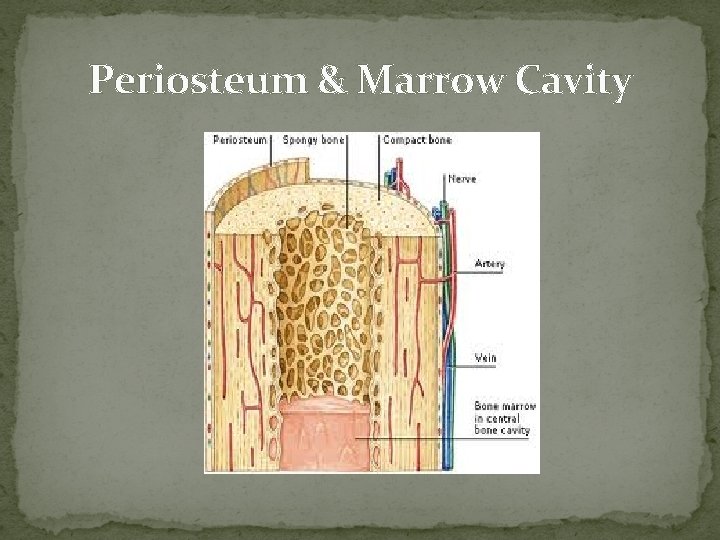
Periosteum & Marrow Cavity
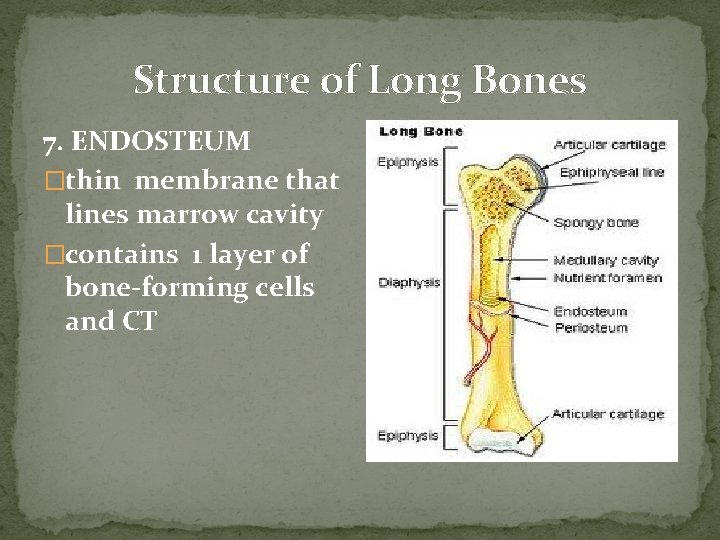
Structure of Long Bones 7. ENDOSTEUM �thin membrane that lines marrow cavity �contains 1 layer of bone-forming cells and CT
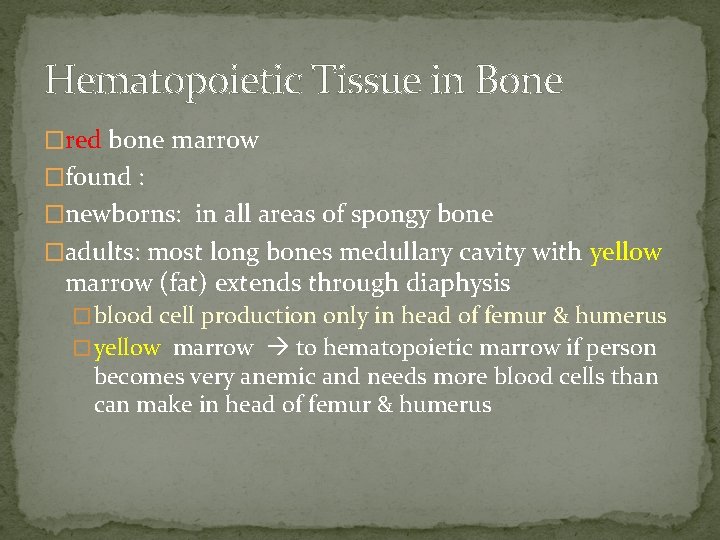
Hematopoietic Tissue in Bone �red bone marrow �found : �newborns: in all areas of spongy bone �adults: most long bones medullary cavity with yellow marrow (fat) extends through diaphysis � blood cell production only in head of femur & humerus � yellow marrow to hematopoietic marrow if person becomes very anemic and needs more blood cells than can make in head of femur & humerus
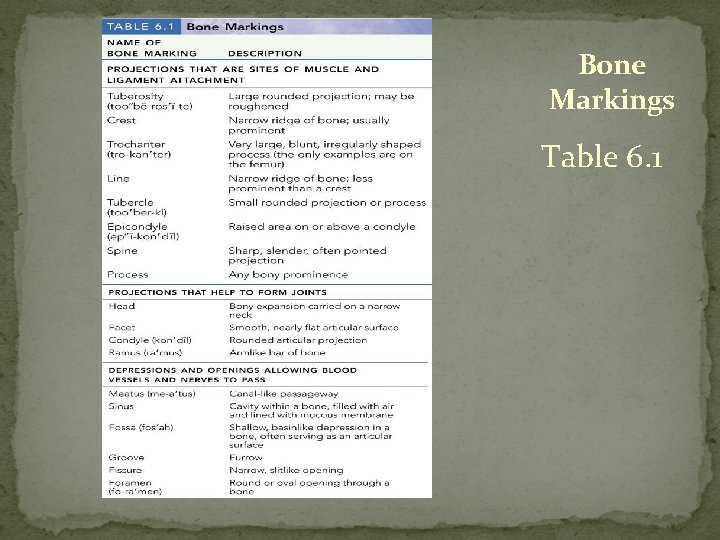
