The Respiratory System I Muse Bio 2440 lab
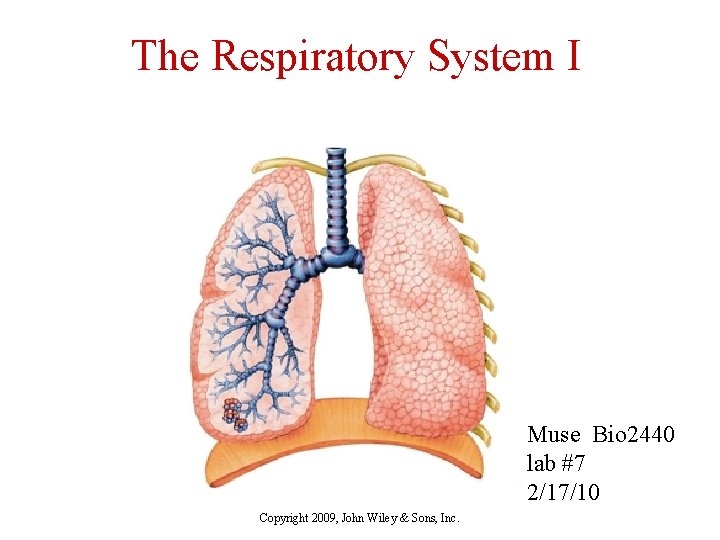
The Respiratory System I Muse Bio 2440 lab #7 2/17/10 Copyright 2009, John Wiley & Sons, Inc.

Activities: ventilation vs. respiration. Respiration and oxygen debt. Spirometer - tidal volume, vital capacity, inspiratory reserve. CO 2 flush - O 2 effect p. H and CO 2 Cat lung inflation Copyright 2009, John Wiley & Sons, Inc.
Components of the Respiratory System n Five Functions of the Respiratory System q q q Provides extensive gas exchange surface area between air and circulating blood Moves air to and from exchange surfaces of lungs Protects respiratory surfaces from outside environment Produces sounds Participates in olfactory sense Copyright 2009, John Wiley & Sons, Inc.
Respiratory System Anatomy n Structurally q Upper respiratory system n q Lower respiratory system n n Nose, pharynx and associated structures Larynx, trachea, bronchi and lungs Functionally q Conducting zone – conducts air to lungs n q Nose, pharynx, larynx, trachea, bronchioles and terminal bronchioles Respiratory zone – main site of gas exchange n Respiratory bronchioles, alveolar ducts, alveolar sacs, and alveoli Copyright 2009, John Wiley & Sons, Inc.
Components of the Respiratory System n Organization of the Respiratory System q The respiratory system is divided into n n Upper respiratory system: above the larynx Lower respiratory system: below the larynx Copyright 2009, John Wiley & Sons, Inc.
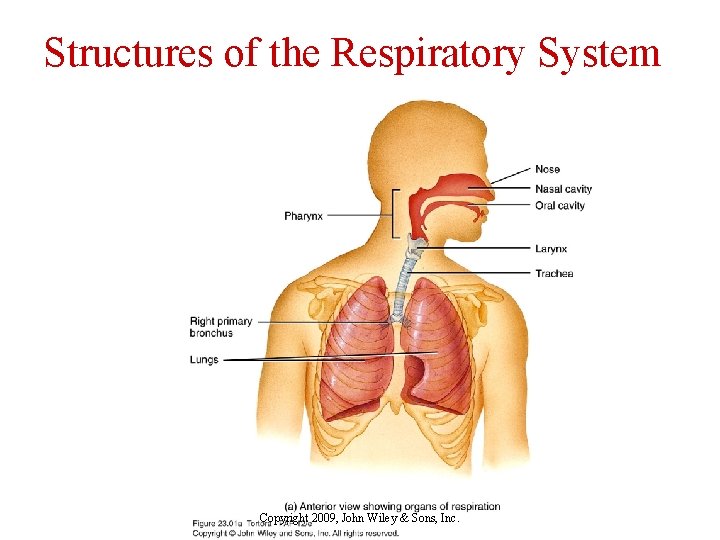
Structures of the Respiratory System Copyright 2009, John Wiley & Sons, Inc.
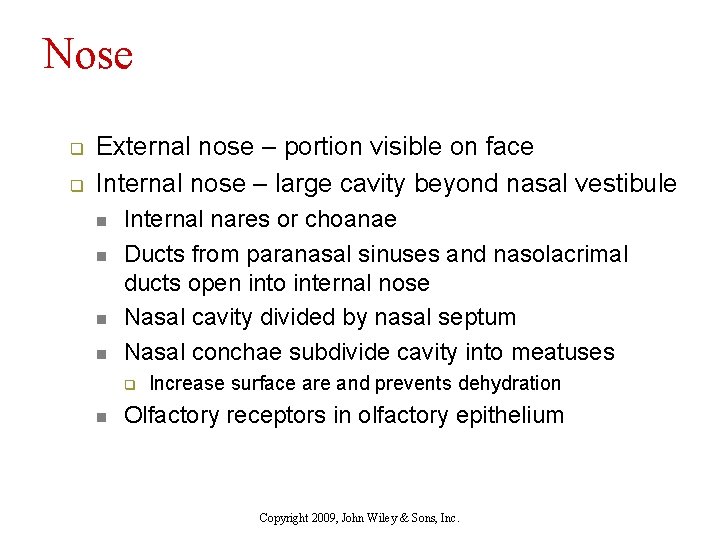
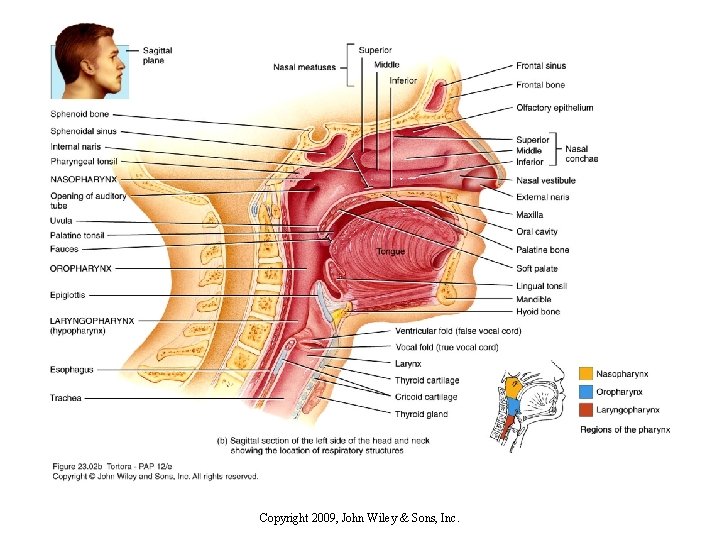
Nose q q External nose – portion visible on face Internal nose – large cavity beyond nasal vestibule n n Internal nares or choanae Ducts from paranasal sinuses and nasolacrimal ducts open into internal nose Nasal cavity divided by nasal septum Nasal conchae subdivide cavity into meatuses q n Increase surface are and prevents dehydration Olfactory receptors in olfactory epithelium Copyright 2009, John Wiley & Sons, Inc.
