The reward pathway The reward pathway the ventral












- Slides: 48
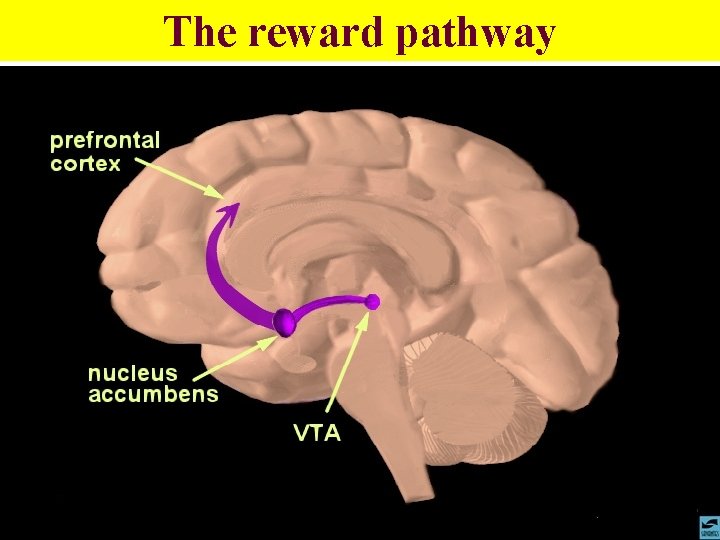
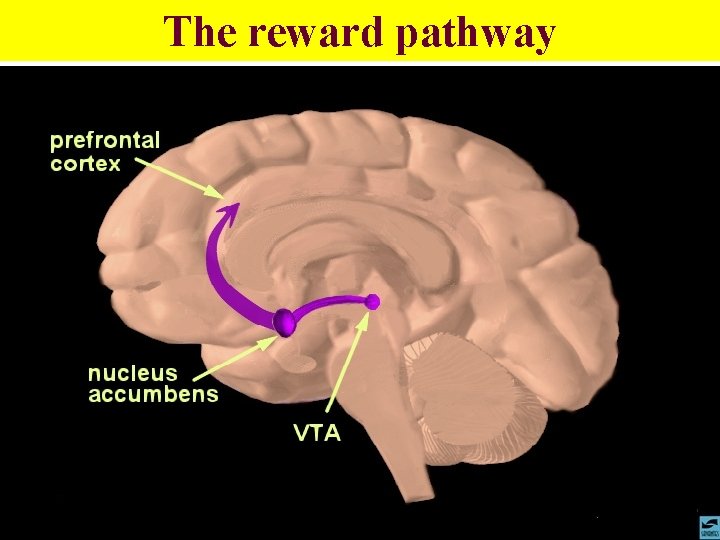
The reward pathway
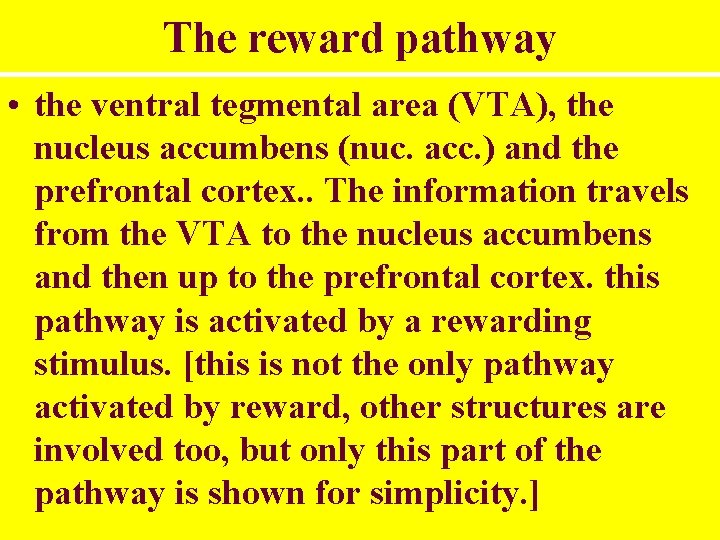
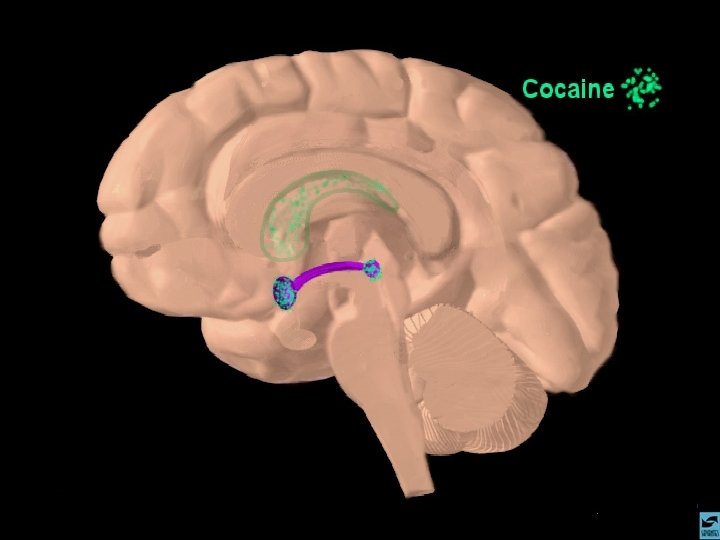
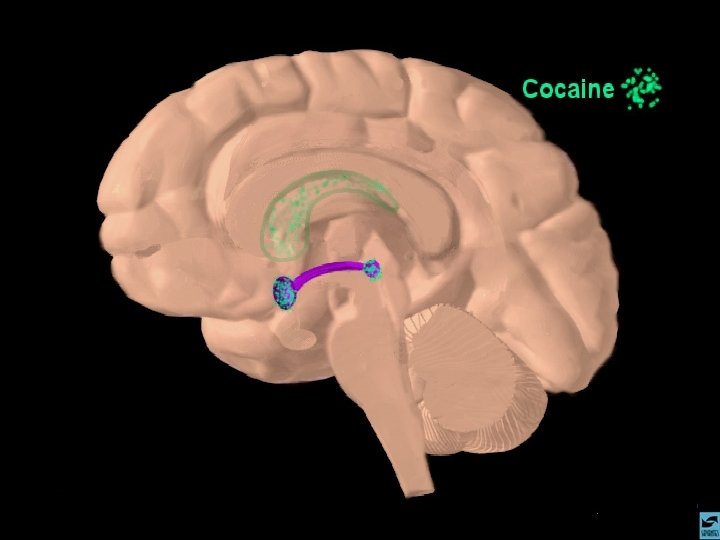
The reward pathway • the ventral tegmental area (VTA), the nucleus accumbens (nuc. acc. ) and the prefrontal cortex. . The information travels from the VTA to the nucleus accumbens and then up to the prefrontal cortex. this pathway is activated by a rewarding stimulus. [this is not the only pathway activated by reward, other structures are involved too, but only this part of the pathway is shown for simplicity. ]
