The Science and Art of Behavior Management Kelly
The Science and Art of Behavior Management Kelly Trevino, Ph. D Clinical Psychologist VA Boston Healthcare System GRECC Audio Conference Series July 29, 2010
Acknowledgements Nurse Managers ◦ Annette Couchenour ◦ Steve Mc. Garry ◦ Connie Soule ◦ Mary Farren Nursing Director ◦ Ronald Molyneaux CLC Nursing Staff Medical Staff ◦ Dr. Juman Hijab ◦ Jack Earnshaw Psychiatrists ◦ Dr. Mohit Chopra ◦ Dr. Ronald Gurrera
Outline �Background �The Science ◦ Learning Behavior Model ◦ Person-Environment Fit Model ◦ Need-Driven Behavior Model �The Art ◦ Staff Training ◦ Behavior Management Team (BMT) ◦ Lessons Learned �Behavior Management �Program Implementation

Background � 5. 3 million persons in the U. S. have Alzheimer's Disease 1 � 11 -16 20502 million persons in US will have AD by � In 2004: 136, 174 veterans with dementia using VHA 3 ◦ 2022: 205, 781 � 47% of nursing home residents have dementia 1 ◦ Up to 70% have memory problems 4 � ~66% of community elders and ~77% nursing home elders with dementia have disruptive behavior 5, 6 � Disruptive behavior associated with negative 7 -9
Psychotropic Medications and Restraints �Psychotropic Medication ◦ Limited effectiveness 10 ◦ Negative side effects 11, 12 �Restraints 13 ◦ Higher rate of falls ◦ Negative psychological outcomes
THE SCIENCE
The Science: Learning Behavior Model �Learned relationship between antecedents, behaviors, and consequences (ABCs of behavior management)14 ◦ A=Antecedents=Triggers ◦ B=Behaviors ◦ C=Consequences=Reinforcement or Punishment �Manipulate antecedents and consequences to change behavior ◦ Provide new learning experience �Comprehensive functional analysis important
The Science: Learning Behavior Model �Instrumental Conditioning Principles 15 ◦ Reinforcer contiguity ◦ Response-reinforcer contingency ◦ Reinforcement �Problems with punishment ◦ Negative affective reaction ◦ Focus on avoiding punishment (rather than improving behavior) ◦ Negativity can generalize to other stimuli (person, environment, time)

