The Reduction of SelfMutilation in Borderline Personality Patients
The Reduction of Self-Mutilation in Borderline Personality Patients using Sensory Integration Therapy Aron Lipman Department of Applied Psychology New York University
Acknowledgements ¡ Specialized Programs in Occupational Therapy Services (SPOTS) ¡ Prudence Heisler, OT/L ¡ Michelle Kafko, OTR/L ¡ Lindsey Britchkow, OTR/L ¡ Peer Reviewers

Self-Mutilation Definition ¡ ¡ A way to cope, release tension, lessen anger, gain control and security, self-regulate, and create a feeling of euphoria. Self-mutilation can also have an immediate orienting effect, acting as intense, calming, or alerting stimuli enabling the individual to feel alive. Types ¡ ¡ Culturally Sanctioned Deviant l Major l Stereotypic l Superficial ¡ Compulsive ¡ Episodic ¡ Repetitive
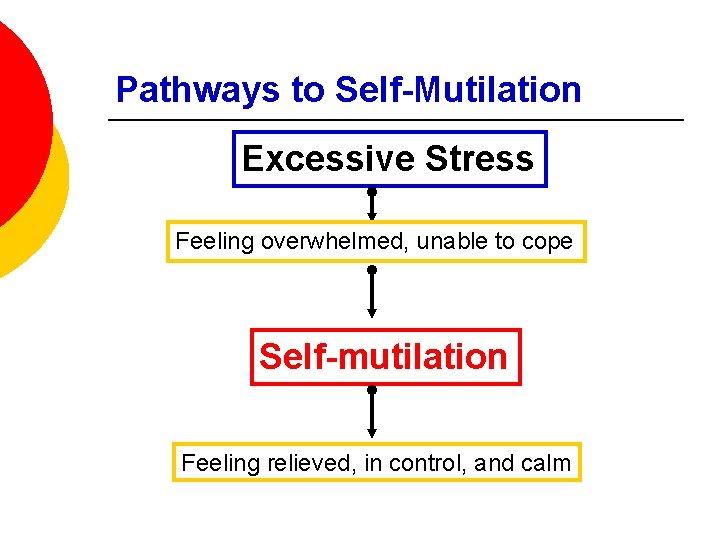
Pathways to Self-Mutilation Excessive Stress Feeling overwhelmed, unable to cope Self-mutilation Feeling relieved, in control, and calm

Pathways to Self-Mutilation Dissociation Feeling numb, overwhelmed, unreal Self-mutilation Feeling real, alive, able to function better
Borderline Personality Disorder ¡ BPD is a “pervasive pattern of instability in interpersonal relationships, self-image, and affects, and marked impulsivity beginning by early adulthood and present in a variety of contexts, as indicated by…recurrent suicidal behavior, gestures, or threats, or selfmutilating behavior. ” ¡ BPD is the only mental illness under personality disorders in the DSM-IV-TR that has self-mutilation as one of its main diagnostic criteria. DSM-IV-TR, 2002

Self-Mutilation among BPD Patients ¡ 6 -10 million Americans are diagnosed with BPD. ¡ 75% of BPD patients engage in self-injurious behavior. ¡ The rate of unintentional suicides, as a result of self-injurious behavior in BPD patients, is rising. ¡ There is a major gap in the research in terms of effective forms of treatment that properly address the growing number self-injurious BPD patients. Moro, 2007
Occupational Therapy ¡ The use of purposeful activity or interventions designed to achieve functional outcomes. ¡ Occupational therapists help people who are injured or ill regain their maximum level of functioning. ¡ Therapists address three crucial aspects of a person’s life: l Activities of daily living l Work/productive activities l Play/leisure activities
