The Role of Radiation Therapy in the Management





- Slides: 34
The Role of Radiation Therapy in the Management of Prostate Cancer Mark L. Merlin, M. D. Radiotherapy Clinics of Georgia 7/14/2010
• Radiation oncology is a field of medicine that specializes in the destruction of cancer cells using various forms of radiation – Balance normal tissue damage versus eradication of cancer • Radiation therapy works by either directly killing cancer cells or by damaging their DNA • Normal tissue cells have a mechanism for repairing DNA damage • Cancer cells have a diminished ability to repair this sub lethal damage
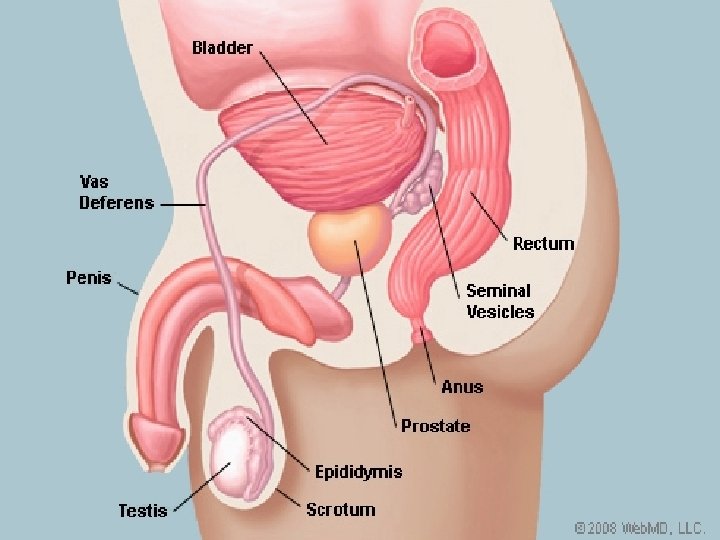
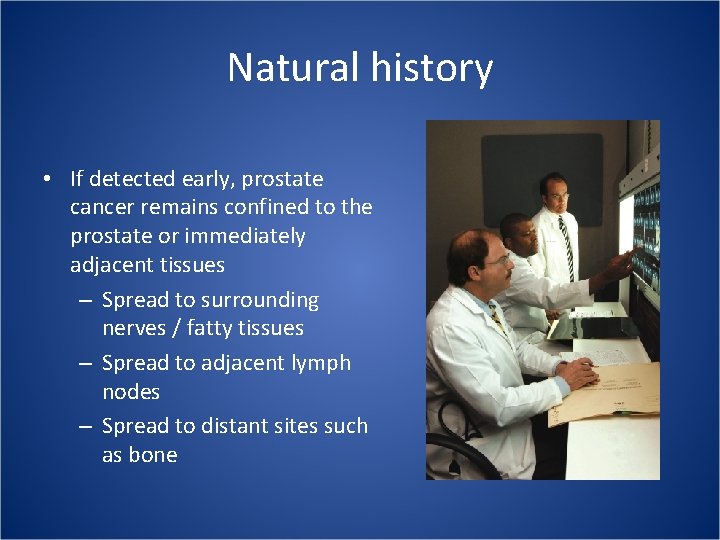
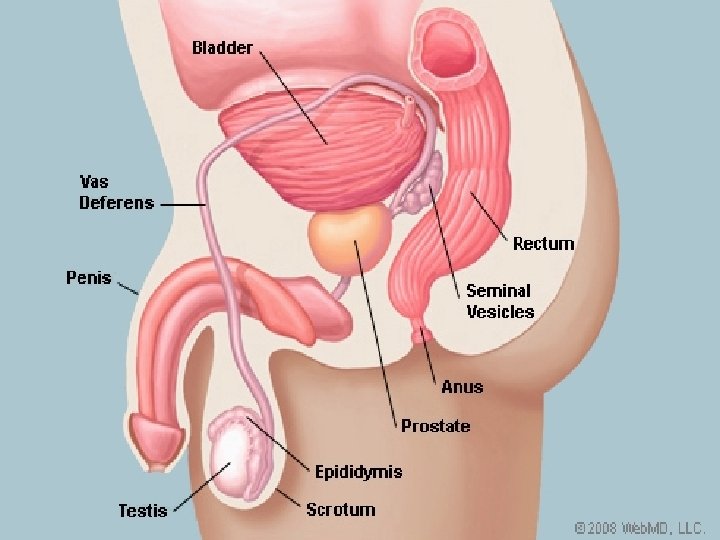
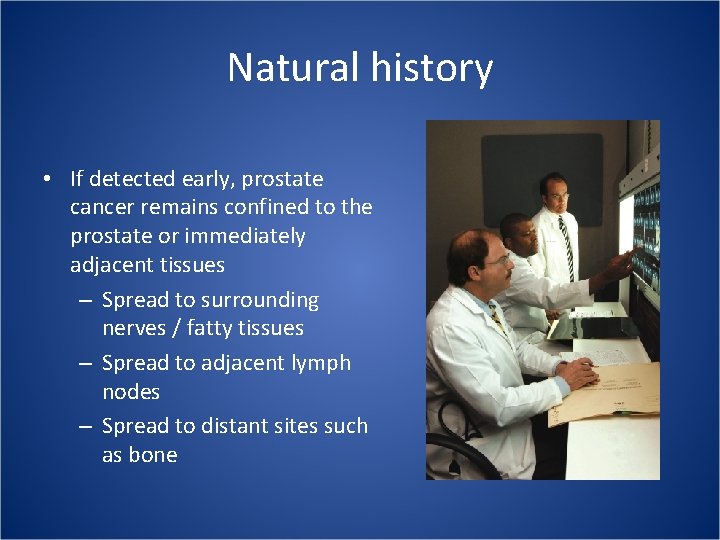
