THE POSTERIOR PITUITARY GLAND The posterior pituitary gland

- Slides: 33
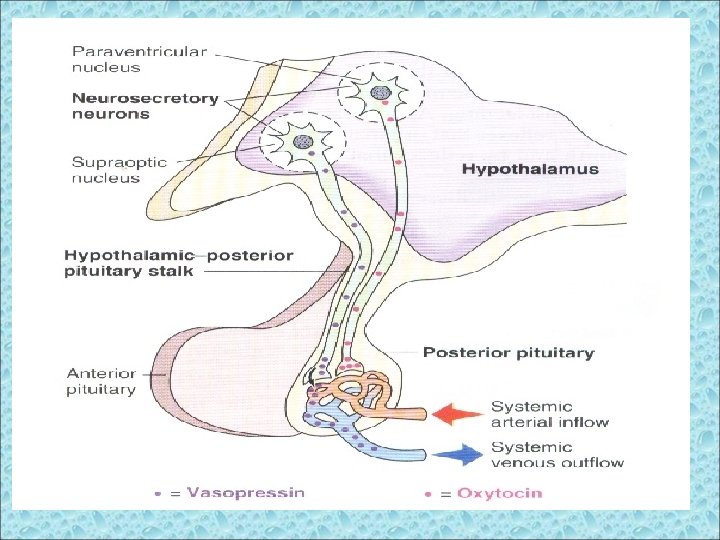
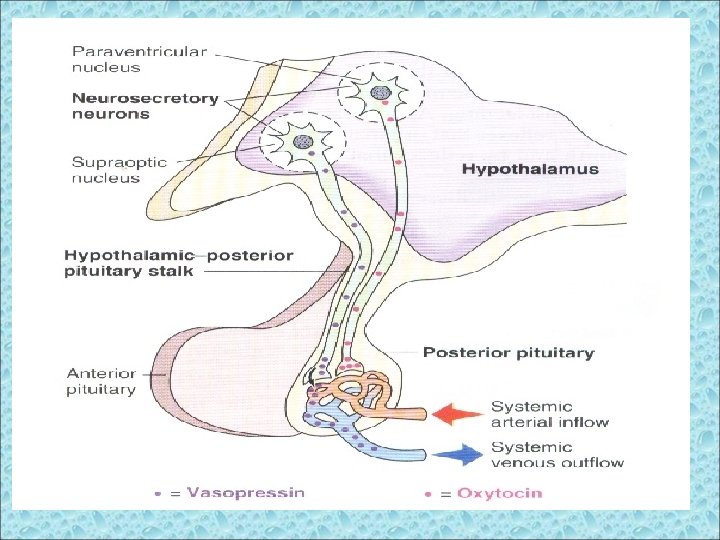
THE POSTERIOR PITUITARY GLAND The posterior pituitary gland, also called neurohypophysis, is composed mainly of glial-like supporting cells called pituicytes. These do not produce hormone but receive terminal nerve endings of large magnocellular neurons that originate in the hypothalamus.
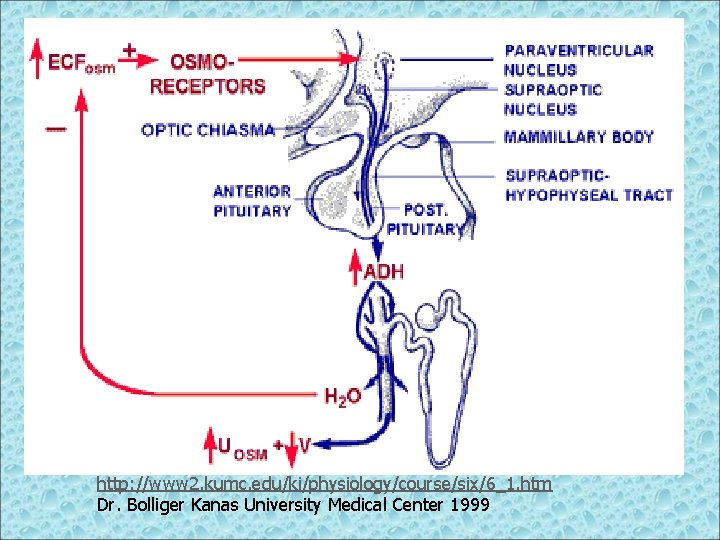
The posterior pituitary gland hormones § Posterior pituitary gland releases 2 hormones: 1. Antidiuretic hormone (ADH), or arginine vasopressin (AVP). 2. Oxytocin § Both hormones are produced in hypothalamic nuclei: - Supraoptic nucleus (ADH + 1/6 oxytocin) - Paraventricular nucleus (Oxytocin + 1/6 ADH)
The posterior pituitary hormones – 1. ADH (vasopressin): § ADH activates (2) second messenger systems: 1. c. AMP 2. IP 3/Ca 2+
Nerve tracts originate in the supraoptic and paraventricular nuclei of the hypothalamus. These tracts pass to the neurohypophysis through the pituitary or hypophyseal stalk. The nerve endings are bulbous knobs that contain many secretory granules called herring bodies. These endings lie on the surfaces of the capillaries onto which they secrete two posterior pituitary hormones 1) Antidiuretic hormone (ADH) or vasopressin 2) Oxytocin
Vasopressin and oxytocin, each has a characteristic binding polypeptide called neurophysin associated with it, in the granules of the neurons that secrete them. These are thought to be: Neurophysin I carries oxytocin and Neurophysin II carries vasopressin.
When nerve impulses are transmitted downward along the fibers, the hormone is released from the secretory granules by Ca-dependant exocytosis and is absorbed into adjacent capillaries. As hormone is loosely bound to neurophysin, it immediately separates while neurophysin has no known functions afterwards.
VASOPRESSIN RECEPTORS VIA, VIB and V 2. All are G protein-coupled. The VIA and VIB act through phosphotidylinositol hydrolysis to increase the intracellular Ca conc. The V 2 act through c-AMP formation.
