The results of cementless cups HAP or Ti
















- Slides: 85
The results of cementless cups (HAP or Ti) with additional divergent pegs and acetabular reconstruction with graft in failed THA The concept of “migration en bloc” (1993) JL. Lerat, C. Falaise LYON - France EFORT Congress (June 2001 - Rhodes)

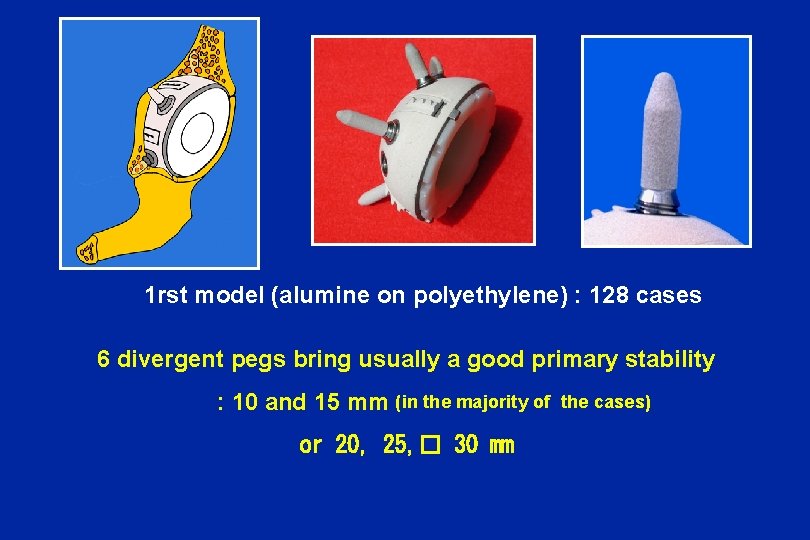
Special Cup with pegs for revision 1 st model : «Spring» ( Landanger-Depuy 1993 - 2000 ) • • • Metallic cup ( Ti ). Hydroxyapatite coating 6 holes for 6 pegs fixed with the cup by threading Alumine on polyethylene
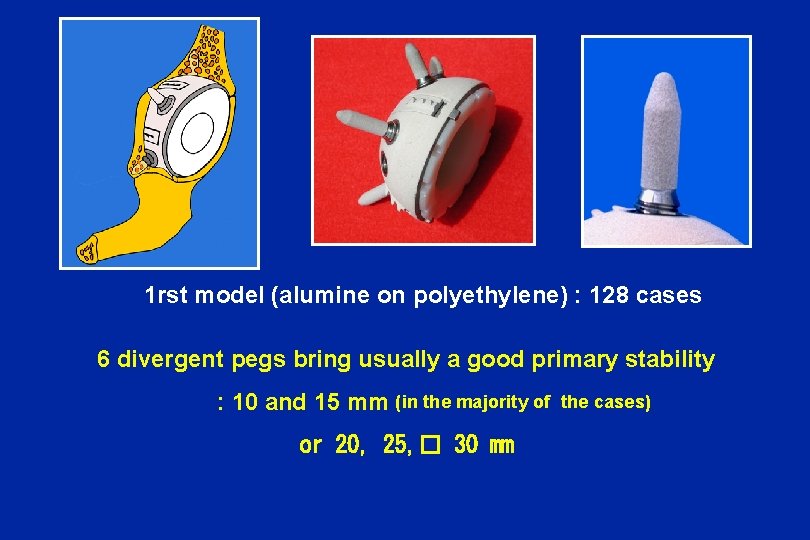
1 rst model (alumine on polyethylene) : 128 cases 6 divergent pegs bring usually a good primary stability : 10 and 15 mm (in the majority of the cases) or 20, 25, � 30 mm
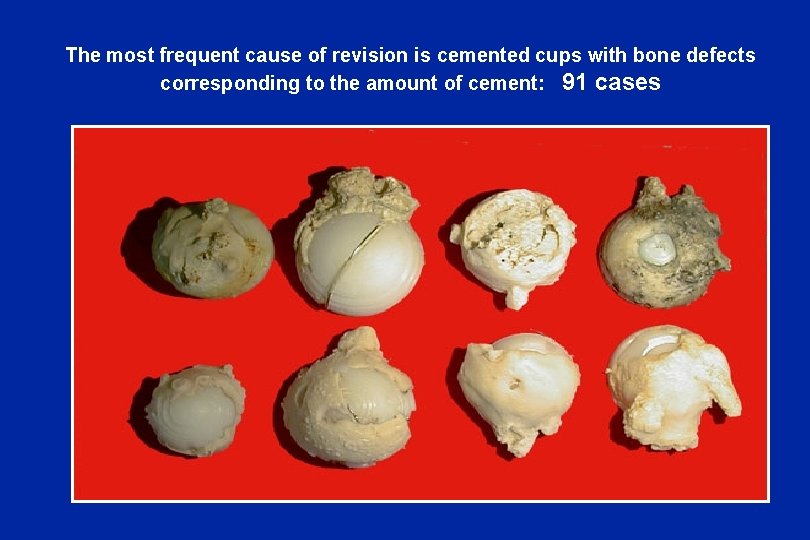
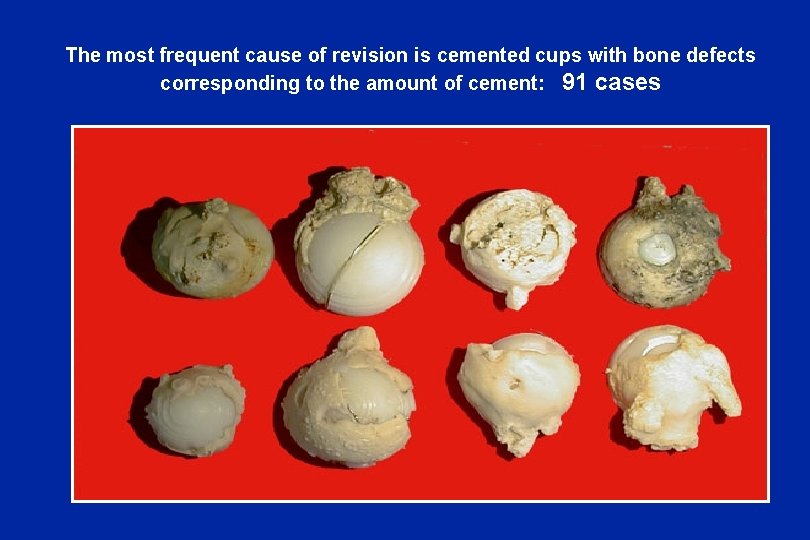
The most frequent cause of revision is cemented cups with bone defects corresponding to the amount of cement: 91 cases
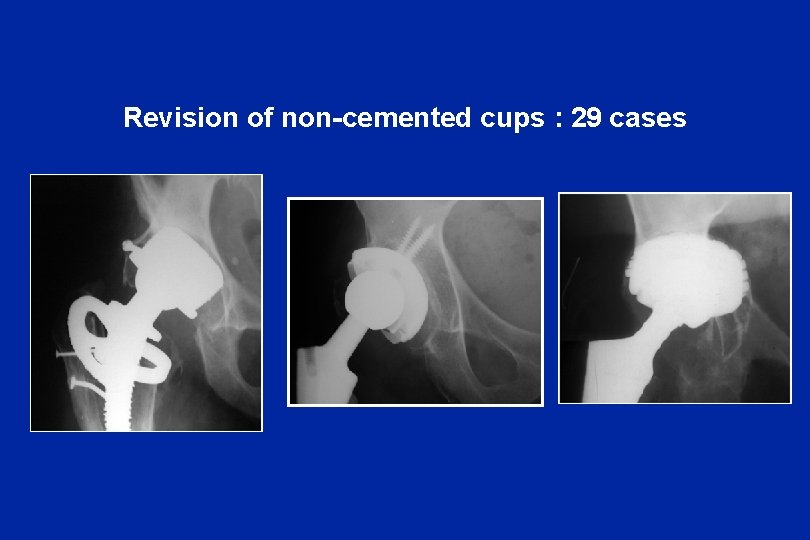
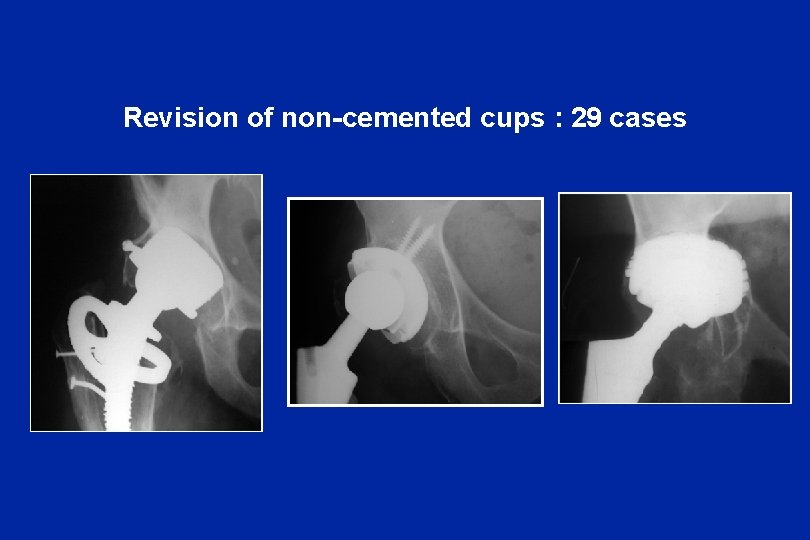
Revision of non-cemented cups : 29 cases
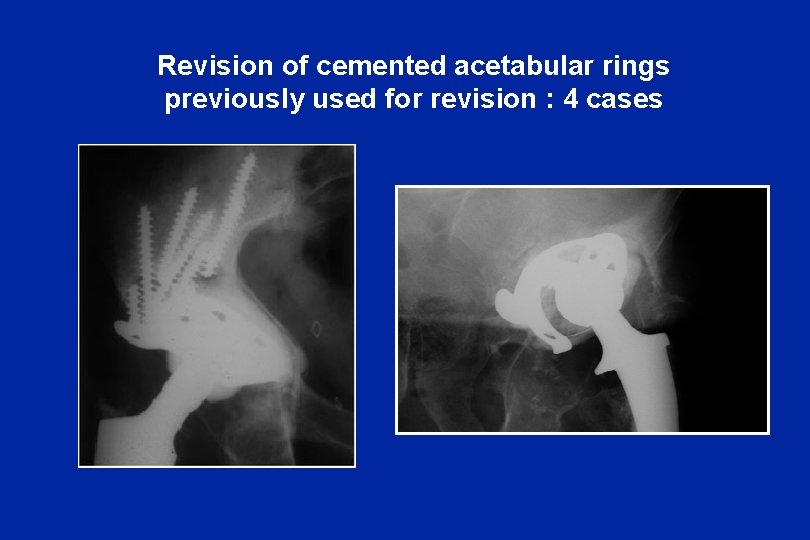
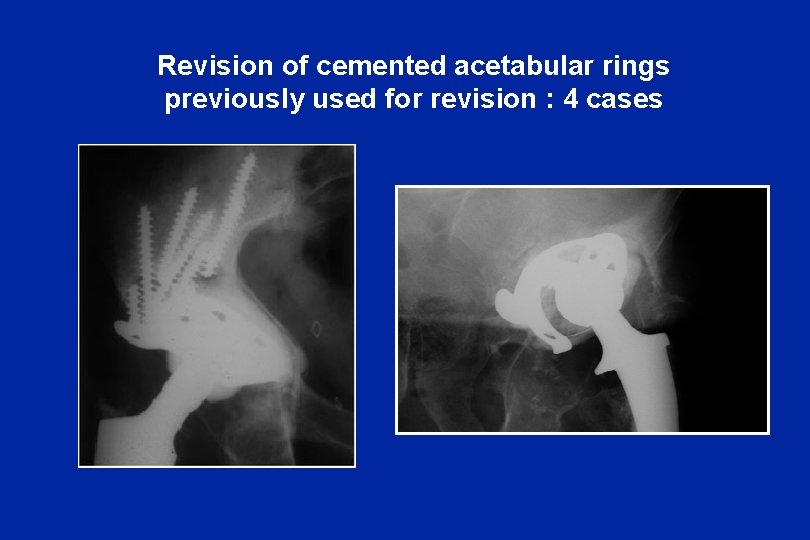
Revision of cemented acetabular rings previously used for revision : 4 cases
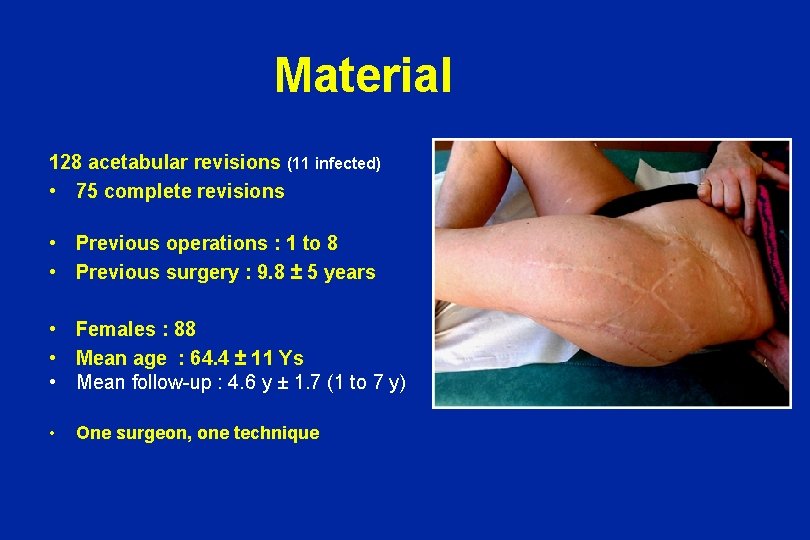
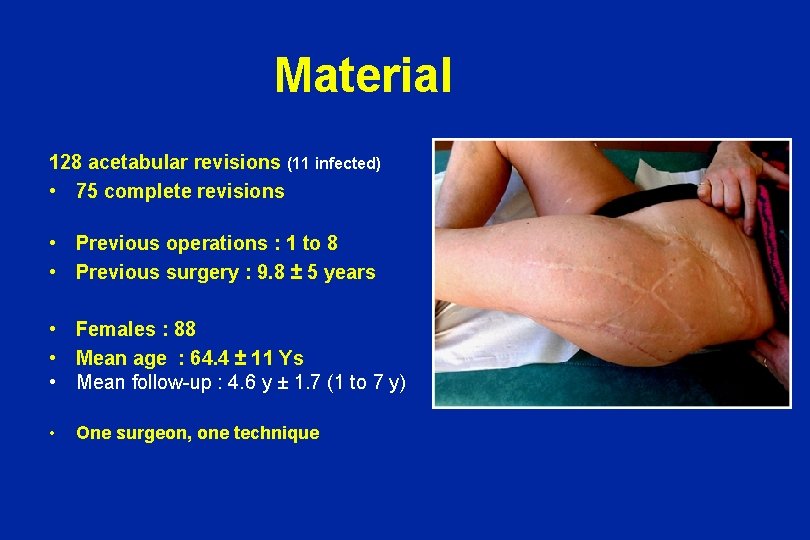
Material 128 acetabular revisions (11 infected) • 75 complete revisions • • • Previous operations : 1 to 8 Previous surgery : 9. 8 ± 5 years • One surgeon, one technique Females : 88 Mean age : 64. 4 ± 11 Ys Mean follow-up : 4. 6 y ± 1. 7 (1 to 7 y)
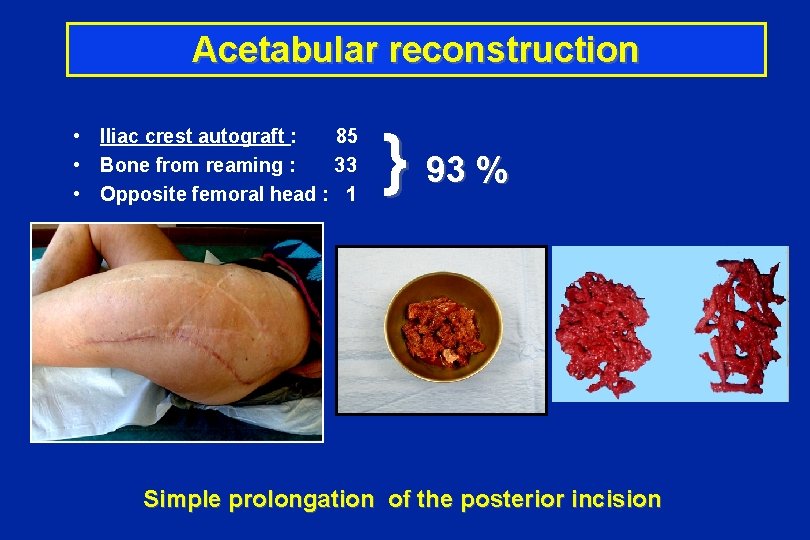
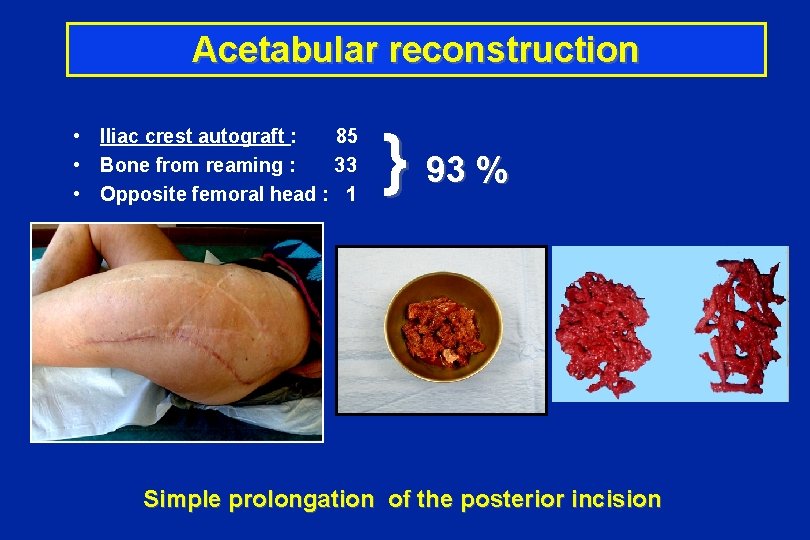
Acetabular reconstruction } 93 % • Iliac crest autograft : 85 • Bone from reaming : 33 • Opposite femoral head : 1 Simple prolongation of the posterior incision
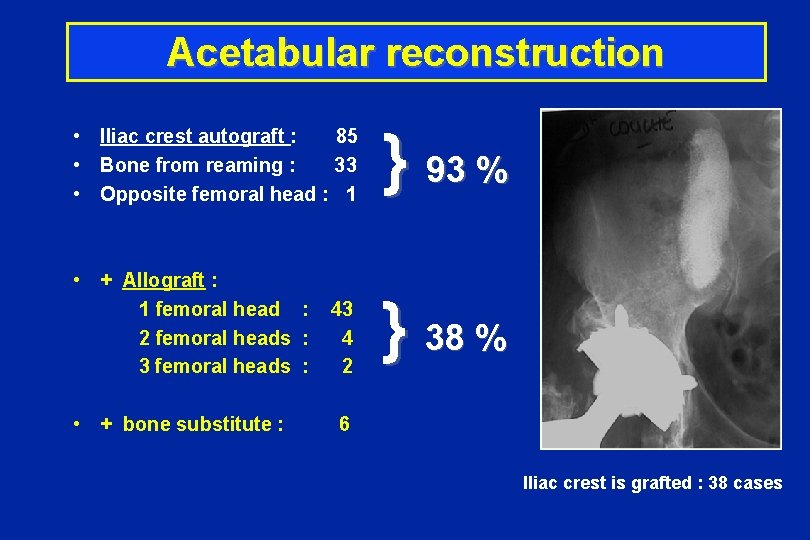
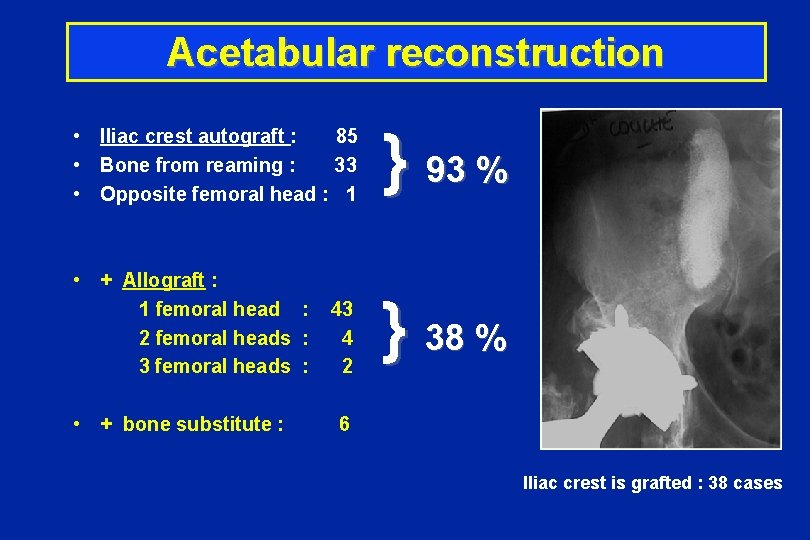
Acetabular reconstruction } 93 % • Iliac crest autograft : 85 • Bone from reaming : 33 • Opposite femoral head : 1 • + Allograft : 1 femoral head : 43 2 femoral heads : 4 3 femoral heads : 2 } 38 % • + bone substitute : 6 Iliac crest is grafted : 38 cases
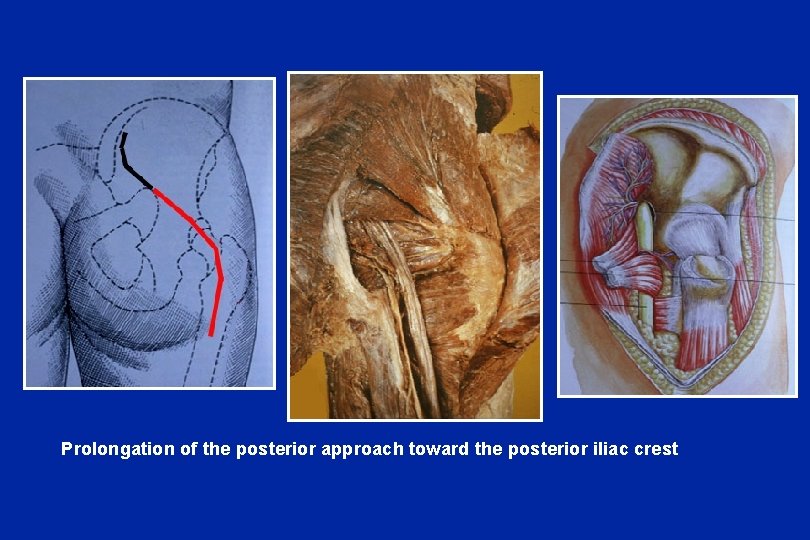
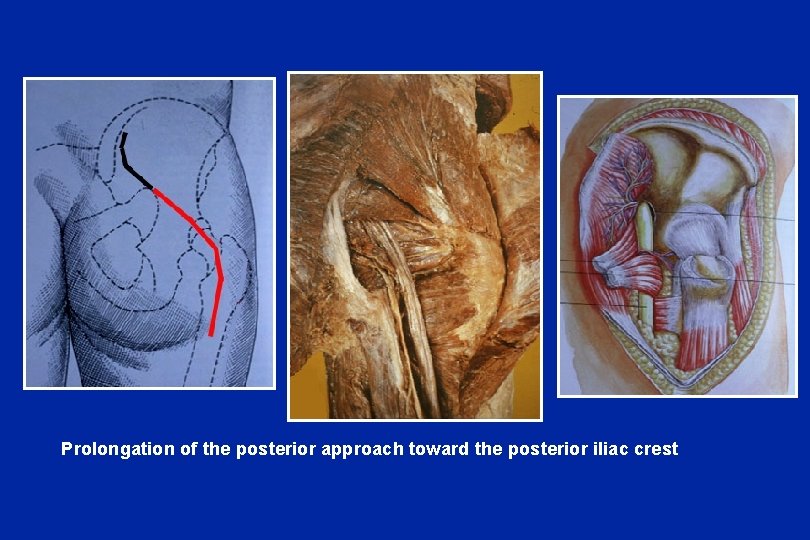
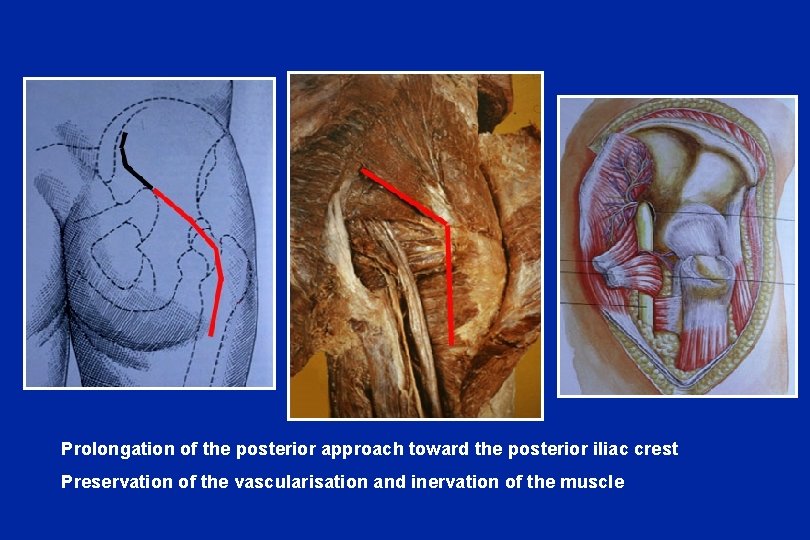
Prolongation of the posterior approach toward the posterior iliac crest
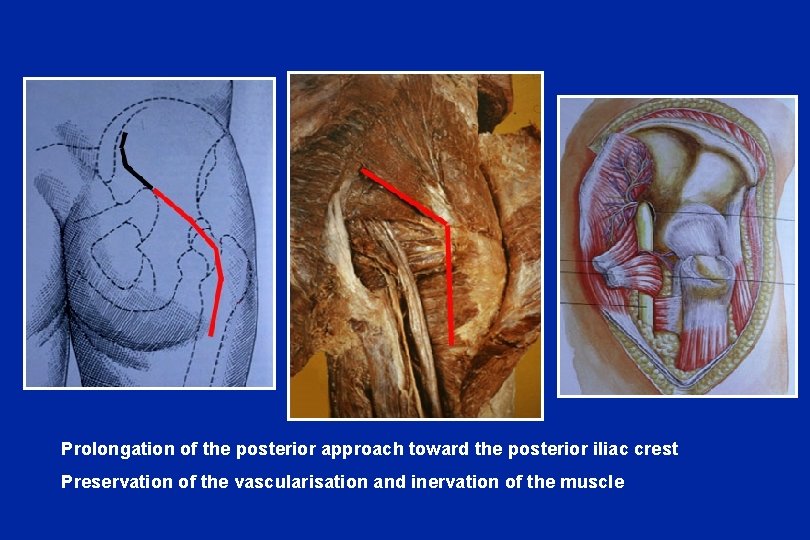
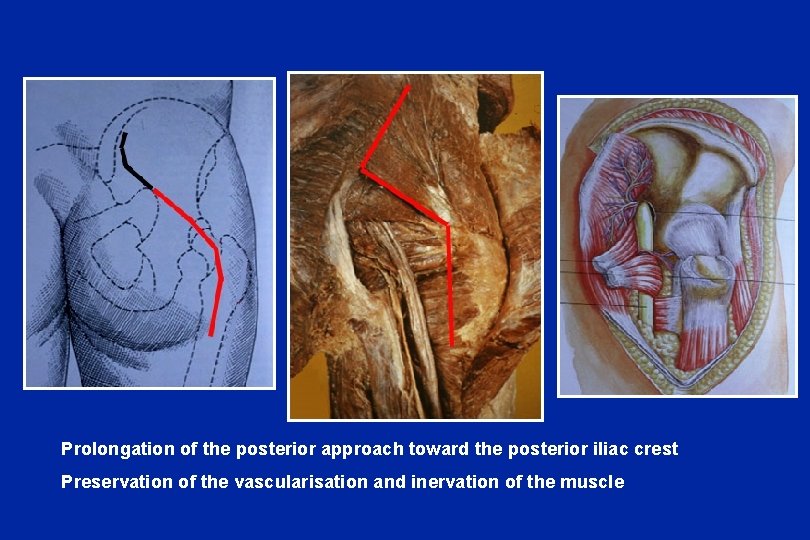
Prolongation of the posterior approach toward the posterior iliac crest Preservation of the vascularisation and inervation of the muscle
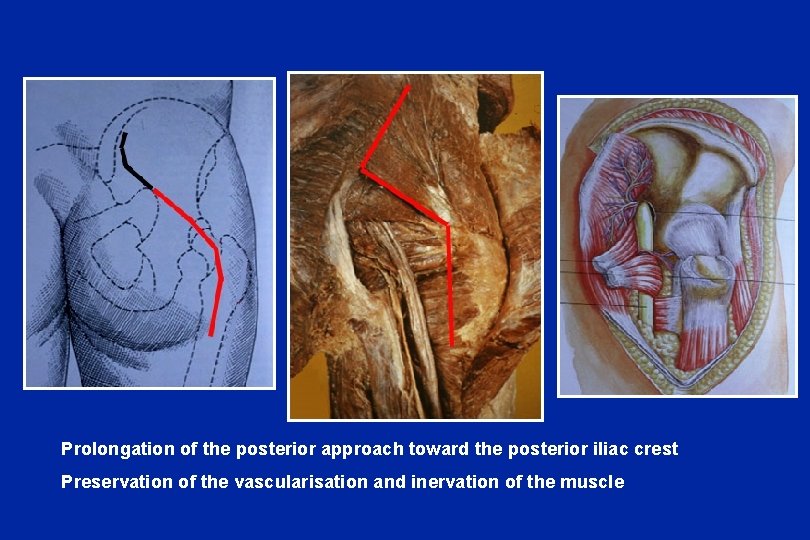
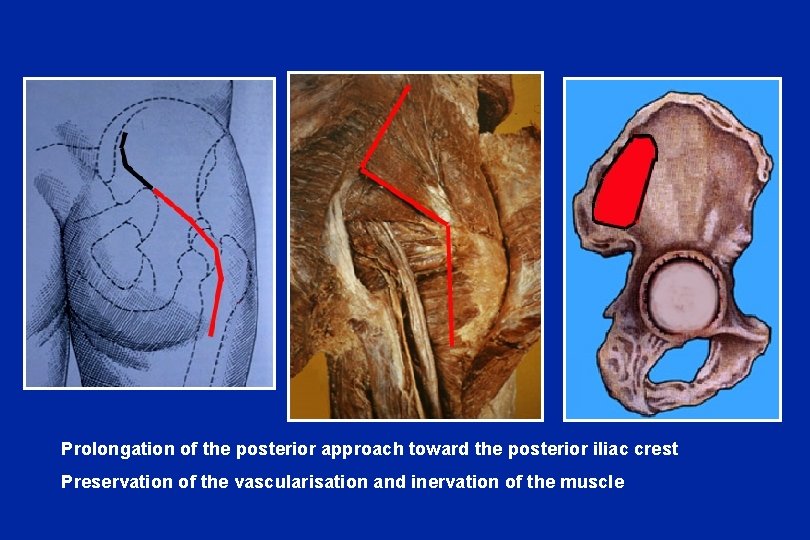
Prolongation of the posterior approach toward the posterior iliac crest Preservation of the vascularisation and inervation of the muscle
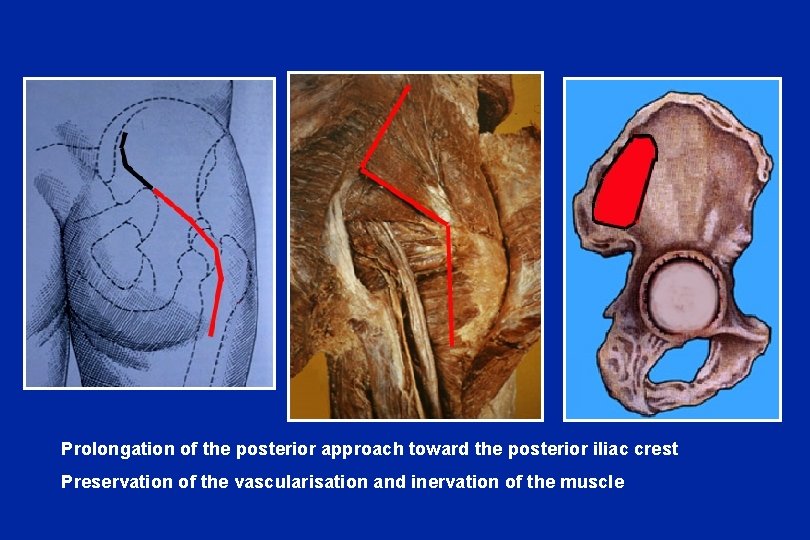
Prolongation of the posterior approach toward the posterior iliac crest Preservation of the vascularisation and inervation of the muscle
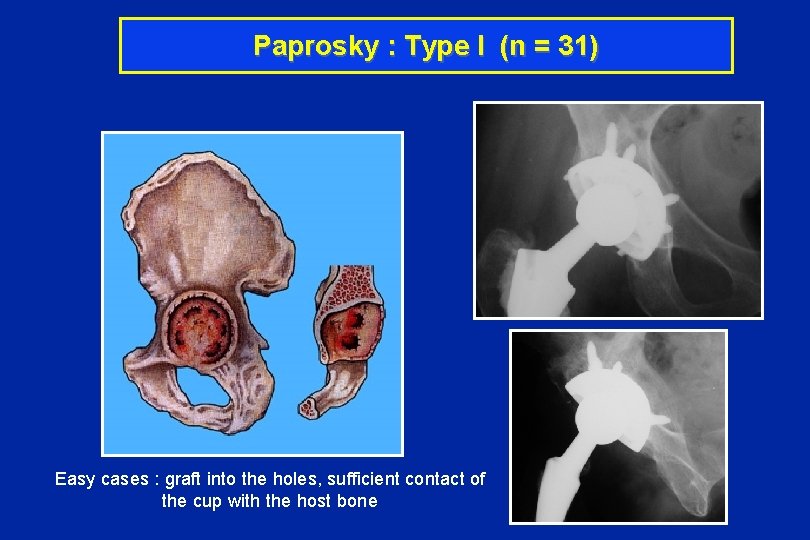
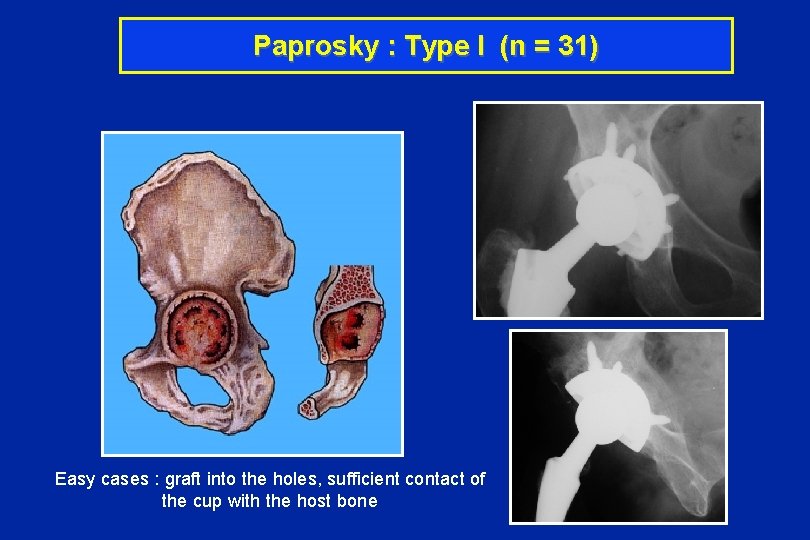
Paprosky : Type I (n = 31) Easy cases : graft into the holes, sufficient contact of the cup with the host bone
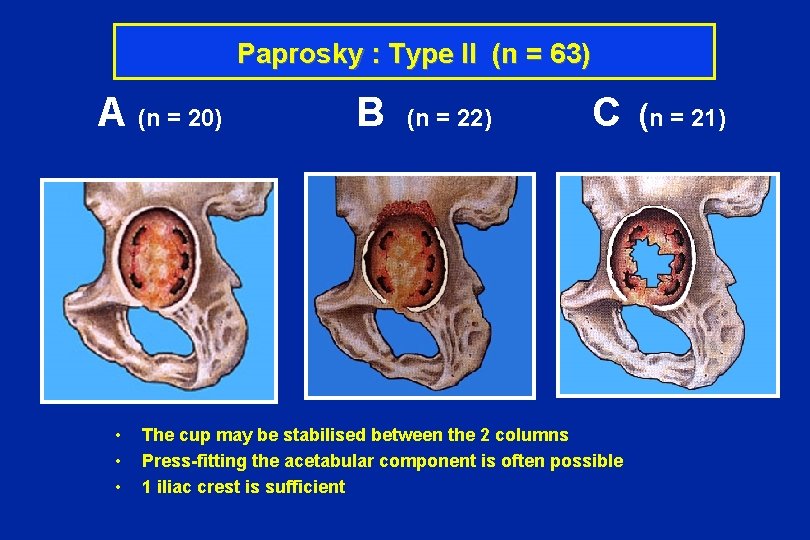
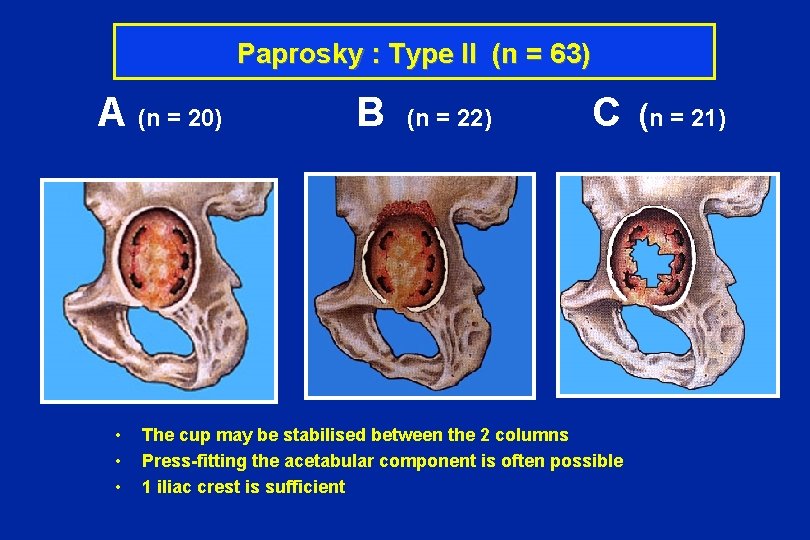
Paprosky : Type II (n = 63) A (n = 20) B (n = 22) C (n = 21) • • • The cup may be stabilised between the 2 columns Press-fitting the acetabular component is often possible 1 iliac crest is sufficient
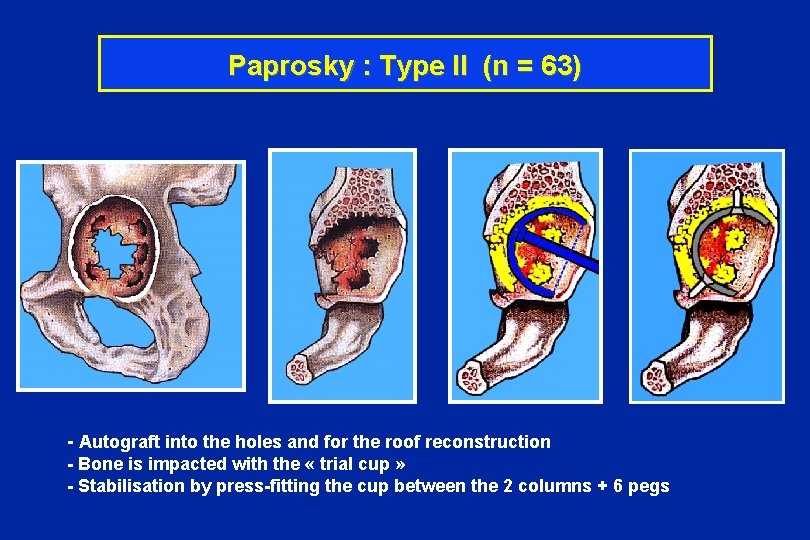
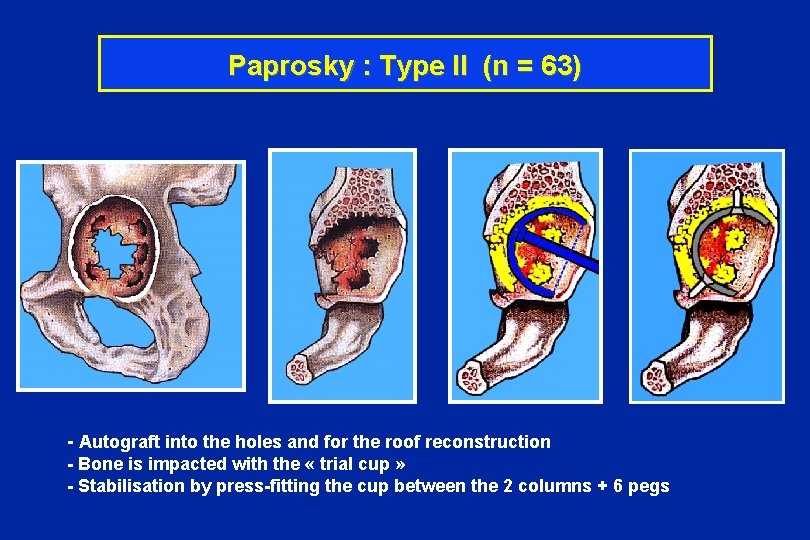
Paprosky : Type II (n = 63) - Autograft into the holes and for the roof reconstruction - Bone is impacted with the « trial cup » - Stabilisation by press-fitting the cup between the 2 columns + 6 pegs
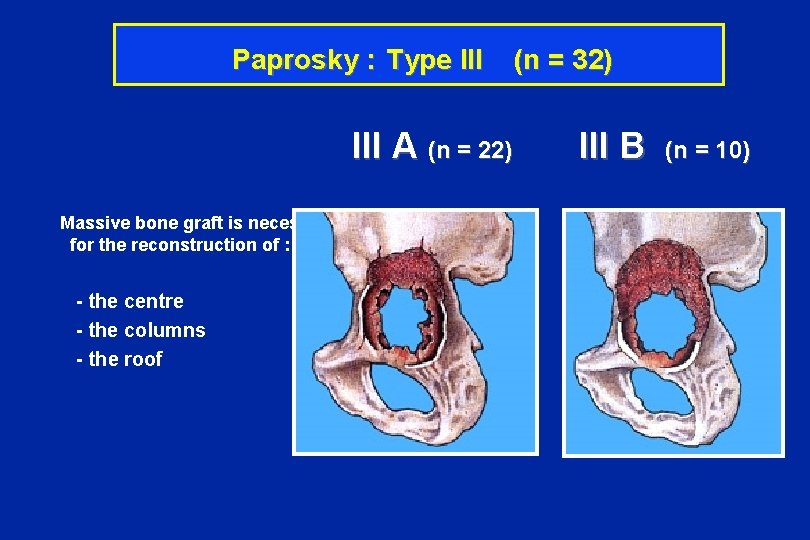
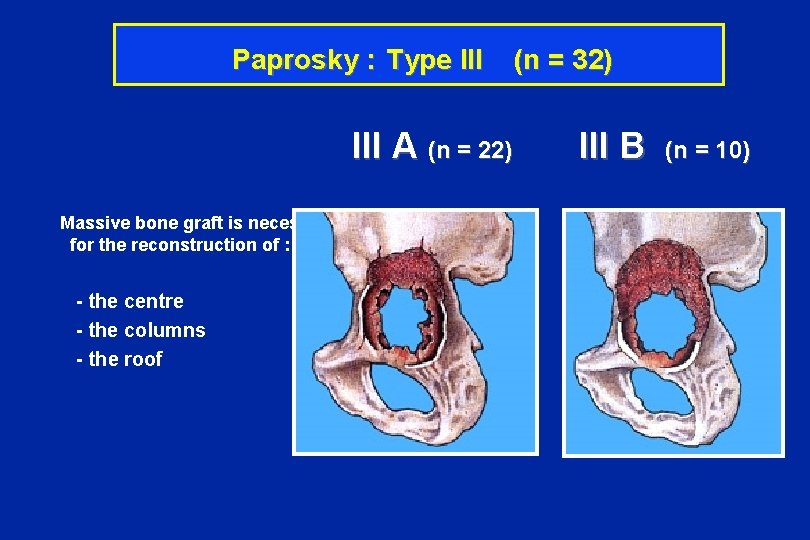
Paprosky : Type III (n = 32) III A (n = 22) III B (n = 10) Massive bone graft is necessary for the reconstruction of : - the centre - the columns - the roof
