The Respiratory System Respiratory System Functions Pulmonary ventilation



- Slides: 45
The Respiratory System
Respiratory System Functions • Pulmonary ventilation movement of air into and out of lungs “breathing” • External respiration movement of O 2 and CO 2 between blood and lungs • Transport of respiratory gases transport of O 2 and CO 2 between tissue and lungs • Internal respiration movement of O 2 and CO 2 between blood and tissue • Olfaction
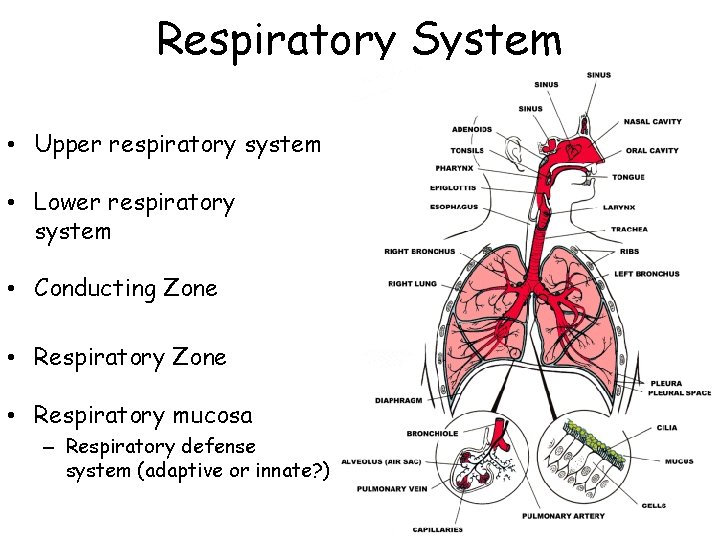
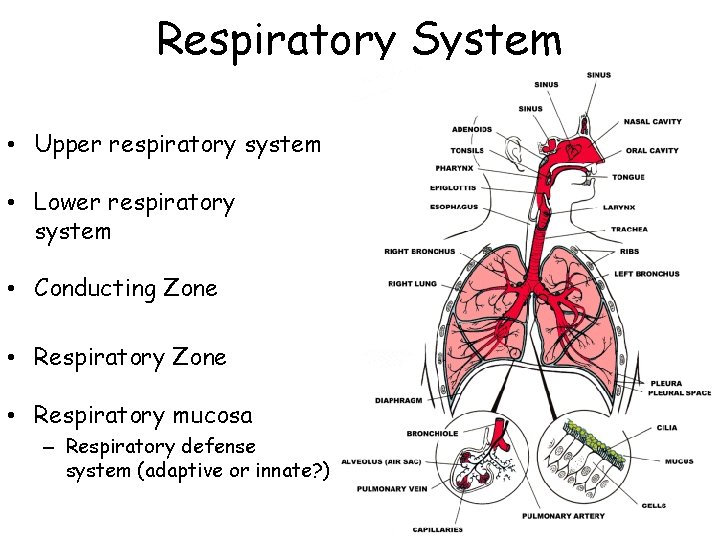
Respiratory System • Upper respiratory system • Lower respiratory system • Conducting Zone • Respiratory mucosa – Respiratory defense system (adaptive or innate? )
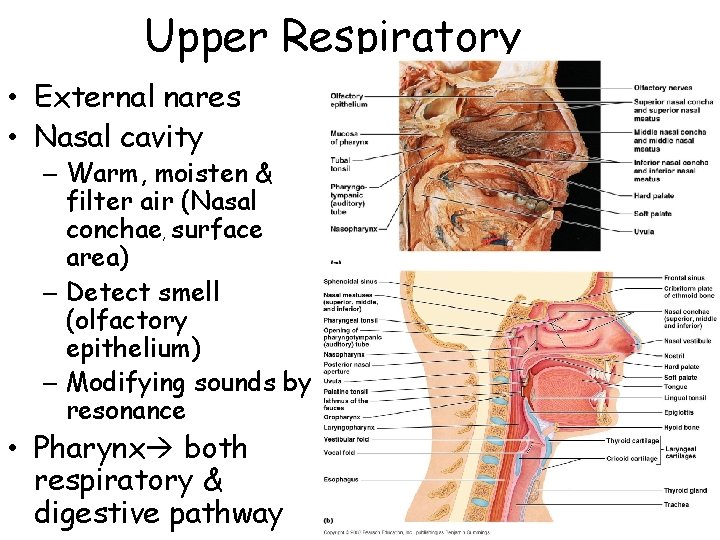
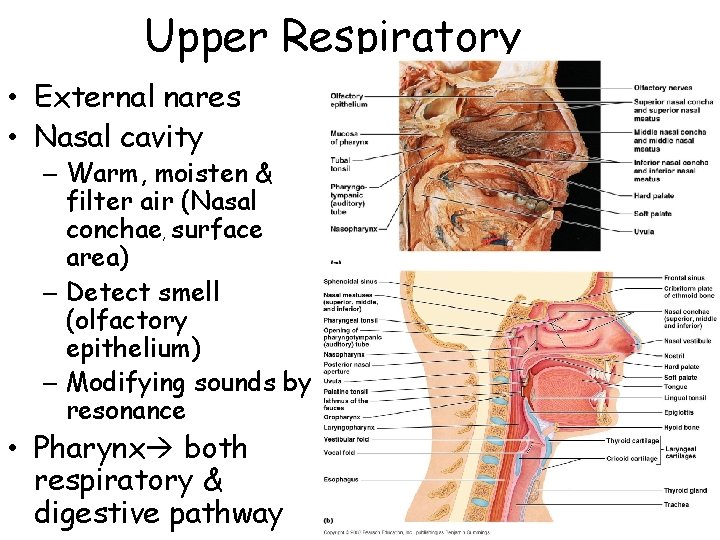
Upper Respiratory • External nares • Nasal cavity – Warm, moisten & filter air (Nasal conchae, surface area) – Detect smell (olfactory epithelium) – Modifying sounds by resonance • Pharynx both respiratory & digestive pathway
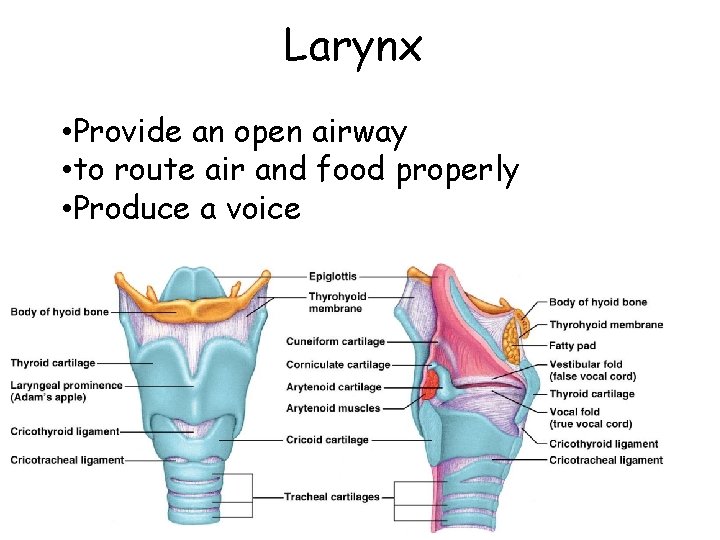
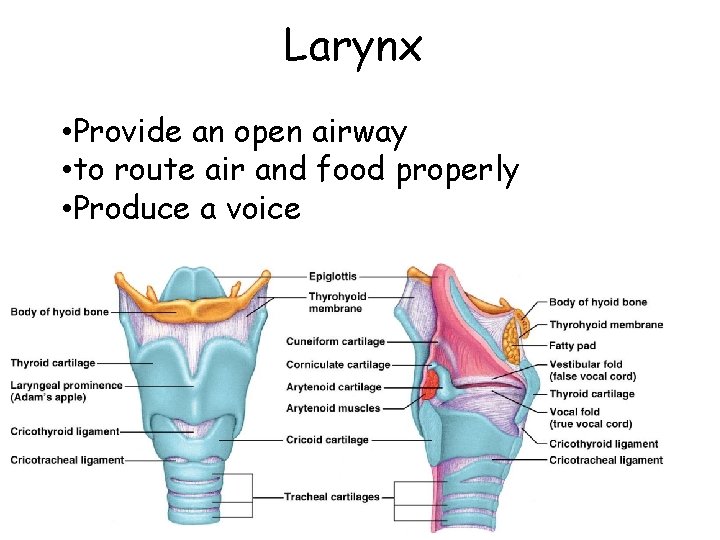
Larynx • Provide an open airway • to route air and food properly • Produce a voice
