The Skeletal System Bones joints and connective tissues
The Skeletal System Bones, joints, and connective tissues
Skeletal System Functions Support Protection of organs Framework for movement l Mineral storage (calcium & phosphate) l Hematopoiesis (Blood cell production in bone marrow) l l l
Axial vs. Appendicular Skeleton Axial: l Skull, rib cage, vertebrae Appendicular: l Limbs and girdles (shoulder, pelvic)
Skeletal cartilage Properties of cartilage: l Made of mostly water l Contains cells called chondrocytes l Avascular and has no nerve endings (heals very slowly) l Stops growing during adolescence (deteriorates from this point on) l 3 different types
Types of Cartilage (see figure 6. 1) l Fibrocartilage - resists very high compression forces (in knee and between vertebrae) l Hyaline - Most common 1) articular - at joints 2) costal - (connect ribs to sternum) 3) respiratory - larynx and trachea 4) nasal l Elastic - least common type - very flexible (external ear and epiglottis)
Types of Bones (see figure 6. 2 pg. 178)
Structure of a Long Bone l l l Epiphyses - end of long bone Diaphysis - shaft Articular cartilage - covers epiphyses (provides cushion and lubrication at joints) Periosteum - double membrane surrounding bone Endosteum - lines inner cavities of bone
Structure of a Long Bone • Medullary cavity contains bone marrow • Spongy (trabecular) bone - contains red marrow (found in epiphyses) • Compact (cortical) bone found in diaphysis • Epiphyseal plate hyaline cartilage from which bone growth occurs in childhood and adolescence
Microscopic Anatomy of Compact Bone (see Figure 6. 6 on pg. 183) Haversian Canal
Chemical Composition of Bone Organic component (35%): bone cells and osteoid l Osteoid - secreted by osteoblasts (most collagen as well as other protein compounds) l Responsible for bone flexibility Inorganic component (65%): mineral component l Hydroxyapatites - Ca 3(PO 4)2 aka calcium phosphate l Responsible for hardness of bone
Cell Types Osteoblasts - bone building cells l Osteoclasts - resorb (break down) bone (secrete HCl) l Osteocytes - mature bone cells (maintain bone matrix) l
What is Ossification? l Ossification (also osteogenesis) means “bone formation” l Starts before birth and extends throughout life l Types: - intramembranous ossification (forms bones of the skull as well as clavicles) - endochondral ossification (forms all bones below the skull and clavicles)
Endochondral Ossification Replacement of hyaline cartilage with bone see Figure 6. 8 on pg 185 l Ossification begins in the middle of the bone (primary ossification center) l At birth, epiphyses remain mostly cartilaginous l By early childhood, hyaline cartilage only remains in the epiphyseal plate and covering the epipyses (articular cartilage) l
Post-natal Bone Growth occurs from the epiphyseal plate (see left side of Figure 6. 10 on pg. 187) l Diaphysis also increases in width as bone lengthens (gives bone more stability) l Regulated by growth hormone (h. GH) in childhood l Growth spurt in teen years cause by androgens (sex hormones): testosterone (males) estrogen (females) l Bone growth at epipyseal plate