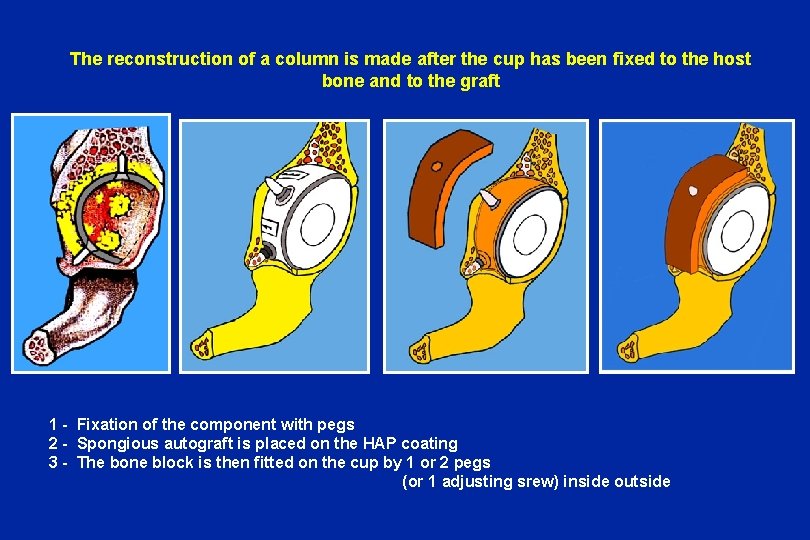
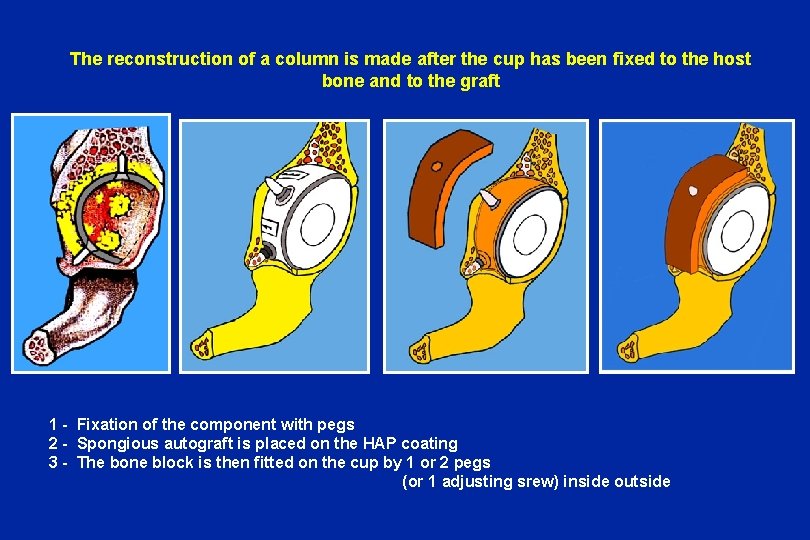
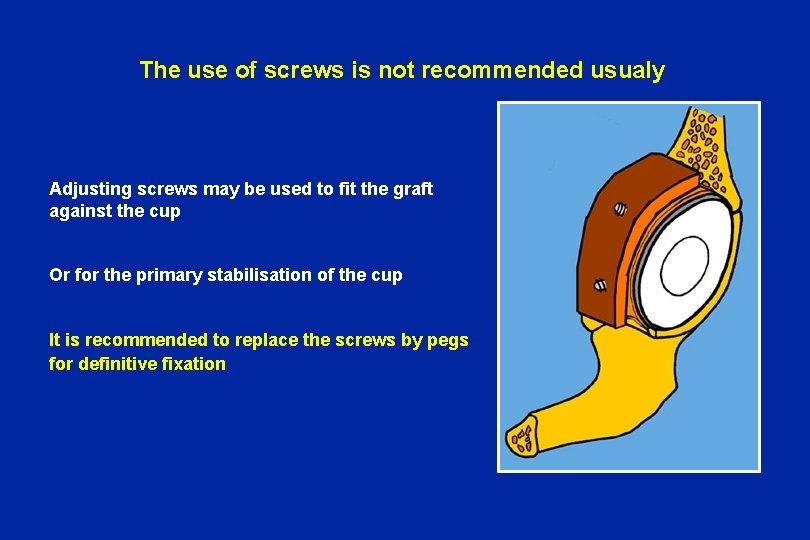
The reconstruction of a column is made after the cup has been fixed to the host bone and to the graft 1 - Fixation of the component with pegs 2 - Spongious autograft is placed on the HAP coating 3 - The bone block is then fitted on the cup by 1 or 2 pegs (or 1 adjusting srew) inside outside
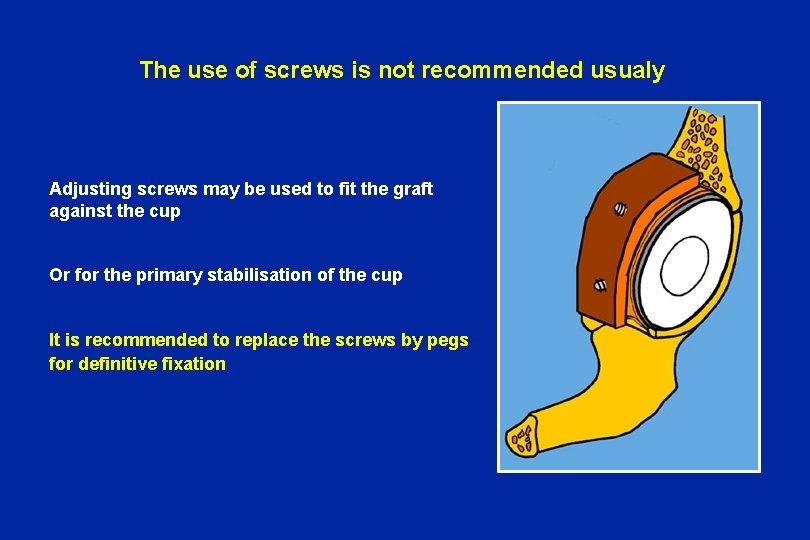
The use of screws is not recommended usualy Adjusting screws may be used to fit the graft against the cup Or for the primary stabilisation of the cup It is recommended to replace the screws by pegs for definitive fixation
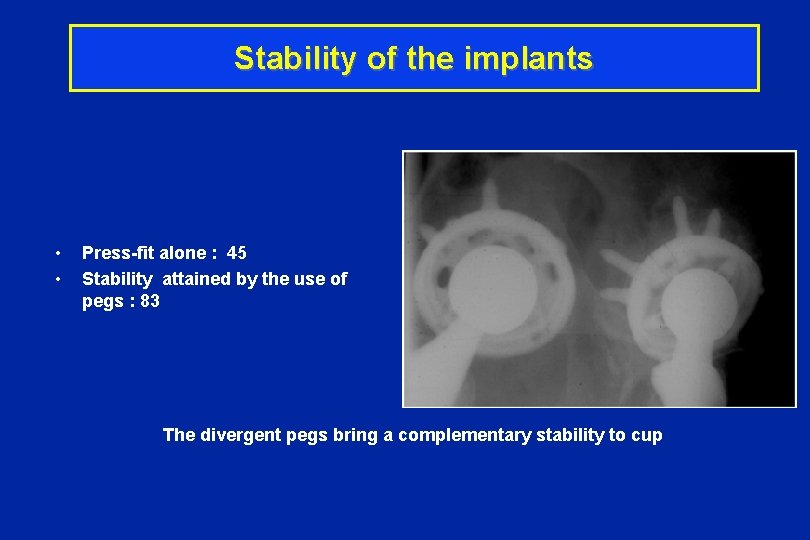
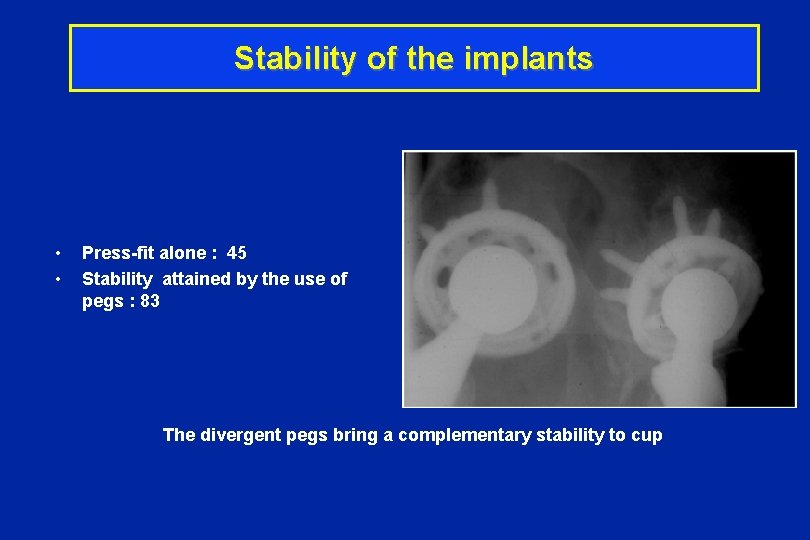
Stability of the implants • • Press-fit alone : 45 Stability attained by the use of pegs : 83 The divergent pegs bring a complementary stability to cup
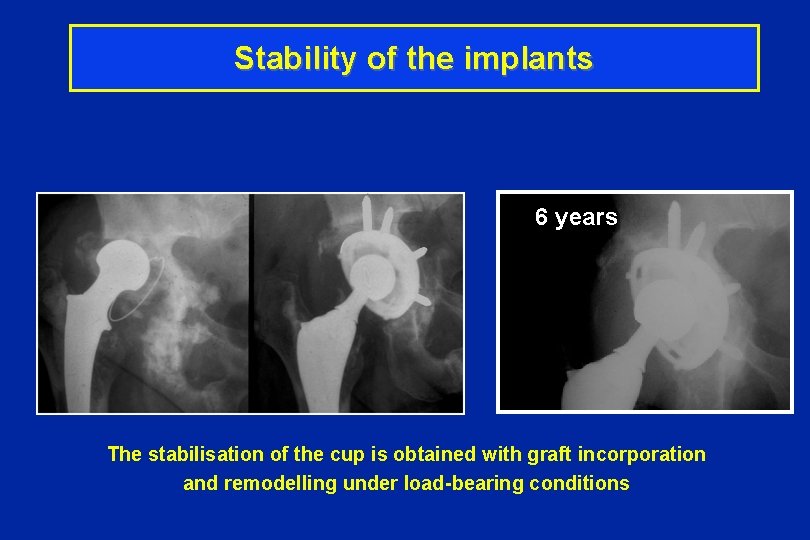
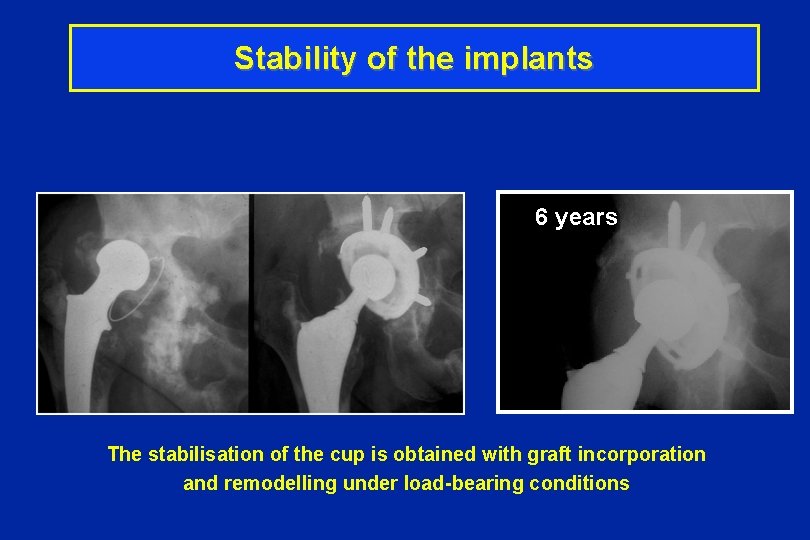
Stability of the implants 6 years The stabilisation of the cup is obtained with graft incorporation and remodelling under load-bearing conditions
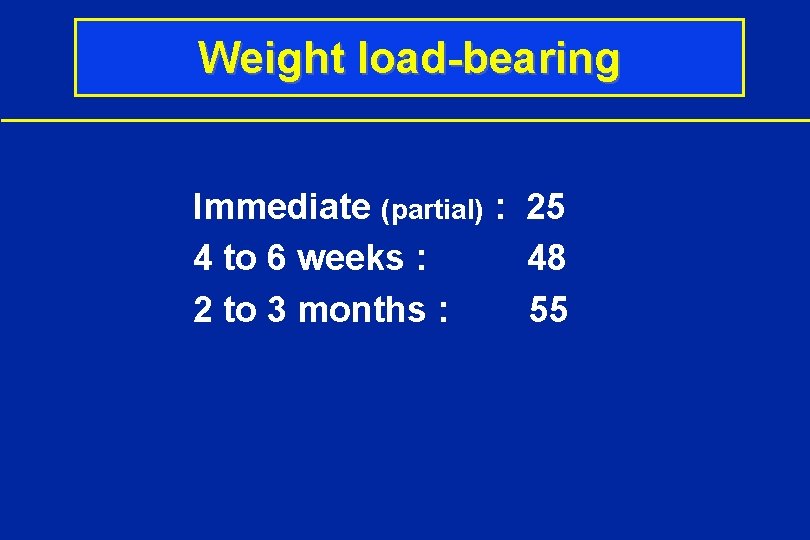
Weight load-bearing Immediate (partial) : 25 4 to 6 weeks : 48 2 to 3 months : 55
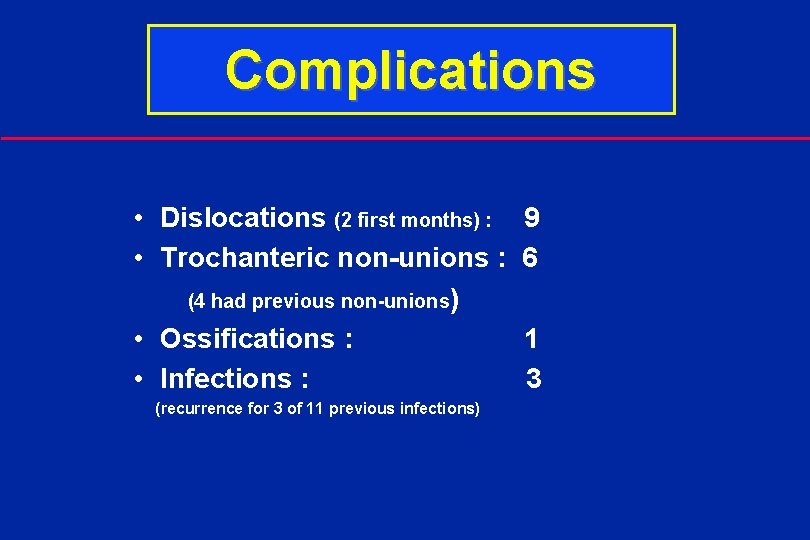
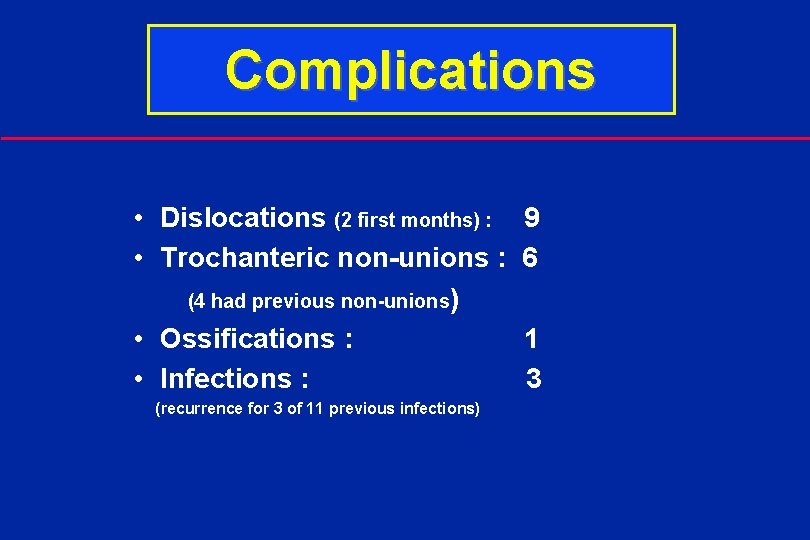
Complications • Dislocations (2 first months) : 9 • Trochanteric non-unions : 6 (4 had previous non-unions) • Ossifications : 1 • Infections : 3 (recurrence for 3 of 11 previous infections)
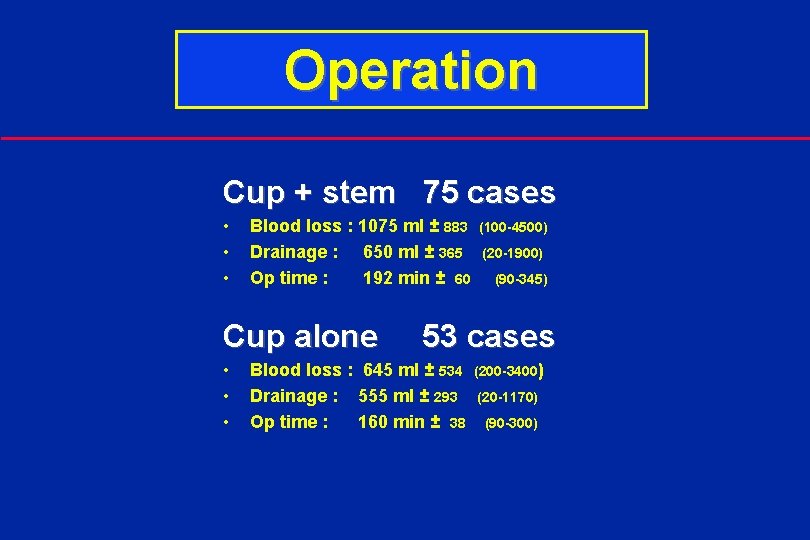
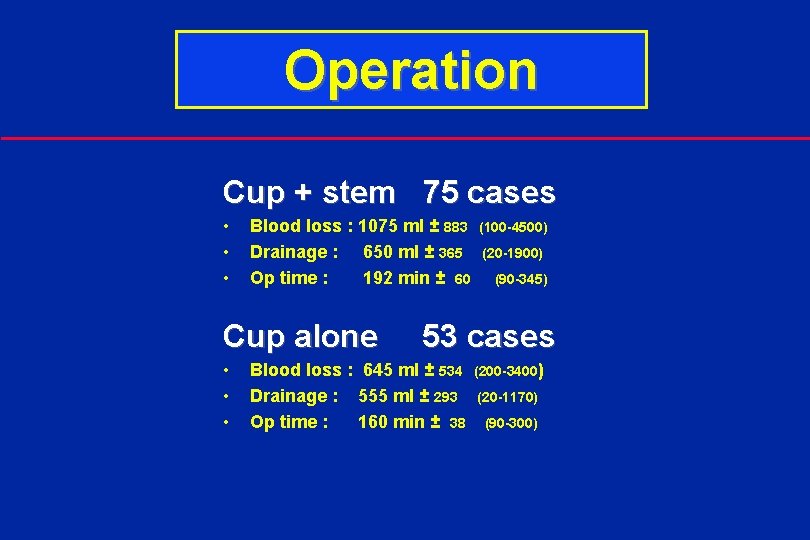
Operation Cup + stem 75 cases • • • Blood loss : 1075 ml ± 883 (100 -4500) Drainage : 650 ml ± 365 (20 -1900) Op time : 192 min ± 60 (90 -345) Cup alone 53 cases • • • Blood loss : 645 ml ± 534 (200 -3400) Drainage : 555 ml ± 293 (20 -1170) Op time : 160 min ± 38 (90 -300)
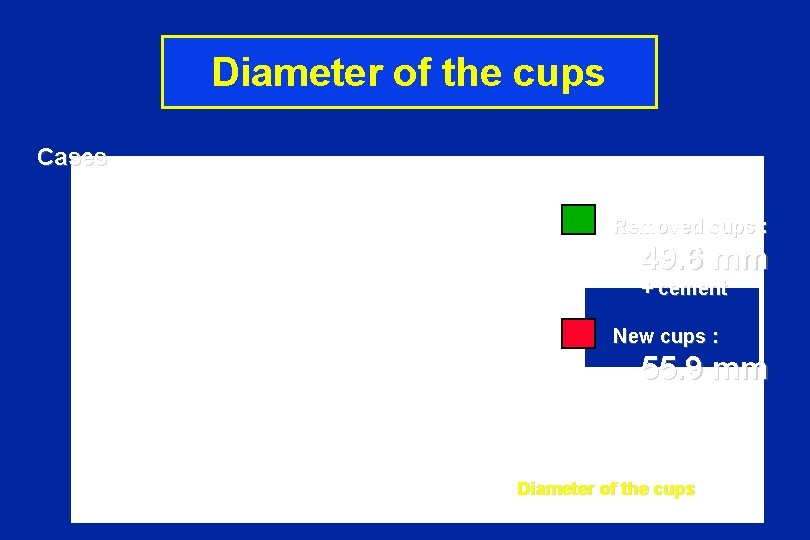
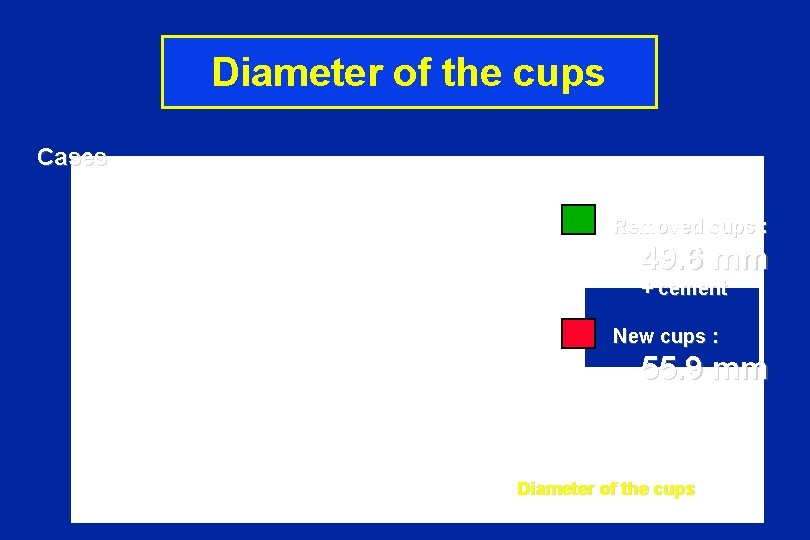
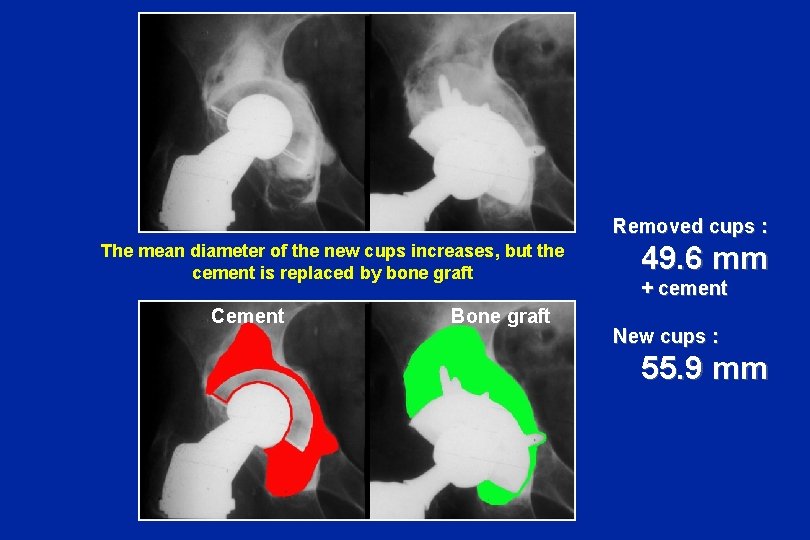
Diameter of the cups Cases Removed cups : 49. 6 mm + cement New cups : 55. 9 mm Diameter of the cups
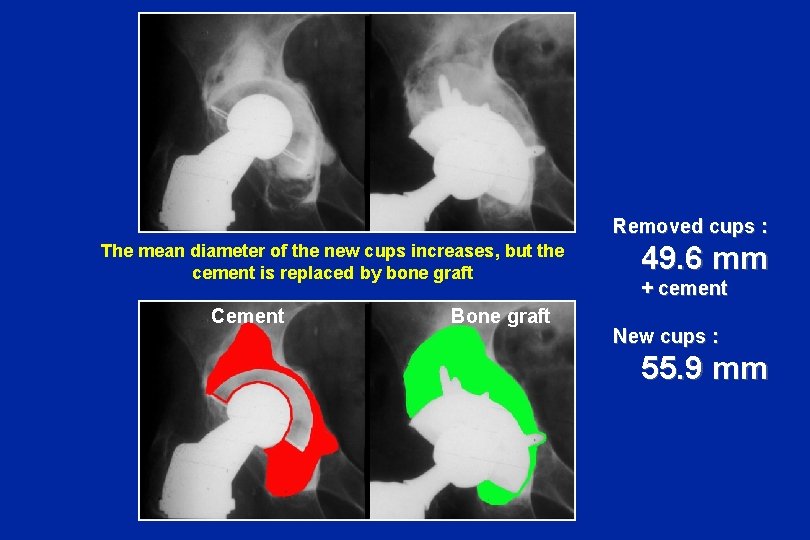
Removed cups : The mean diameter of the new cups increases, but the cement is replaced by bone graft Cement Bone graft 49. 6 mm + cement New cups : 55. 9 mm
Evaluation Radiographic measurements • Incorporation /radio lucent line • Stability in the 3 planes - Numerised X-rays - Precise measurements (special software : “Metr. Os” C. Falaise) Functional value • PMA Score (Postel - Merle d'Aubigné)
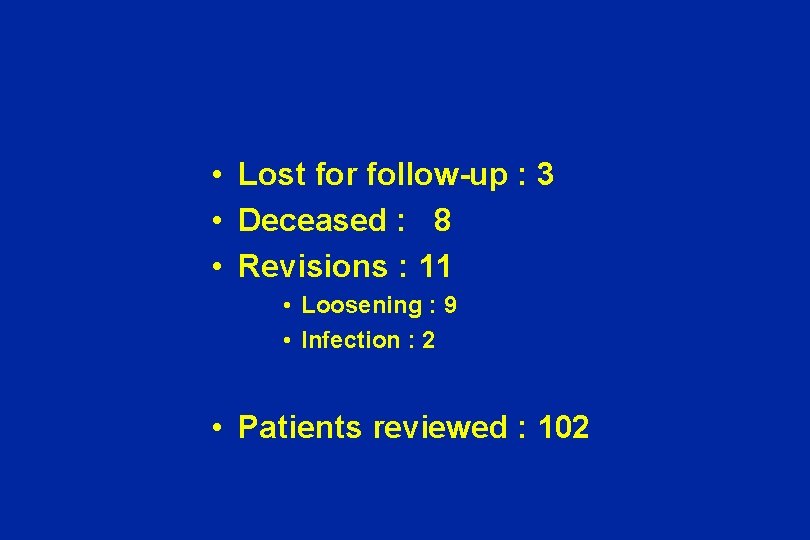
• Lost for follow-up : 3 • Deceased : 8 • Revisions : 11 • Loosening : 9 • Infection : 2 • Patients reviewed : 102
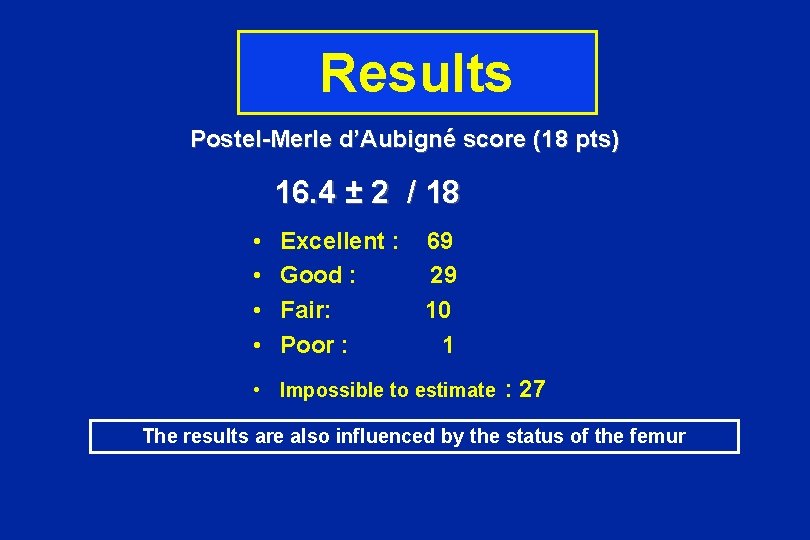
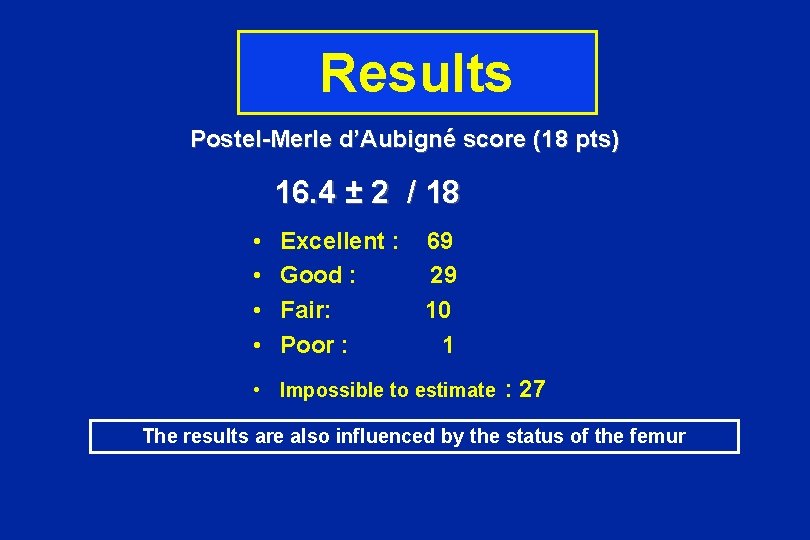
Results Postel-Merle d’Aubigné score (18 pts) 16. 4 ± 2 / 18 • • Excellent : 69 Good : 29 Fair: 10 Poor : 1 • Impossible to estimate : 27 The results are also influenced by the status of the femur
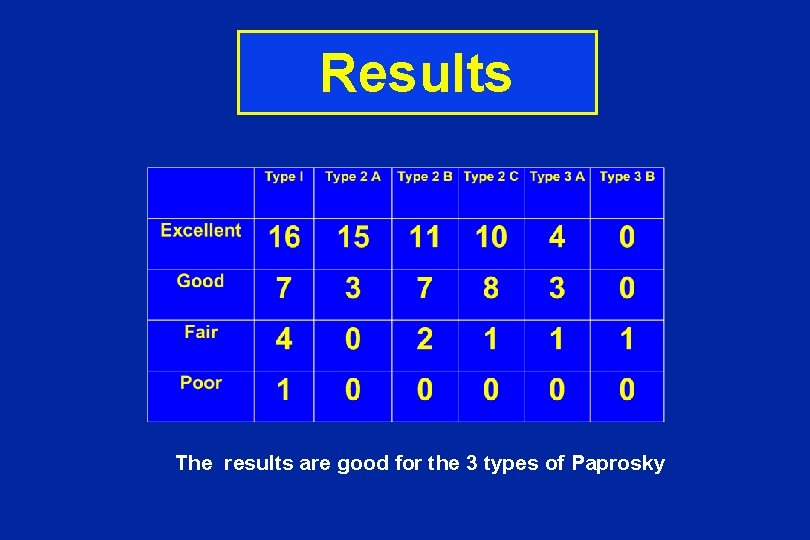
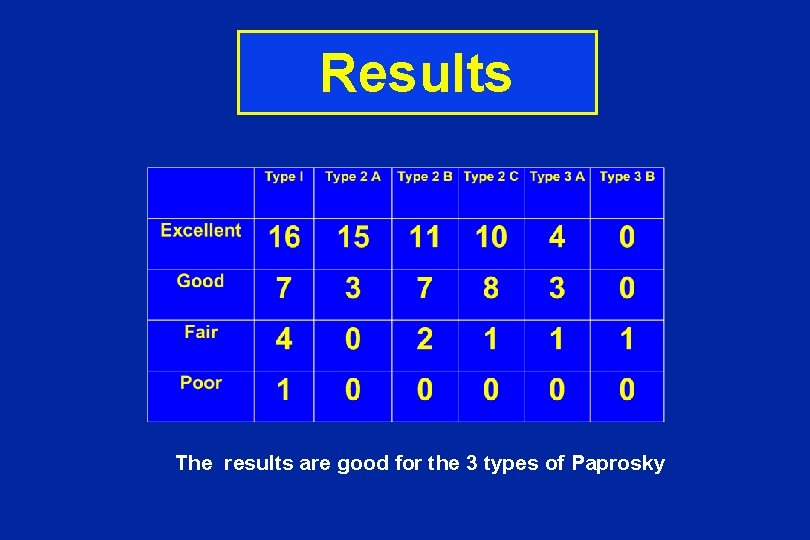
Results The results are good for the 3 types of Paprosky
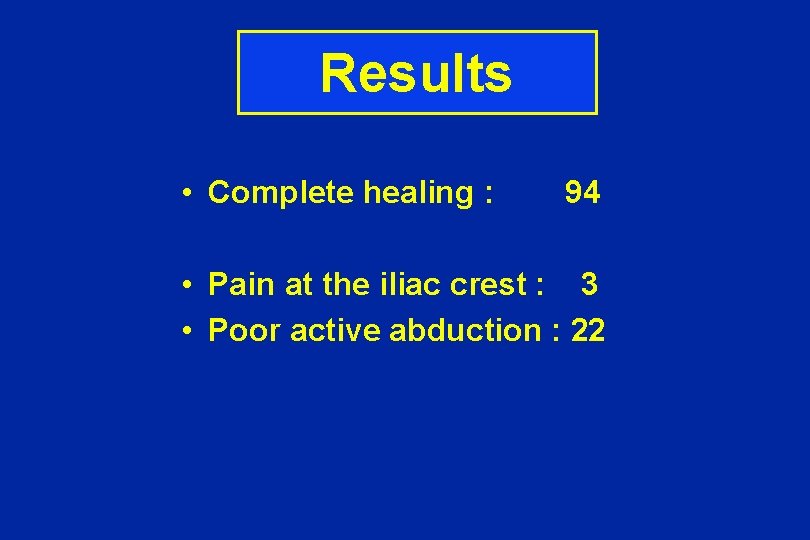
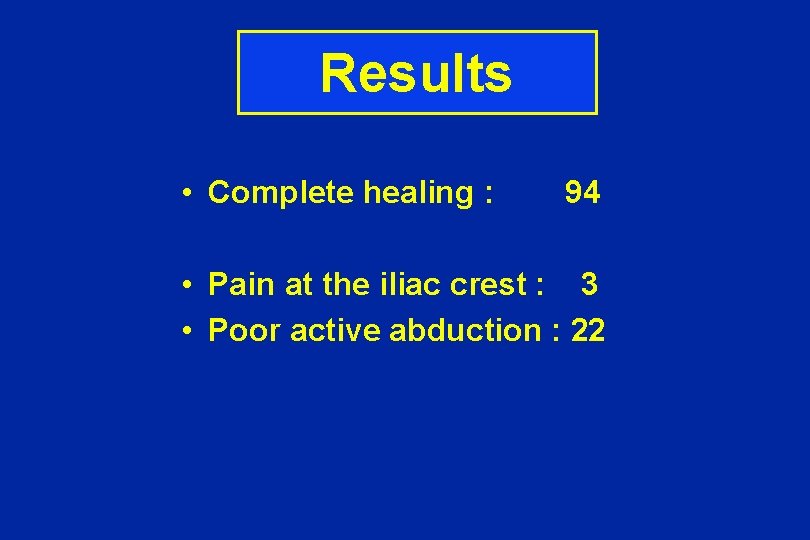
Results • Complete healing : 94 • Pain at the iliac crest : 3 • Poor active abduction : 22
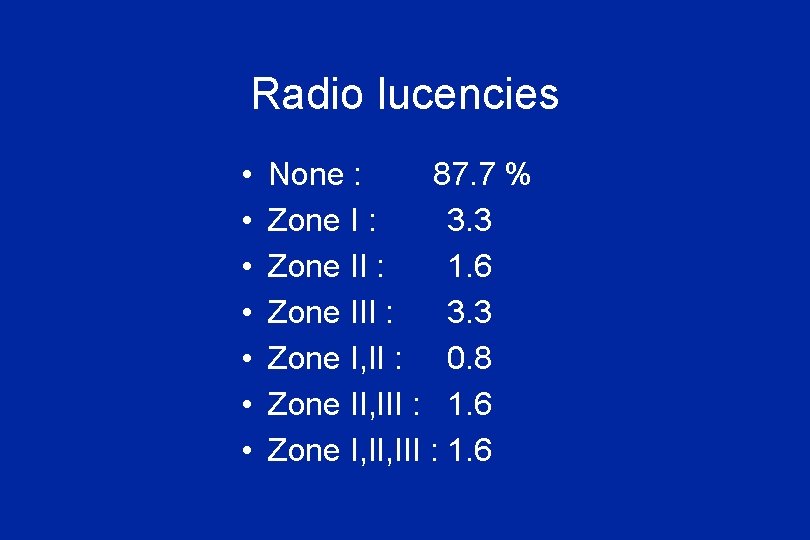
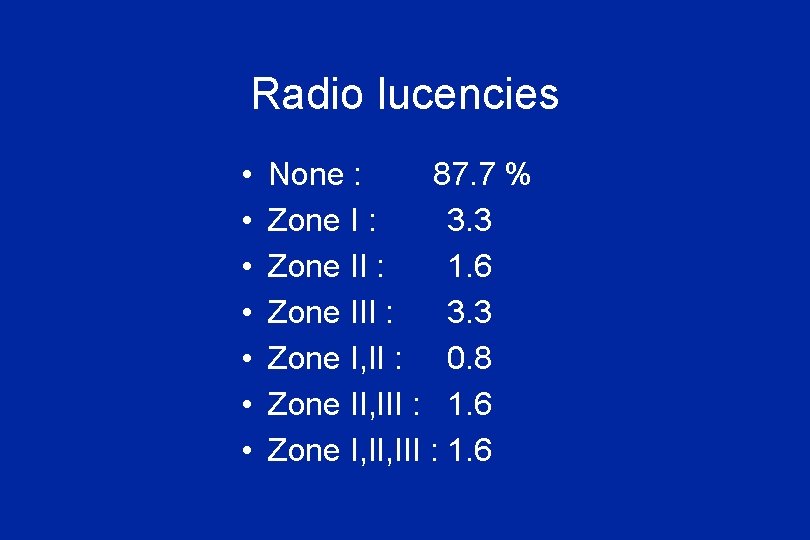
Radio lucencies • • None : 87. 7 % Zone I : 3. 3 Zone II : 1. 6 Zone III : 3. 3 Zone I, II : 0. 8 Zone II, III : 1. 6 Zone I, III : 1. 6
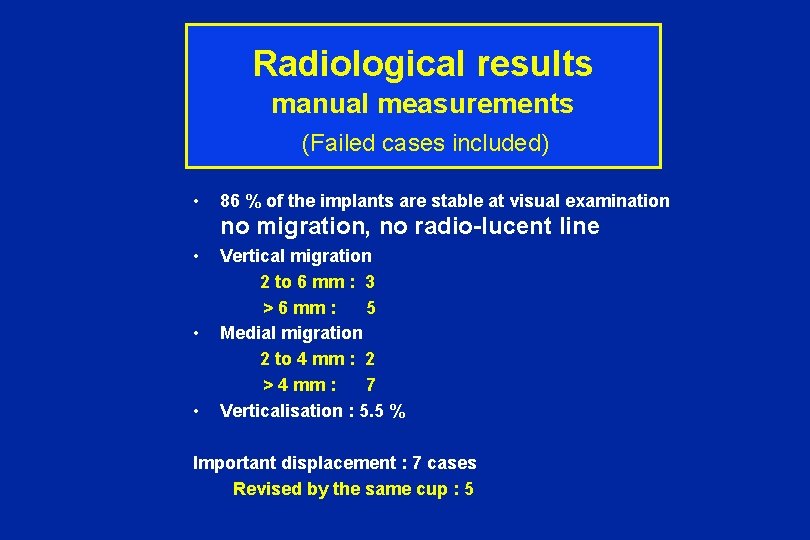
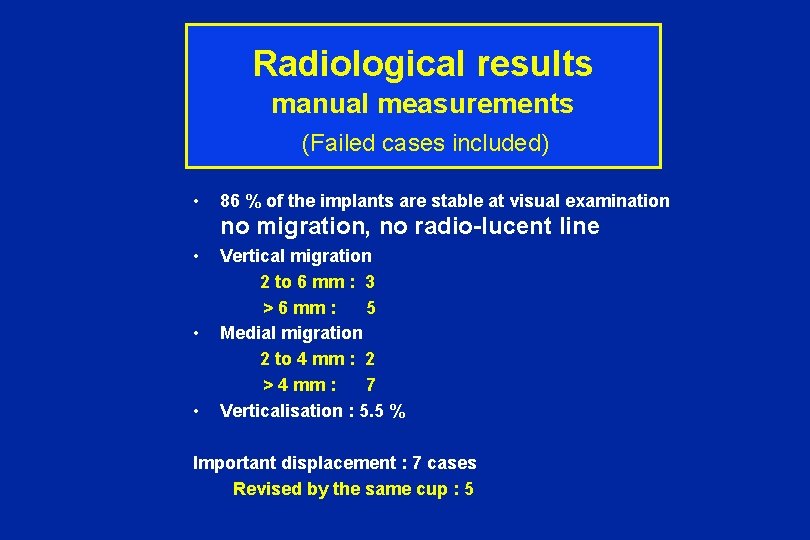
Radiological results manual measurements (Failed • cases included) 86 % of the implants are stable at visual examination no migration, no radio-lucent line • Vertical migration 2 to 6 mm : 3 > 6 mm : 5 • Medial migration 2 to 4 mm : 2 > 4 mm : 7 • Verticalisation : 5. 5 % Important displacement : 7 cases Revised by the same cup : 5

