The Quick Mild Cognitive Impairment Screen Qmci A


- Slides: 68
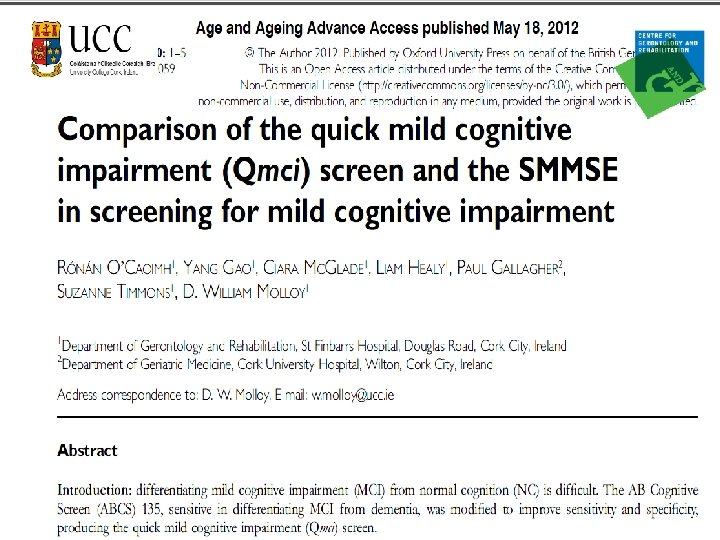
The Quick Mild Cognitive Impairment Screen: (Qmci) A NEW SCREENING TOOL FOR MILD COGNITIVE IMPAIRMENT (MCI) PROF D. W MOLLOY DR RÓNÁN O’CAOIMH CENTRE FOR GERONTOLOGY & REHABILITATION ST FINBARRS HOSPITAL/UNIVERSITY COLLEGE CORK CITY IRELAND
Overview 1. Demographics of cognitive impairment. 2. Challenges in screening, diagnosing & assessing cognition…. . How to choose appropriate cognitive screening tools. 3. Introduction to the Qmci. 4. Development of the Qmci. 5. The Quick Memory Check. 6. RAPCOG (The Rapid Community COGnitive screening programme. )
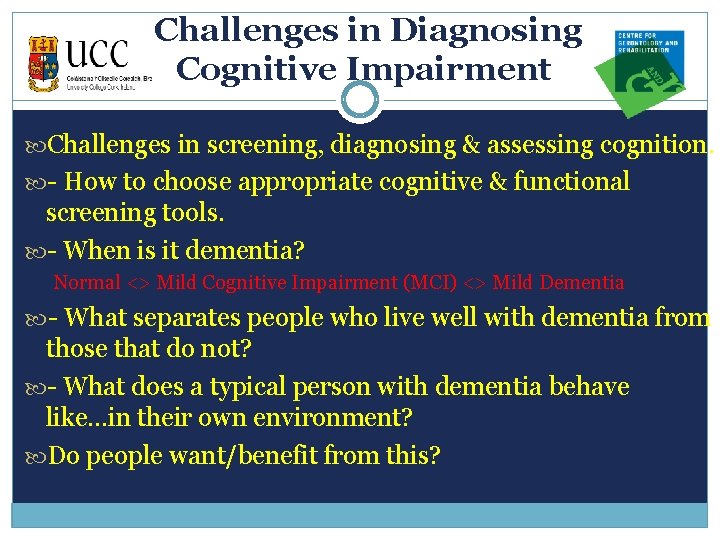
Challenges in Diagnosing Cognitive Impairment Challenges in screening, diagnosing & assessing cognition. - How to choose appropriate cognitive & functional screening tools. - When is it dementia? Normal <> Mild Cognitive Impairment (MCI) <> Mild Dementia - What separates people who live well with dementia from those that do not? - What does a typical person with dementia behave like. . . in their own environment? Do people want/benefit from this?
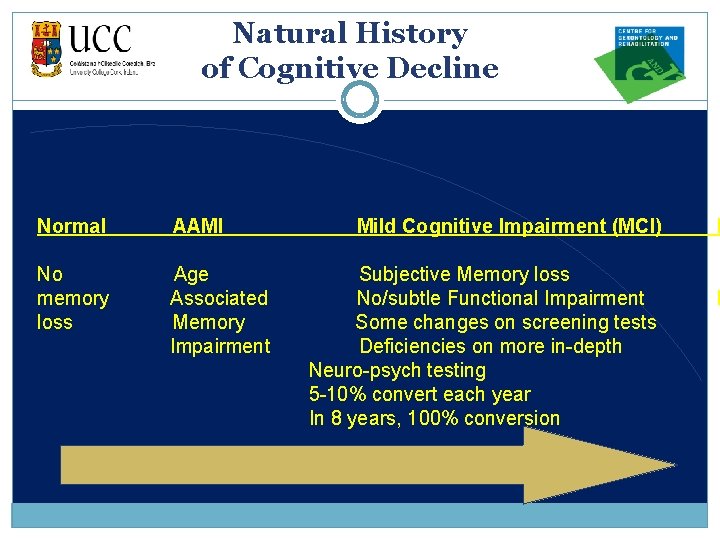
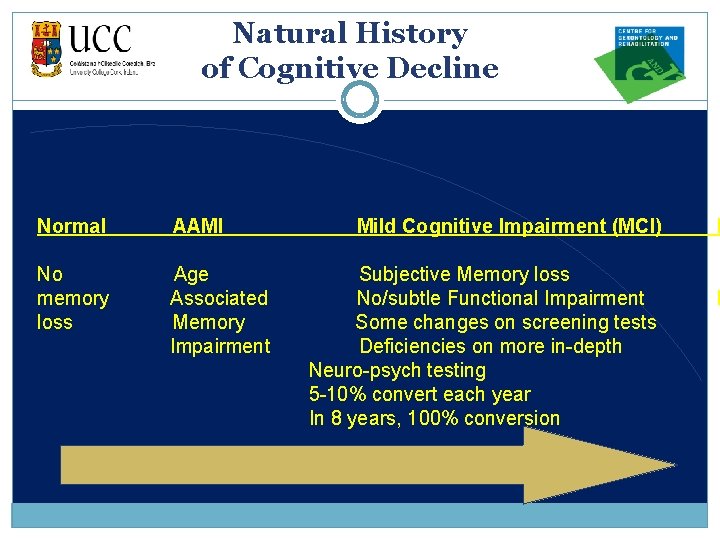
Natural History of Cognitive Decline Normal AAMI No memory loss Age Associated Memory Impairment Mild Cognitive Impairment (MCI) D Subjective Memory loss No/subtle Functional Impairment Some changes on screening tests Deficiencies on more in-depth Neuro-psych testing 5 -10% convert each year In 8 years, 100% conversion F I

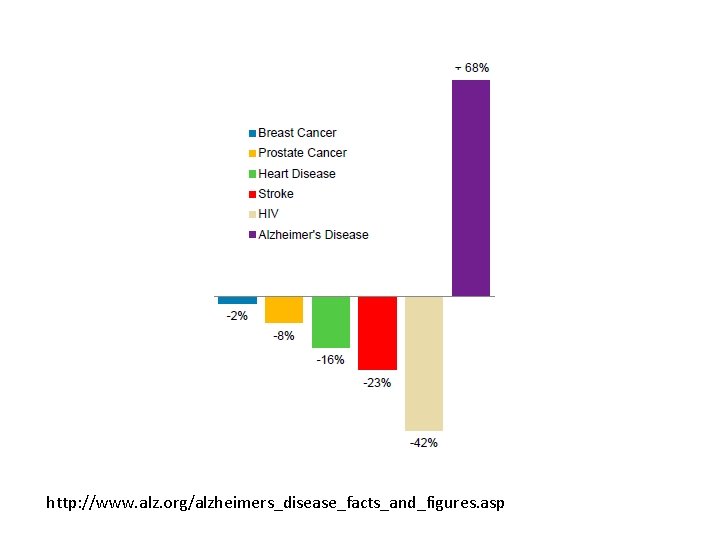
http: //www. alz. org/alzheimers_disease_facts_and_figures. asp
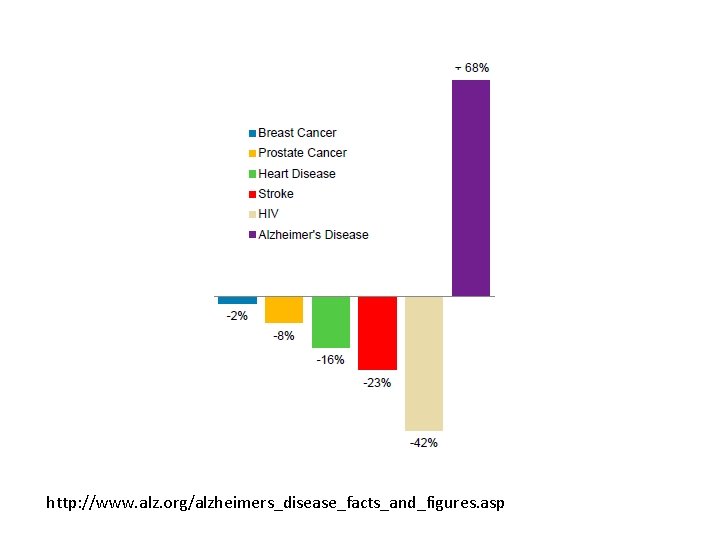
http: //www. alz. org/alzheimers_disease_facts_and_figures. asp
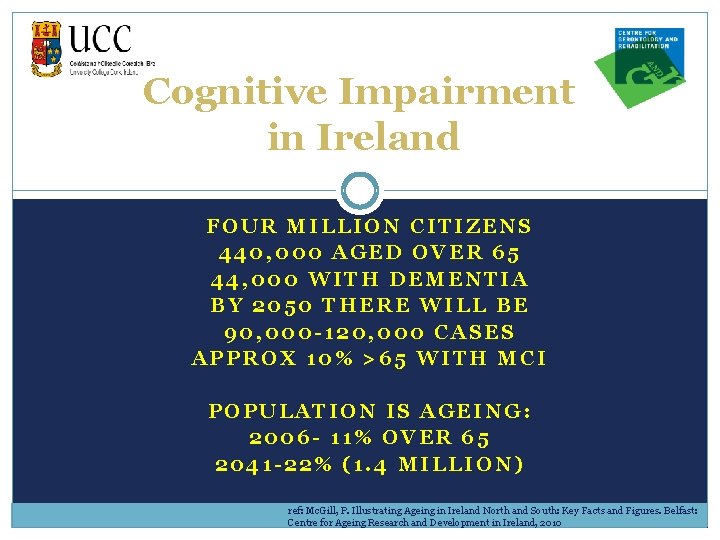
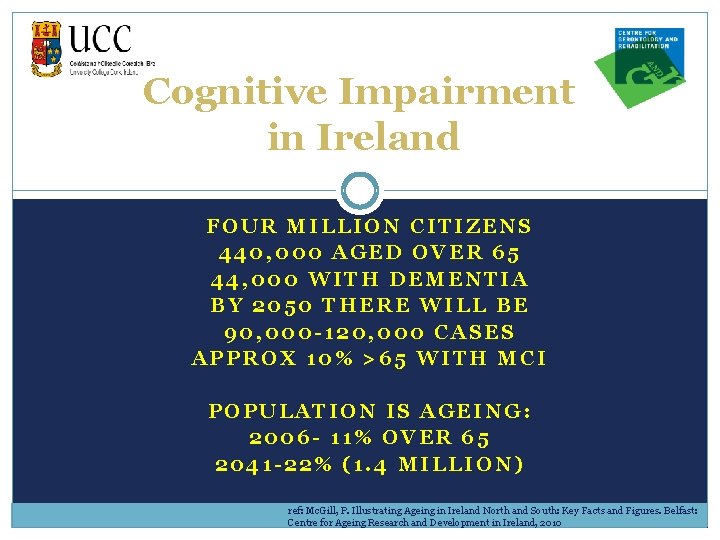
Cognitive Impairment in Ireland FOUR MILLION CITIZENS 440, 000 AGED OVER 65 44, 000 WITH DEMENTIA BY 2050 THERE WILL BE 90, 000 -120, 000 CASES APPROX 10% >65 WITH MCI POPULATION IS AGEING: 2006 - 11% OVER 65 2041 -22% (1. 4 MILLION) ref: Mc. Gill, P. Illustrating Ageing in Ireland North and South: Key Facts and Figures. Belfast: Centre for Ageing Research and Development in Ireland, 2010
Cognitive Impairment in the Community in Ireland • COMMON IN COMMUNITY. • 16. 7% OF PATIENTS FOLLOWED BY THEIR PUBLIC HEALTH • NURSE, LIVING IN THE COMMUNITY HAVE CI. • MEAN AGE 81. 8 YEARS, SD +/-7 (OLDER, P=0. 001). • PREDOMINANTLY FEMALE (70%). • MORE FUNCTIONALLY IMPAIRED, (MEDIAN BARTHEL SCORE 14 VS 18, P<0. 001). • HALF LIVE ALONE (P=0. 11).
Screening for Cognitive Impairment Strong evidence that cognitive impairment is under- recognised: 40 -75% attending their GP are missed. ref Valcour et al, Arch Int Med 2000 Detecting & distinguishing mild dementia & MCI is a challenge. ref Löppönen et al Age and Ageing 2003 MCI represents a heterogeneous group of disorders of memory impairment. How can the “worried well” be differentiated from patients with MCI? Need sensitive & specific cognitive screening instruments.
Screening for Cognitive Impairment Sensitivity: If I have the disease, is the test positive? Specificity: If I do not have the disease, is the test negative? Too Sensitive: over diagnose, normal's misdiagnosed (including the “worried well”). Too Specific: under diagnose, people with the disease called normal (“miss highly educated”). Many screening instruments with different sensitivities & specificities.
Why Screen? Early Dx allows Prompt initiation of appropriate care. Important to differentiate between MCI, NC & Dementia – Different Rx & prognosis. Allows identification of reversible causes – 10 -50 % of referrals to memory clinics ( <1. 5% cases of mild to mod dementia). Screening for vascular risk factors. Initiation of lifestyle advice. Planning for the future (advanced care plans/power of attorney). Potential for future treatments & reducing stigma.
