The PNS Afferent Nervous System two kinds of
- Slides: 68
The PNS: Afferent Nervous System • two kinds of pathways: – 1. Somatic: sensory/afferent information from skeletal muscles, joints, tendons, skin – part of the somatosensory system – receptors are scattered at the body surface, proprioceptors – touch, vibration, itch, tickle, temperature, pain & proprioception – processed in the somatosensory cortex – receptors can also become specialized = Special senses
The PNS: Afferent Nervous System – 2. Visceral: sensory information from the internal viscera • receptors are scattered throughout the organs – e. g. blood pressure, body fluid concentration, respiratory gas concentration • never reaches a conscious level • although you can become aware of pain • this information is critical form determining the appropriate efferent output to maintain homeostasis
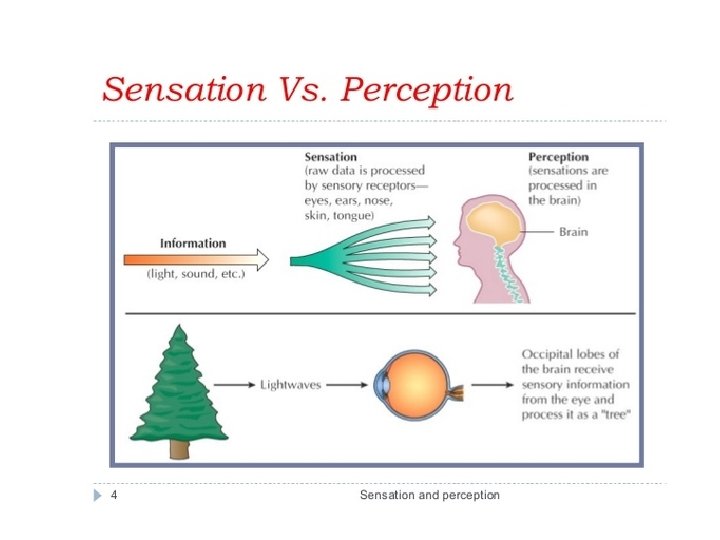
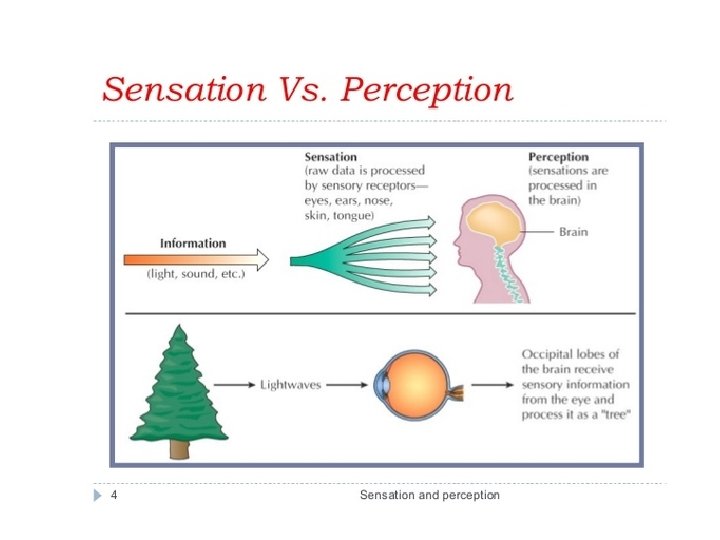
Perception & Sensation • Sensation: response to environment via generation of nerve impulses –before nerve impulse is generated - sensory receptors integrate or sum up the incoming signals –nerve impulses then sent via ascending tracts in spinal cord to the brain • several types of integration: one type is adaptation - decrease in response to a stimulus –role of the thalamus? ? (gatekeeper? ? ) • Perception: