The Seronegative Spondyloarthropathies Surabhi A Khanna MD Assistant
The Seronegative Spondyloarthropathies Surabhi A Khanna, MD Assistant Professor of Medicine Division of Allergy, Immunology and Rheumatology
Disclosures I have no actual or potential conflict of interest in relation to this program/presentation
What are the Seronegative Spondyloarthropathies • With the discovery of rheumatoid factor (RF) in 1940 (Rose) and 1948 (Waller), and after widespread use of the test, it was realized (1950’s) not all diseases with inflamed joints were associated with a RF, hence they are seronegative. Yet these diseases were still called seronegative variants of rheumatoid arthritis until the term spondarthridities was published in 1974 after extensive family studies done in the 1960’s noted the association of several phenotypic features in common amongst these diseases. (1) • Genetically, often associated with HLA B 27 – identified in 1973 • Phenotypically - inflammatory back pain, peripheral arthritis, certain extraarticular features (they are interrelated) (1). Moll JM, Haslock I et al. Associations between ankylosing spondyloarthritis, psoriatic arthritis, Reiter’s disease, the intestinal arthropathies, and Bechet's syndrome. Baltimore: Medicine; 1974. P 343 -64.
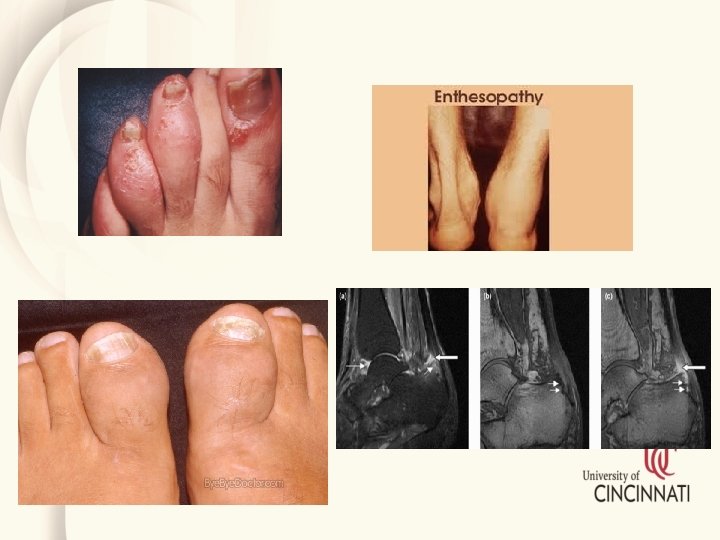
Clinical, laboratory, and imaging parameters characteristic for Sp. A These parameters comprise: • Inflammatory Bowel Disease • Enthesitis • Peripheral arthritis • Dactylitis • Acute anterior uveitis (AAU) • Family history of AS, AAU, inflammatory bowel disease (IBD), or reactive arthritis (Re. A) • Psoriasis • Good response to nonsteroidal anti-inflammatory drugs (NSAIDs) • Elevated acute phase reactants • Presence of HLA-B 27 • MRI evidence of sacroiliitis
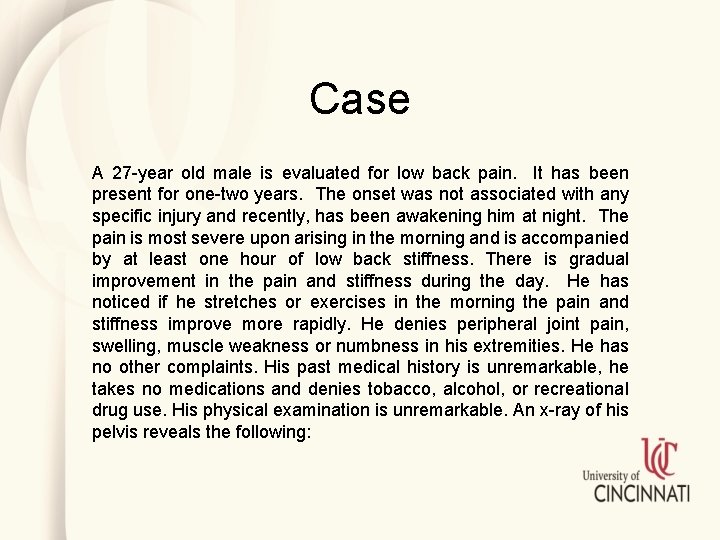
Case A 27 -year old male is evaluated for low back pain. It has been present for one-two years. The onset was not associated with any specific injury and recently, has been awakening him at night. The pain is most severe upon arising in the morning and is accompanied by at least one hour of low back stiffness. There is gradual improvement in the pain and stiffness during the day. He has noticed if he stretches or exercises in the morning the pain and stiffness improve more rapidly. He denies peripheral joint pain, swelling, muscle weakness or numbness in his extremities. He has no other complaints. His past medical history is unremarkable, he takes no medications and denies tobacco, alcohol, or recreational drug use. His physical examination is unremarkable. An x-ray of his pelvis reveals the following:
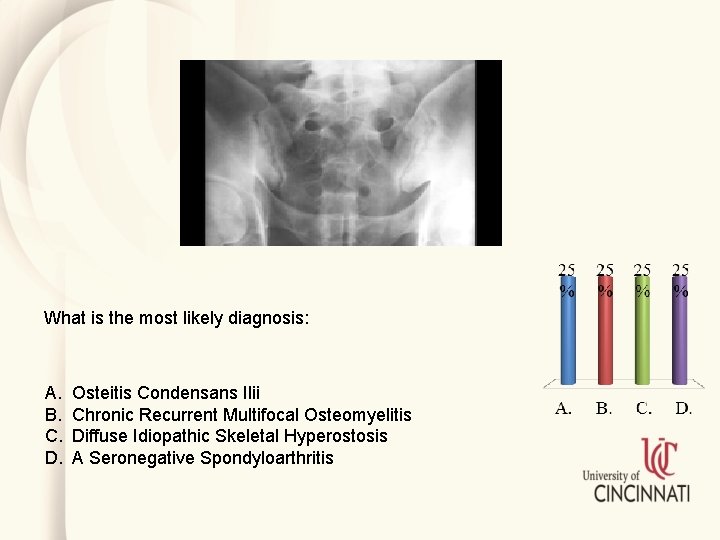
What is the most likely diagnosis: A. B. C. D. Osteitis Condensans Ilii Chronic Recurrent Multifocal Osteomyelitis Diffuse Idiopathic Skeletal Hyperostosis A Seronegative Spondyloarthritis