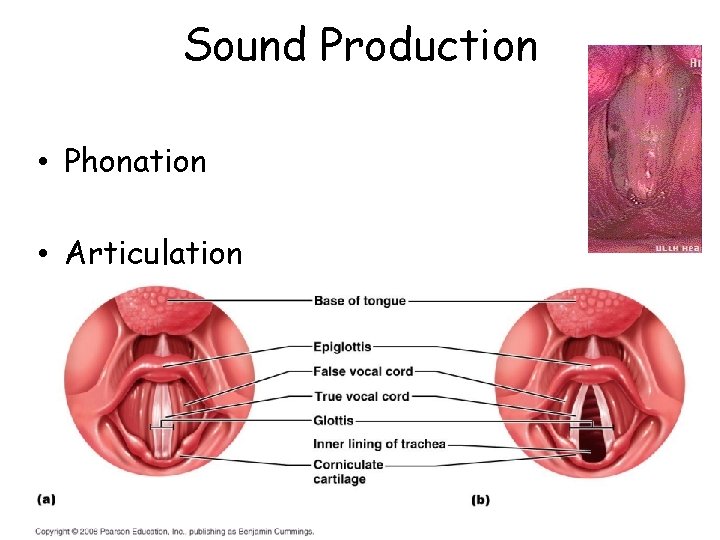
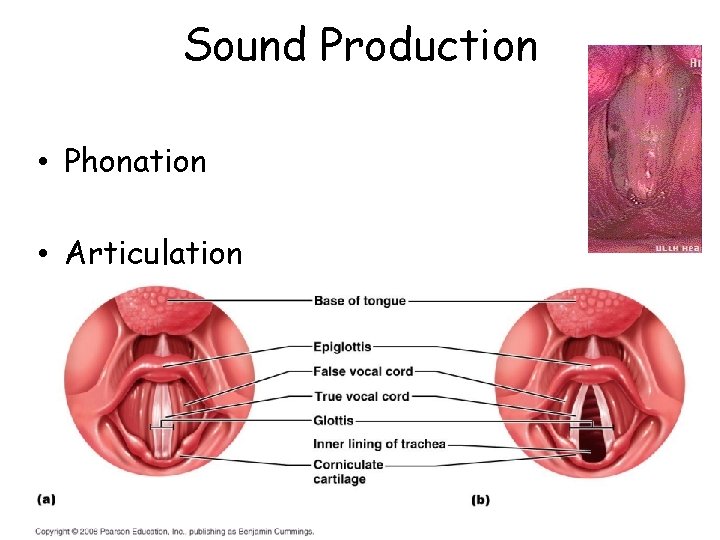
Sound Production • Phonation • Articulation
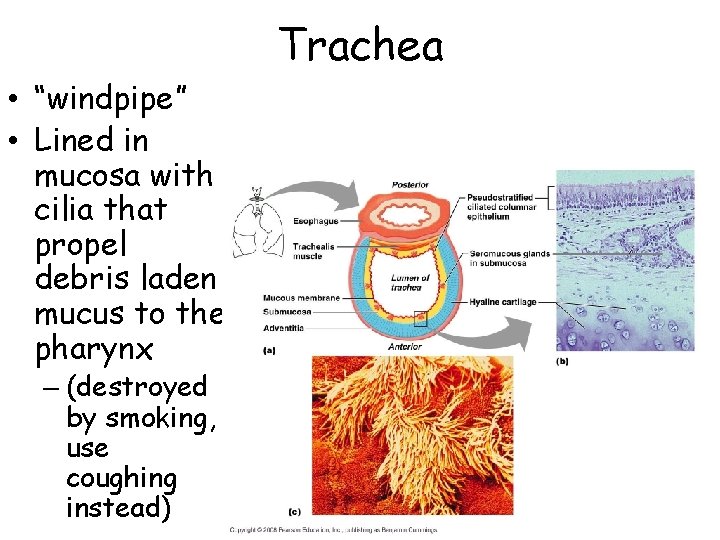
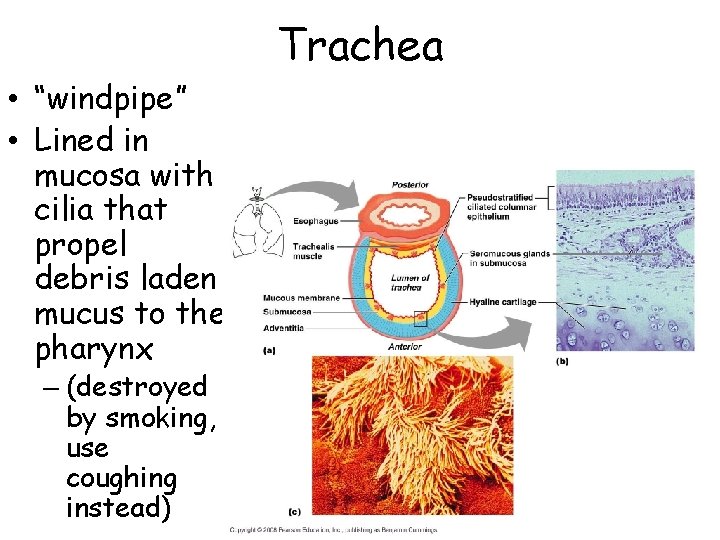
Trachea • “windpipe” • Lined in mucosa with cilia that propel debris laden mucus to the pharynx – (destroyed by smoking, use coughing instead)
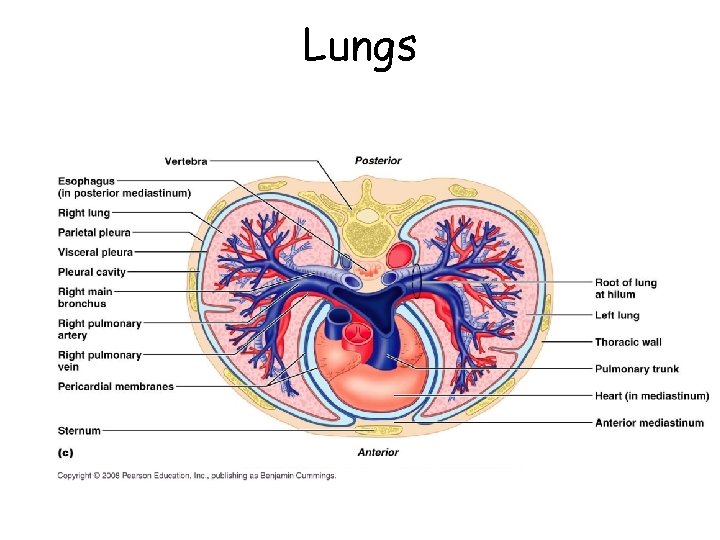
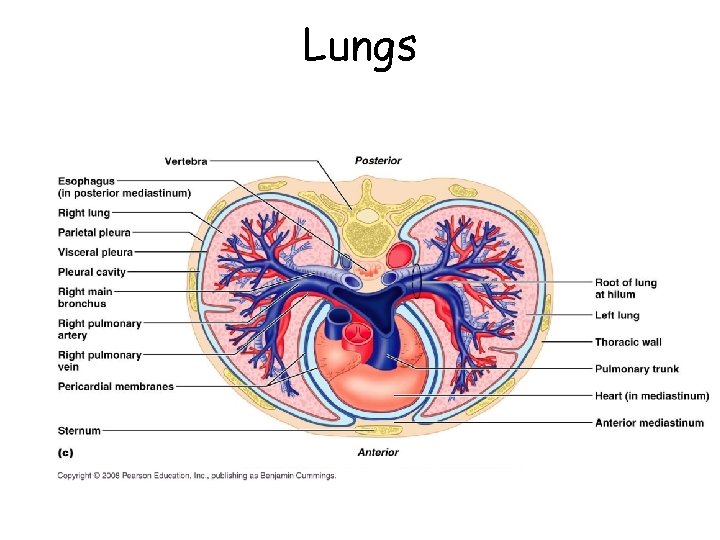
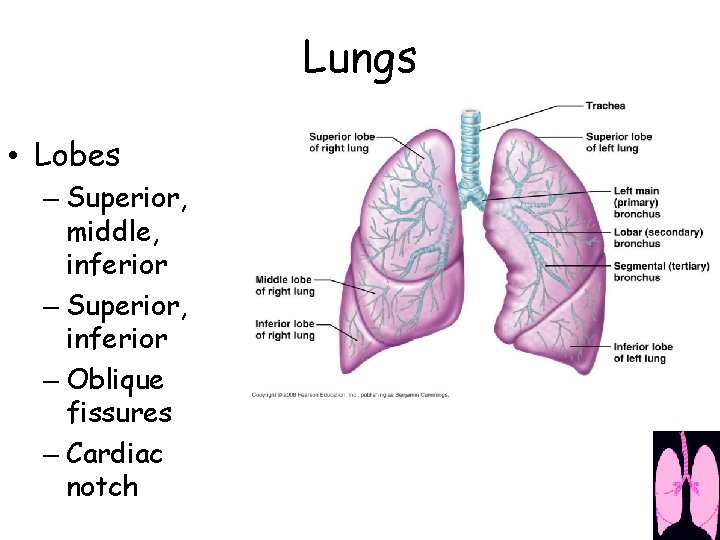
Lungs
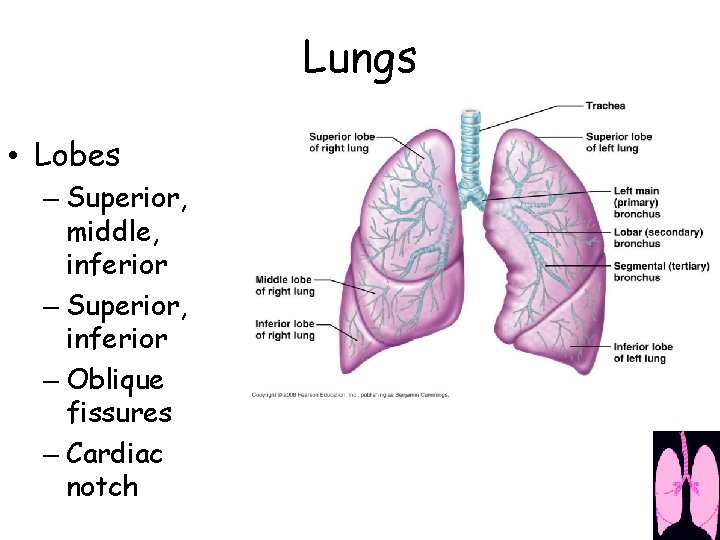
Lungs • Lobes – Superior, middle, inferior – Superior, inferior – Oblique fissures – Cardiac notch
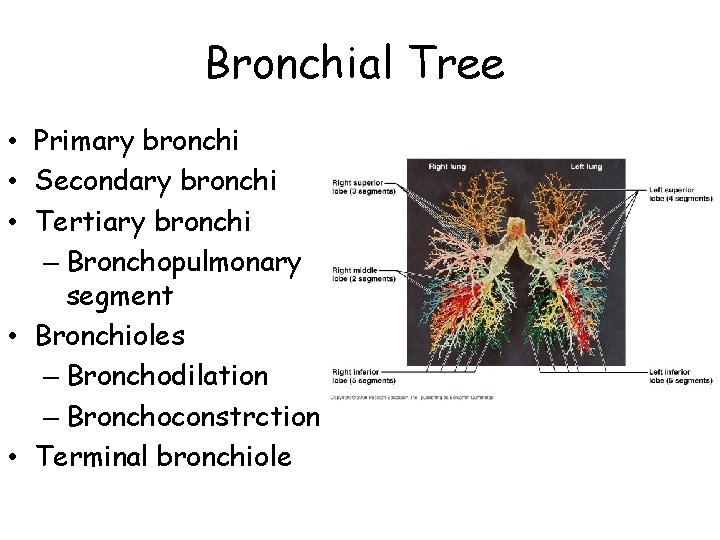
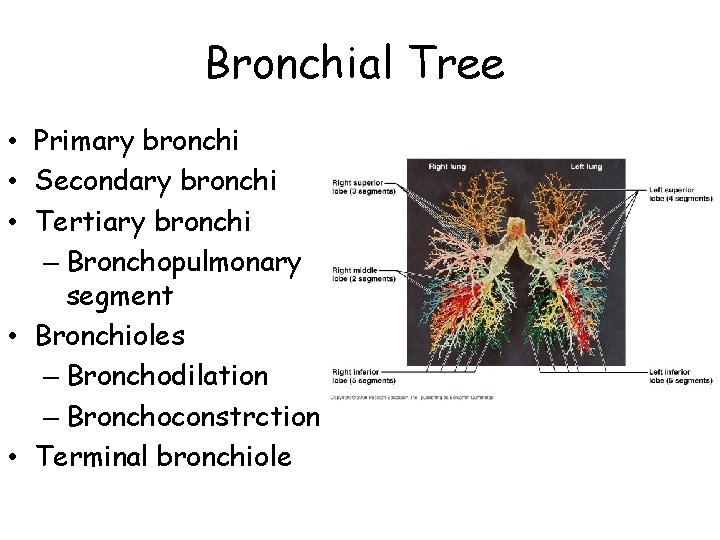
Bronchial Tree • Primary bronchi • Secondary bronchi • Tertiary bronchi – Bronchopulmonary segment • Bronchioles – Bronchodilation – Bronchoconstrction • Terminal bronchiole
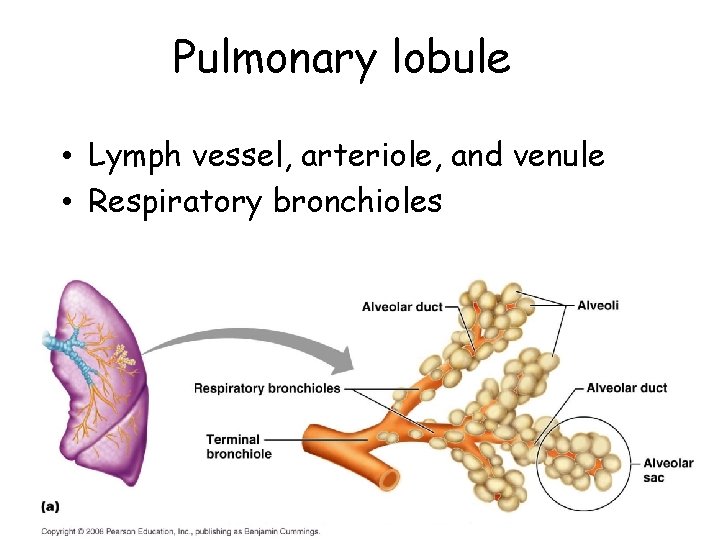
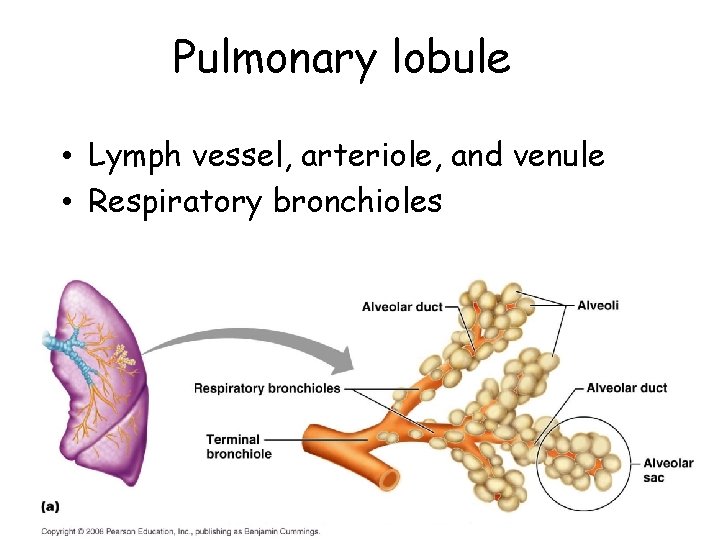
Pulmonary lobule • Lymph vessel, arteriole, and venule • Respiratory bronchioles
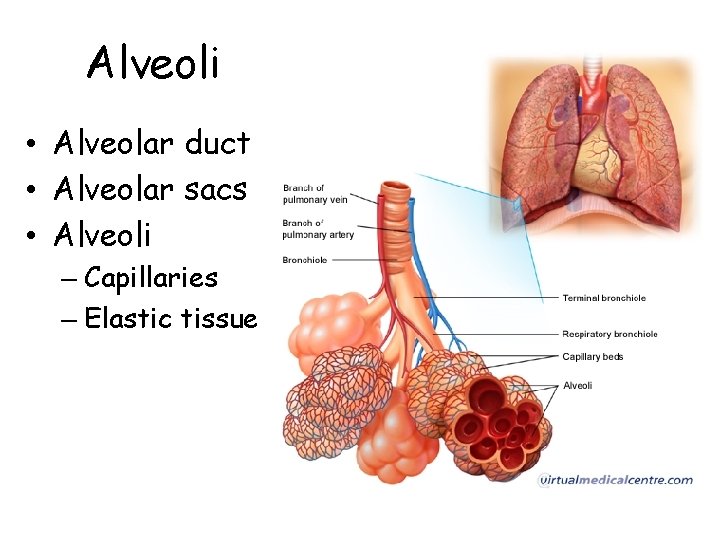
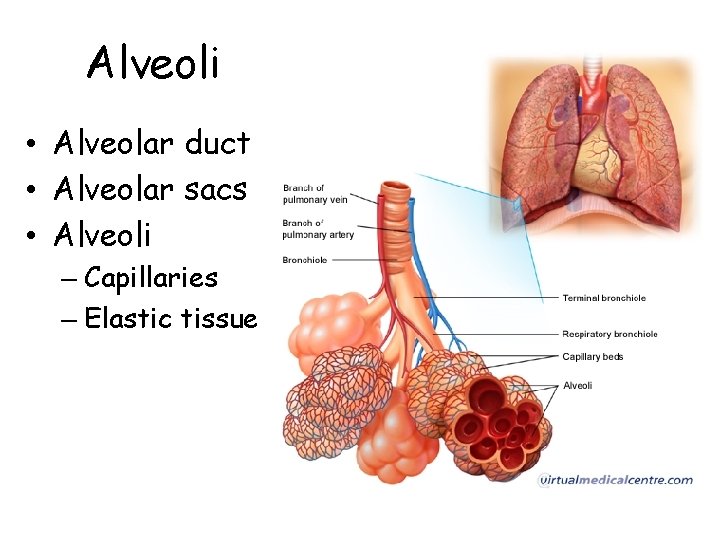