Copyright 2009, John Wiley & Sons, Inc.
Nasal Cavity n Superior, middle, and inferior nasal conchae q q q Protrude from the lateral walls Increase mucosal area Enhance air turbulence Copyright 2009, John Wiley & Sons, Inc.
Pharynx q q q Starts at internal nares and extends to cricoid cartilage of larynx Contraction of skeletal muscles assists in deglutition Functions n n n q Passageway for air and food Resonating chamber Houses tonsils 3 anatomical regions n n n Nasopharynx Oropharynx Laryngopharynx Copyright 2009, John Wiley & Sons, Inc.
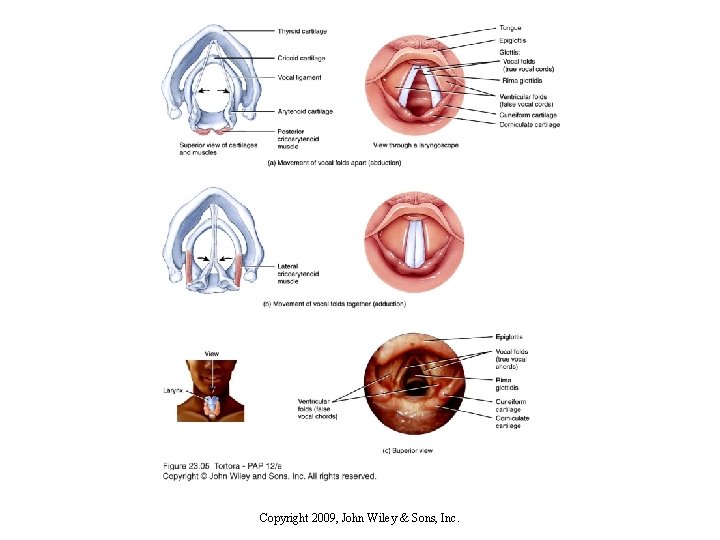
Larynx q q Short passageway connecting laryngopharynx with trachea Composed of 9 pieces of cartilage n n q q Thyroid cartilage or Adam’s apple Cricoid cartilage hallmark for tracheotomy Epiglottis closes off glottis during swallowing Glottis – pair of folds of mucous membranes, vocal folds (true vocal cords, and rima glottidis (space) Cilia in upper respiratory tract move mucous and trapped particles down toward pharynx Cilia in lower respiratory tract move them up toward pharynx Copyright 2009, John Wiley & Sons, Inc.
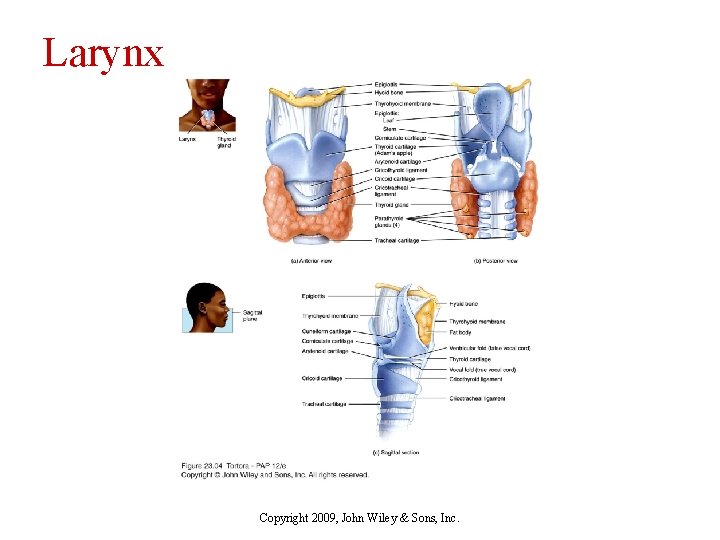
Larynx Copyright 2009, John Wiley & Sons, Inc.
Structures of Voice Production q Mucous membrane of larynx forms n Ventricular folds (false vocal cords) – superior pair q n Vocal folds (true vocal cords) – inferior pair q q q n Function in holding breath against pressure in thoracic cavity Muscle contraction pulls elastic ligaments which stretch vocal folds out into airway Vibrate and produce sound with air Folds can move apart or together, elongate or shorten, tighter or looser Androgens make folds thicker and longer – slower vibration and lower pitch Copyright 2009, John Wiley & Sons, Inc.
Copyright 2009, John Wiley & Sons, Inc.