Inflammatory Back pain (IBP) • ASAS set of criteria for IBP – based on real cases in which 13 experts determined the parameters with the highest concordance rate (. 83) for those patients with a confirmed diagnosis of IBP. (1) 1. Age at onset younger than 40 years 2. Insidious onset 3. Improvement with exercise 4. No improvement at rest 5. Pain at night (improvement on getting up) Sensitivity of 77% and specificity of 91. 7% that IBP is present in your patient if 4/5 parameters are met Sieper J et al. New criteria for inflammatory back pain in patients with chronic back pain: a real patient exercise of the ASAS Ann Rheum Dis 2009; 68: 784 -8.
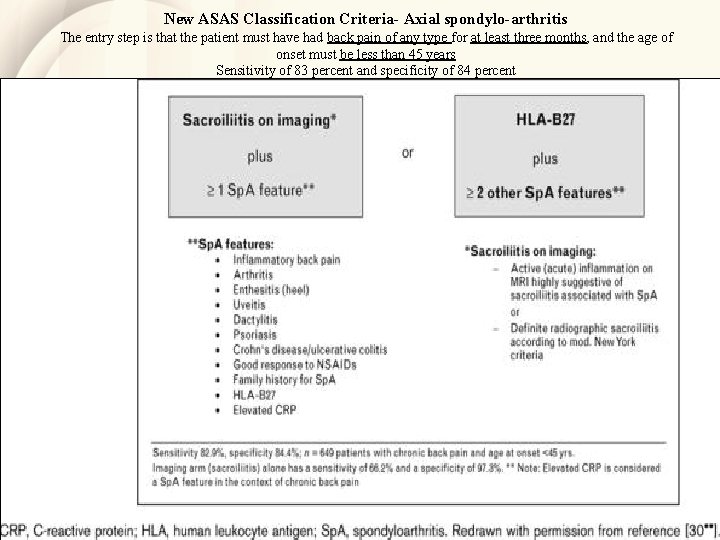
New ASAS Classification Criteria- Axial spondylo-arthritis The entry step is that the patient must have had back pain of any type for at least three months, and the age of onset must be less than 45 years Sensitivity of 83 percent and specificity of 84 percent sensitivity 82. 9% and specificity 84. 4%
Peripheral spondyloarthritis • For classification as having peripheral Sp. A, the patient should NOT have concurrent inflammatory back pain • the ASAS classification criteria for peripheral Sp. A had a sensitivity of 78 percent and a specificity of 83 percent
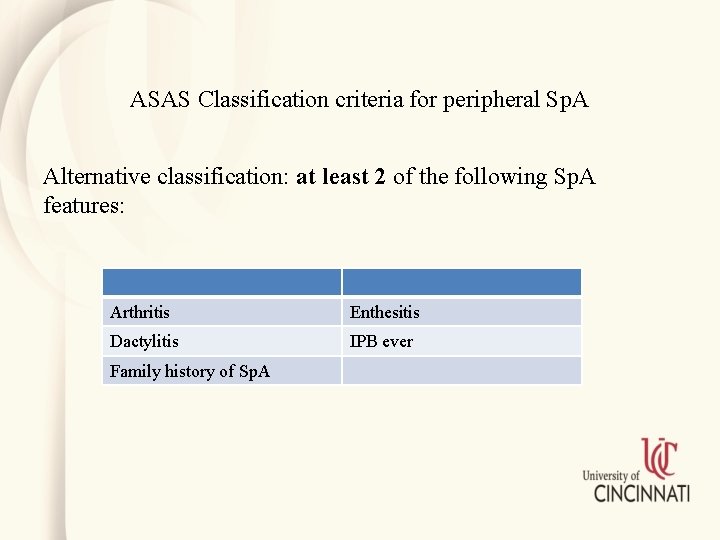
ASAS Classification criteria for peripheral Sp. A Alternative classification: at least 2 of the following Sp. A features: Arthritis Enthesitis Dactylitis IPB ever Family history of Sp. A
Seronegative Spondylarthropathies • • Ankylosing spondylitis (AS) Non-radiographic axial Sp. A (nr-ax. Sp. A) Peripheral Sp. A associated with psoriasis or psoriatic arthritis Sp. A associated with Crohn disease and ulcerative colitis Reactive arthritis (formerly called Reiter syndrome) Juvenile-onset Sp. A Copyright © 1972 -2004 American College of Rheumatology Slide Collection. All rights reserved.
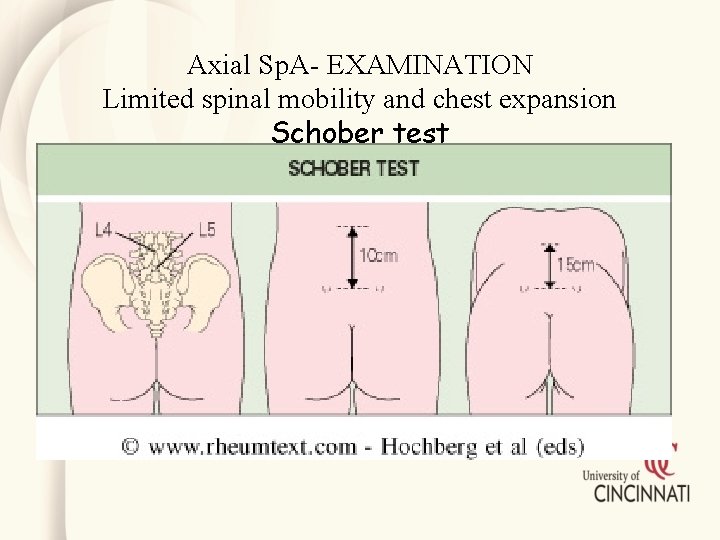
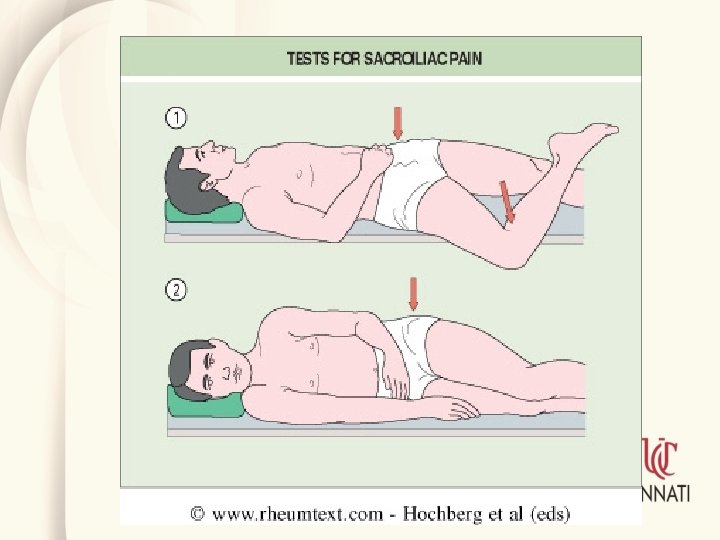
Axial Sp. A- EXAMINATION Limited spinal mobility and chest expansion Schober test
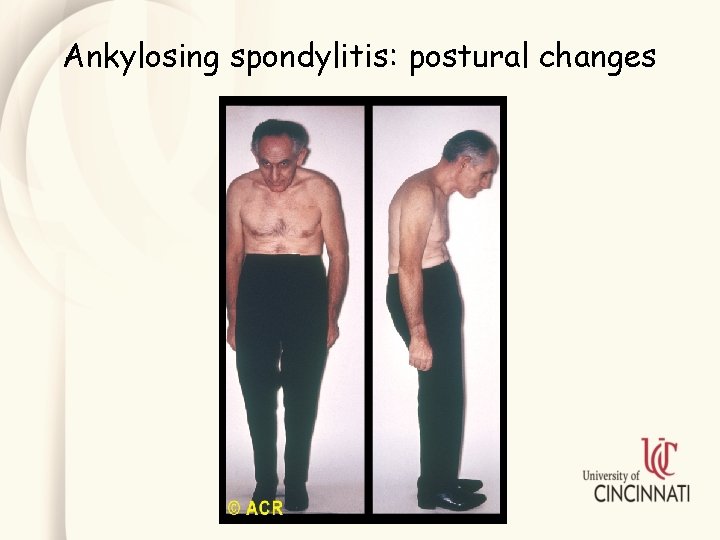
Ankylosing spondylitis: postural changes
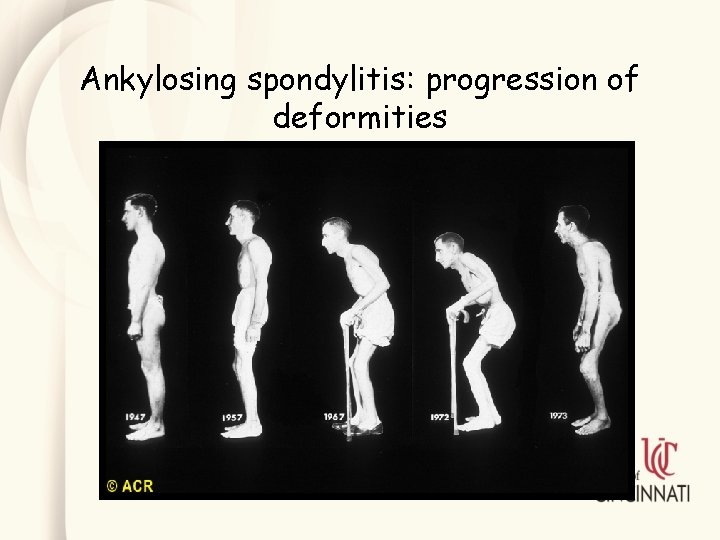
Ankylosing spondylitis: progression of deformities