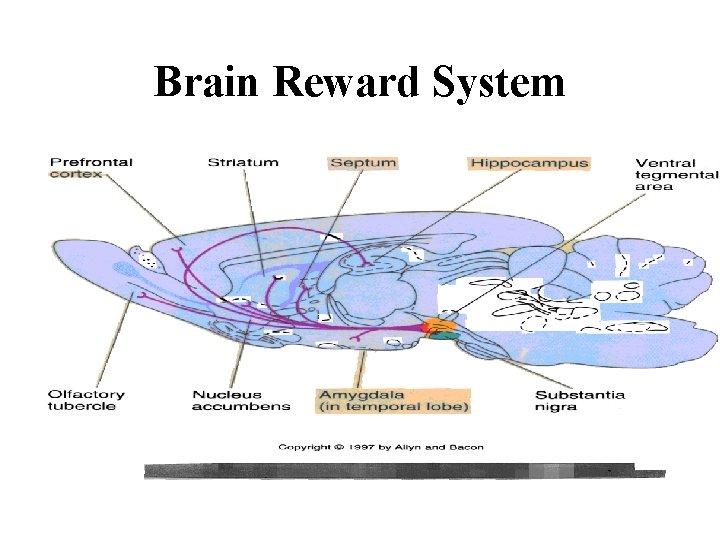
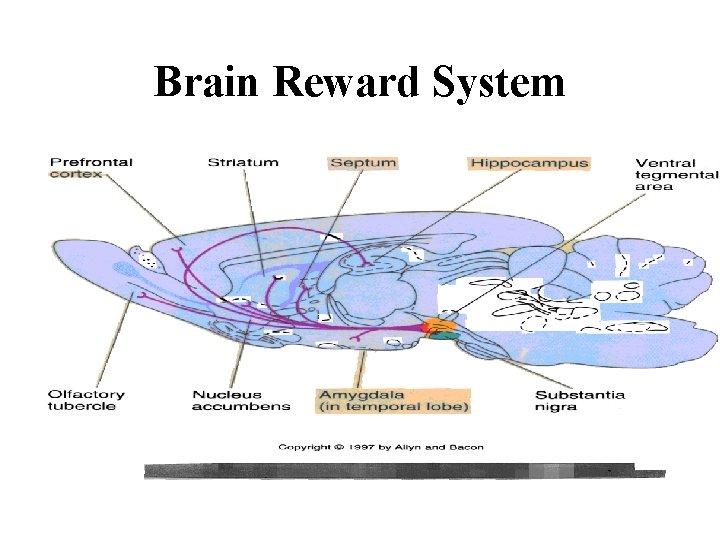
Brain Reward System
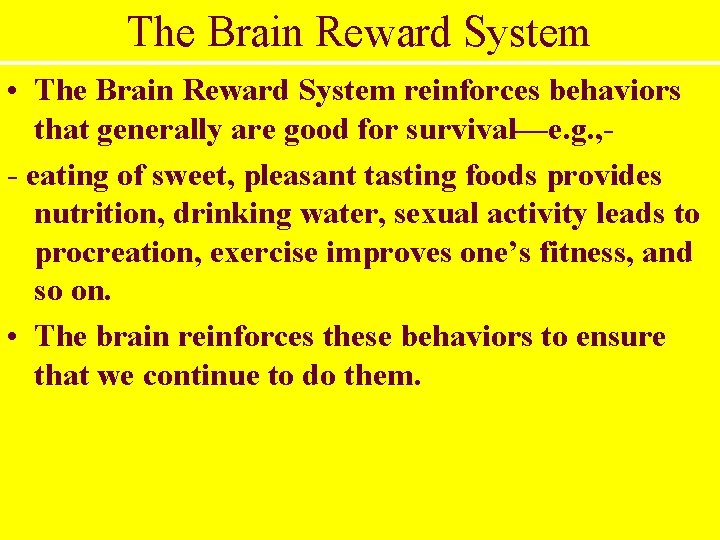
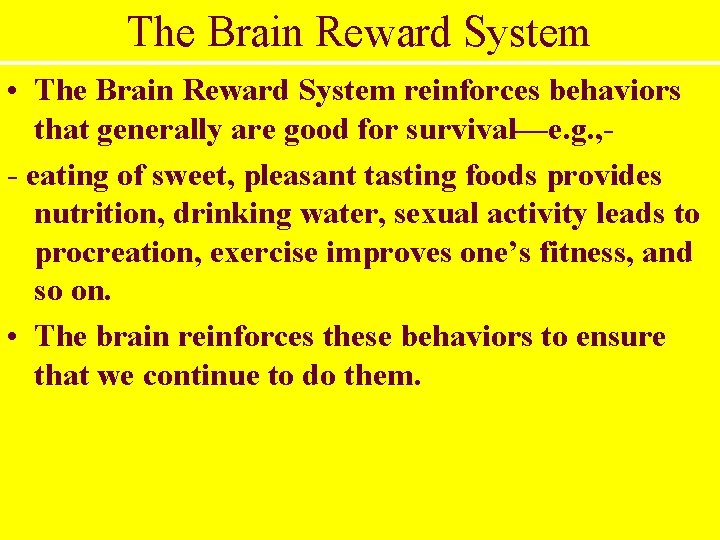
The Brain Reward System • The Brain Reward System reinforces behaviors that generally are good for survival—e. g. , - eating of sweet, pleasant tasting foods provides nutrition, drinking water, sexual activity leads to procreation, exercise improves one’s fitness, and so on. • The brain reinforces these behaviors to ensure that we continue to do them.