Bone Markings Table 6. 1
HISTOLOGY of BONE �Bones are hard due to calcification: calcium carbonate & other minerals (Mg, F, K, S) form crystals around collagen fibers �bone hardness depends on crystallized inorganic mineral salts �bone flexibility depends on collagen fibers
Types of Bone Cells OSTEOGENIC CELLS � Stem cells from mesenchyme (origin of all CT) � only bone cells to divide 1.
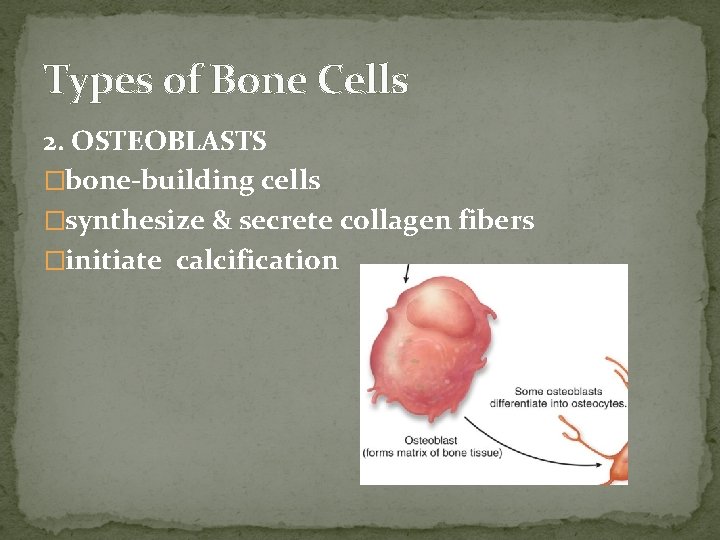
Types of Bone Cells 2. OSTEOBLASTS �bone-building cells �synthesize & secrete collagen fibers �initiate calcification
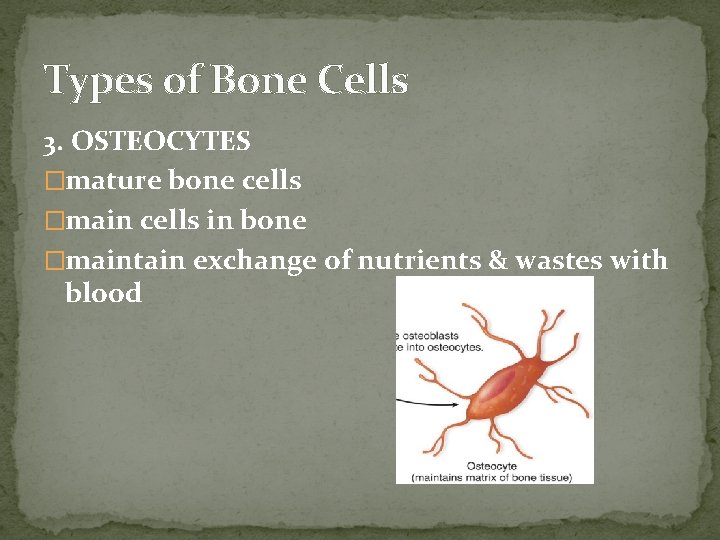
Types of Bone Cells 3. OSTEOCYTES �mature bone cells �main cells in bone �maintain exchange of nutrients & wastes with blood