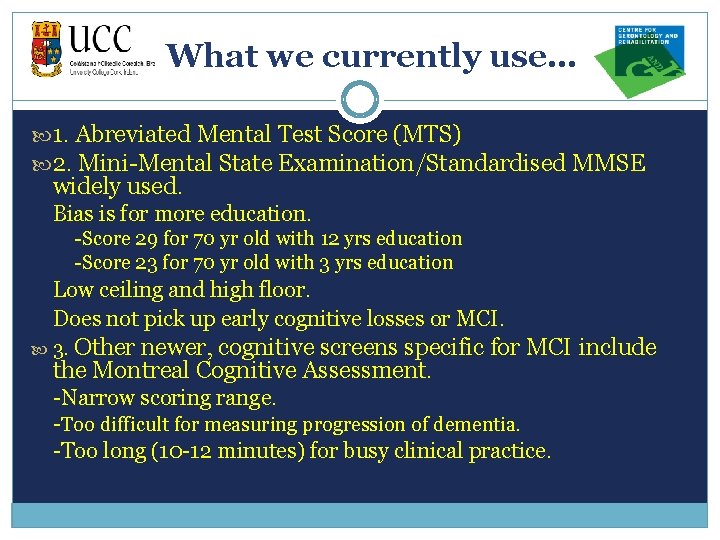
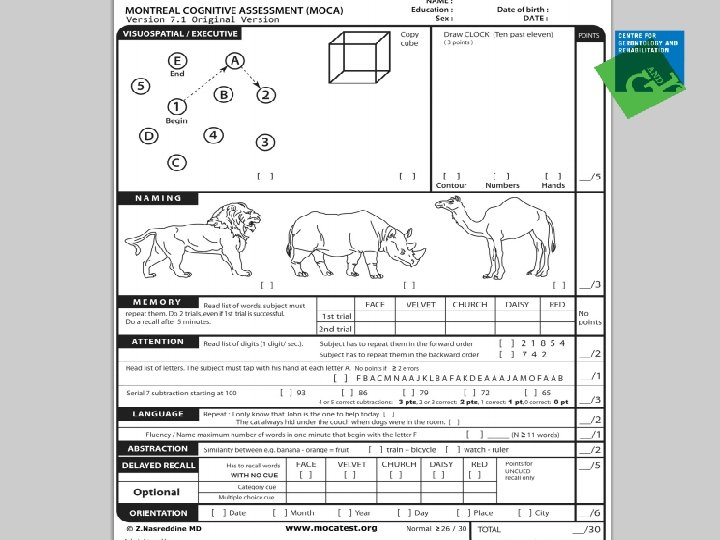
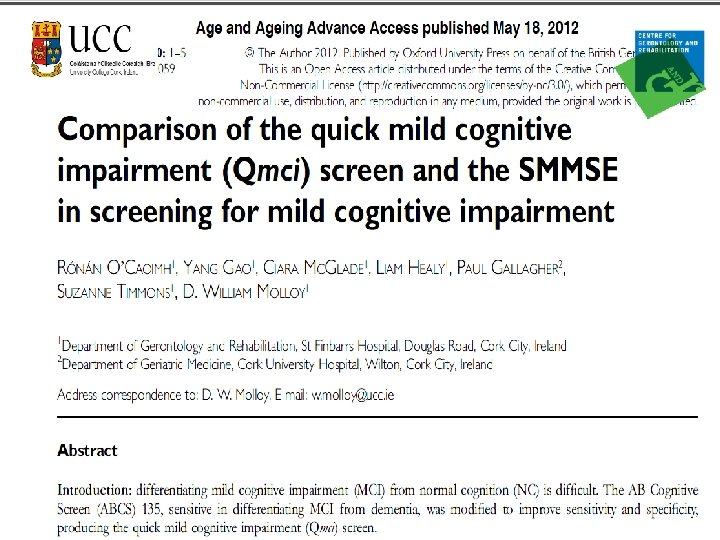
What we currently use… 1. Abreviated Mental Test Score (MTS) 2. Mini-Mental State Examination/Standardised MMSE widely used. Bias is for more education. -Score 29 for 70 yr old with 12 yrs education -Score 23 for 70 yr old with 3 yrs education Low ceiling and high floor. Does not pick up early cognitive losses or MCI. 3. Other newer, cognitive screens specific for MCI include the Montreal Cognitive Assessment. -Narrow scoring range. -Too difficult for measuring progression of dementia. -Too long (10 -12 minutes) for busy clinical practice.
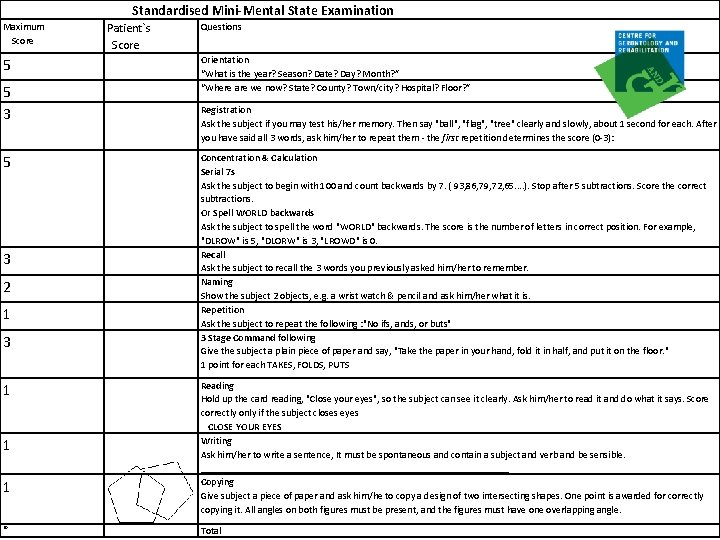
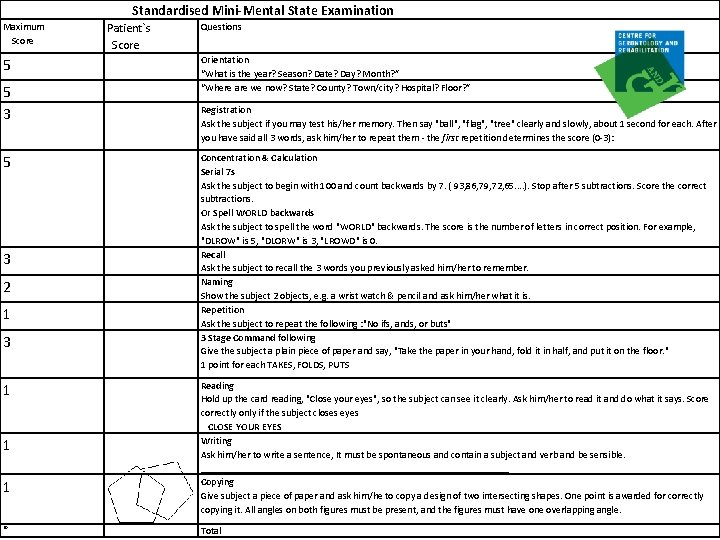
Standardised Mini-Mental State Examination Maximum Score 5 5 3 2 1 3 1 1 1 30 Patient`s Score Questions Orientation “What is the year? Season? Date? Day? Month? ” “Where are we now? State? County? Town/city? Hospital? Floor? ” Registration Ask the subject if you may test his/her memory. Then say "ball", "flag", "tree" clearly and slowly, about 1 second for each. After you have said all 3 words, ask him/her to repeat them - the first repetition determines the score (0 -3): Concentration & Calculation Serial 7 s Ask the subject to begin with 100 and count backwards by 7. ( 93, 86, 79, 72, 65. . ). Stop after 5 subtractions. Score the correct subtractions. Or Spell WORLD backwards Ask the subject to spell the word "WORLD" backwards. The score is the number of letters in correct position. For example, "DLROW" is 5, "DLORW" is 3, "LROWD" is 0. Recall Ask the subject to recall the 3 words you previously asked him/her to remember. Naming Show the subject 2 objects, e. g. a wrist watch & pencil and ask him/her what it is. Repetition Ask the subject to repeat the following : "No ifs, ands, or buts" 3 Stage Command following Give the subject a plain piece of paper and say, "Take the paper in your hand, fold it in half, and put it on the floor. " 1 point for each TAKES, FOLDS, PUTS Reading Hold up the card reading, "Close your eyes", so the subject can see it clearly. Ask him/her to read it and do what it says. Score correctly only if the subject closes eyes CLOSE YOUR EYES Writing Ask him/her to write a sentence, It must be spontaneous and contain a subject and verb and be sensible. _______________________________ Copying Give subject a piece of paper and ask him/he to copy a design of two intersecting shapes. One point is awarded for correctly copying it. All angles on both figures must be present, and the figures must have one overlapping angle. Total
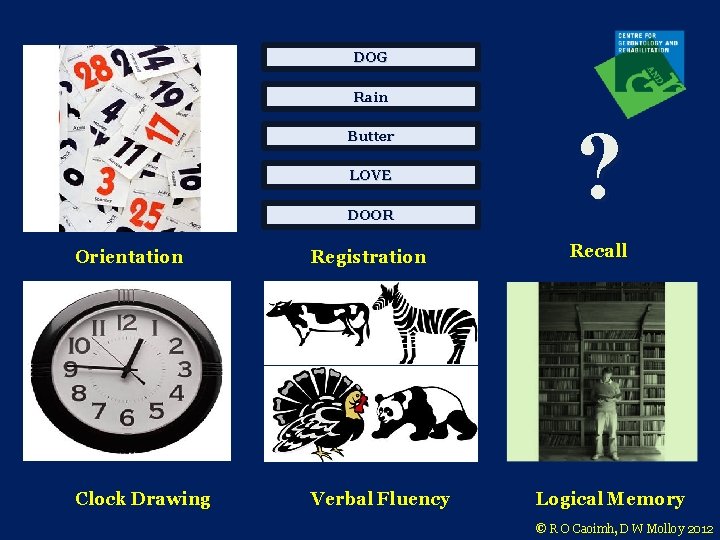
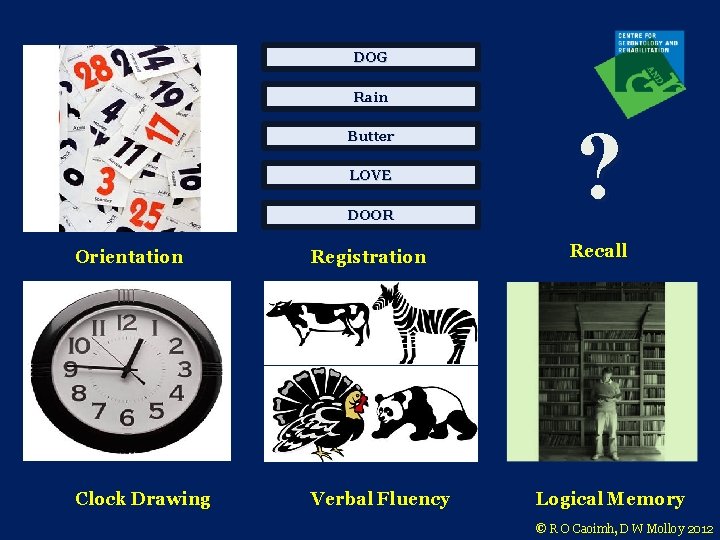
DOG Rain DOOR ? Orientation Registration Recall Clock Drawing Verbal Fluency Butter LOVE Logical Memory © R O Caoimh, D W Molloy 2012
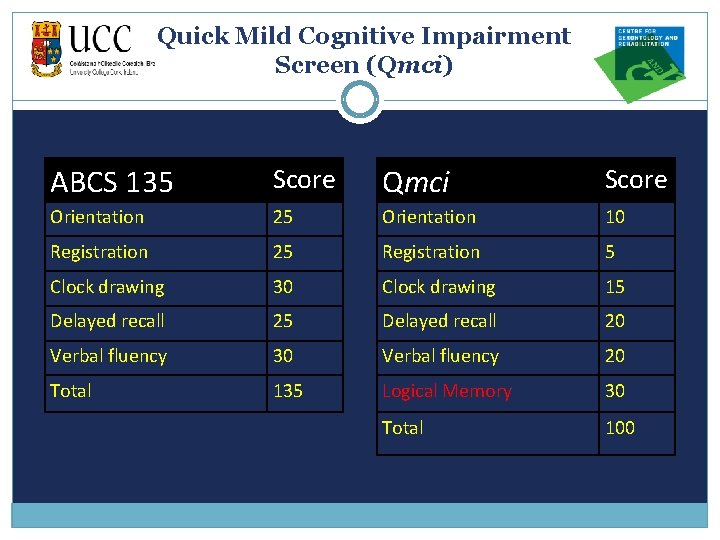
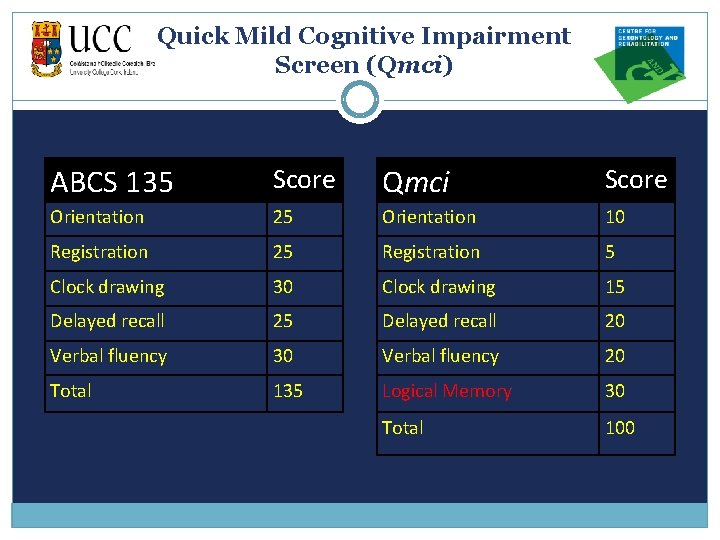
Quick Mild Cognitive Impairment Screen (Qmci) ABCS 135 Score Qmci Score Orientation 25 Orientation 10 Registration 25 Registration 5 Clock drawing 30 Clock drawing 15 Delayed recall 20 Verbal fluency 30 Verbal fluency 20 Total 135 Logical Memory 30 Total 100
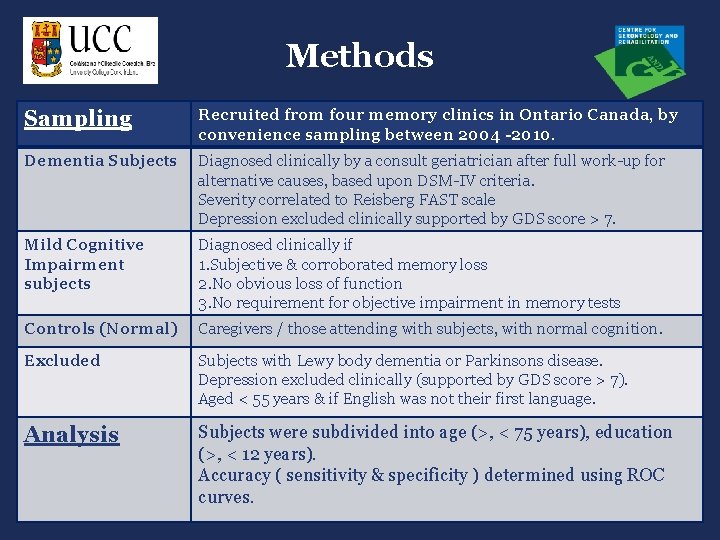
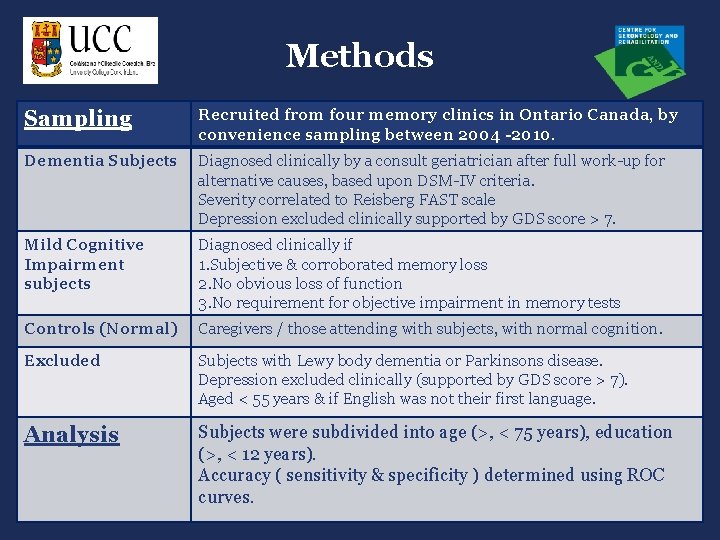
Methods Sampling Recruited from four memory clinics in Ontario Canada, by convenience sampling between 2004 -2010. Dementia Subjects Diagnosed clinically by a consult geriatrician after full work-up for alternative causes, based upon DSM-IV criteria. Severity correlated to Reisberg FAST scale Depression excluded clinically supported by GDS score > 7. Mild Cognitive Impairment subjects Diagnosed clinically if 1. Subjective & corroborated memory loss 2. No obvious loss of function 3. No requirement for objective impairment in memory tests Controls (Normal) Caregivers / those attending with subjects, with normal cognition. Excluded Subjects with Lewy body dementia or Parkinsons disease. Depression excluded clinically (supported by GDS score > 7). Aged < 55 years & if English was not their first language. Analysis Subjects were subdivided into age (>, < 75 years), education (>, < 12 years). Accuracy ( sensitivity & specificity ) determined using ROC curves.