Brain Reward System • Drugs of dependence, like heroin, cause long lasting, possibly permanent, changes to the nerves in the area of the Brain Reward System. • This is why addiction is difficult to overcome and, why relapse occurs so often, and why it sometimes takes many years before addicts are successful in permanently stopping drug use.
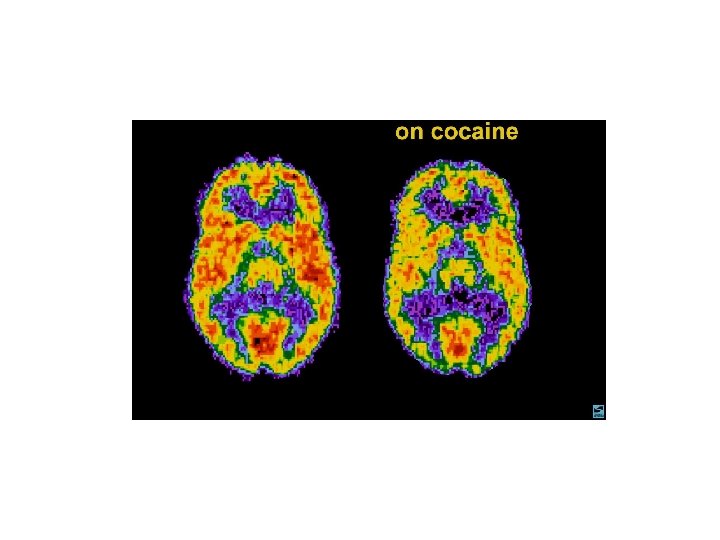
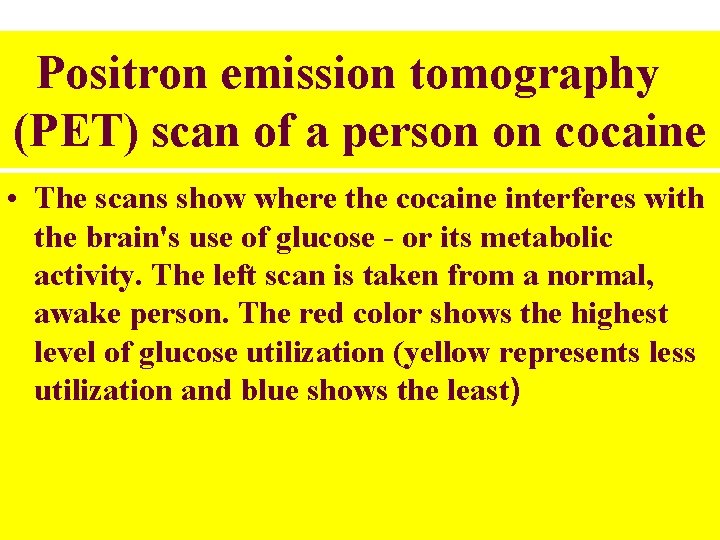
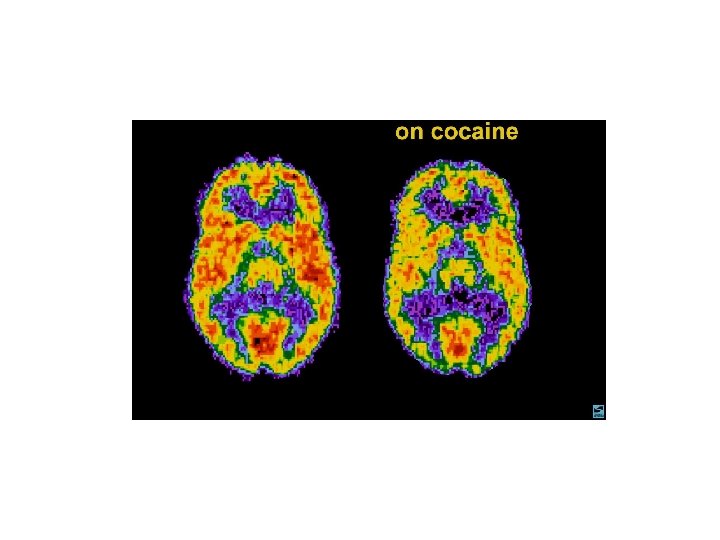
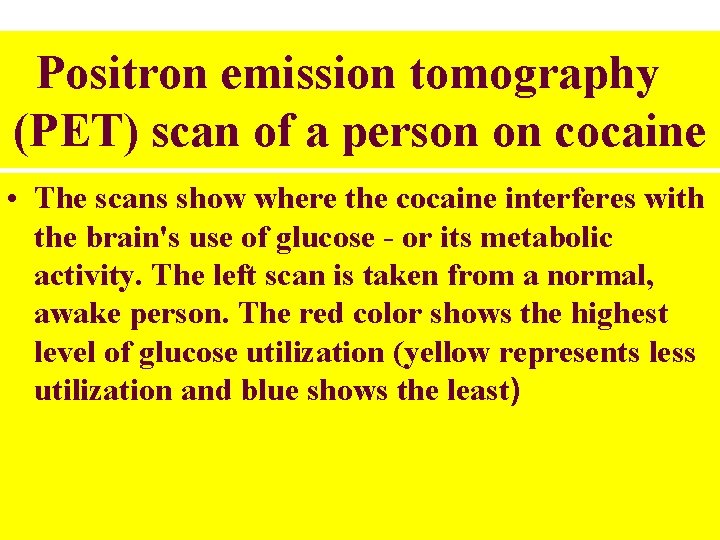
Positron emission tomography (PET) scan of a person on cocaine • The scans show where the cocaine interferes with the brain's use of glucose - or its metabolic activity. The left scan is taken from a normal, awake person. The red color shows the highest level of glucose utilization (yellow represents less utilization and blue shows the least)
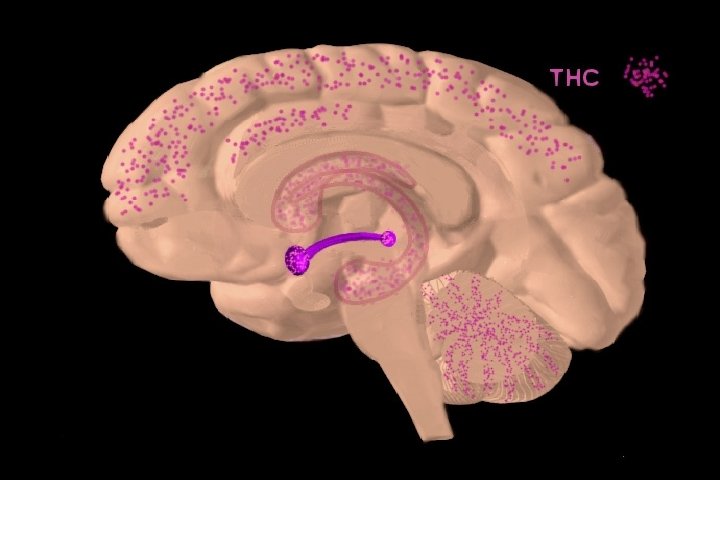
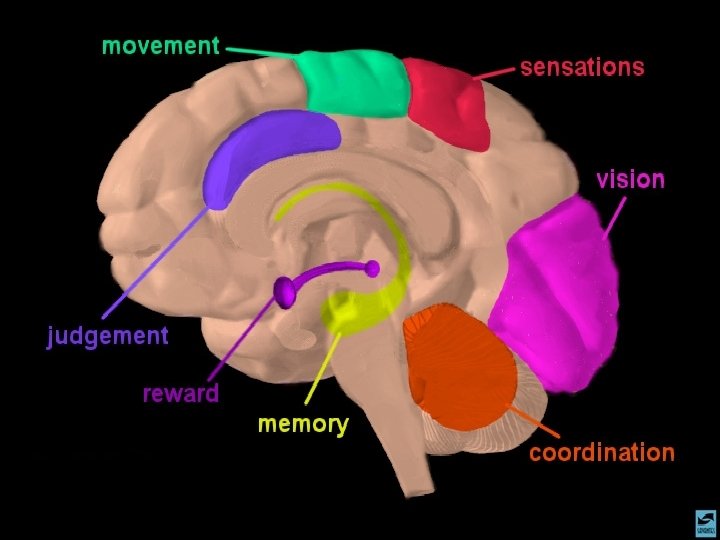
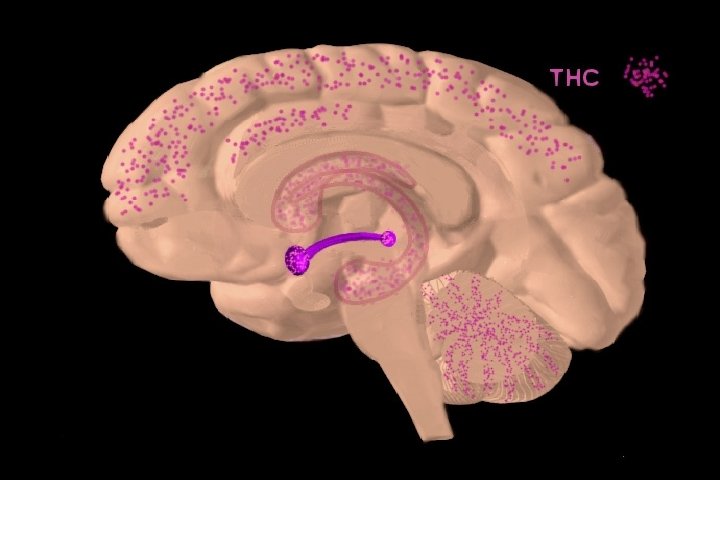
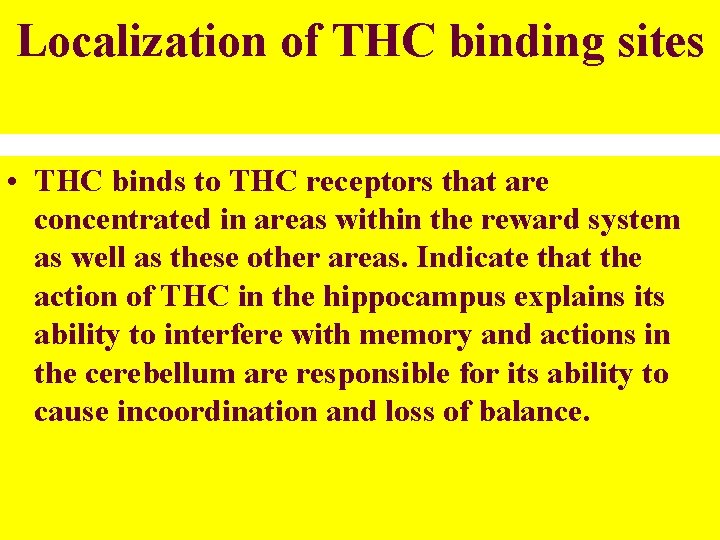
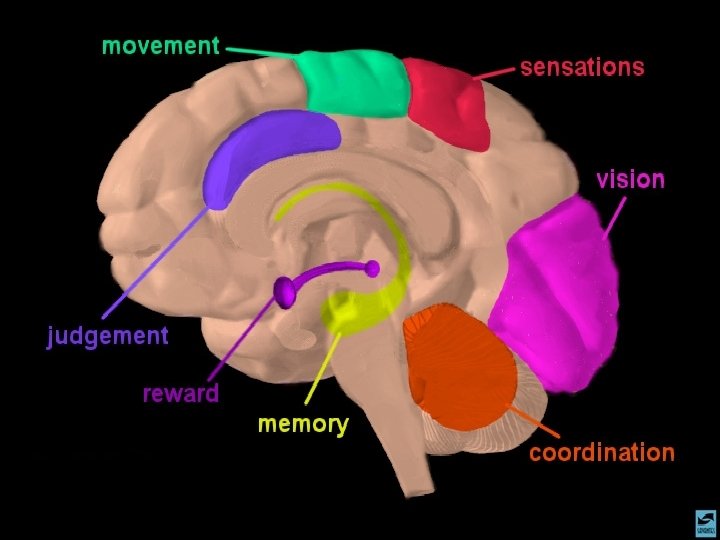
Localization of THC binding sites • THC binds to THC receptors that are concentrated in areas within the reward system as well as these other areas. Indicate that the action of THC in the hippocampus explains its ability to interfere with memory and actions in the cerebellum are responsible for its ability to cause incoordination and loss of balance.