Location V 2 ---- in the luminal membranes of renal collecting duct system VIA---- in the vascular smooth muscle, liver and brain
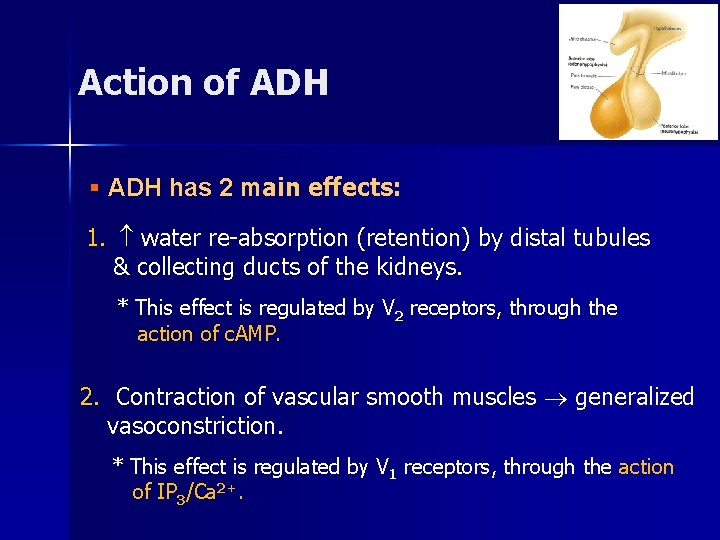
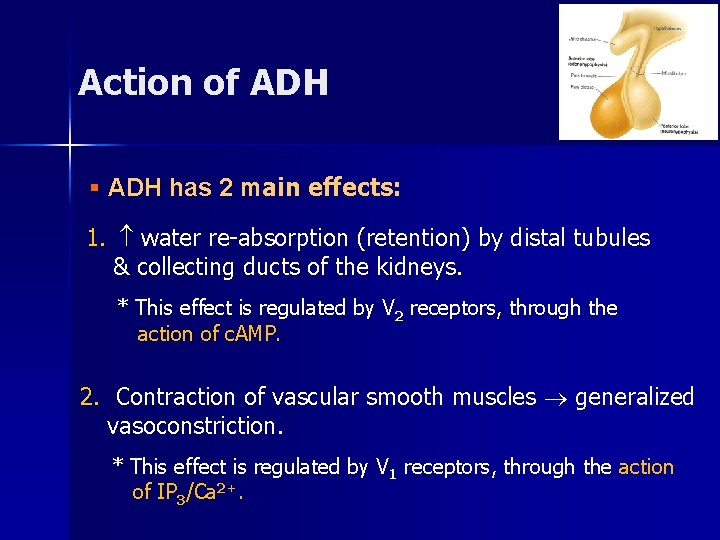
Action of ADH § ADH has 2 main effects: 1. water re-absorption (retention) by distal tubules & collecting ducts of the kidneys. * This effect is regulated by V 2 receptors, through the action of c. AMP. 2. Contraction of vascular smooth muscles generalized vasoconstriction. * This effect is regulated by V 1 receptors, through the action of IP 3/Ca 2+.
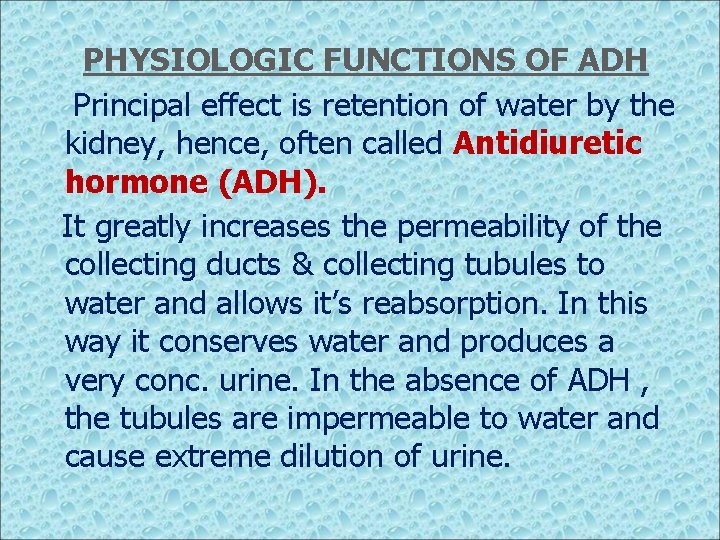
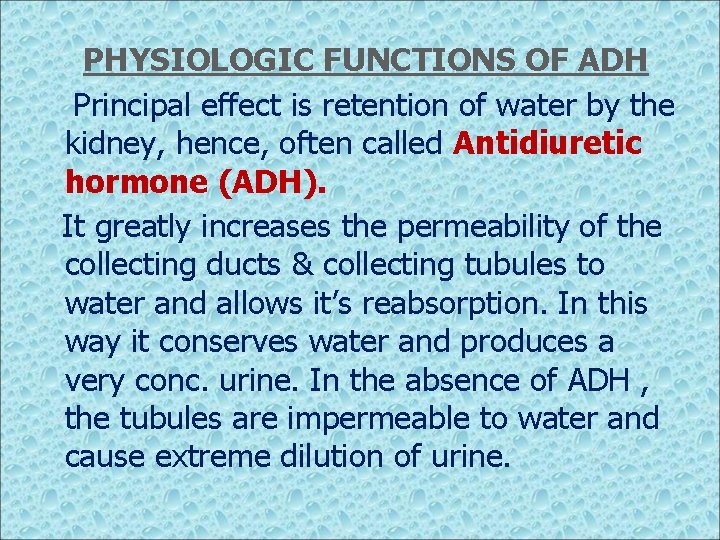
