The sensory system and pain syndromes Vth year
- Slides: 53
The sensory system and pain syndromes Vth year, dentistry, 30. 09. 2008 Department of Neurology Semmelweis University
Sensory system Receptors: - specialised (smell, vision, hearing, taste - visceral (viscera, smooth muscle unconscious or autonomic) - somatic (skin, striated muscle, joints)
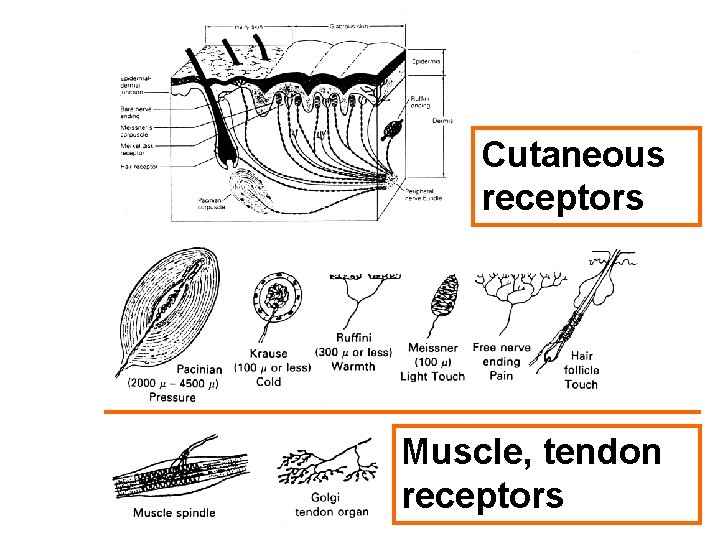
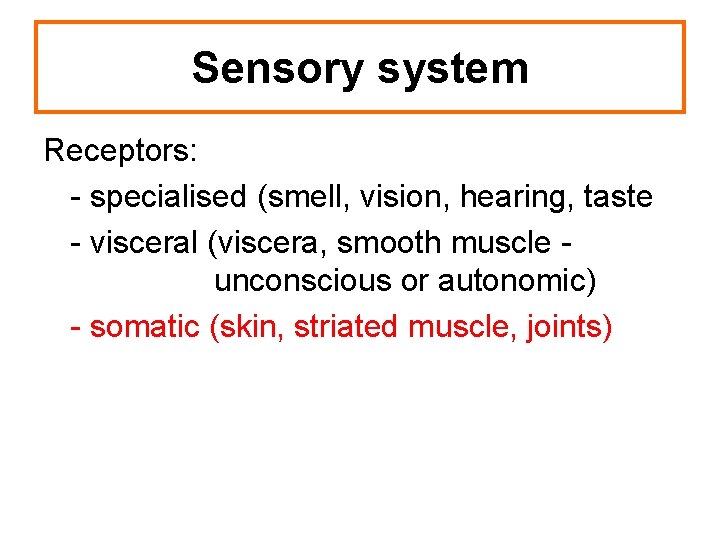
Cutaneous receptors Muscle, tendon receptors
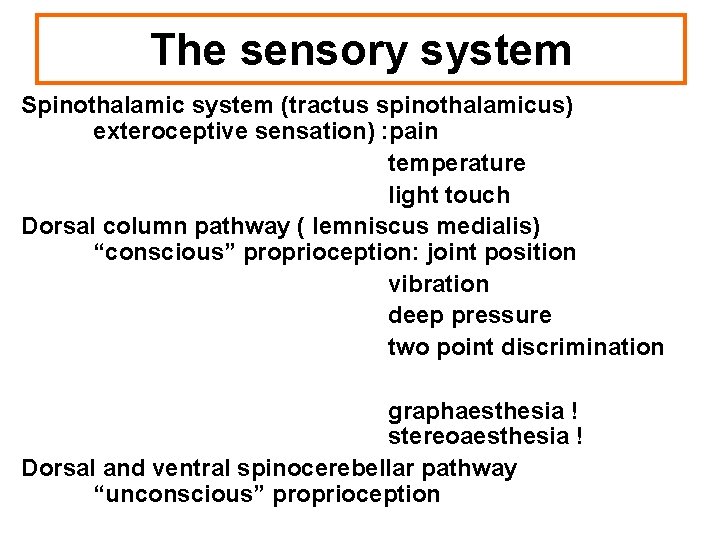
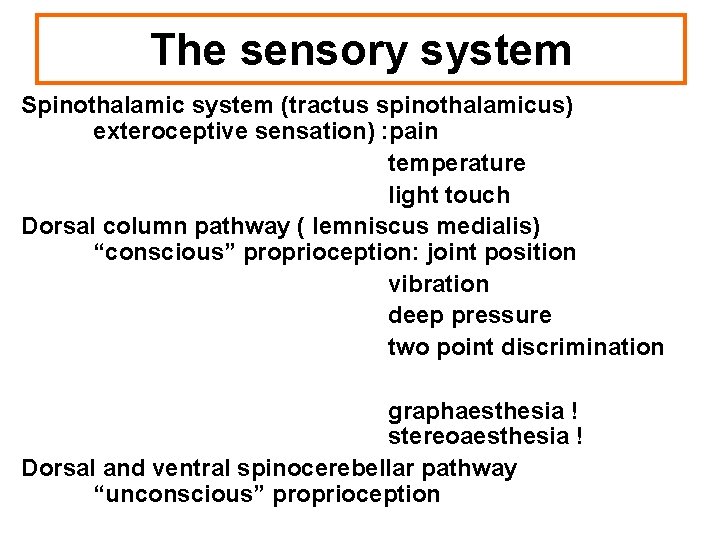
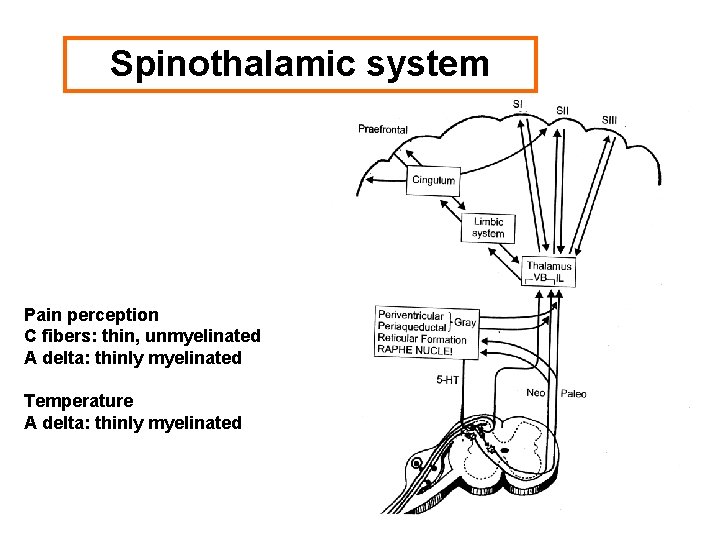
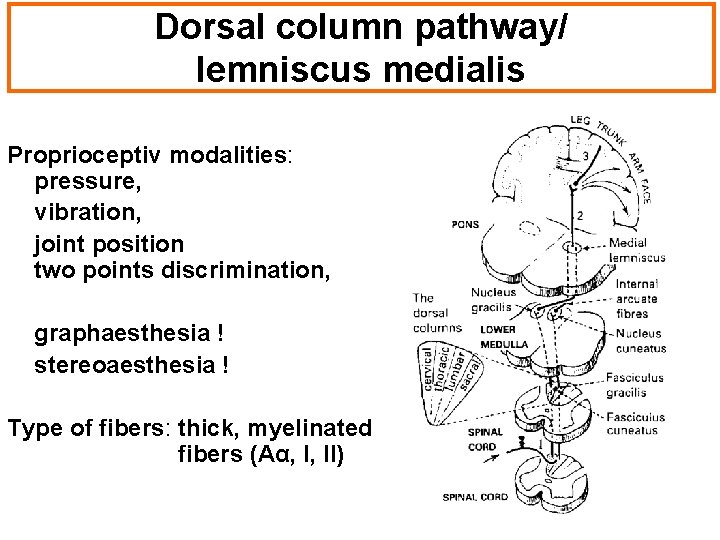
The sensory system Spinothalamic system (tractus spinothalamicus) exteroceptive sensation) : pain temperature light touch Dorsal column pathway ( lemniscus medialis) “conscious” proprioception: joint position vibration deep pressure two point discrimination graphaesthesia ! stereoaesthesia ! Dorsal and ventral spinocerebellar pathway “unconscious” proprioception
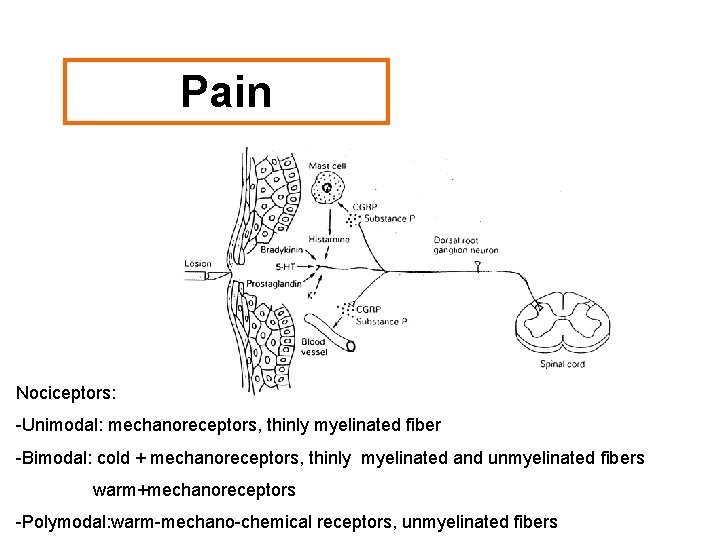
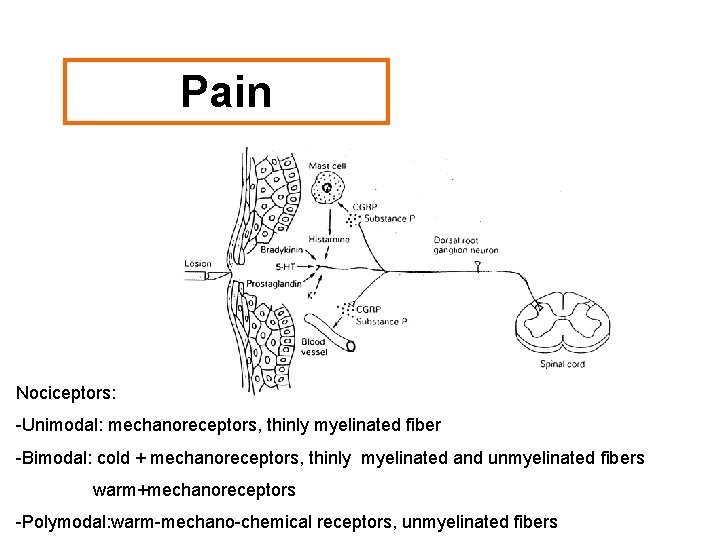
Pain Nociceptors: -Unimodal: mechanoreceptors, thinly myelinated fiber -Bimodal: cold + mechanoreceptors, thinly myelinated and unmyelinated fibers warm+mechanoreceptors -Polymodal: warm-mechano-chemical receptors, unmyelinated fibers
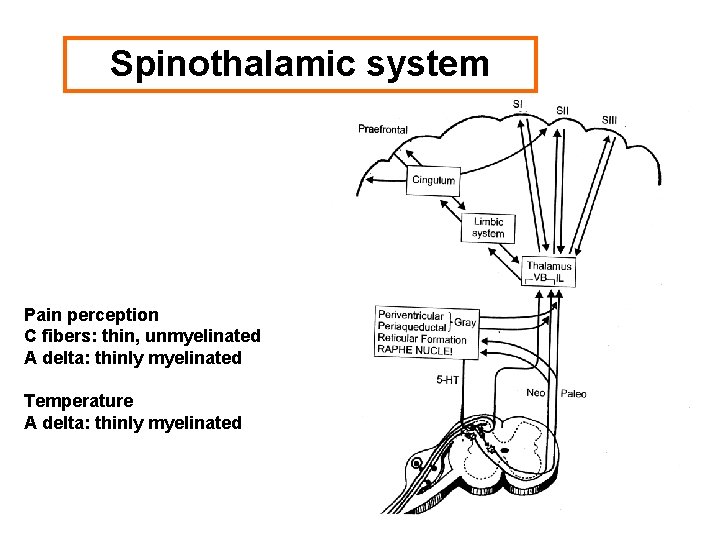
Spinothalamic system Pain perception C fibers: thin, unmyelinated A delta: thinly myelinated Temperature A delta: thinly myelinated
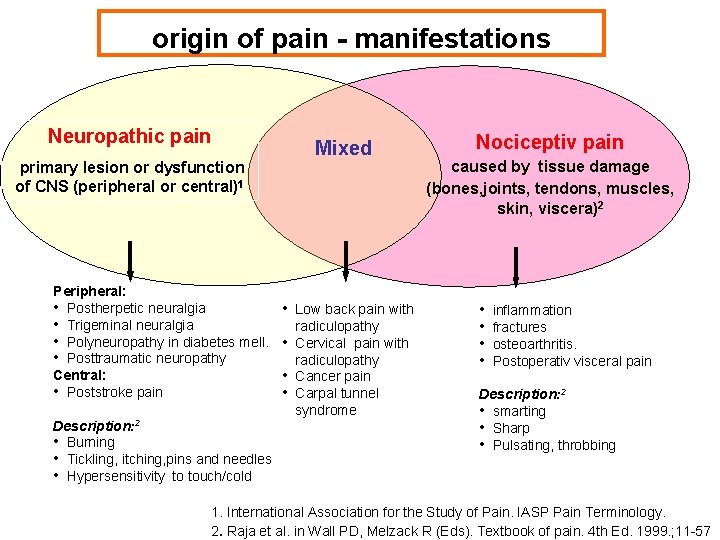
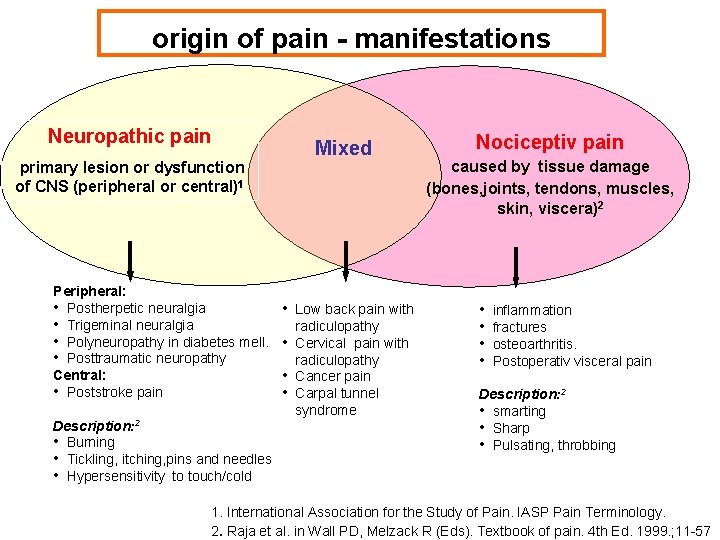
origin of pain - manifestations Neuropathic pain Mixed primary lesion or dysfunction of CNS (peripheral or central)1 Peripheral: • Postherpetic neuralgia • Trigeminal neuralgia • Polyneuropathy in diabetes mell. • Posttraumatic neuropathy Central: • Poststroke pain Description: 2 • Burning • Tickling, itching, pins and needles • Hypersensitivity to touch/cold • Low back pain with • • • radiculopathy Cervical pain with radiculopathy Cancer pain Carpal tunnel syndrome Nociceptiv pain caused by tissue damage (bones, joints, tendons, muscles, skin, viscera)2 • • inflammation fractures osteoarthritis. Postoperativ visceral pain Description: 2 • smarting • Sharp • Pulsating, throbbing 1. International Association for the Study of Pain. IASP Pain Terminology. 2. Raja et al. in Wall PD, Melzack R (Eds). Textbook of pain. 4 th Ed. 1999. ; 11 -57
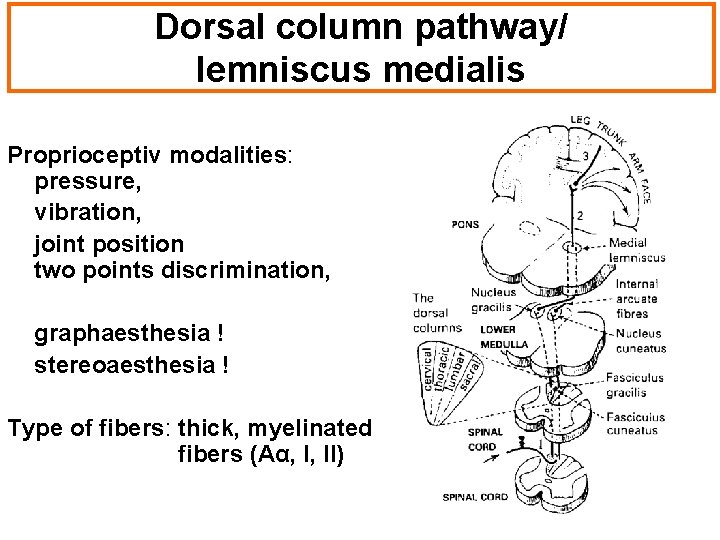
Dorsal column pathway/ lemniscus medialis Proprioceptiv modalities: pressure, vibration, joint position two points discrimination, graphaesthesia ! stereoaesthesia ! Type of fibers: thick, myelinated fibers (Aα, I, II)
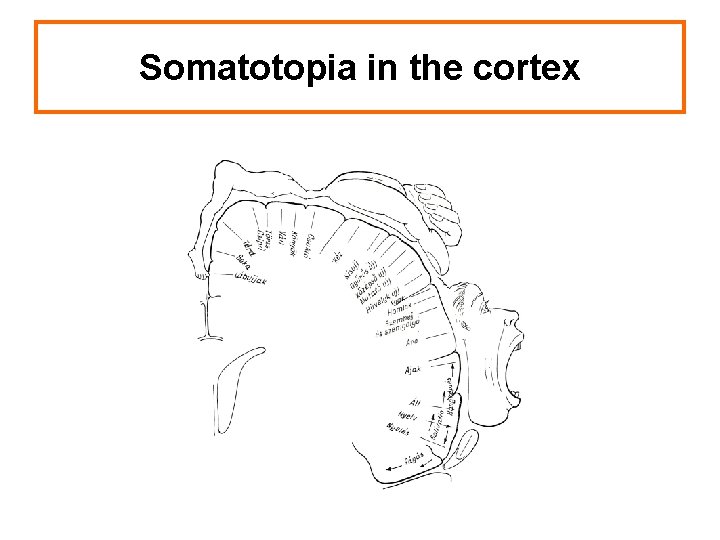
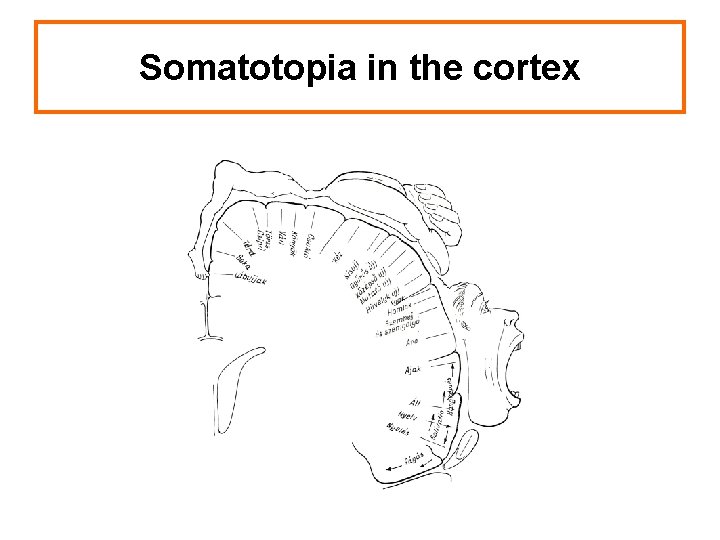
Somatotopia in the cortex
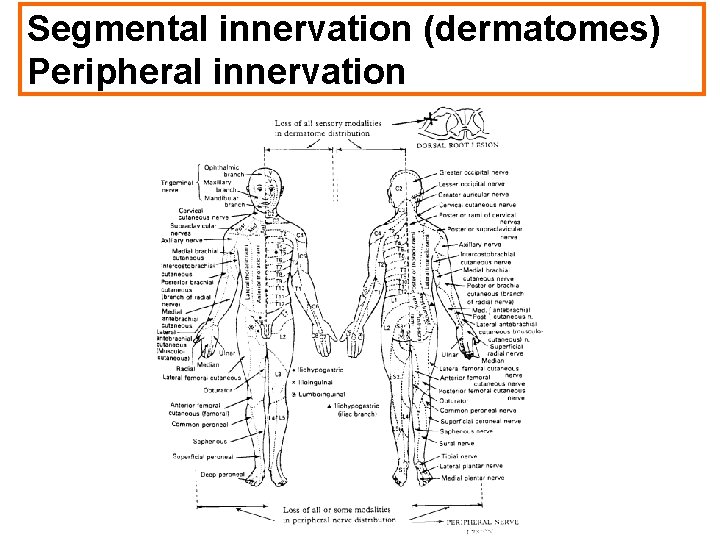
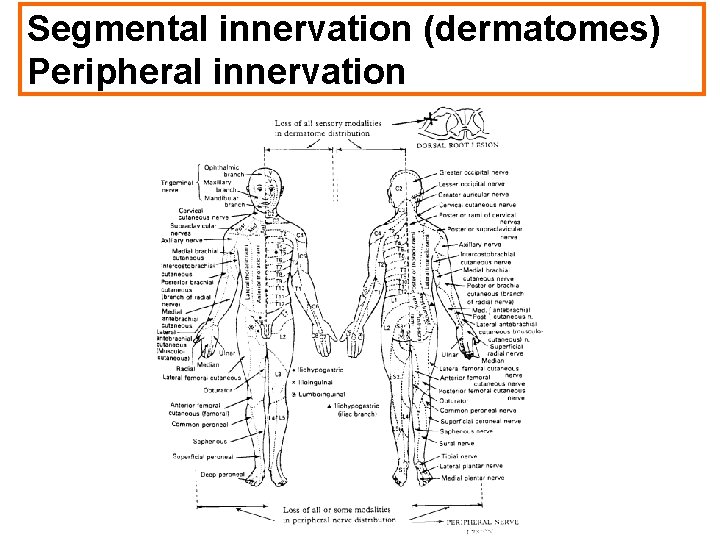
Segmental innervation (dermatomes) Peripheral innervation
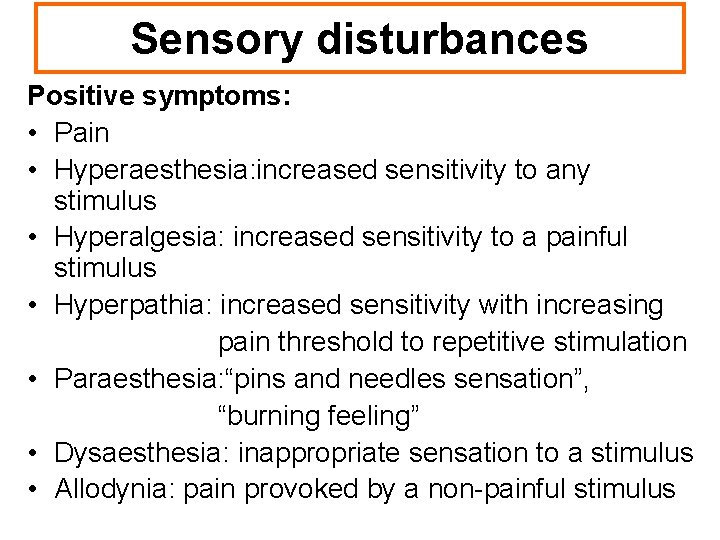