Alveoli • Alveolar duct • Alveolar sacs • Alveoli – Capillaries – Elastic tissue

Alveoli • Type I alveolar cells • Alveolar macrophage • Type II alveolar cells (septal cells) – Surfactant – Surface tension – Respiratory distress syndrome (RDS)
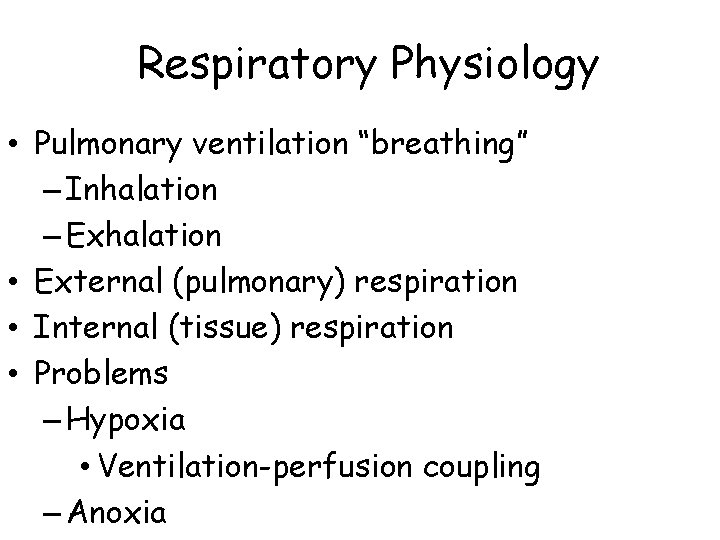
Respiratory Physiology • Pulmonary ventilation “breathing” – Inhalation – Exhalation • External (pulmonary) respiration • Internal (tissue) respiration • Problems – Hypoxia • Ventilation-perfusion coupling – Anoxia
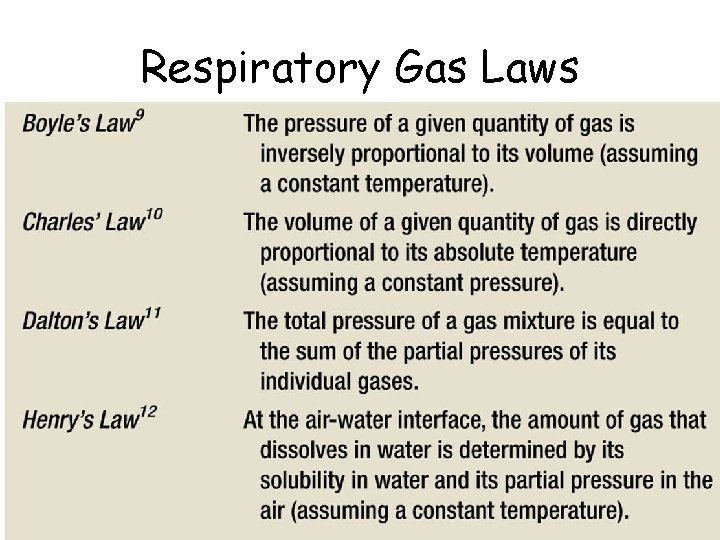
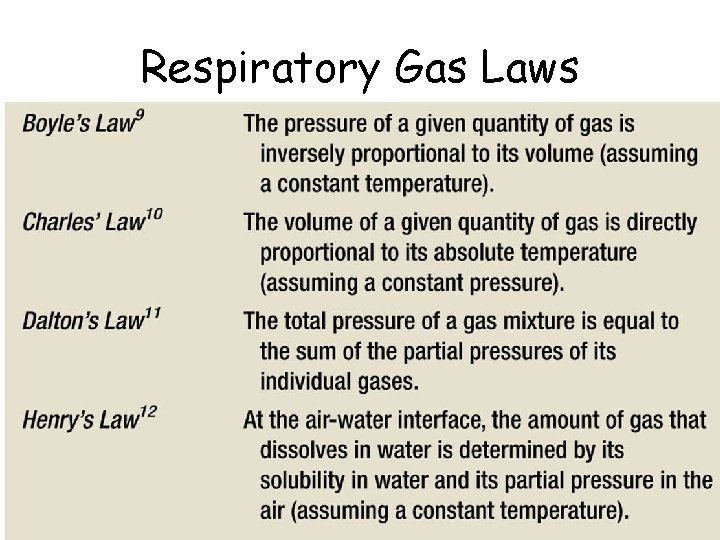
Respiratory Gas Laws
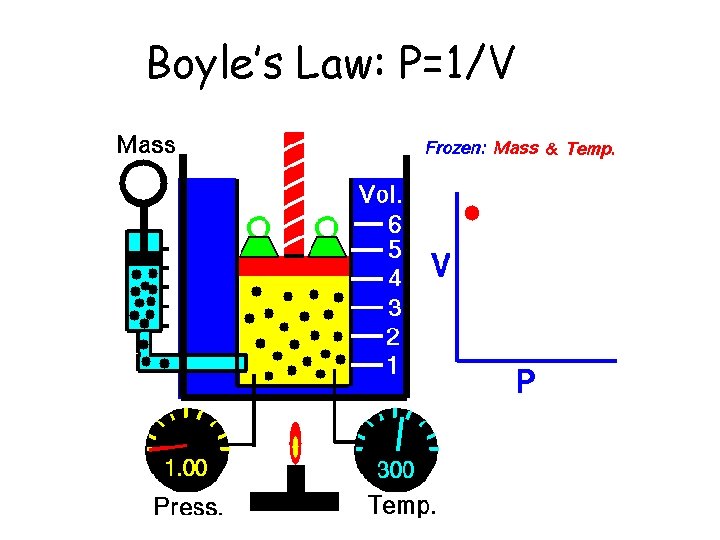
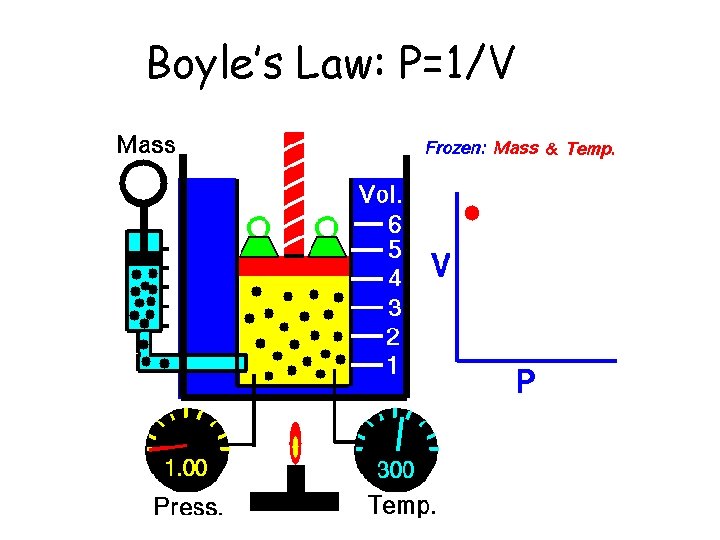
Boyle’s Law: P=1/V
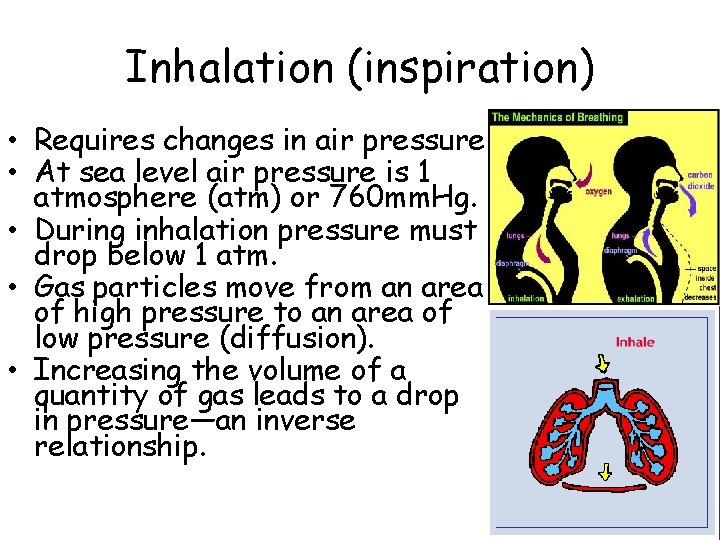
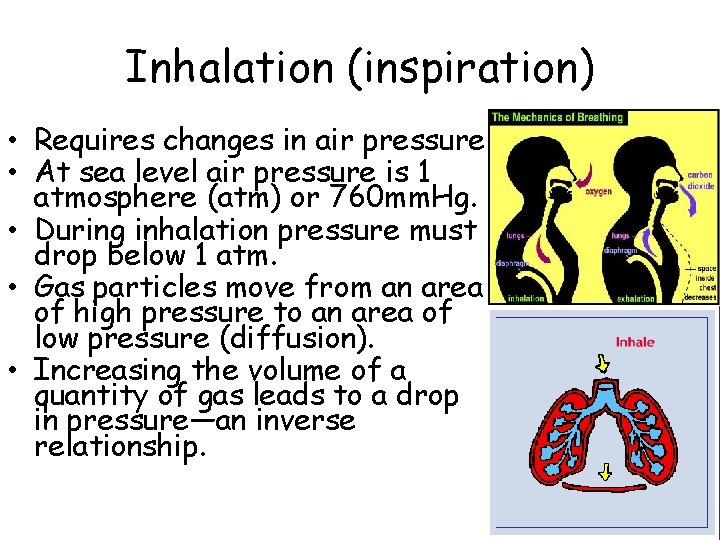
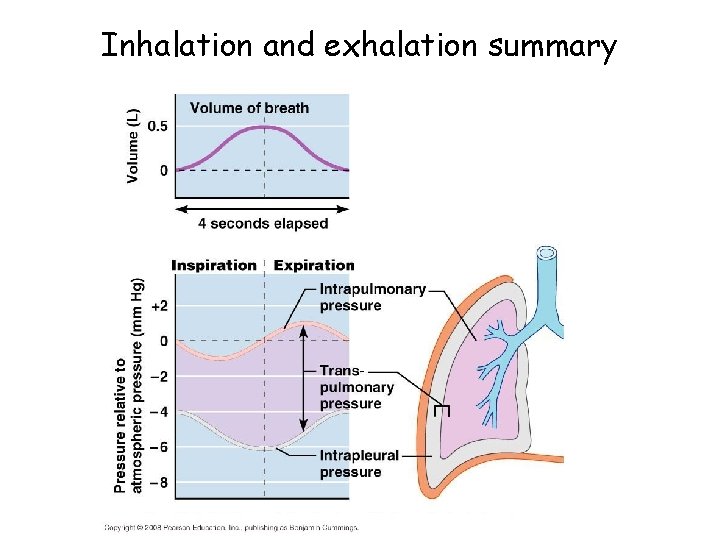
Inhalation (inspiration) • Requires changes in air pressure. • At sea level air pressure is 1 atmosphere (atm) or 760 mm. Hg. • During inhalation pressure must drop below 1 atm. • Gas particles move from an area of high pressure to an area of low pressure (diffusion). • Increasing the volume of a quantity of gas leads to a drop in pressure—an inverse relationship.