Ankylosing spondylitis: early sacroiliitis
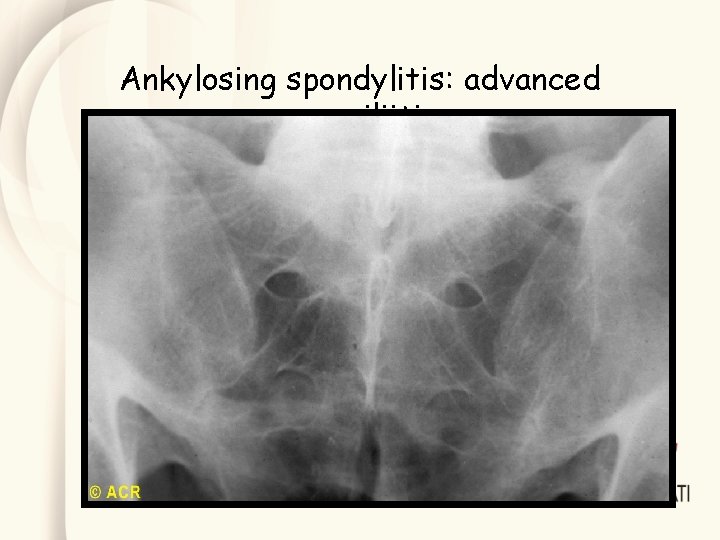
Ankylosing spondylitis: advanced sacroiliitis