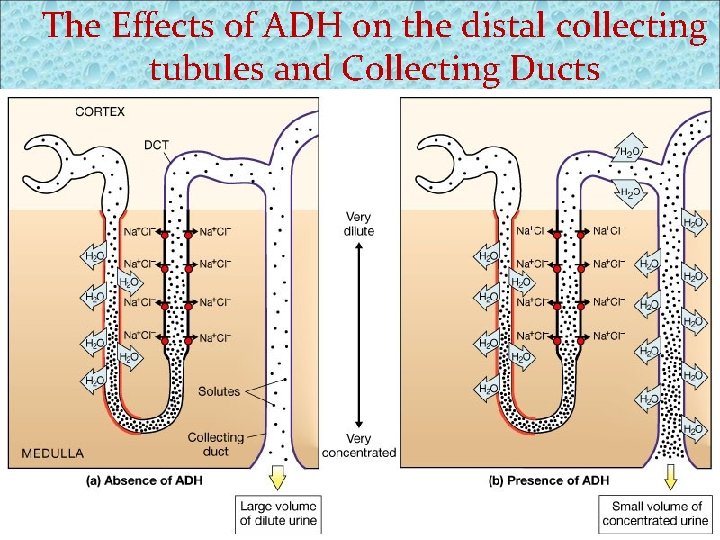
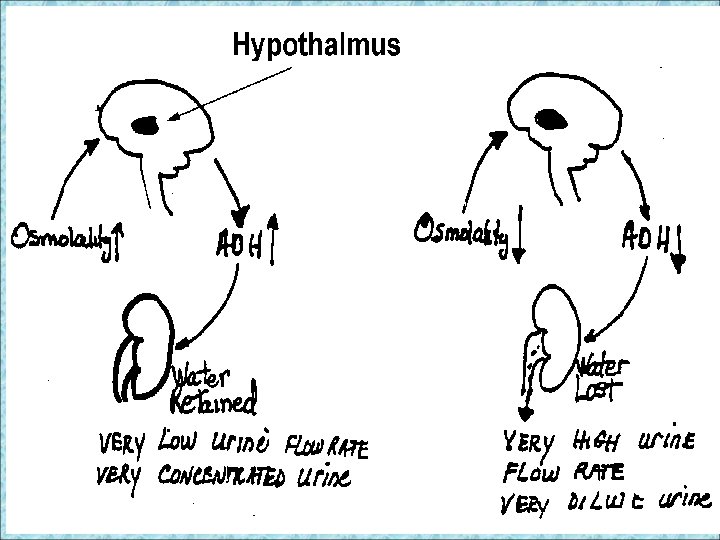
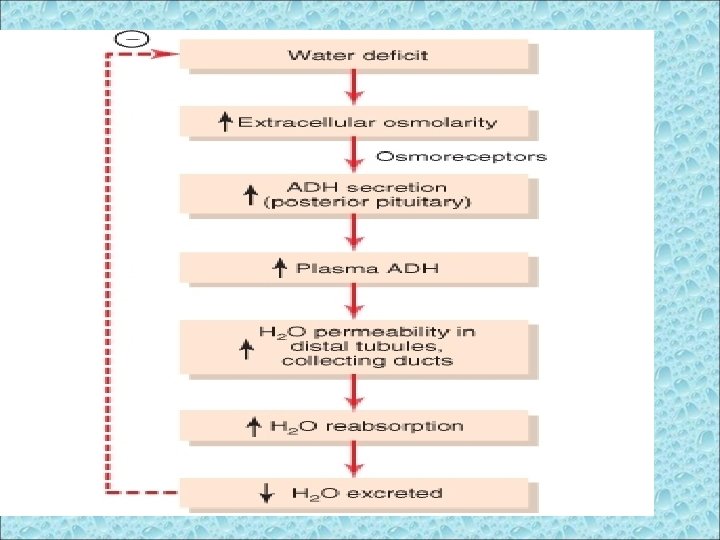
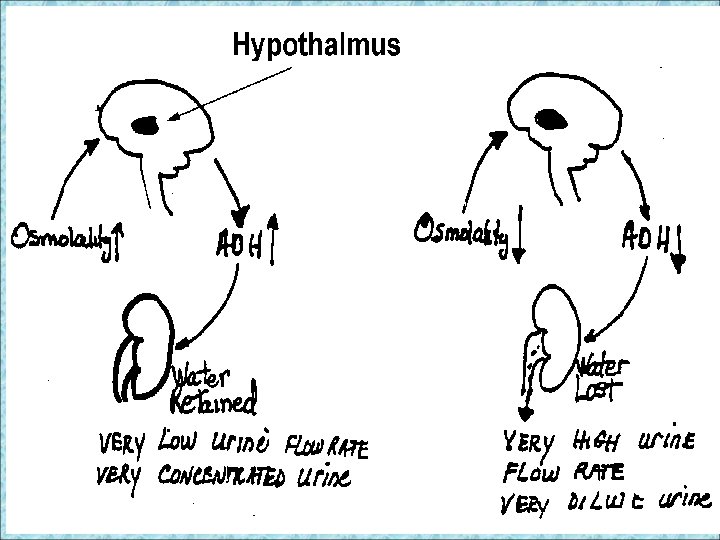
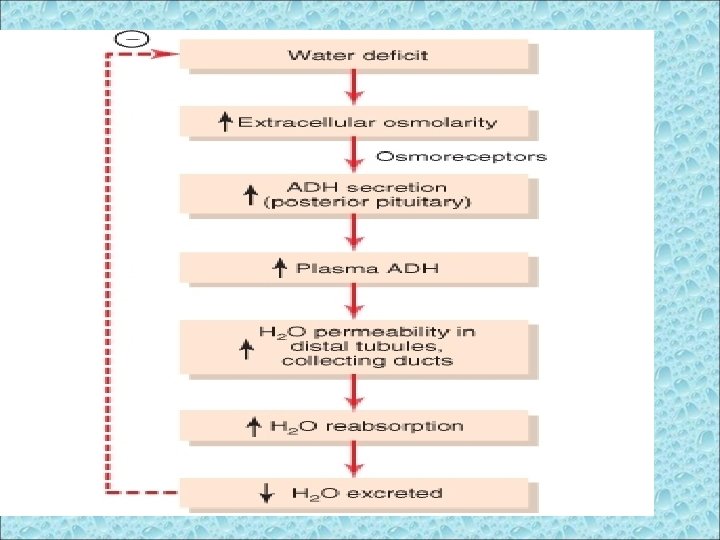
PHYSIOLOGIC FUNCTIONS OF ADH Principal effect is retention of water by the kidney, hence, often called Antidiuretic hormone (ADH). It greatly increases the permeability of the collecting ducts & collecting tubules to water and allows it’s reabsorption. In this way it conserves water and produces a very conc. urine. In the absence of ADH , the tubules are impermeable to water and cause extreme dilution of urine.