Sensory Integration ¡ Sensory-based therapy addresses: l An understanding of the sensory dimensions of human behavior. l The brain’s interpretation and organization of stimuli from an individual’s environment. l Adaptive responses for appropriate engagement in occupation. l The use of controlled sensorimotor experiences that help individuals function better in their environment. Baranek, 1998; Bright, Bittick, & Fleeman, 1981; Moro, 2007
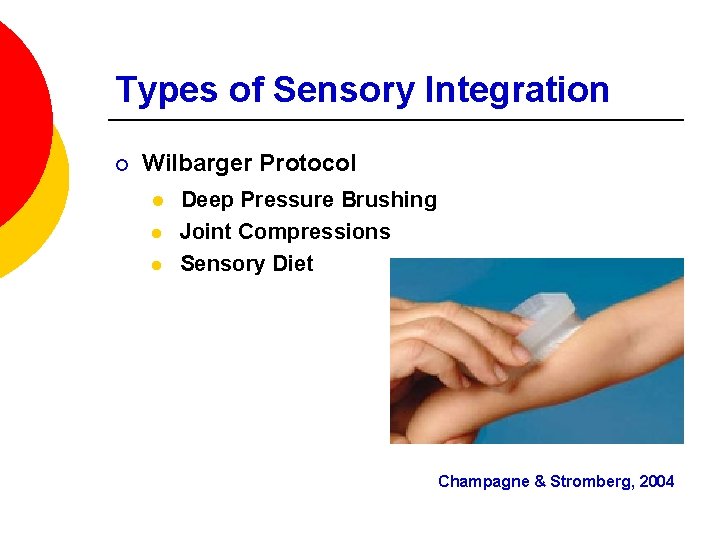
Types of Sensory Integration ¡ Wilbarger Protocol l Deep Pressure Brushing Joint Compressions Sensory Diet Champagne & Stromberg, 2004
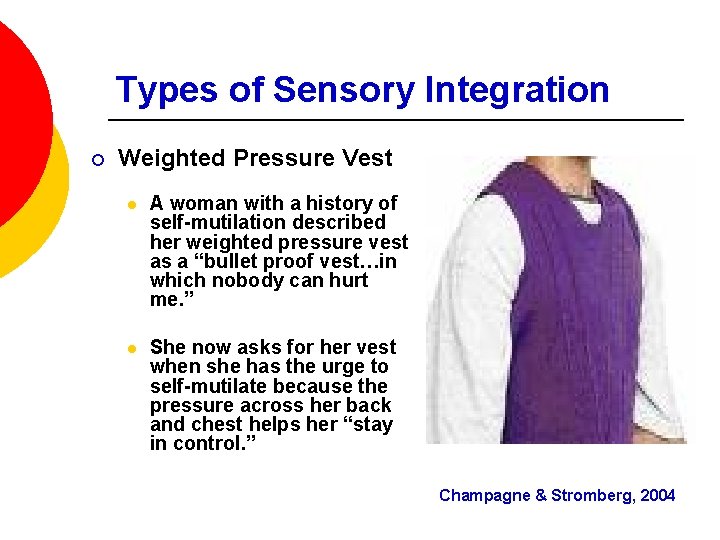
Types of Sensory Integration ¡ Weighted Pressure Vest l A woman with a history of self-mutilation described her weighted pressure vest as a “bullet proof vest…in which nobody can hurt me. ” l She now asks for her vest when she has the urge to self-mutilate because the pressure across her back and chest helps her “stay in control. ” Champagne & Stromberg, 2004
Types of Sensory Integration ¡ The Sensory-Modulation Room offers a combination of sensorimotor activities with calming and alerting options for all sensory areas. Champagne & Stromberg, 2004
Related Studies ¡ There have only been two studies looking at the use of sensory-based techniques and sensory-modulation rooms as treatment for self-injurious behavior. l In one study (N=47), 89% of the participants reported positive effects from the use of a sensorymodulation room. l In the second study (N=3), 2 out of the 3 women reported that after receiving sensory based treatment they no longer felt the urge to engage in self-injurious behavior. Champagne & Sayer, 2003; Moore & Henry, 2002
Research Question & Hypothesis ¡ Is Sensory Integration, as provided by an occupational therapist, an effective form of treatment for people diagnosed with borderline personality disorder who self-mutilate? The use of sensory integration therapy, specifically the Wilbarger Protocol and sensorymodulation rooms, will significantly reduce the desire and incidence of self-mutilation on patients diagnosed with BPD.