Sensory disturbances Positive symptoms: • Pain • Hyperaesthesia: increased sensitivity to any stimulus • Hyperalgesia: increased sensitivity to a painful stimulus • Hyperpathia: increased sensitivity with increasing pain threshold to repetitive stimulation • Paraesthesia: “pins and needles sensation”, “burning feeling” • Dysaesthesia: inappropriate sensation to a stimulus • Allodynia: pain provoked by a non-painful stimulus
Sensory disturbances Negative symptoms: • Hypoalgesia: reduced sensitivity to a painful stimulus • Hypoesthesia: reduced sensitivity to any stimulus • Analgesia: absent sensitivity to a painful stimulus • Anaesthesia: absent sensitivity to any stimulus
Examination of the sensory system 1. Special standpoints: • “Subjective “ examination • Requires good cooperation on the patient`s side. • Allows accurate localisation of the pathology. • Preliminary diagnosis is needed. Examine according to the expected damage ! • Most often we compare different parts of the body. • Do not tell the patient what should be felt ! • The patient should not see the examined part of the body ! • “Subjective” sensory disturbance ( pain, paraesthesia ) is not necessarily accompanied by “objective” sensory disturbance (hypaesthesia, anaesthesia )
Examination of the sensory system 2. Pain: pin prick, tooth picks Light touch: use a wisp of cotton wool ! Temperature: use cold (5 -10 0 C)/or hot (40 -45 0 C) test tubes ! -Instruct the patient to reply: “Tell me if you feel the stimulus ! Name the area stimulated !” “Is it equal on both sides? -Map out the extent of abnormality by moving from the abnormal to the normal area (“Tell me if sensation changes!”) Joint position / motion: -Hold the sides of the patient’s finger ! Move it up and down at random ! Ask to specify the direction of movement ! Vibration: -Place a vibrating tuning fork on a bony prominence ( ankle, knee, processus spinosus, processus styloideus radii et ulnae, elbow, clavicula)
Examination of the sensory system 3. • Two point discrimination: -The ability to discriminate two blunt points when applied simultaneously. (3 -5 mm on the finger, 4 -7 cm on the trunk) • Sensory inattention (perceptual rivalry) -The ability to detect sensory stimuli applied simultaneously on both limbs. -Subdominant parietal lobe, associative areas • Stereoaesthesia - An object is placed in the patient’s hand. - Ask patient to describe its size, shape, surface, material ! - Stereoanaesthesia: disturbance of the sensory afferent tracts.
Examination of the sensory system 4. • Astereognosis. -Inability to identify an object by palpation -The primary sense data being intact -Lesion of the opposite hemisphere, postcentral gyrus • Tactile agnosia : -The patient is unable to recognize an object by touch in both hands -Disorder of perception of symbols. -Lesion of the dominant parietal lobe, associative areas • Graphaesthesia - The ability to recognize numbers or letters traced out on the palm.