Ankylosing spondylitis: thoracic and lumbar vertebrae "squaring, " osteopenia, and ossification
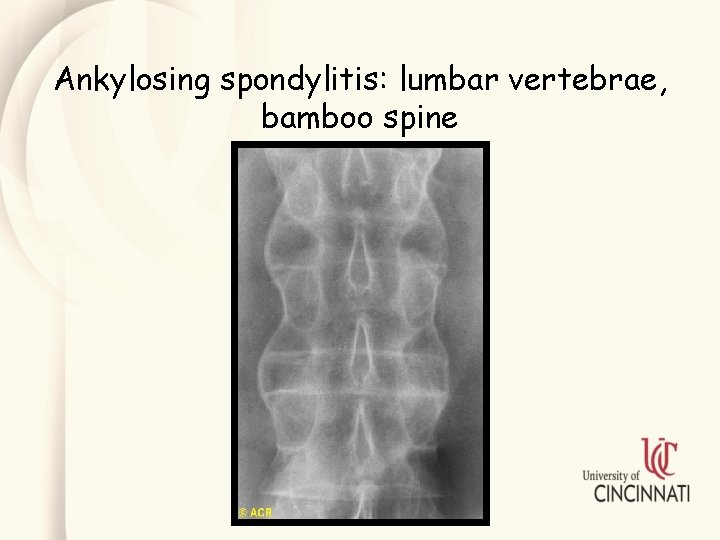
Ankylosing spondylitis: lumbar vertebrae, bamboo spine