our conscious interpretation of the external world –occurs upon arrival of nerve impulse at cerebral cortex –created by the brain based on information it receives from sensory receptors –interpretation of sensation
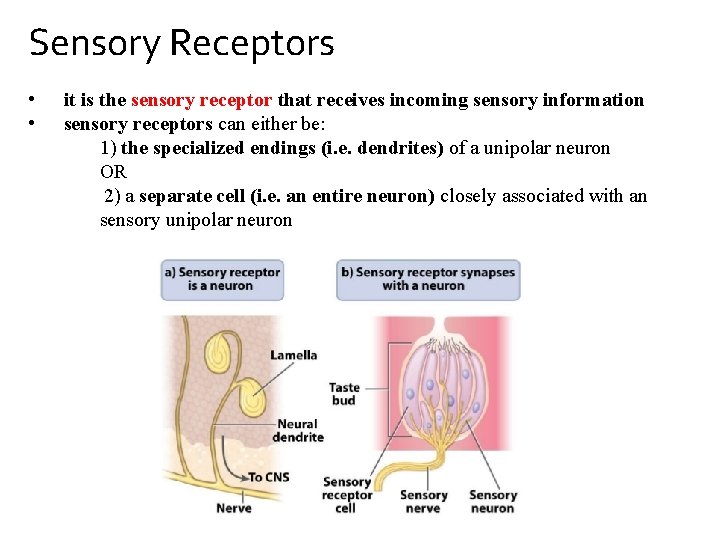
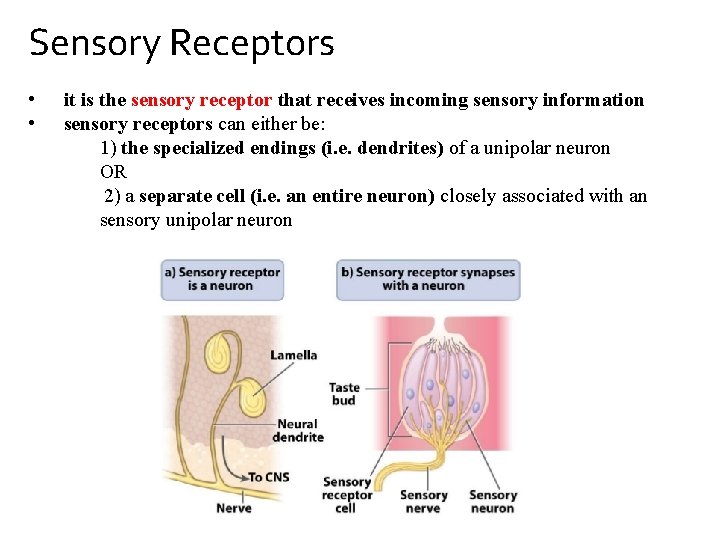
Sensory Receptors • • it is the sensory receptor that receives incoming sensory information sensory receptors can either be: 1) the specialized endings (i. e. dendrites) of a unipolar neuron OR 2) a separate cell (i. e. an entire neuron) closely associated with an sensory unipolar neuron
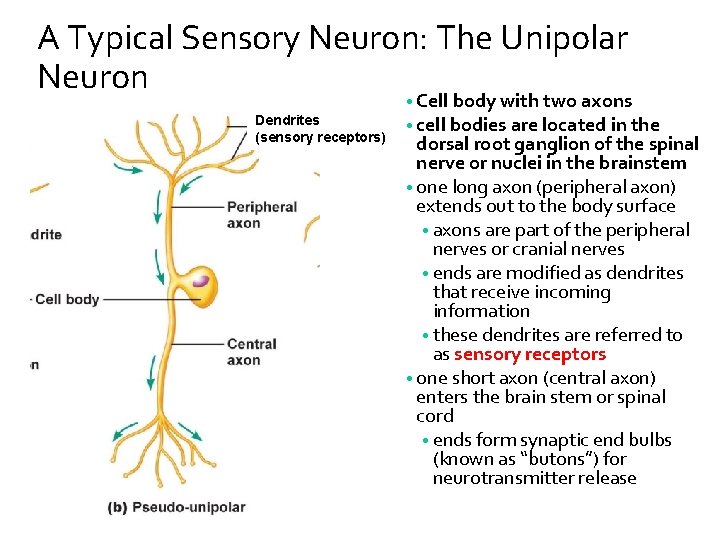
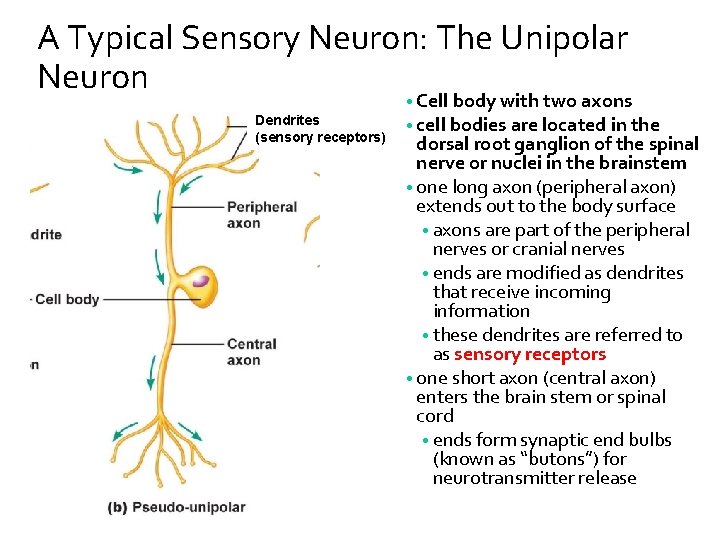
A Typical Sensory Neuron: The Unipolar Neuron Dendrites (sensory receptors) • Cell body with two axons • cell bodies are located in the dorsal root ganglion of the spinal nerve or nuclei in the brainstem • one long axon (peripheral axon) extends out to the body surface • axons are part of the peripheral nerves or cranial nerves • ends are modified as dendrites that receive incoming information • these dendrites are referred to as sensory receptors • one short axon (central axon) enters the brain stem or spinal cord • ends form synaptic end bulbs (known as “butons”) for neurotransmitter release
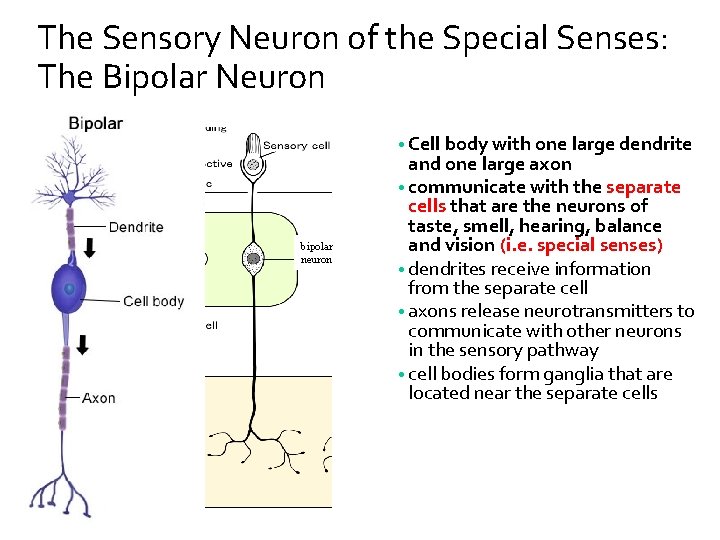