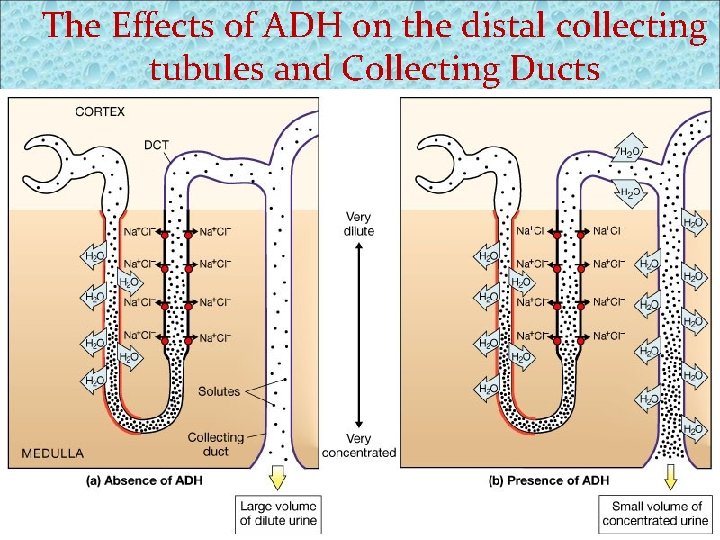
The Effects of ADH on the distal collecting tubules and Collecting Ducts Figure 26. 15 a, b
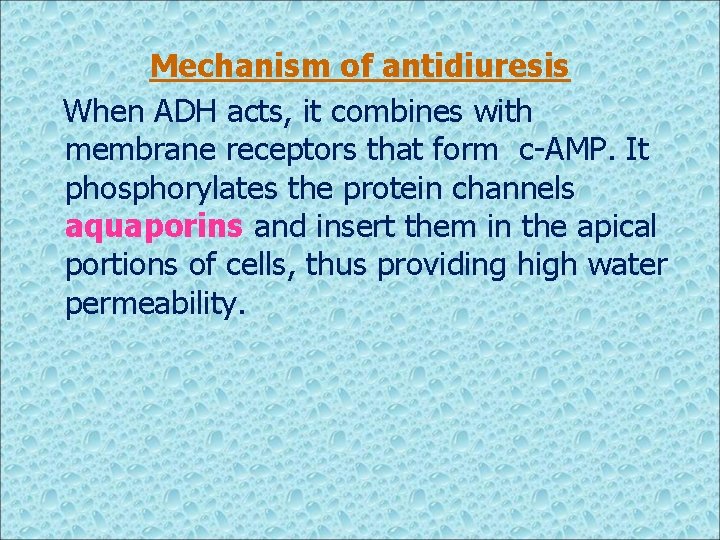
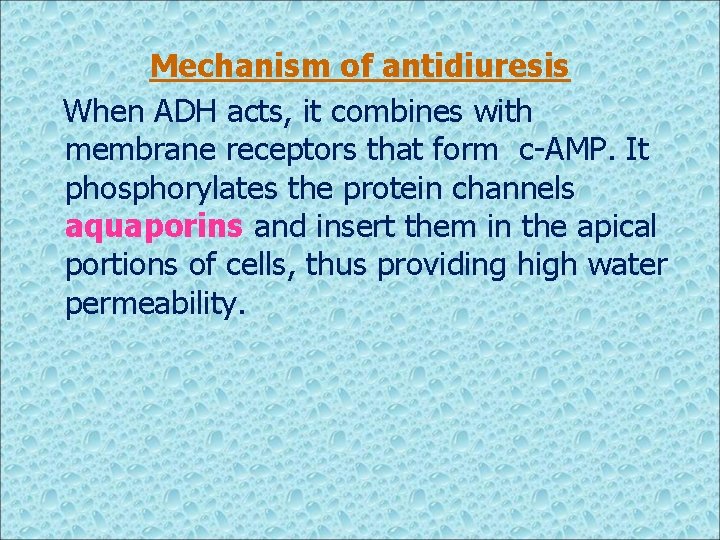
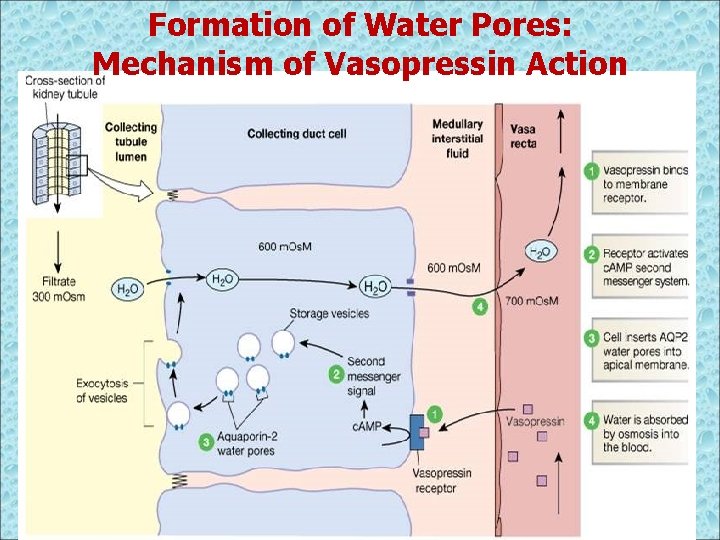
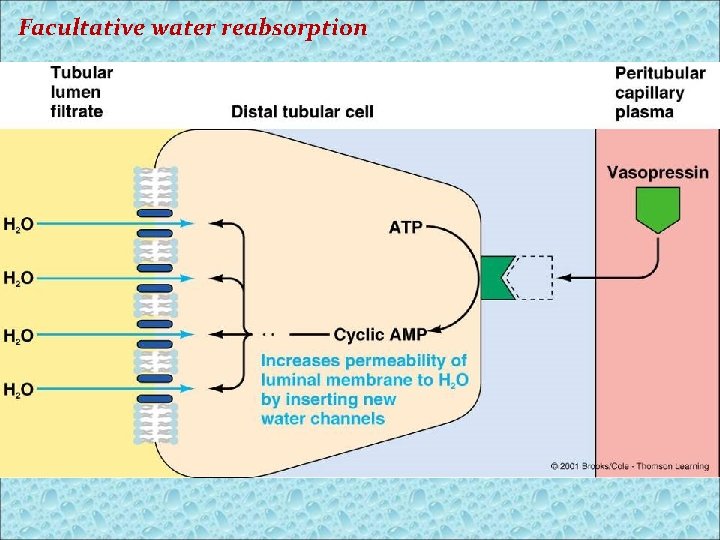
Mechanism of antidiuresis When ADH acts, it combines with membrane receptors that form c-AMP. It phosphorylates the protein channels aquaporins and insert them in the apical portions of cells, thus providing high water permeability.