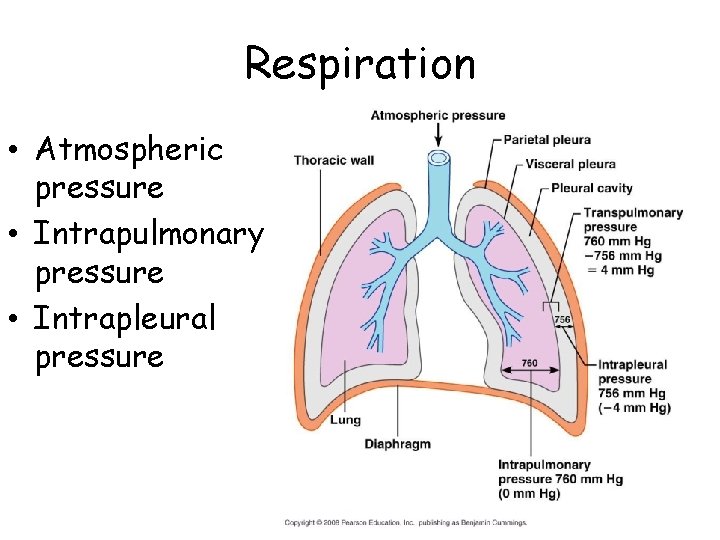
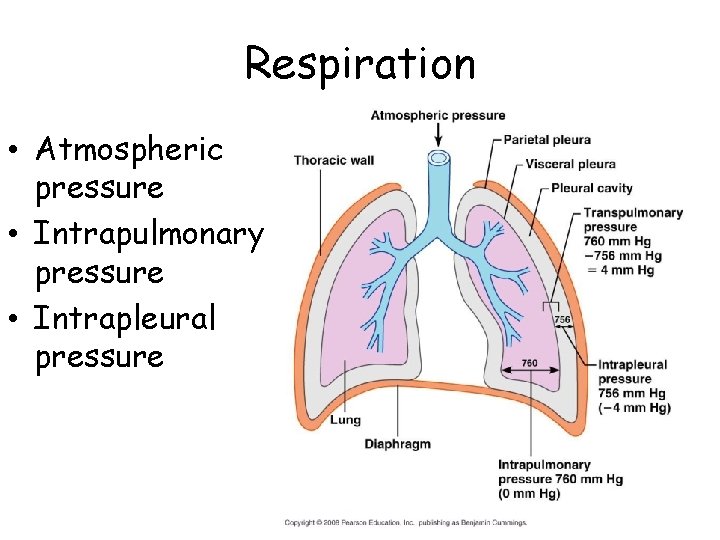
Respiration • Atmospheric pressure • Intrapulmonary pressure • Intrapleural pressure
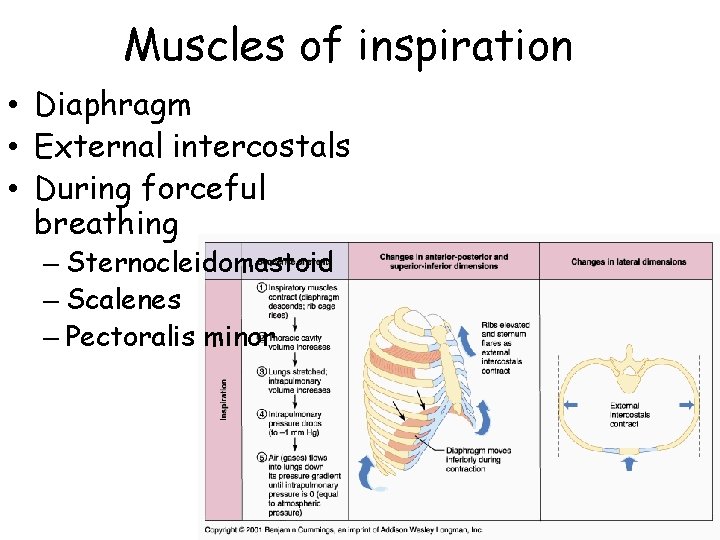
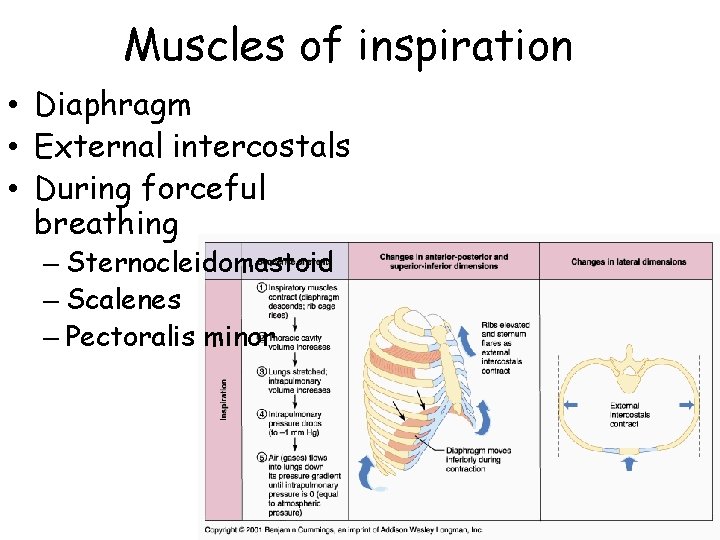
Muscles of inspiration • Diaphragm • External intercostals • During forceful breathing – Sternocleidomastoid – Scalenes – Pectoralis minor
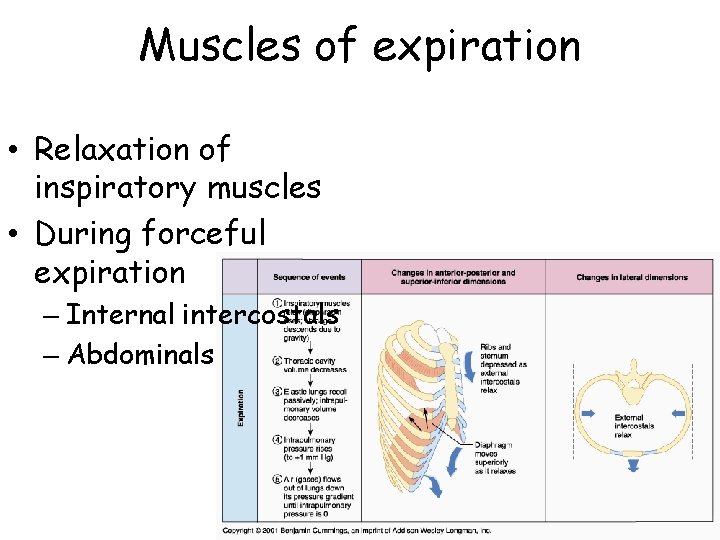
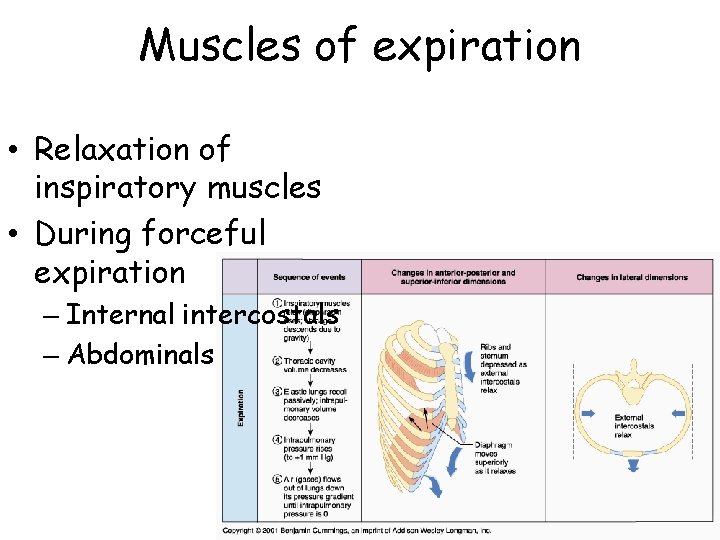
Muscles of expiration • Relaxation of inspiratory muscles • During forceful expiration – Internal intercostals – Abdominals
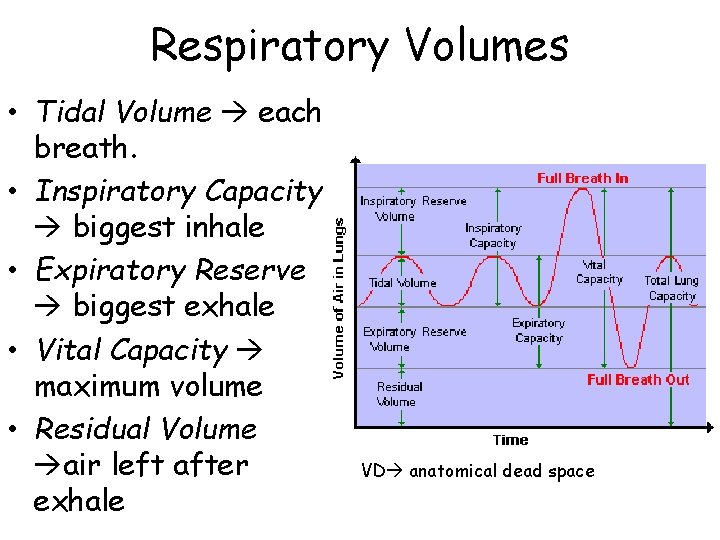
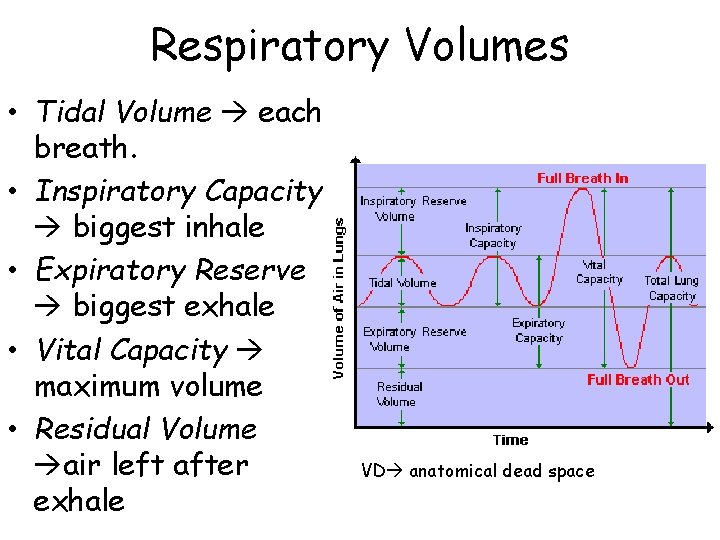
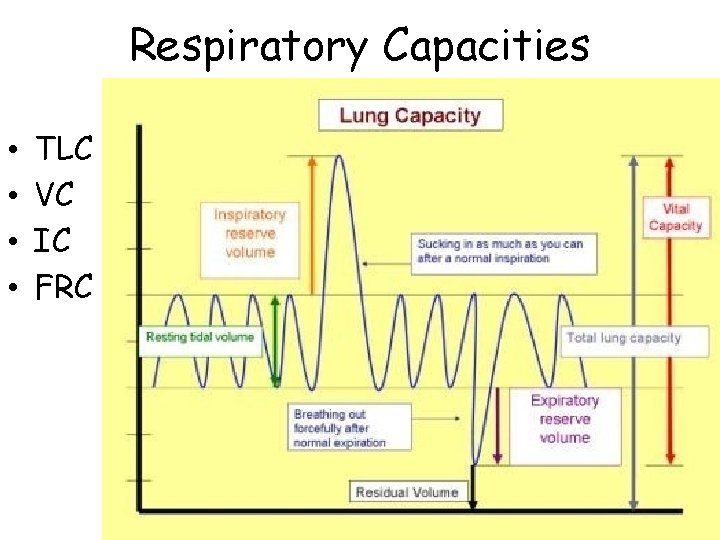
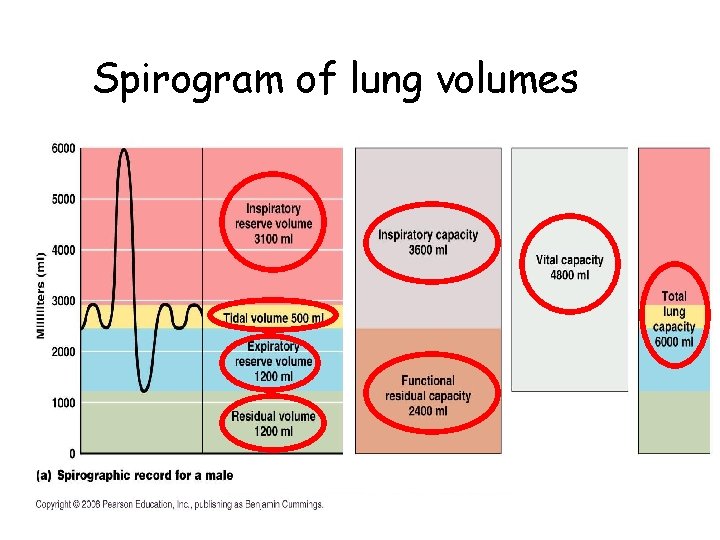
Respiratory Volumes • Tidal Volume each breath. • Inspiratory Capacity biggest inhale • Expiratory Reserve biggest exhale • Vital Capacity maximum volume • Residual Volume air left after exhale VD anatomical dead space
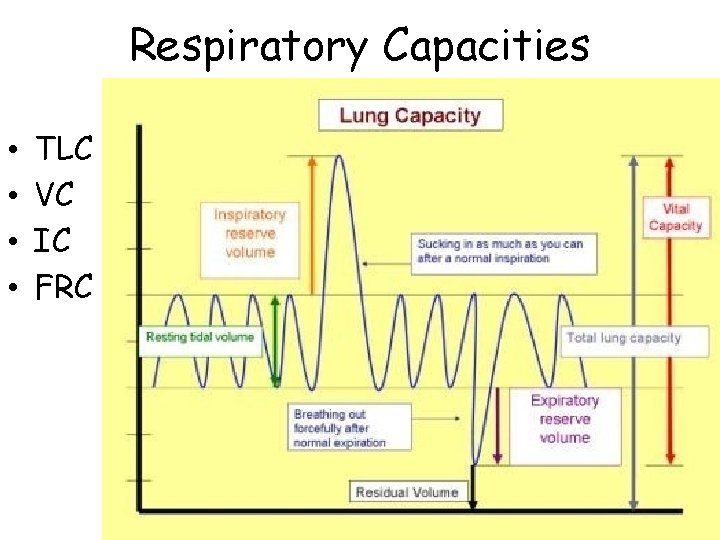
Respiratory Capacities • • TLC VC IC FRC