Participants ¡ 150 females all diagnosed with BPD and with known self-injurious behavior. ¡ Must be 20 years of age or older at the beginning of study. ¡ SES, race, and ethnicity will not be taken into account. ¡ Participants must be willing to commit to a twoyear longitudinal study.
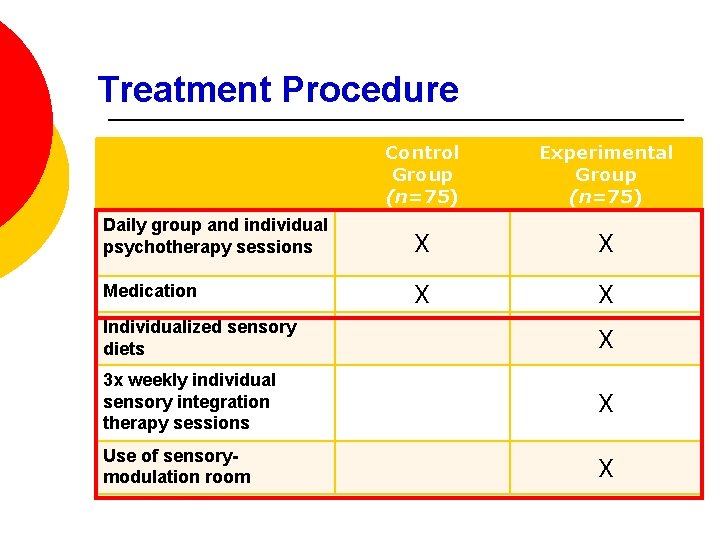
Treatment Procedure Control Group (n=75) Experimental Group (n=75) Daily group and individual psychotherapy sessions X X Medication X X Individualized sensory diets X 3 x weekly individual sensory integration therapy sessions X Use of sensorymodulation room X
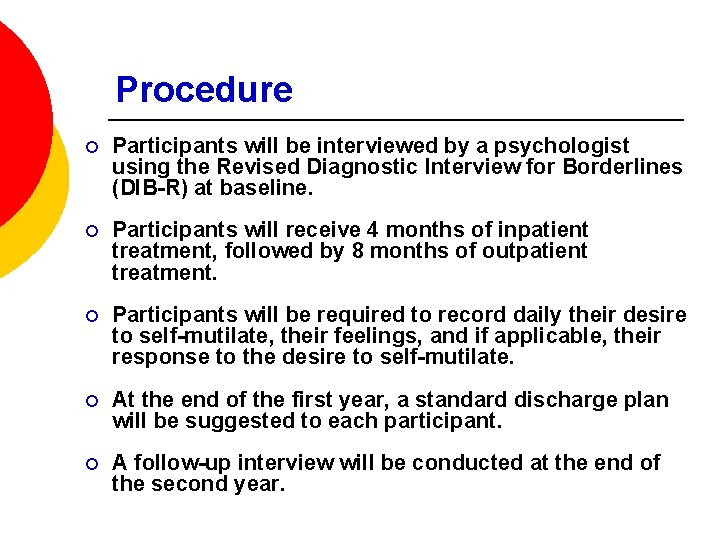
Procedure ¡ Participants will be interviewed by a psychologist using the Revised Diagnostic Interview for Borderlines (DIB-R) at baseline. ¡ Participants will receive 4 months of inpatient treatment, followed by 8 months of outpatient treatment. ¡ Participants will be required to record daily their desire to self-mutilate, their feelings, and if applicable, their response to the desire to self-mutilate. ¡ At the end of the first year, a standard discharge plan will be suggested to each participant. ¡ A follow-up interview will be conducted at the end of the second year.
Expected Results and Benefits ¡ The results of this study will show that sensory integration therapy and the use of a sensorymodulation room as components of a larger treatment plan will reduce the use of self-injurious behavior in patients diagnosed with BPD. ¡ Current trends indicate that the numbers of people self-mutilating are increasing, and as a result unintentional suicides are also increasing. ¡ Additionally, the results of the study will benefit all people who use self-mutilation as a coping mechanism or a way to self-regulate.
- Slides: 18