Natural history • If detected early, prostate cancer remains confined to the prostate or immediately adjacent tissues – Spread to surrounding nerves / fatty tissues – Spread to adjacent lymph nodes – Spread to distant sites such as bone
Radiation versus Surgery • Data is retrospective • Patient selection varies • Overall data does not suggest one option is better than another • Some clinical situations may benefit more from one type of therapy • Side effects vary significantly • Patients should research all options • Focus on cure rates, side effects, and quality of life issues • Centers of excellence
Radiation therapy options • External beam therapy with photons - IMRT (Intensity Modulated Radiation Therapy) • Brachytherapy – Permanent or temporary seeds • Brachytherapy / External beam therapy • Particle therapy – Protons, Neutrons • Stereotactic radiation – Cyberknife, Tomotherapy
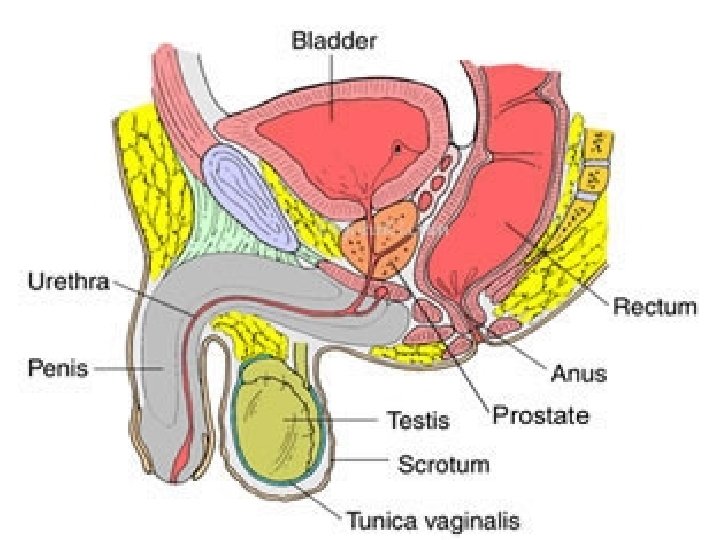
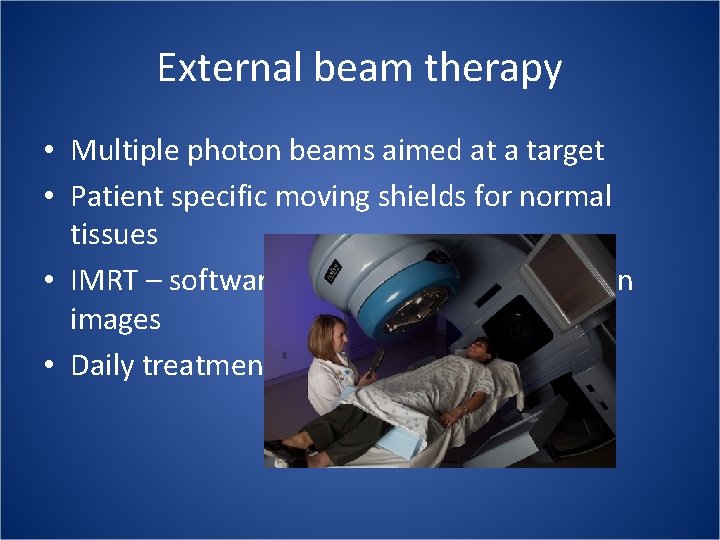
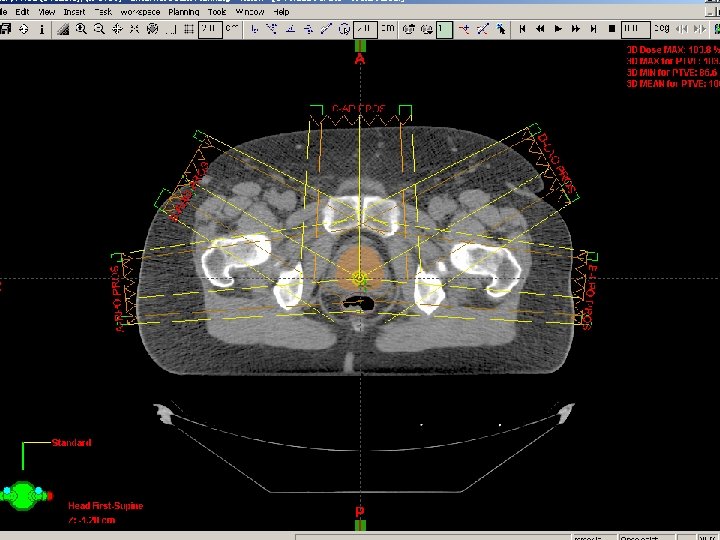
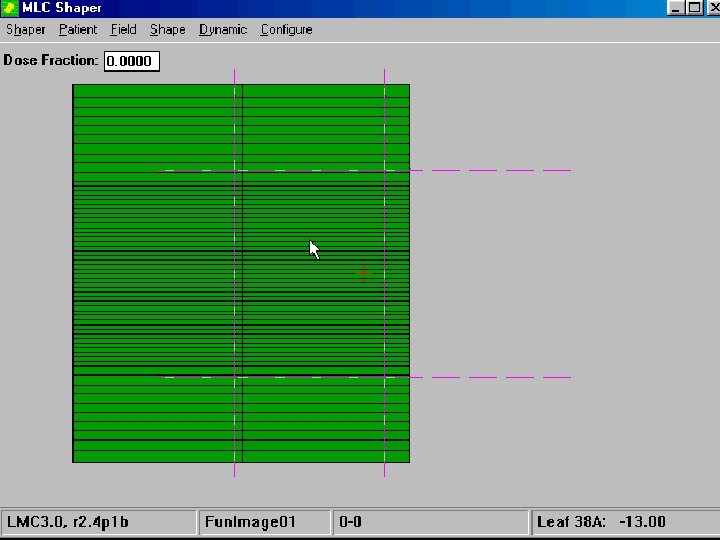
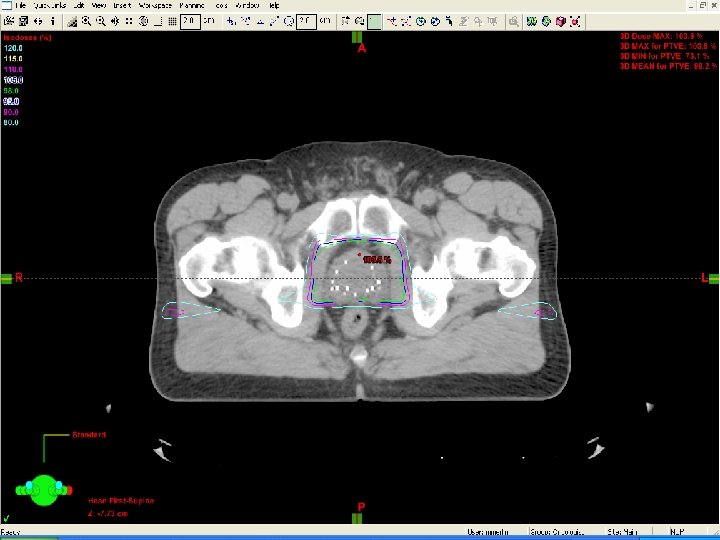
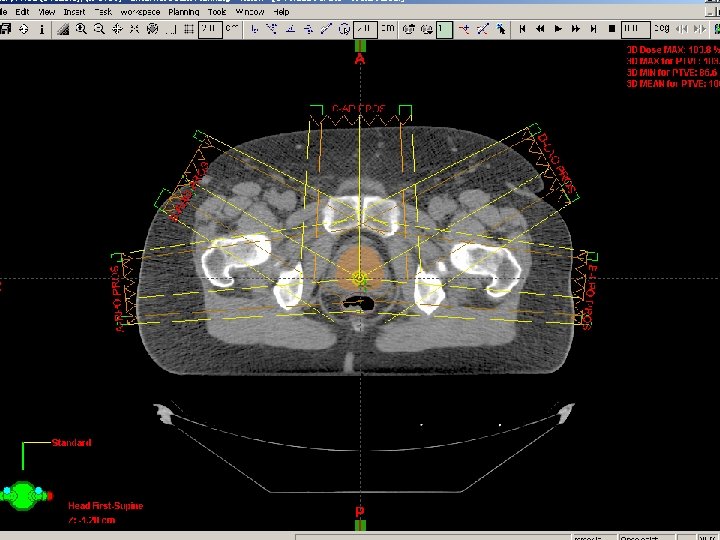
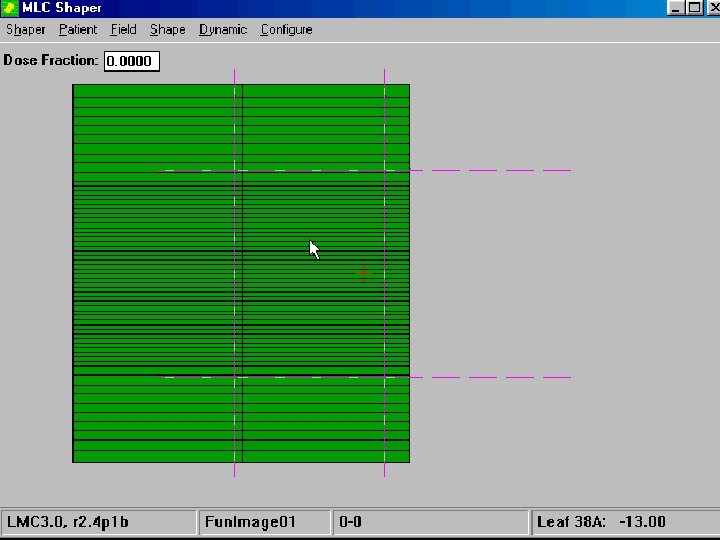
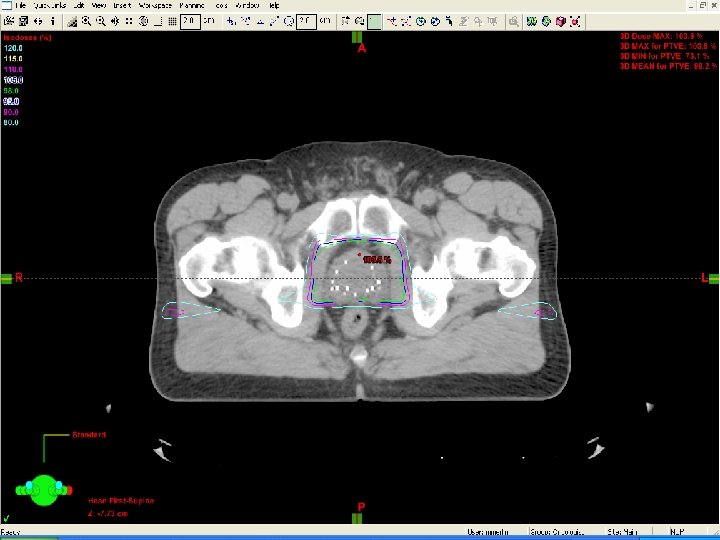
External beam therapy • Multiple photon beams aimed at a target • Patient specific moving shields for normal tissues • IMRT – software planning based on CT scan images • Daily treatment
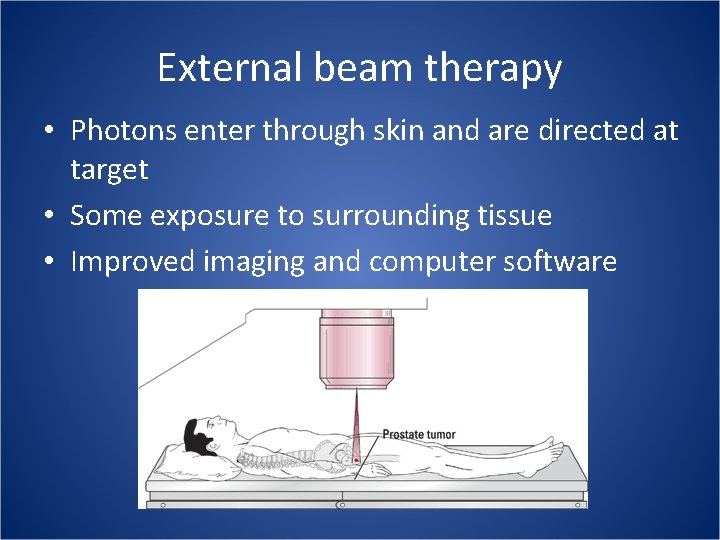
External beam therapy • Photons enter through skin and are directed at target • Some exposure to surrounding tissue • Improved imaging and computer software



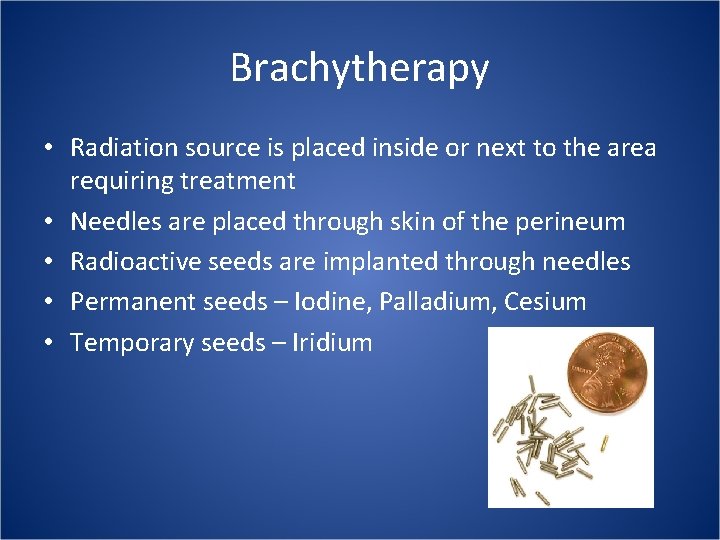
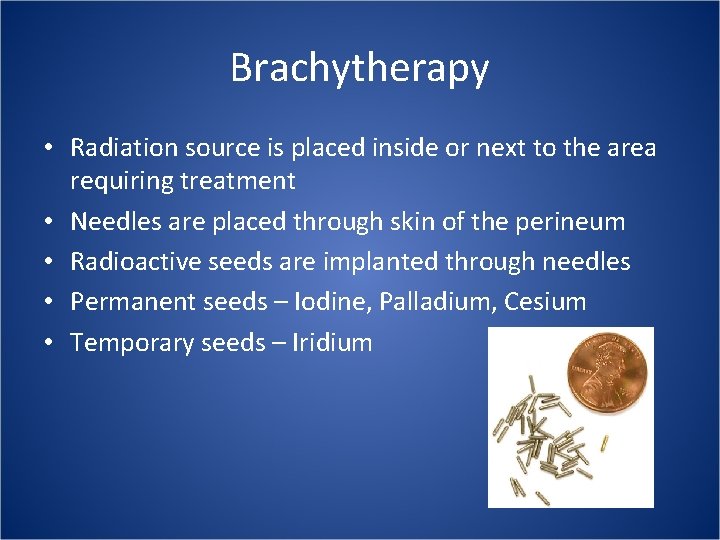
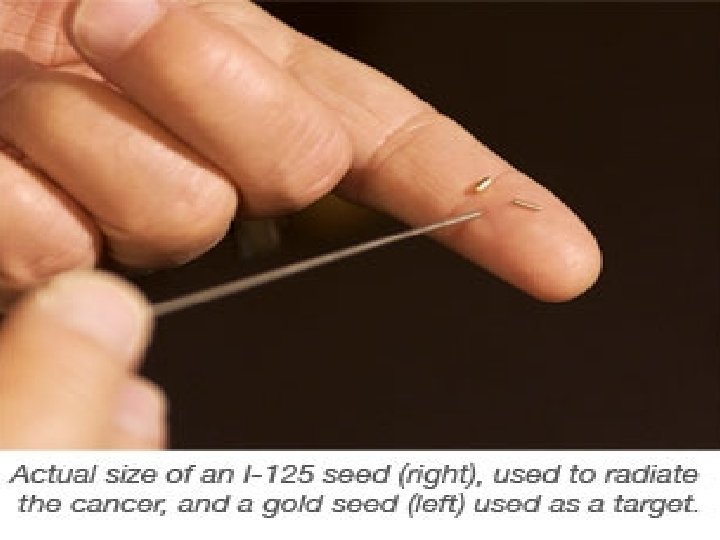