Examination of the sensory system • Nerve conduction studies: sensory antidrom neurography median nerve, ulnar nerve • Somatosensory evoked potentials (SEP) median nerve, tibial nerve
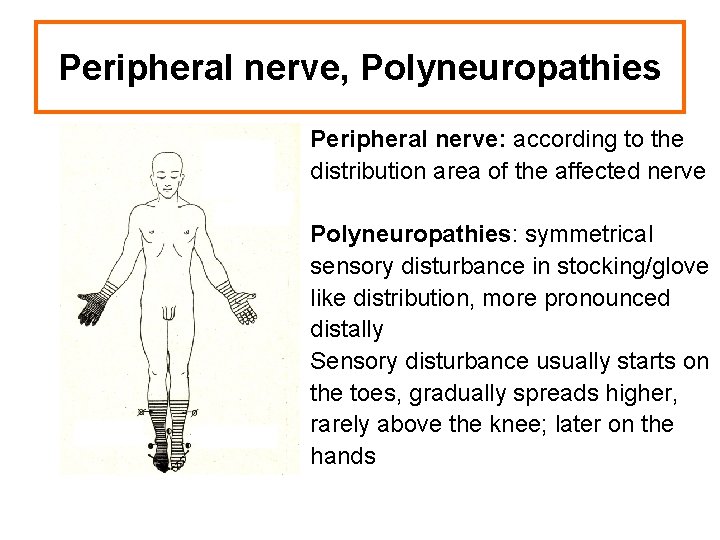
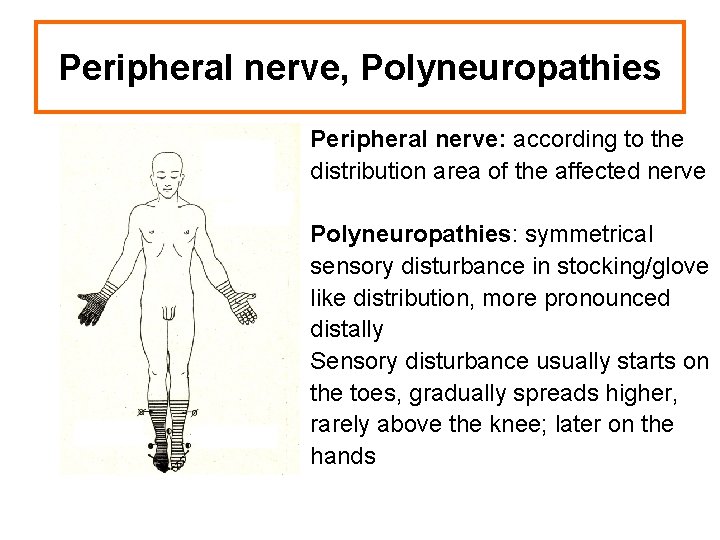
Peripheral nerve, Polyneuropathies Peripheral nerve: according to the distribution area of the affected nerve Polyneuropathies: symmetrical sensory disturbance in stocking/glove like distribution, more pronounced distally Sensory disturbance usually starts on the toes, gradually spreads higher, rarely above the knee; later on the hands
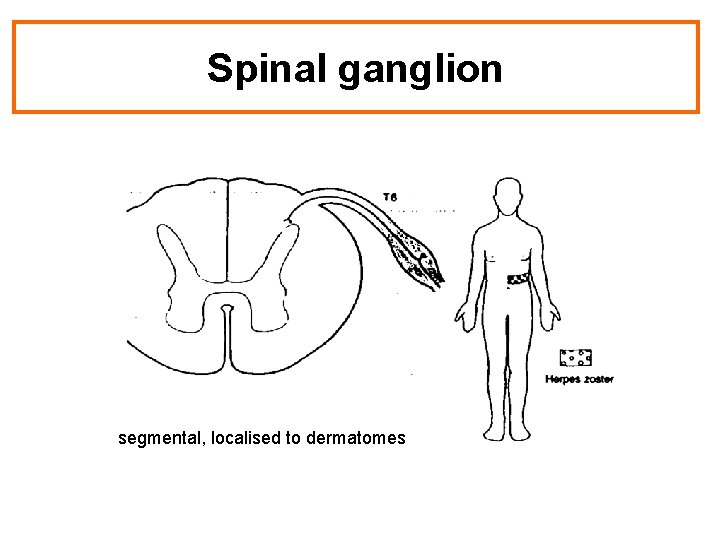
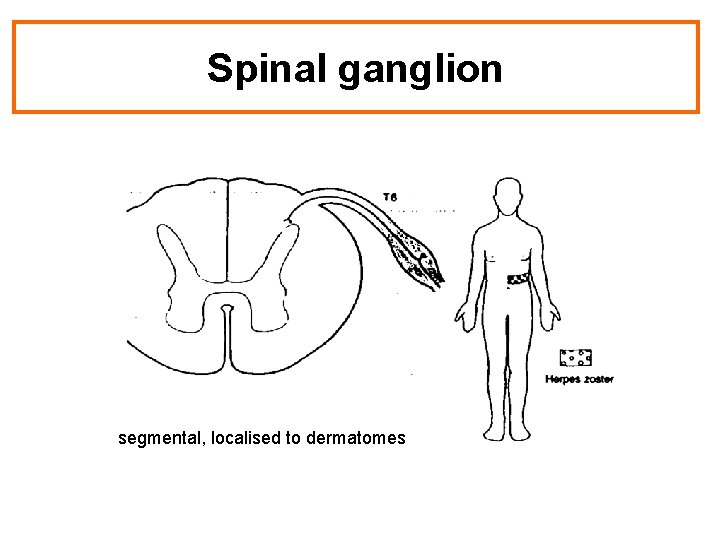
Spinal ganglion segmental, localised to dermatomes
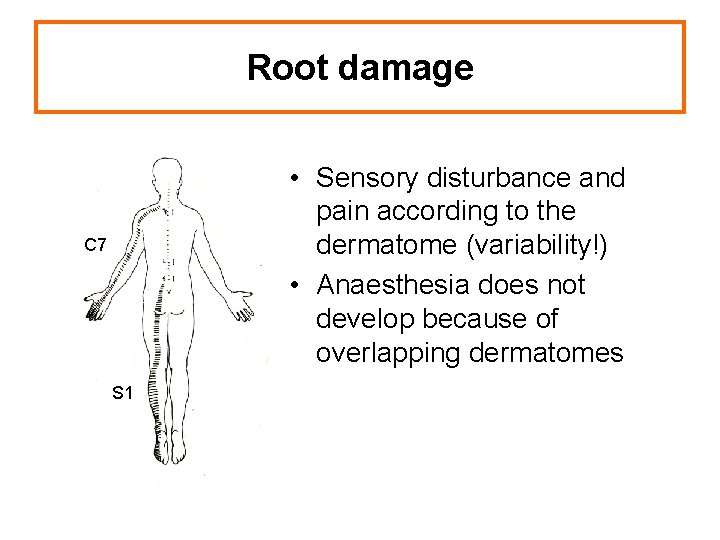
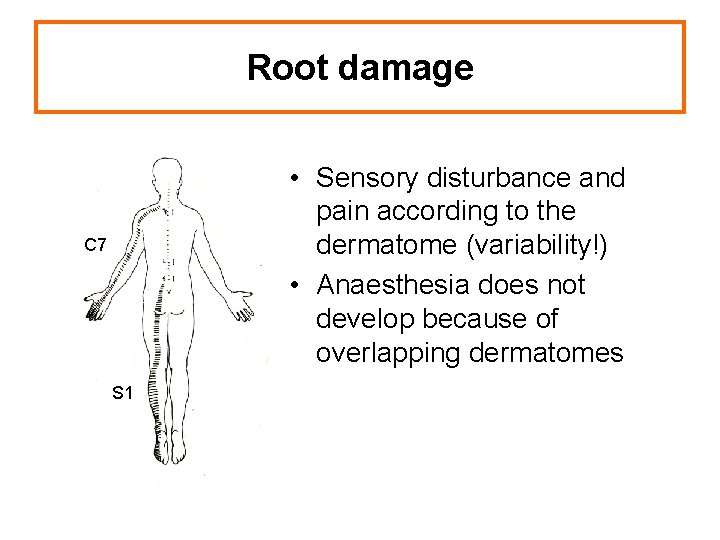
Root damage • Sensory disturbance and pain according to the dermatome (variability!) • Anaesthesia does not develop because of overlapping dermatomes C 7 S 1
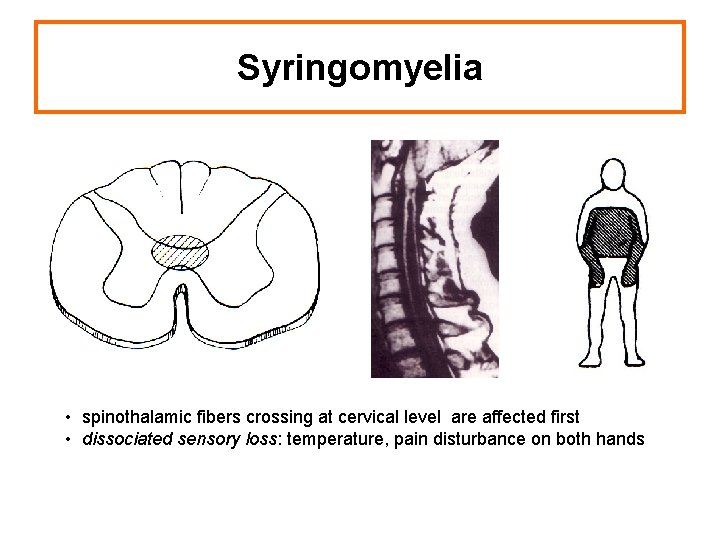
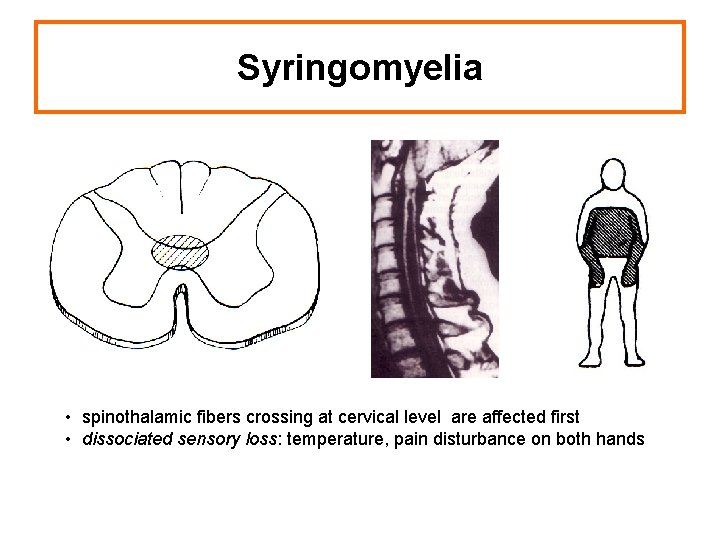
Syringomyelia • spinothalamic fibers crossing at cervical level are affected first • dissociated sensory loss: temperature, pain disturbance on both hands
Cranial structures - pain • • skull cervical spine eyes ears nose, sinuses teeth temporomandibular joint
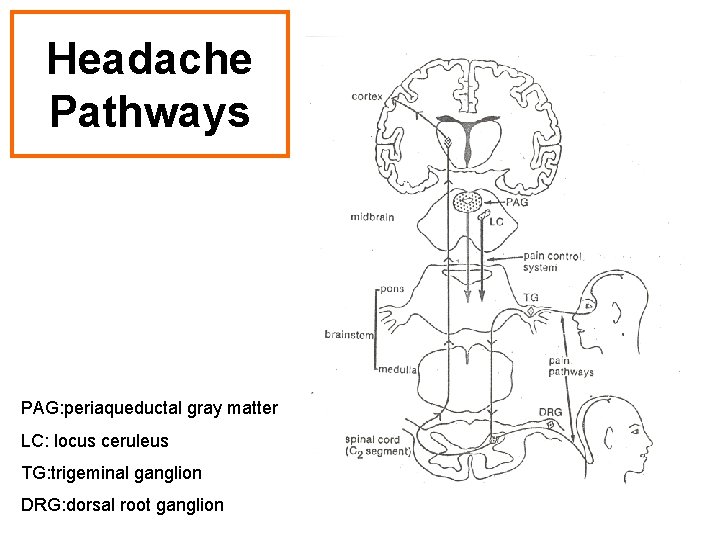
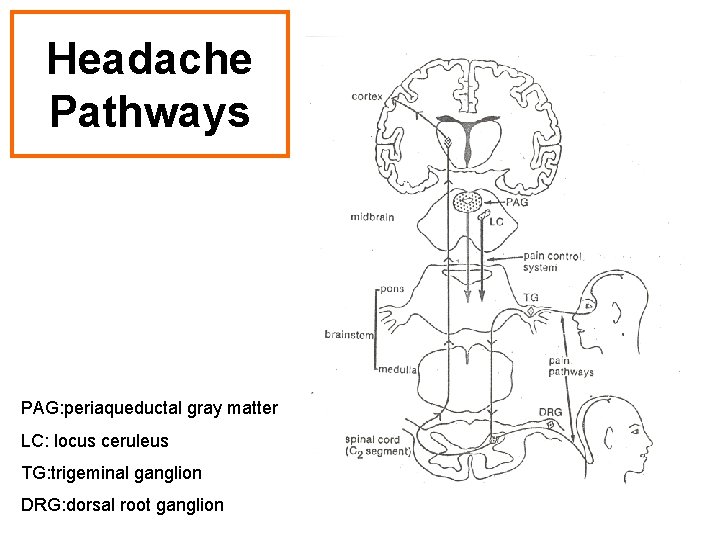
Headache Pathways PAG: periaqueductal gray matter LC: locus ceruleus TG: trigeminal ganglion DRG: dorsal root ganglion
Taking a headache history • Age of onset ? • Duration of complaint ? • Time pattern Continuous or transient ? Frequency and duration of each headache ? • Site ? • Intensity, quality ? • Associated phenomena ?