The Science: Learning Behavior Model �Characteristics of Interventions 16 -18 ◦ Staff education �Topics: Dementia, Psychiatric disorders, Behavior problems, ABCs of behavior management, communicating with persons with dementia �Method: Didactic, discussion, role playing, video case vignettes, handouts ◦ Assistance with care planning ◦ On-site supervision ◦ Increasing resident participation in pleasant events ◦ Peer support ◦ Caregiver problem-solving skills ◦ Exercise program
The Science: Person. Environment Fit � Dementia increases vulnerability to the environment 19 ◦ Stimuli affect people with dementia at a lower threshold � People with dementia have fewer coping resources � Poor fit b/w person and environment impairs functioning and increases disruptive behavior � Intervention ◦ Create a familiar and comforting environment ◦ Stimulate through reliance on remote memory and positive emotions
The Science: Person. Environment Fit �Characteristics of Interventions 20 -22 ◦ Simulated presence therapy ◦ Activity programming �Based on mental and physical abilities �Adjust for mood and behavior �Incorporate periods of stimulation and rest ◦ Individualized music ◦ Environmental modifications ◦ In-home counseling
The Science: Need-Driven Behavior �Normal needs + Abnormal conditions = Disruptive behavior 23 ◦ Behavior is response to unmet need �Adjust environment and build on strengths/preferences of individual to meet and prevent unmet needs ◦ Consider sensory deficits �Treatment Routes for Exploration of Agitation (TREA)24 ◦ Identify correlates of particular behaviors ◦ Provide suggestions for changing the correlates
General Guidelines �Basic principles ◦ Specificity ◦ Individualization ◦ Consistency: Implementation and documentation �Behavior may increase initially ◦ Re-examine plan after 2 -3 days �Behaviors ◦ ◦ are not Voluntary or purposeful Rudeness Due to a “bad attitude” Attempt to make your job difficult
Boston VA CLC THE ART Behavior Management Team (BMT)

BMT: Creation �Recognition of a problem �Weekly interdisciplinary meetings ◦ Psychology, nursing, medicine �Identified: ◦ Problem ◦ Goals ◦ Process ◦ Staff Training ◦ Documentation
Staff Training: BMT What is the BMT ◦ Explain why ◦ Explain how ◦ Get feedback/ideas BMT Documentation ◦ Focus on BMT Shift Note Outcome ◦ ◦ measures Frequency of behaviors Severity of behaviors Referrals to BMT Medications for behaviors ◦ Inpatient psych transfers ◦ Code greens for behaviors ◦ Staff feedback on BMT