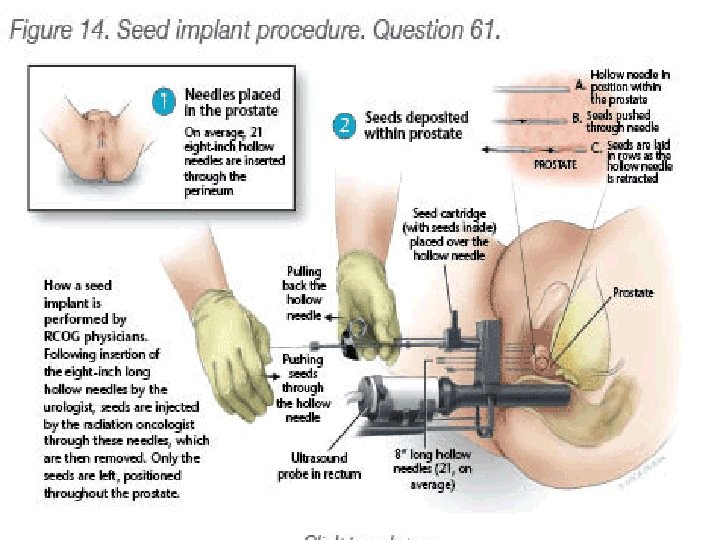
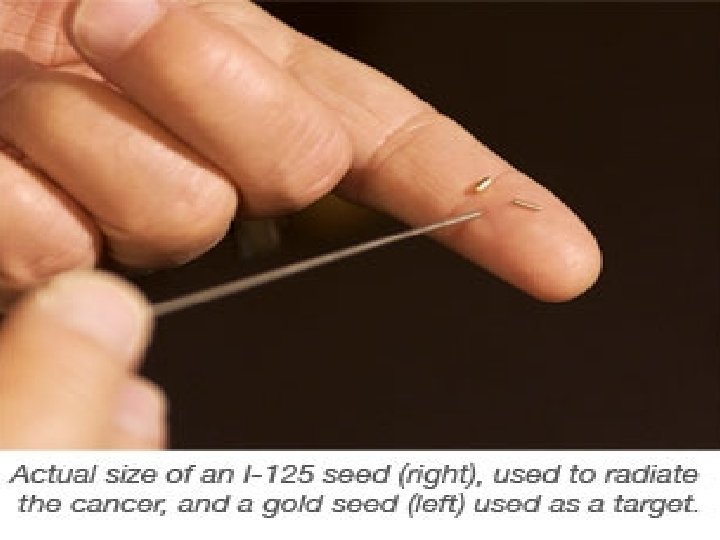
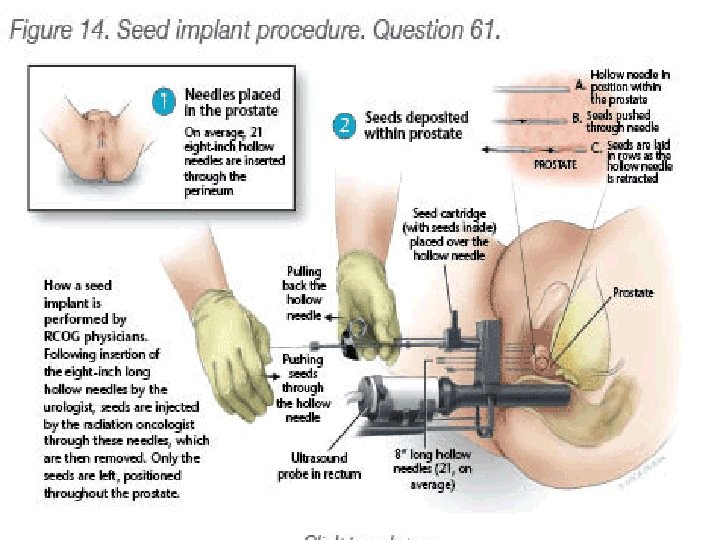
Brachytherapy • Radiation source is placed inside or next to the area requiring treatment • Needles are placed through skin of the perineum • Radioactive seeds are implanted through needles • Permanent seeds – Iodine, Palladium, Cesium • Temporary seeds – Iridium
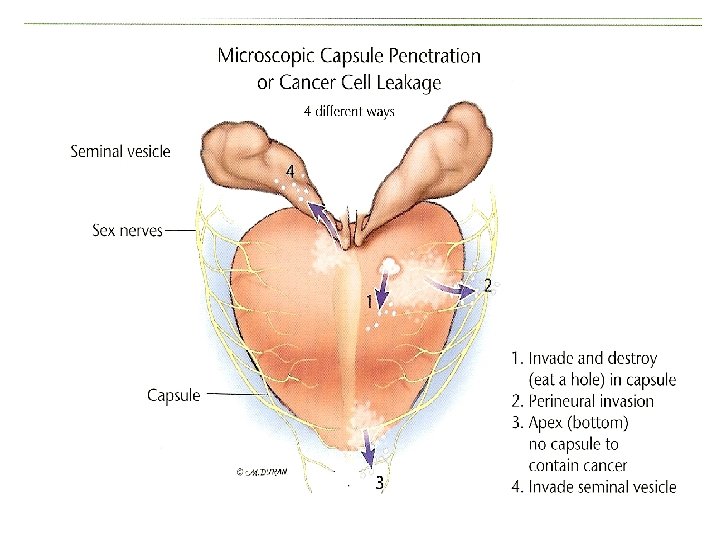
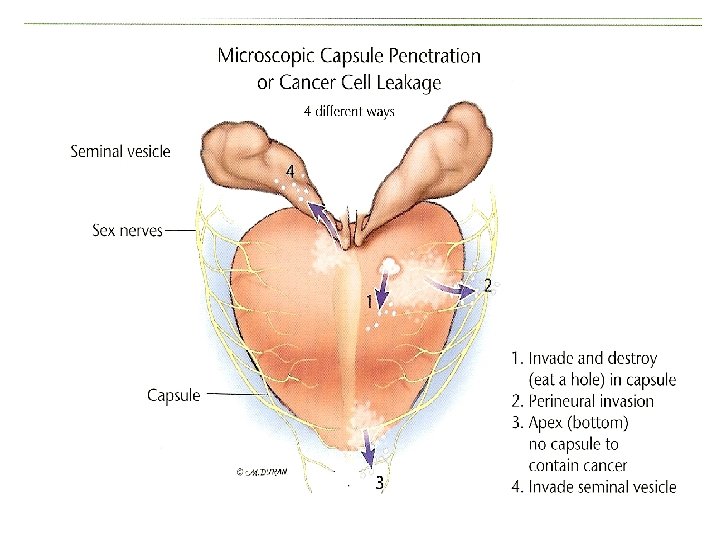
Brachytherapy • Best used alone if the chance for extracapsular spread is low • Chance for extracapsular spread relies on certain clinical factors: – PSA – Gleason score – Number of positive biopsies – Stage (findings on digital rectal exam) – Presence of perineural invasion