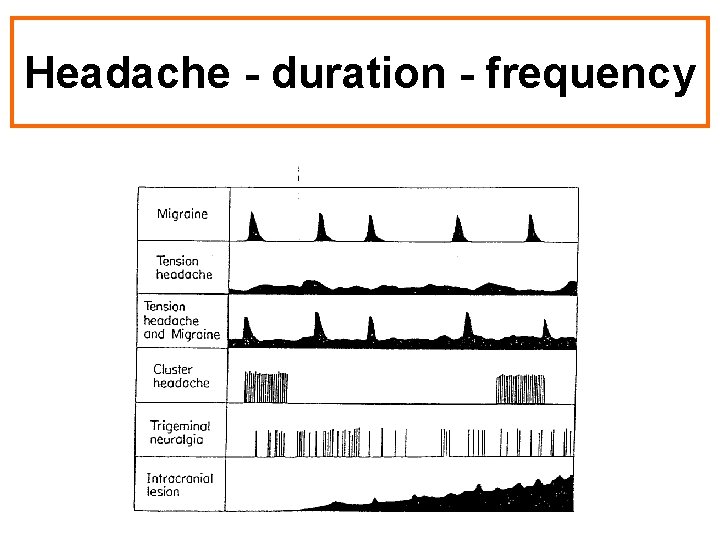
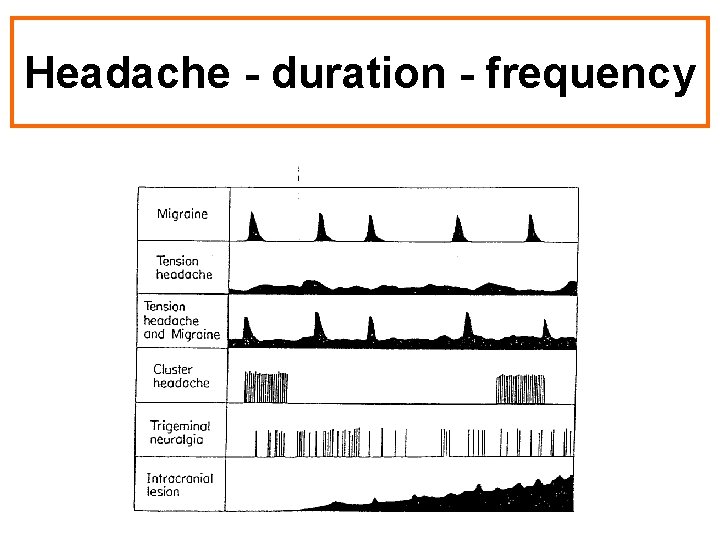
Headache - duration - frequency
Headache - „danger signals” „Danger signals”: • sudden onset of new, severe headache • onset of headache after exertion, straining, coughing or sexual activity • progressively worsening headache • any abnormality on neurological examination • systemic features: fever, arthralgia • onset of first headache after the age of 50 years Refer to specialist: • Cooperating patient – ineffective treatment • Chronic daily headache – drug abuse, dependency • Severe anxiety , depression • Severe comorbid diseases
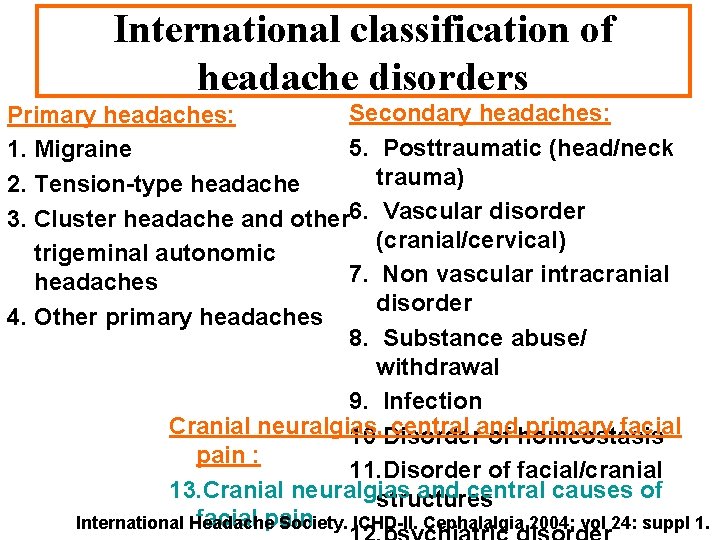
International classification of headache disorders Primary headaches: Secondary headaches: 1. Migraine 5. Posttraumatic (head/neck trauma) 2. Tension-type headache 3. Cluster headache and other 6. Vascular disorder (cranial/cervical) trigeminal autonomic 7. Non vascular intracranial headaches disorder 4. Other primary headaches 8. Substance abuse/ withdrawal 9. Infection Cranial neuralgias, central and primary facial 10 Disorder of homeostasis pain : 11. Disorder of facial/cranial 13. Cranial neuralgias and central causes of structures facial pain International Headache Society. ICHD-II. Cephalalgia 2004; vol 24: suppl 1.
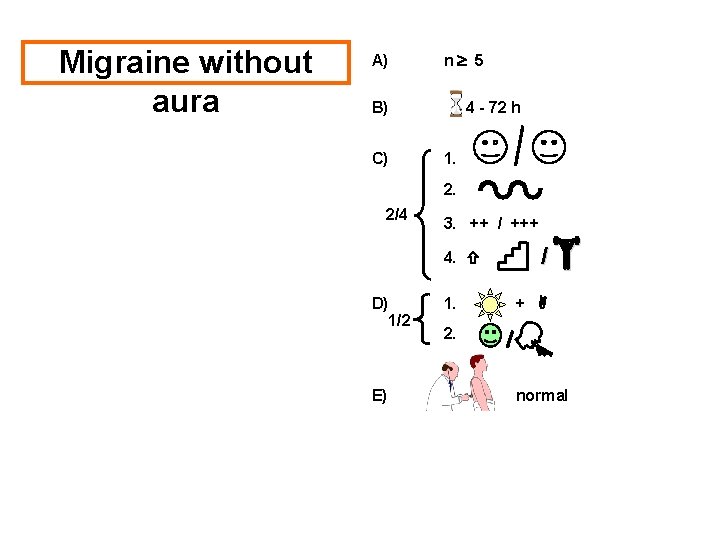
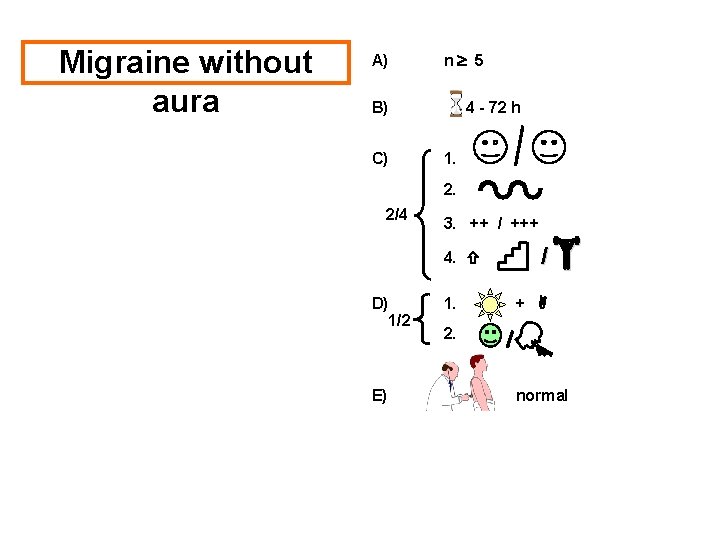
Migraine without aura A) n 5 B) C) 4 - 72 h 1. 2. 2/4 3. ++ / +++ 4. D) 1/2 E) 1. / + 2. normal
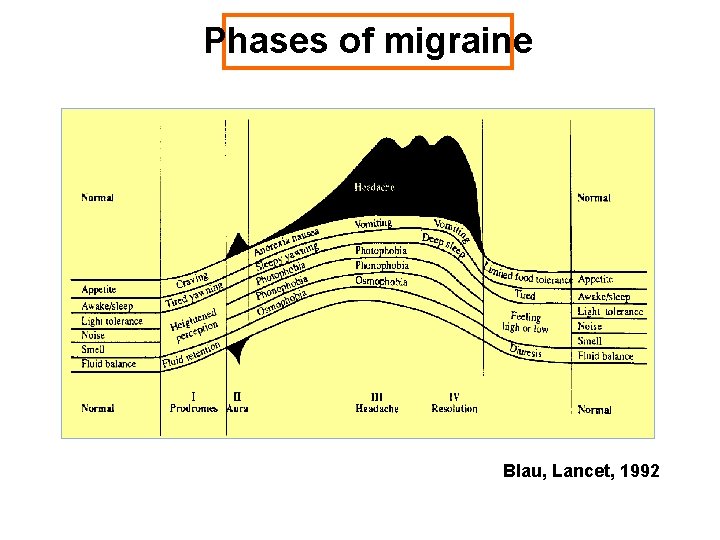
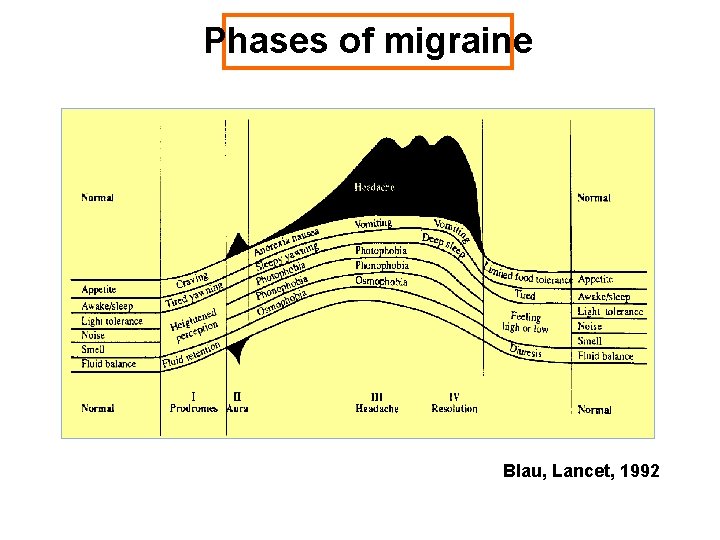
Phases of migraine Blau, Lancet, 1992
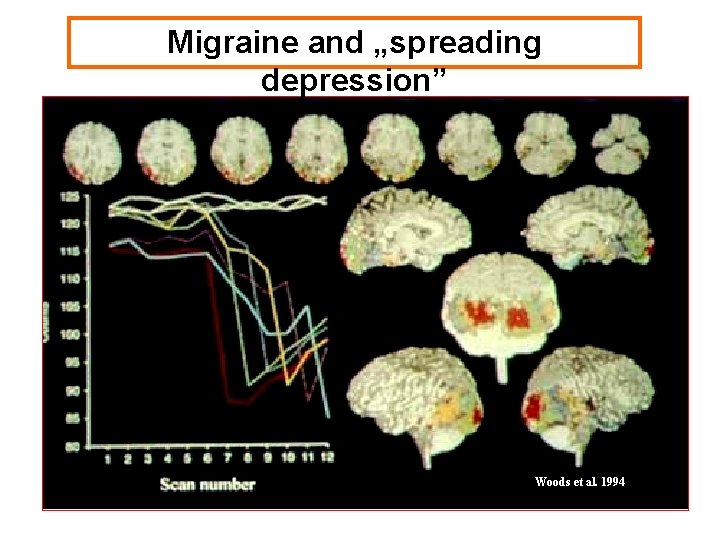
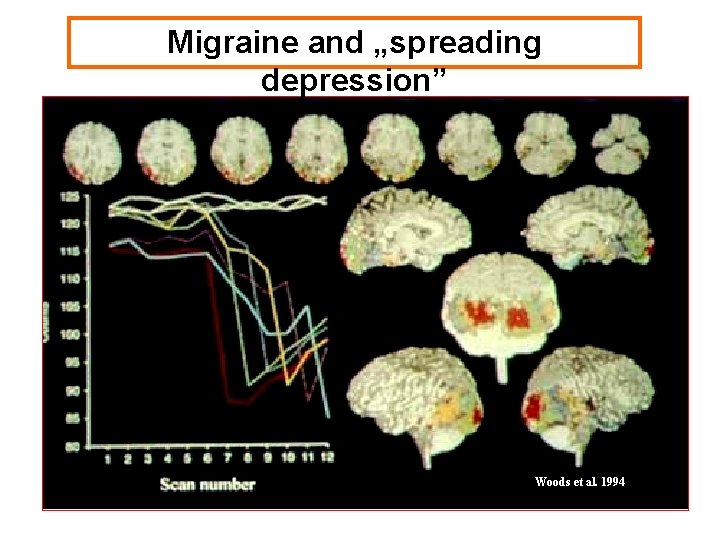
Migraine and „spreading depression” Woods et al. 1994
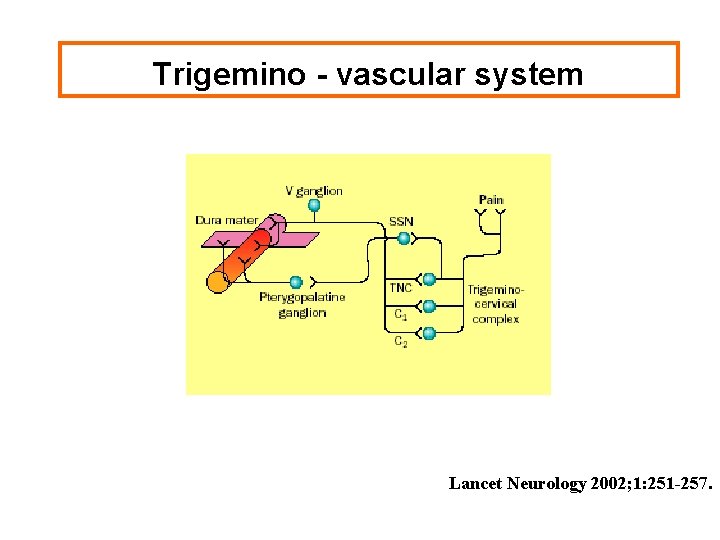
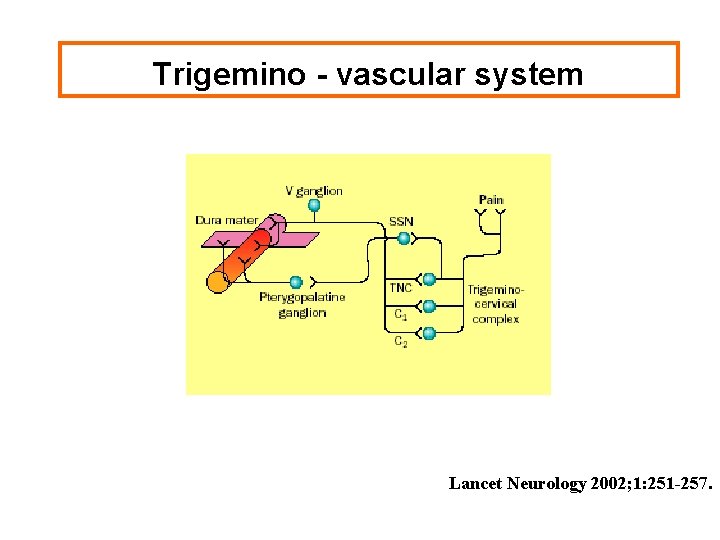
Trigemino - vascular system Lancet Neurology 2002; 1: 251 -257.