Treatment Options • Methadone • Clonidine (Alpha-adrenergic receptor agonist) • Ultra rapid detox • Methadone maintenance • LAMM (Levo-alpha-acetylmethadol).
Rapid Detox • Substance abuse and dependency is a major public health concern in the United States because of the economic and human costs. • Current drug abuse treatment approaches, developed primarily during the 1960’s and 1970’s, have changed very little since their inception. The changes that have occurred in treatment in the last decade have been primarily structural and have been propelled by the tide of managed care reforms rather than the emergency of treatment models.
Common trade names for rapid detox treatment programs • • Rapid detox (RO) Neuroregulated detox Neuro-adaptation treatment OADUSA (opioid antagonist agent detox under sedation or anesthesia) IND (intensive narcotic detox) UROD (Ultra-rapid opiate detox) RAND (rapidly accelerated narcotic detox) KIYSR (kick in your sleep rapid relief)
Rapid Detox • Rapid detox procedures has been done by employing two novel approaches. • First, general anesthesia is to ensure no subjective distress is felt. • Second, use of large dosages of opiate antagonist in order to rapidly and completely remove the exogenous opiate drugs from the opiate receptors in the brain. • Because patient can not feel no subjective distress from withdrawal, detox can be completed within few hours (46) rather than 3 to 15 days with traditional detox.
• It is important to differentiate between: • Rapid detox, similar to traditional detox strategies, but patient receives more sedation than usual during the withdrawal. sedation is accomplished through the use of benzodiazepines and can decrease the time of withdrawal by a day or two. The sedation is done to minimize the subjective distress of withdrawal symptoms allowing detox to progress more rapidly. • Ultra-rapid detox. An approach using general anesthesia to induce complete unconsciousness, thus ensure complete comfort during detox.
Procedures • Rapid detox programs require either overnight monitoring or one day program where individuals checks-in early in the morning and leaves at the same day. • All programs require pre-evaluation entails drug history, psychological evaluation, medical history and current health status evaluation. • Start I. V. and induce general anesthesia.
• Ultra-rapid detox (UROD) has become potent protected treatment name however literature still refer to it as rapid detox.
• Most programs offering rapid detox require an anesthesiologist to be present to monitor the anesthesia and perform the procedure in the location (hospital) where emergency services are quickly available should complication arise. • Once general anesthesia has been induced and no subjective withdrawal discomfort felt by the patient. opiate receptor blockade is accomplished with the use of opiate antagonist agents. • Three common opiate antagonists exist: Naltrexone, naloxone and nalmefene. By far naltrexone is the most widely used opiate antagonist during rapid detox.