Staff Training: Functional Analysis �Prevalence of behaviors �Difficulty of managing behaviors �Define types of behaviors and correlates �DON’T PANIC �ABCs of behavior management �Unmet needs �Questions behaviors for describing context of
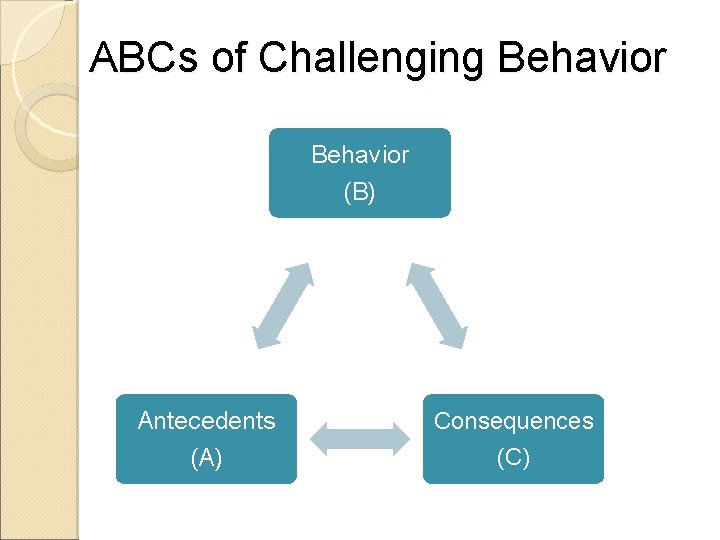
ABCs of Challenging Behavior (B) Antecedents (A) Consequences (C)
Staff Training: Creating/Implementing Behavior Plans �Basic principles ◦ Specificity ◦ Individualization ◦ Consistency: Implementation and documentation �Behavior may increase initially ◦ Re-examine plan after 2 -3 days �Behaviors ◦ ◦ are not Voluntary or purposeful Rudeness Due to a “bad attitude” Attempt to make your job difficult �Questions for identifying new ABCs
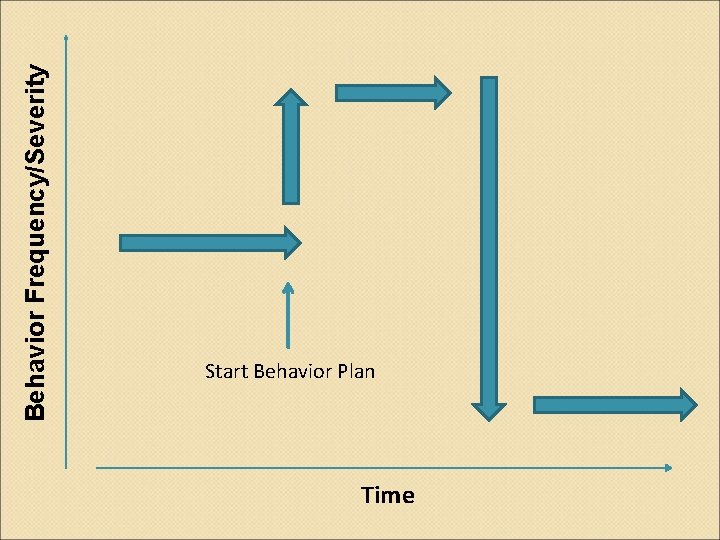
Behavior Frequency/Severity Start Behavior Plan Time
The Art: Behavior Management Team ◦ BMT Members: �Psychologist �Nursing staff �Nurse manager �MD/PA �Geriatric psychiatrist consulted, as needed �Identification of residents ◦ CPRS consult ◦ Direct communication from staff
The Art: Behavior Management Team �Inclusion criteria ◦ Demonstrate physical and/or verbal behaviors that: �Create potential harm/distress to the resident, staff, other veterans �Are difficult to manage (are not re-directable) � Do NOT refer residents that are an immediate safety risk �Treatment implementation ◦ Functional analysis of behavior ◦ Create behavior plan �Set behavioral goal ◦ Monitor over time ◦ Change as needed ◦ Discharge when goal met 2 consecutive weeks
The Art: Behavior Management Team �Weekly meeting on each unit ◦ Learning circle ◦ “Rounding” ◦ Meet with floor staff and PA, then consult nurse manager �Documentation ◦ BMT Management Plan ◦ BMT Shift Note ◦ BMT Weekly note
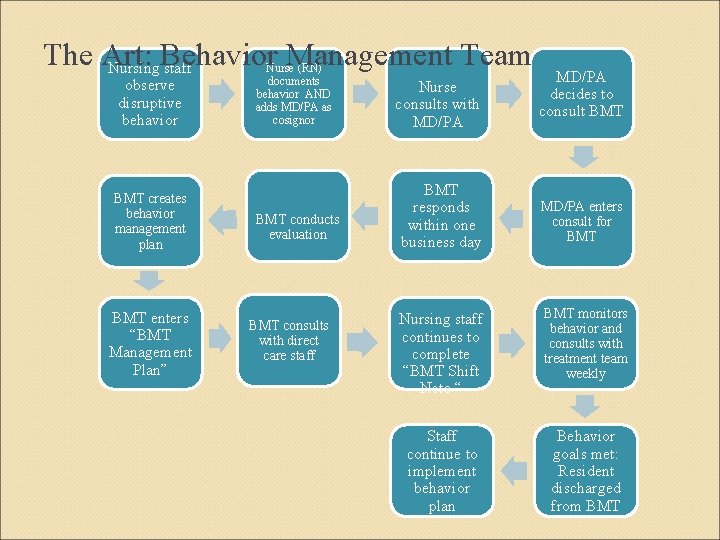
The Art: Behavior Management Team Nursing staff observe disruptive behavior BMT creates behavior management plan BMT enters “BMT Management Plan” Nurse (RN) documents behavior AND adds MD/PA as cosignor BMT conducts evaluation BMT consults with direct care staff Nurse consults with MD/PA BMT responds within one business day MD/PA decides to consult BMT MD/PA enters consult for BMT Nursing staff continues to complete “BMT Shift Note “ BMT monitors behavior and consults with treatment team weekly Staff continue to implement behavior plan Behavior goals met: Resident discharged from BMT