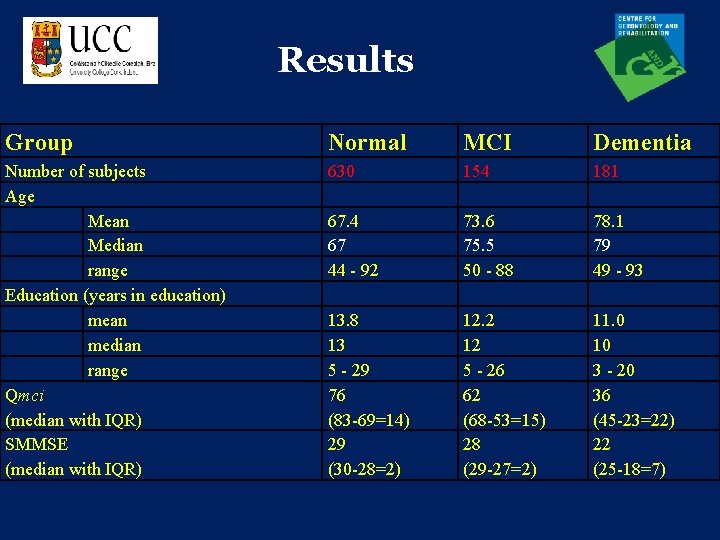
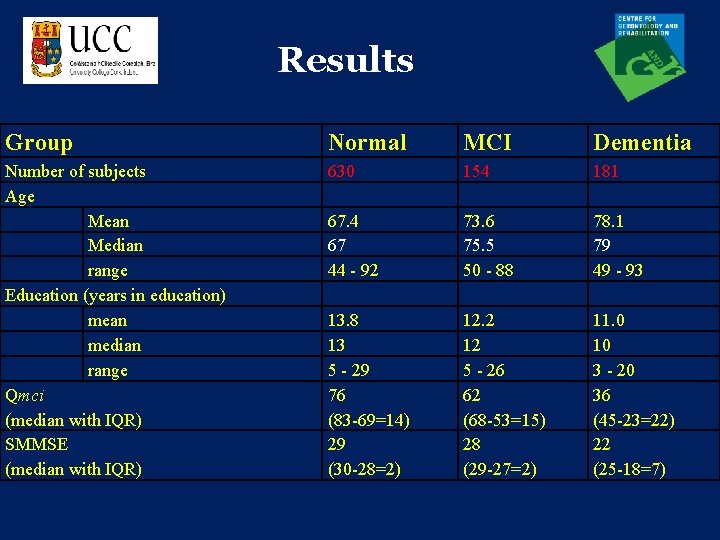
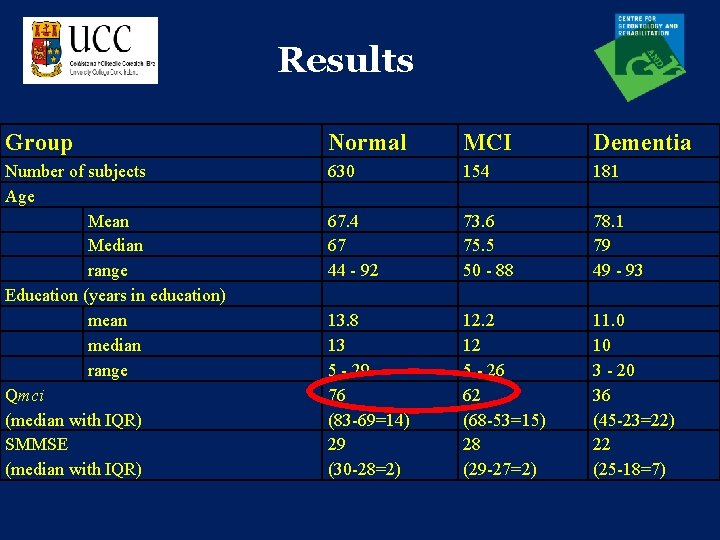
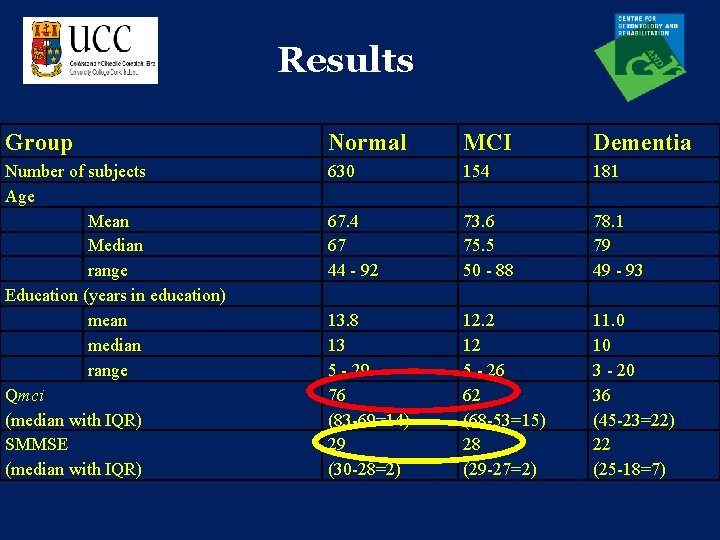
Results Group Normal MCI Dementia Number of subjects Age Mean Median range Education (years in education) mean median range Qmci (median with IQR) SMMSE (median with IQR) 630 154 181 67. 4 67 44 - 92 73. 6 75. 5 50 - 88 78. 1 79 49 - 93 13. 8 13 5 - 29 76 (83 -69=14) 29 (30 -28=2) 12. 2 12 5 - 26 62 (68 -53=15) 28 (29 -27=2) 11. 0 10 3 - 20 36 (45 -23=22) 22 (25 -18=7)
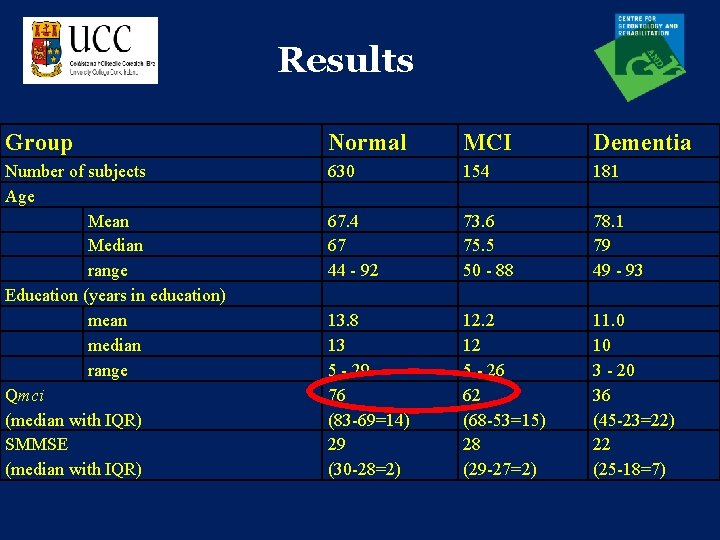
Results Group Normal MCI Dementia Number of subjects Age Mean Median range Education (years in education) mean median range Qmci (median with IQR) SMMSE (median with IQR) 630 154 181 67. 4 67 44 - 92 73. 6 75. 5 50 - 88 78. 1 79 49 - 93 13. 8 13 5 - 29 76 (83 -69=14) 29 (30 -28=2) 12. 2 12 5 - 26 62 (68 -53=15) 28 (29 -27=2) 11. 0 10 3 - 20 36 (45 -23=22) 22 (25 -18=7)
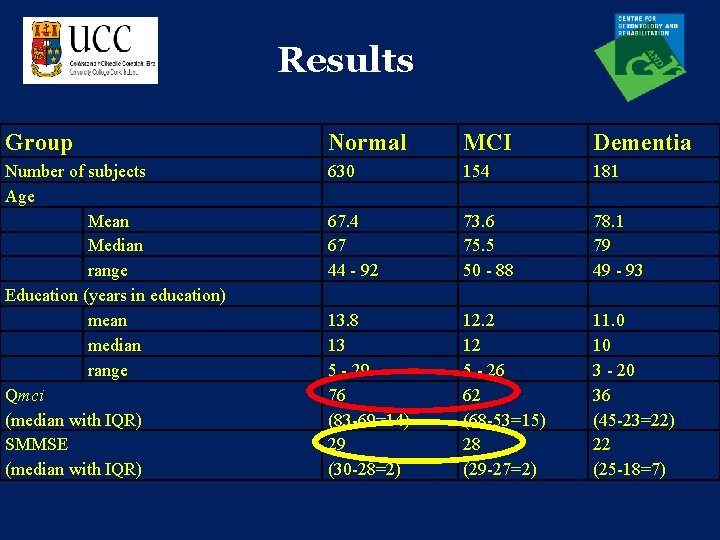
Results Group Normal MCI Dementia Number of subjects Age Mean Median range Education (years in education) mean median range Qmci (median with IQR) SMMSE (median with IQR) 630 154 181 67. 4 67 44 - 92 73. 6 75. 5 50 - 88 78. 1 79 49 - 93 13. 8 13 5 - 29 76 (83 -69=14) 29 (30 -28=2) 12. 2 12 5 - 26 62 (68 -53=15) 28 (29 -27=2) 11. 0 10 3 - 20 36 (45 -23=22) 22 (25 -18=7)
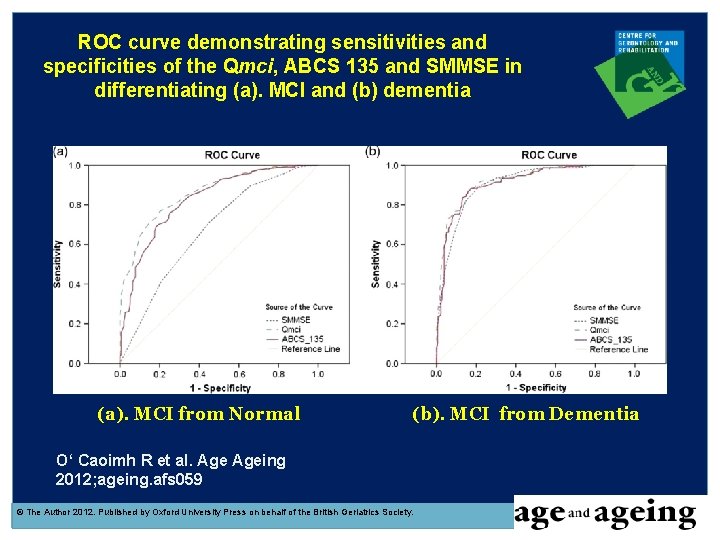
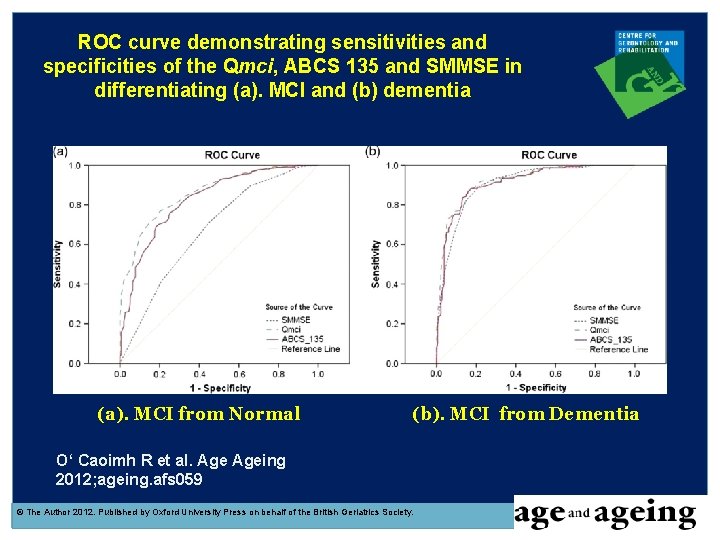
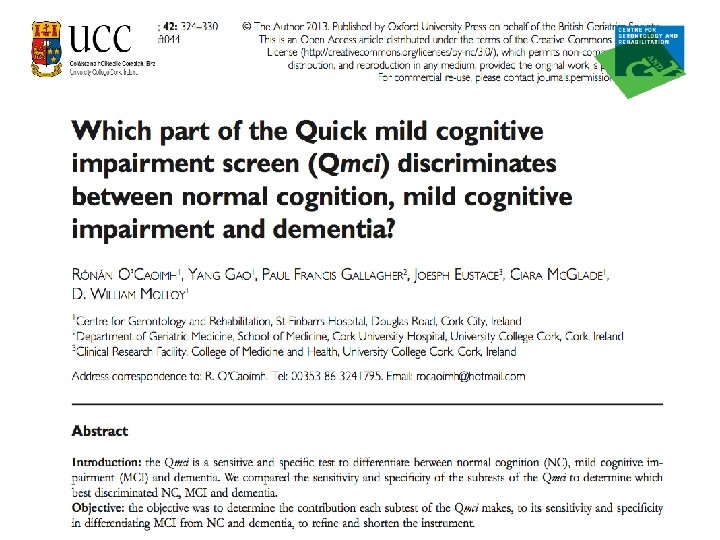
ROC curve demonstrating sensitivities and specificities of the Qmci, ABCS 135 and SMMSE in differentiating (a). MCI and (b) dementia (a). MCI from Normal (b). MCI from Dementia O‘ Caoimh R et al. Ageing 2012; ageing. afs 059 © The Author 2012. Published by Oxford University Press on behalf of the British Geriatrics Society.