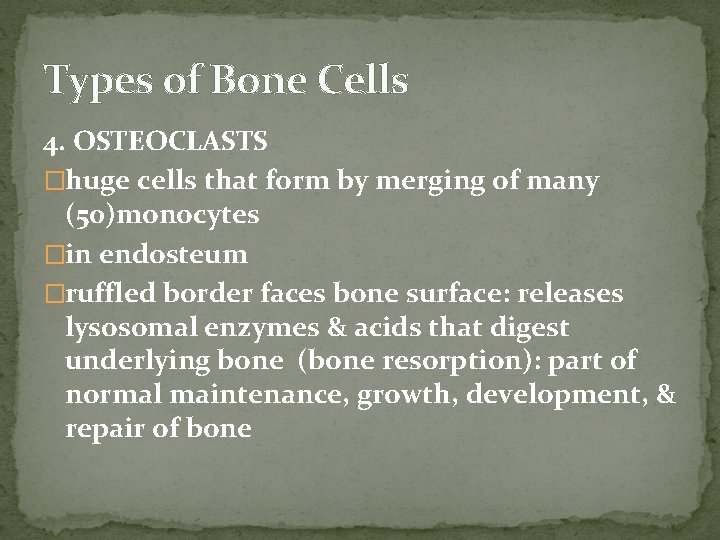
Types of Bone Cells 4. OSTEOCLASTS �huge cells that form by merging of many (50)monocytes �in endosteum �ruffled border faces bone surface: releases lysosomal enzymes & acids that digest underlying bone (bone resorption): part of normal maintenance, growth, development, & repair of bone
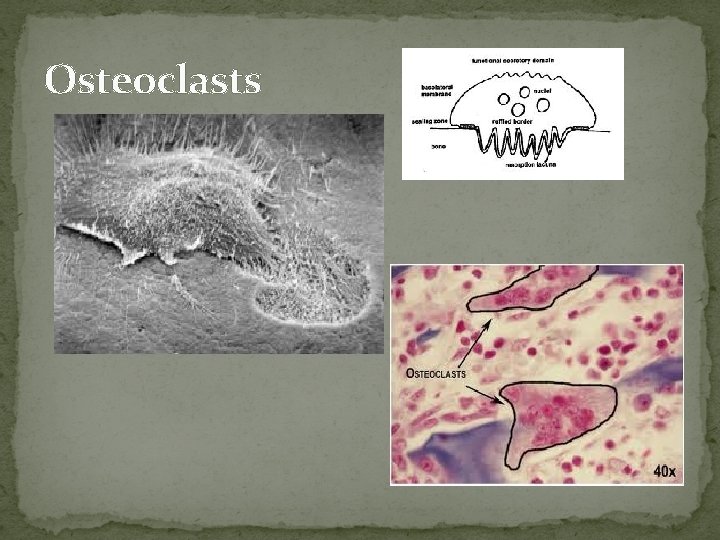
Osteoclasts
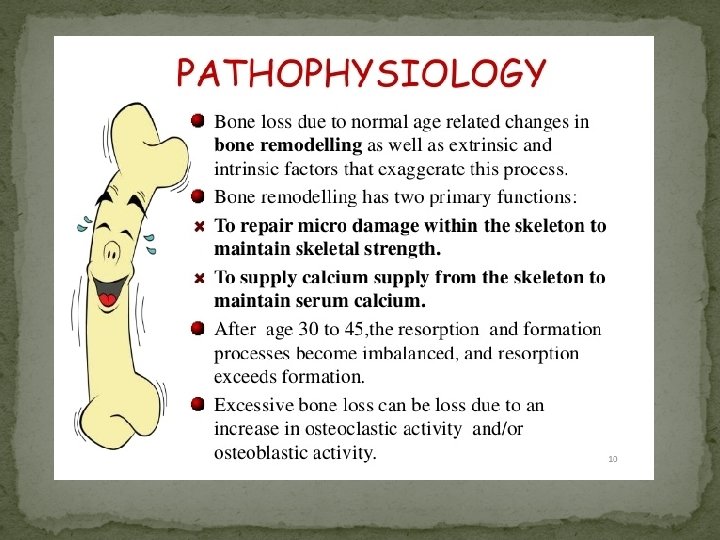
Bone Remodeling �Most bones are formed b/4 birth but each one continually renews itself for rest of life �~5% of bone being remodeled @ any given time �Bone Remodeling is the ongoing replacement of old bone tissue by new bone tissue 1. Bone Resorption 2. Bone Deposition