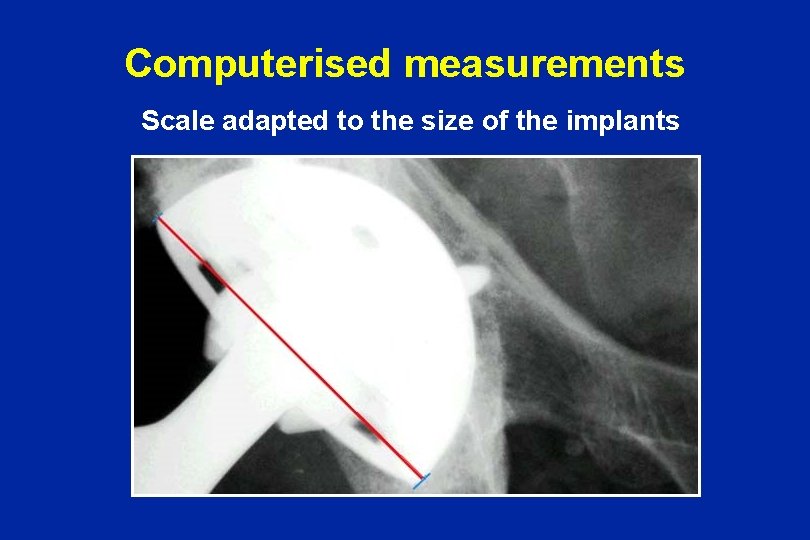
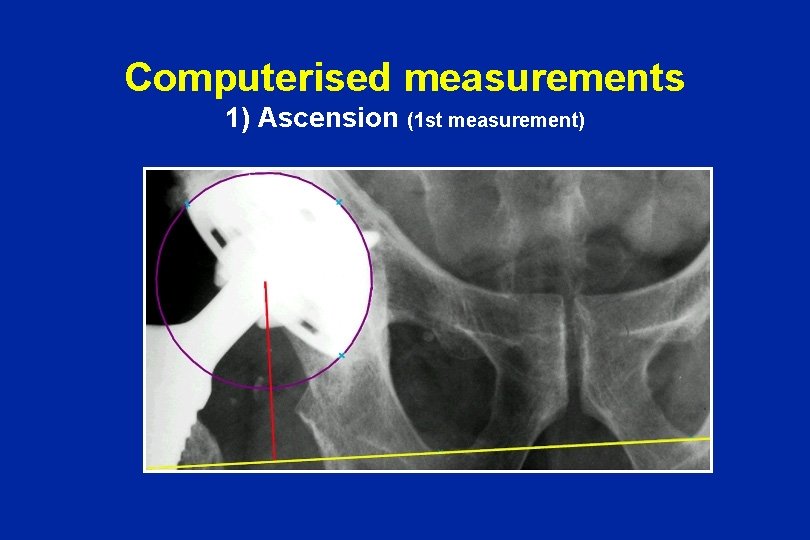
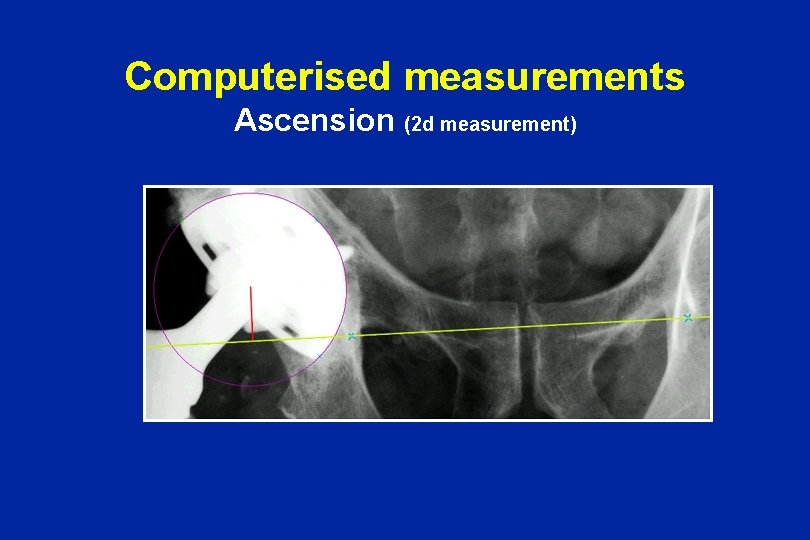
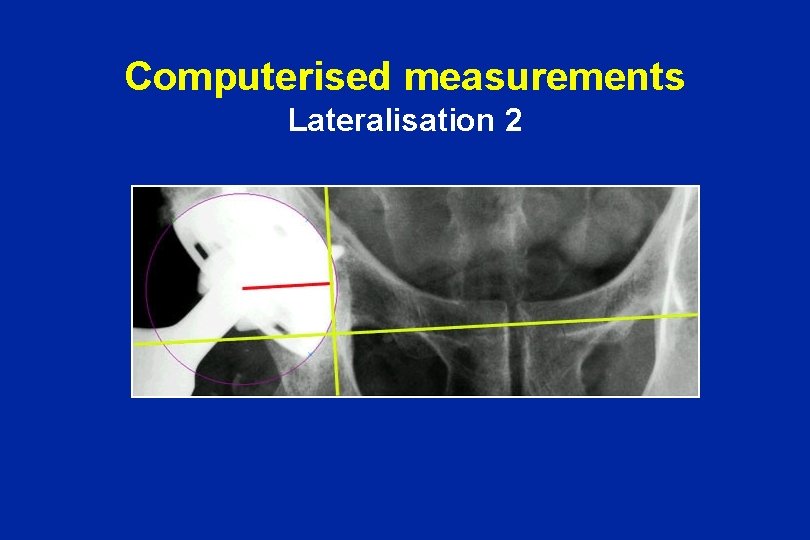
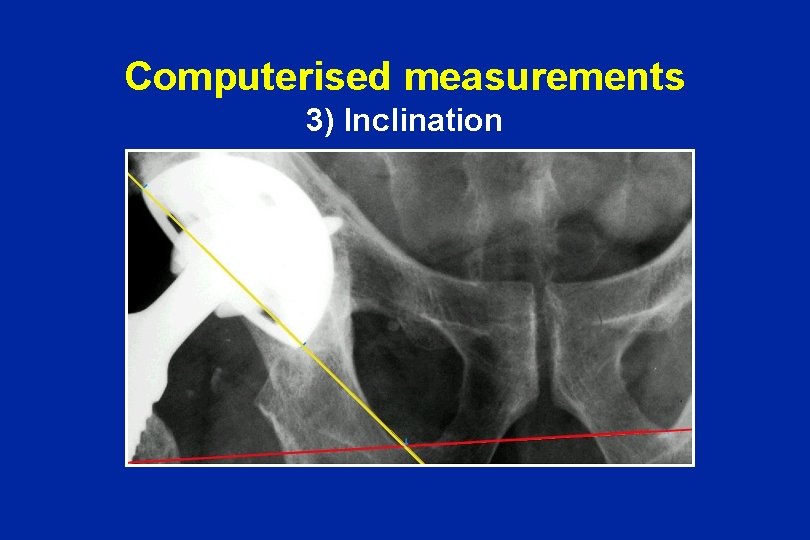
Computerised measurements • • Scanner Vidar Definition : 150 Dot per inch Selection 1 Pixel : 0. 17 mm Special software «Mètr. Os» (C. FALAISE) • • Navigation into the image with magnification Adjustment of the luminosity and contrast Scale adapted to the size of the implants Geometric constructions and calculation of index automatically • « EBRA » method (� Krismer - Innsbruck) – 6 index (3 longitudinal, 3 transversal) – 11 measurements – Accuracy : 0. 7 mm
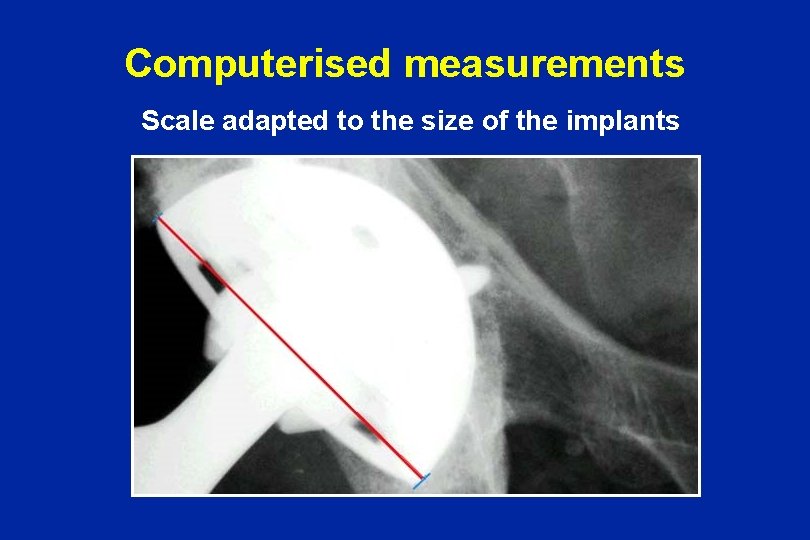
Computerised measurements Scale adapted to the size of the implants
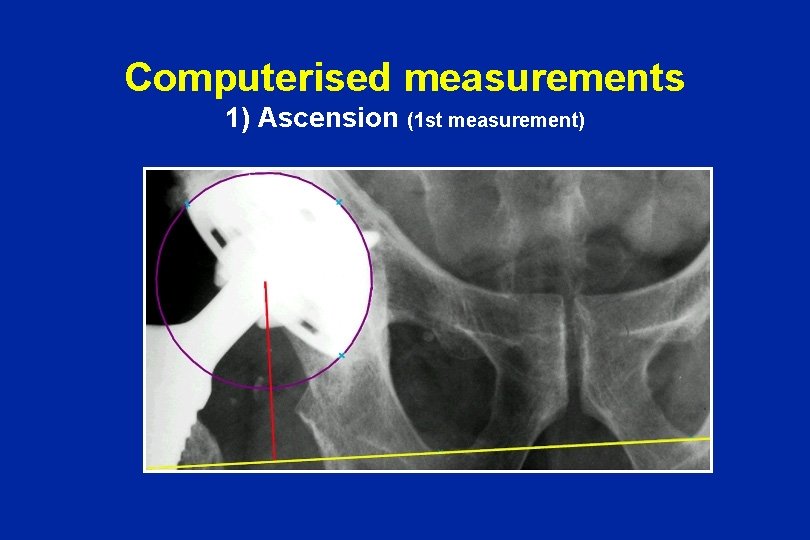
Computerised measurements 1) Ascension (1 st measurement)
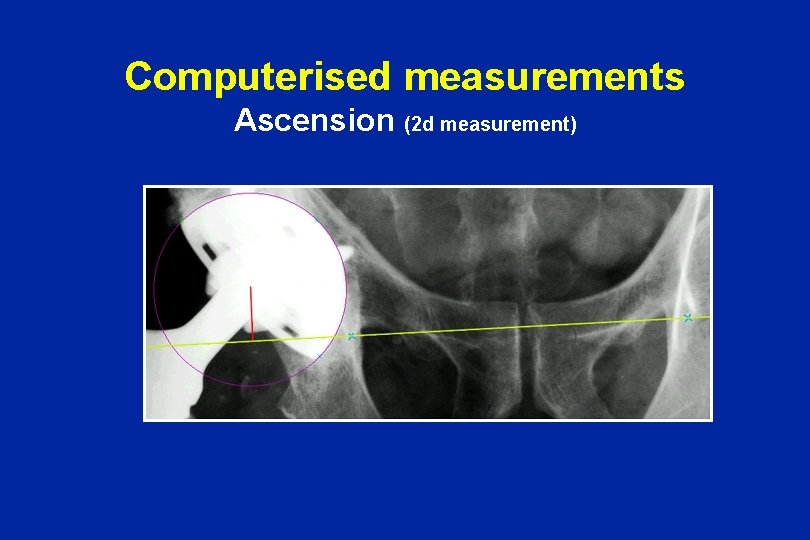
Computerised measurements Ascension (2 d measurement)