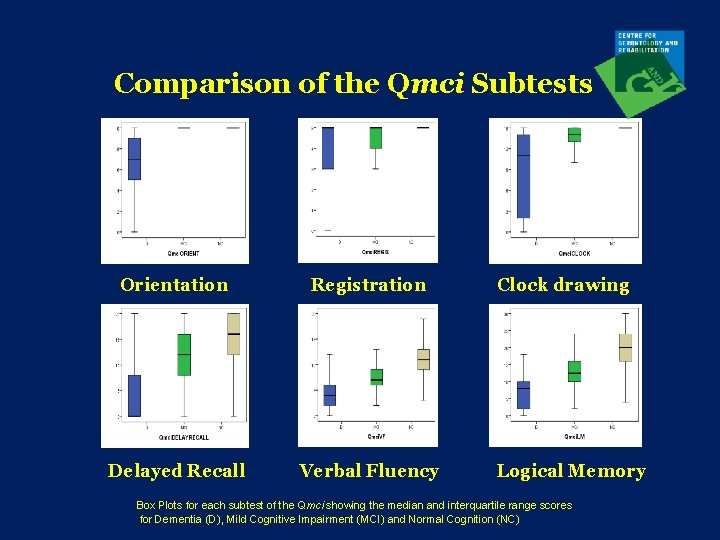
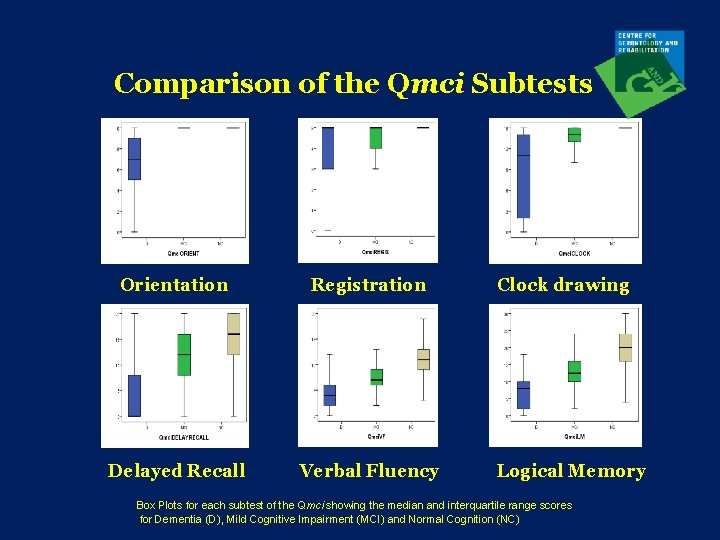
Comparison of the Qmci Subtests Orientation Registration Delayed Recall Verbal Fluency Clock drawing Logical Memory Box Plots for each subtest of the Qmci showing the median and interquartile range scores for Dementia (D), Mild Cognitive Impairment (MCI) and Normal Cognition (NC)
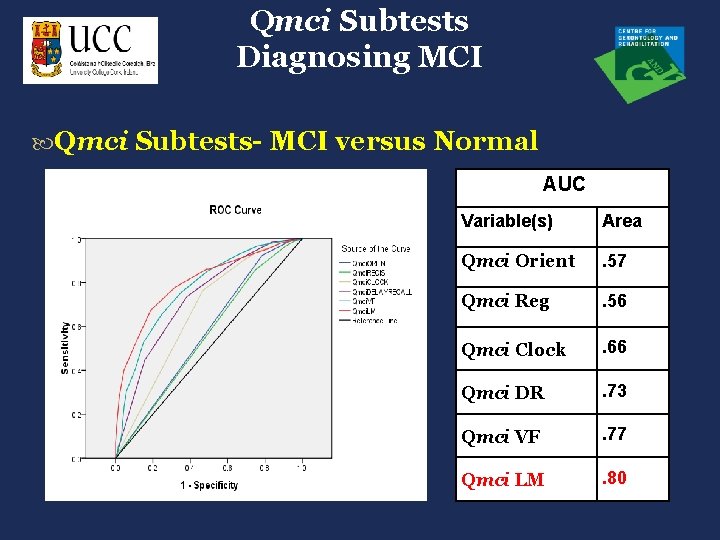
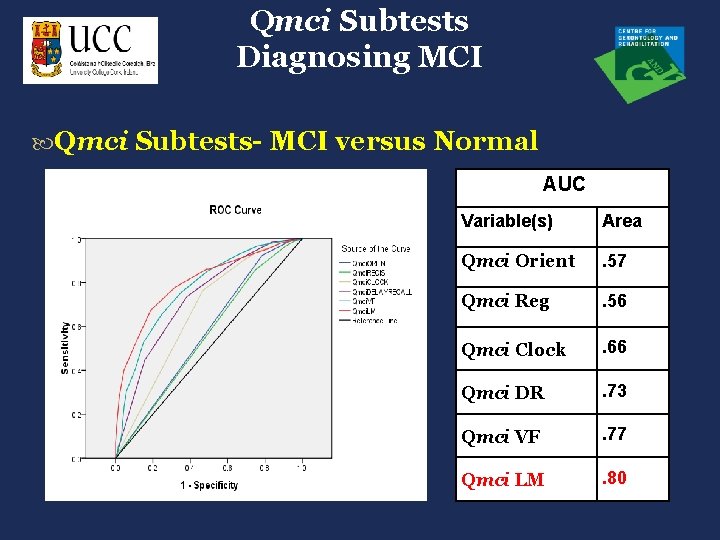
Qmci Subtests Diagnosing MCI Qmci Subtests- MCI versus Normal AUC Variable(s) Area Qmci Orient . 57 Qmci Reg . 56 Qmci Clock . 66 Qmci DR . 73 Qmci VF . 77 Qmci LM . 80
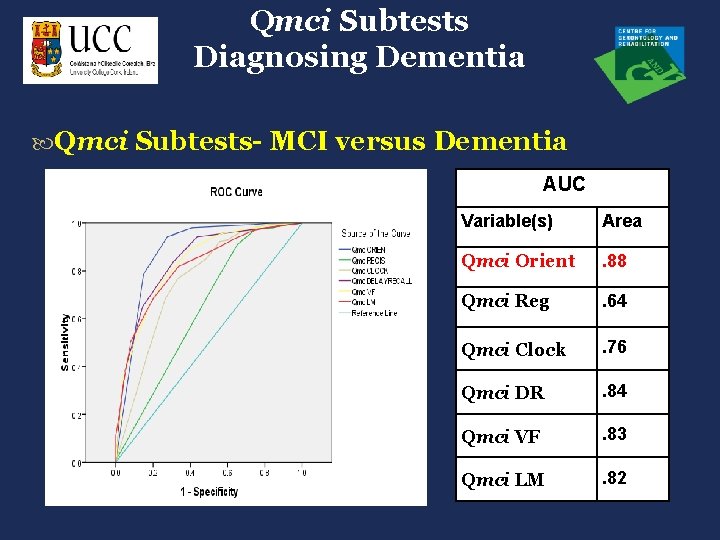
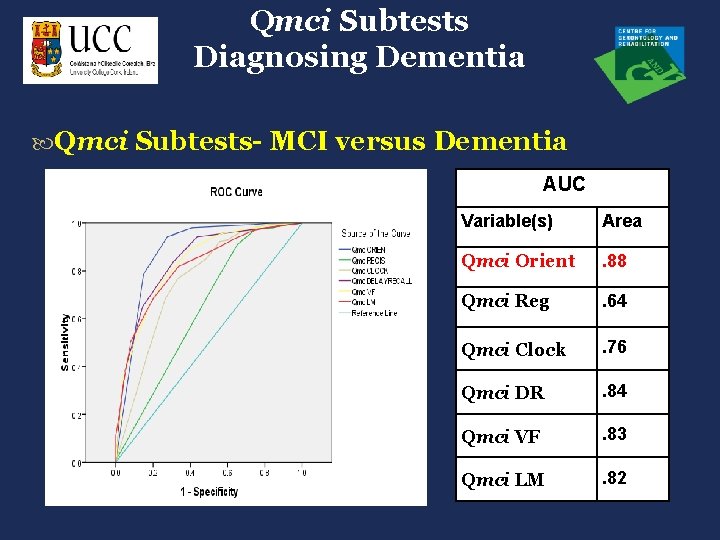
Qmci Subtests Diagnosing Dementia Qmci Subtests- MCI versus Dementia AUC Variable(s) Area Qmci Orient . 88 Qmci Reg . 64 Qmci Clock . 76 Qmci DR . 84 Qmci VF . 83 Qmci LM . 82
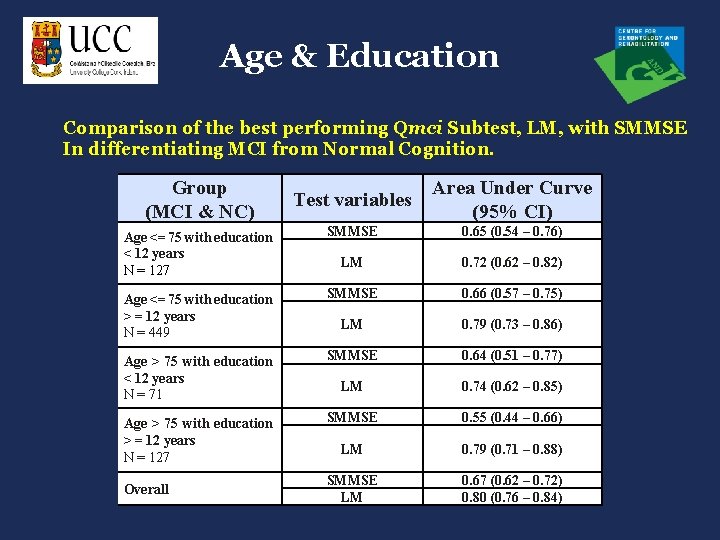
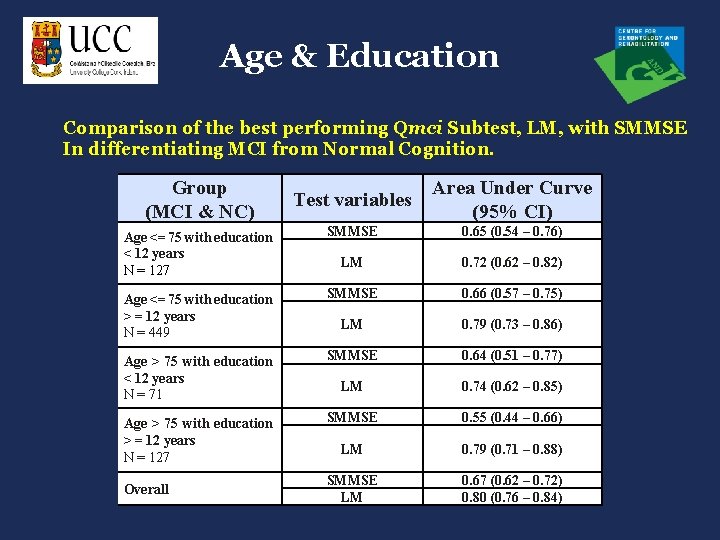
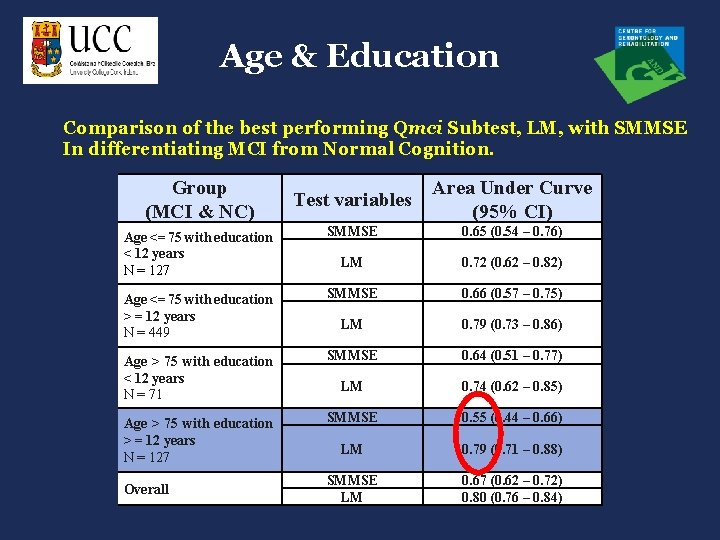
Age & Education Comparison of the best performing Qmci Subtest, LM, with SMMSE In differentiating MCI from Normal Cognition. Group (MCI & NC) Test variables Area Under Curve (95% CI) Age <= 75 with education < 12 years N = 127 SMMSE 0. 65 (0. 54 – 0. 76) LM 0. 72 (0. 62 – 0. 82) Age <= 75 with education > = 12 years N = 449 SMMSE 0. 66 (0. 57 – 0. 75) LM 0. 79 (0. 73 – 0. 86) Age > 75 with education < 12 years N = 71 SMMSE 0. 64 (0. 51 – 0. 77) LM 0. 74 (0. 62 – 0. 85) Age > 75 with education > = 12 years N = 127 SMMSE 0. 55 (0. 44 – 0. 66) LM 0. 79 (0. 71 – 0. 88) SMMSE LM 0. 67 (0. 62 – 0. 72) 0. 80 (0. 76 – 0. 84) Overall
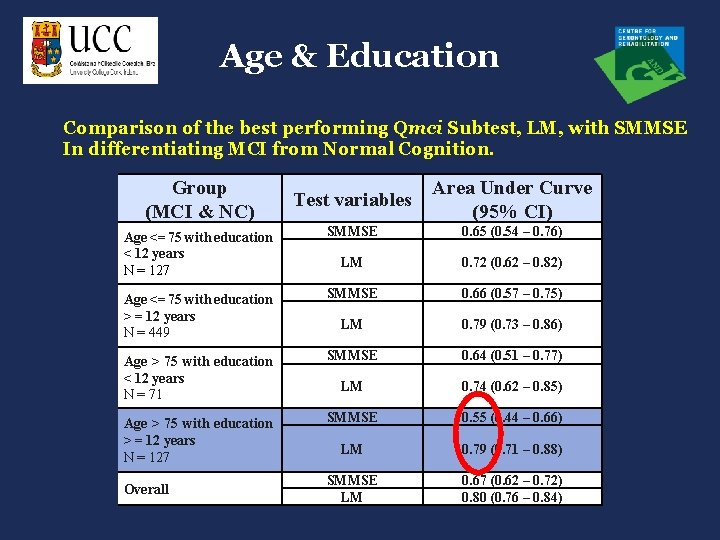
Age & Education Comparison of the best performing Qmci Subtest, LM, with SMMSE In differentiating MCI from Normal Cognition. Group (MCI & NC) Test variables Area Under Curve (95% CI) Age <= 75 with education < 12 years N = 127 SMMSE 0. 65 (0. 54 – 0. 76) LM 0. 72 (0. 62 – 0. 82) Age <= 75 with education > = 12 years N = 449 SMMSE 0. 66 (0. 57 – 0. 75) LM 0. 79 (0. 73 – 0. 86) Age > 75 with education < 12 years N = 71 SMMSE 0. 64 (0. 51 – 0. 77) LM 0. 74 (0. 62 – 0. 85) Age > 75 with education > = 12 years N = 127 SMMSE 0. 55 (0. 44 – 0. 66) LM 0. 79 (0. 71 – 0. 88) SMMSE LM 0. 67 (0. 62 – 0. 72) 0. 80 (0. 76 – 0. 84) Overall
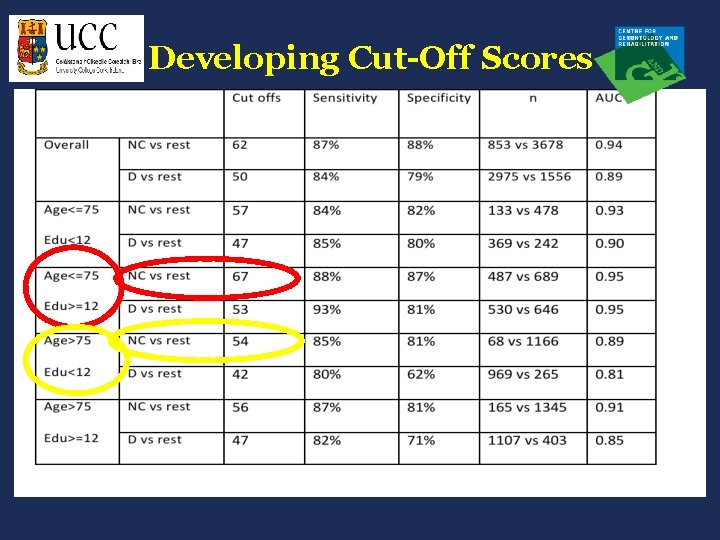
Developing Cut-Off Scores
Developing Cut-Off Scores Large variety of cognitive scores available for any test based upon sensitivity & specificity. Represent “transition points” between different cognitive states. Placing emphasis on cut-offs, rather than profiles of impairment or clinical judgement, can therefore be misleading. Individual variations in age and educational level (Crum et al, JAMA, 1993).