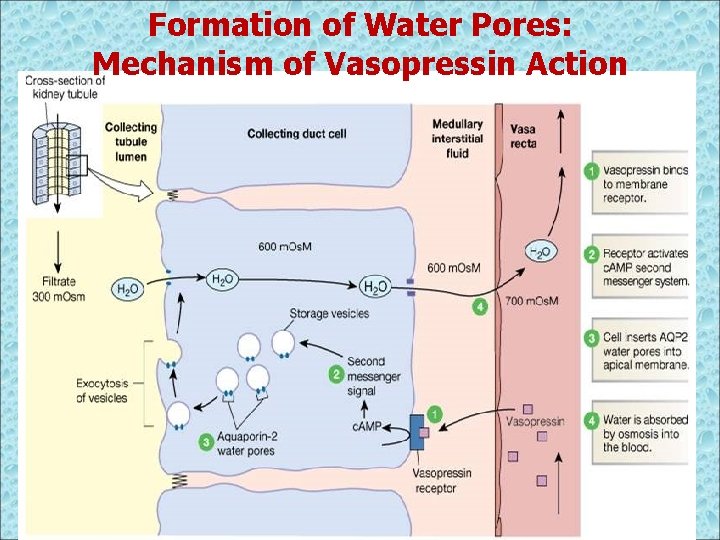
Formation of Water Pores: Mechanism of Vasopressin Action
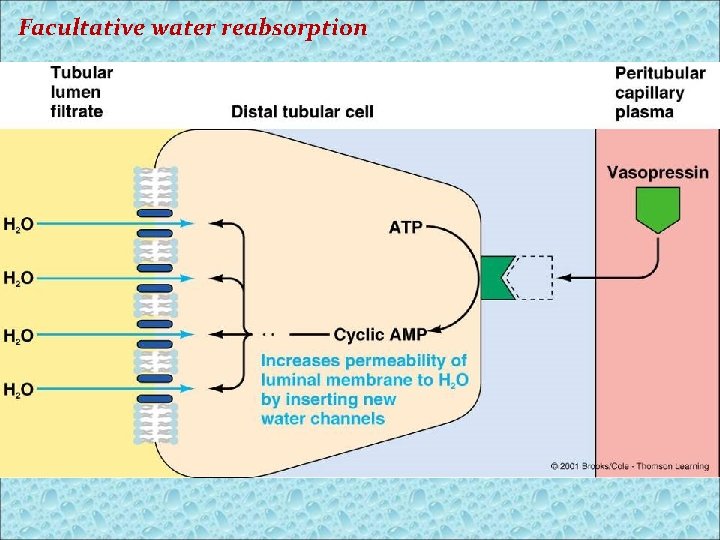
Facultative water reabsorption
All this occurs in 5 to 10 minutes. Movement of water is by simple diffusion. At least 5 types of aquaporins have been identified. 1, 2 &3 are found in the kidneys, 4 is found in the brain and 5 is found in the salivary and lacrimal glands and in the resp. tract.
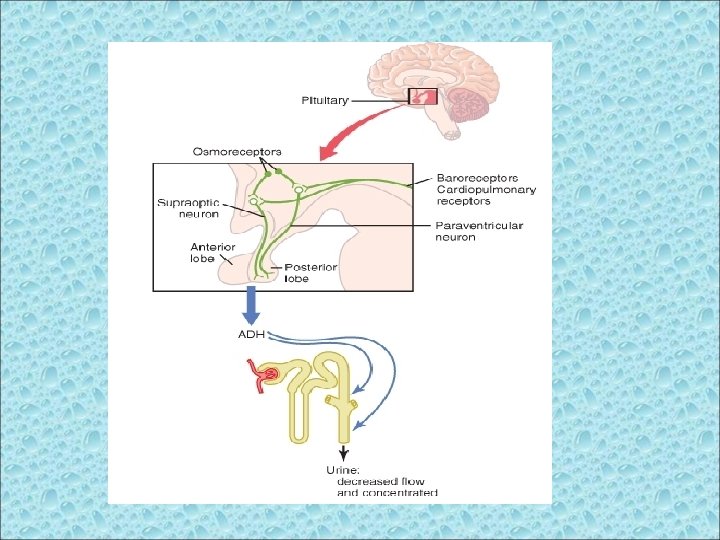
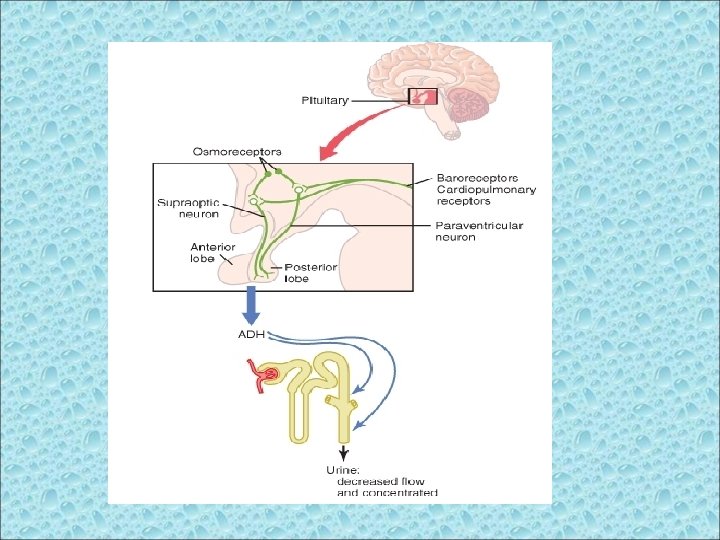
REGULATION OF ADH Near the hypothalamus are modified neuron receptors called osmoreceptors. When the ECF becomes too conc. , fluid is pulled by osmosis out of the osmoreceptor cell decreasing it’s size and sending signal to the hypothalamus to secrete ADH. Vice versa.