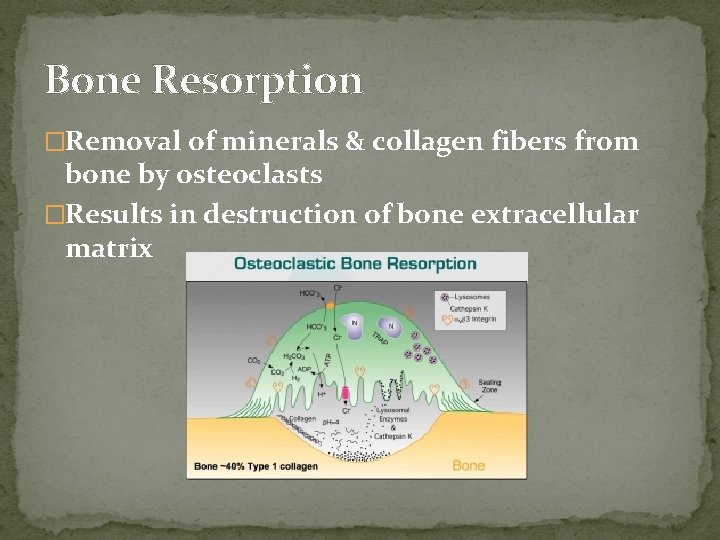
Bone Resorption �Removal of minerals & collagen fibers from bone by osteoclasts �Results in destruction of bone extracellular matrix
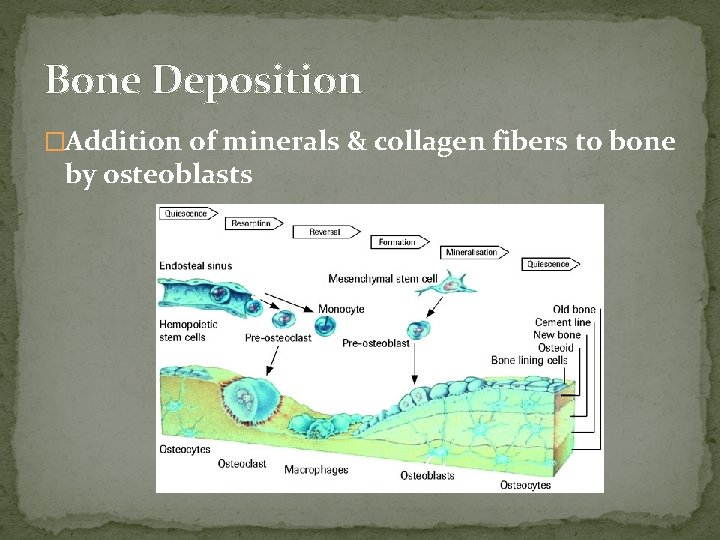
Bone Deposition �Addition of minerals & collagen fibers to bone by osteoblasts
Factors Affecting Bone Growth & Remodeling Minerals � Ca, P, F, Mg, Fe, Mn 2. Vitamins � C needed to make collagen fibers & for differentiation osteoblast osteocyte � E & B 12 needed for protein synthesis 3. Hormones � IGF’s in childhood (insulin-like growth factors) � estrogens & androgens important in puberty 1.