Developing Cut-Off Scores Normal Cognition (NC) Mild Cognitive Impairment (MCI) Dementia (D)
Developing Cut-Off Scores Normal Cognition (NC) Mild Cognitive Impairment (MCI) Dementia (D) CI
Developing Cut-Off Scores Normal Cognition (NC) Mild Cognitive Impairment (MCI) Dementia (D) D
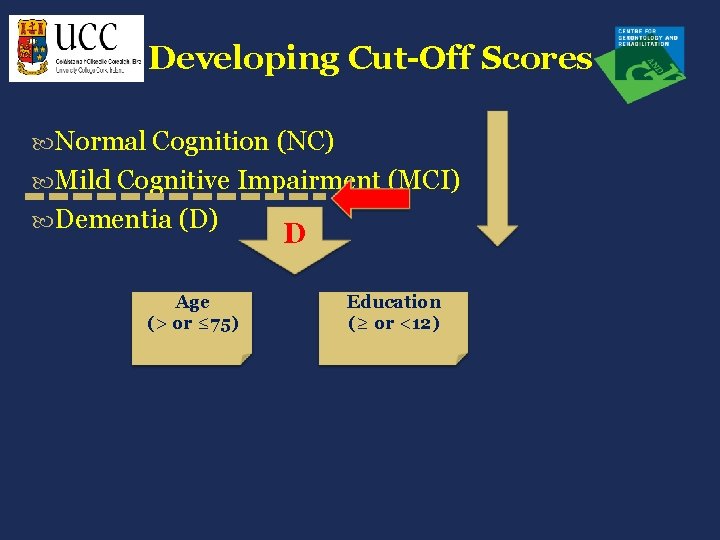
Developing Cut-Off Scores Normal Cognition (NC) Mild Cognitive Impairment (MCI) Dementia (D) Age (> or ≤ 75) D Education (≥ or <12)
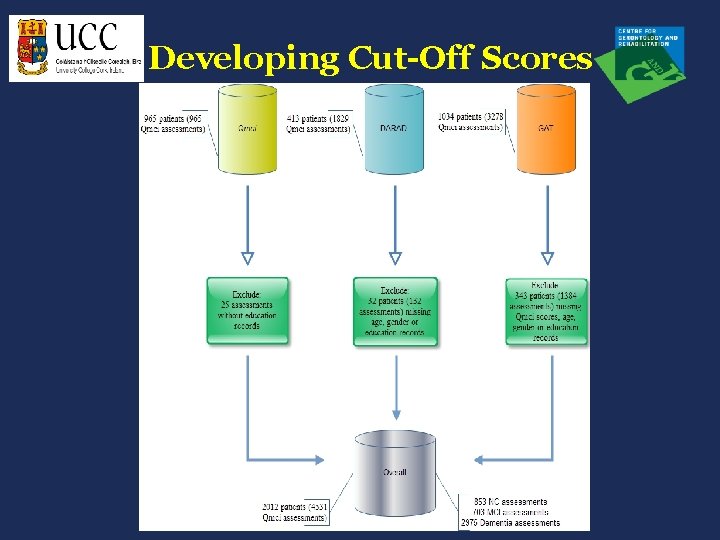
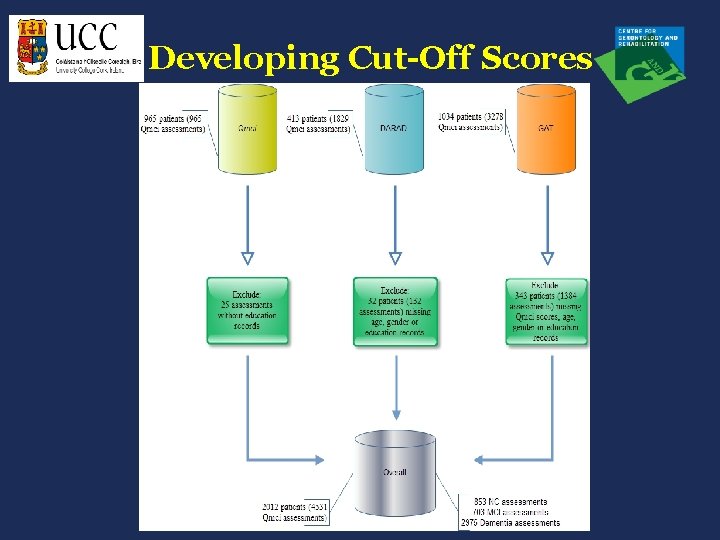
Developing Cut-Off Scores
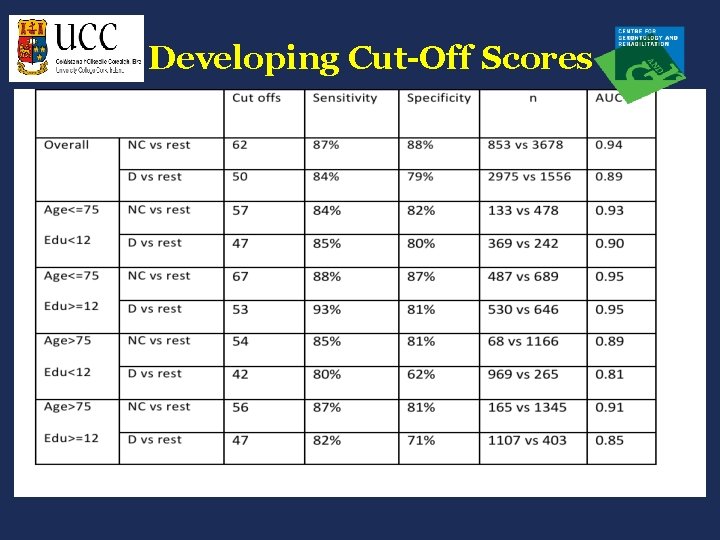
Developing Cut-Off Scores
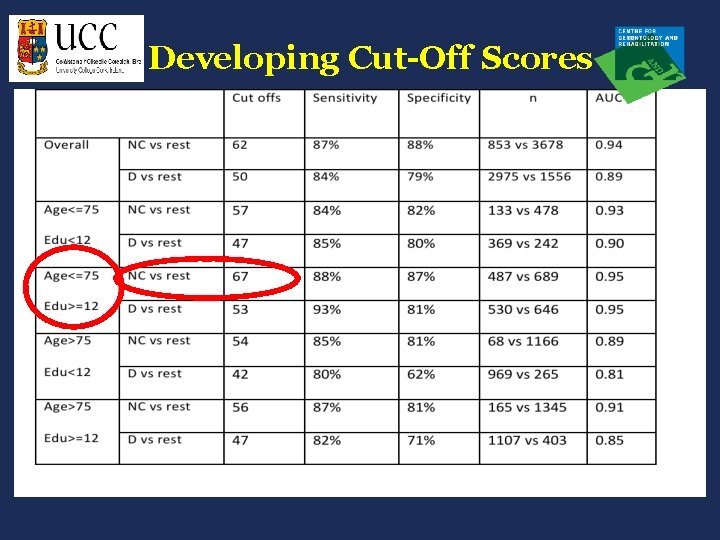
Developing Cut-Off Scores
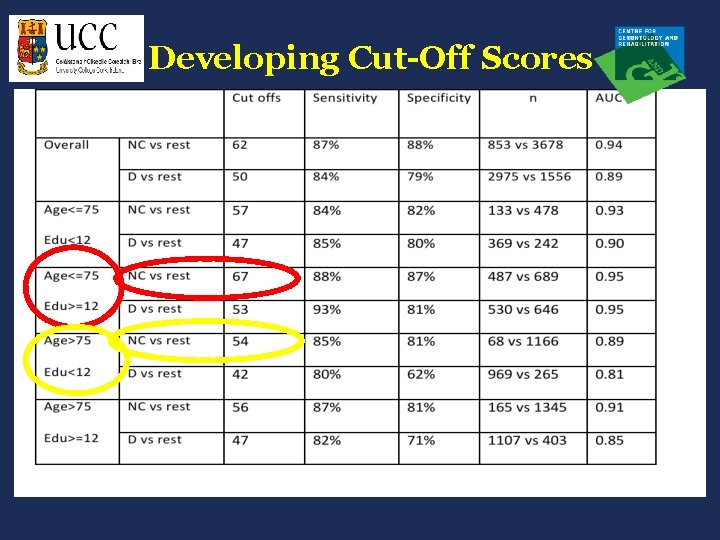
Developing Cut-Off Scores
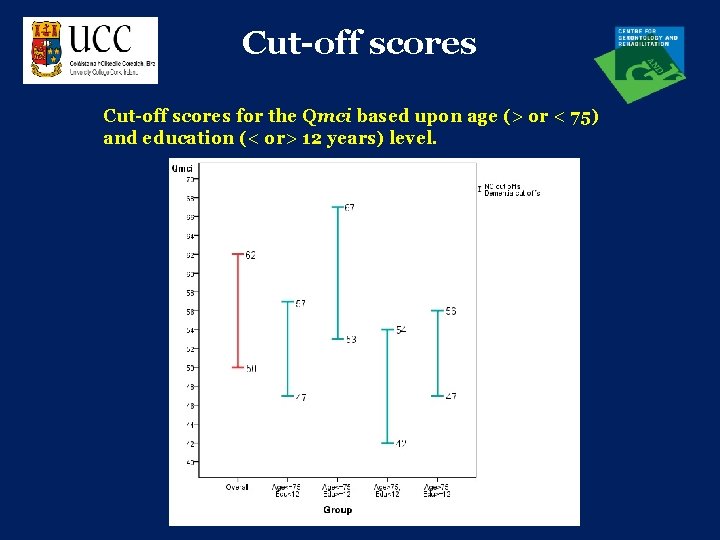
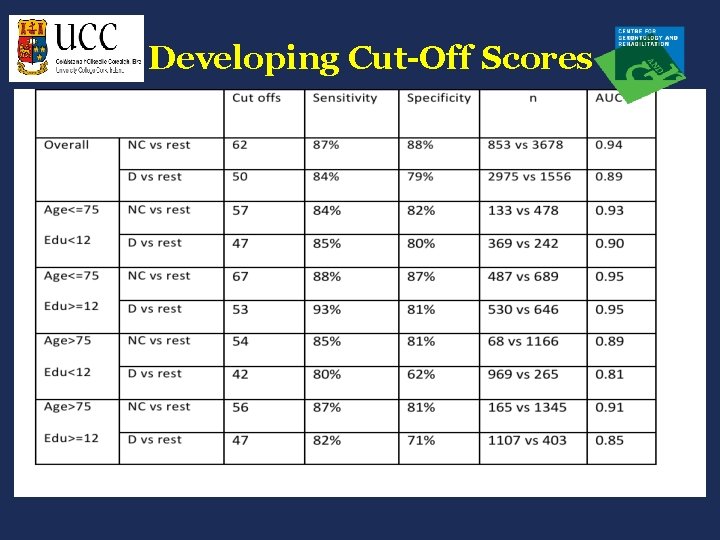
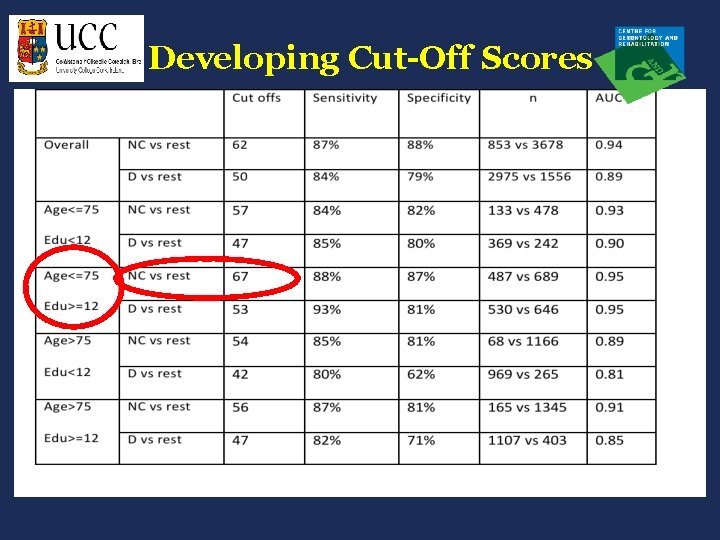
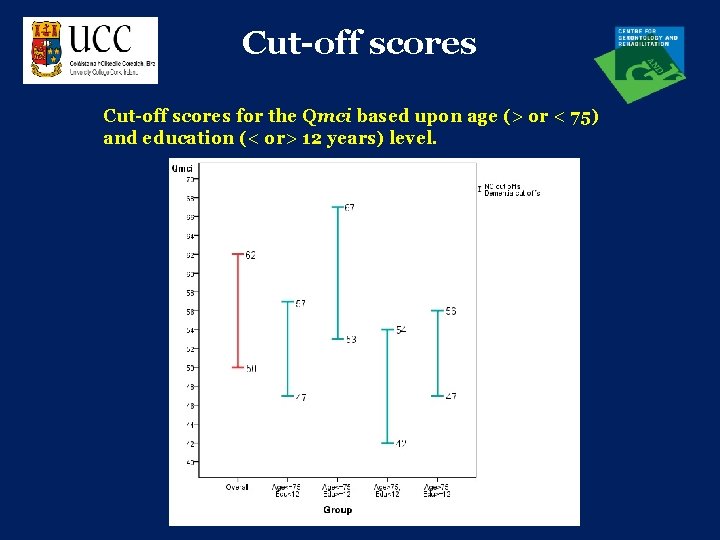
Cut-off scores for the Qmci based upon age (> or < 75) and education (< or> 12 years) level.