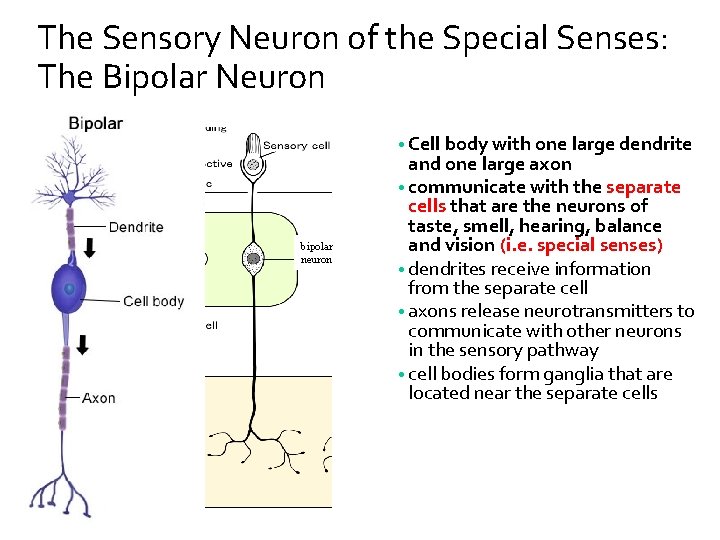
The Sensory Neuron of the Special Senses: The Bipolar Neuron • Cell body with one large dendrite bipolar neuron and one large axon • communicate with the separate cells that are the neurons of taste, smell, hearing, balance and vision (i. e. special senses) • dendrites receive information from the separate cell • axons release neurotransmitters to communicate with other neurons in the sensory pathway • cell bodies form ganglia that are located near the separate cells
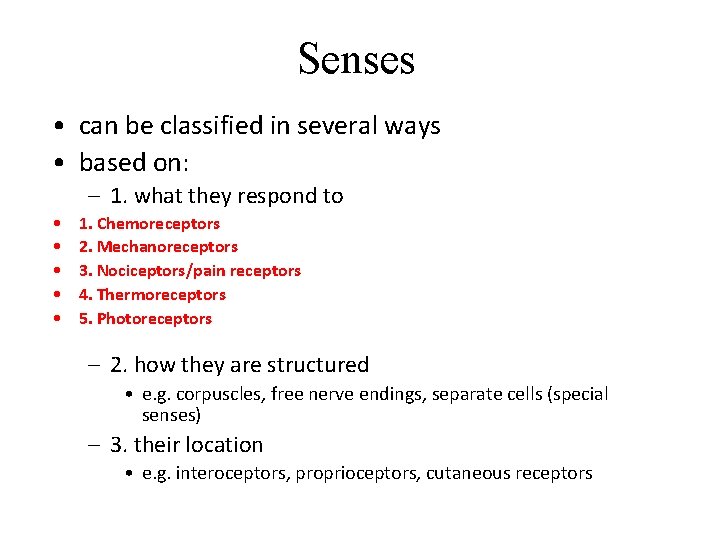
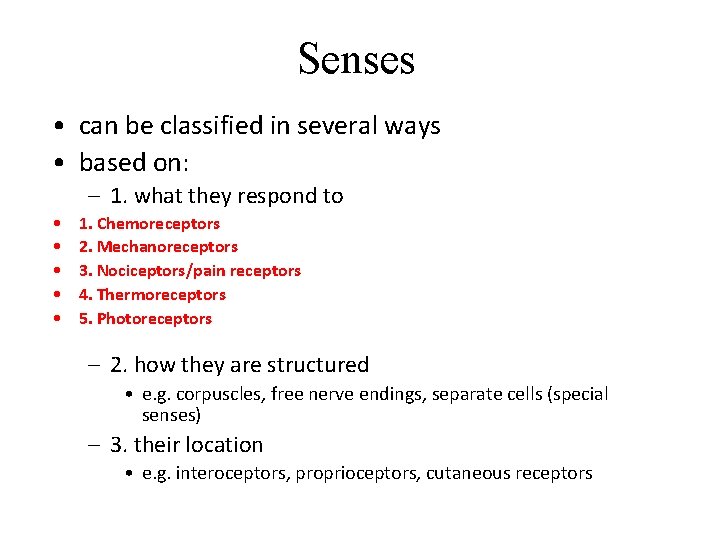
Senses • can be classified in several ways • based on: – 1. what they respond to • • • 1. Chemoreceptors 2. Mechanoreceptors 3. Nociceptors/pain receptors 4. Thermoreceptors 5. Photoreceptors – 2. how they are structured • e. g. corpuscles, free nerve endings, separate cells (special senses) – 3. their location • e. g. interoceptors, proprioceptors, cutaneous receptors
General vs. Special Senses • General – Touch, pressure, itch, tickle, heat/cold = cutaneous receptors (touch) – Proprioception - proprioceptors • Special – – Taste Hearing Vision Smell
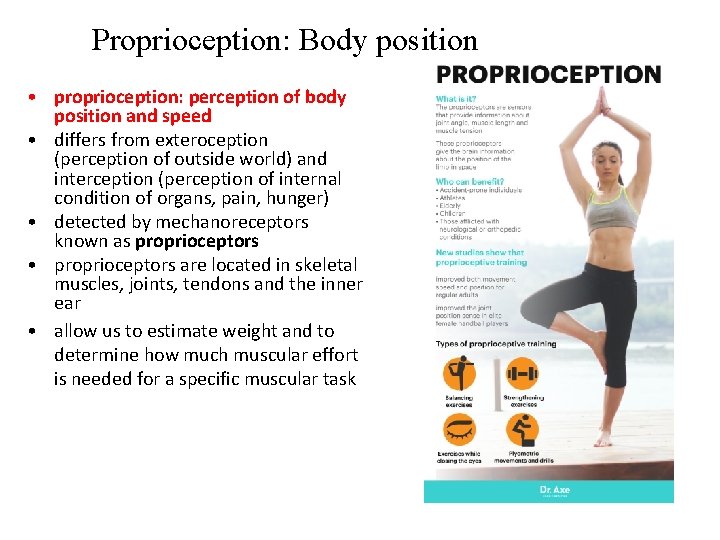