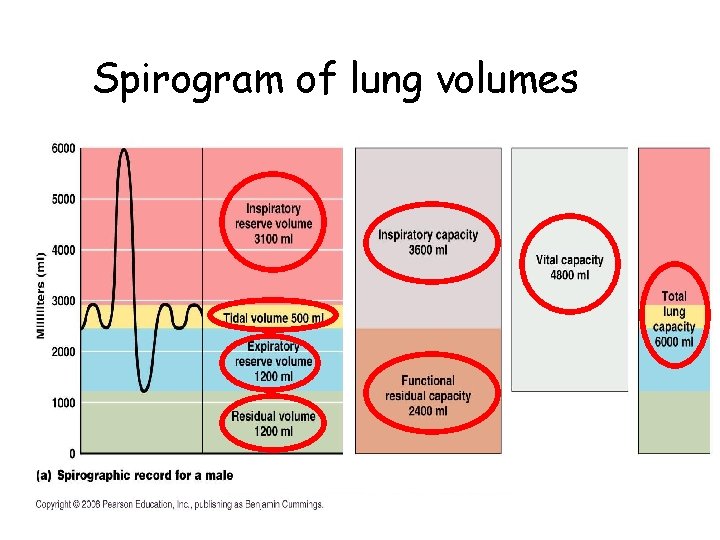
Spirogram of lung volumes
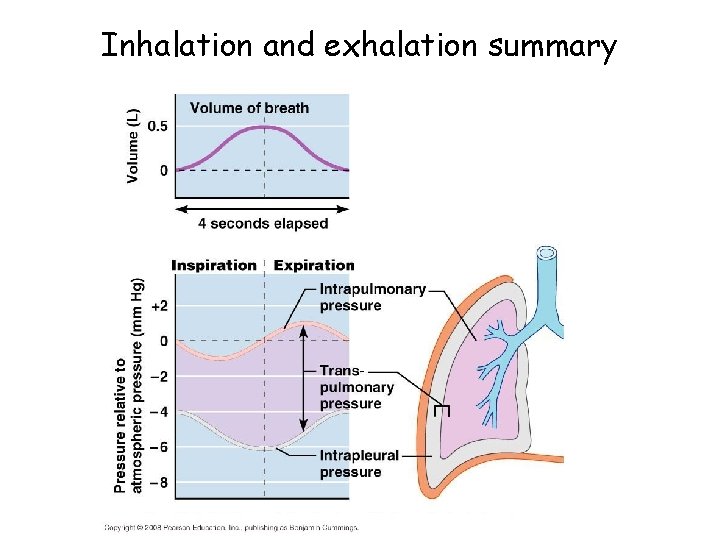
Inhalation and exhalation summary

Other factors affecting ventilation • Compliance – Elasticity – Surface tension – Thoracic mobility • Airway resistance – Airway diameter • Contraction and relaxation of smooth muscles • ANS input • Greatest resistance is in medium bronchi – Obstruction or collapse of airways
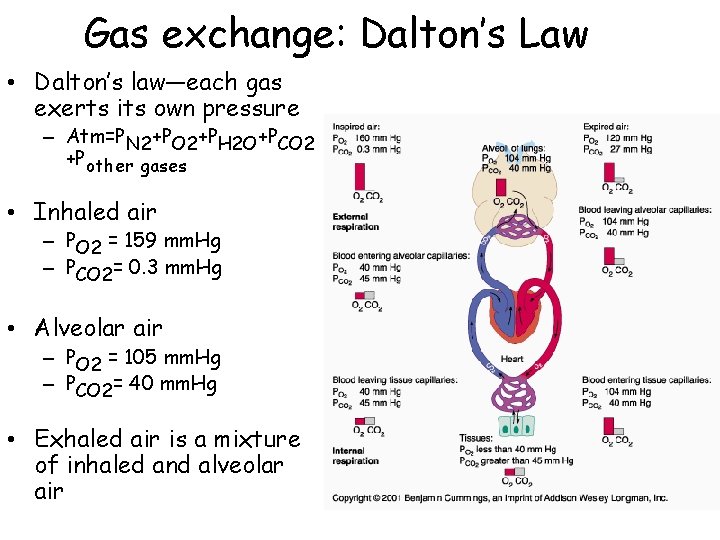
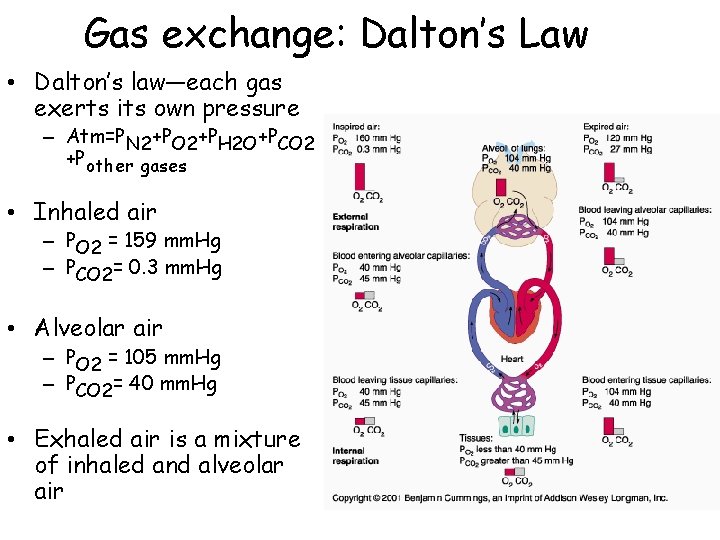
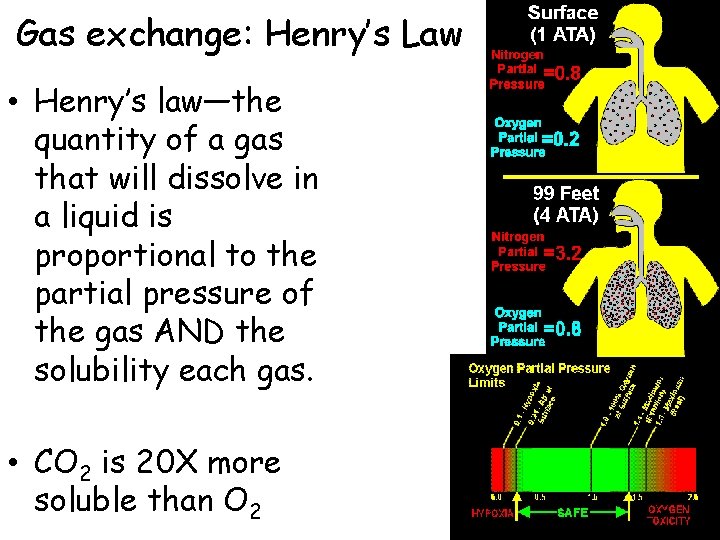
Gas exchange: Dalton’s Law • Dalton’s law—each gas exerts its own pressure – Atm=PN 2+PO 2+PH 2 O+PCO 2 +Pother gases • Inhaled air – PO 2 = 159 mm. Hg – PCO 2= 0. 3 mm. Hg • Alveolar air – PO 2 = 105 mm. Hg – PCO 2= 40 mm. Hg • Exhaled air is a mixture of inhaled and alveolar air
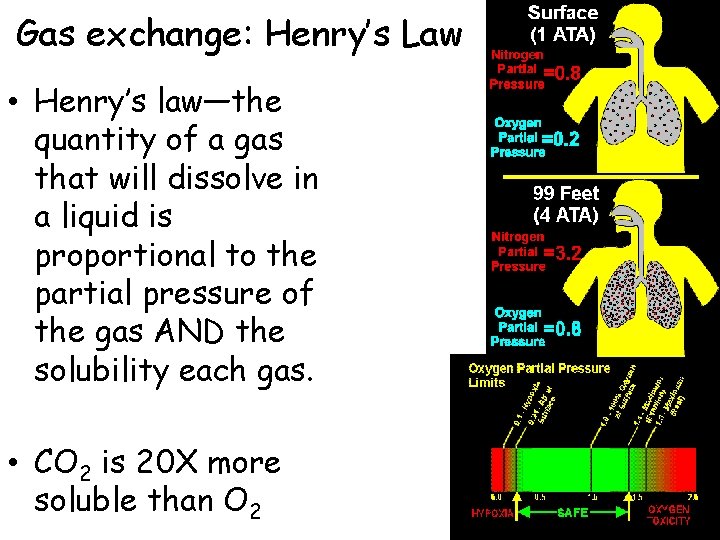
Gas exchange: Henry’s Law • Henry’s law—the quantity of a gas that will dissolve in a liquid is proportional to the partial pressure of the gas AND the solubility each gas. • CO 2 is 20 X more soluble than O 2