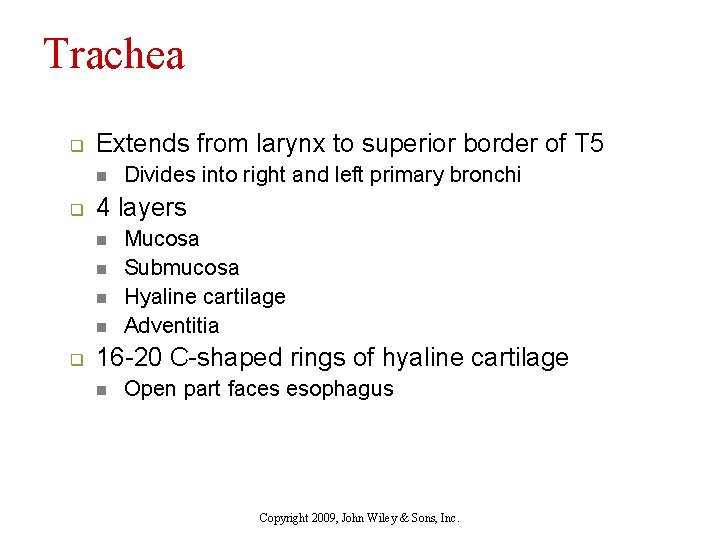
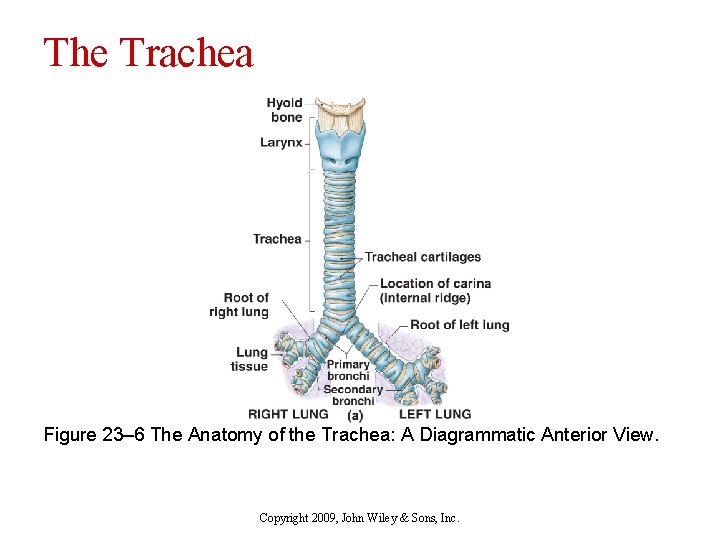
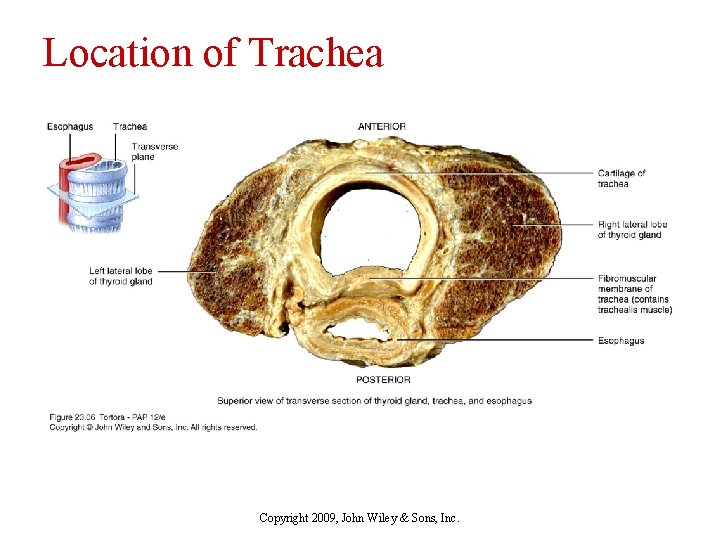
Trachea q Extends from larynx to superior border of T 5 n q 4 layers n n q Divides into right and left primary bronchi Mucosa Submucosa Hyaline cartilage Adventitia 16 -20 C-shaped rings of hyaline cartilage n Open part faces esophagus Copyright 2009, John Wiley & Sons, Inc.
The Trachea Figure 23– 6 The Anatomy of the Trachea: A Diagrammatic Anterior View. Copyright 2009, John Wiley & Sons, Inc.
Location of Trachea Copyright 2009, John Wiley & Sons, Inc.
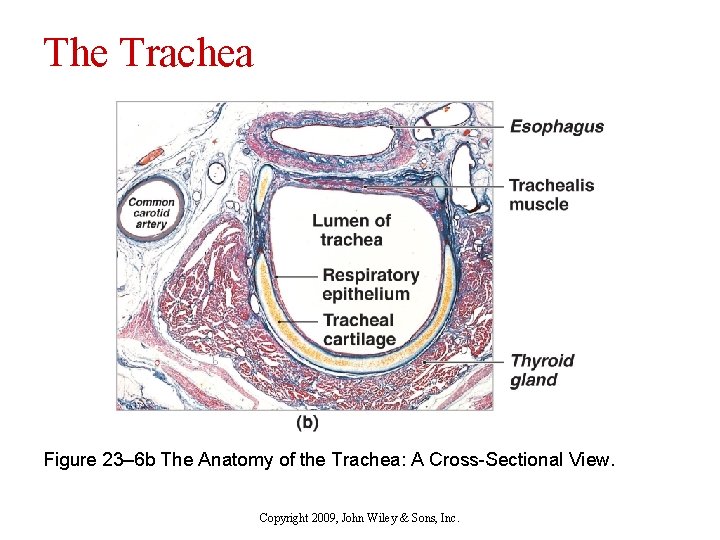
The Trachea Figure 23– 6 b The Anatomy of the Trachea: A Cross-Sectional View. Copyright 2009, John Wiley & Sons, Inc.