Proprioception: Body position • proprioception: perception of body position and speed • differs from exteroception (perception of outside world) and interception (perception of internal condition of organs, pain, hunger) • detected by mechanoreceptors known as proprioceptors • proprioceptors are located in skeletal muscles, joints, tendons and the inner ear • allow us to estimate weight and to determine how much muscular effort is needed for a specific muscular task
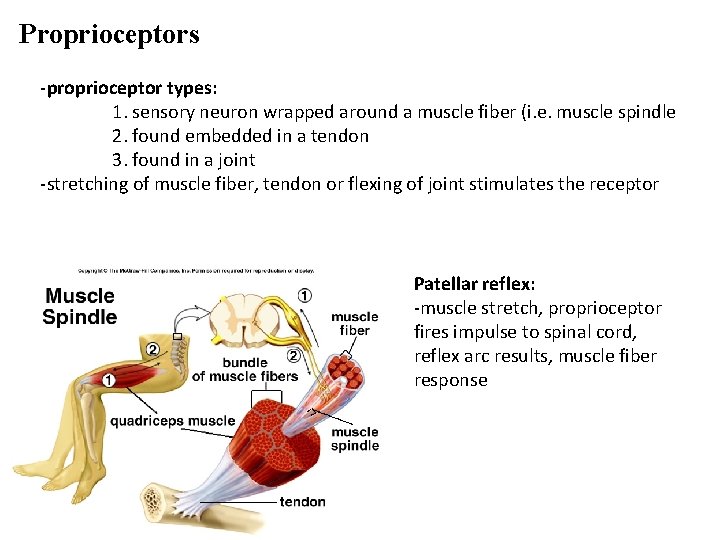
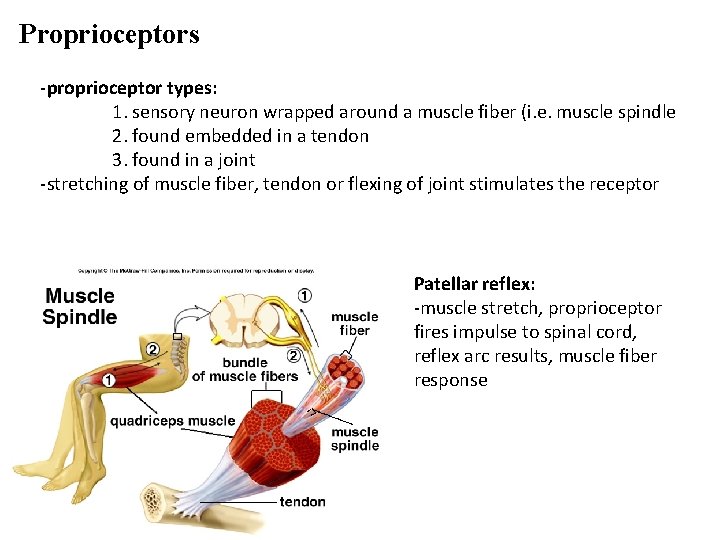
Proprioceptors -proprioceptor types: 1. sensory neuron wrapped around a muscle fiber (i. e. muscle spindle 2. found embedded in a tendon 3. found in a joint -stretching of muscle fiber, tendon or flexing of joint stimulates the receptor Patellar reflex: -muscle stretch, proprioceptor fires impulse to spinal cord, reflex arc results, muscle fiber response
Cutaneous receptors – General Sensation of Touch -located in skin -receptors can be classified as exteroceptors but are often called cutaneous receptors because they are in the skin -can also be classified as thermoreceptors, mechanoceptors, nociceptors etc…. -can also be classified as free nerve endings (exposed dendrites) or corpuscles (covered dendrites) -impulses first sent to primary somatosensory area of brain = postcentral gyrus of parietal lobe -association areas of the parietal lobe continue the processing