Gas Exchange • Partial pressure differences • Small distance • Molecular weight and solubility of gases • Large surface area • Coordinated blood- and airflow

Ventilation-perfusion coupling • Necessary for efficient gas exchange • Ventilation the amount of gas reaching the alveoli • Perfusion blood flow in the capillaries
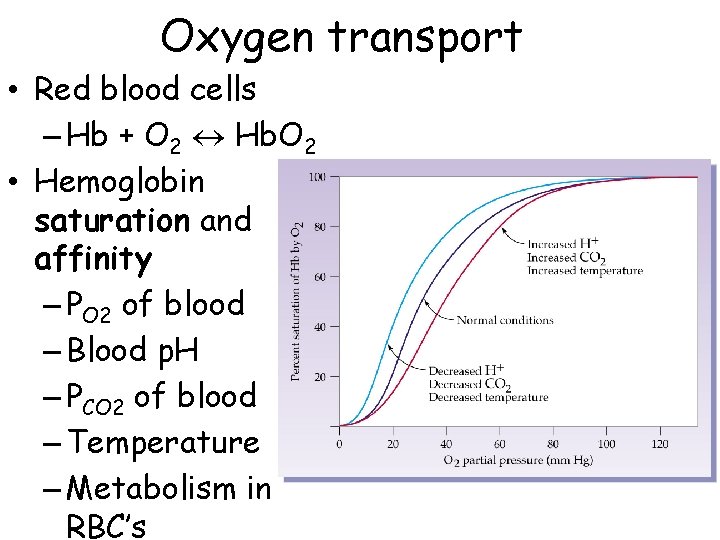
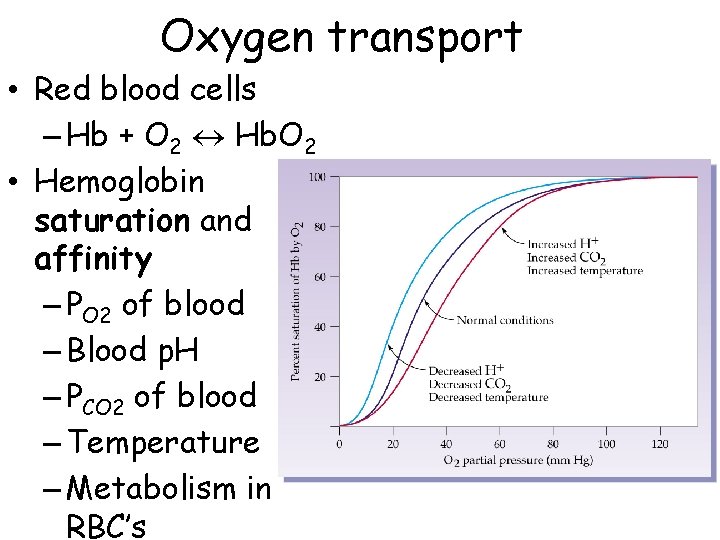
Oxygen transport • Red blood cells – Hb + O 2 « Hb. O 2 • Hemoglobin saturation and affinity – PO 2 of blood – Blood p. H – PCO 2 of blood – Temperature – Metabolism in RBC’s
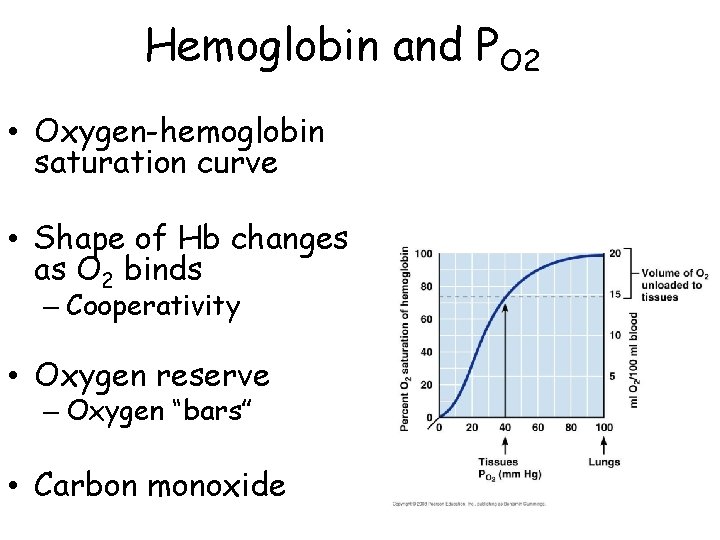
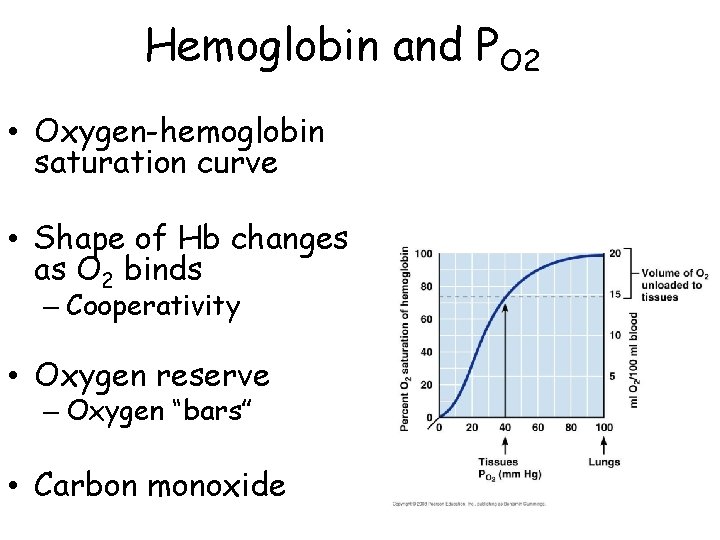
Hemoglobin and PO 2 • Oxygen-hemoglobin saturation curve • Shape of Hb changes as O 2 binds – Cooperativity • Oxygen reserve – Oxygen “bars” • Carbon monoxide
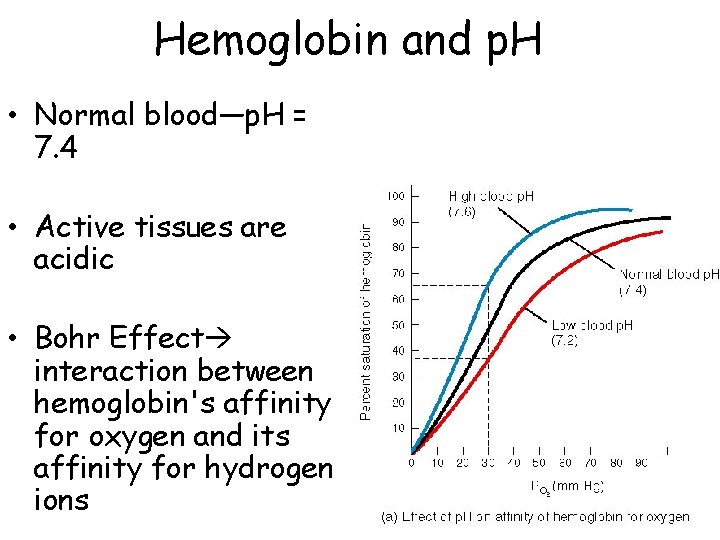
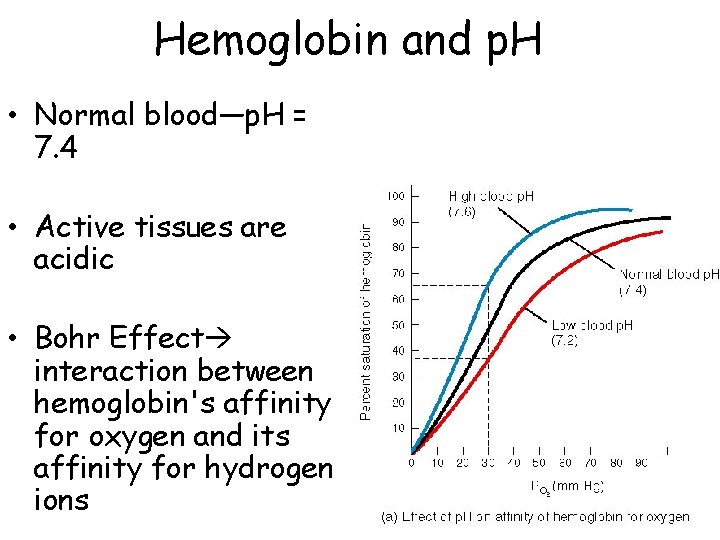
Hemoglobin and p. H • Normal blood—p. H = 7. 4 • Active tissues are acidic • Bohr Effect interaction between hemoglobin's affinity for oxygen and its affinity for hydrogen ions