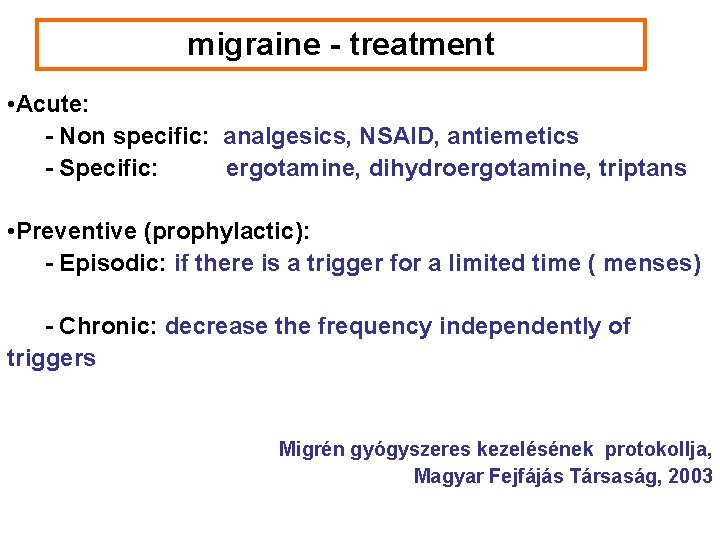
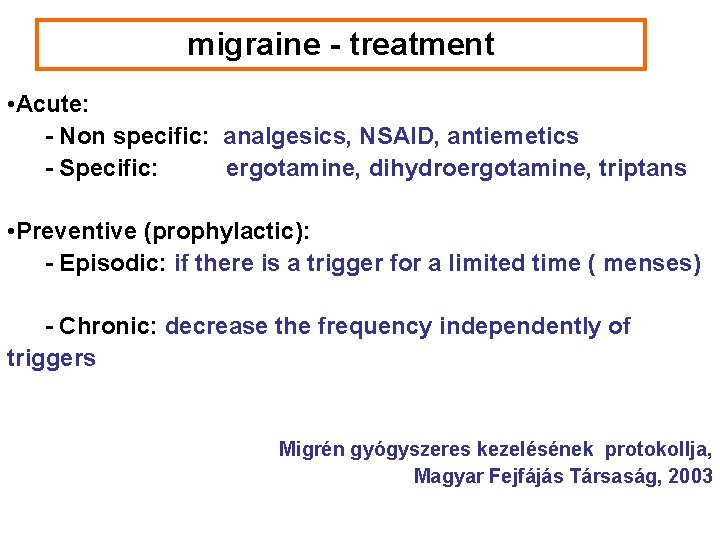
migraine - treatment • Acute: - Non specific: analgesics, NSAID, antiemetics - Specific: ergotamine, dihydroergotamine, triptans • Preventive (prophylactic): - Episodic: if there is a trigger for a limited time ( menses) - Chronic: decrease the frequency independently of triggers Migrén gyógyszeres kezelésének protokollja, Magyar Fejfájás Társaság, 2003
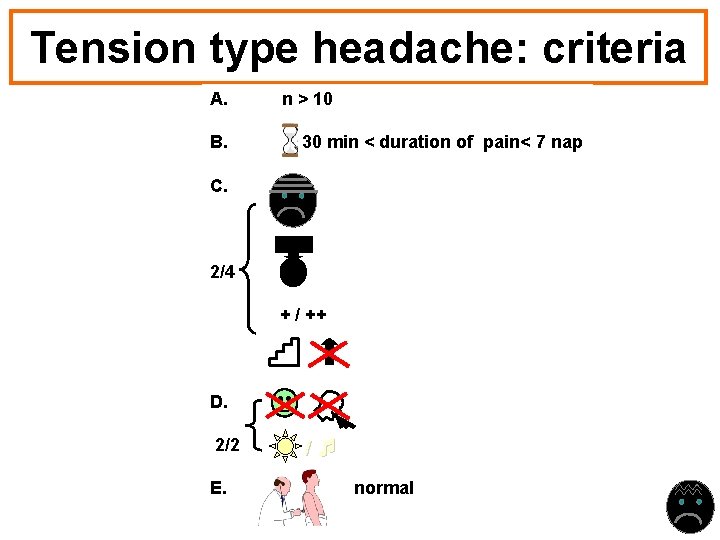
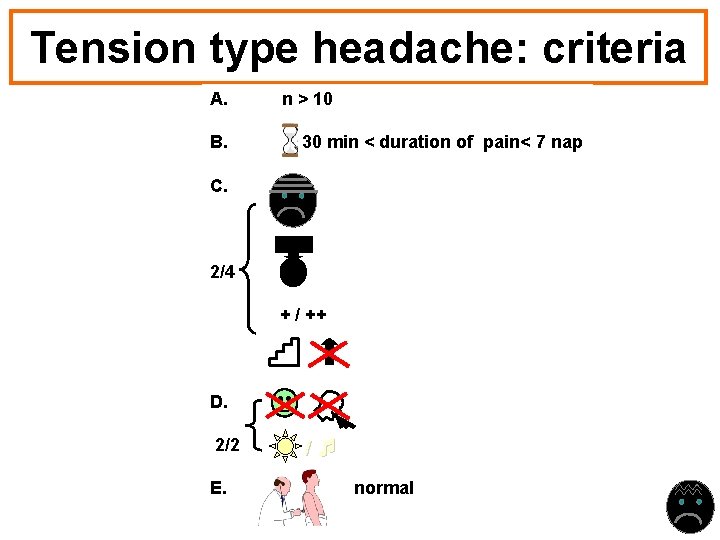
Tension type headache: criteria A. B. n > 10 30 min < duration of pain< 7 nap C. 2/4 + / ++ D. 2/2 E. / normal
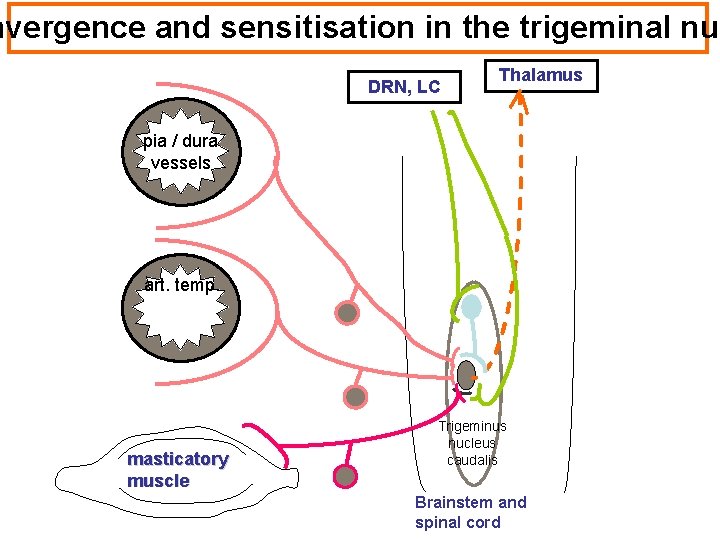
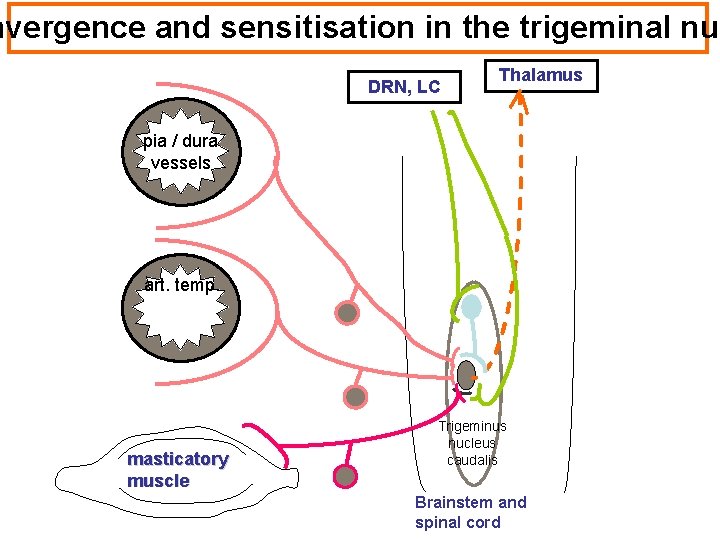
nvergence and sensitisation in the trigeminal nuc DRN, LC Thalamus pia / dura vessels art. temp. masticatory muscle Trigeminus nucleus caudalis Brainstem and spinal cord
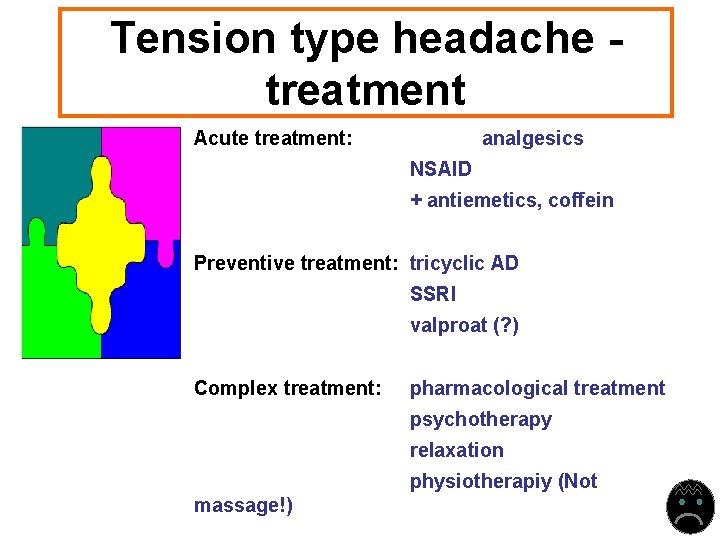
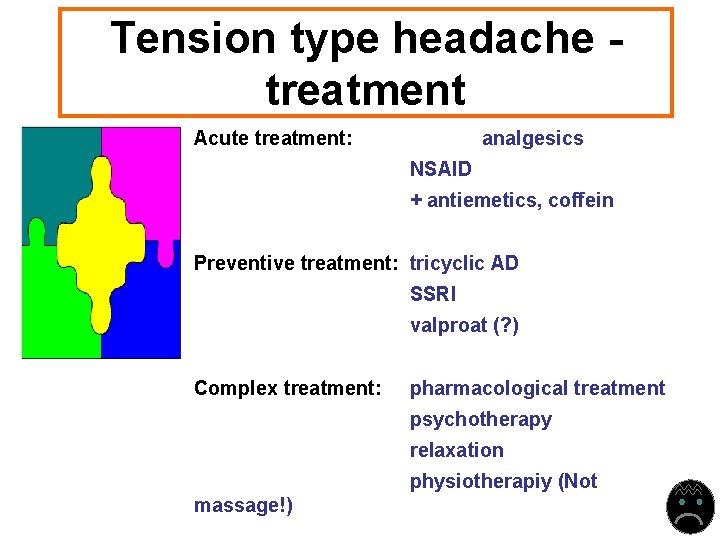
Tension type headache treatment Acute treatment: analgesics NSAID + antiemetics, coffein Preventive treatment: tricyclic AD SSRI valproat (? ) Complex treatment: pharmacological treatment psychotherapy relaxation physiotherapiy (Not massage!)
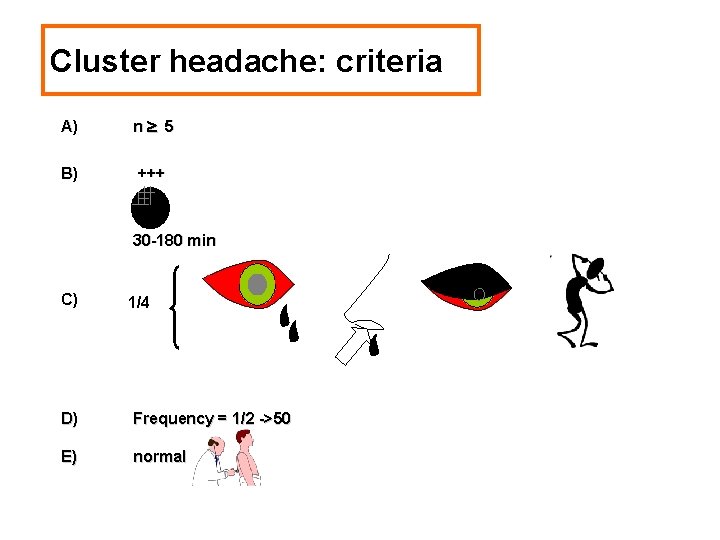
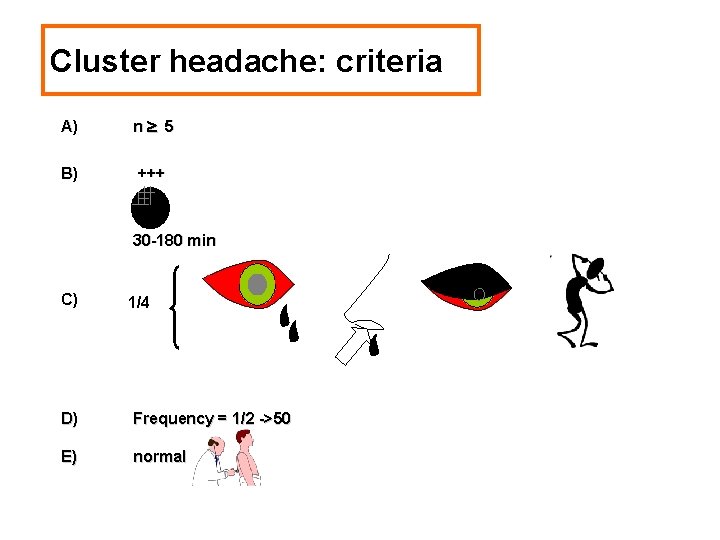
Cluster headache: criteria A) n 5 B) +++ 30 -180 min C) 1/4 D) Frequency = 1/2 ->50 E) normal
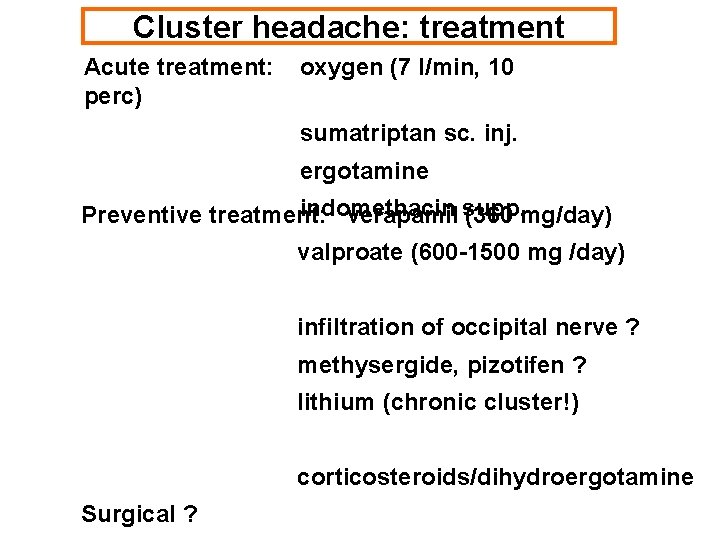
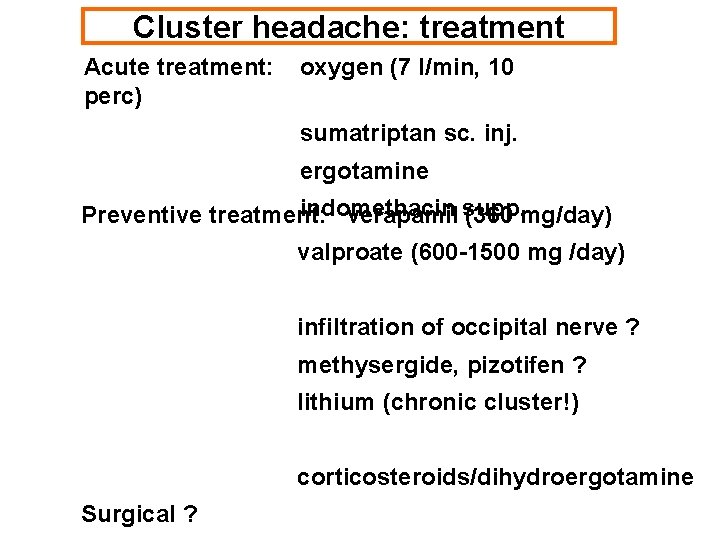
Cluster headache: treatment Acute treatment: perc) oxygen (7 l/min, 10 sumatriptan sc. inj. ergotamine indomethacin Preventive treatment: verapamil supp. (360 mg/day) valproate (600 -1500 mg /day) infiltration of occipital nerve ? methysergide, pizotifen ? lithium (chronic cluster!) corticosteroids/dihydroergotamine Surgical ?