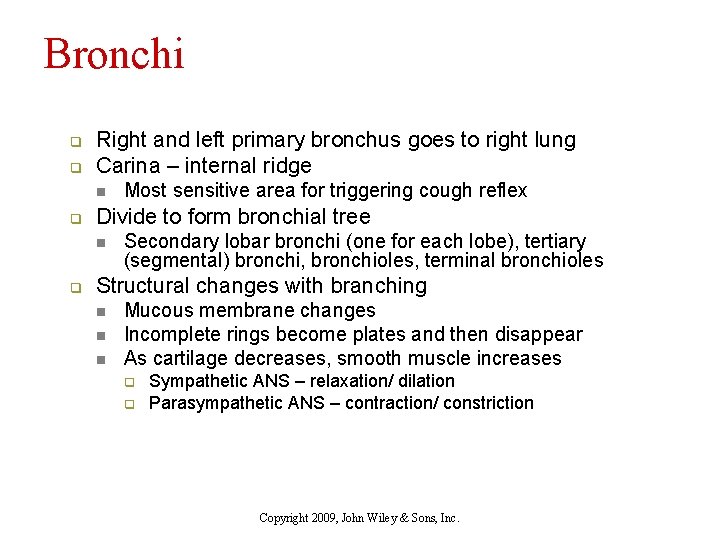
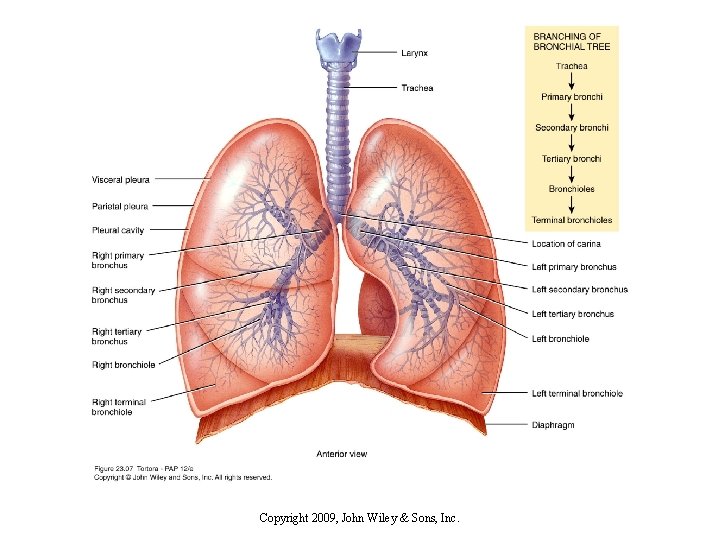
Bronchi q q Right and left primary bronchus goes to right lung Carina – internal ridge n q Divide to form bronchial tree n q Most sensitive area for triggering cough reflex Secondary lobar bronchi (one for each lobe), tertiary (segmental) bronchi, bronchioles, terminal bronchioles Structural changes with branching n n n Mucous membrane changes Incomplete rings become plates and then disappear As cartilage decreases, smooth muscle increases q q Sympathetic ANS – relaxation/ dilation Parasympathetic ANS – contraction/ constriction Copyright 2009, John Wiley & Sons, Inc.
Copyright 2009, John Wiley & Sons, Inc.
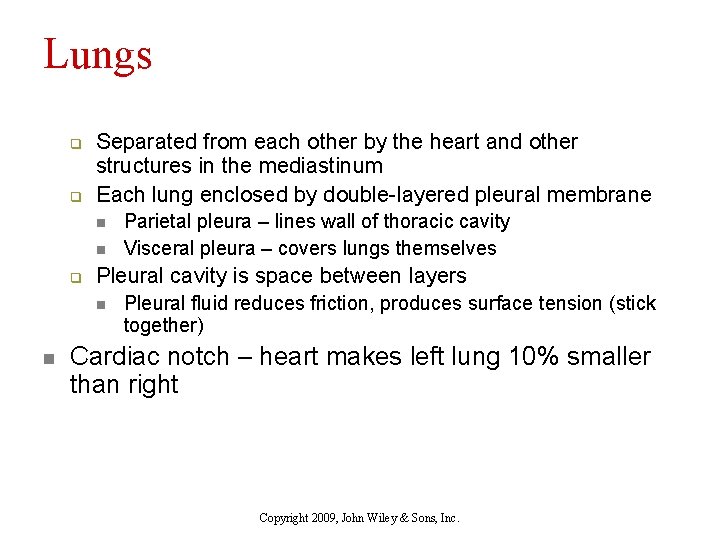
Lungs q q Separated from each other by the heart and other structures in the mediastinum Each lung enclosed by double-layered pleural membrane n n q Pleural cavity is space between layers n n Parietal pleura – lines wall of thoracic cavity Visceral pleura – covers lungs themselves Pleural fluid reduces friction, produces surface tension (stick together) Cardiac notch – heart makes left lung 10% smaller than right Copyright 2009, John Wiley & Sons, Inc.
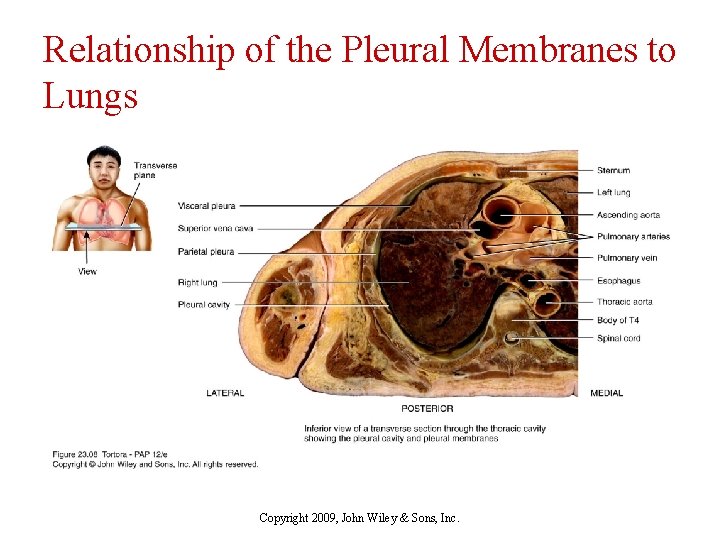
Relationship of the Pleural Membranes to Lungs Copyright 2009, John Wiley & Sons, Inc.