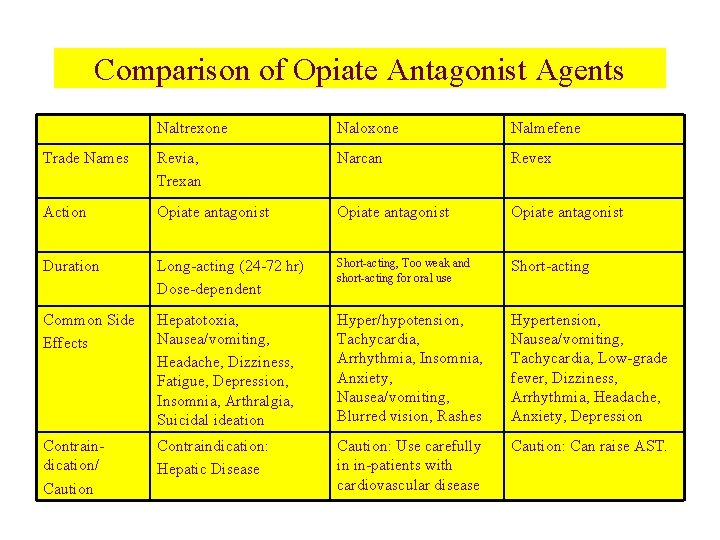
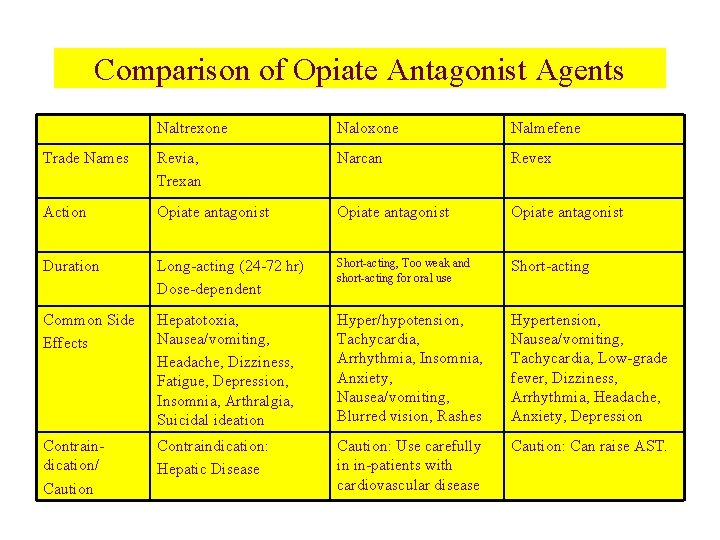
Comparison of Opiate Antagonist Agents Naltrexone Naloxone Nalmefene Trade Names Revia, Trexan Narcan Revex Action Opiate antagonist Duration Long-acting (24 -72 hr) Dose-dependent Short-acting, Too weak and short-acting for oral use Short-acting Common Side Effects Hepatotoxia, Nausea/vomiting, Headache, Dizziness, Fatigue, Depression, Insomnia, Arthralgia, Suicidal ideation Hyper/hypotension, Tachycardia, Arrhythmia, Insomnia, Anxiety, Nausea/vomiting, Blurred vision, Rashes Hypertension, Nausea/vomiting, Tachycardia, Low-grade fever, Dizziness, Arrhythmia, Headache, Anxiety, Depression Contraindication/ Caution Contraindication: Hepatic Disease Caution: Use carefully in in-patients with cardiovascular disease Caution: Can raise AST.
Treatment Indications • • Addiction to opiate agents Motivated for treatment No co-morbid health condition Failure of past traditional detox programs Normal liver function lab values Normal thyroid function lab values Limited cardiovascular risk factors.