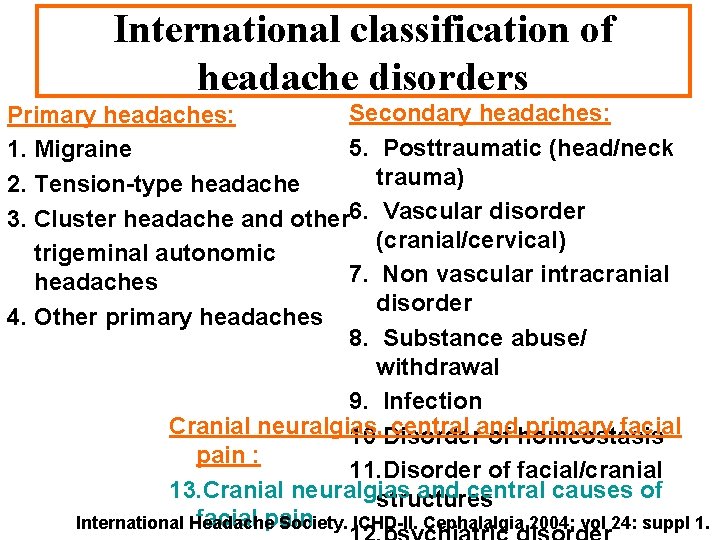
International classification of headache disorders Secondary headaches: Primary headaches: 5. Posttraumatic (head/neck 1. Migraine trauma) 2. Tension-type headache 3. Cluster headache and other 6. Vascular disorder (cranial/cervical) trigeminal autonomic 7. Non vascular intracranial headaches disorder 4. Other primary headaches 8. Substance abuse/ withdrawal 9. Infection Cranial neuralgias, central and primary facial 10 Disorder of homeostasis pain : 11. Disorder of facial/cranial 13. Cranial neuralgias and central causes of structures facial pain International Headache Society. ICHD-II. Cephalalgia 2004; vol 24: suppl 1.
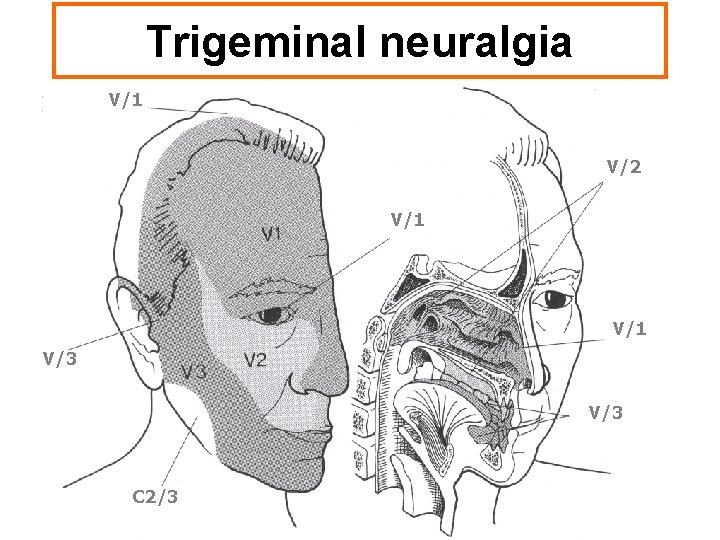
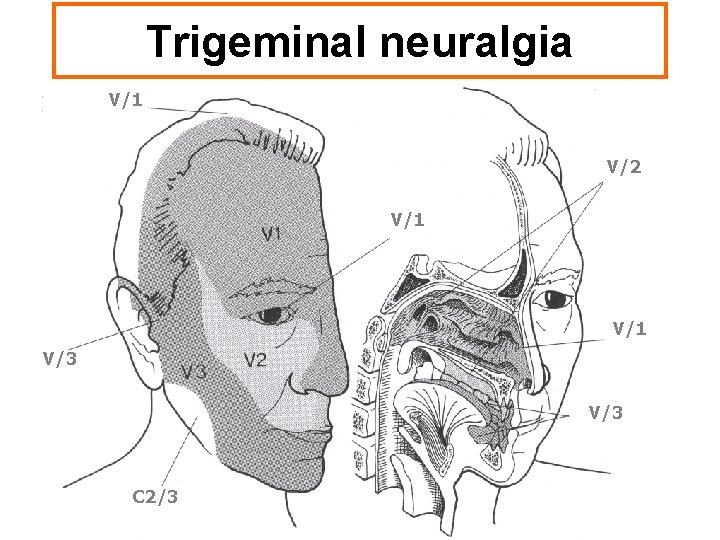
Trigeminal neuralgia V/1 V/2 V/1 V/3 C 2/3
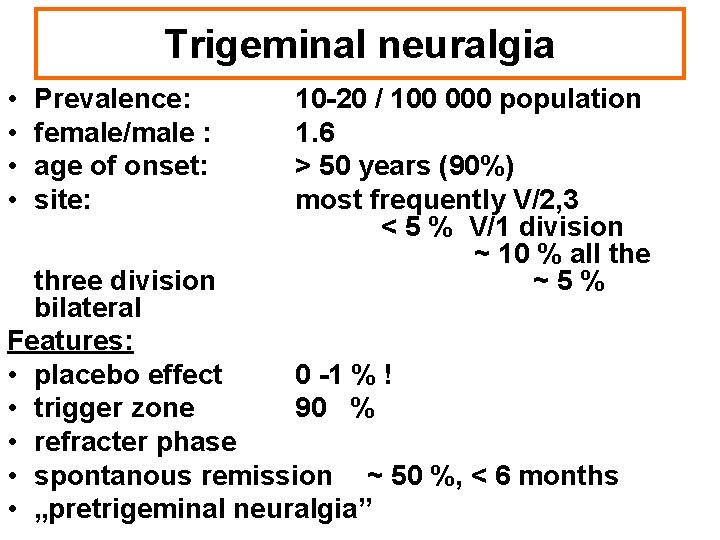
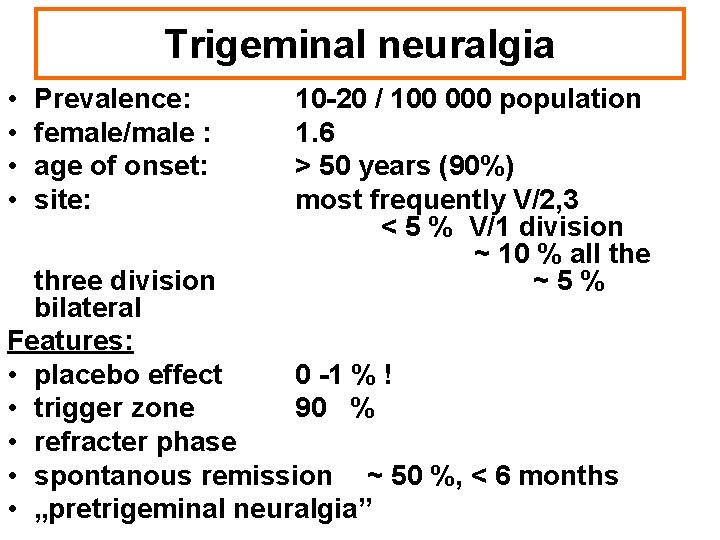
Trigeminal neuralgia • • Prevalence: female/male : age of onset: site: 10 -20 / 100 000 population 1. 6 > 50 years (90%) most frequently V/2, 3 < 5 % V/1 division ~ 10 % all the ~5% three division bilateral Features: • placebo effect 0 -1 % ! • trigger zone 90 % • refracter phase • spontanous remission ~ 50 %, < 6 months • „pretrigeminal neuralgia”
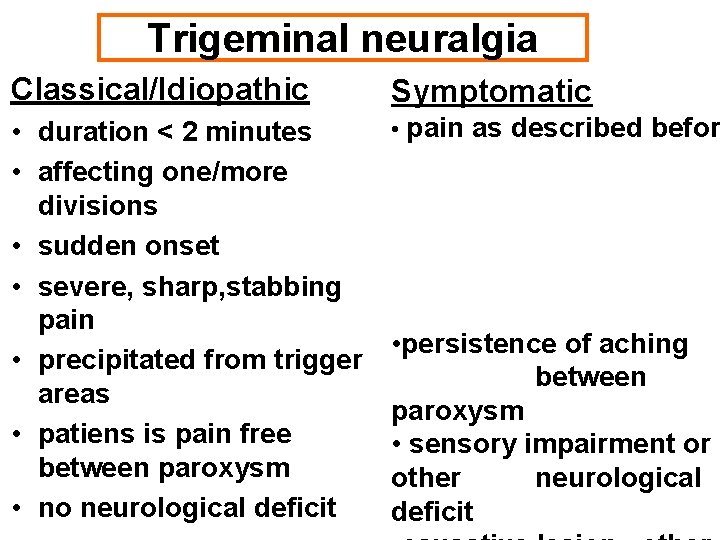
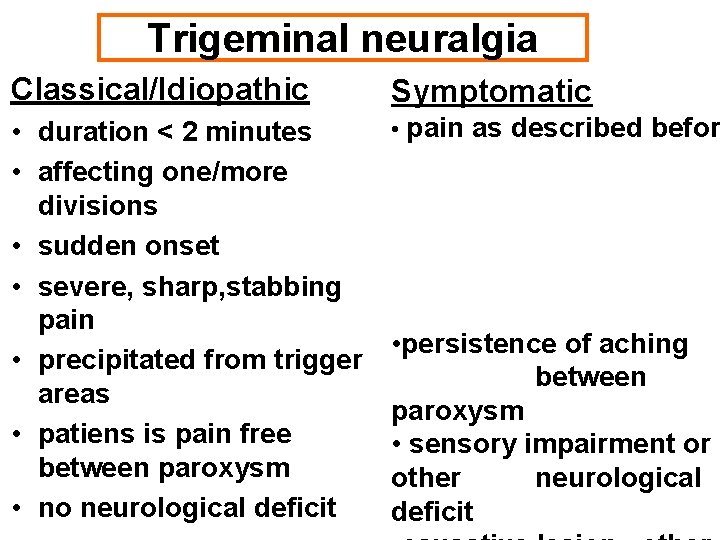
Trigeminal neuralgia Classical/Idiopathic Symptomatic • duration < 2 minutes • affecting one/more divisions • sudden onset • severe, sharp, stabbing pain • precipitated from trigger areas • patiens is pain free between paroxysm • no neurological deficit • pain as described befor • persistence of aching between paroxysm • sensory impairment or other neurological deficit
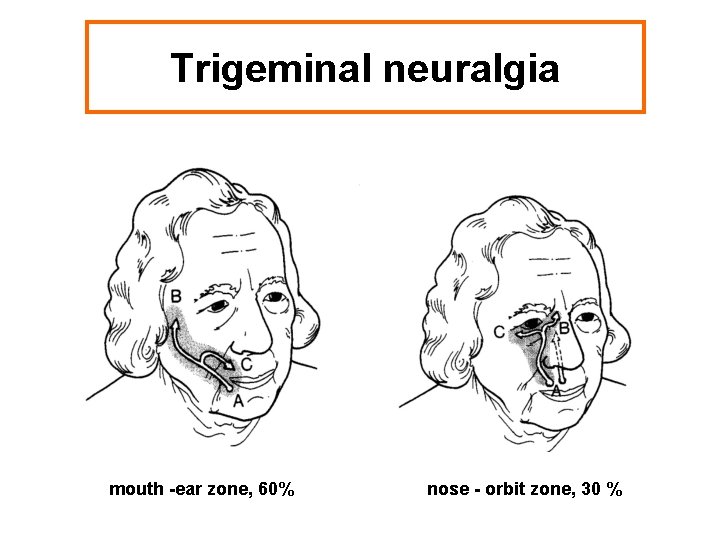
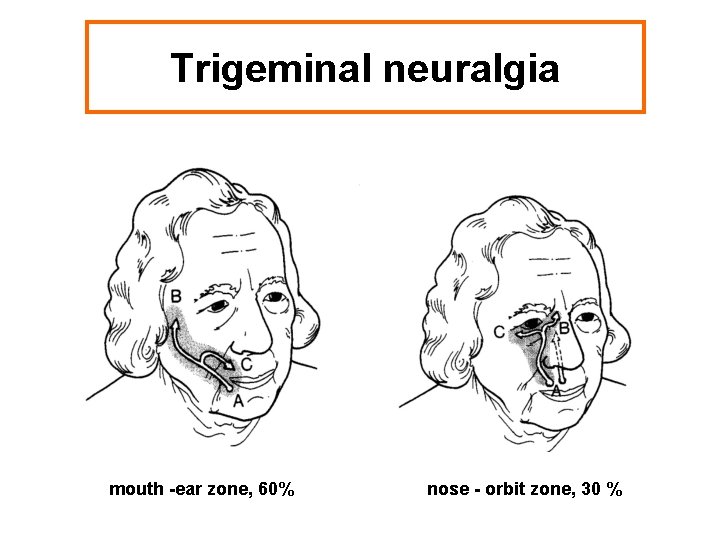
Trigeminal neuralgia mouth -ear zone, 60% nose - orbit zone, 30 %
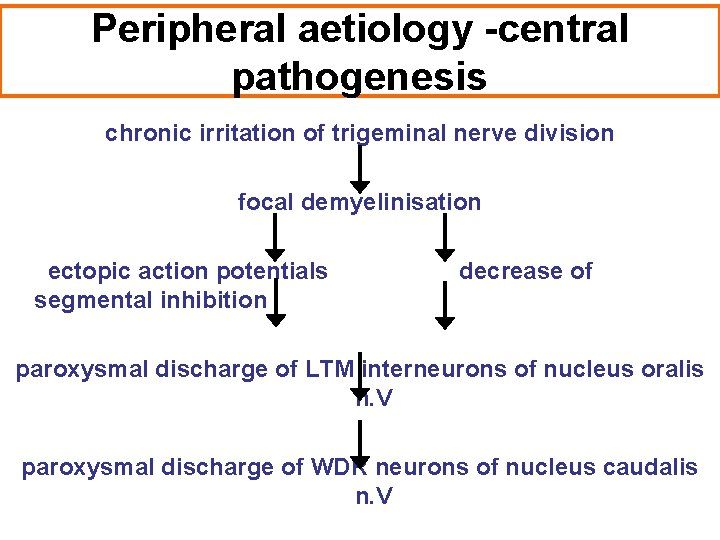
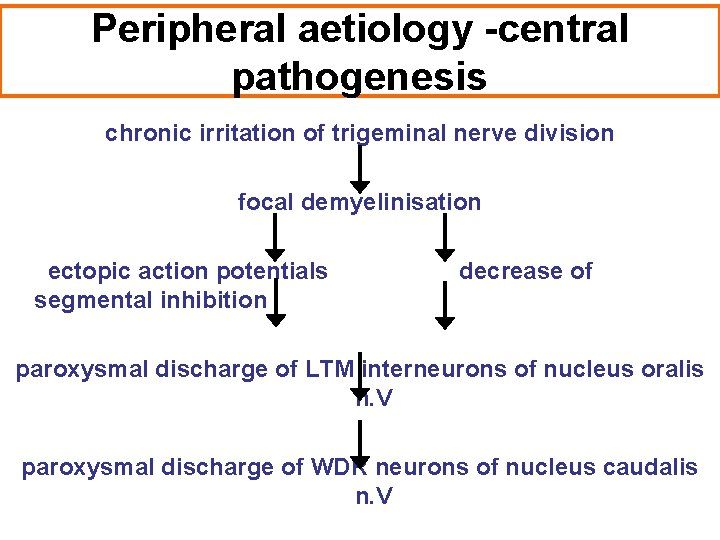
Peripheral aetiology -central pathogenesis chronic irritation of trigeminal nerve division focal demyelinisation ectopic action potentials segmental inhibition decrease of paroxysmal discharge of LTM interneurons of nucleus oralis n. V paroxysmal discharge of WDR neurons of nucleus caudalis n. V