Computerised measurements 2) Lateralisation 1
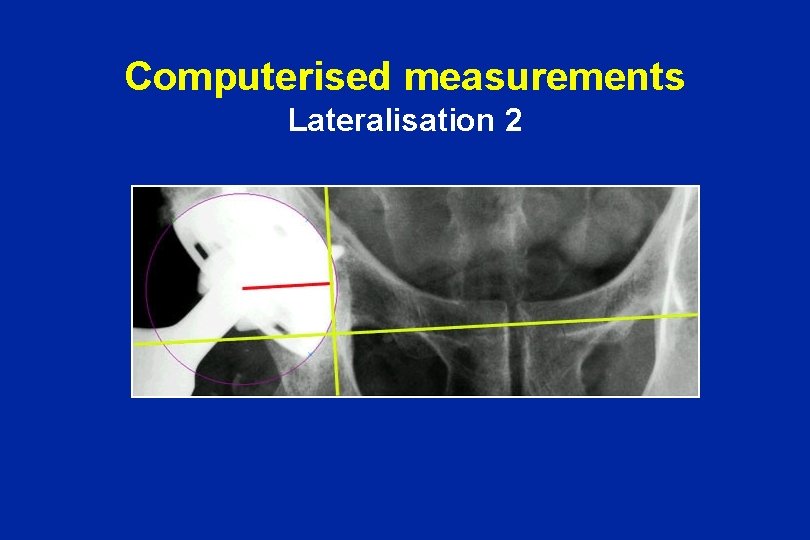
Computerised measurements Lateralisation 2
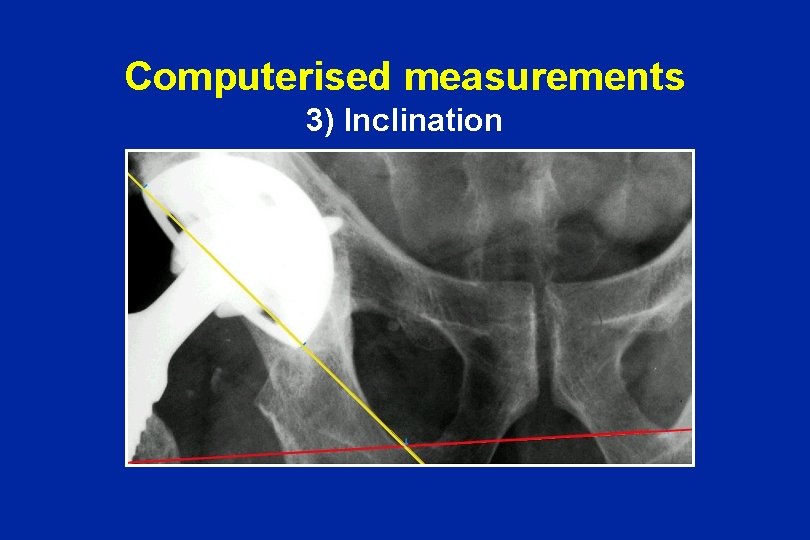
Computerised measurements 3) Inclination
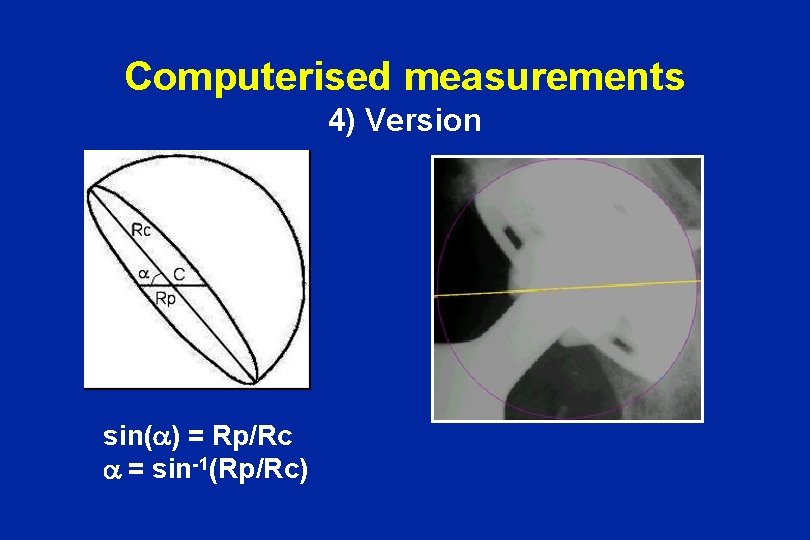
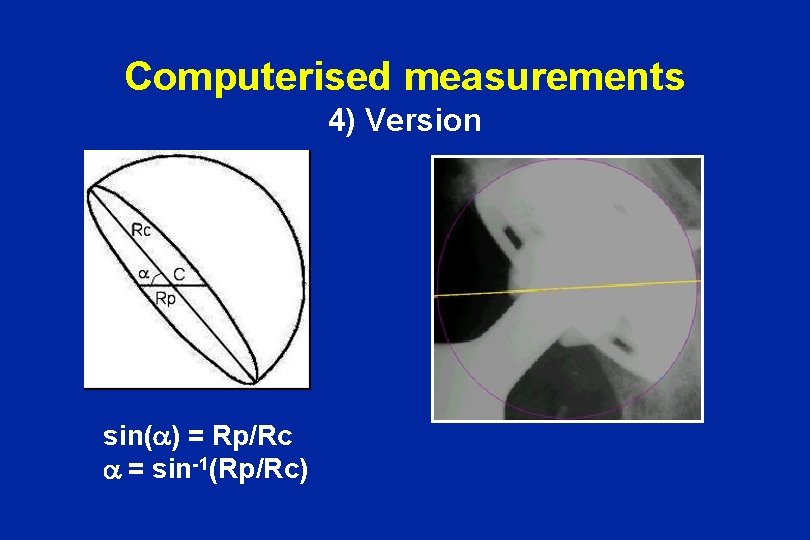
Computerised measurements 4) Version sin(a) = Rp/Rc a = sin-1(Rp/Rc)
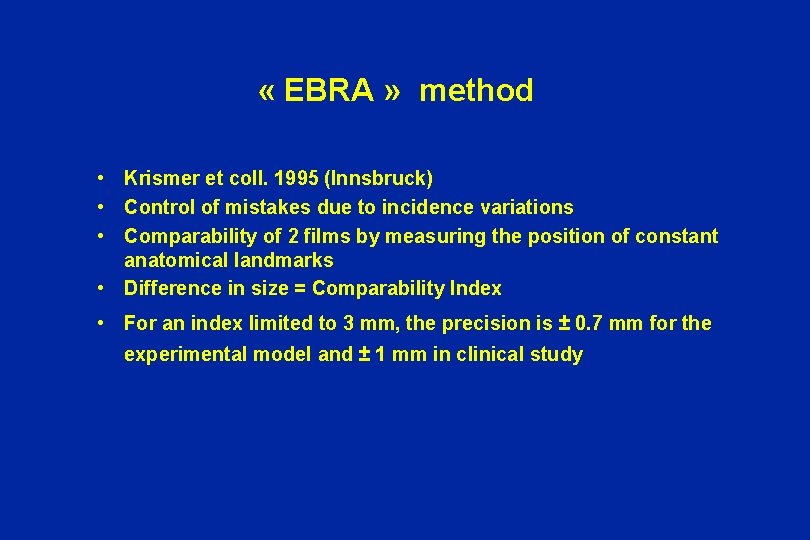
« EBRA » method • Krismer et coll. 1995 (Innsbruck) • Control of mistakes due to incidence variations • Comparability of 2 films by measuring the position of constant anatomical landmarks • Difference in size = Comparability Index • For an index limited to 3 mm, the precision is ± 0. 7 mm for the experimental model and ± 1 mm in clinical study
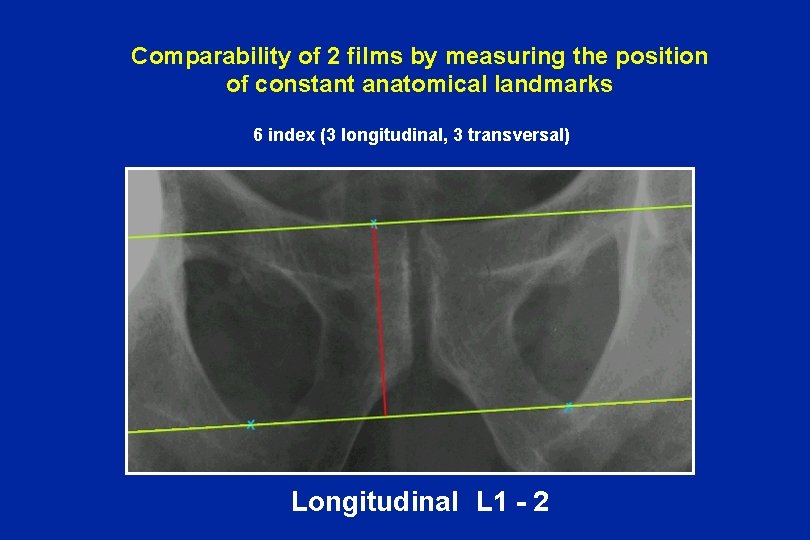
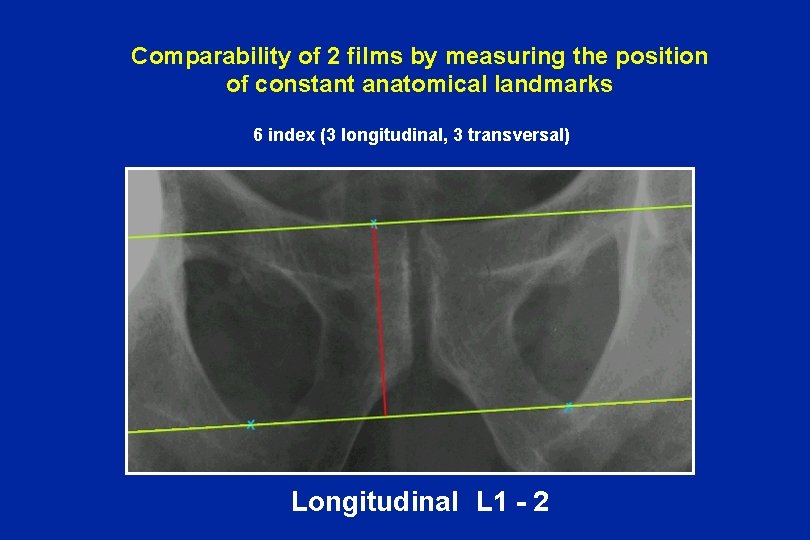
Comparability of 2 films by measuring the position of constant anatomical landmarks 6 index (3 longitudinal, 3 transversal) Longitudinal L 1 - 2
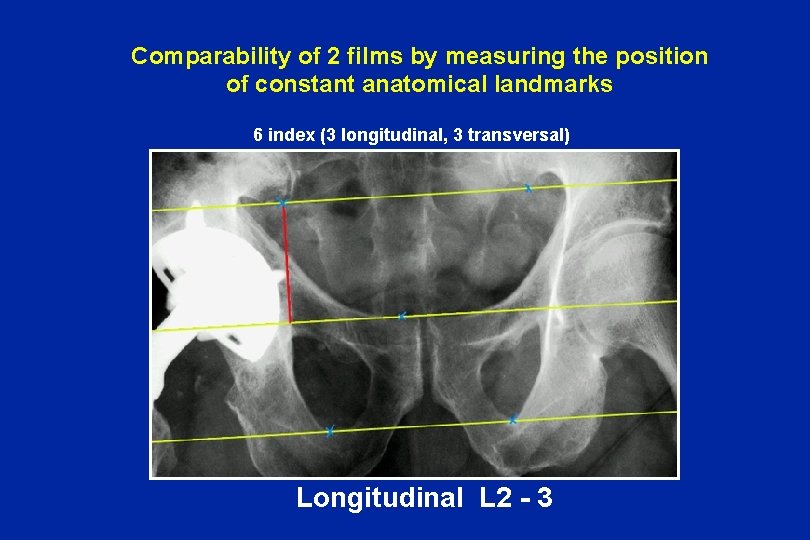
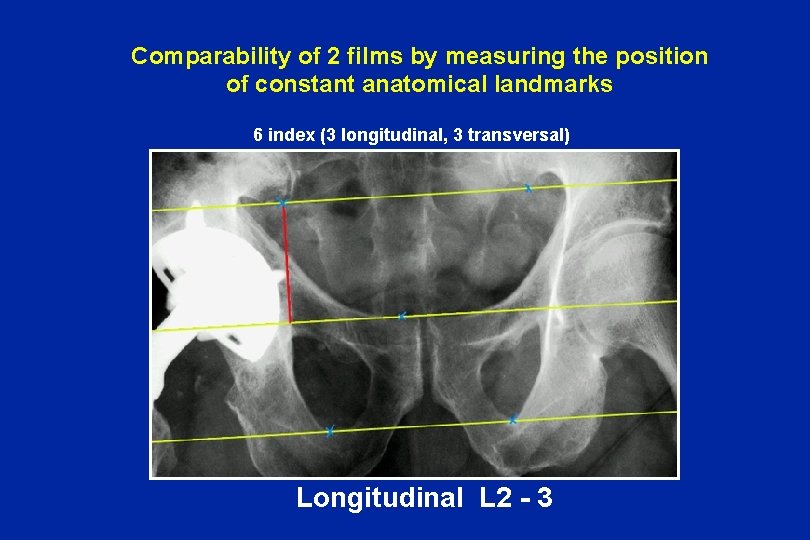
Comparability of 2 films by measuring the position of constant anatomical landmarks 6 index (3 longitudinal, 3 transversal) Longitudinal L 2 - 3
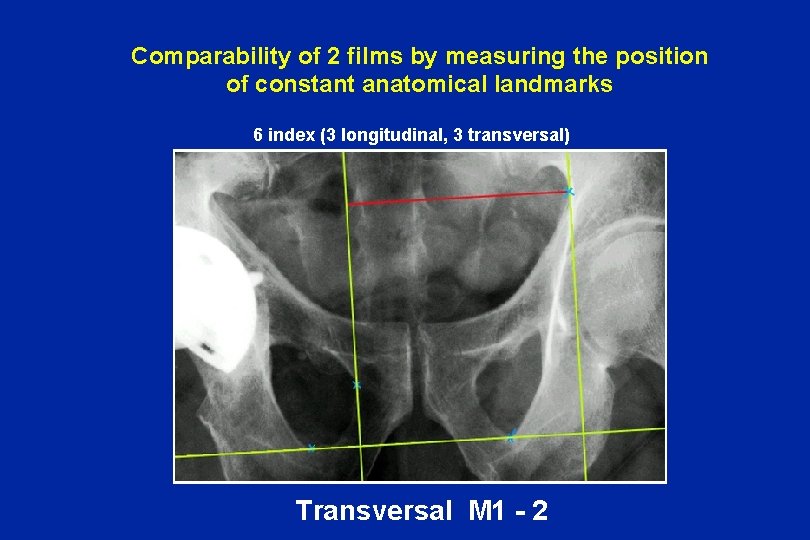
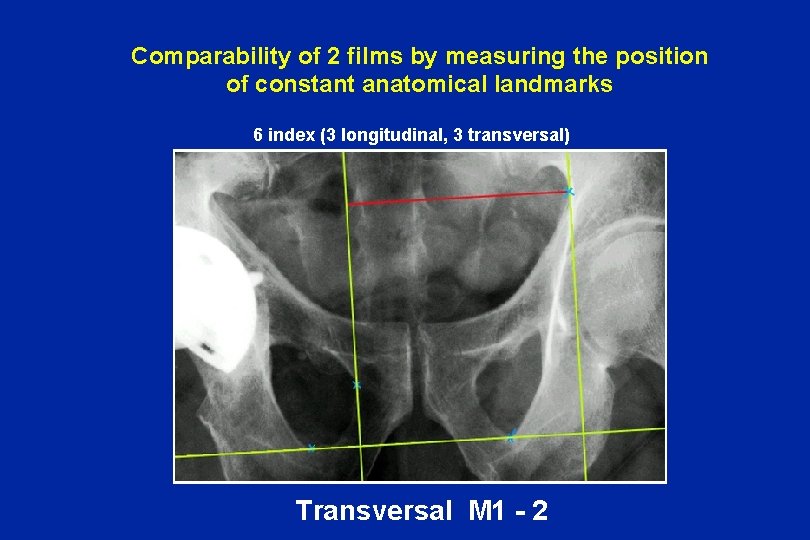
Comparability of 2 films by measuring the position of constant anatomical landmarks 6 index (3 longitudinal, 3 transversal) Transversal M 1 - 2
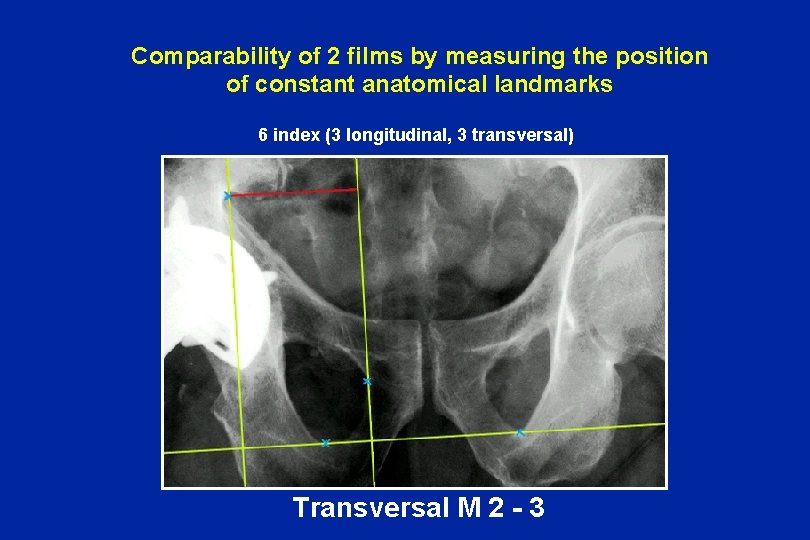
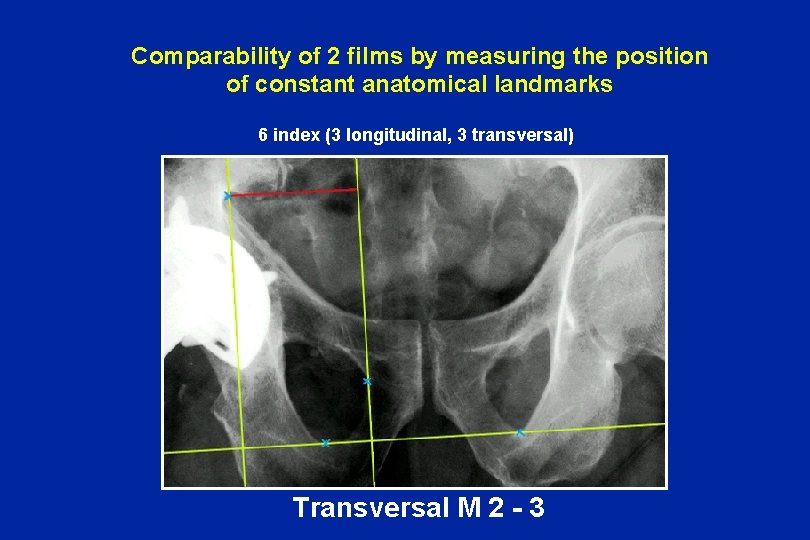
Comparability of 2 films by measuring the position of constant anatomical landmarks 6 index (3 longitudinal, 3 transversal) Transversal M 2 - 3
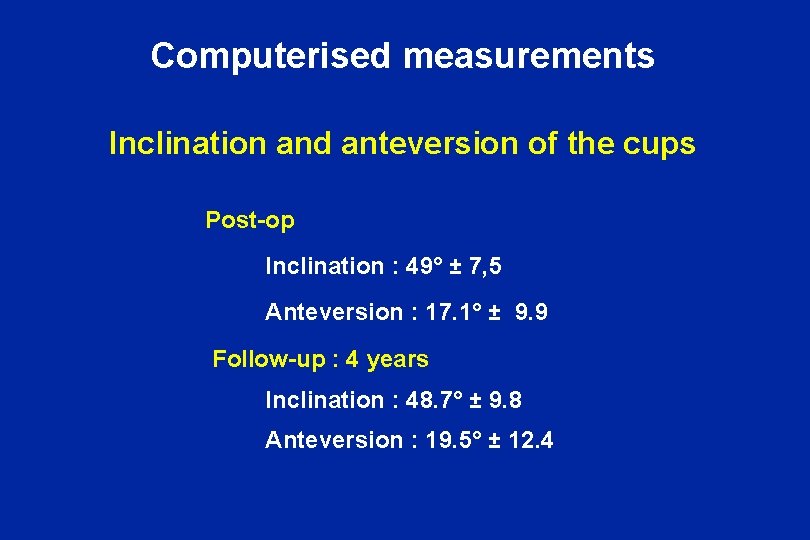
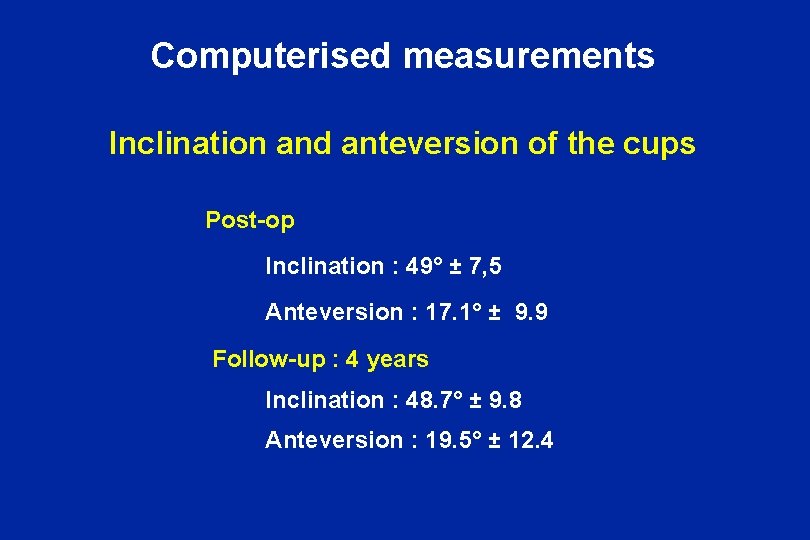
Computerised measurements Inclination and anteversion of the cups Post-op Inclination : 49° ± 7, 5 Anteversion : 17. 1° ± 9. 9 Follow-up : 4 years Inclination : 48. 7° ± 9. 8 Anteversion : 19. 5° ± 12. 4
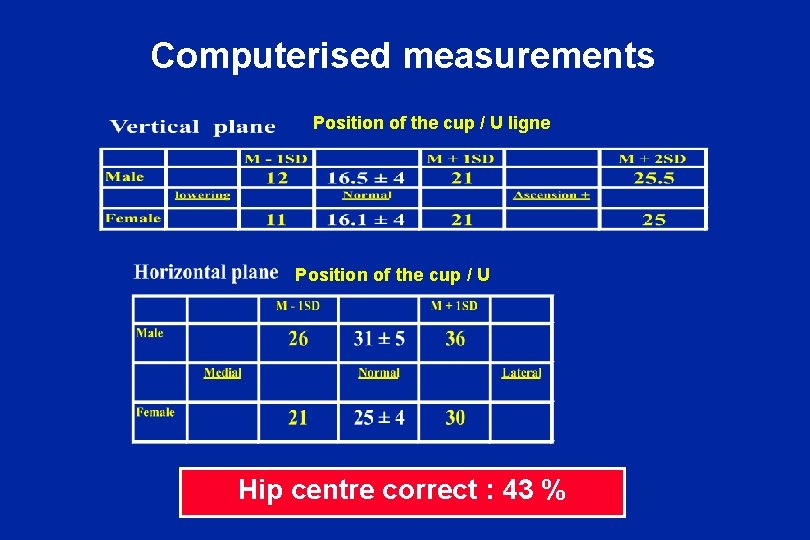
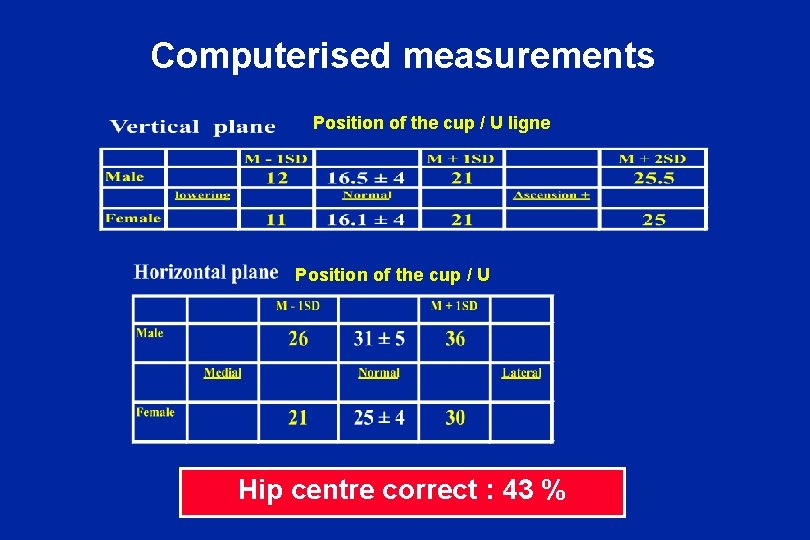
Computerised measurements Position of the cup / U ligne Position of the cup / U Hip centre correct : 43 %
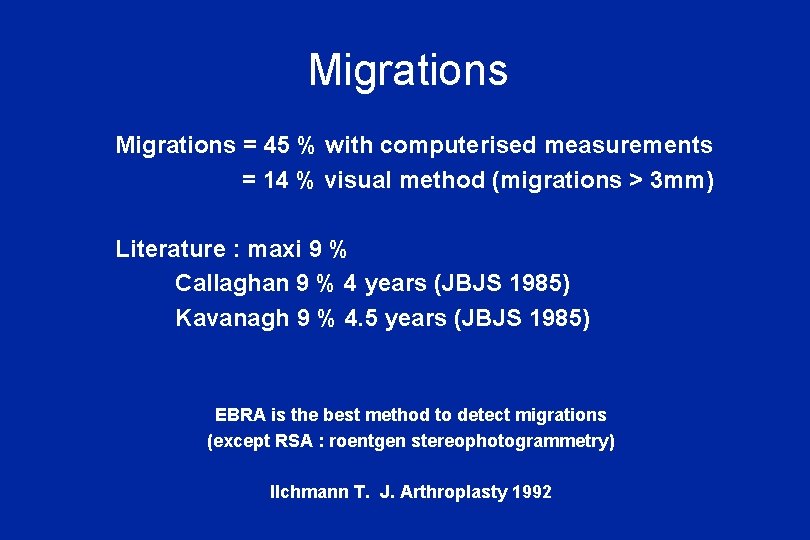
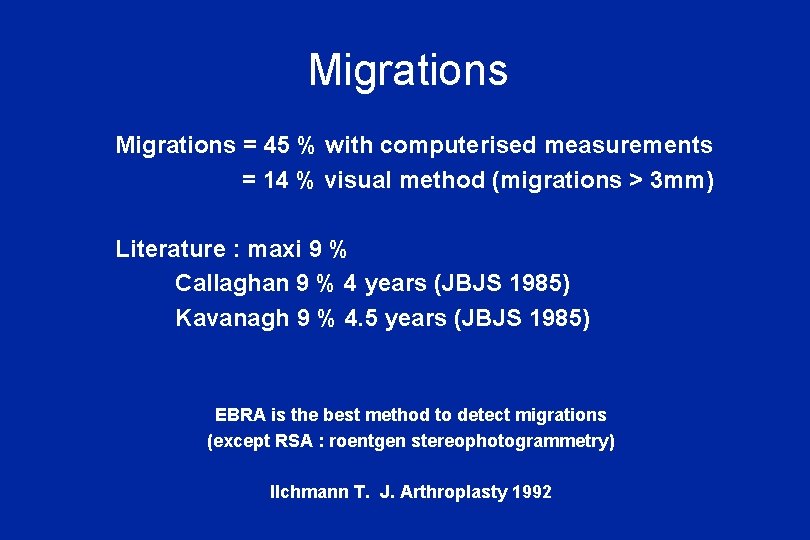
Migrations = 45 % with computerised measurements = 14 % visual method (migrations > 3 mm) Literature : maxi 9 % Callaghan 9 % 4 years (JBJS 1985) Kavanagh 9 % 4. 5 years (JBJS 1985) EBRA is the best method to detect migrations (except RSA : roentgen stereophotogrammetry) Ilchmann T. J. Arthroplasty 1992