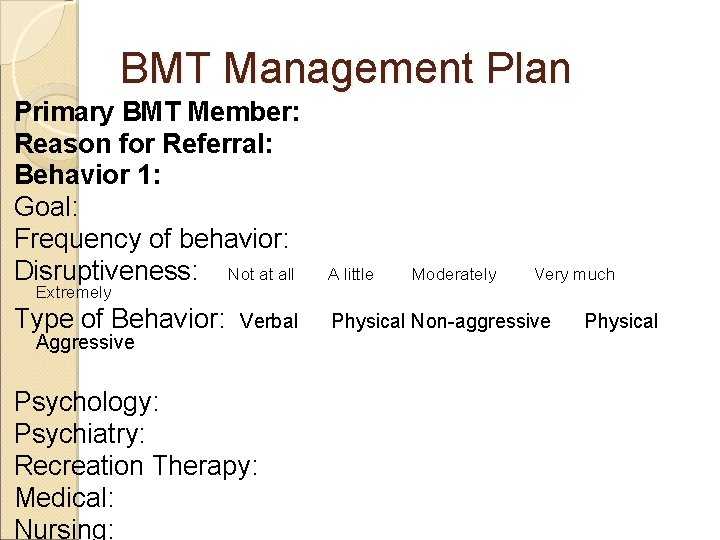
BMT Management Plan Primary BMT Member: Reason for Referral: Behavior 1: Goal: Frequency of behavior: Disruptiveness: Not at all A little Type of Behavior: Physical Non-aggressive Extremely Aggressive Verbal Psychology: Psychiatry: Recreation Therapy: Medical: Nursing: Moderately Very much Physical
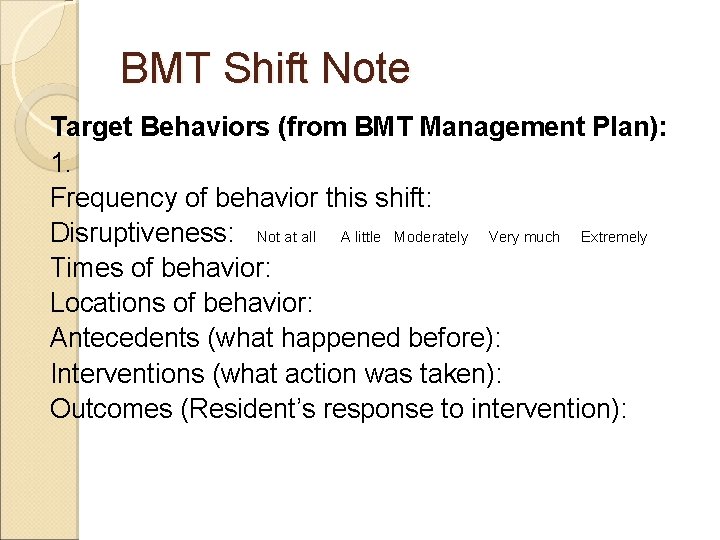
BMT Shift Note Target Behaviors (from BMT Management Plan): 1. Frequency of behavior this shift: Disruptiveness: Not at all A little Moderately Very much Extremely Times of behavior: Locations of behavior: Antecedents (what happened before): Interventions (what action was taken): Outcomes (Resident’s response to intervention):
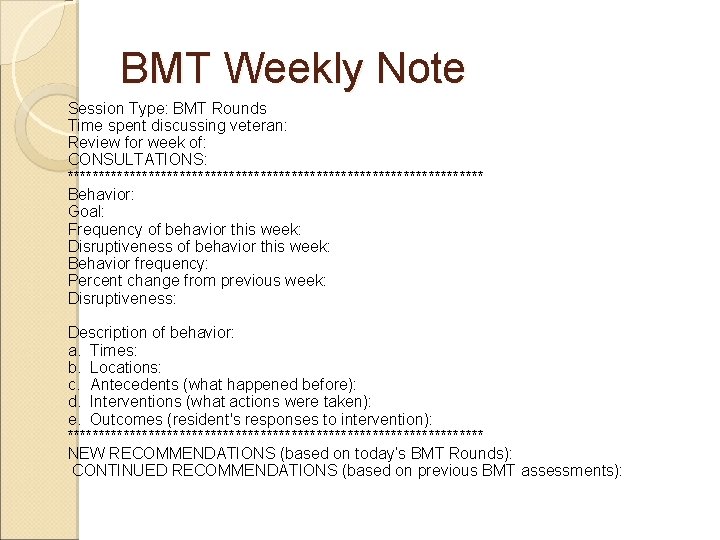
BMT Weekly Note Session Type: BMT Rounds Time spent discussing veteran: Review for week of: CONSULTATIONS: ********************************** Behavior: Goal: Frequency of behavior this week: Disruptiveness of behavior this week: Behavior frequency: Percent change from previous week: Disruptiveness: Description of behavior: a. Times: b. Locations: c. Antecedents (what happened before): d. Interventions (what actions were taken): e. Outcomes (resident's responses to intervention): ********************************** NEW RECOMMENDATIONS (based on today’s BMT Rounds): CONTINUED RECOMMENDATIONS (based on previous BMT assessments):
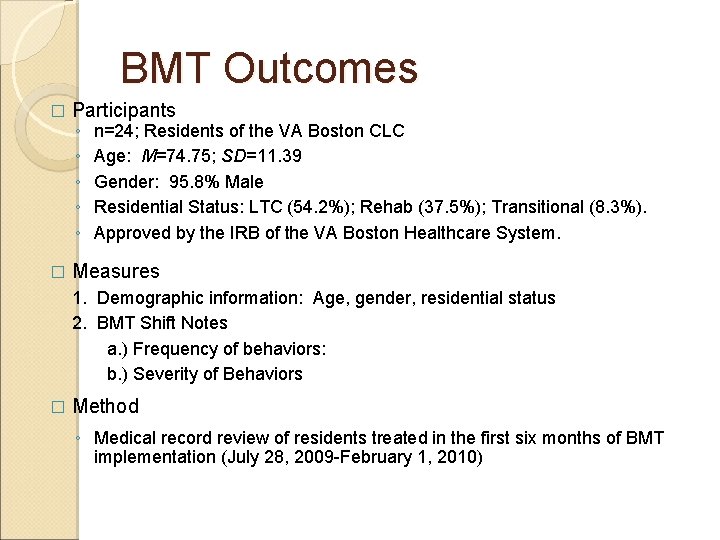
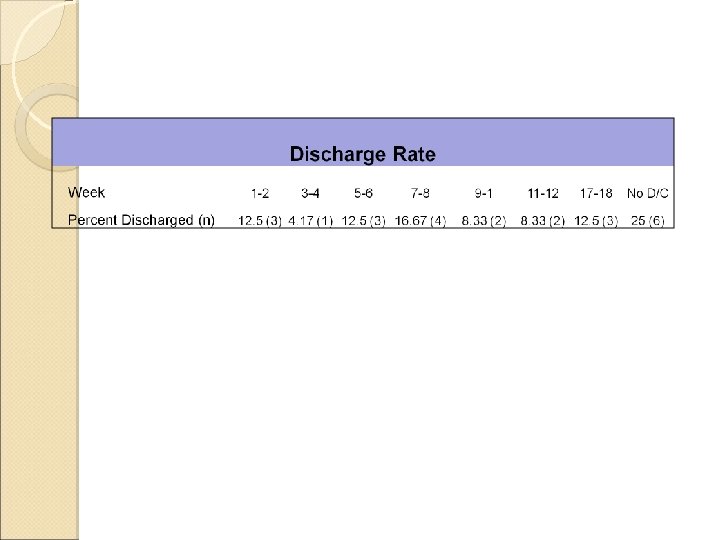
BMT Outcomes � � Participants ◦ ◦ ◦ n=24; Residents of the VA Boston CLC Age: M=74. 75; SD=11. 39 Gender: 95. 8% Male Residential Status: LTC (54. 2%); Rehab (37. 5%); Transitional (8. 3%). Approved by the IRB of the VA Boston Healthcare System. Measures 1. Demographic information: Age, gender, residential status 2. BMT Shift Notes a. ) Frequency of behaviors: b. ) Severity of Behaviors � Method ◦ Medical record review of residents treated in the first six months of BMT implementation (July 28, 2009 -February 1, 2010)