Cutaneous receptors – General Sensation of Touch -touch receptors: Meissner’s corpuscles(fingertips, lips, tongue, nipples, penis/clitoris) Merkel disks (epidermis/dermis) Root hair plexus (root of hair) -pressure receptors: Pacinian corpuscles (lamellated corpuscle) -temp receptors: free nerve endings that respond to cold OR warmth -Krause end bulbs, Ruffini endings
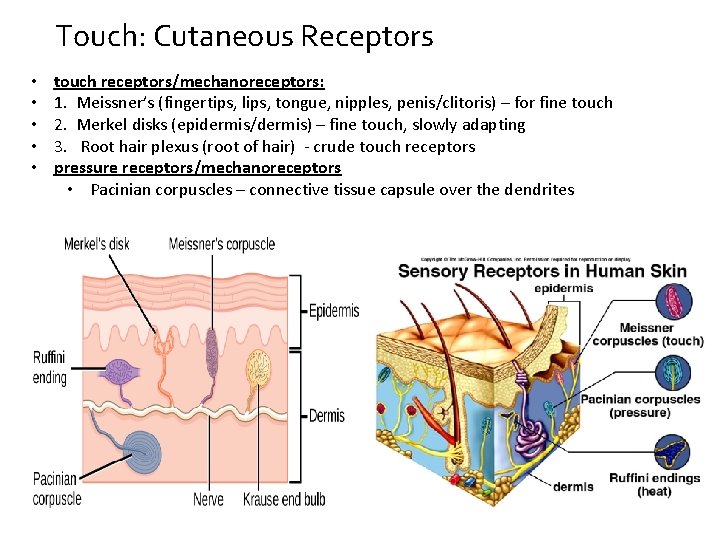
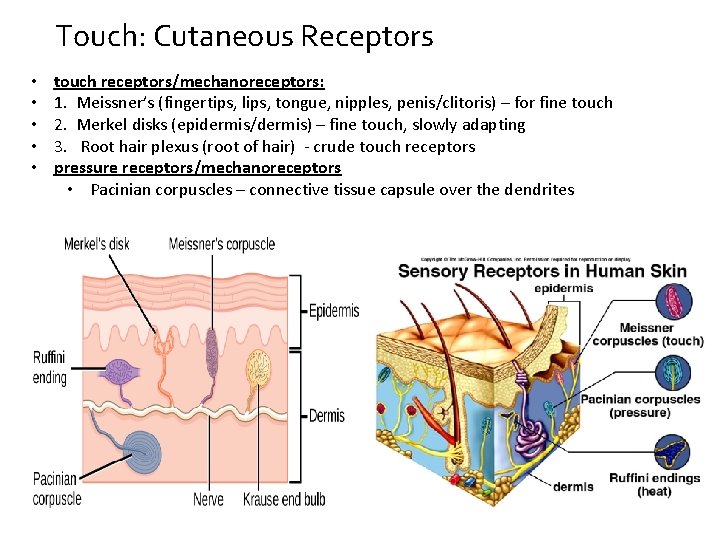
Touch: Cutaneous Receptors • • • touch receptors/mechanoreceptors: 1. Meissner’s (fingertips, lips, tongue, nipples, penis/clitoris) – for fine touch 2. Merkel disks (epidermis/dermis) – fine touch, slowly adapting 3. Root hair plexus (root of hair) - crude touch receptors pressure receptors/mechanoreceptors • Pacinian corpuscles – connective tissue capsule over the dendrites
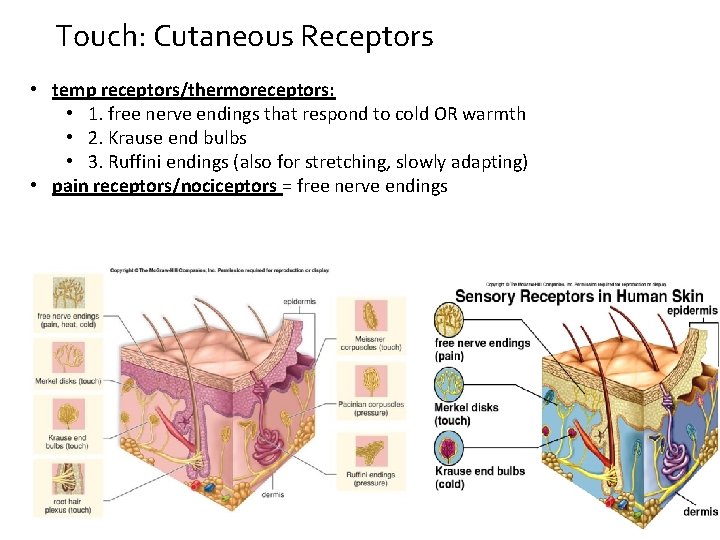
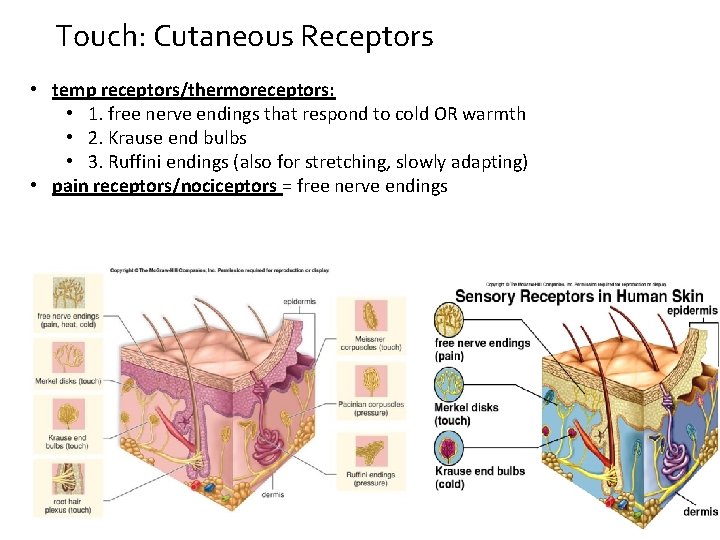
Touch: Cutaneous Receptors • temp receptors/thermoreceptors: • 1. free nerve endings that respond to cold OR warmth • 2. Krause end bulbs • 3. Ruffini endings (also for stretching, slowly adapting) • pain receptors/nociceptors = free nerve endings
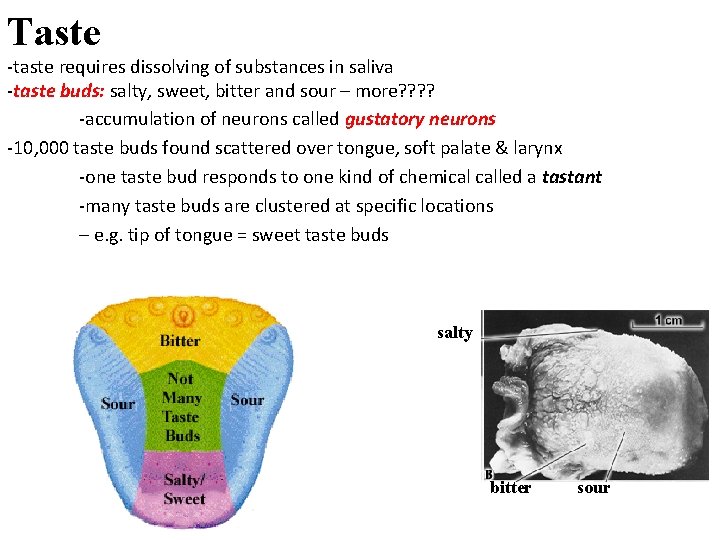
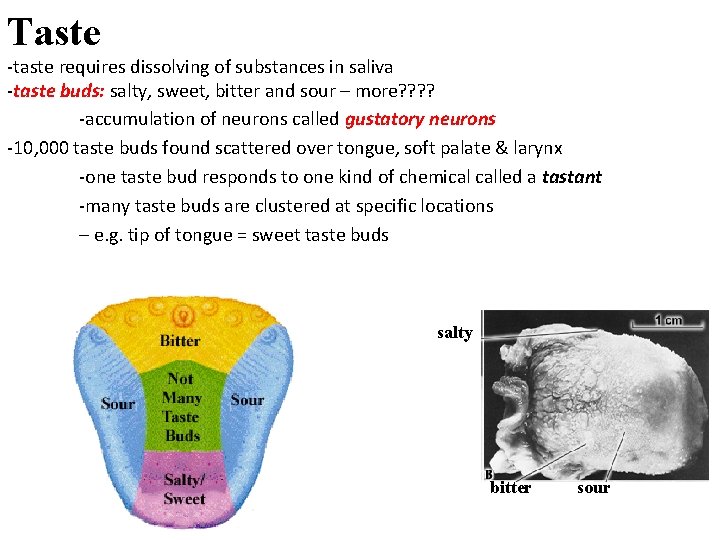
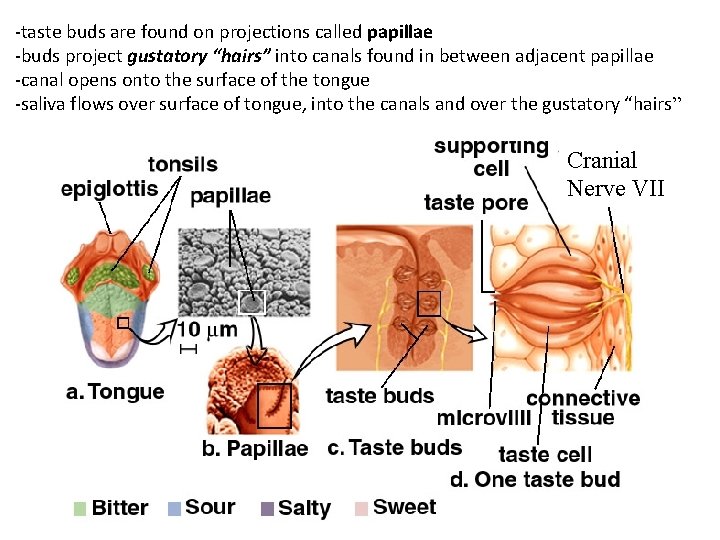
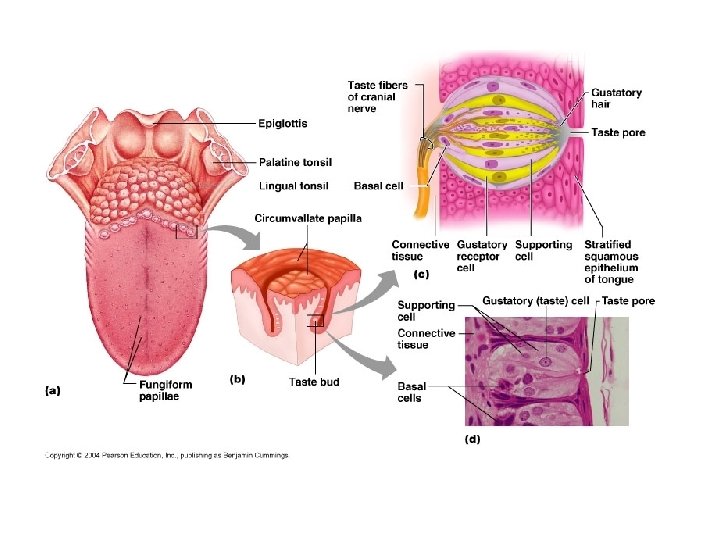