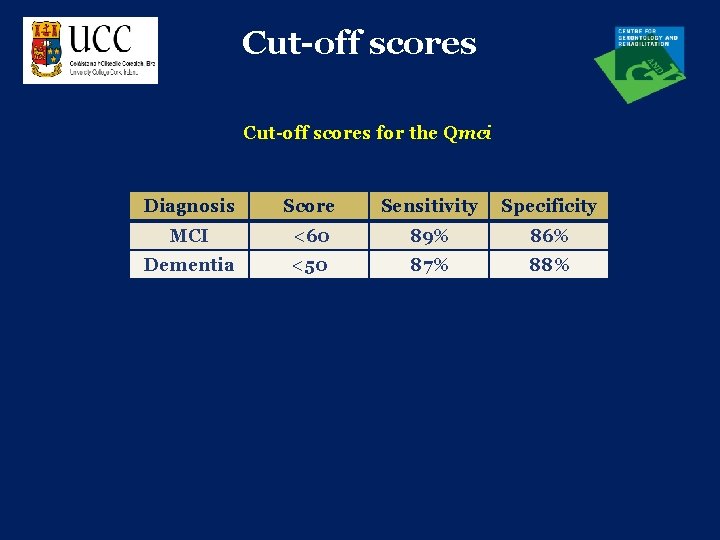
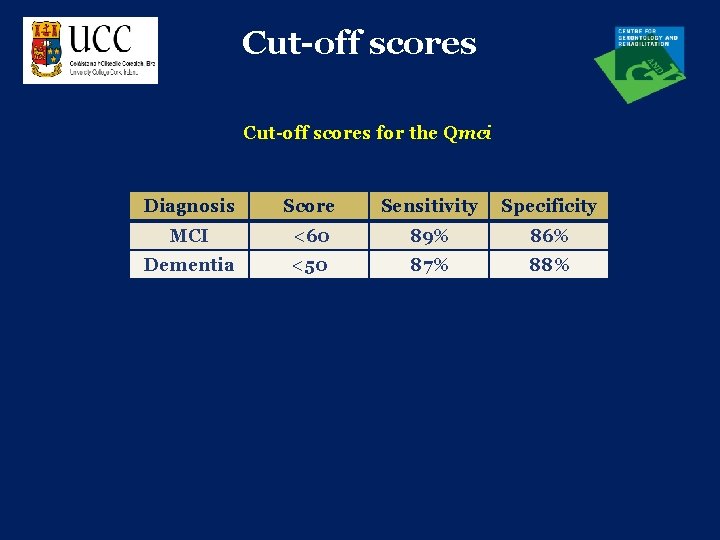
Cut-off scores for the Qmci Diagnosis Score Sensitivity Specificity MCI <60 89% 86% Dementia <50 87% 88%
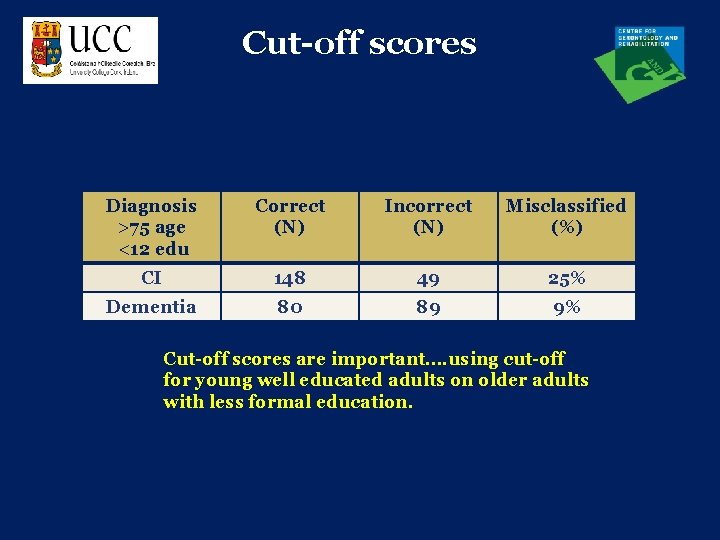
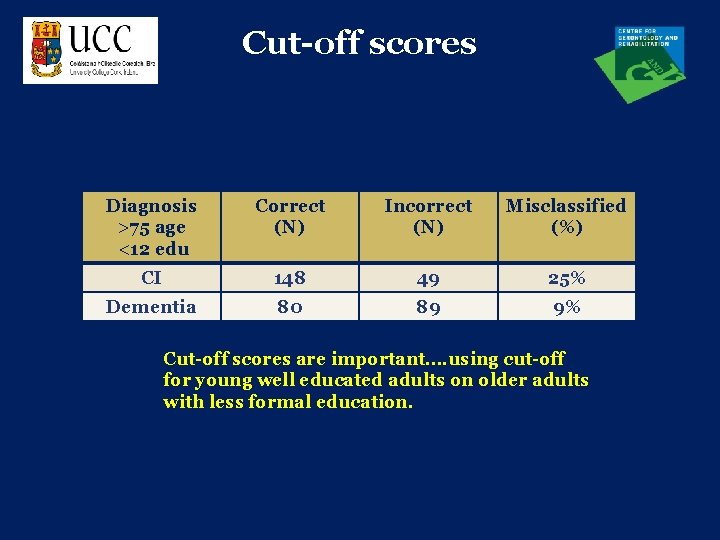
Cut-off scores Diagnosis >75 age <12 edu Correct (N) Incorrect (N) Misclassified (%) CI 148 49 25% Dementia 80 89 9% Cut-off scores are important…. using cut-off for young well educated adults on older adults with less formal education.
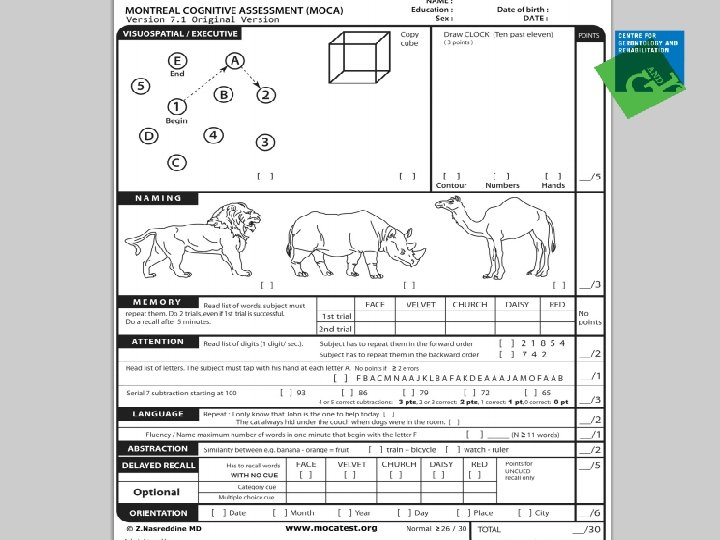
Qmci Vs Mo. CA
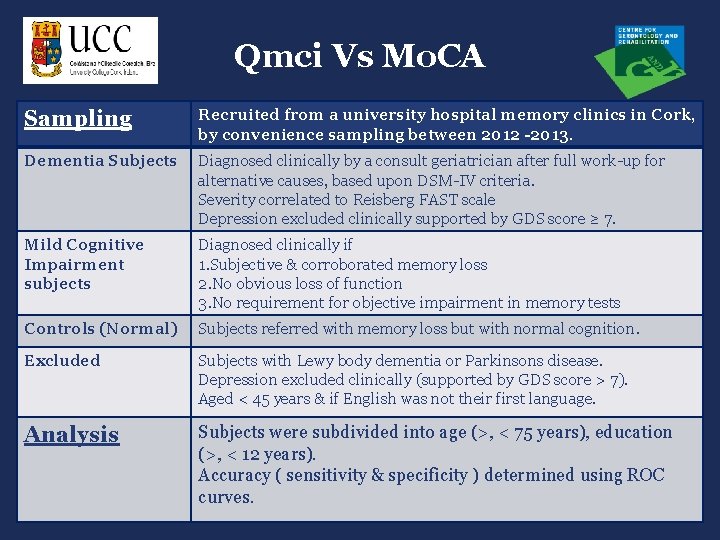
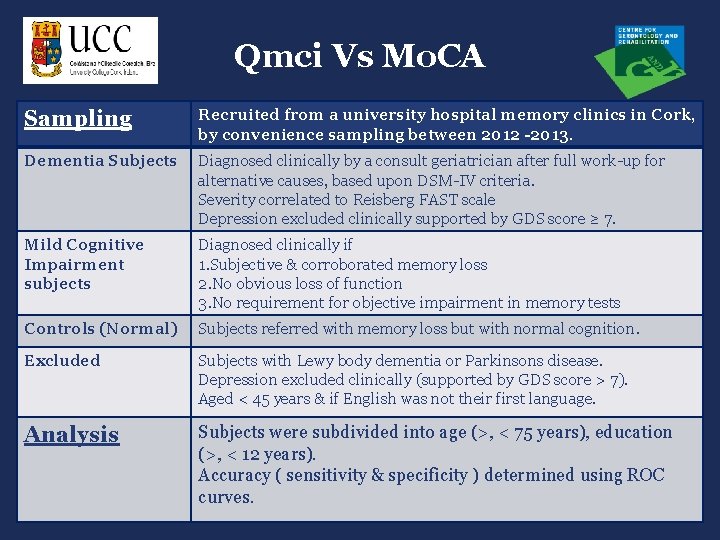
Qmci Vs Mo. CA Sampling Recruited from a university hospital memory clinics in Cork, by convenience sampling between 2012 -2013. Dementia Subjects Diagnosed clinically by a consult geriatrician after full work-up for alternative causes, based upon DSM-IV criteria. Severity correlated to Reisberg FAST scale Depression excluded clinically supported by GDS score ≥ 7. Mild Cognitive Impairment subjects Diagnosed clinically if 1. Subjective & corroborated memory loss 2. No obvious loss of function 3. No requirement for objective impairment in memory tests Controls (Normal) Subjects referred with memory loss but with normal cognition. Excluded Subjects with Lewy body dementia or Parkinsons disease. Depression excluded clinically (supported by GDS score > 7). Aged < 45 years & if English was not their first language. Analysis Subjects were subdivided into age (>, < 75 years), education (>, < 12 years). Accuracy ( sensitivity & specificity ) determined using ROC curves.
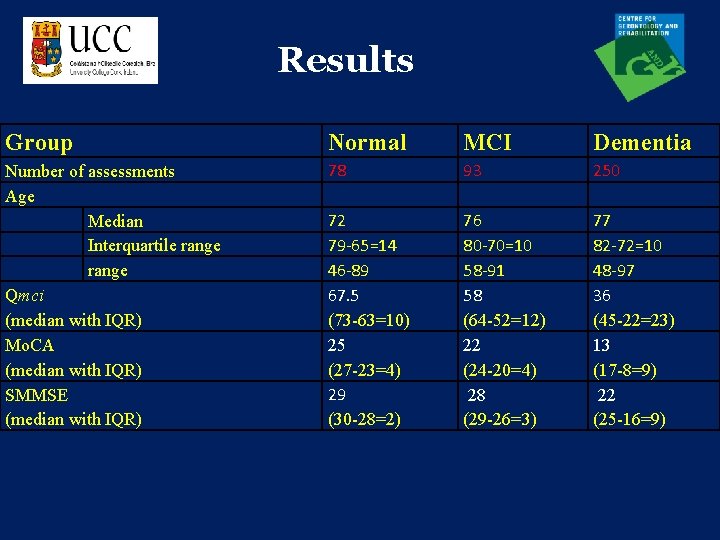
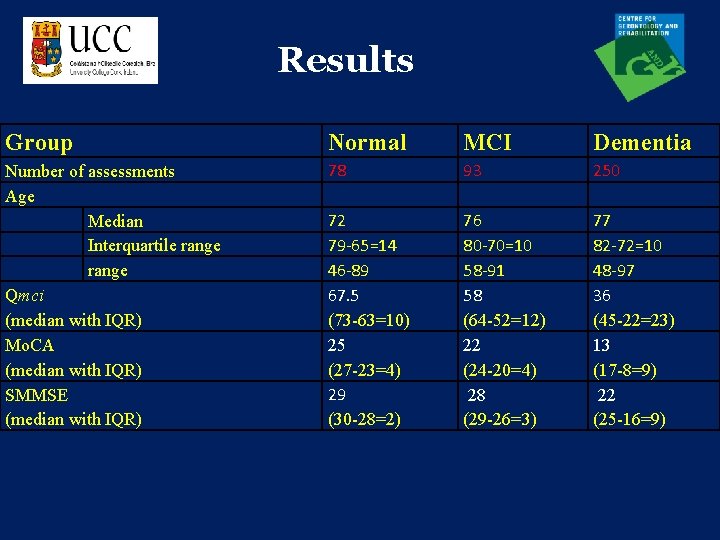
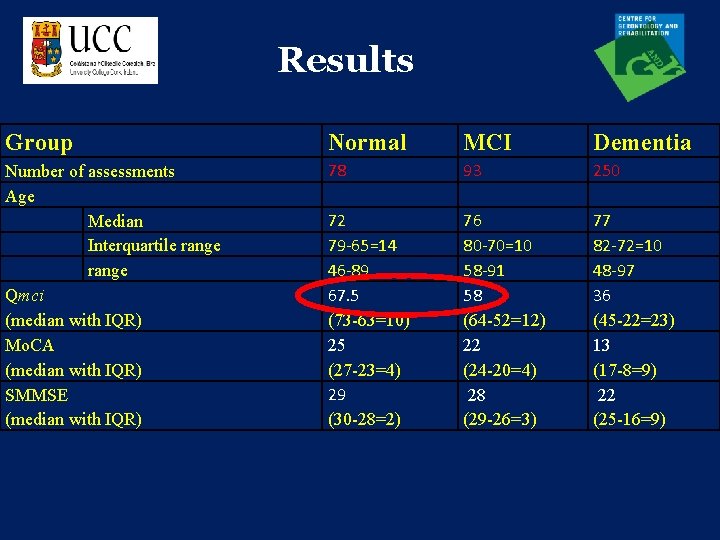
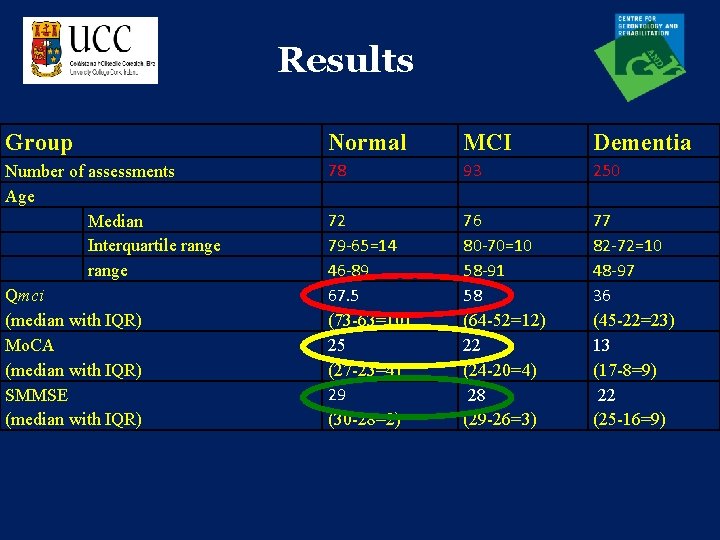
Results Group Normal MCI Dementia Number of assessments Age Median Interquartile range Qmci (median with IQR) Mo. CA (median with IQR) SMMSE (median with IQR) 78 93 250 72 79 -65=14 46 -89 67. 5 (73 -63=10) 25 (27 -23=4) 29 (30 -28=2) 76 80 -70=10 58 -91 58 (64 -52=12) 22 (24 -20=4) 28 (29 -26=3) 77 82 -72=10 48 -97 36 (45 -22=23) 13 (17 -8=9) 22 (25 -16=9)
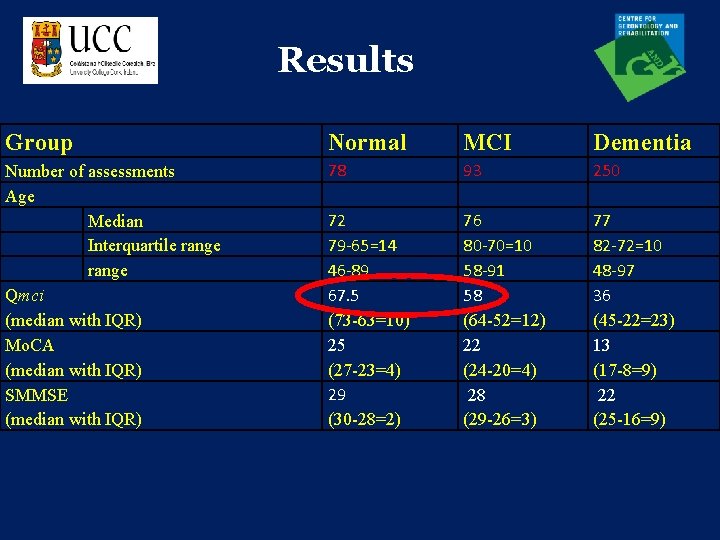
Results Group Normal MCI Dementia Number of assessments Age Median Interquartile range Qmci (median with IQR) Mo. CA (median with IQR) SMMSE (median with IQR) 78 93 250 72 79 -65=14 46 -89 67. 5 (73 -63=10) 25 (27 -23=4) 29 (30 -28=2) 76 80 -70=10 58 -91 58 (64 -52=12) 22 (24 -20=4) 28 (29 -26=3) 77 82 -72=10 48 -97 36 (45 -22=23) 13 (17 -8=9) 22 (25 -16=9)
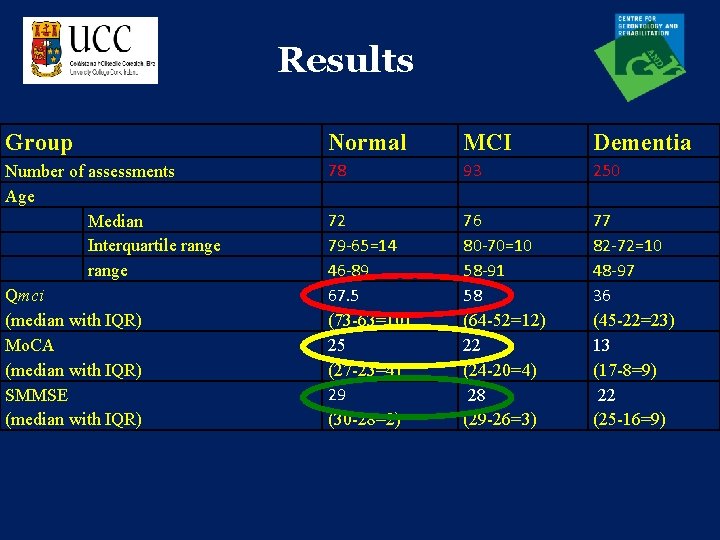
Results Group Normal MCI Dementia Number of assessments Age Median Interquartile range Qmci (median with IQR) Mo. CA (median with IQR) SMMSE (median with IQR) 78 93 250 72 79 -65=14 46 -89 67. 5 (73 -63=10) 25 (27 -23=4) 29 (30 -28=2) 76 80 -70=10 58 -91 58 (64 -52=12) 22 (24 -20=4) 28 (29 -26=3) 77 82 -72=10 48 -97 36 (45 -22=23) 13 (17 -8=9) 22 (25 -16=9)
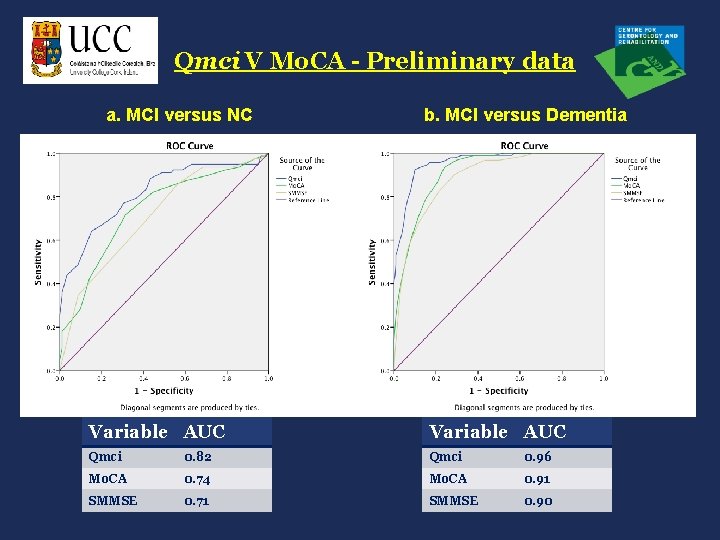
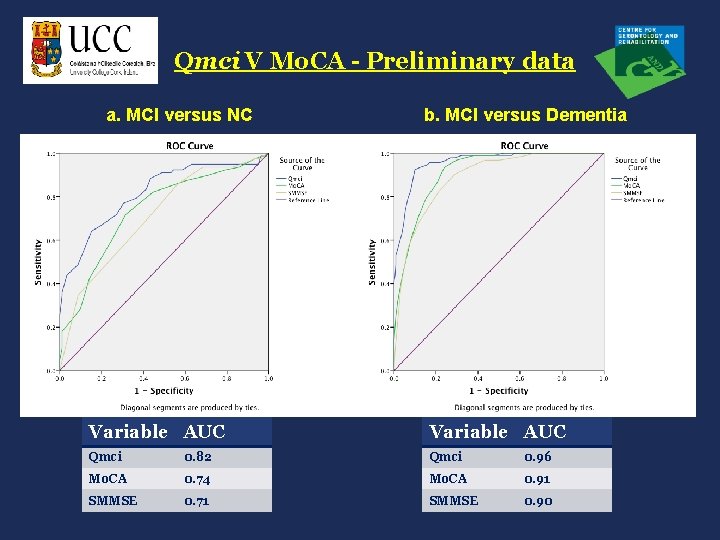
Qmci V Mo. CA - Preliminary data a. MCI versus NC b. MCI versus Dementia Variable AUC Qmci 0. 82 Qmci 0. 96 Mo. CA 0. 74 Mo. CA 0. 91 SMMSE 0. 71 SMMSE 0. 90