1 example of verticalisation and ascencion Post op 6 months Stable after 1 year
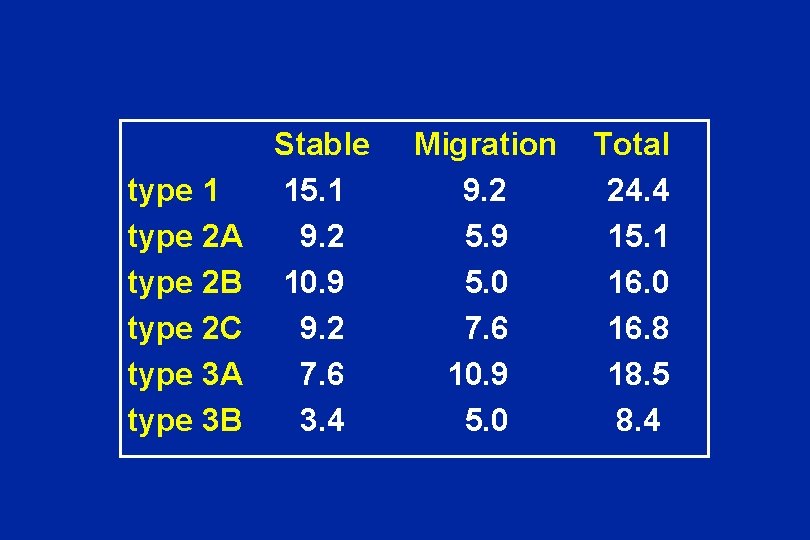
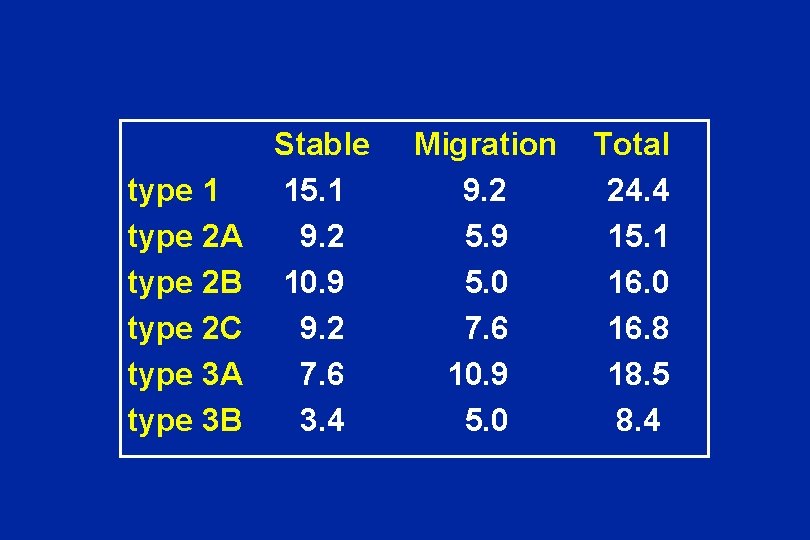
Stable Migration Total type 1 15. 1 9. 2 24. 4 type 2 A 9. 2 5. 9 15. 1 type 2 B 10. 9 5. 0 16. 0 type 2 C 9. 2 7. 6 16. 8 type 3 A 7. 6 10. 9 18. 5 type 3 B 3. 4 5. 0 8. 4
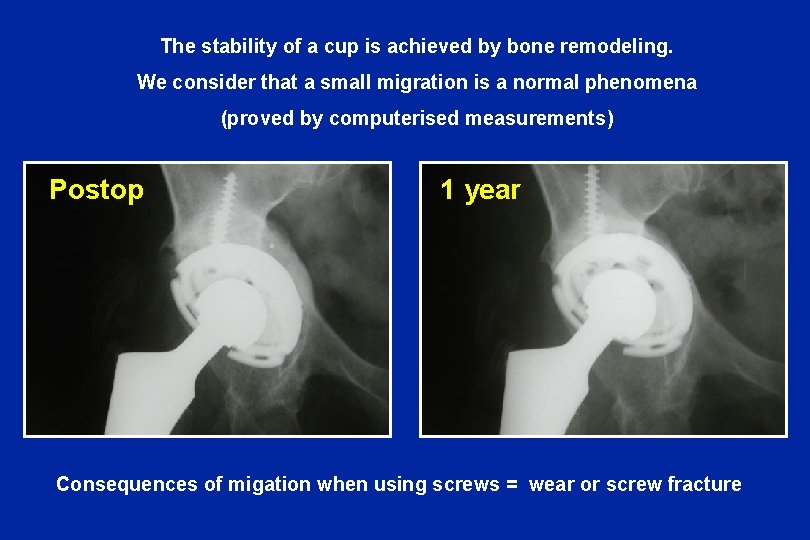
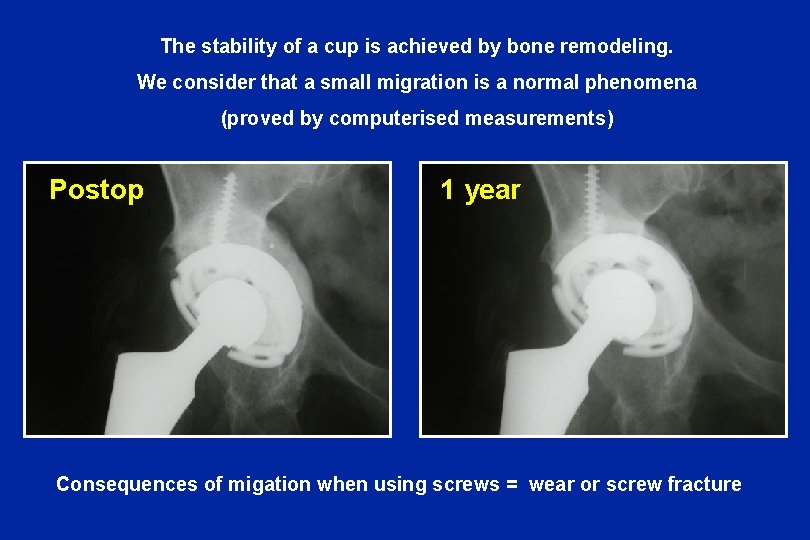
The stability of a cup is achieved by bone remodeling. We consider that a small migration is a normal phenomena (proved by computerised measurements) Postop 1 year Consequences of migation when using screws = wear or screw fracture