Taste -taste requires dissolving of substances in saliva -taste buds: salty, sweet, bitter and sour – more? ? -accumulation of neurons called gustatory neurons -10, 000 taste buds found scattered over tongue, soft palate & larynx -one taste bud responds to one kind of chemical called a tastant -many taste buds are clustered at specific locations – e. g. tip of tongue = sweet taste buds salty bitter sour
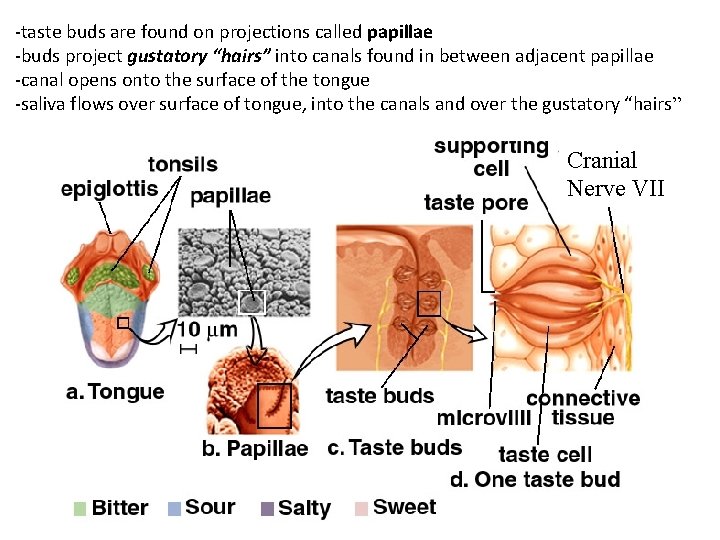
-taste buds are found on projections called papillae -buds project gustatory “hairs” into canals found in between adjacent papillae -canal opens onto the surface of the tongue -saliva flows over surface of tongue, into the canals and over the gustatory “hairs” Cranial Nerve VII
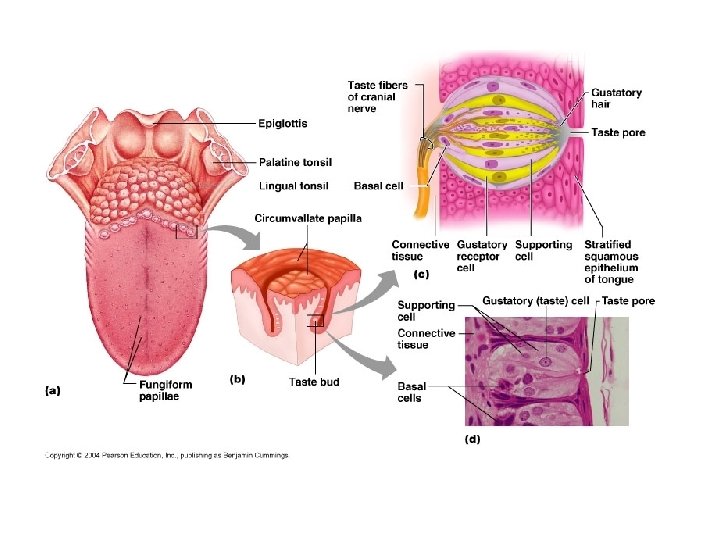
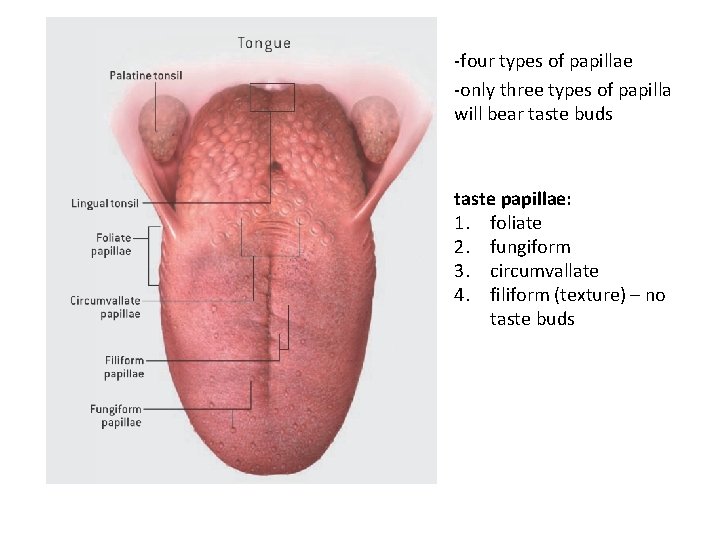
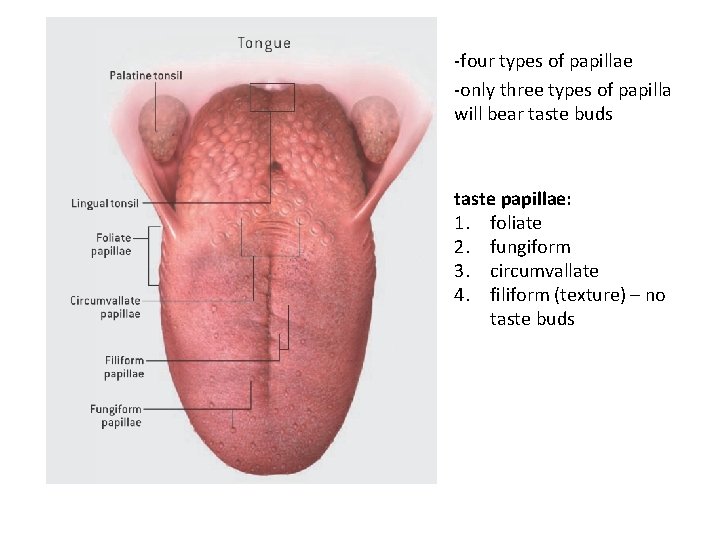
-four types of papillae -only three types of papilla will bear taste buds taste papillae: 1. foliate 2. fungiform 3. circumvallate 4. filiform (texture) – no taste buds
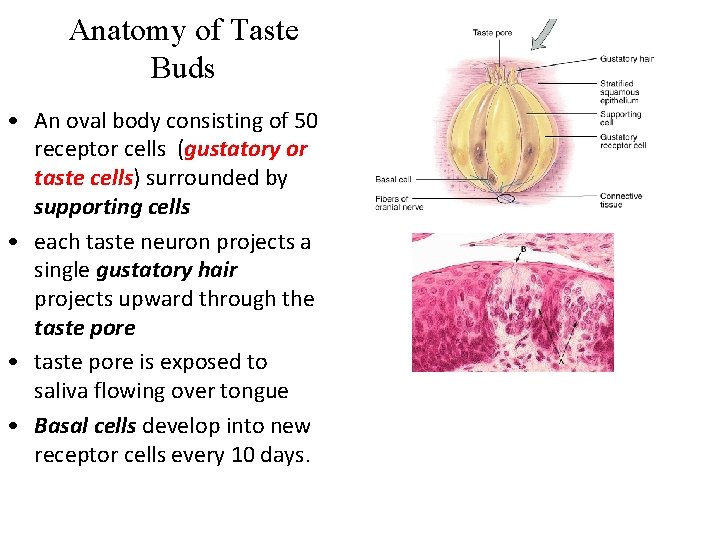
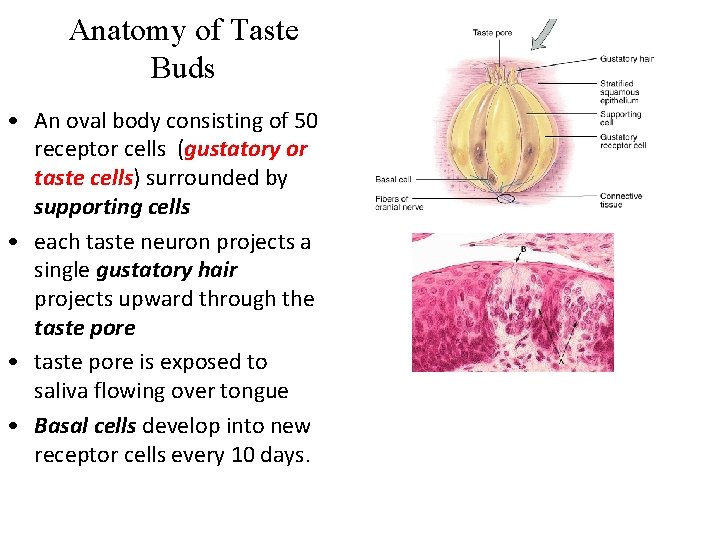
Anatomy of Taste Buds • An oval body consisting of 50 receptor cells (gustatory or taste cells) surrounded by supporting cells • each taste neuron projects a single gustatory hair projects upward through the taste pore • taste pore is exposed to saliva flowing over tongue • Basal cells develop into new receptor cells every 10 days.