Case A 29 y/o female comes to your office with a 6 month history of right heel pain. She notices it first thing getting out of bed in the morning but on occasion, it has awakened her during the night. It improves after thirty minutes of activity or a warm shower. She is an avid runner and although the heel may be painful when she starts her runs, it has not interfered with the half marathon training schedule she has been following lately. She ran on a cross country team in college but had to drop out her senior year when her left knee inexplicably became swollen for a several month period of time. She currently denies morning stiffness, back or buttock pain, any painful or swollen joints. She has no history of eye pain or redness, skin rashes, or problems with her bowels. Physical examination is unremarkable except for mild tenderness of her right heel at the insertion point of the Achilles tendon. You prescribe naproxen 500 mg bid. She calls your office three weeks later complaining of abdominal pain accompanied by several bowel movements per day. Her only other new complaint is sporadic mouth sores. You recommend which of the following:
You recommend which of the following: A. A. Stopping the naproxen and referral to allergist possible NSAID allergy B. Stopping the naproxen and switching to Tylenol C. Stopping the naproxen and referral to gastroenterology for a colonoscopy D. No change in her current management
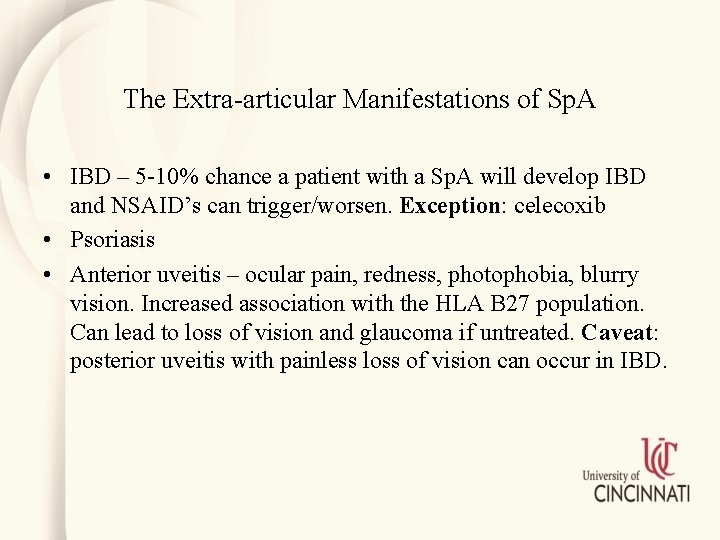
The Extra-articular Manifestations of Sp. A • IBD – 5 -10% chance a patient with a Sp. A will develop IBD and NSAID’s can trigger/worsen. Exception: celecoxib • Psoriasis • Anterior uveitis – ocular pain, redness, photophobia, blurry vision. Increased association with the HLA B 27 population. Can lead to loss of vision and glaucoma if untreated. Caveat: posterior uveitis with painless loss of vision can occur in IBD.

Ankylosing spondylitis: iridocyclitis with synechiae
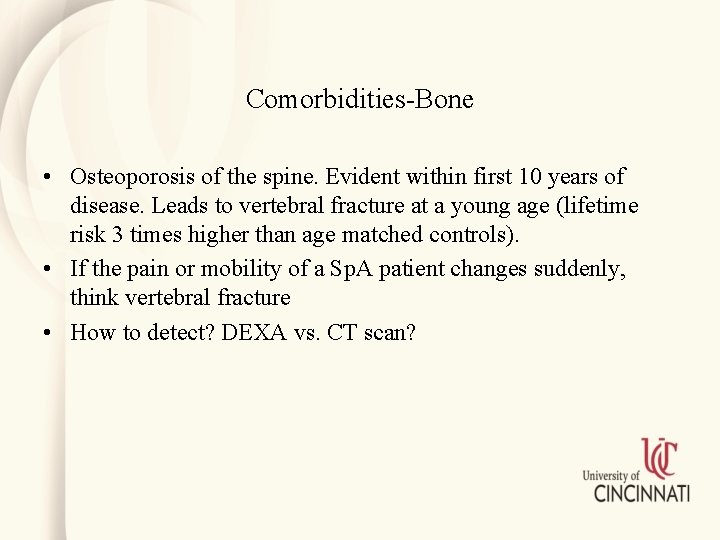
Comorbidities-Bone • Osteoporosis of the spine. Evident within first 10 years of disease. Leads to vertebral fracture at a young age (lifetime risk 3 times higher than age matched controls). • If the pain or mobility of a Sp. A patient changes suddenly, think vertebral fracture • How to detect? DEXA vs. CT scan?