Mobility between the cup and the screws has consequences : Impression in the polyethylene ± metallic wear ± fractures of the screws
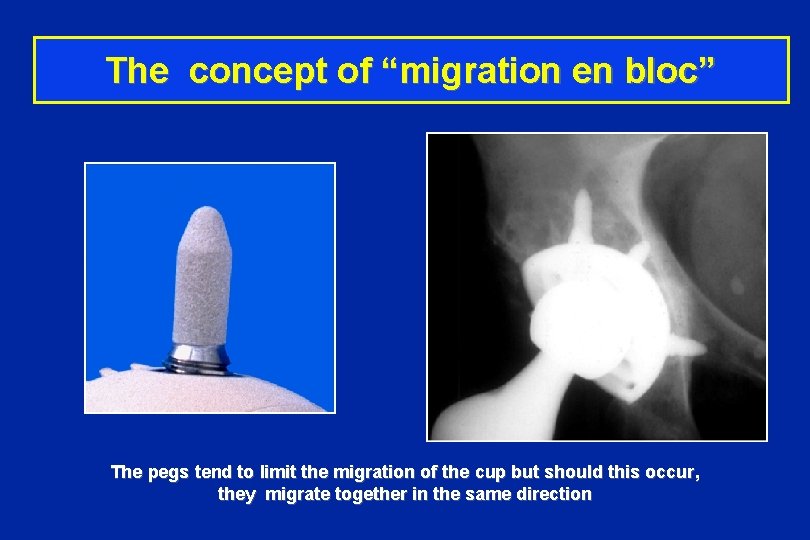
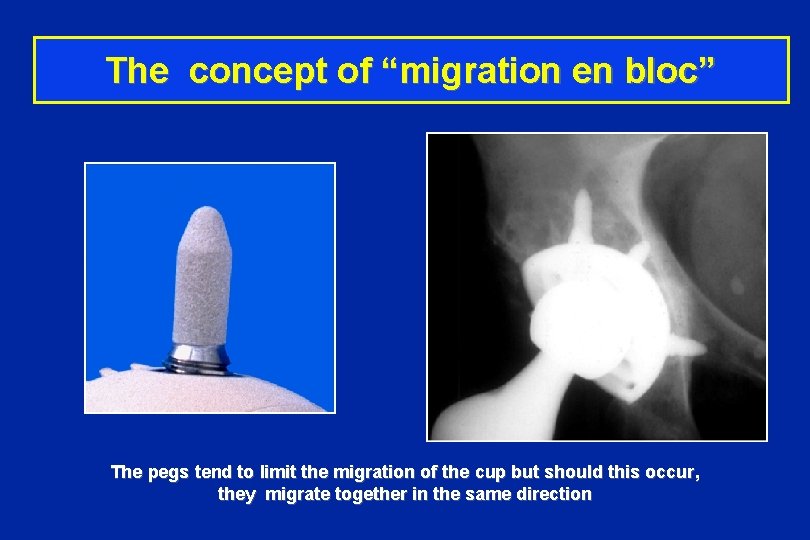
The concept of “migration en bloc” The pegs tend to limit the migration of the cup but should this occur, they migrate together in the same direction
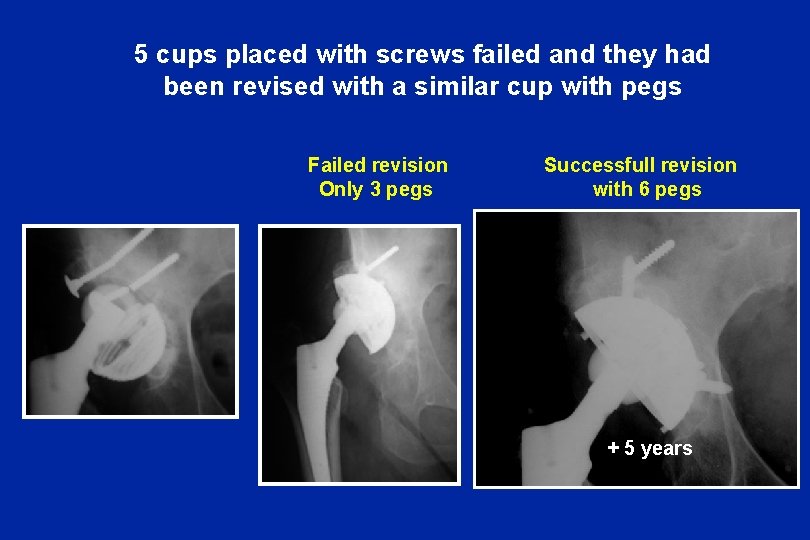
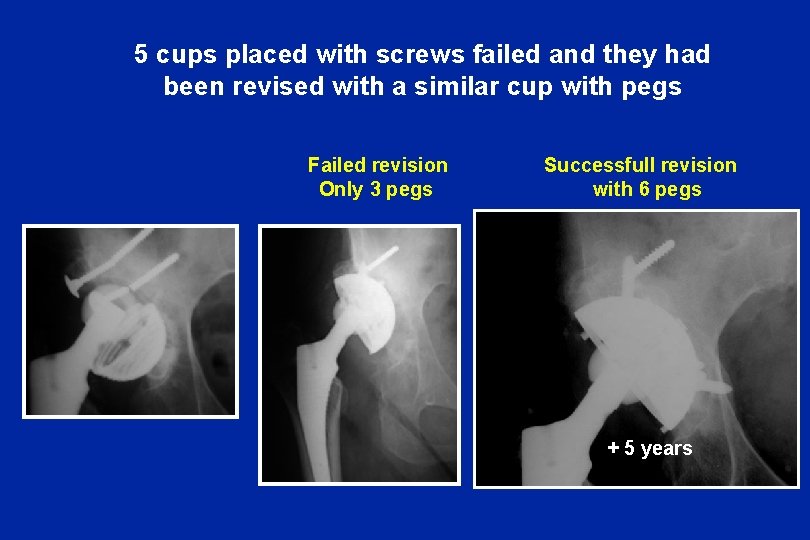
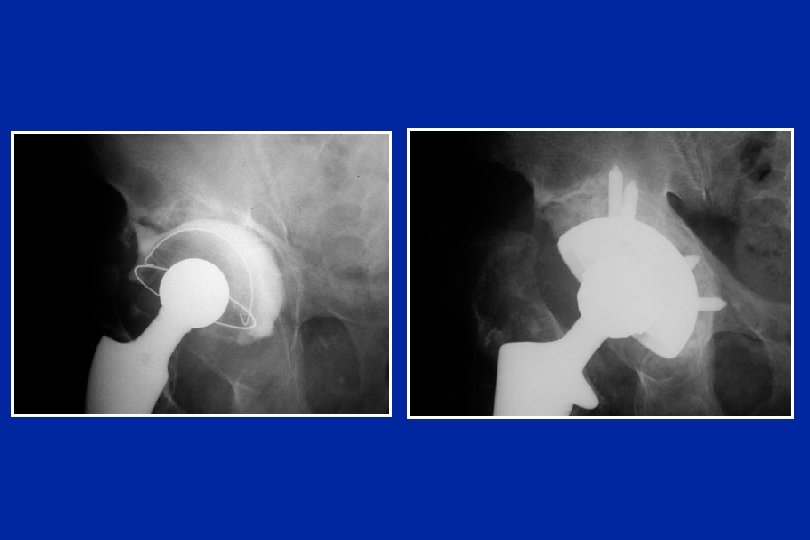
5 cups placed with screws failed and they had been revised with a similar cup with pegs Failed revision Only 3 pegs Successfull revision with 6 pegs + 5 years

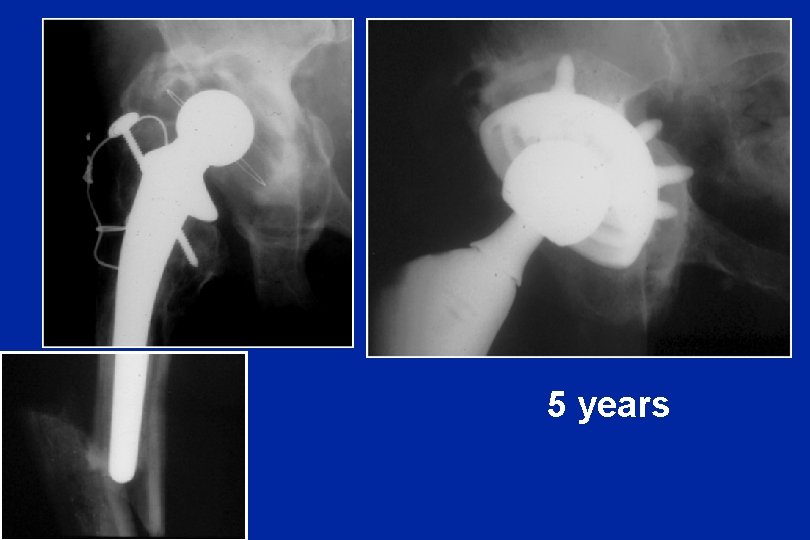
5 years 5 ans
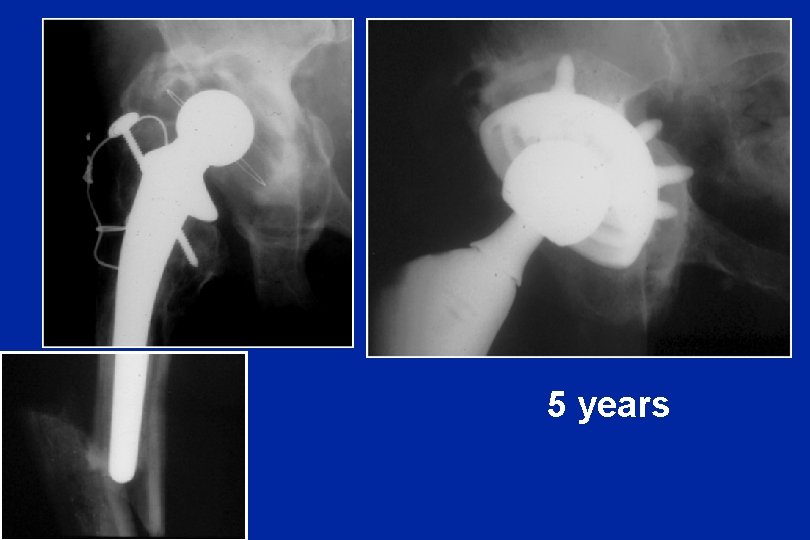
5 years

6 years

13 infected cases Two-steps revision 3 recurences of infection finally healed

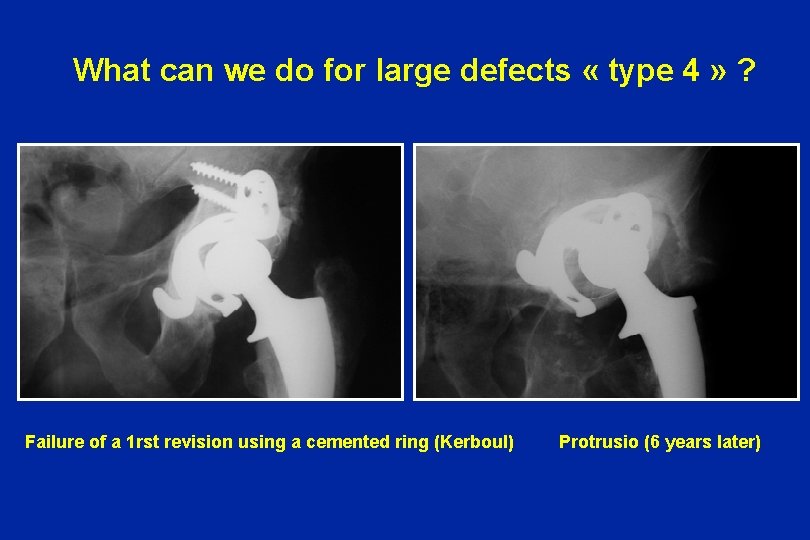
The limits of this cup Type 4 Destruction of the roof and 2 columns + destruction of inferior bone
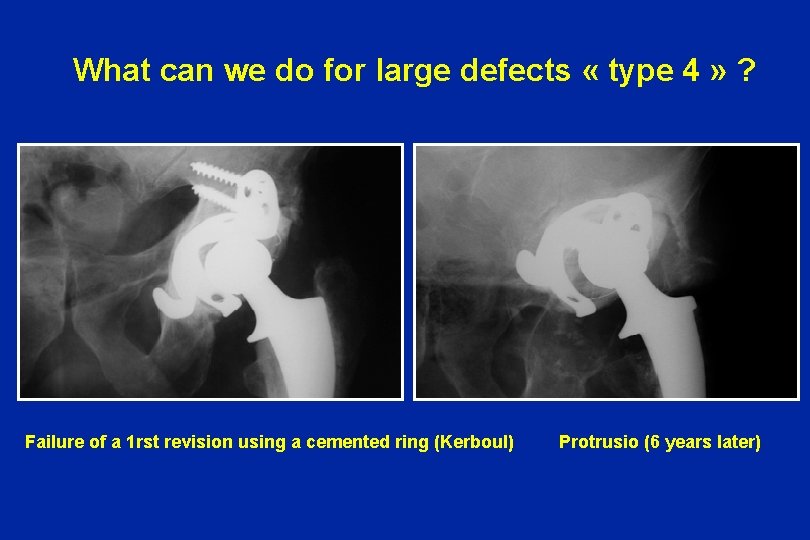
What can we do for large defects « type 4 » ? Failure of a 1 rst revision using a cemented ring (Kerboul) Protrusio (6 years later)
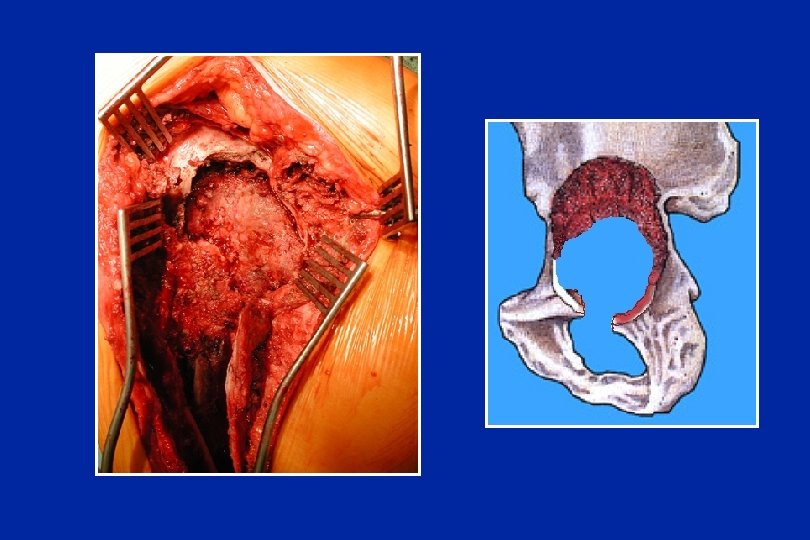