Brachytherapy combined with External Beam therapy • Allows more intense radiation dose to prostate through brachytherapy • Allows treatment with external radiation to encompass some areas around prostate for potential spread • Combination may overcome limits of either modality on its own
Stereotactic Radiation • Focused radiation beams targeting a well defined tumor using extremely detailed imaging scans – Cyberknife – Tomotherapy • Cure rate data following treatment is not available due to short follow-up

Particle therapy • Special case of external beam radiation where the particles are protons or heavier ions • Dose increases while the particle penetrates the tissue up to a maximum that occurs near the end of the particle’s range • The dose then drops to almost zero
Proton beam therapy § Loma Linda 2004 article § 1255 pts treated with protons for prostate cancer § Overall cure rate 73% § Massachusetts General 2008 article § Recommended further study on protocol before rapid adoption § Cited tremendous increase in price for machines with no proven benefit over current linear accelerators § Protocols for dose, treatment setup, and parameters for shielding uninvolved tissues remain in evolution § Standard long term radiation effects on urinary and rectal function do exist
Hormone therapy combined with radiation • Two large randomized studies have shown that patients with locally advanced prostate cancer treated with standard external beam therapy have higher cure rates if they also receive testosterone suppression • EORTC (2002) – GS 8 -10 and T 1/T 2 or any T 3/T 4 pts – RT alone vs RT + LHRH x 3 yrs – 5 yr OS 62% vs 78% • RTOG (2005) – T 3 or N 1 – RT alone vs. RT + LHRH x 28 months – 10 yr absol surv 39% vs. 49%