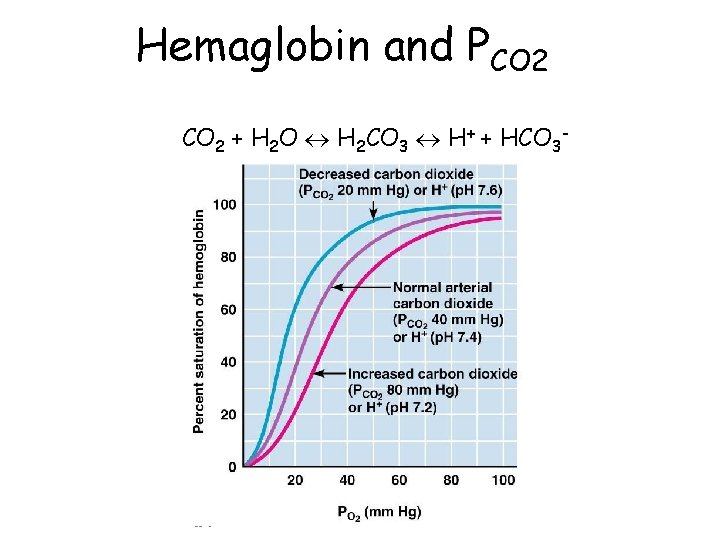
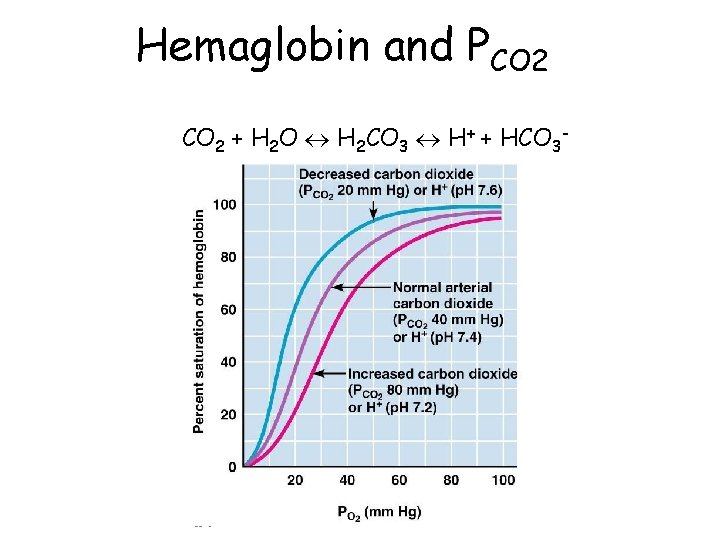
Hemaglobin and PCO 2 + H 2 O « H 2 CO 3 « H+ + HCO 3 -
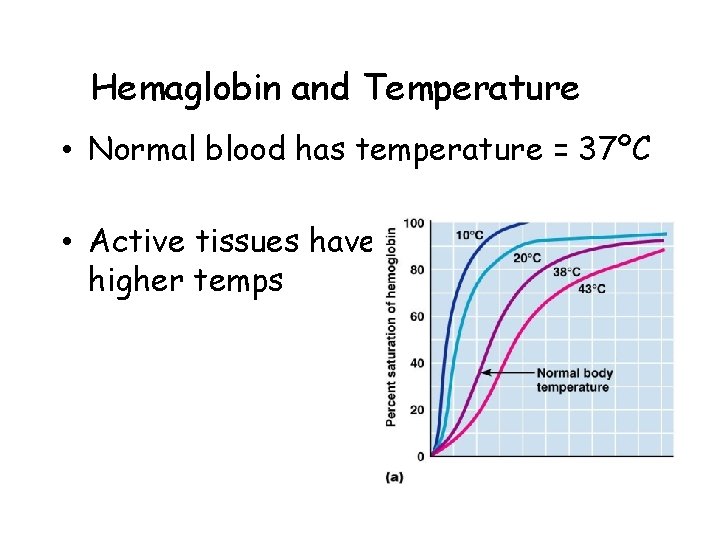
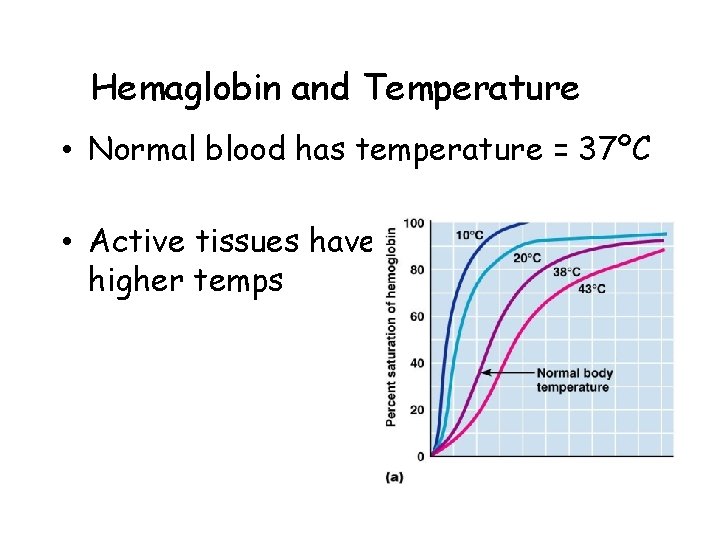
Hemaglobin and Temperature • Normal blood has temperature = 37ºC • Active tissues have higher temps
Hemaglobin and BPG • Biphosphoglycerate (BPG) found in RBCs decreases the affinity of Hb for O 2 • Glycolysis produces lactic acid and BPG • BPG binds reversibly to Hb and is required for Hb to release O 2
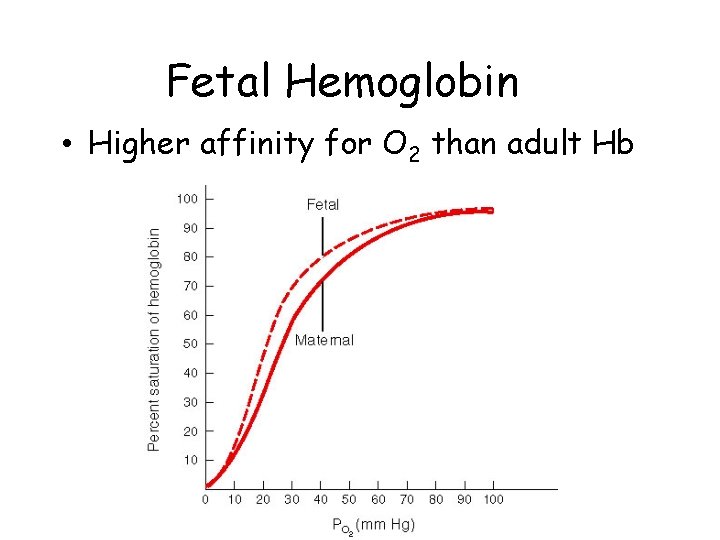
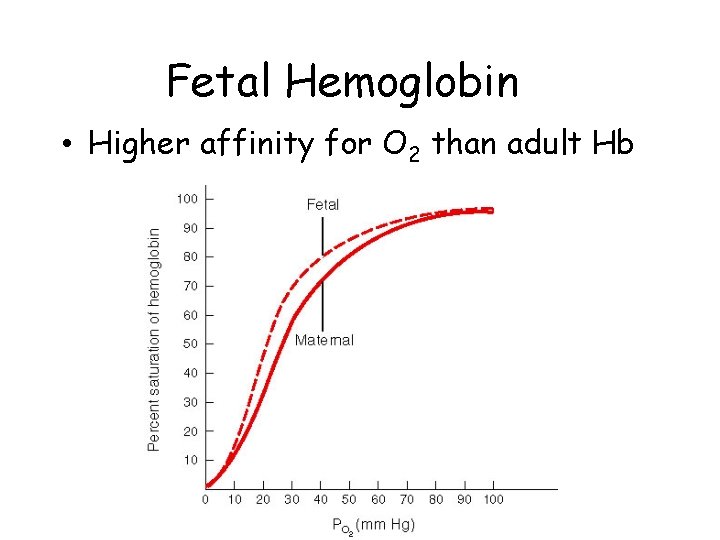
Fetal Hemoglobin • Higher affinity for O 2 than adult Hb
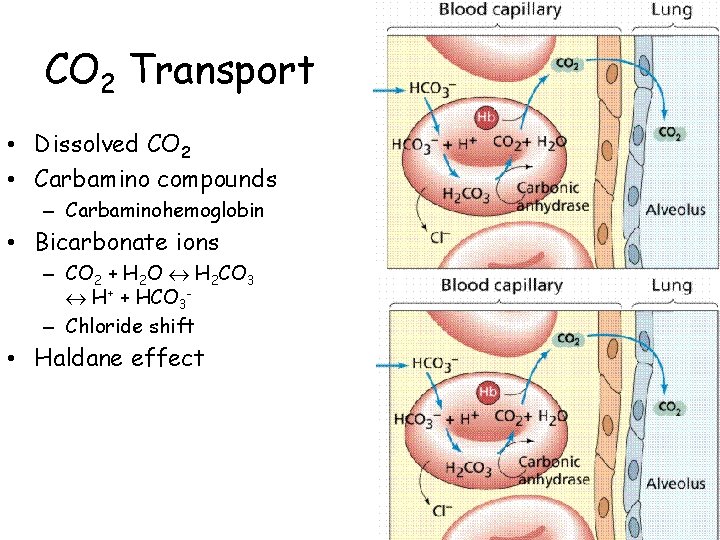
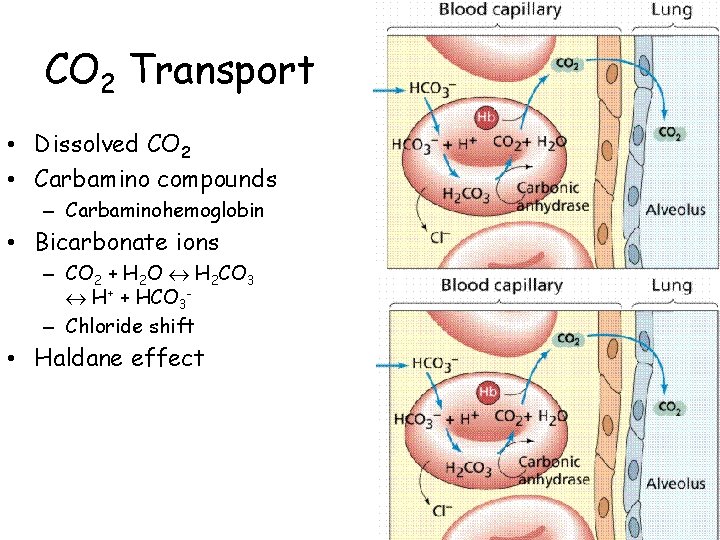
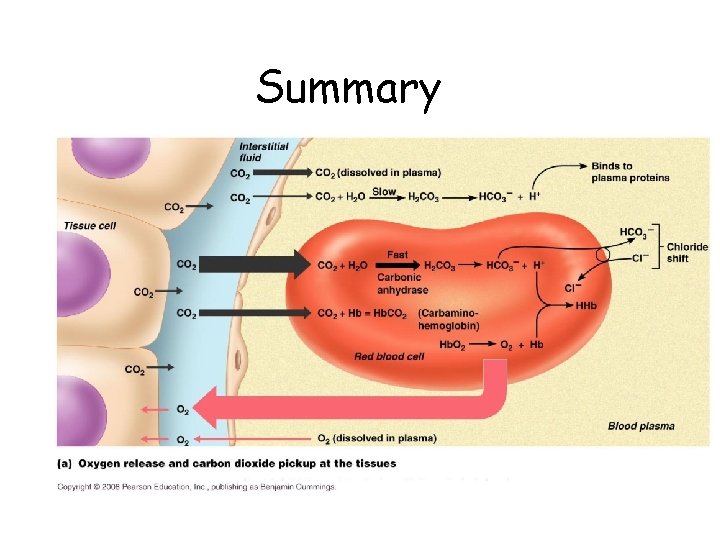
CO 2 Transport • Dissolved CO 2 • Carbamino compounds – Carbaminohemoglobin • Bicarbonate ions – CO 2 + H 2 O « H 2 CO 3 « H+ + HCO 3– Chloride shift • Haldane effect
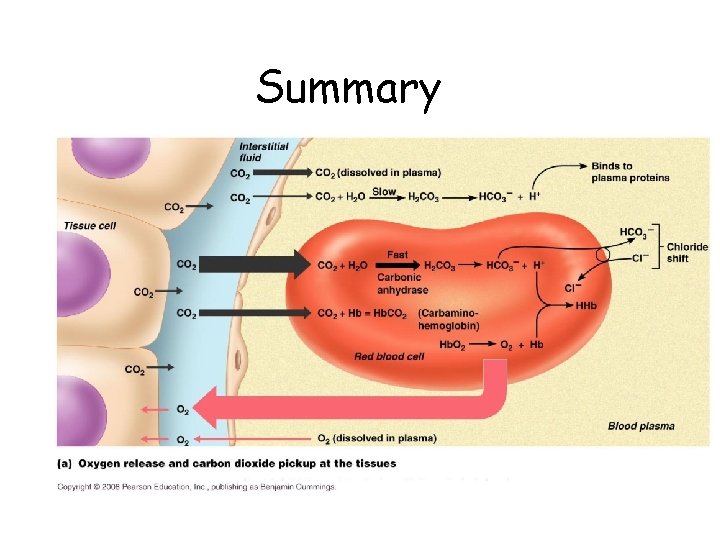
Summary
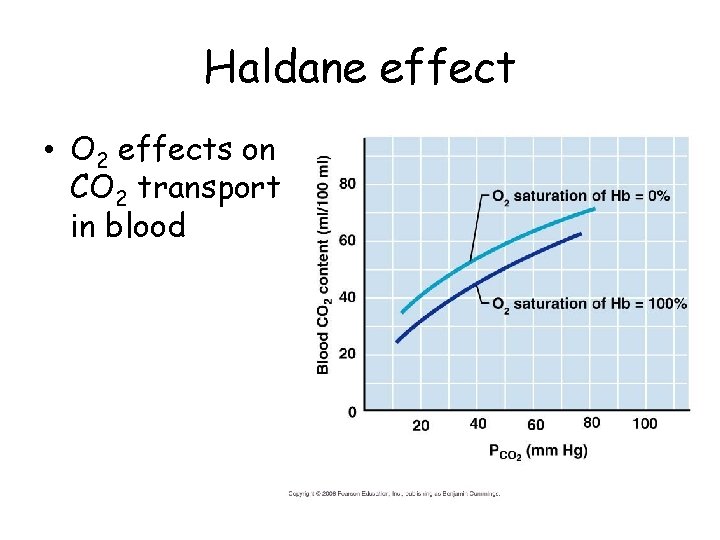
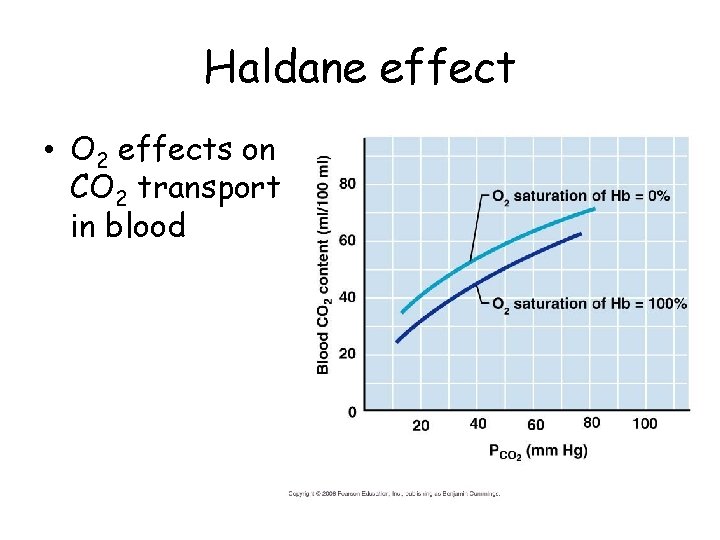