Bone Remodeling �https: //www. youtube. com/watch? v=0 d. V 1 Bwe 2 v 6 c �https: //www. youtube. com/watch? v=5 gpysd. G 1 Ho. E
Fracture & Repair of Bone �Fracture: any break in a bone �Fractures named by: �severity �shape or position of fracture line �person who 1 st described it
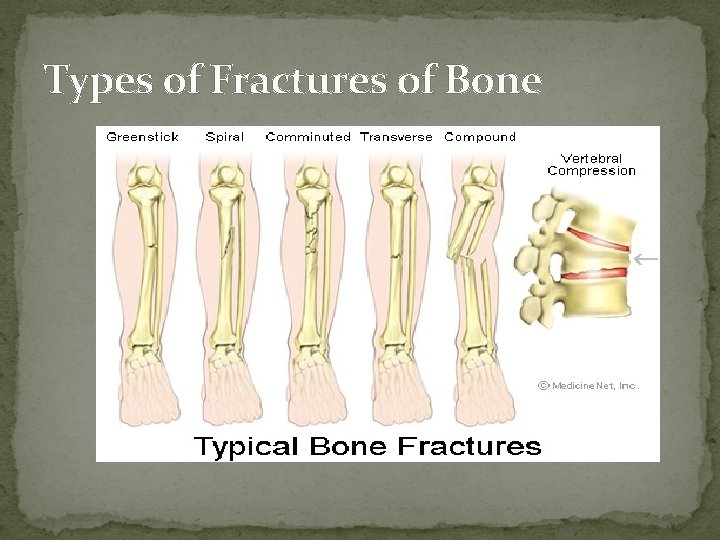
Types of Fractures of Bone
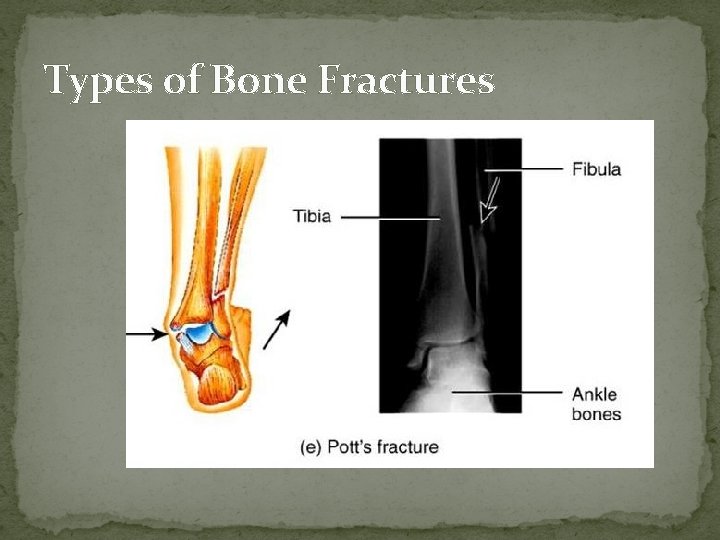
Types of Bone Fractures
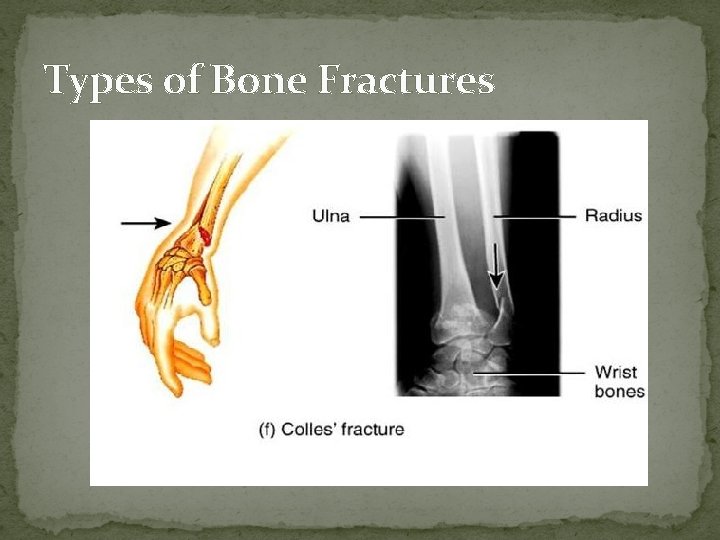
Types of Bone Fractures
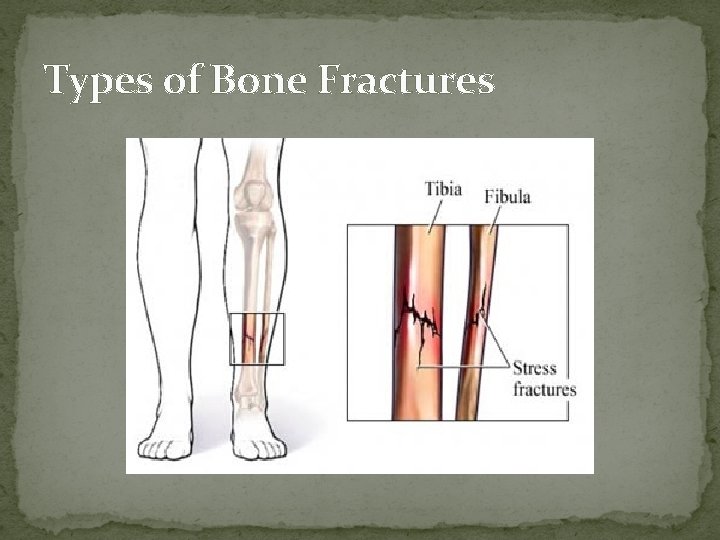
Types of Bone Fractures
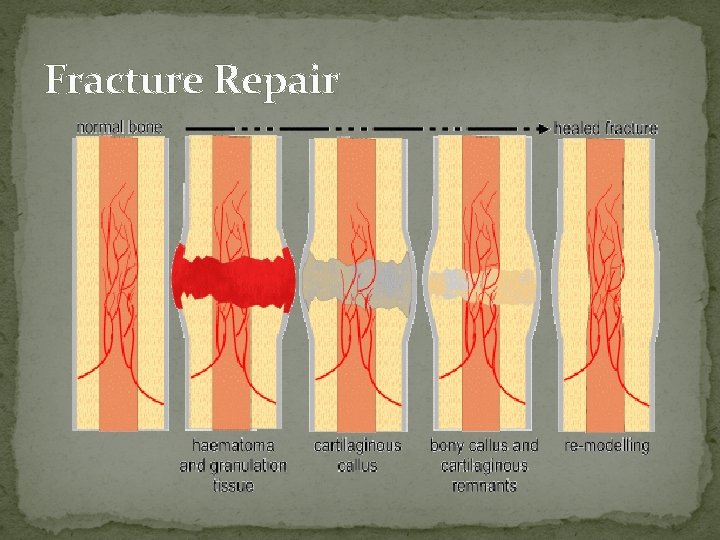
Fracture Repair
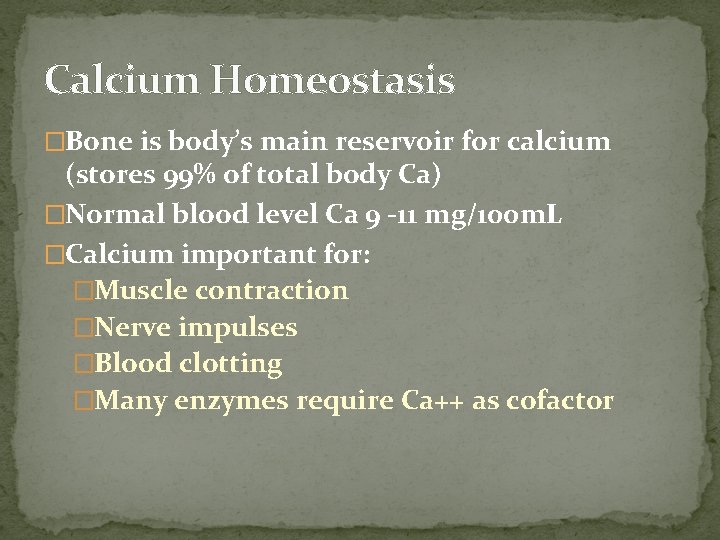