Comorbidities-Neurologic • 11 x higher risk of spinal cord injury than general population especially with vertebral fracture • Atlanto-axial subluxation • Cauda equina – actually rare complication of longstanding disease.
Comorbidities-cardiovascular Axial specific • Aortic regurgitation 1%-10%, less commonly mitral valve involvement • ? Conduction disturbances – old literature, yes, newer literature, association less clear • LV dysfunction
Comorbidities-cardiovascular Atherosclerotic disease Likely traditional risk factors – dyslipidemia, smoking, metabolic syndrome etc. play a role and some may even be increased in subsets of disease Inflammation also likely plays a role Use of NSAID’s?
Comorbidities-other • Pulmonary – restrictive lung disease in those with significant spinal involvement, apical fibrosis • Renal – uncommon but amyloidosis and Ig. A nephropathy have been described in the predominantly axial variants
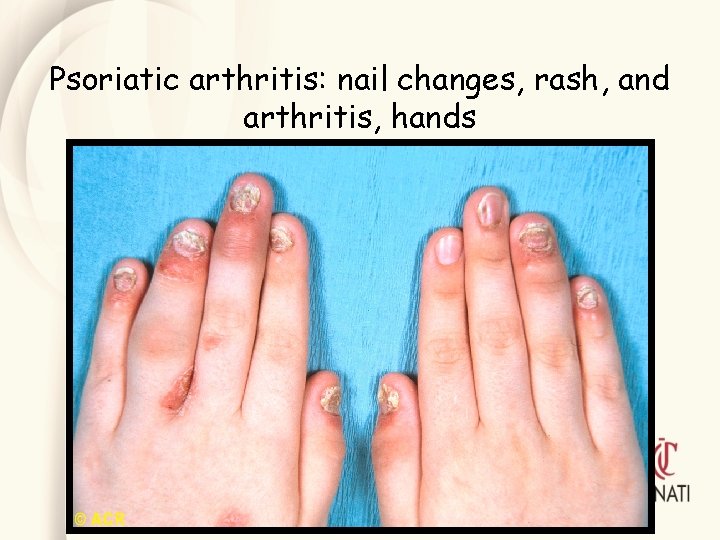
Psoriatic arthritis: nail changes, rash, and arthritis, hands

Psoriatic arthritis: nail changes, rash, and arthritis, hands

Psoriatic arthritis: hands

Psoriatic arthritis: nail dystrophy and arthritis
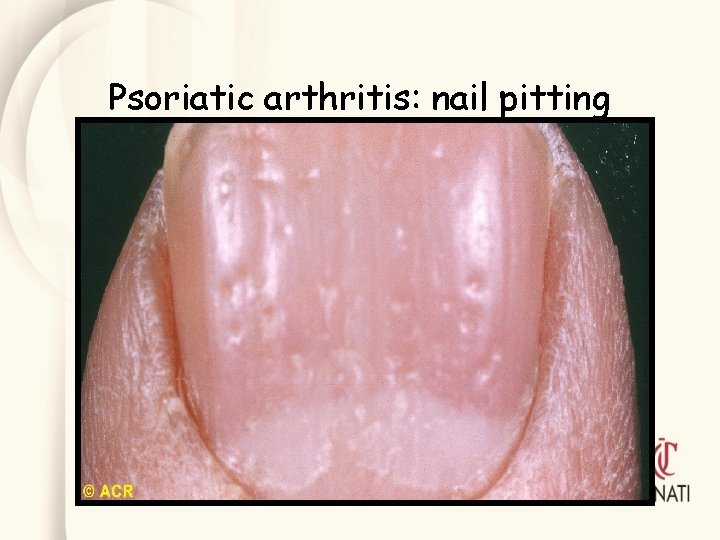
Psoriatic arthritis: nail pitting

Psoriatic arthritis: “sausage” digits and rash

Psoriatic arthritis: hand

Psoriatic arthritis: progressive joint changes

• Reactive arthritis ~ 50% cases can be attributed to a specific pathogen (serologies and cultures) – Chlamydia – Salmonella – Shigella – Yersinia – Campylobacter • Usually, lower extremities, asymmetric, oligoarticular pattern • Dactylitis (sausage digit) in the feet is typical • Cutaneous manifestations: keratoderma blenorrhagicum and circinate balanitis