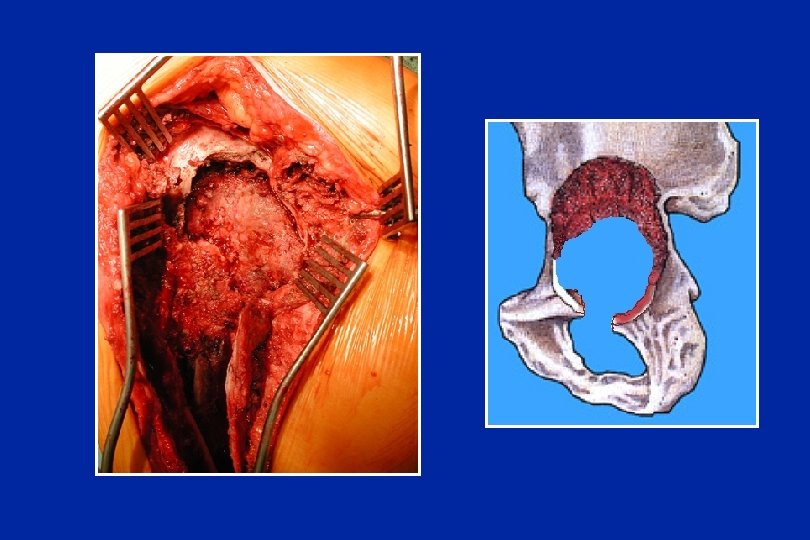
Granuloma + cement

The host bone and the cancellous bone graft cannot find any possibility of ingrowht on this surface
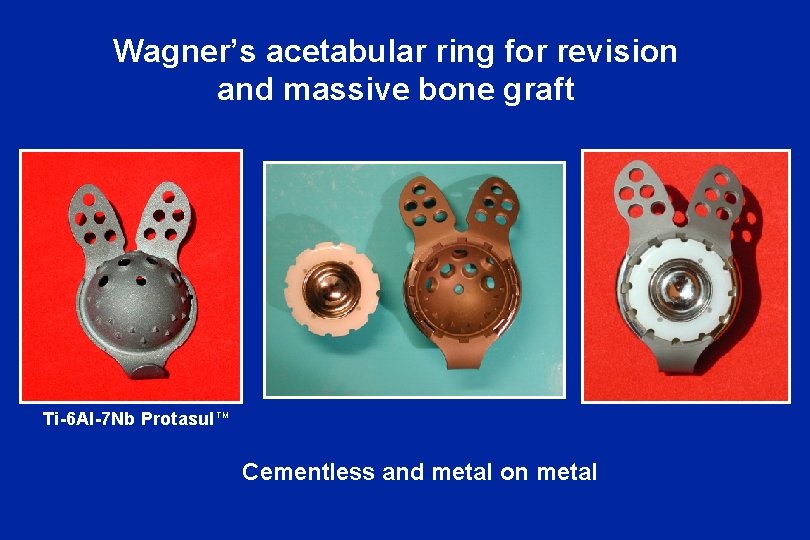
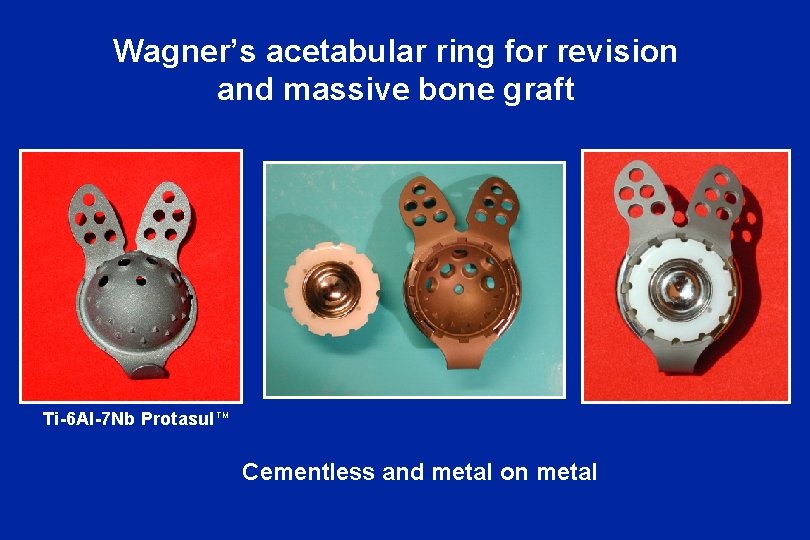
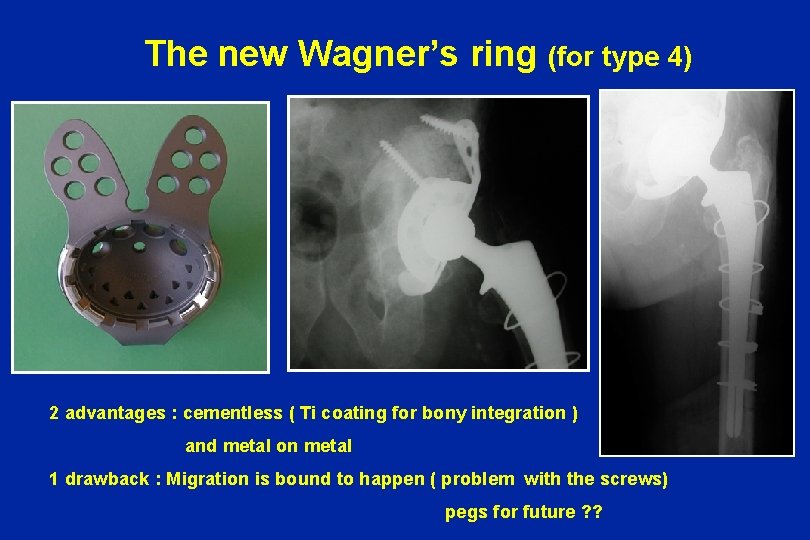
Wagner’s acetabular ring for revision and massive bone graft Ti-6 Al-7 Nb Protasul TM Cementless and metal on metal
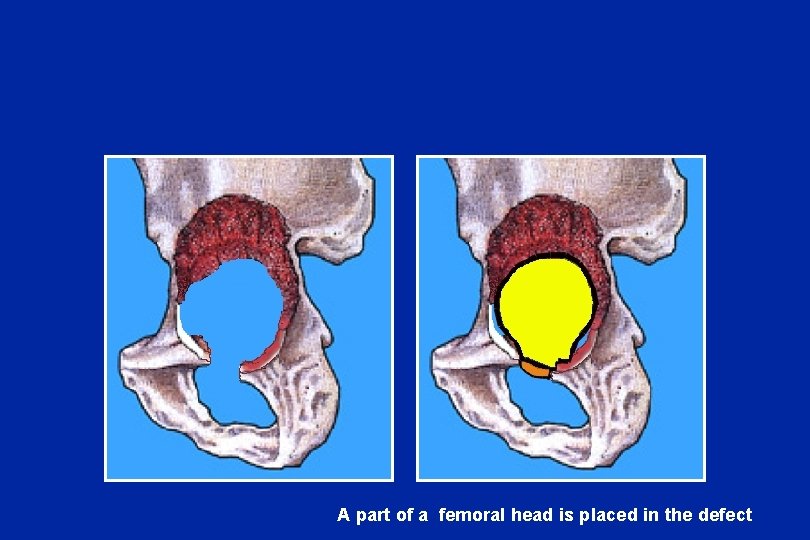
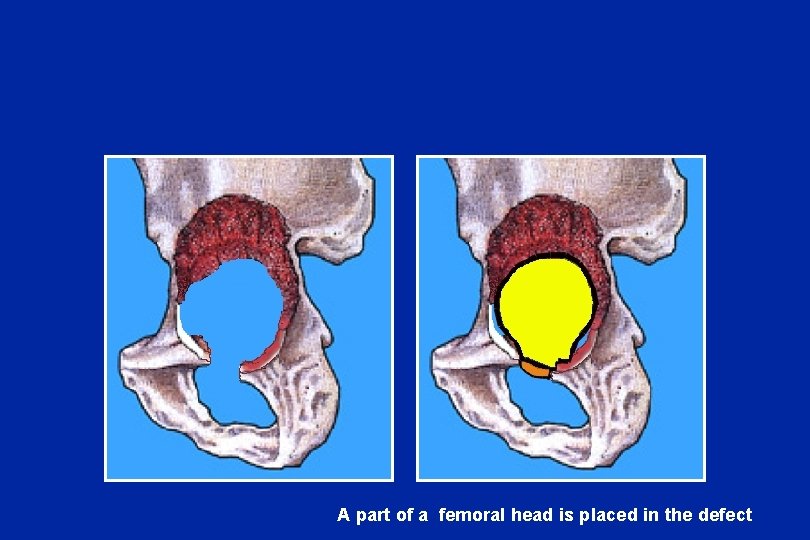
A part of a femoral head is placed in the defect

Cortico-spongious blocks to reconstruct the columns and the roof
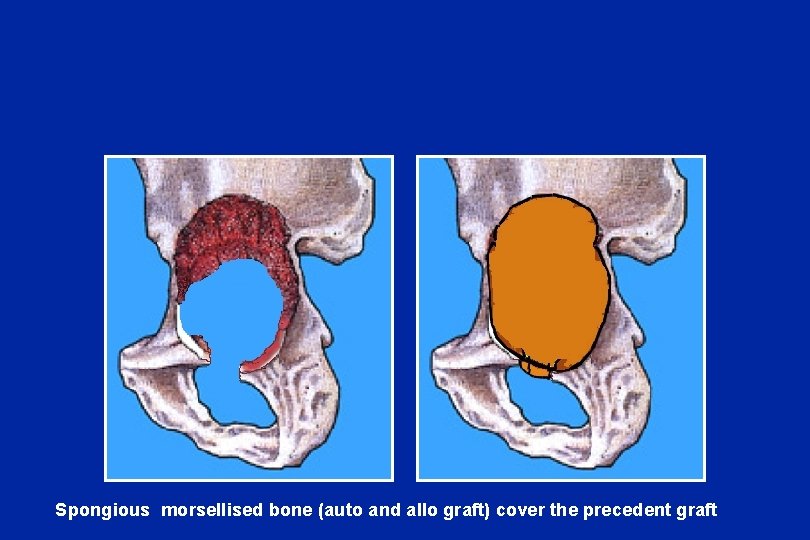
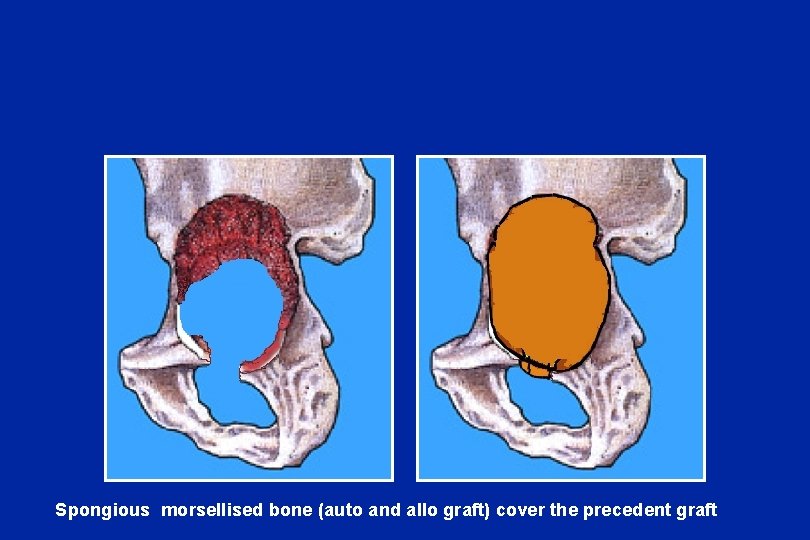
Spongious morsellised bone (auto and allo graft) cover the precedent graft
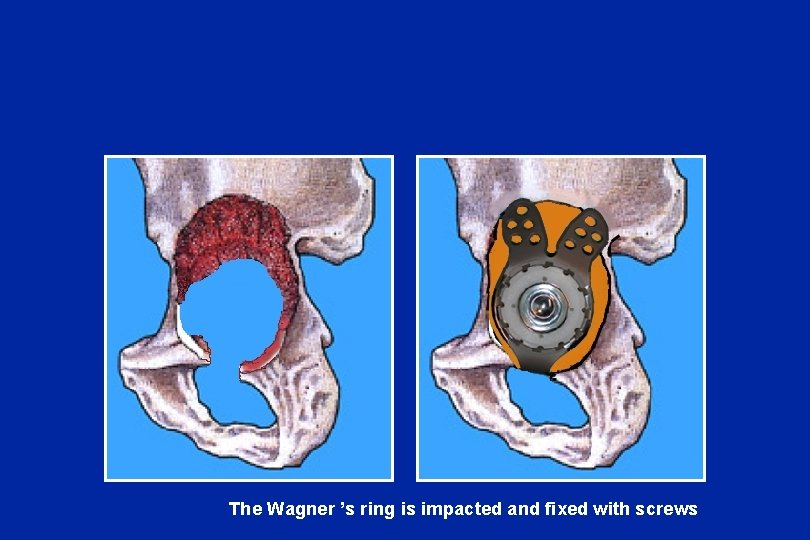
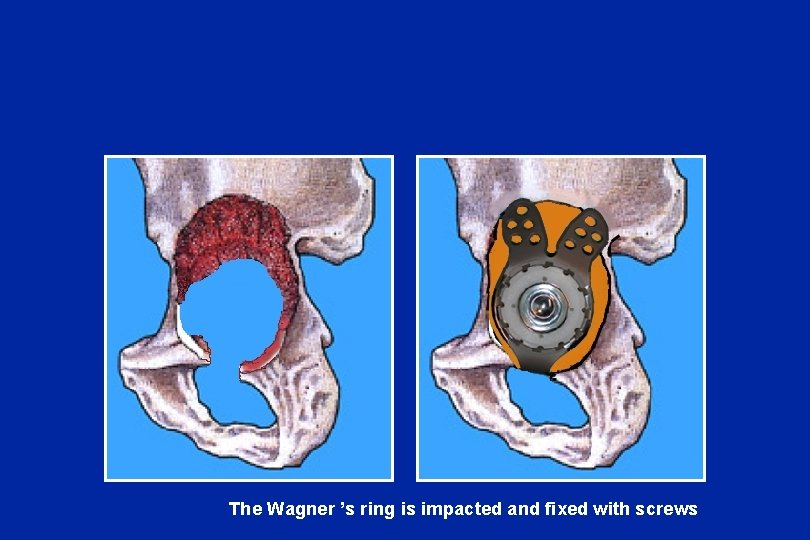
The Wagner ’s ring is impacted and fixed with screws
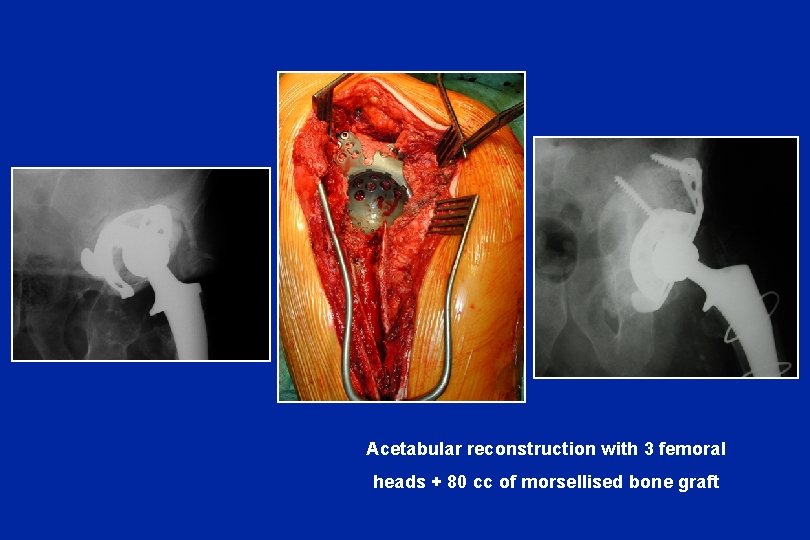
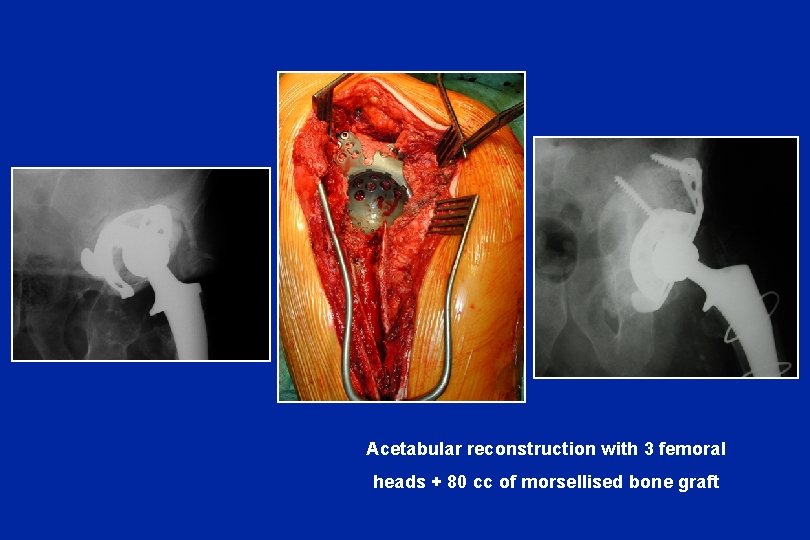
Acetabular reconstruction with 3 femoral heads + 80 cc of morsellised bone graft
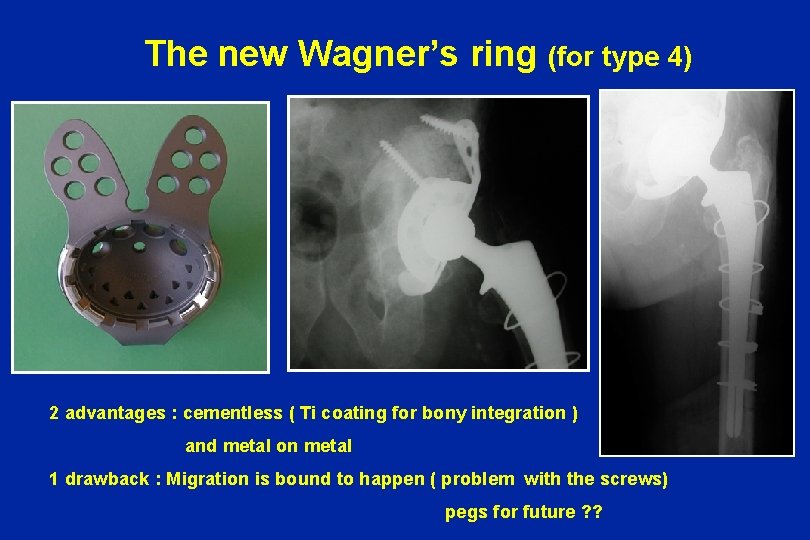
The new Wagner’s ring (for type 4) 2 advantages : cementless ( Ti coating for bony integration ) and metal on metal 1 drawback : Migration is bound to happen ( problem with the screws) pegs for future ? ?
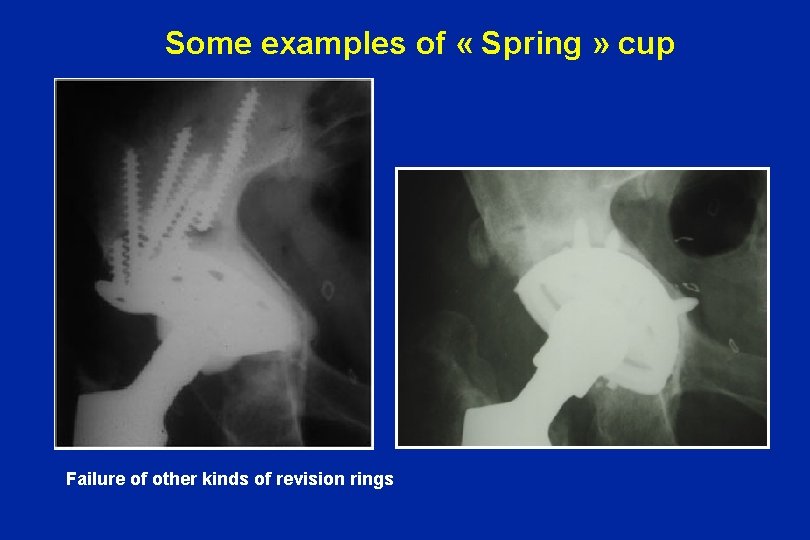
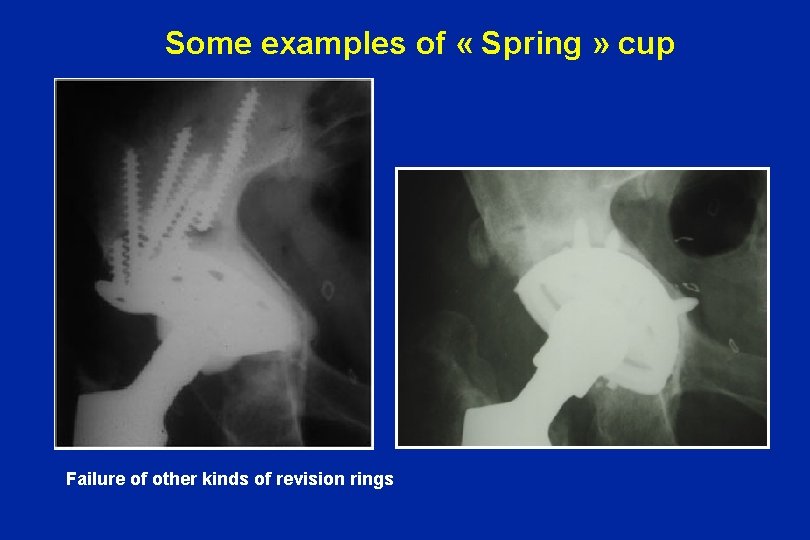
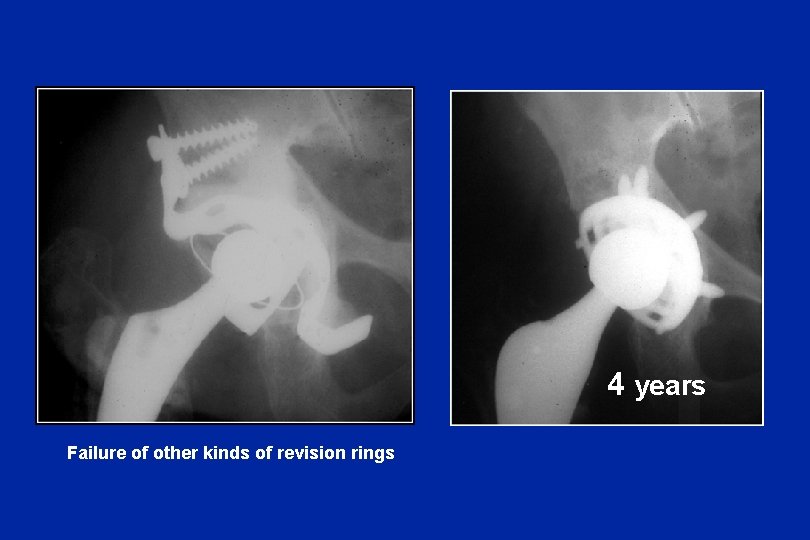
Some examples of « Spring » cup Failure of other kinds of revision rings
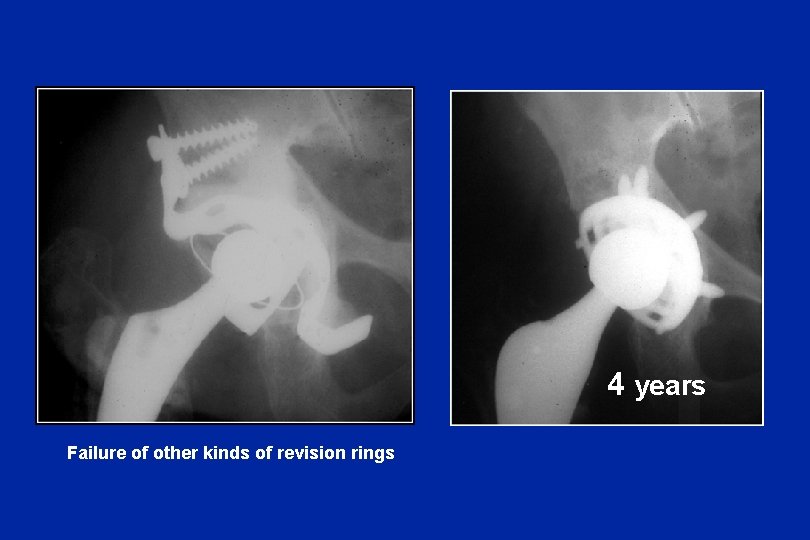
4 years Failure of other kinds of revision rings
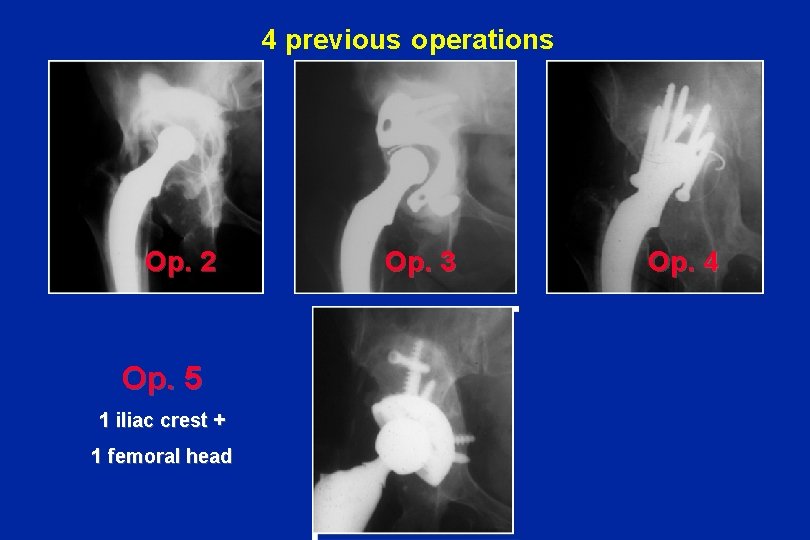
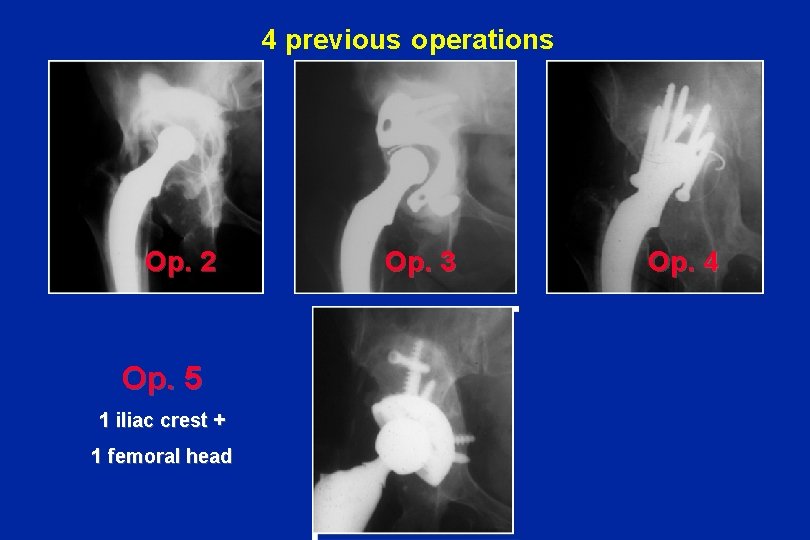
4 previous operations Op. 2 Op. 3 Op. 5 1 iliac crest + 1 femoral head Face + 5 ans Op. 4
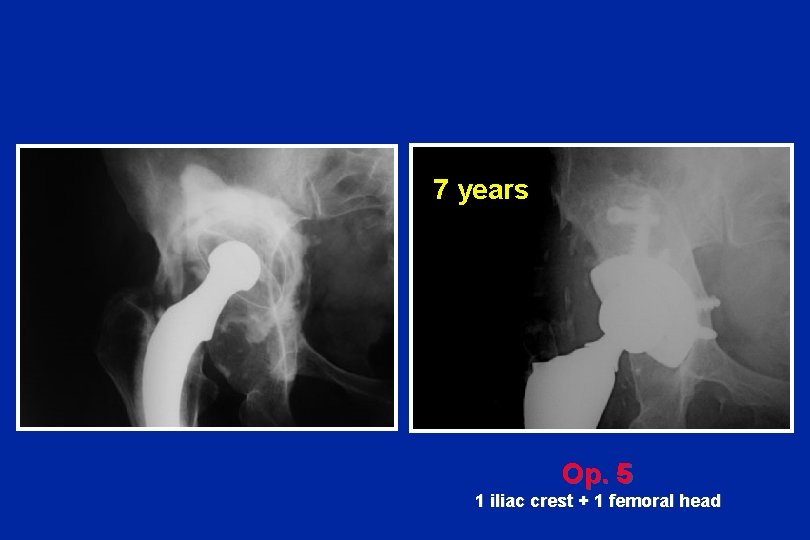
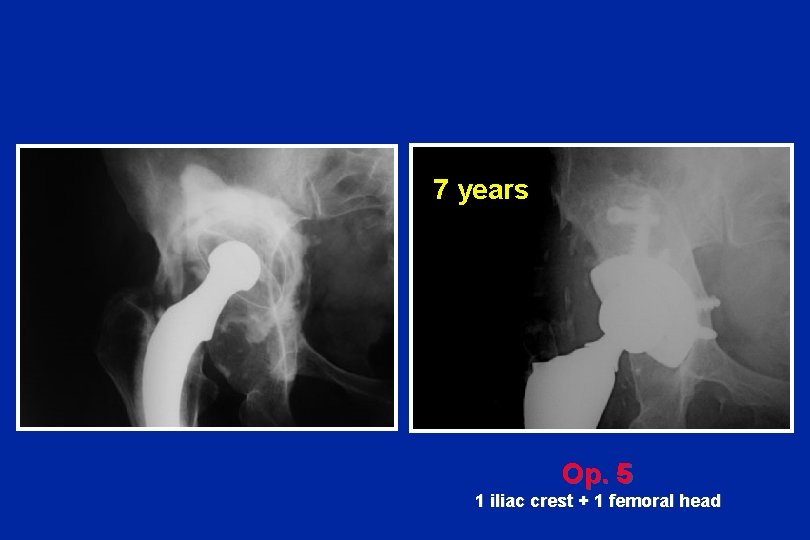
7 years Op. 5 1 iliac crest + 1 femoral head
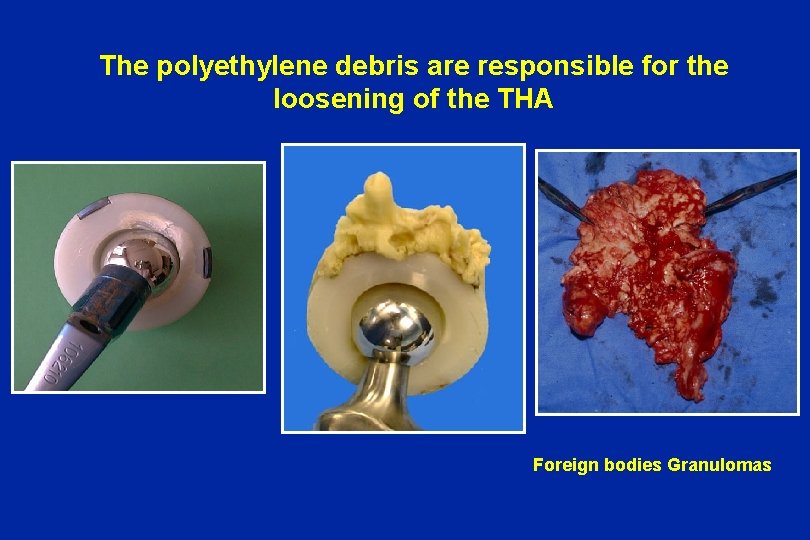
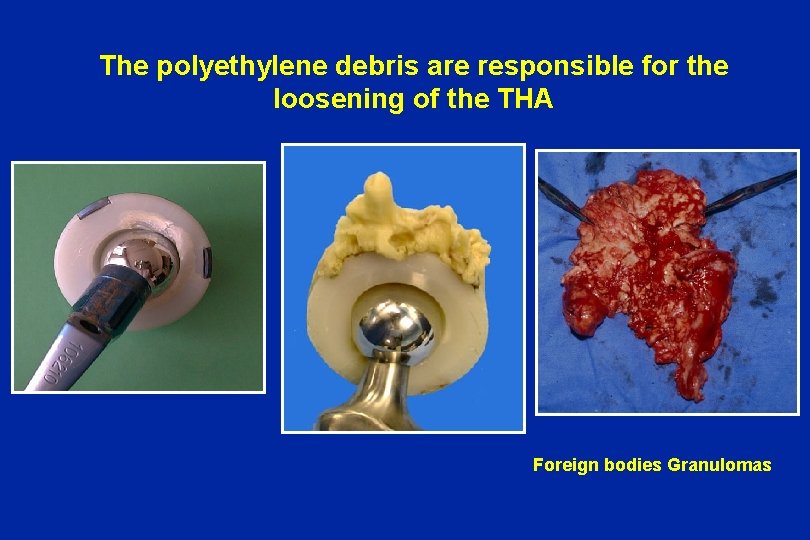
The polyethylene debris are responsible for the loosening of the THA Foreign bodies Granulomas