Calcium Homeostasis �Bone is body’s main reservoir for calcium (stores 99% of total body Ca) �Normal blood level Ca 9 -11 mg/100 m. L �Calcium important for: �Muscle contraction �Nerve impulses �Blood clotting �Many enzymes require Ca++ as cofactor
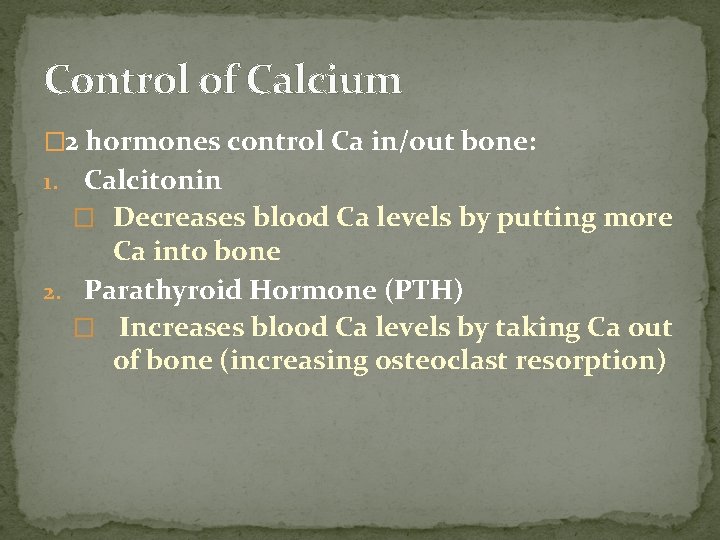
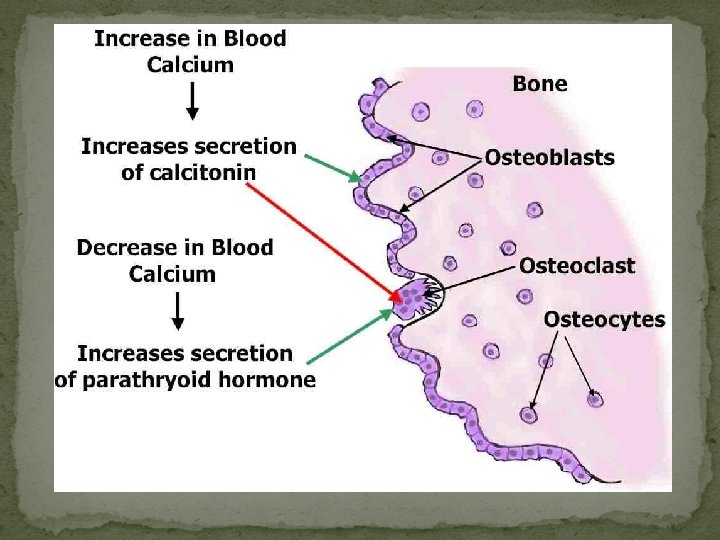
Control of Calcium � 2 hormones control Ca in/out bone: Calcitonin � Decreases blood Ca levels by putting more Ca into bone 2. Parathyroid Hormone (PTH) � Increases blood Ca levels by taking Ca out of bone (increasing osteoclast resorption) 1.
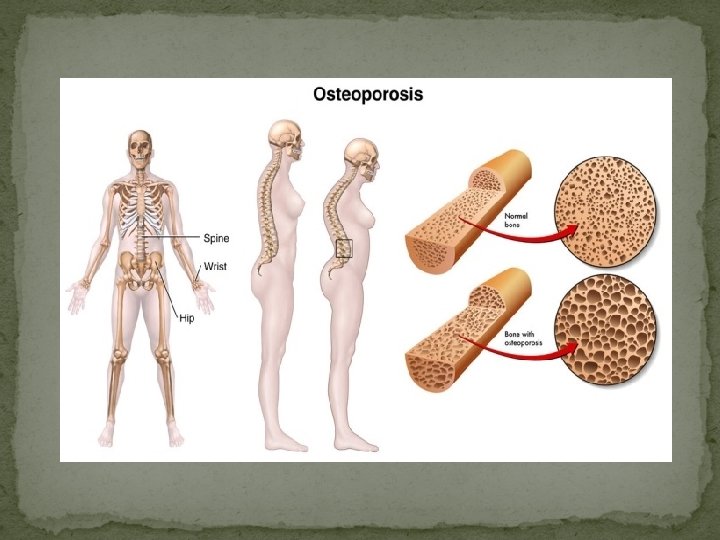
Homeostatic Imbalances in Bone 1. Osteoporosis � Condition of porous bones (resorption > deposition) � Causes: deficient Ca in diet � USA: > 1 million fractures (hip, wrist, vertebrae) & afflicts 30 million Americans � Decreased stature, hunched back, bone pain
Treatment of Osteoporosis �traditionally tx’d with: �weight-bearing exercise �calcium & Vit D �estrogen replacement
Treatment of Osteoporosis � Biphosphonates : � decrease osteoclast activity & partially reverse osteoporosis in the spine � SERMS: � “selective estrogen receptor modulators “ mimic estrogen’s beneficial bone-sparing properties without targeting the uterus or breasts �Statins: �(lower serum cholesterol) have been found to also increase bone mineral density (up to 8% over 4 yrs) �Denosubmab: (monoclonal aby drug) �↓ fractures& improves bone density
Go to this site on i. Pad then take the quiz http: //highered. mheducati on. com/sites/0072495855/s tudent_view 0/chapter 6/ani mation__osteoporosis. html
- Slides: 52