Reactive arthritis: tendinitis, heels
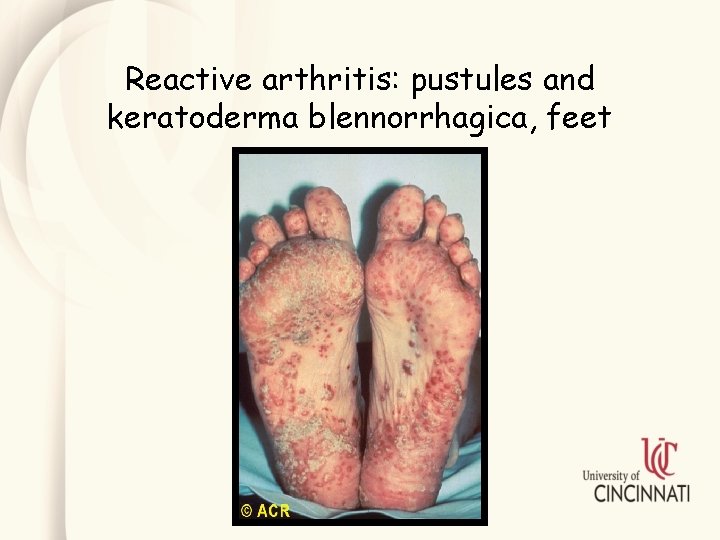
Reactive arthritis: pustules and keratoderma blennorrhagica, feet
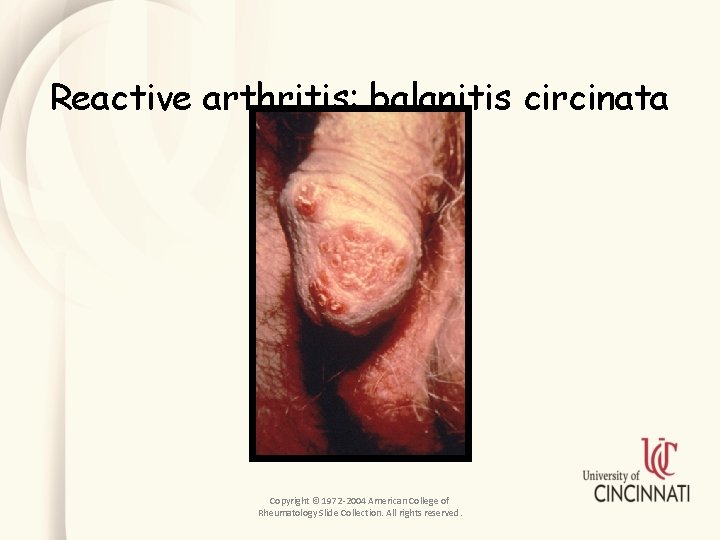
Reactive arthritis: balanitis circinata Copyright © 1972 -2004 American College of Rheumatology Slide Collection. All rights reserved.
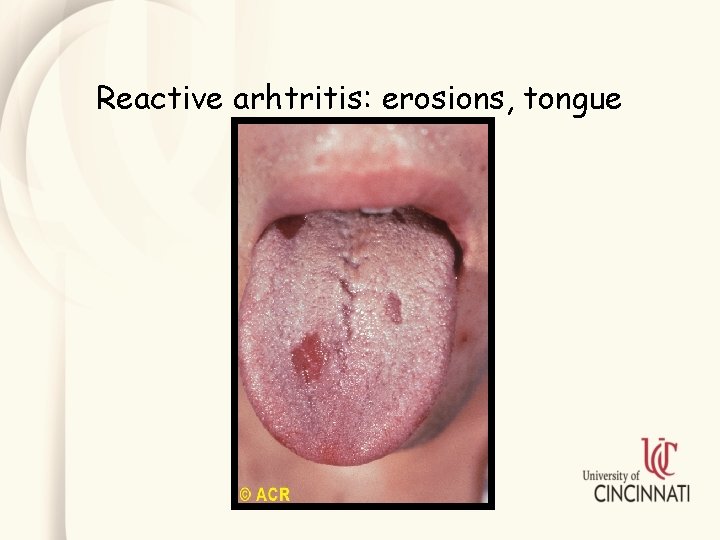
Reactive arhtritis: erosions, tongue

Reactive arthritis: conjunctivitis

Case • A 35 -year-old woman who works in a nursing home develops acute abdominal pain and bloody diarrhea. Many residents of the nursing home developed a similar disorder. Several weeks later, she complains of diffuse musculoskeletal pain involving the neck, left wrist, left knee, and low back. On examination she has marked swelling, warmth, and loss of motion of the left wrist and left knee, as well as pain and restricted motion of the neck and lower lumbar spine. • A diagnosis of reactive arthritis is strongly suspected.

Which one of the following statements is most likely to be true of this patient? A. B. C. D. E. Her gastroenteritis was caused by Escherichia coli. Her arthritis will likely resolve completely within 4 to 6 months, without complications. Antibiotic treatment of the underlying infection would have prevented her arthritis. Shigella flexneri, more than any other organism associated with reactive arthritis, is predictive of a recurrent course. Neisseria gonorrhoeae, more than any other organism associated with reactive arthritis, is predictive of a recurrent course.