Post-natal Bone Growth After epiphyseal plate has completely ossified, bones can only grow in width (appositional growth) l Bone remodeling occurs throughout life l Bone deposit (osteoblasts) and bone resorption (osteoclasts) balance each other out in healthy young adults l See right side of Figure 6. 10 on pg 187 l Bone growth at epipyseal plate
Bone Remodeling Bone deposit and bone resorption of the adult skeleton l Occurs to prevent bones from becoming brittle l Spongy bone is replaced every 3 -4 years; compact every 10 years l
Control of Bone Remodeling l Mechanical stress n l weight bearing activity leads to bone deposit to strengthen areas most in need (Wolff’s Law) Hormonal control (see figure 6. 12 on pg. 189) Calcitonin - stimulates bone deposit n Parathyroid hormone (PTH) - stimulates bone resorption n
Types of fractures (pg. 191) l Nondisplaced vs. displaced l Complete vs. incomplete l Linear vs. transverse l Open (compound) vs. closed (simple) * Fractures are treated with closed reduction (hands are used to align bone ends) or open reduction (screws, rods, wires, etc are used to keep bone ends together)
What is a joint? l Area where two bones meet
Ligaments and Tendons Ligaments l Connect two bones together at a joint Tendons l Connect muscles to bones
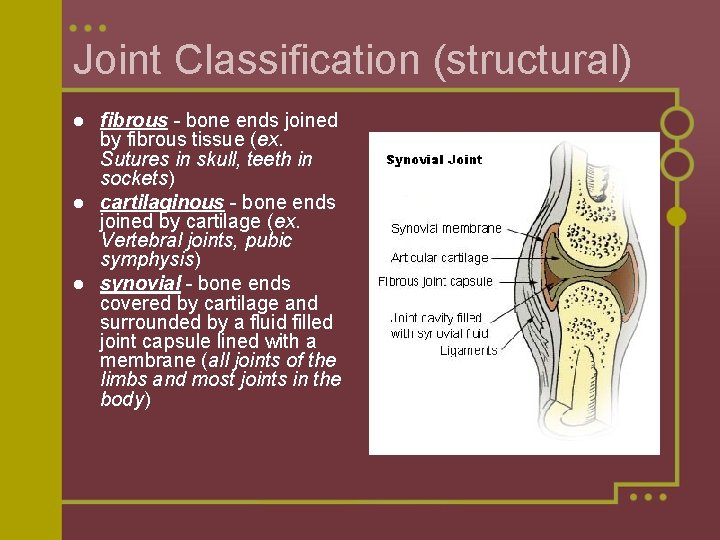
Joint Classification (structural) fibrous - bone ends joined by fibrous tissue (ex. Sutures in skull, teeth in sockets) l cartilaginous - bone ends joined by cartilage (ex. Vertebral joints, pubic symphysis) l synovial - bone ends covered by cartilage and surrounded by a fluid filled joint capsule lined with a membrane (all joints of the limbs and most joints in the body) l
Joint Classification (functional) Synarthroses immovable joints (ex. Sutures in skull) l Amphiarthroses slightly movable (ex. Vertebral joints) l Diarthroses movable (most joints) l
Joint Classification (functional) Synarthroses immovable joints (ex. Sutures in skull) l Amphiarthroses slightly movable (ex. Vertebral joints) l Diarthroses movable (most joints) l
Synovial joint movements and types of synovial joints Movements allowed by synovial joints l See pages 260 -263 Types of Synovial joints l Plane, pivot, hinge, condyloid, saddle, ball-and-socket l See pages 264 -265
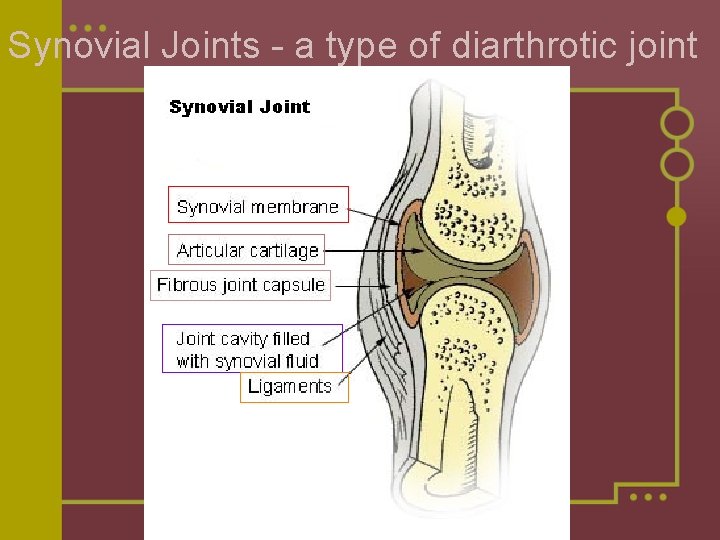
Synovial Joints - a type of diarthrotic joint
Bursae and Tendon Sheaths Function to reduce friction during joint movement l Bursae are fluid filled sacs found where ligaments, muscles, tendons, skin, and bones rub together. l Tendon sheaths wrap around tendons that are subjected to friction l
Synovial joint movements and types of synovial joints Movements allowed by synovial joints l See pages 260 -263 Types of Synovial joints l Plane, pivot, hinge, condyloid, saddle, ball-and-socket l See pages 264 -265
- Slides: 27