Lessons Learned: Behavior Management �Person-centered care ◦ Implement WITH the resident, not TO the resident �Interdisciplinary ◦ Consider role of MD/PA �Individualization �Consistency �Communication ◦ Team ◦ Ask/Talk to the resident �Dementia-care skills
Lessons Learned: Program Implementation �Identify and include relevant stakeholders ◦ Facility specific ◦ All services ◦ All levels �Union ◦ Include early �Intervention-setting ◦ Resources ◦ Limitations fit
Lessons Learned: Program Implementation �Education ◦ First step to buy-in �Hands-on demonstration ◦ Don’t be afraid to make mistakes �Observe impact and make changes ◦ Be flexible �Sustainability ◦ Repeat education ◦ Leadership support �Policy
Questions
References 1. Alzheimer’s Association (2010). 2010 Alzheimer’s Disease Facts and Figures (2010). Alzheimer’s & Dementia, vol. 6. http: //www. alz. org/alzheimers_disease_facts_figures. asp 2. Hebert, L. E. , Scherr, P. A. , Bienias, J. L. , Bennett, D. A. , & Evans, D. A. (2003). Alzheimer disease in the U. S. population: prevalence estimates using the 2000 census. Arch Neurol, 60, 1119 -1122. 3. Office of the Assistant Deputy Under Secretary for Health (2004). Projections of the prevalence and incidence of dementias including Alzheimer’s disease for the total, enrolled, and patient veteran populations age 65 or over. http: //www. index. va. gov/search/va/va_search. jsp? QT=dementia&SQ=url: http%3 A%2 F% 2 Fwww 4. va. gov%2 FHEALTHPOLICYPLANNING%2 F 4. Kraus, N. A. , & Altman, B. M. (1998). Characteristics of Nursing Home residents-1996. Agency for Health Care Policy and Research, MEPS Research Findings No. 5, AHCPR Pub No. 99 -0006. http: //www. meps. ahrq. gov/mepsweb/data_files/publications/rf 5. shtml 5. Bartels D. J. , Horn, S. D. , Smout, R. J. , Dums, A. R. , Flaherty, E. , Jones, J. K. , Monane, M. , Taler, G. A. , & Voss, A. C. (2003). Agitation and depression in frail nursing home elderly patients with dementia: Treatment characteristics and service. Am J of Geriatr Psych, 11, 231 -238. 6. Chan, D. C. , Kasper, J. D. , Black, B. S. , & Rabins, P. V. (2003). Prevalence and correlates of behavioral and psychiatric symptoms in community-dwelling elders with dementia or mild cognitive impairment: the memory and medical care study. Int J of Geriatr Psyc, 18, 174 -182.