Acetabular reconstruction is often associated with femoral problems


Polyethylene and metal-back must be eradicated

Polyethylene must be replaced by better materials Alumina on alumina Alumine - polyéthylène Alumine - alumine Metal on metal Zircone - zircone
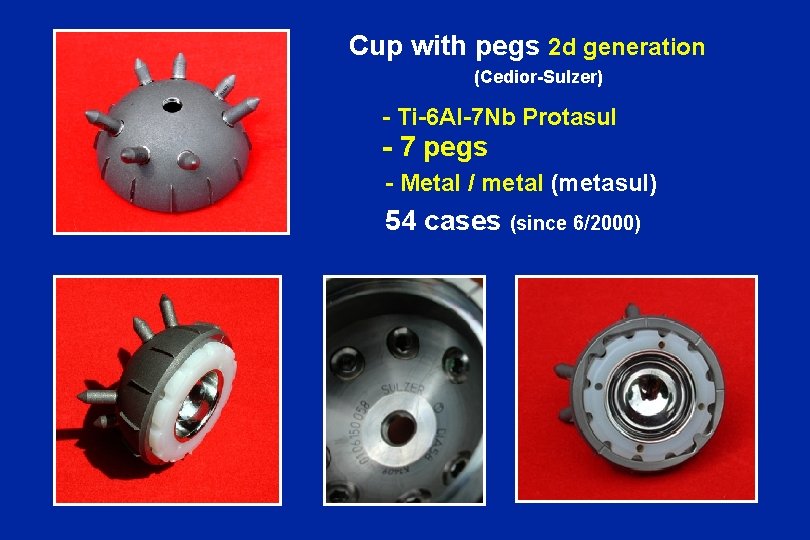
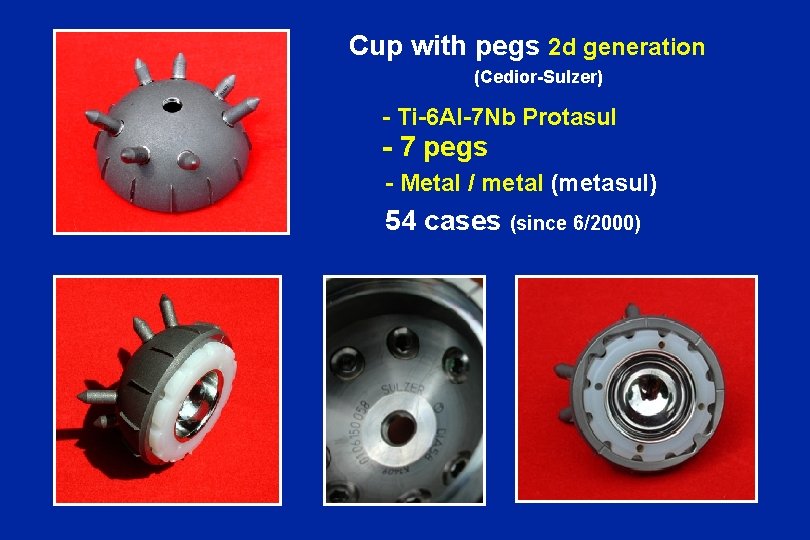
Cup with pegs 2 d generation (Cedior-Sulzer) - Ti-6 Al-7 Nb Protasul - 7 pegs - Metal / metal (metasul) 54 cases (since 6/2000)
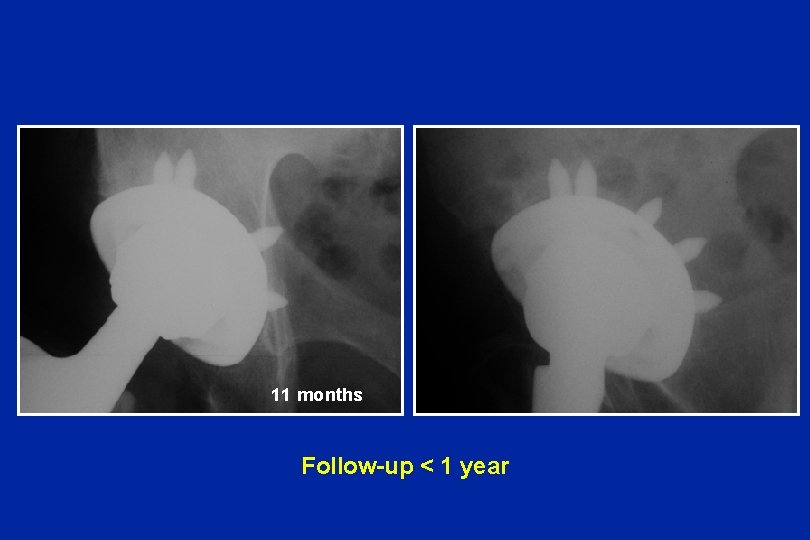
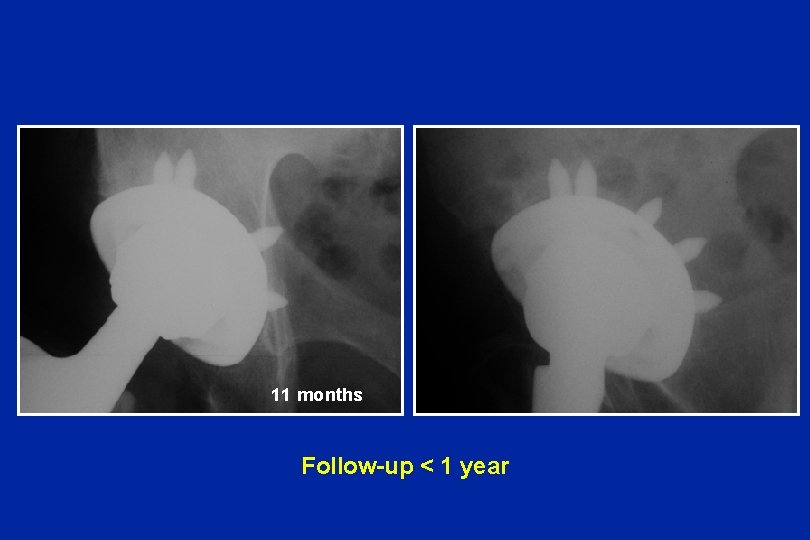
11 months Follow-up < 1 year
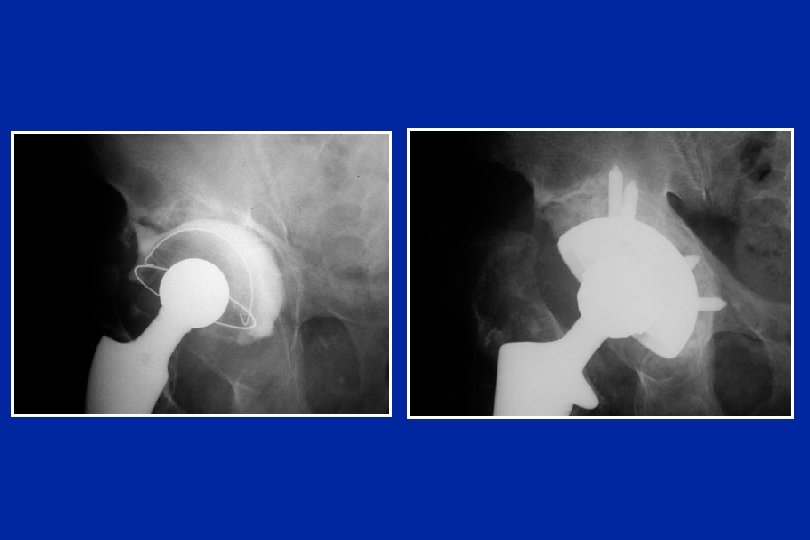
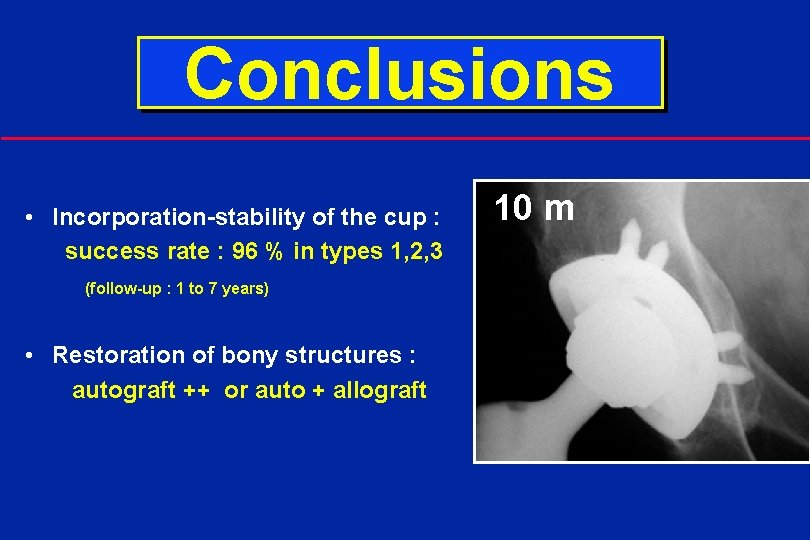
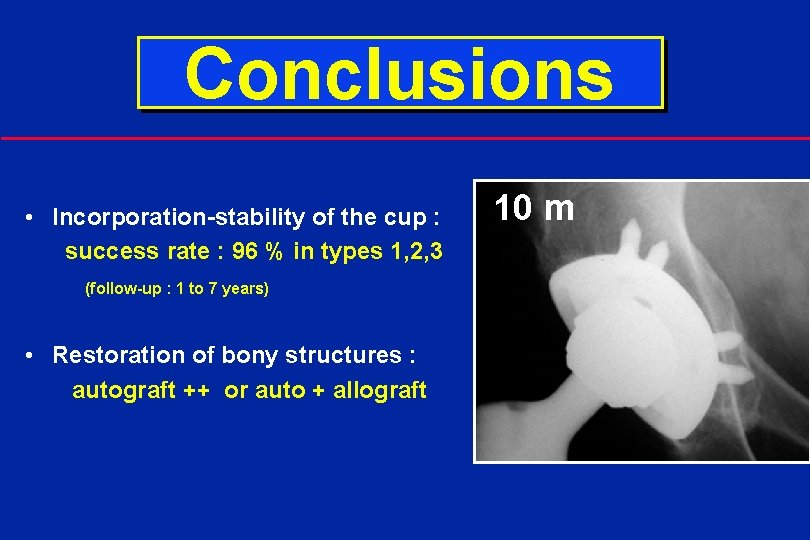
Conclusions • Incorporation-stability of the cup : success rate : 96 % in types 1, 2, 3 (follow-up : 1 to 7 years) • Restoration of bony structures : autograft ++ or auto + allograft 10 m
Conclusions • Usefulness of non cemented cups (HAP or Ti) • Interest of the pegs fixed to the cup • Pegs are preferable to screws • Pegs do not interfere with small migration during osteo-integration
 Hap
Hap Szte hap
Szte hap Hap ci
Hap ci Health informatics gmu
Health informatics gmu Hap python
Hap python Bu nedir
Bu nedir Hap farber
Hap farber Hap introduction
Hap introduction Hệ hô hấp
Hệ hô hấp Map hap
Map hap Hap griffin
Hap griffin I must have drunk four cups of cocoa
I must have drunk four cups of cocoa Does the cup and string work
Does the cup and string work An overheated marathon runner accepts cups
An overheated marathon runner accepts cups Cups ems acronym
Cups ems acronym Dustpan function
Dustpan function Standard dry/solid measuring cups come in what four sizes
Standard dry/solid measuring cups come in what four sizes Half of 1 1/3 cup
Half of 1 1/3 cup Kloiber cups
Kloiber cups Ecology measuring cups
Ecology measuring cups I must have drunk four cups of cocoa
I must have drunk four cups of cocoa 8 of cups artinya
8 of cups artinya Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan Sự nuôi và dạy con của hươu
Sự nuôi và dạy con của hươu điện thế nghỉ
điện thế nghỉ Một số thể thơ truyền thống
Một số thể thơ truyền thống Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Slidetodoc
Slidetodoc So nguyen to
So nguyen to đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Fecboak
Fecboak Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Tư thế worms-breton
Tư thế worms-breton Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất ưu thế lai là gì
ưu thế lai là gì Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Tư thế ngồi viết
Tư thế ngồi viết Cái miệng nó xinh thế chỉ nói điều hay thôi
Cái miệng nó xinh thế chỉ nói điều hay thôi Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Bổ thể
Bổ thể Tư thế ngồi viết
Tư thế ngồi viết Thẻ vin
Thẻ vin Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Bài hát chúa yêu trần thế alleluia
Bài hát chúa yêu trần thế alleluia Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Hổ sinh sản vào mùa nào
Hổ sinh sản vào mùa nào Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Diễn thế sinh thái là
Diễn thế sinh thái là Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau V. c c
V. c c Phép trừ bù
Phép trừ bù Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Lời thề hippocrates
Lời thề hippocrates đại từ thay thế
đại từ thay thế Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Các môn thể thao bắt đầu bằng từ đua
Các môn thể thao bắt đầu bằng từ đua Công thức tính thế năng
Công thức tính thế năng Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Dot
Dot Thế nào là sự mỏi cơ
Thế nào là sự mỏi cơ Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể độ dài liên kết
độ dài liên kết Chó sói
Chó sói Preliminary results example
Preliminary results example Cpea results 2012 grenada
Cpea results 2012 grenada Erasmus+ project results platform
Erasmus+ project results platform Pace palette results
Pace palette results Csca ima
Csca ima A transformation of δdef results in δd'e'f'.
A transformation of δdef results in δd'e'f'. Niat results
Niat results Every system is designed to get the results it gets
Every system is designed to get the results it gets Nhls trakcare lab results
Nhls trakcare lab results Weltec design
Weltec design Erasmus result platform
Erasmus result platform Results and discussion in research
Results and discussion in research Albane demblans
Albane demblans Pisa 2018 results
Pisa 2018 results Middle ages regents questions
Middle ages regents questions Atca results
Atca results Sap sd benchmark
Sap sd benchmark Eu results framework
Eu results framework Rso test results
Rso test results Lincoln
Lincoln Flame test results table
Flame test results table Rpms phase 1
Rpms phase 1 Unearh
Unearh