A second neuronal area important in controlling osmolarity and ADH secretion is located along the anteroventral region of the third ventricle, called the AV 3 V region. At the upper part of this region is a structure called the subfornical organ, and at the inferior part is another structure called the organum vasculosum of the lamina terminalis (OVLT). Between these two organs is the median preoptic nucleus, which has multiple nerve connections with the two organs as well as with the supraoptic nuclei and the blood pressure control centers in the medulla of the brain.
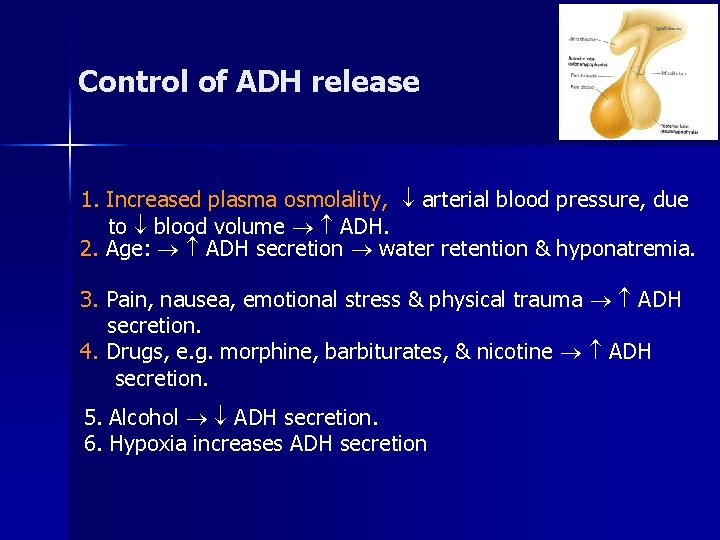
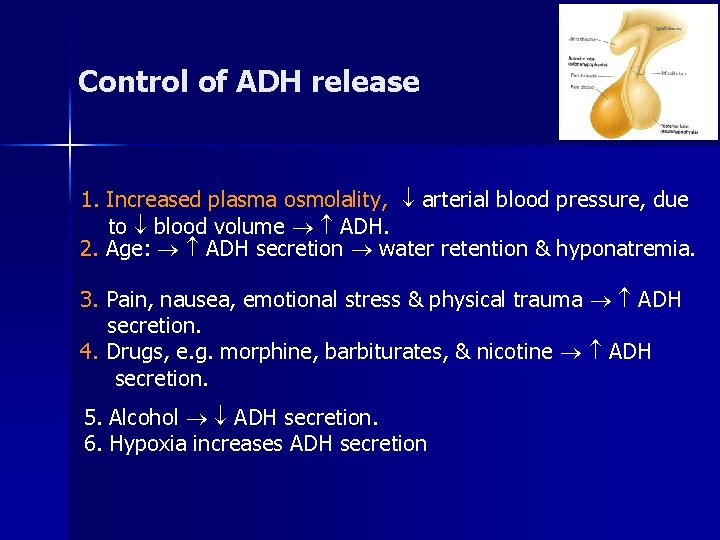
Control of ADH release 1. Increased plasma osmolality, arterial blood pressure, due to blood volume ADH. 2. Age: ADH secretion water retention & hyponatremia. 3. Pain, nausea, emotional stress & physical trauma ADH secretion. 4. Drugs, e. g. morphine, barbiturates, & nicotine ADH secretion. 5. Alcohol ADH secretion. 6. Hypoxia increases ADH secretion
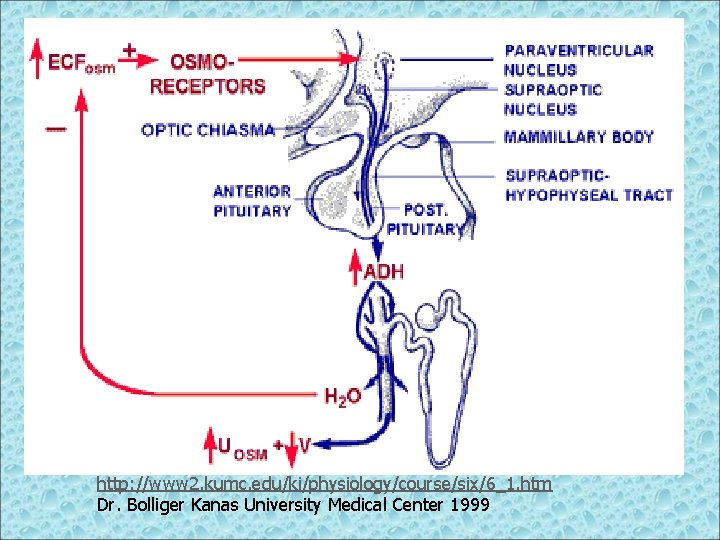
http: //www 2. kumc. edu/ki/physiology/course/six/6_1. htm Dr. Bolliger Kanas University Medical Center 1999
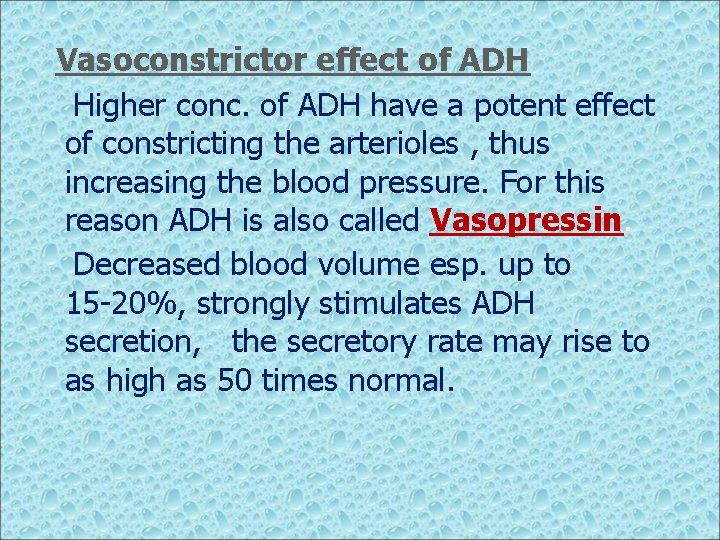