Qmci Vs SADAS-cog
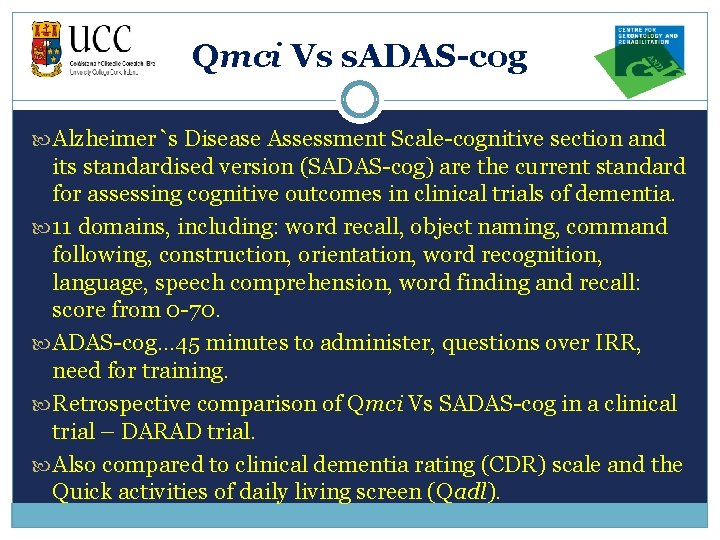
Qmci Vs s. ADAS-cog Alzheimer`s Disease Assessment Scale-cognitive section and its standardised version (SADAS-cog) are the current standard for assessing cognitive outcomes in clinical trials of dementia. 11 domains, including: word recall, object naming, command following, construction, orientation, word recognition, language, speech comprehension, word finding and recall: score from 0 -70. ADAS-cog… 45 minutes to administer, questions over IRR, need for training. Retrospective comparison of Qmci Vs SADAS-cog in a clinical trial – DARAD trial. Also compared to clinical dementia rating (CDR) scale and the Quick activities of daily living screen (Qadl).
Qmci Vs s. ADAS-cog Multicentre randomised clinical trial of 406 patients with mild to moderate Alzheimer’s dementia. Correlations were estimated using regression: - at each time point - all time points - mean values across time
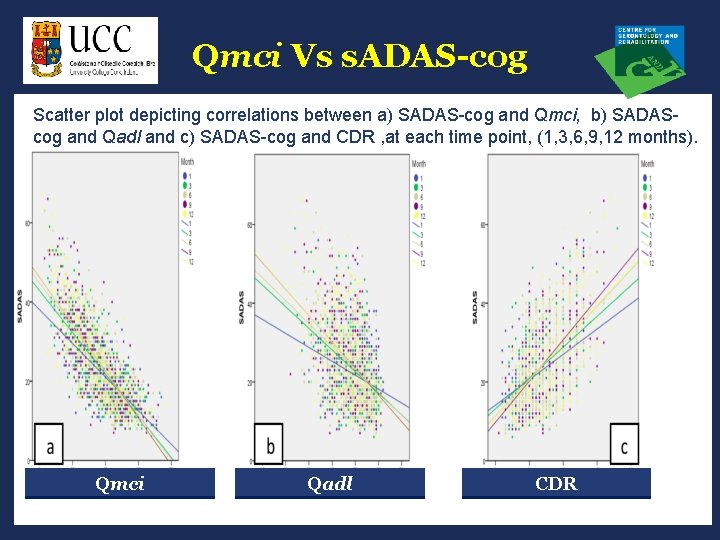
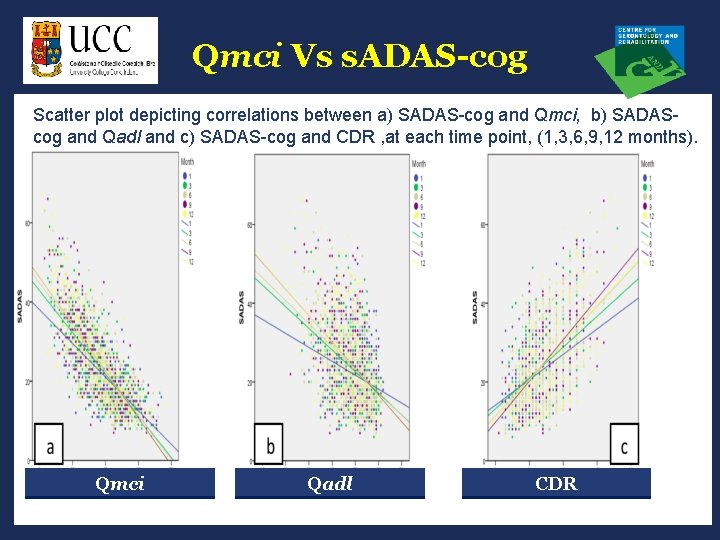
Qmci Vs s. ADAS-cog Scatter plot depicting correlations between a) SADAS-cog and Qmci, b) SADAScog and Qadl and c) SADAS-cog and CDR , at each time point, (1, 3, 6, 9, 12 months). Qmci Qadl CDR
Qmci Vs s. ADAS-cog Strong and significant correlation between the SADAS-cog and Qmci, r=-0. 75, p<0. 001. SADAS-cog and Qmci also correlated (moderate) with CDR and Qadl scores. Qmci correlated strongly with the SADAS-cog and both were equally responsive to deterioration. Qmci could be substituted or used in conjunction with longer tests to allow for more frequent assessment of cognition.
Qmci Summary Qmci more accurately differentiated MCI from NC than the original ABCS 135, the SMMSE & Mo. CA. Ability of the Qmci to identify MCI was better for those over 75 years. It is as accurate as the SMMSE in distinguishing MCI from Dementia (monitoring progression). LM is the best performing subtest for differentiating MCI from NC, irrespective of age or educational status. Orientation was the best performing subtest for identifying/monitoring progression to dementia. QMT (based upon Qmci) is accurate for detecting both MCI and dementia.
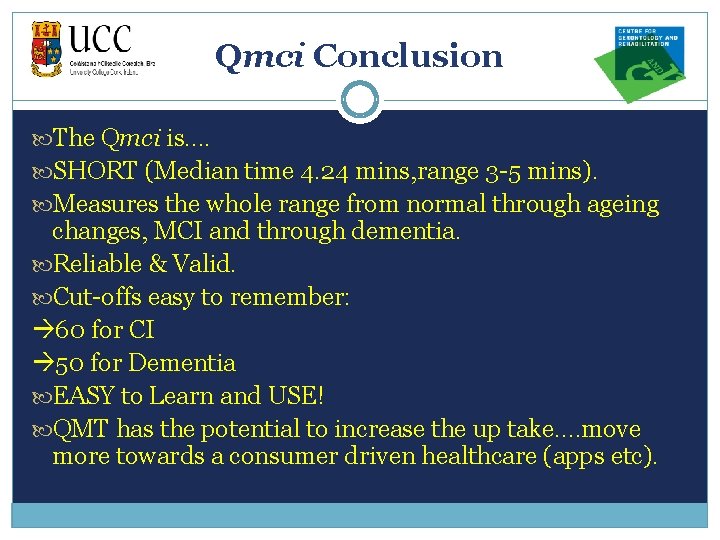
Qmci Conclusion The Qmci is…. SHORT (Median time 4. 24 mins, range 3 -5 mins). Measures the whole range from normal through ageing changes, MCI and through dementia. Reliable & Valid. Cut-offs easy to remember: 60 for CI 50 for Dementia EASY to Learn and USE! QMT has the potential to increase the up take. …move more towards a consumer driven healthcare (apps etc).
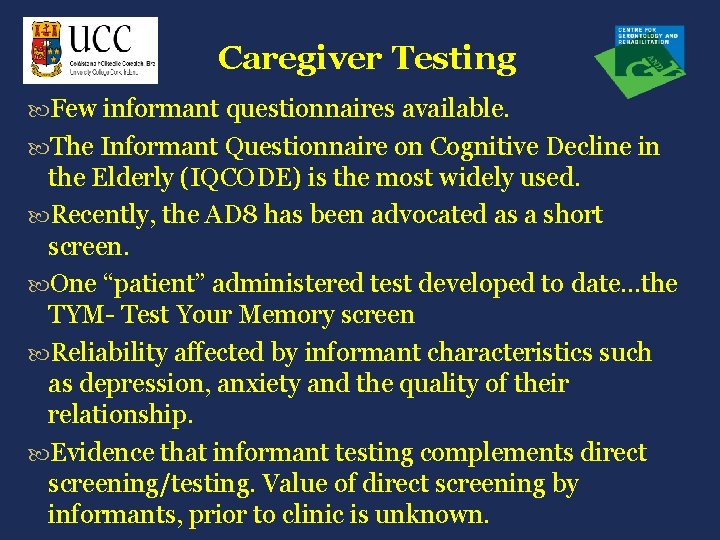
Caregiver Testing Few informant questionnaires available. The Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE) is the most widely used. Recently, the AD 8 has been advocated as a short screen. One “patient” administered test developed to date…the TYM- Test Your Memory screen Reliability affected by informant characteristics such as depression, anxiety and the quality of their relationship. Evidence that informant testing complements direct screening/testing. Value of direct screening by informants, prior to clinic is unknown.