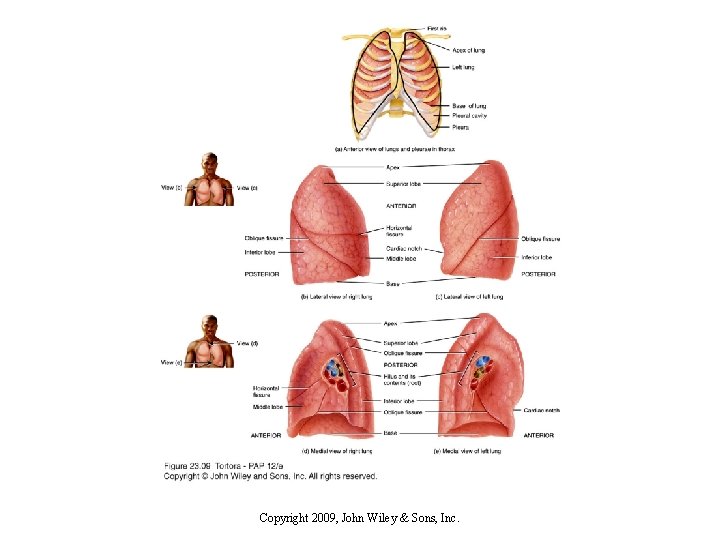
Copyright 2009, John Wiley & Sons, Inc.
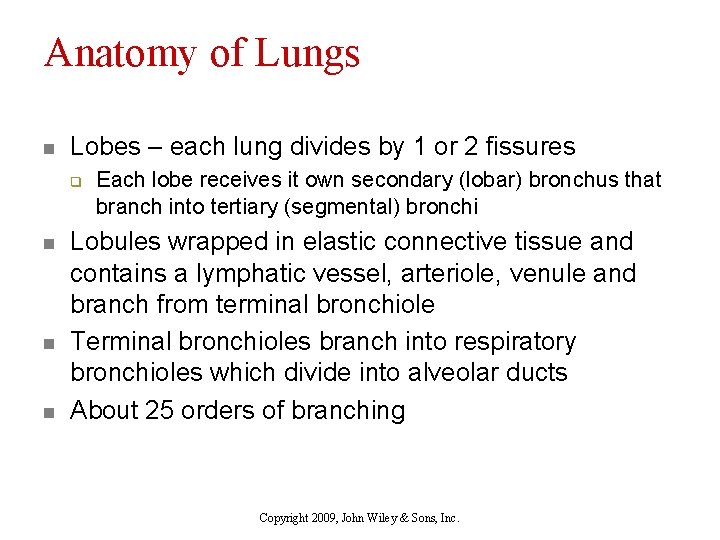
Anatomy of Lungs n Lobes – each lung divides by 1 or 2 fissures q n n n Each lobe receives it own secondary (lobar) bronchus that branch into tertiary (segmental) bronchi Lobules wrapped in elastic connective tissue and contains a lymphatic vessel, arteriole, venule and branch from terminal bronchiole Terminal bronchioles branch into respiratory bronchioles which divide into alveolar ducts About 25 orders of branching Copyright 2009, John Wiley & Sons, Inc.

Components of the Respiratory System Figure 23– 2 b, c The Respiratory Epithelium of the Nasal Cavity and Conducting System. Copyright 2009, John Wiley & Sons, Inc.
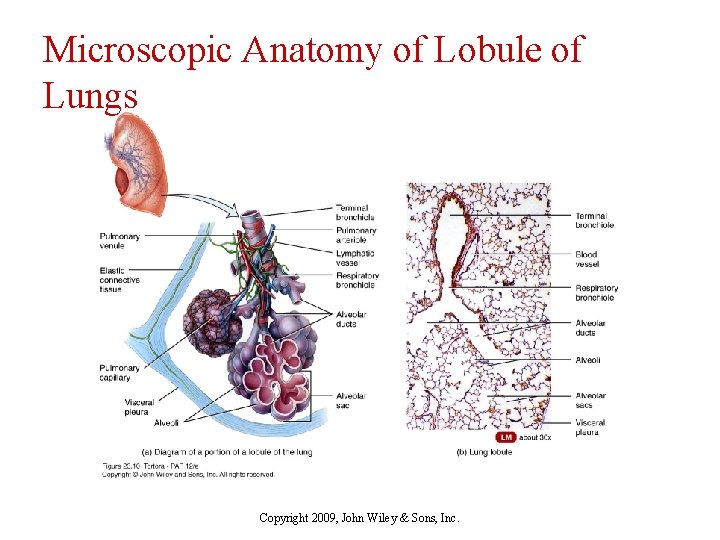
Microscopic Anatomy of Lobule of Lungs Copyright 2009, John Wiley & Sons, Inc.
Alveoli q q q Cup-shaped outpouching Alveolar sac – 2 or more alveoli sharing a common opening 2 types of alveolar epithelial cells n n Type I alveolar cells – form nearly continuous lining, more numerous than type II, main site of gas exchange Type II alveolar cells (septal cells) – free surfaces contain microvilli, secrete alveolar fluid (surfactant reduces tendency to collapse) Copyright 2009, John Wiley & Sons, Inc.
Alveolus n Respiratory membrane q q q n Alveolar wall – type I and type II alveolar cells Epithelial basement membrane Capillary endothelium Very thin – only 0. 5 µm thick to allow rapid diffusion of gases Lungs receive blood from q q Pulmonary artery - deoxygenated blood Bronchial arteries – oxygenated blood to perfuse muscular walls of bronchi and bronchioles Copyright 2009, John Wiley & Sons, Inc.