Vasoconstrictor effect of ADH Higher conc. of ADH have a potent effect of constricting the arterioles , thus increasing the blood pressure. For this reason ADH is also called Vasopressin. Decreased blood volume esp. up to 15 -20%, strongly stimulates ADH secretion, the secretory rate may rise to as high as 50 times normal.
Mechanism of vasoconstriction The atria, esp. right atrium, have stretch receptors which are stimulated by overfilling. When they are excited, they send signals to brain to inhibit ADH secretion. Conversely when unexcited due to under filling, greatly increased secretion of ADH occurs.
Decreased stretch of baroreceptors of the carotid, aortic and pulmonary regions participate in increased ADH secretion.
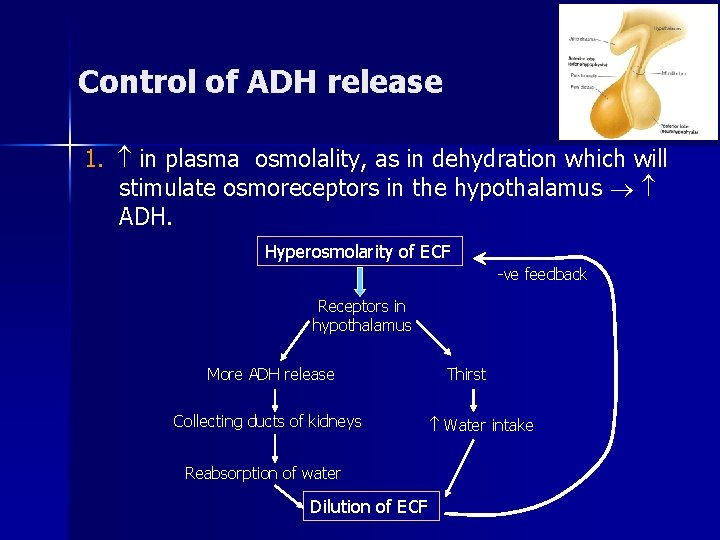
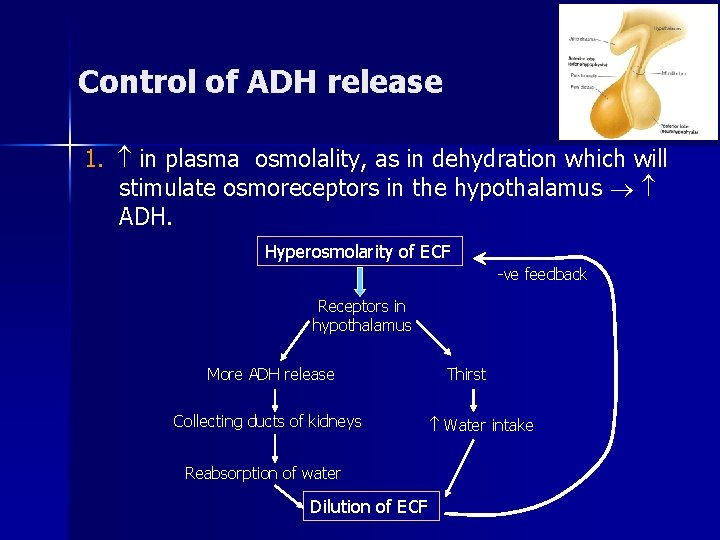
Control of ADH release 1. in plasma osmolality, as in dehydration which will stimulate osmoreceptors in the hypothalamus ADH. Hyperosmolarity of ECF -ve feedback Receptors in hypothalamus More ADH release Collecting ducts of kidneys Reabsorption of water Dilution of ECF Thirst Water intake
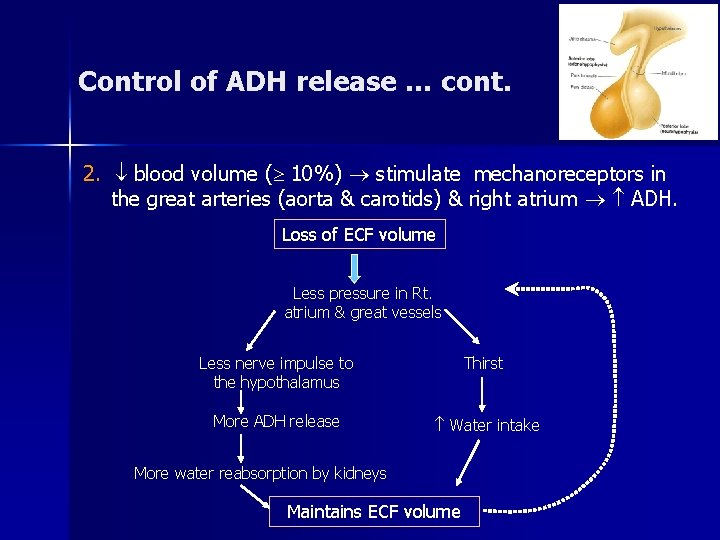
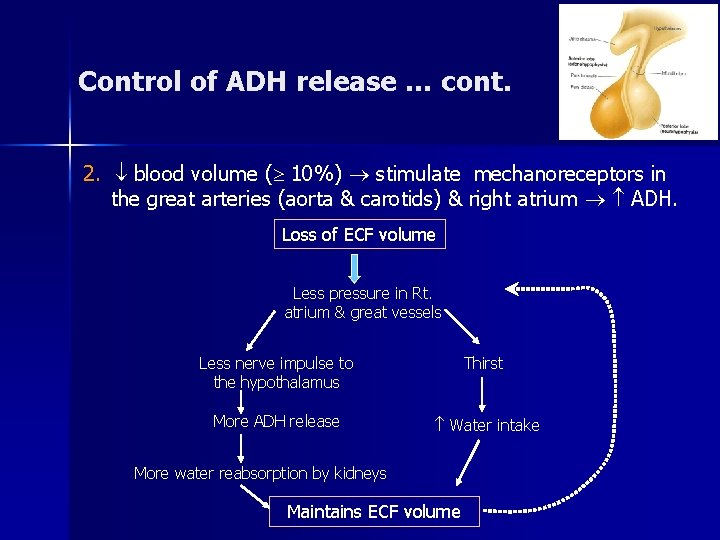