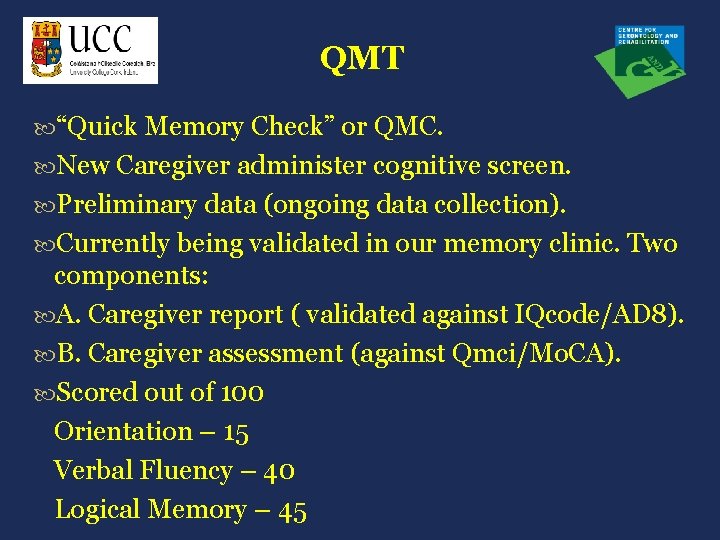
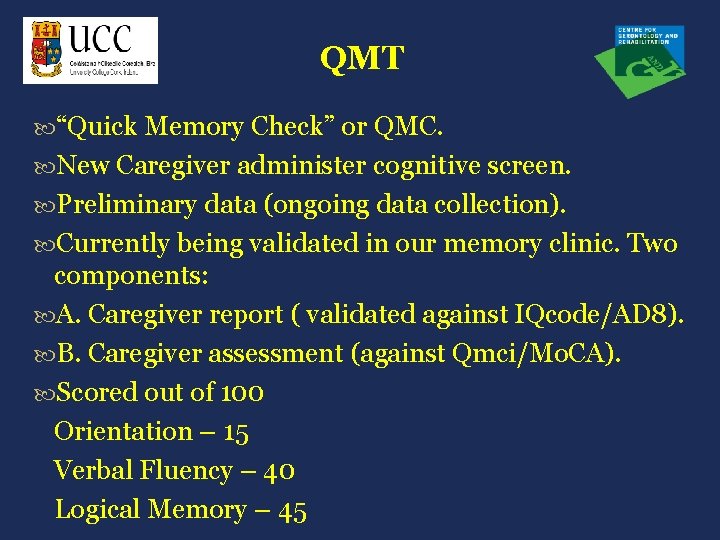
QMT “Quick Memory Check” or QMC. New Caregiver administer cognitive screen. Preliminary data (ongoing data collection). Currently being validated in our memory clinic. Two components: A. Caregiver report ( validated against IQcode/AD 8). B. Caregiver assessment (against Qmci/Mo. CA). Scored out of 100 Orientation – 15 Verbal Fluency – 40 Logical Memory – 45
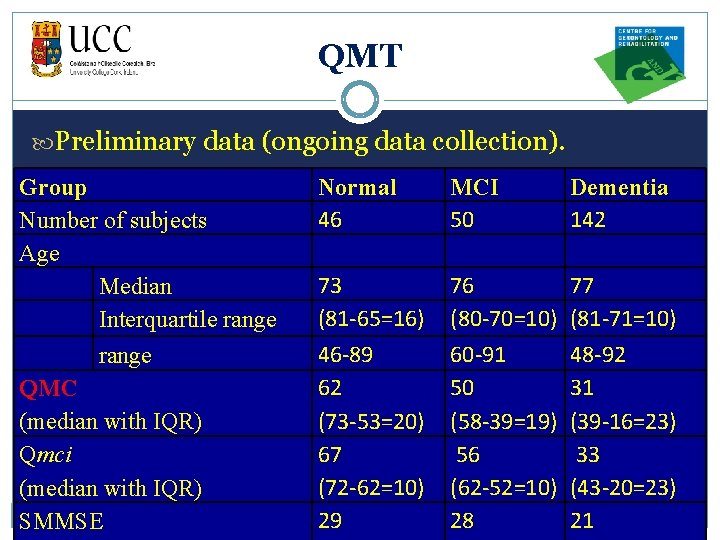
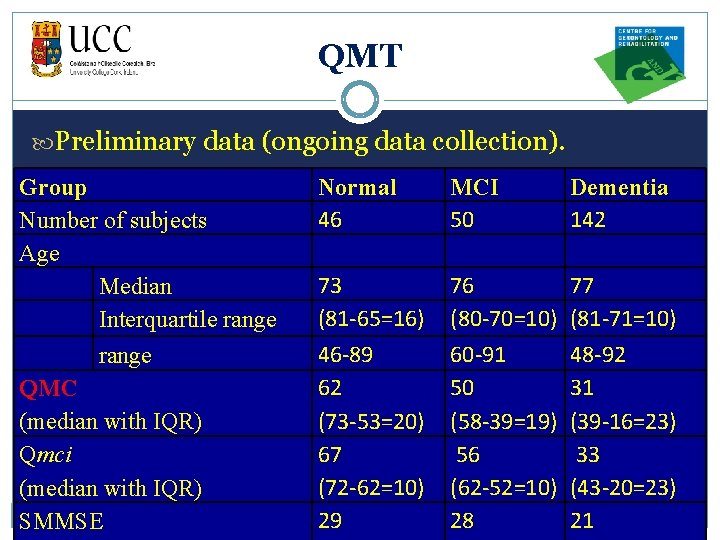
QMT Preliminary data (ongoing data collection). Group Number of subjects Age Median Interquartile range QMC (median with IQR) Qmci (median with IQR) SMMSE Normal 46 MCI 50 Dementia 142 73 (81 -65=16) 46 -89 62 (73 -53=20) 67 (72 -62=10) 29 76 (80 -70=10) 60 -91 50 (58 -39=19) 56 (62 -52=10) 28 77 (81 -71=10) 48 -92 31 (39 -16=23) 33 (43 -20=23) 21
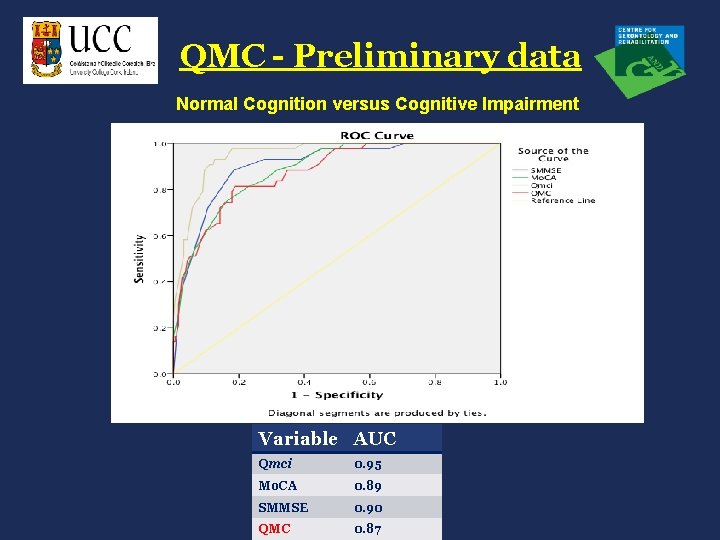
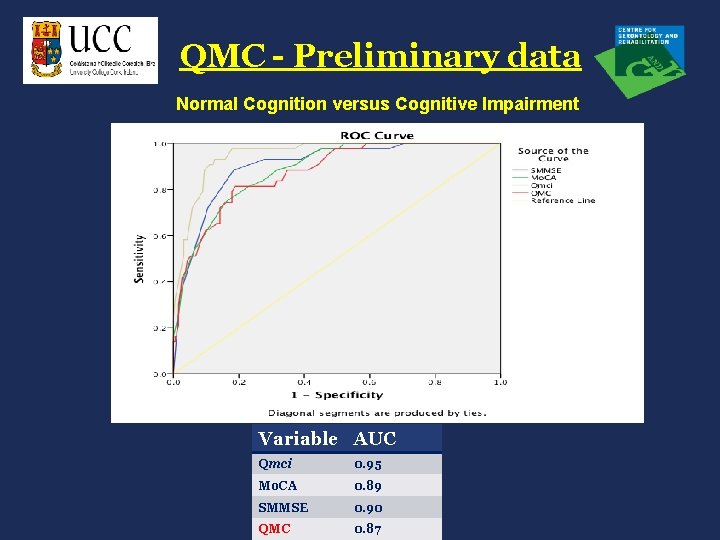
QMC - Preliminary data Normal Cognition versus Cognitive Impairment Variable AUC Qmci 0. 95 Mo. CA 0. 89 SMMSE 0. 90 QMC 0. 87
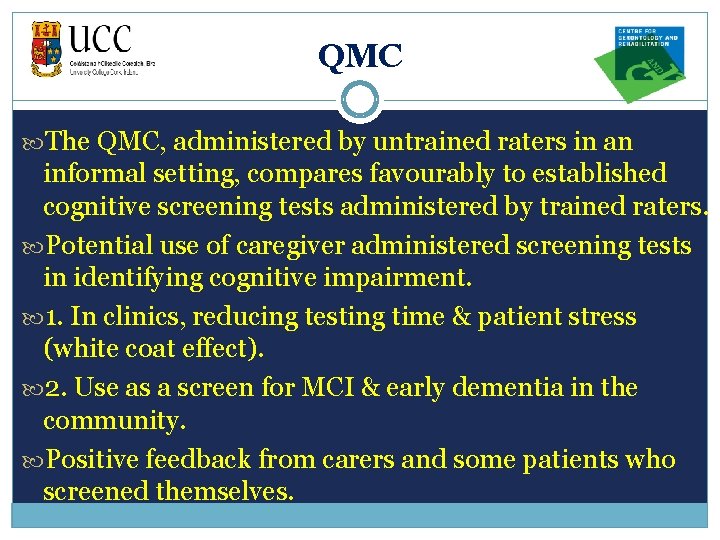
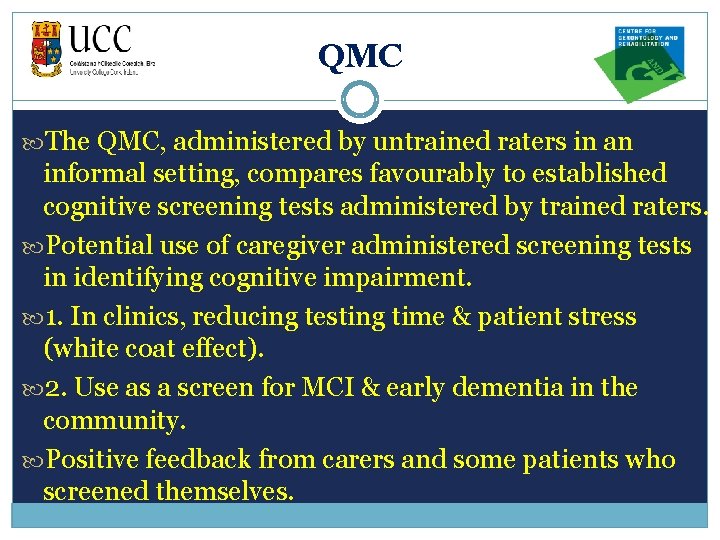
QMC The QMC, administered by untrained raters in an informal setting, compares favourably to established cognitive screening tests administered by trained raters. Potential use of caregiver administered screening tests in identifying cognitive impairment. 1. In clinics, reducing testing time & patient stress (white coat effect). 2. Use as a screen for MCI & early dementia in the community. Positive feedback from carers and some patients who screened themselves.
Community Screening programmes for detecting CI are advocated (Boustani 2003). Limited evidence supporting routine screening in clinical practice (Boustani 2005). Insufficient evidence for sensitive and specific cognitive tests to differentiate between normal cognition (NC), MCI and dementia (Winblad 2004, Boustani 2005).
i l RAPCOG Pathway y / Commu c nity a Screenin g r e g Caregi i ver v. GC Qiveognit uick e. P RS ild creen r em s fcogniti ve e rimpair ment r(Qmci Cork a ) Memor lscreen y Clinic
i l y Pathway RAPCOG / Comm c unity a Screeni ng r e Care g giver Cuick og i. GQ nitive v. Pm ild e Scre en ognitive rc R siempairme f nt e(Q r. Cork mci r Mem a) ory lscreen Clinic
RAPCOG Pilot study, screening 700 older adults, will being in July 2013. RAPCOG has the potential to improve integration between the general public, primary & secondary care. Qmci is now translated and being validated in several different languages Qmci-P (Portuguese) Qmci-D (Dutch) Qmci-T (Turkish) Qmci-G (German) Qmci-PL (Polish)
RAPCOG Need to develop a stronger evidence base for early diagnosis AND treatment. Screening people in the community for decline in cognition and function is a delicate matter and not everyone will be amenable to it. Improving knowledge & reducing stigma will help. See: www. ucc. ie/alzcafe
Conclusion There is a need to diagnose MCI early. We need to study the natural history of this disease more to understand it better. We need better, shorter instruments to detect it and to measure change over time in the clinic and in General practice. Qmci may be that instrument. Ongoing research: -examining its performance in GP, (IRR & Validity). -use in the community to rapidly screen and triage those with CI. -IRR and Validity of Qmci App. -Comparison of QMT (caregiver report to Iqcode & AD 8). RAPCOG: The Rapid Community Cognitive Screening program.

Thank you QUESTIONS? HTTP: //WWW. HSELAND. IE/COURSEFILES/PACKAGES/ OPENBROOKES_FS 12/PLAYER. HTML
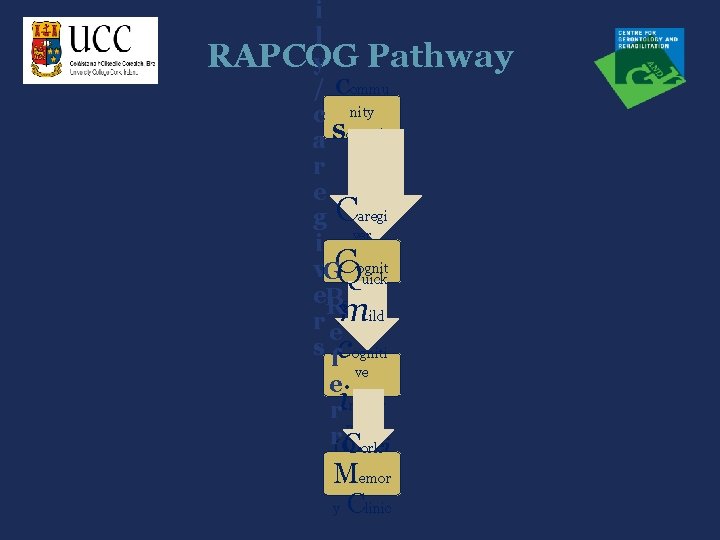
i l RAPCOG Pathway y / Commu c nity a Screenin g r e g Caregi i ver v. GC Qiveognit uick e. P RS ild creen r em s fcogniti ve e rimpair ment r(Qmci Cork a ) Memor lscreen y Clinic