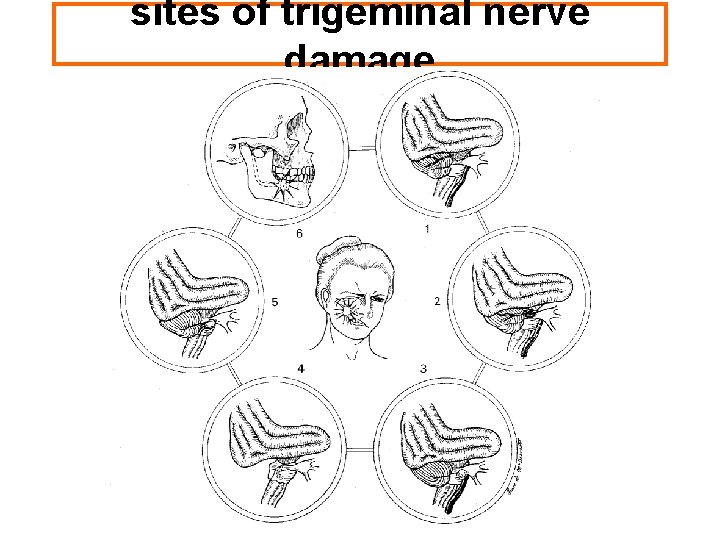
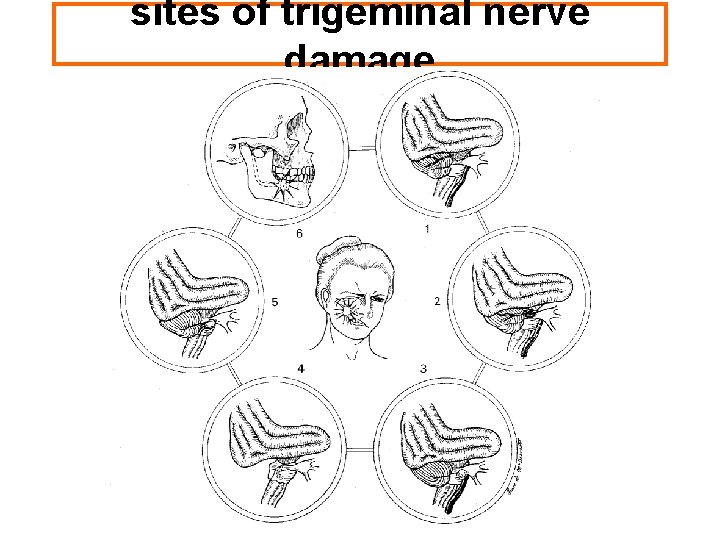
sites of trigeminal nerve damage
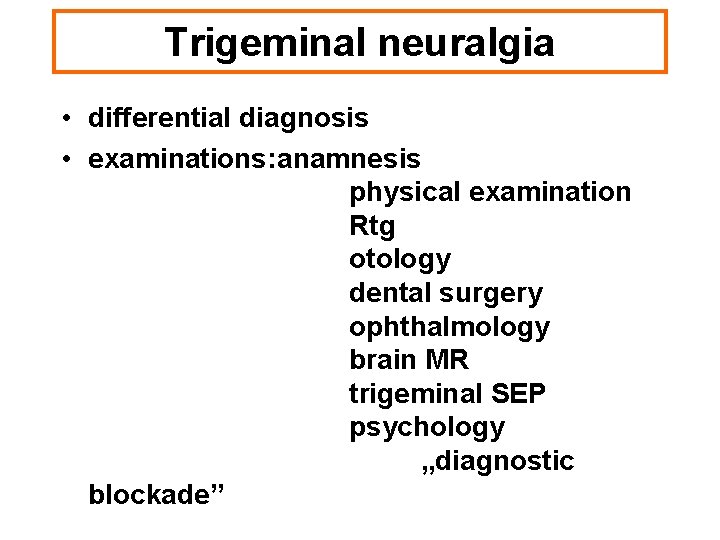
Trigeminal neuralgia • differential diagnosis • examinations: anamnesis physical examination Rtg otology dental surgery ophthalmology brain MR trigeminal SEP psychology „diagnostic blockade”
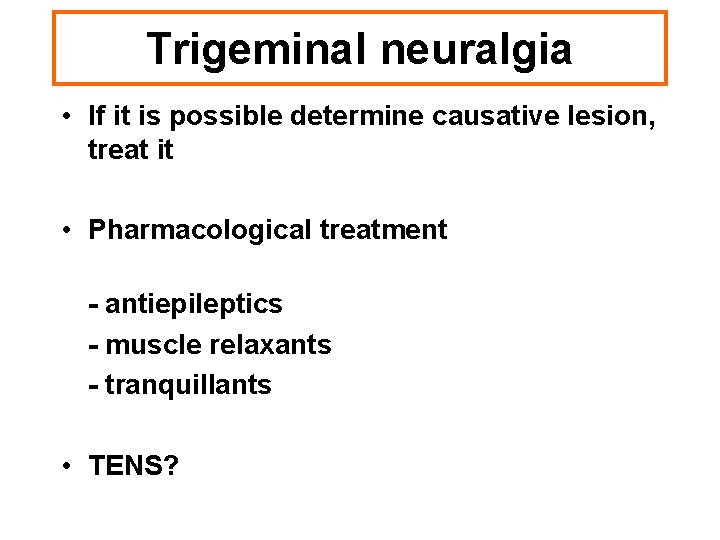
Trigeminal neuralgia • If it is possible determine causative lesion, treat it • Pharmacological treatment - antiepileptics - muscle relaxants - tranquillants • TENS?
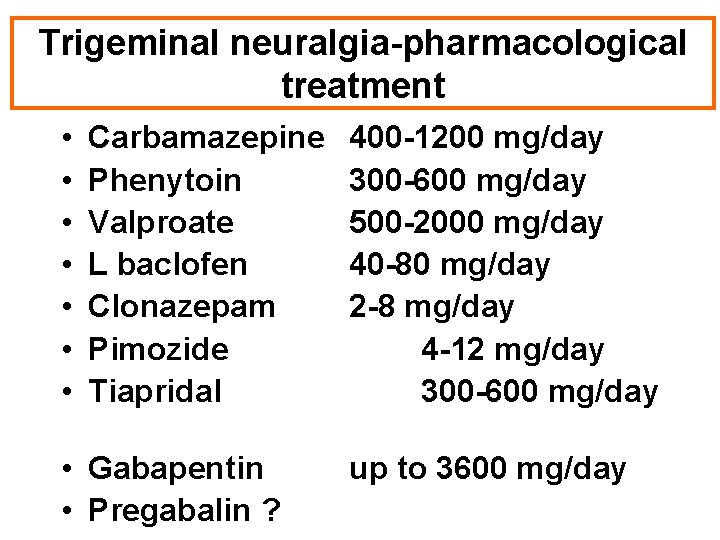
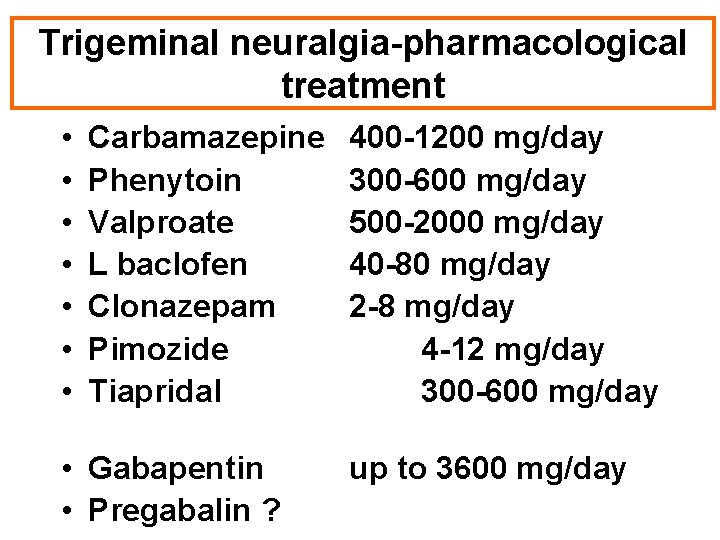
Trigeminal neuralgia-pharmacological treatment • • Carbamazepine Phenytoin Valproate L baclofen Clonazepam Pimozide Tiapridal • Gabapentin • Pregabalin ? 400 -1200 mg/day 300 -600 mg/day 500 -2000 mg/day 40 -80 mg/day 2 -8 mg/day 4 -12 mg/day 300 -600 mg/day up to 3600 mg/day
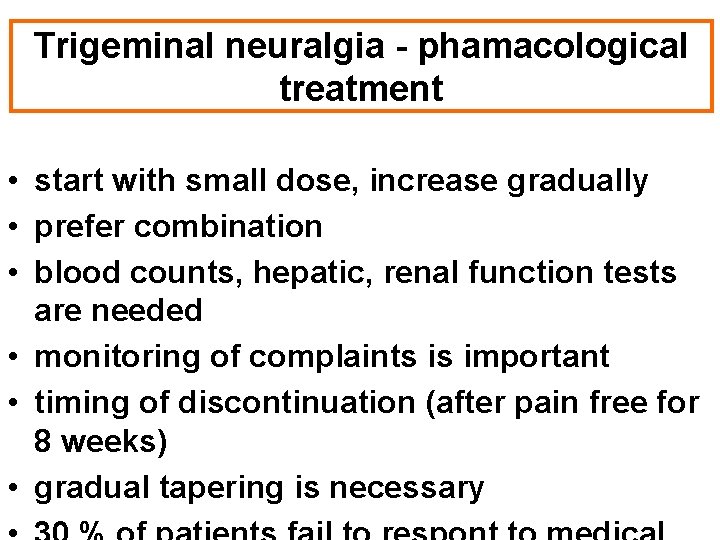
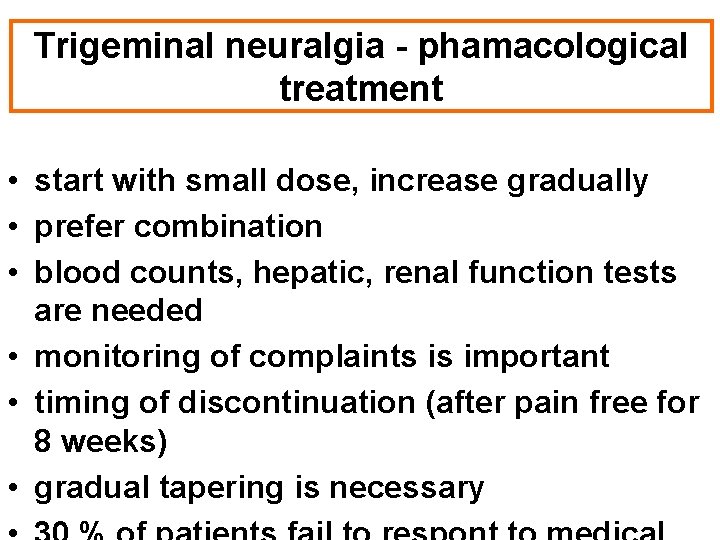
Trigeminal neuralgia - phamacological treatment • start with small dose, increase gradually • prefer combination • blood counts, hepatic, renal function tests are needed • monitoring of complaints is important • timing of discontinuation (after pain free for 8 weeks) • gradual tapering is necessary
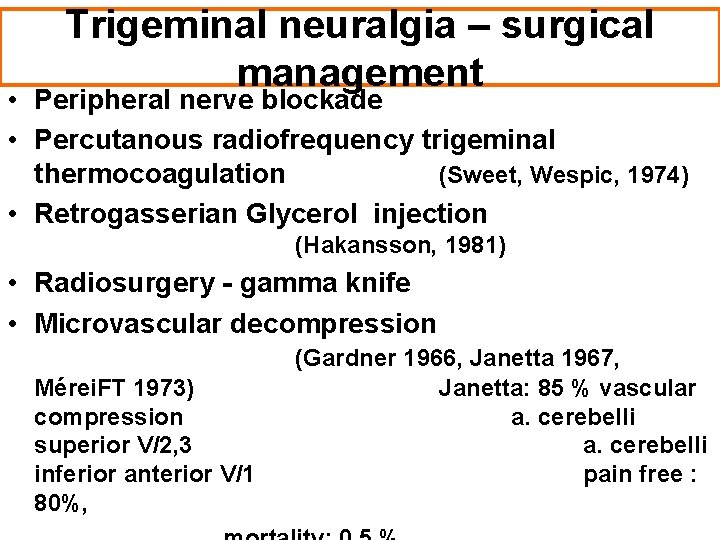
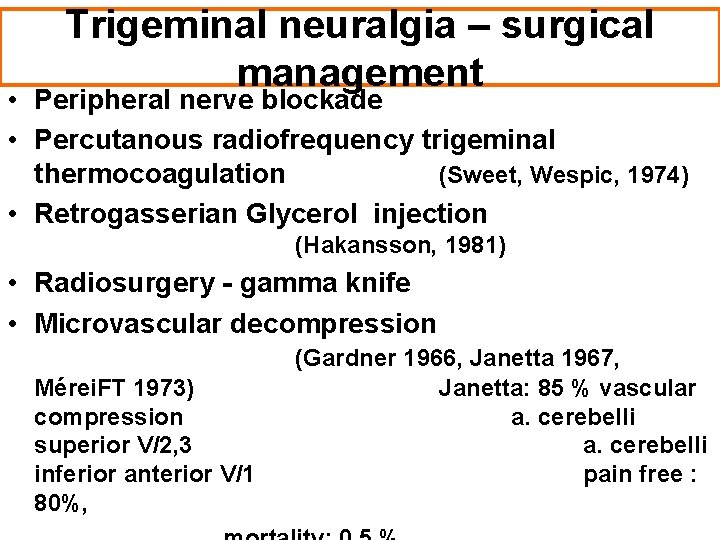
Trigeminal neuralgia – surgical management • Peripheral nerve blockade • Percutanous radiofrequency trigeminal thermocoagulation (Sweet, Wespic, 1974) • Retrogasserian Glycerol injection (Hakansson, 1981) • Radiosurgery - gamma knife • Microvascular decompression Mérei. FT 1973) compression superior V/2, 3 inferior anterior V/1 80%, (Gardner 1966, Janetta 1967, Janetta: 85 % vascular a. cerebelli pain free :
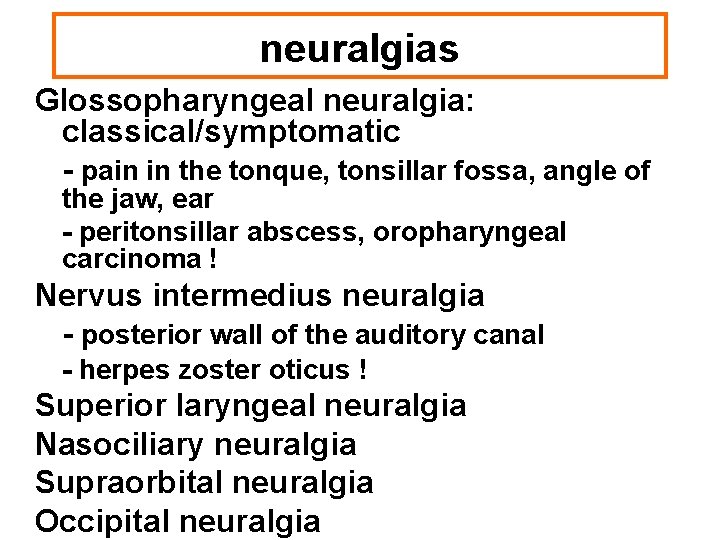
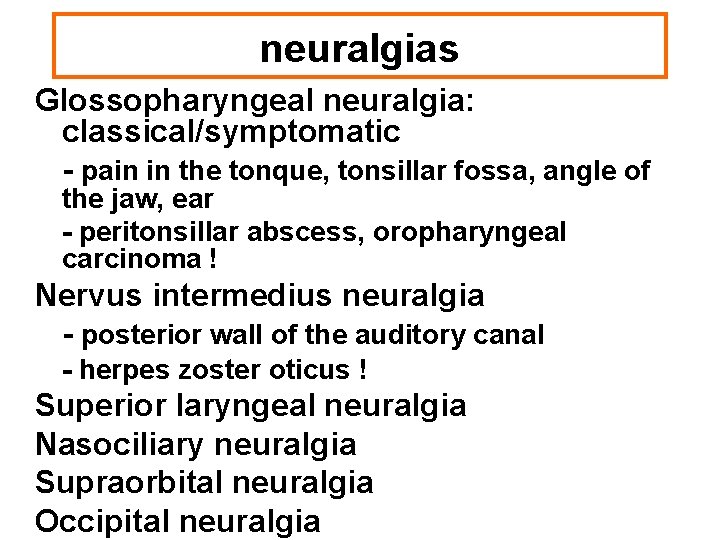