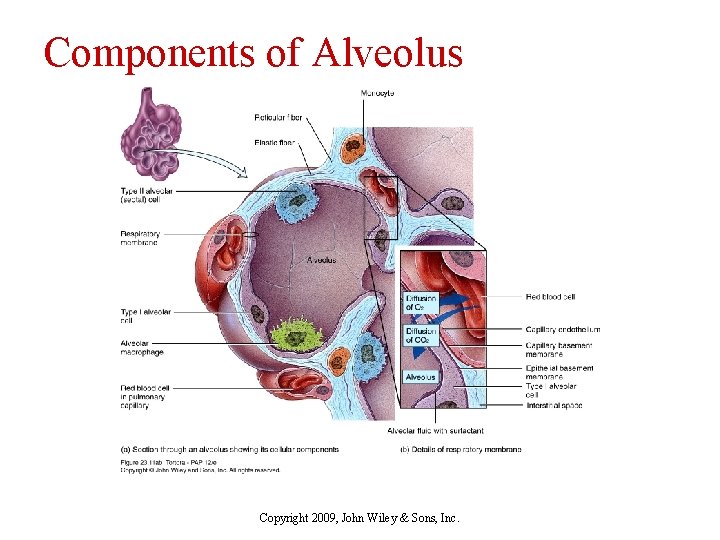
Components of Alveolus Copyright 2009, John Wiley & Sons, Inc.
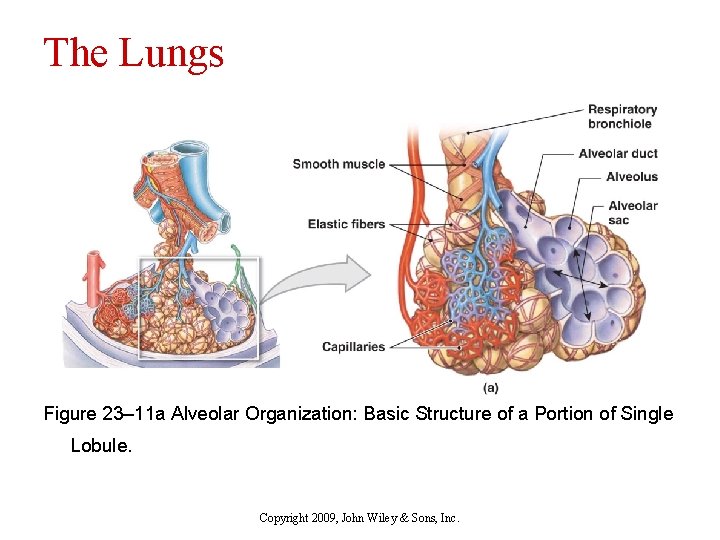
The Lungs Figure 23– 11 a Alveolar Organization: Basic Structure of a Portion of Single Lobule. Copyright 2009, John Wiley & Sons, Inc.
Components of the Respiratory System n The Respiratory Epithelium q For gases to exchange efficiently n n Alveoli walls must be very thin (<1 µm) Surface area must be very great (about 35 times the surface area of the body) Surface must be moist Concentration of oxygen in water at 20 degrees = 250 u. M Concentration of oxygen in air = 9 M Copyright 2009, John Wiley & Sons, Inc.
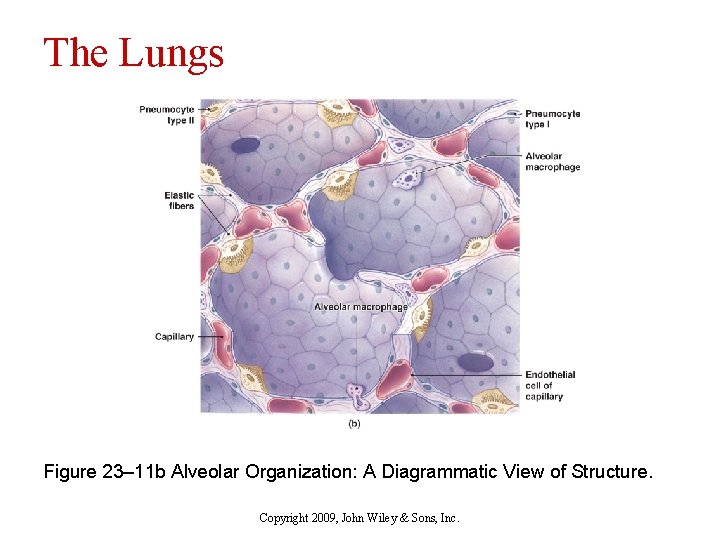
The Lungs Figure 23– 11 b Alveolar Organization: A Diagrammatic View of Structure. Copyright 2009, John Wiley & Sons, Inc.
Pulmonary ventilation n Respiration (gas exchange) steps 1. Pulmonary ventilation/ breathing n n 2. External (pulmonary) respiration n 3. Inhalation and exhalation Exchange of air between atmosphere and alveoli Exchange of gases between alveoli and blood Internal (tissue) respiration n n Exchange of gases between systemic capillaries and tissue cells Supplies cellular respiration (makes ATP) Copyright 2009, John Wiley & Sons, Inc.
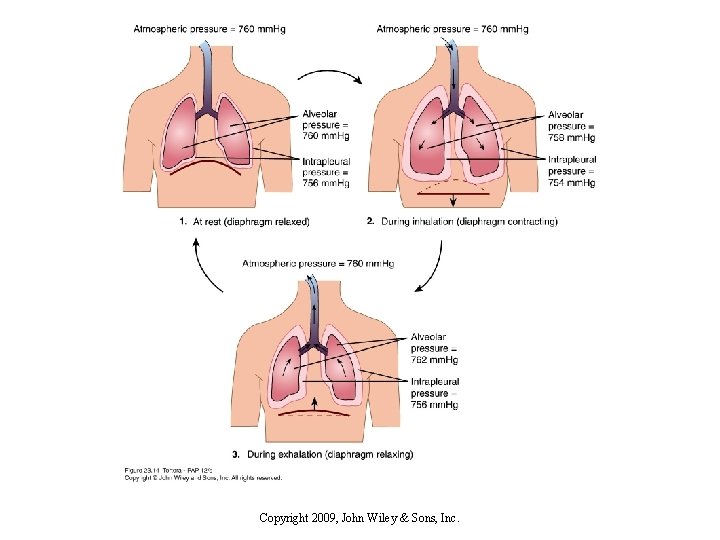
Inhalation/ inspiration q Pressure inside alveoli lust become lower than atmospheric pressure for air to flow into lungs n q Achieved by increasing size of lungs n q 760 millimeters of mercury (mm. Hg) or 1 atmosphere (1 atm) Boyle’s Law – pressure of a gas in a closed container is inversely proportional to the volume of the container Inhalation – lungs must expand, increasing lung volume, decreasing pressure below atmospheric pressure Copyright 2009, John Wiley & Sons, Inc.