Control of ADH release … cont. 2. blood volume ( 10%) stimulate mechanoreceptors in the great arteries (aorta & carotids) & right atrium ADH. Loss of ECF volume Less pressure in Rt. atrium & great vessels Less nerve impulse to the hypothalamus Thirst More ADH release Water intake More water reabsorption by kidneys Maintains ECF volume
Abnormalities of ADH release – Hyposecretion: § Lack of ADH Diabetes insipidus. 2 types of DI: a. Neurogenic (central, or cranial) … Problem in Hypothalamus or Post pituitary gland. b. Nephrogenic …resistance of V 2 receptors in collecting ducts of the kidneys. - No ADH is needed as treatment. Symptoms: Polyuria 20 L/day (N 1. 5 L/d) specific gravity of urine (diluted urine), plasma osmolality.
Primary Polydypsia Patient drinks too much water that continuously suppresses ADH
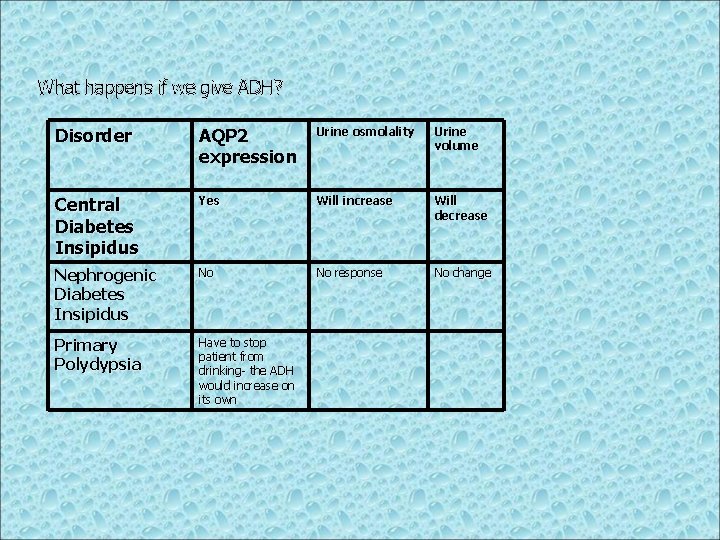
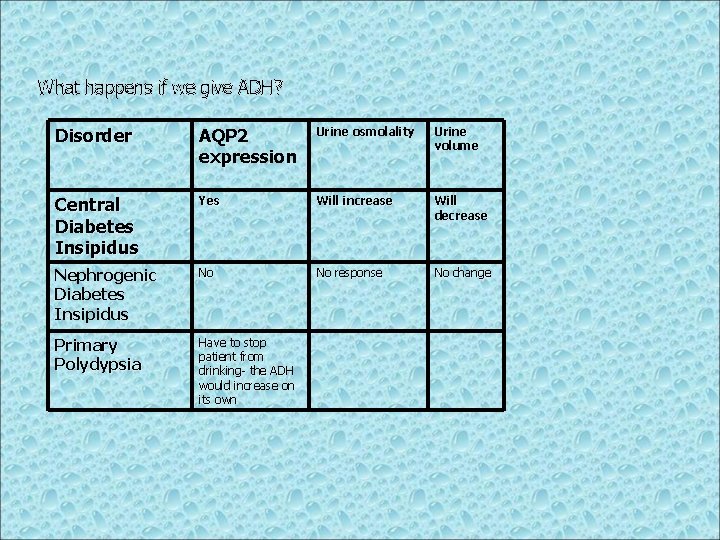
What happens if we give ADH? Disorder AQP 2 expression Urine osmolality Urine volume Central Diabetes Insipidus Yes Will increase Will decrease Nephrogenic Diabetes Insipidus No No response No change Primary Polydypsia Have to stop patient from drinking- the ADH would increase on its own
Abnormalities of ADH release – Hypersecretion: § ADH, ‘Schwartz-Bartter Syndrome’: - occurs after surgery. - adenoma. - Bronchial carcinoma. Signs & Symptoms: - Hyponatremia - Mental confusion. - Coma.

Is it Christmas yet. . .