IBD related arthritis Remember: joint disease may preceed the inflammatory bowel disease!!!
IBD related arthritis- peripheral • Type I arthropathy — tends to be acute, pauc-iarticular, often associated with IBD flares, occurs early in the course of IBD, is self-limiting (90 percent under 6 months), and does not result in joint deformities – Most commonly affects knee – 5% of IBD patients develop type 1 arthropathy – Joint s/s may occur prior to onset of symptoms suggestive of IBD • Type II arthropathy — polyarticular disease – MC-MCP joints – Often migratory arthritis. – Active synovitis may persist for months, and may recur repeatedly – Episodes of exacerbations and remissions may continue for years. – Affects 3 to 4 percent of patients with IBD – Articular involvement rarely precedes the diagnosis of IBD – Joint symptoms typically do not parallel the activity of bowel disease

IBD associated arthritis- Axial • • • Spondylitis occurs in 1 to 26 percent of patients with IBD More common in males Back s/s may be unrelated to those of GI disease Asymptomatic sacroiliitis, detected by radiography, occurs in 4 to 18 percent of patients with IBD. Sacroiliitis in patients with Crohn's disease is strongly associated with CARD 15 gene polymorphisms Radiographs of the spine and pelvis may show typical findings of ankylosing spondylitis and sacroiliitis

A word about therapy: Despite attempts to alter classification of these diseases and potentially the terminology for diagnosis – treatment, including treatment guidelines being developed for these diseases, still divides the treatment into the traditional Categories of Ankylosing Spondylitis vs. Psoriatic Arthritis vs Crohns etc. The focus here is the axial vs. peripheral arthritis

Which of the following medication reduces radiographic progression of spinal disease in Sp. A? A. B. C. D. Methotrexate Celecoxib Sulfasalazine Corticosteroids
Therapy of Axial Spondyloarthropathy • NSAID’s are first-line therapy • Continuous therapy is needed • Multiple trials demonstrating clinical efficacy – all NSAID’s appear equally efficacious if given at full anti-inflammatory dose • NSAID’s have been shown to decrease CRP and decrease radiographic progression • Recommendation: determine NSAID therapy based on level of pain and stiffness. Risk for radiographic progression is considered secondary. Full dose continuous NSAID therapy is first line of treatment
Therapy of Axial Spondyloarthropathy • TNFi’s – Second line therapy after NSAID (NSAID failure) • Initial studies of two years duration failed to show inhibition of radiographic progression despite dramatic improvement in clinical symptoms and elevated inflammatory markers • TNFI’s studies of four or more years of therapy do demonstrate up to a 50% reduction in radiographic progression • Efficacy better in early vs late disease
Therapy of Axial Spondyloarthropathy • If fail one TNFi, try a second agent • In 2016 Secukinumab, a fully humanized monoclonal antibody that binds IL 17 A released by activated Th 17 cells, was FDA approved for use is 3 specific subsets of Sp. A (psoriasis, ankylosing spondylitis and psoriatic arthritis) • Good 2 year clinical efficacy data

Treatment of Peripheral Spondyloarthritis Traditional disease-modifying rheumatic agents Sulfasalazine Methotrexate Cyclosporine Leflunomide All help peripheral arthritis, none help dactylitis or enthesitis, ? Methotrexate reduces radiographic progression
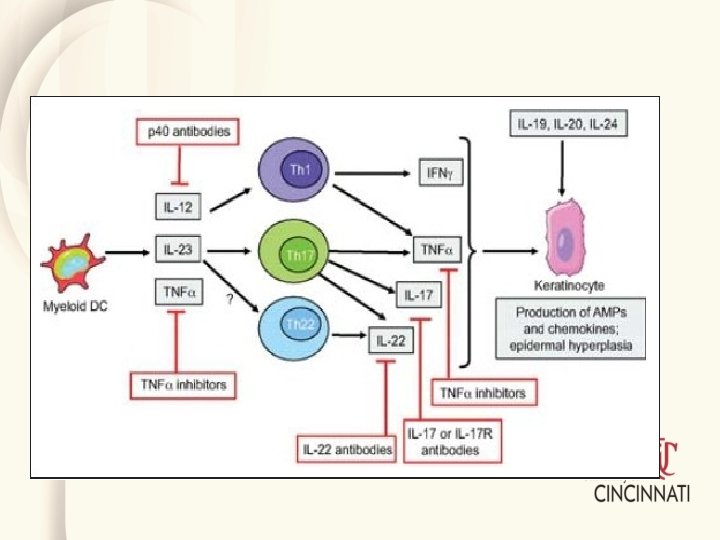
Treatment of Peripheral Spondyloarthritis Biologic Therapy TNFi’s – clinical symptoms and structural damage Ustekinumab – blocks IL 12 and IL 23, clinical symptoms and structural damage, works better in TNFi naïve patients Secukinumab Others is development
Treatment of Peripheral Spondyloarthritis Small Molecules – targeted synthetic disease-modifying antirheumatic therapy Apremilast - inhibits phosphodiesterase 4,

Thank you
- Slides: 58