Treatment contraindications • Poly-substance abuse to primarily nonopiates • Little internal motivation • Medically compromised or unstable • No attempts at detox • Liver disease • Thyroid disease • Cardiovascular disease.
Advantages of ultra-rapid detox • Minimizing the very clinical significant, subjectively distressing withdrawal symptoms of opiate addiction. • Rapid detox occurs at the neuroreceptor level and affords the patient an opportunity to start intensive follow up immediately while feeling physically capable to engage in ongoing treatment.
• Confidentiality can be facilitated when patients do not require protracted hospitalization, making treatment more acceptable to some. • Continuous use of opiate antagonists post detox affords the patient a measure of protection against relapse and decreases cravings and increases the likelihood of successful treatment.
Intensive follow up counseling is required after the rapid detox to address needed lifestyle changes, psychological factors and continued abstinence.
Disadvantages of ultra-rapid detox • Risks related to general anesthesia use the risk of death associated with general anesthesia is 1 in 250, 000 and risk of adverse events rises to 1 in 10, 000. • Rapid detox accomplishes medical detox or removal of the physiological effects of the opiate. It does little to affect the physiological withdrawal syndrome, and substantial psychological support and counseling are required for the patient to maintain a drug-free lifestyle.
• Because rapid detox is considered experimental, insurance companies do not cover the cost. • Lack of reliable and valid empirical studies regarding the efficacy of the treatment.
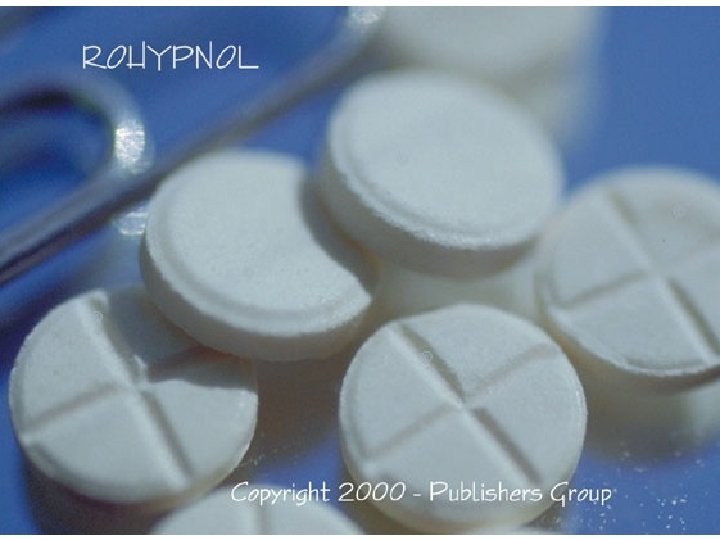
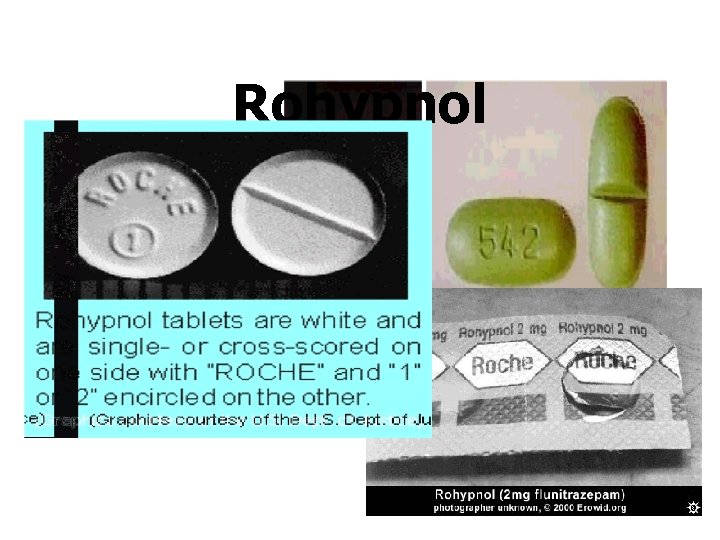
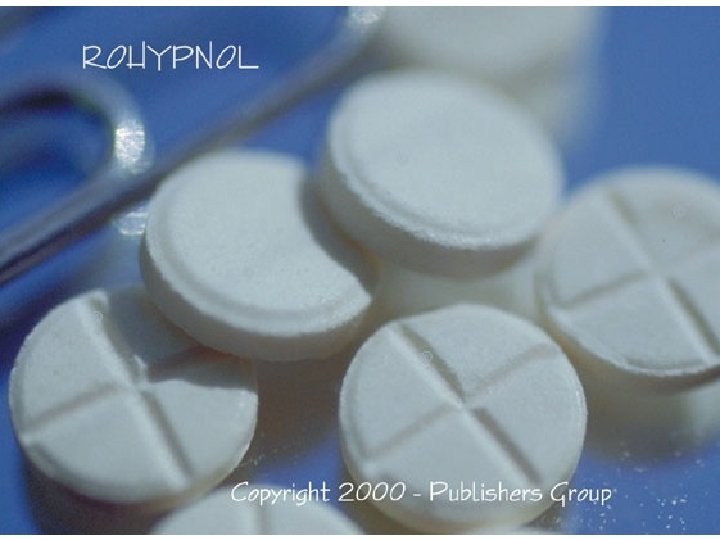
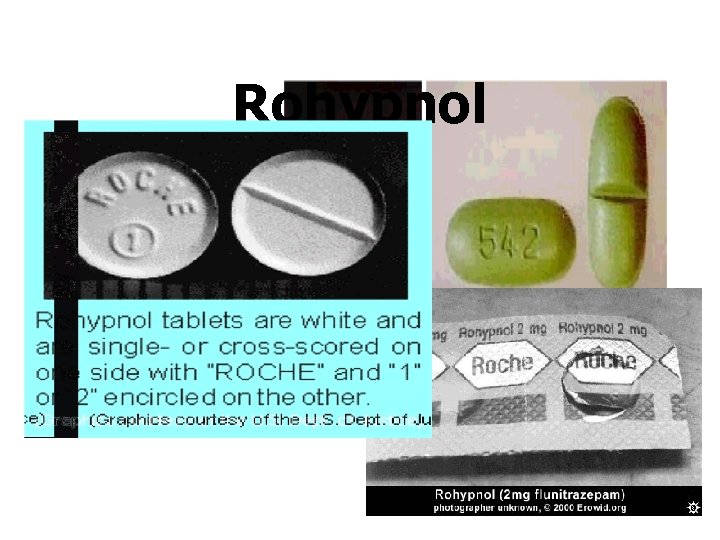
Rohypnol

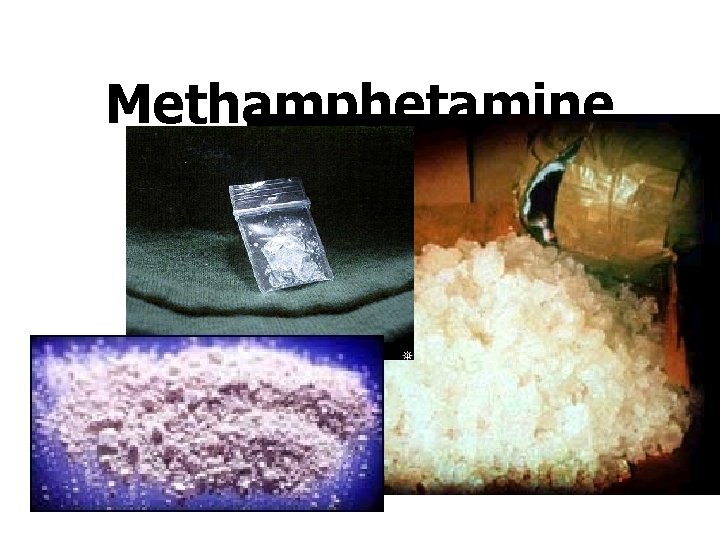
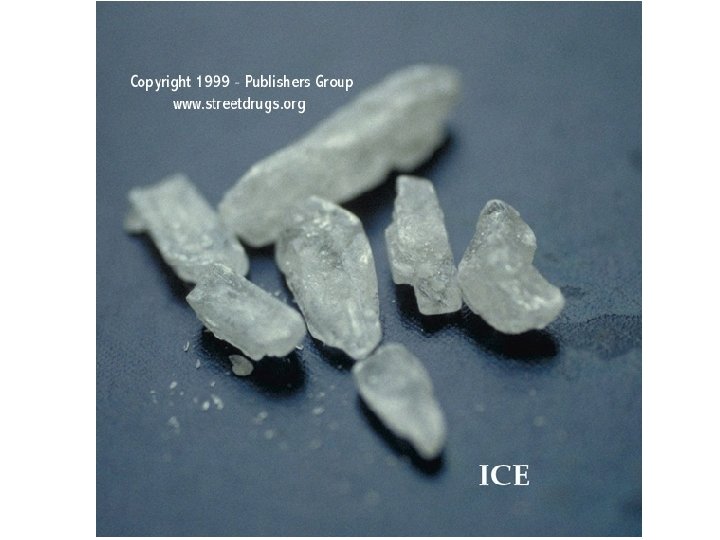
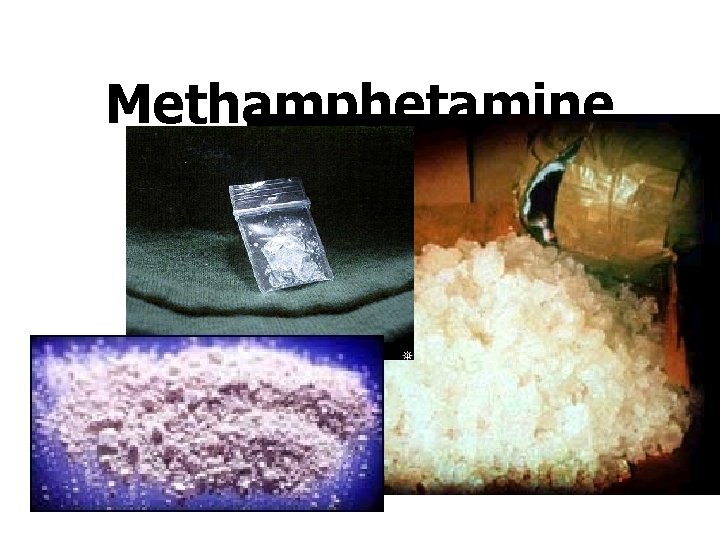
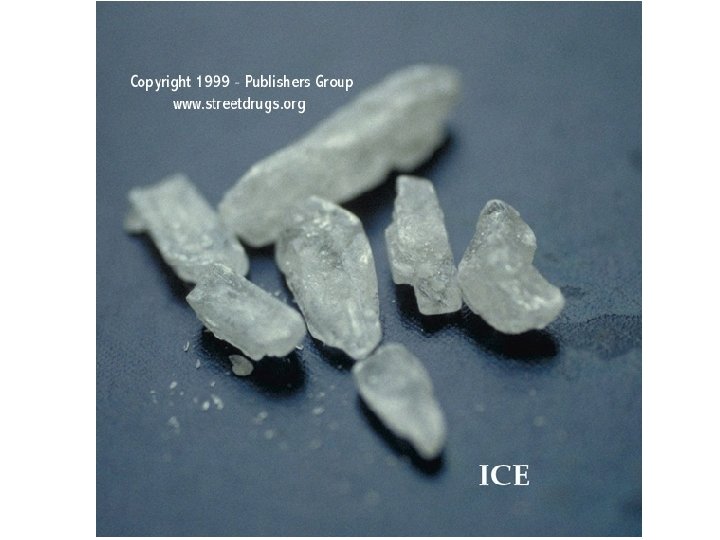
Methamphetamine

LSD

GHB (Gamma-Hydroxybutyrate)

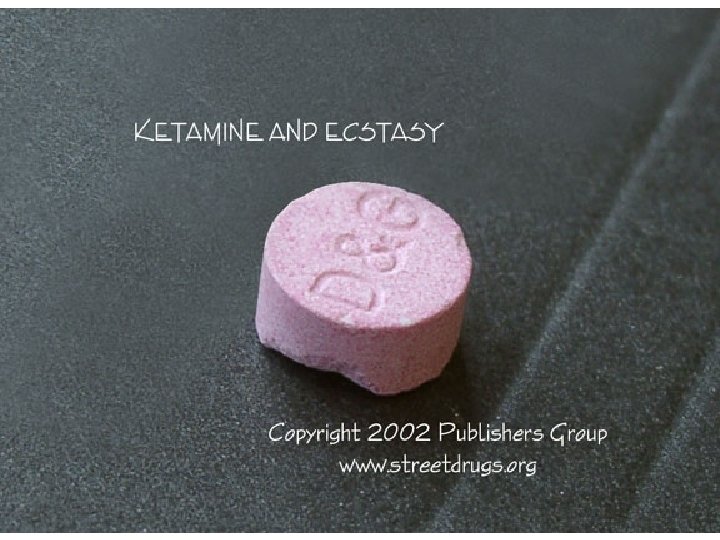
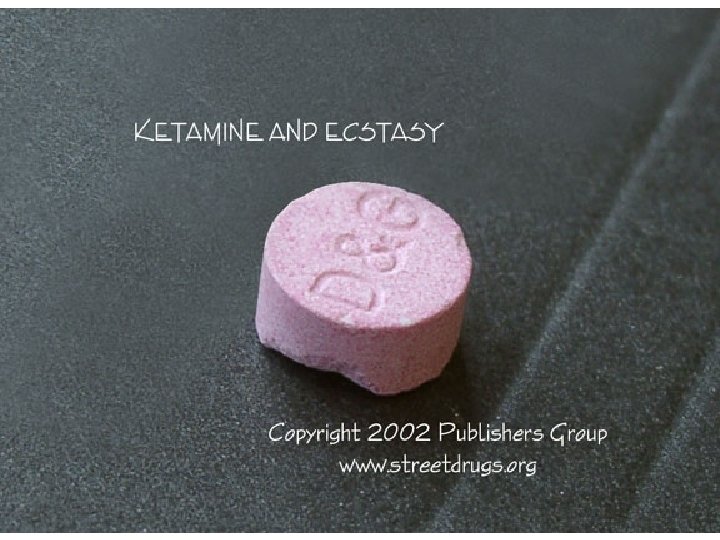
Ketamine
Khat • Contains two psychoactive compounds: cathinone and cathine.