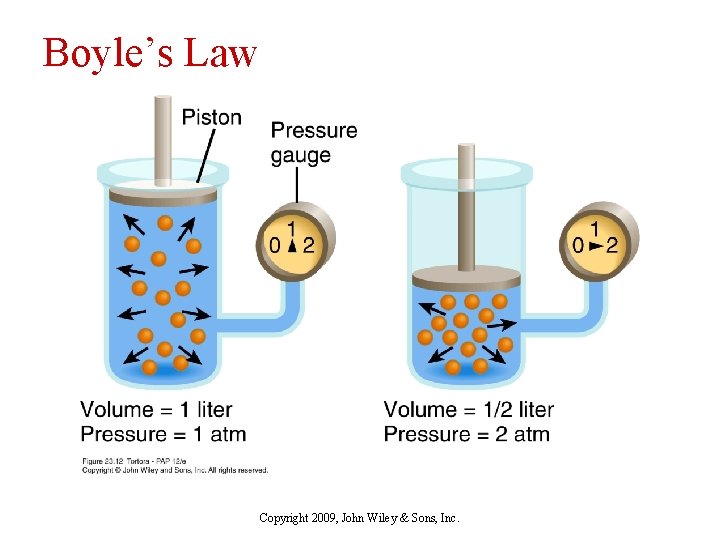
Boyle’s Law Copyright 2009, John Wiley & Sons, Inc.
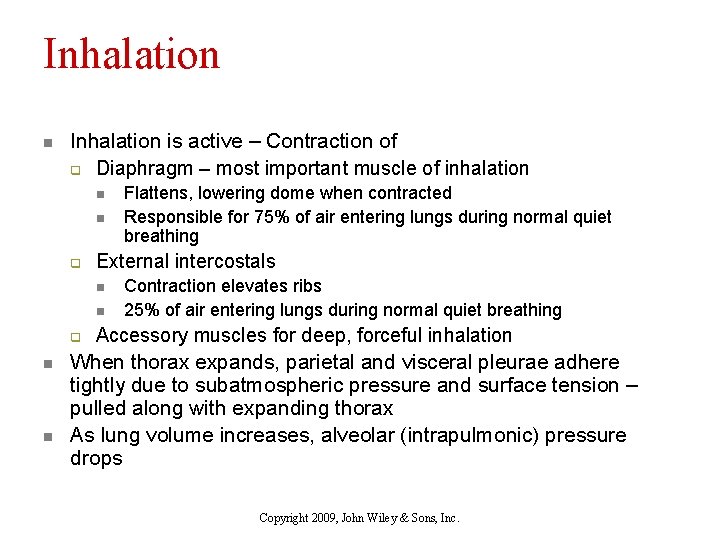
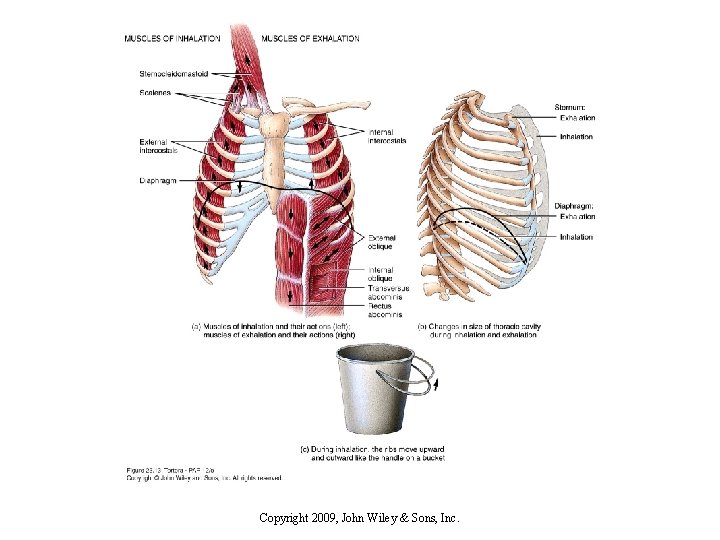
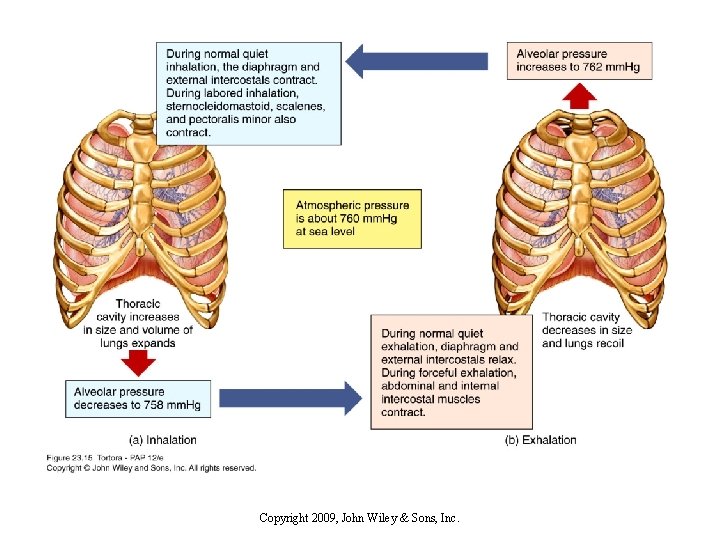
Inhalation n Inhalation is active – Contraction of q Diaphragm – most important muscle of inhalation n n q External intercostals n n q n n Flattens, lowering dome when contracted Responsible for 75% of air entering lungs during normal quiet breathing Contraction elevates ribs 25% of air entering lungs during normal quiet breathing Accessory muscles for deep, forceful inhalation When thorax expands, parietal and visceral pleurae adhere tightly due to subatmospheric pressure and surface tension – pulled along with expanding thorax As lung volume increases, alveolar (intrapulmonic) pressure drops Copyright 2009, John Wiley & Sons, Inc.