References 7. Burgio, L. D. , Jones, L. T. , Butler, F. , & Engler, B. T. (1988). Behavior problems in an urban nursing home. J of Gerontol Nurs, 14, 31 -34. 8. Brotons, M. & Pickett-Cooper, P. (1996). The effects of music therapy intervention on agitation behaviours of Alzheimer's disease patients. J Music Ther, 33 (1), 2 -18. 9. Conely, L. & Campbell, L. (1991). The use of restraints in caring for the elderly: realities, consequences and alternatives. Nurs Pract, 16, 48 -52. 10. Schneider, L. S. , Dagerman, K. , & Insel, P. S. Efficacy and adverse effects of atypical antipsychotics for dementia: meta-analysis of randomized, placebo-controlled trials. Am J Geriatr Psychiatry. 2006; 14: 191– 210. 11. Schneider, L. S. , Dagerman, K. S. , & Insel, P. Risk of death with atypical antipsychotic drug treatment for dementia: meta-analysis of randomized placebo-controlled trials. JAMA. 2005; 294: 1934– 1943. 12. Kales, H. C. , Valenstein, M. , Kim, H. M. , Mc. Carthy, J. F. , Ganoczy, D. , Cunningham, F. , & Blow, F. C. (2007). Mortality risk in patients with dementia treated with antipsychotics versus other psychiatric medications. American Journal of Psychiatry, 164, 1568 – 76. 13. Cotter, V. T. (2005). Restraint free care in older adults with dementia. Keio J Med, 54, 80 -84. 14. Cohen-Mansfield, J. (2001). Nonpharmacologic interventions for inappropriate behaviors in dementia. American Journal of Geriatric Psychiatry, 9, 361 -381. 15. Tarpy, R. M. (1997). Contemporary Learning Theory and Research. Mc. Graw Hill: Boston. 16. Proctor, R. , Burns, A. , Powell, H. S. , Tarrier, N. , Faragher, B. , Richardson, G. , et al. (1999). Behavioural management in nursing and residential homes: A randomized controlled trial. Lancet, 354, 26 -29. �
References 17. Teri, L. , Huda, P. , Gibbons, L. , Young, H. , van Leynseele, J. (2005) STAR: A dementia-specific training program for staff in assisted living residences. The Gerontologist, 45, 686 -693. 18. Lichtenberg, P. A. , Kemp-Havican, J. , Mac. Neill, S. E. , & Schafer Johnson, A. (2005). Pilot study of behavioral treatment in dementia care units. The Gerontologist, 45, 406410. 19. Lawton, M. P. , & Nahemow, L. Ecology and the aging process. (1973). In: The Psychology of Adult development and Aging, Eisdorfer L, Lawton MP. (eds). Washington DC, 619 -674. 20. Camberg, L. , Woods, P. , Ooi, W. L. , Hurley, A. , Volicer, L. , Ashley, J. , Odenheimer, G. & Mc. Intyre, K. (1999). Evaluation of Simulated Presence: a personalized approach to enhance well-being in persons with Alzheimer's disease. J Am Geriatr Soc, 47(4), 44652. 21. Boyle, M. , Bayles, K. A. , Kim, E. , Chapman, S. B. , Zientz, J. , Rackley, A. , Mahendra, N. , Hopper, T. , & Cleary, S. J. (2006). Evidence-based practice recommendations for working with individuals with dementia: Simulated Presence Therapy. Journal of Medical Speech-Language Pathology, 14 (3), xiii-xxi. 22. Volicer, L. , Simard, J. , Pupa, J. , Medrek, R. , & Riordan, M. (2007). Effects of continuous activity programming on behavioral symptoms of dementia. J American Medical Directors Association, 7(7), 426 -431. 23. Algase, D. , Beck, C. , Kolanowski, A. , Whall, A. , Berent, S. , Richards, K. , & Beatty, E. (1996). Need-driven dementia-compromised behavior: an alternative view of disruptive behavior. Am J of Alzheimer’s Dis Other Demen, 11, 10 -19. 24. Cohen-Mansfield J. (2000). Nonpharmacological management of behavioral problems in persons with dementia: the TREA model. Alzheimer’s Care Quarterly, 1, 22 -34.
- Slides: 39