Haldane effect • O 2 effects on CO 2 transport in blood
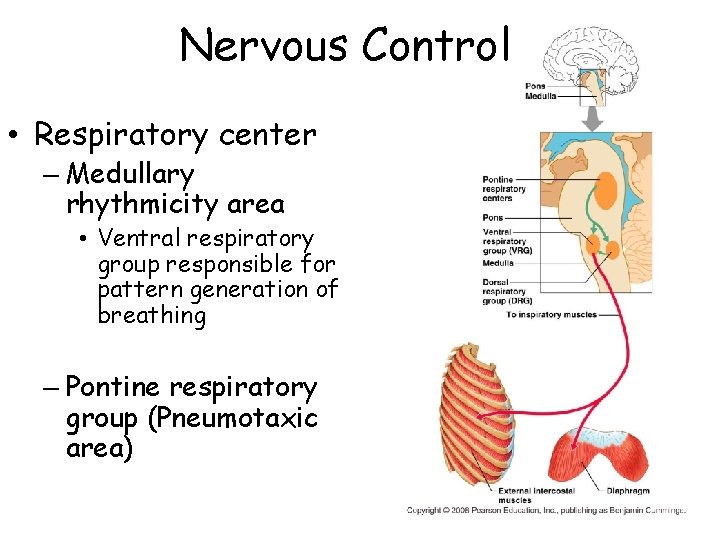
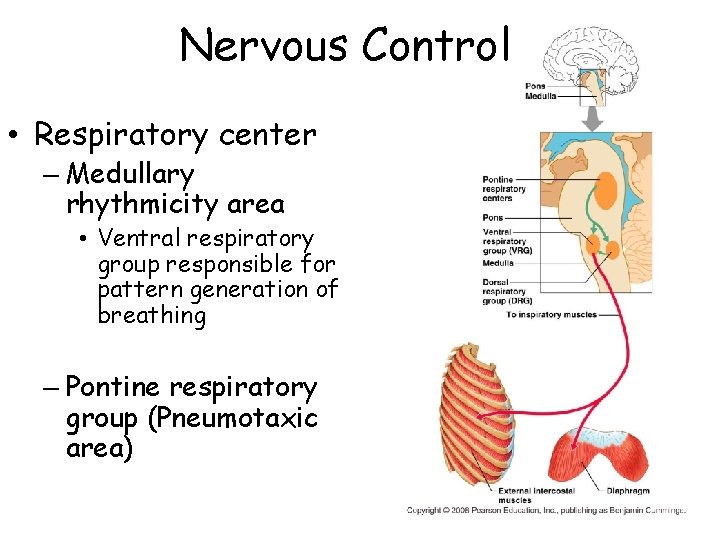
Nervous Control • Respiratory center – Medullary rhythmicity area • Ventral respiratory group responsible for pattern generation of breathing – Pontine respiratory group (Pneumotaxic area)
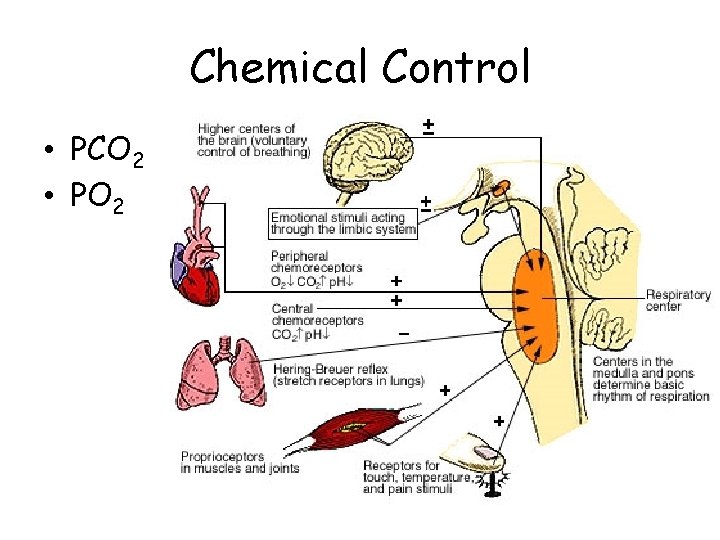
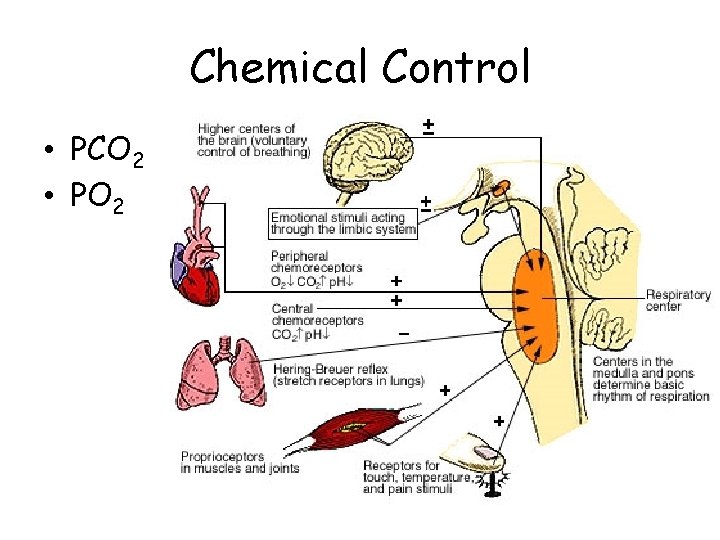
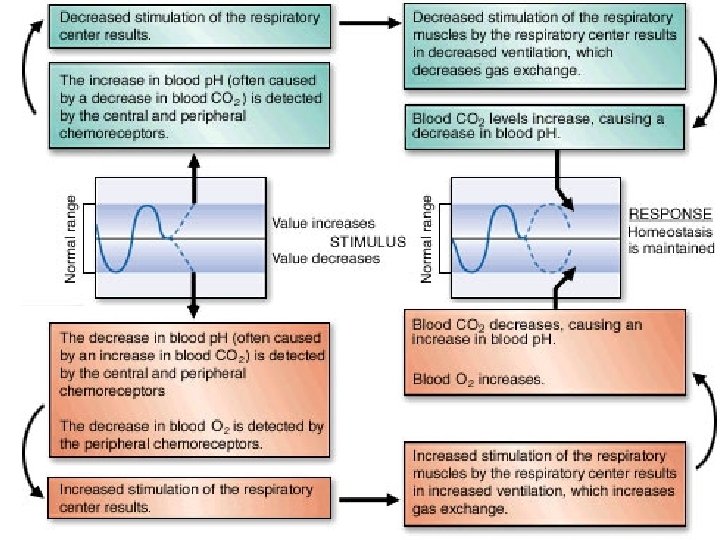
Chemical Control • PCO 2 • PO 2
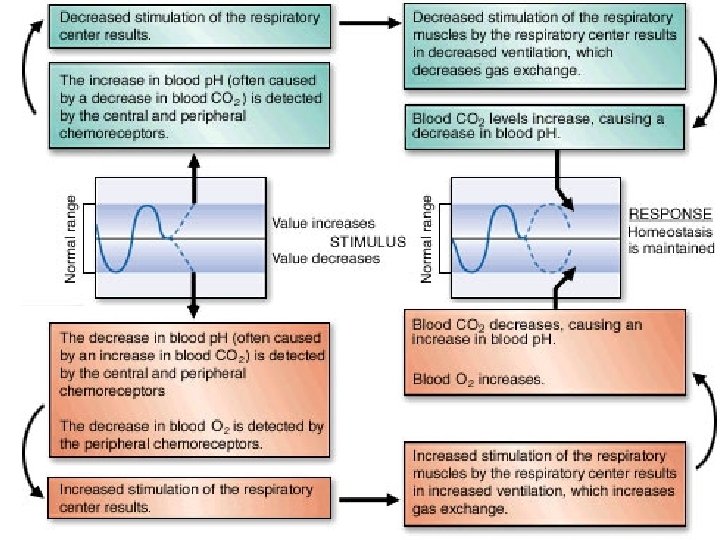
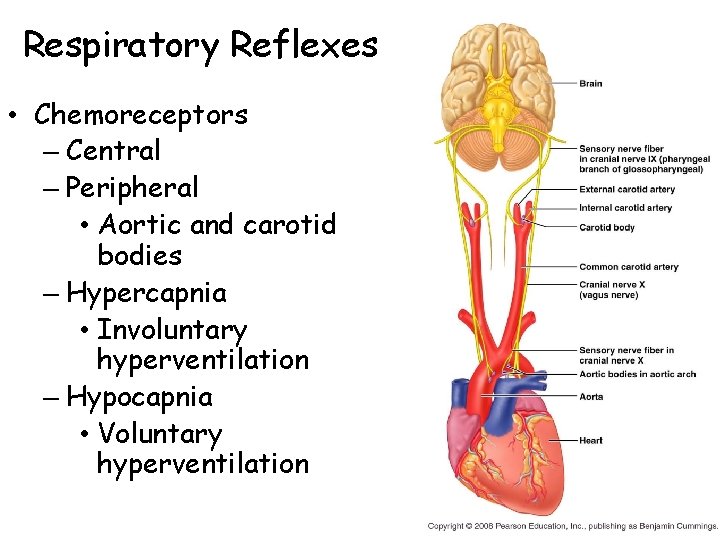
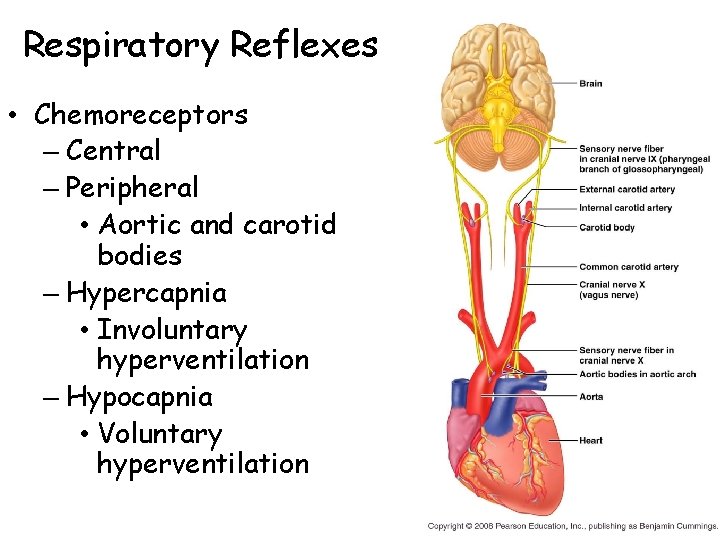
Respiratory Reflexes • Chemoreceptors – Central – Peripheral • Aortic and carotid bodies – Hypercapnia • Involuntary hyperventilation – Hypocapnia • Voluntary hyperventilation
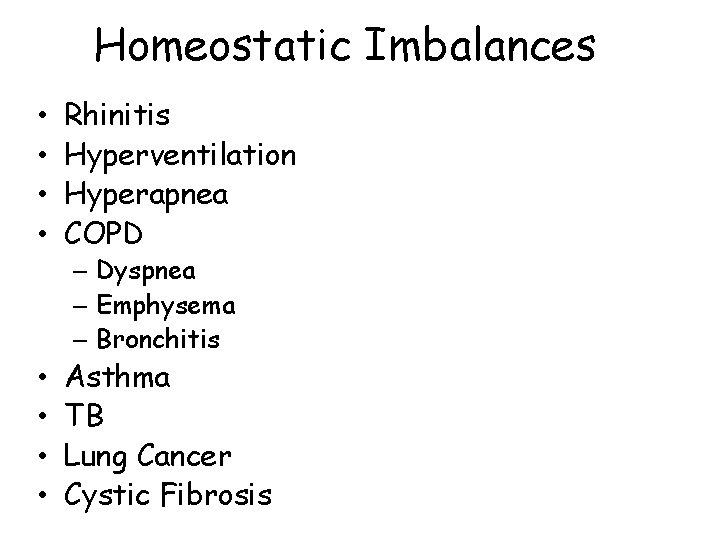
Homeostatic Imbalances • • Rhinitis Hyperventilation Hyperapnea COPD – Dyspnea – Emphysema – Bronchitis • • Asthma TB Lung Cancer Cystic Fibrosis
Resources • Interactive Respiratory Physiology • Function of the Respiratory System