Copyright 2009, John Wiley & Sons, Inc.
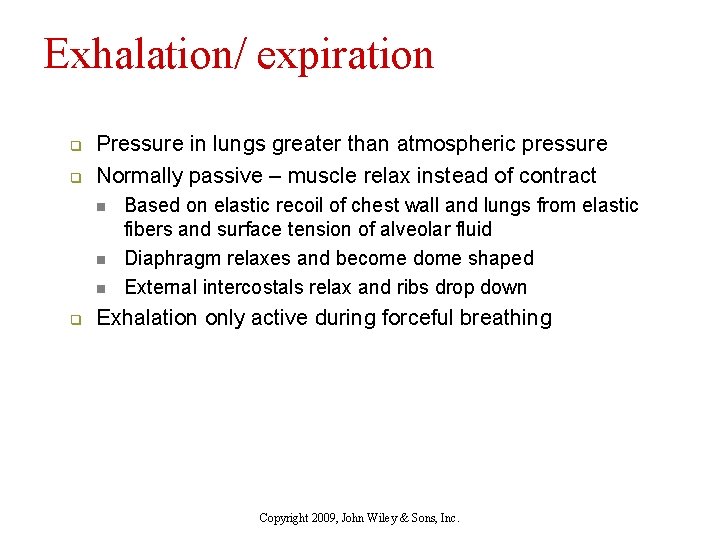
Exhalation/ expiration q q Pressure in lungs greater than atmospheric pressure Normally passive – muscle relax instead of contract n n n q Based on elastic recoil of chest wall and lungs from elastic fibers and surface tension of alveolar fluid Diaphragm relaxes and become dome shaped External intercostals relax and ribs drop down Exhalation only active during forceful breathing Copyright 2009, John Wiley & Sons, Inc.
Copyright 2009, John Wiley & Sons, Inc.
Copyright 2009, John Wiley & Sons, Inc.
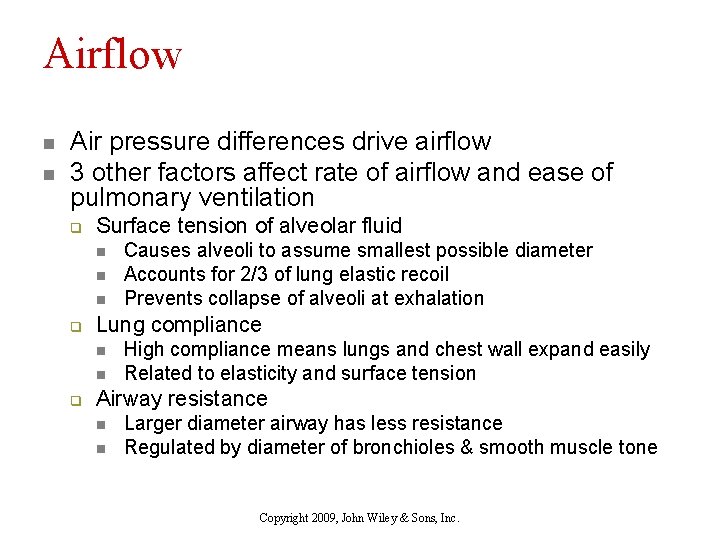
Airflow n n Air pressure differences drive airflow 3 other factors affect rate of airflow and ease of pulmonary ventilation q Surface tension of alveolar fluid n n n q Lung compliance n n q Causes alveoli to assume smallest possible diameter Accounts for 2/3 of lung elastic recoil Prevents collapse of alveoli at exhalation High compliance means lungs and chest wall expand easily Related to elasticity and surface tension Airway resistance n n Larger diameter airway has less resistance Regulated by diameter of bronchioles & smooth muscle tone Copyright 2009, John Wiley & Sons, Inc.
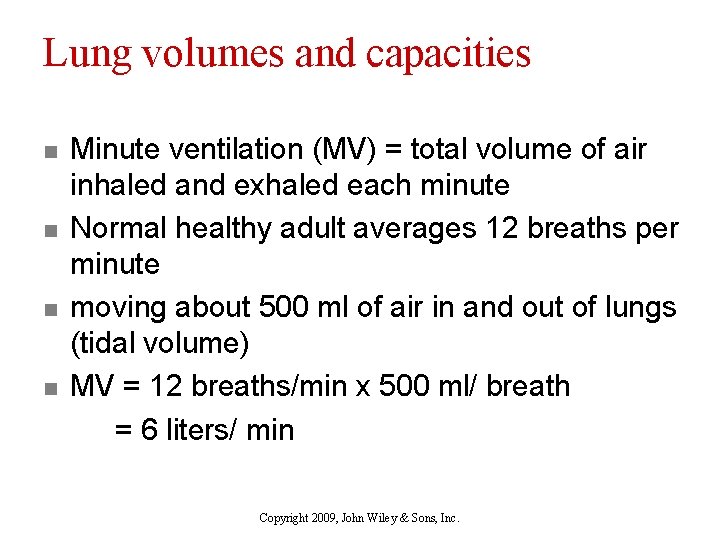
Lung volumes and capacities n n Minute ventilation (MV) = total volume of air inhaled and exhaled each minute Normal healthy adult averages 12 breaths per minute moving about 500 ml of air in and out of lungs (tidal volume) MV = 12 breaths/min x 500 ml/ breath = 6 liters/ min Copyright 2009, John Wiley & Sons, Inc.

Spirogram of Lung Volumes and Capacities Copyright 2009, John Wiley & Sons, Inc.
- Slides: 43