neuralgias Glossopharyngeal neuralgia: classical/symptomatic - pain in the tonque, tonsillar fossa, angle of the jaw, ear - peritonsillar abscess, oropharyngeal carcinoma ! Nervus intermedius neuralgia - posterior wall of the auditory canal - herpes zoster oticus ! Superior laryngeal neuralgia Nasociliary neuralgia Supraorbital neuralgia Occipital neuralgia
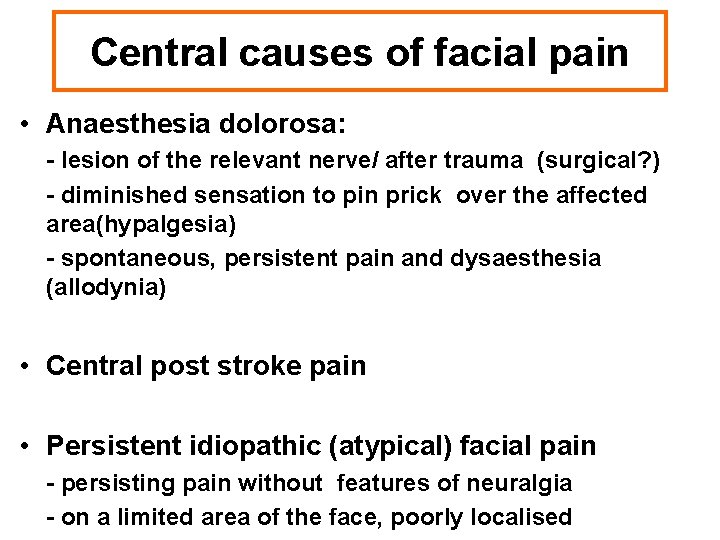
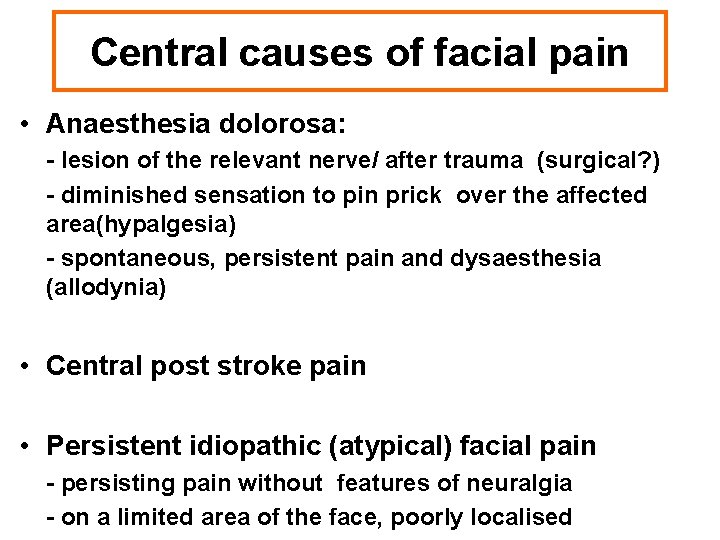
Central causes of facial pain • Anaesthesia dolorosa: - lesion of the relevant nerve/ after trauma (surgical? ) - diminished sensation to pin prick over the affected area(hypalgesia) - spontaneous, persistent pain and dysaesthesia (allodynia) • Central post stroke pain • Persistent idiopathic (atypical) facial pain - persisting pain without features of neuralgia - on a limited area of the face, poorly localised
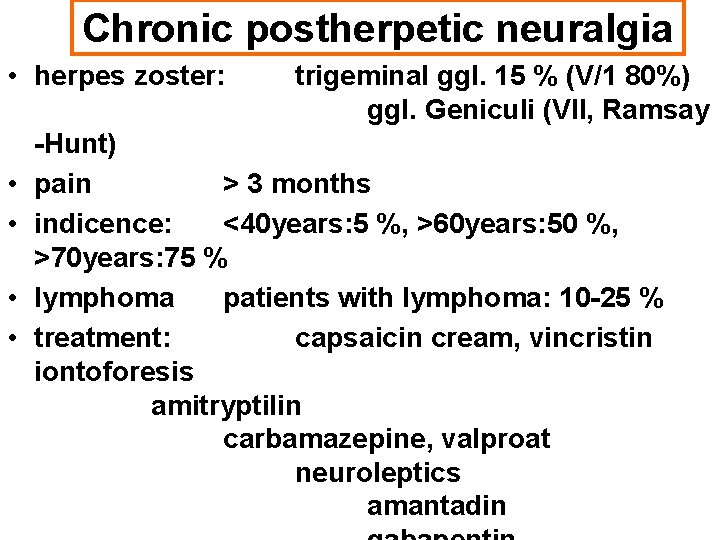
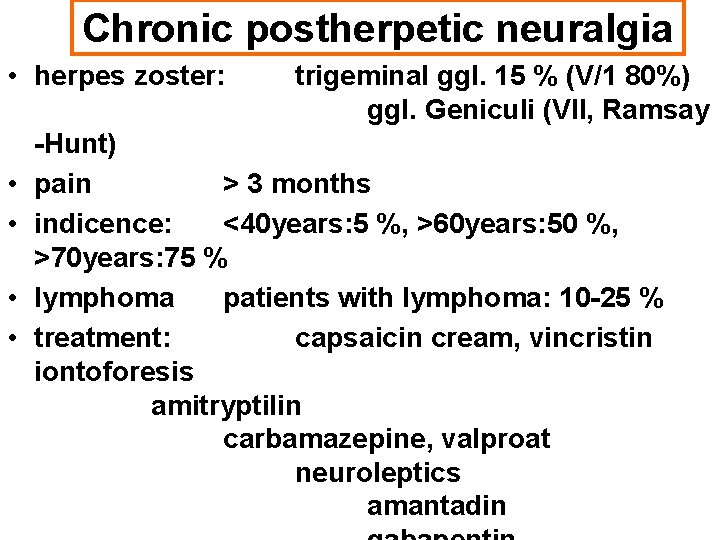
Chronic postherpetic neuralgia • herpes zoster: • • trigeminal ggl. 15 % (V/1 80%) ggl. Geniculi (VII, Ramsay -Hunt) pain > 3 months indicence: <40 years: 5 %, >60 years: 50 %, >70 years: 75 % lymphoma patients with lymphoma: 10 -25 % treatment: capsaicin cream, vincristin iontoforesis amitryptilin carbamazepine, valproat neuroleptics amantadin
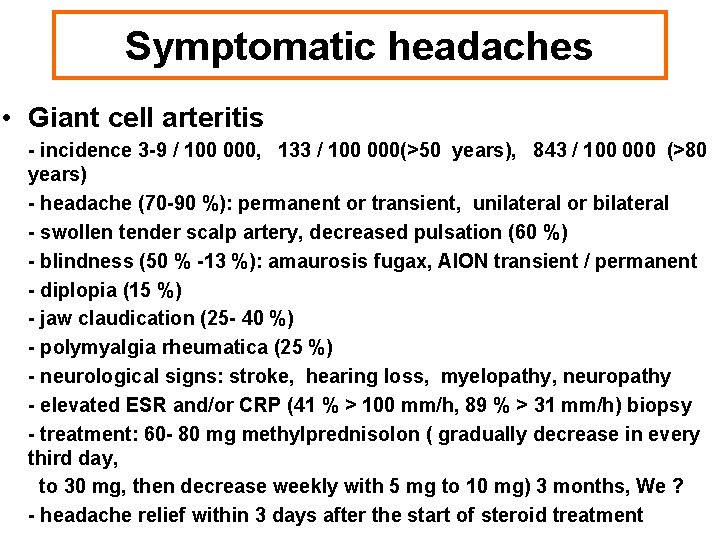
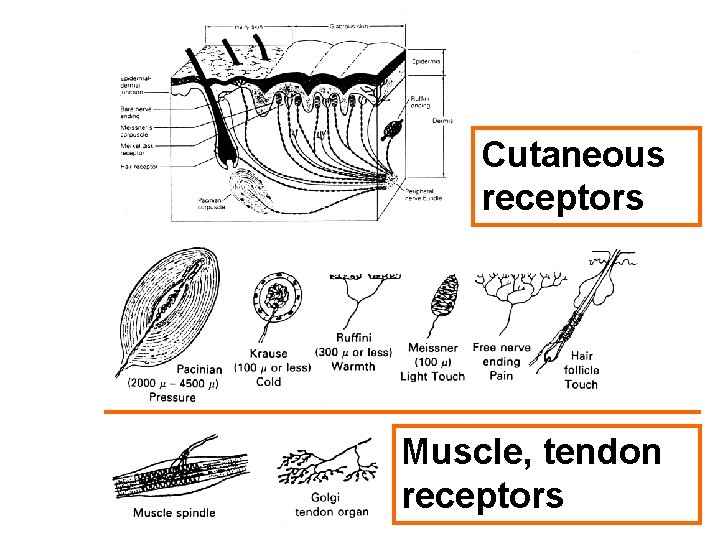
Symptomatic headaches • Giant cell arteritis - incidence 3 -9 / 100 000, 133 / 100 000(>50 years), 843 / 100 000 (>80 years) - headache (70 -90 %): permanent or transient, unilateral or bilateral - swollen tender scalp artery, decreased pulsation (60 %) - blindness (50 % -13 %): amaurosis fugax, AION transient / permanent - diplopia (15 %) - jaw claudication (25 - 40 %) - polymyalgia rheumatica (25 %) - neurological signs: stroke, hearing loss, myelopathy, neuropathy - elevated ESR and/or CRP (41 % > 100 mm/h, 89 % > 31 mm/h) biopsy - treatment: 60 - 80 mg methylprednisolon ( gradually decrease in every third day, to 30 mg, then decrease weekly with 5 mg to 10 mg) 3 months, We ? - headache relief within 3 days after the start of steroid treatment