• • • Hormone therapy side effects Hot flashes Decrease in muscle tone Weight gain Impotence Decreased libido Fatigue Emotional lability Increased risk of cardiovascular death Breast enlargement / tenderness
Radiation following radical prostatectomy • Following surgical removal of the prostate, a careful pathological analysis is done • Organ confined vs. not confined (seminal vesicle involvement, capsule penetration, or margin involvement) • Patients with certain features have a higher risk of cancer recurrence within the prostate bed
Radiation following radical prostatectomy • In the past, many patients and physicians have followed the PSA level after surgery • Recent randomized trials suggest that those patients with high-risk features should be evaluated for immediate radiation to the prostate bed • Improved survival rates have been found with immediate vs. delayed radiation – 10 yr OS 71% vs. 61% • Standard of care is to evaluate all high risk patients following surgery for possible radiation therapy
Radiation side effects • Acute effects (during treatment) – Urinary – Rectal – General • Late effects (months – years after treatment) – Urinary / Sexual – Rectal – Secondary Cancer
Get educated! • • • Do your own research Talk with friends and family Use the internet Get second opinions Read prostate books literature
• Organizations such as The Prostate Net help to raise public awareness and promote education of available resources • Evidence based medicine • Centers of excellence with database of prior patients

Any Questions?
Contact Information Mark L. Merlin, M. D. Radiation Oncologist Phone: 404 -633 -5606 Ext. 180 Email: mmerlin@rccancercenters. com