Physiology of Taste • receptor-ligand interaction – ligand is the tastant and the receptor is the gustatory cell • tastant binding leads to a change in the receptor potential – action potential – mechanism differs based on the tastant • release of neurotransmitters from the taste cell – binds to and stimulates the first order neuron (cranial nerves VII, IX and X) • complete adaptation in 1 to 5 minutes • thresholds for tastes vary among the 4 primary tastes – most sensitive to bitter (poisons) – least sensitive to salty and sweet
Gustatory Pathway • gustatory fibers/axons found in three cranial nerves – VII (facial) serves anterior 2/3 of tongue – IX (glossopharyngeal) serves posterior 1/3 of tongue – X (vagus) serves palate & epiglottis • Signals travel to thalamus - extend from the thalamus to the primary gustatory area on parietal lobe of the cerebral cortex • provide conscious perception of taste • Taste fibers also extend to limbic system – association of taste with a memory
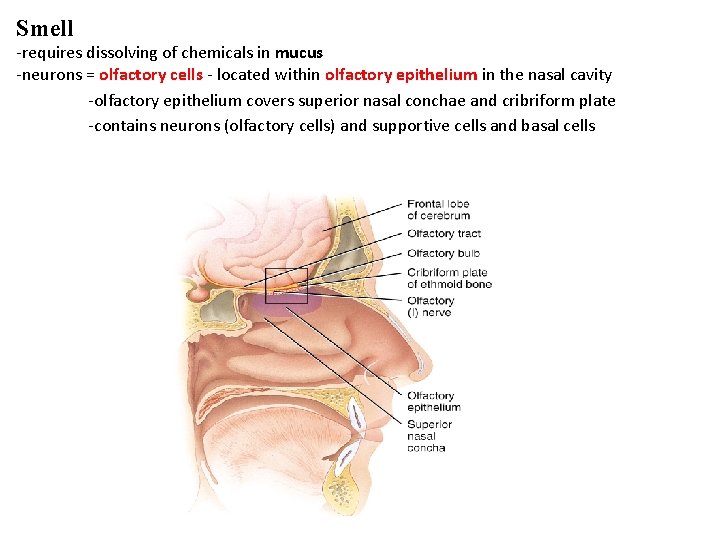
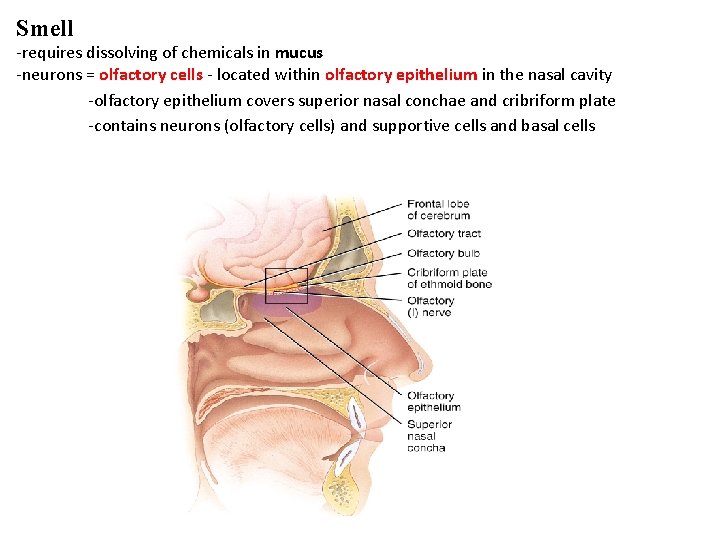
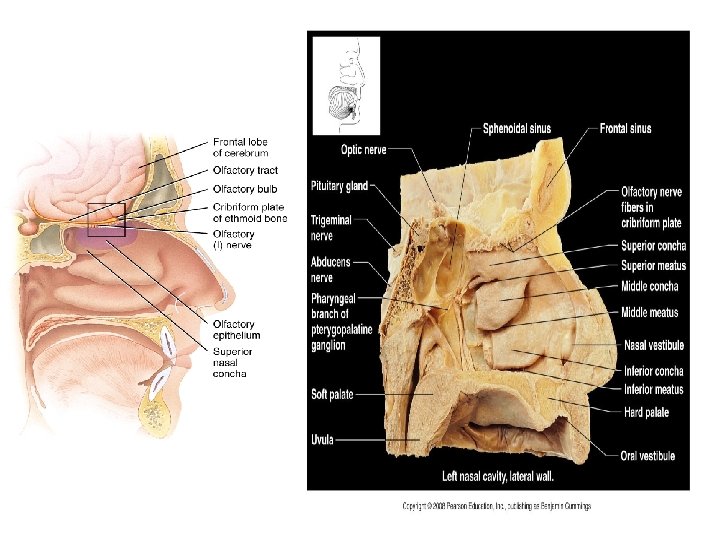
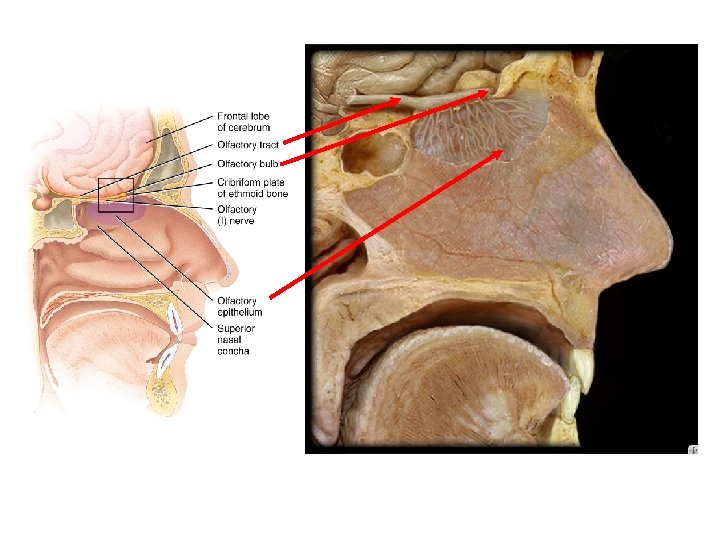
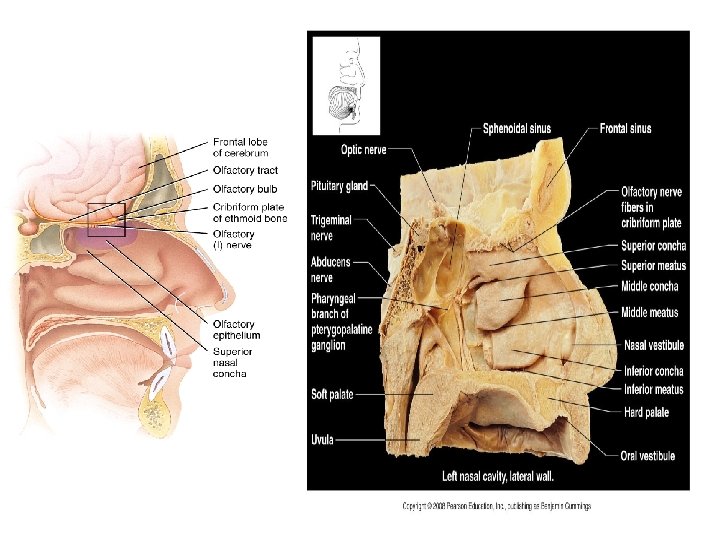
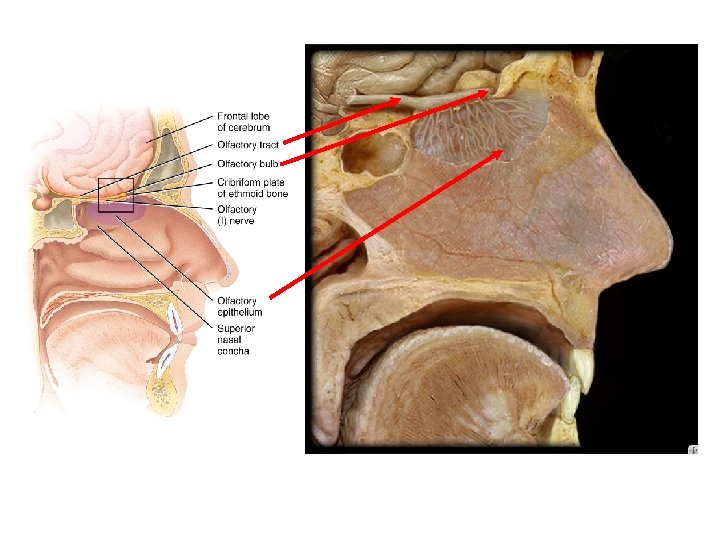
Smell -requires dissolving of chemicals in mucus -neurons = olfactory cells - located within olfactory epithelium in the nasal cavity -olfactory epithelium covers superior nasal conchae and cribriform plate -contains neurons (olfactory cells) and supportive cells and basal cells
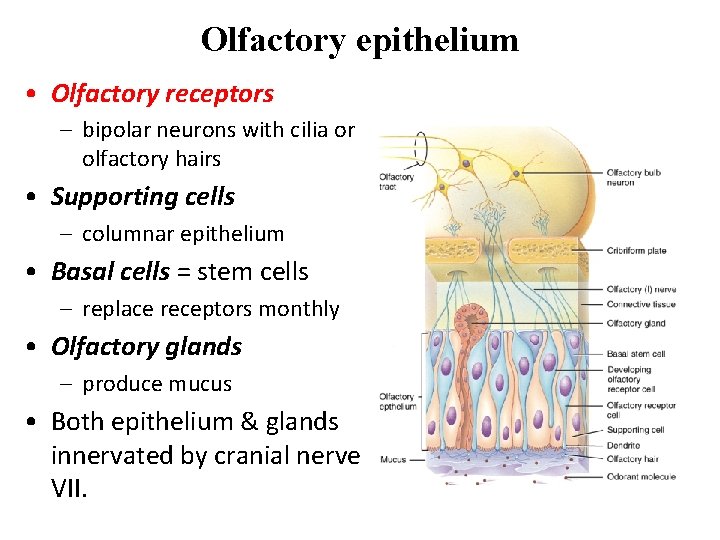
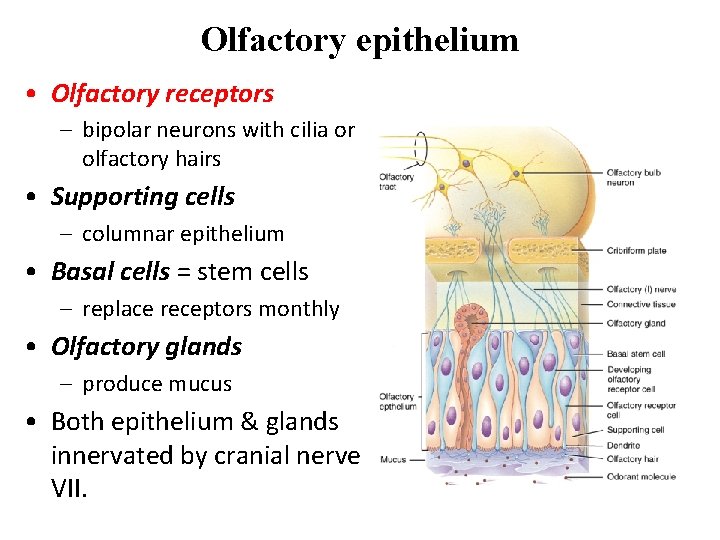
Olfactory epithelium • Olfactory receptors – bipolar neurons with cilia or olfactory hairs • Supporting cells – columnar epithelium • Basal cells = stem cells – replace receptors monthly • Olfactory glands – produce mucus • Both epithelium & glands innervated by cranial nerve VII.
Eustacian tube With tubal tonsil
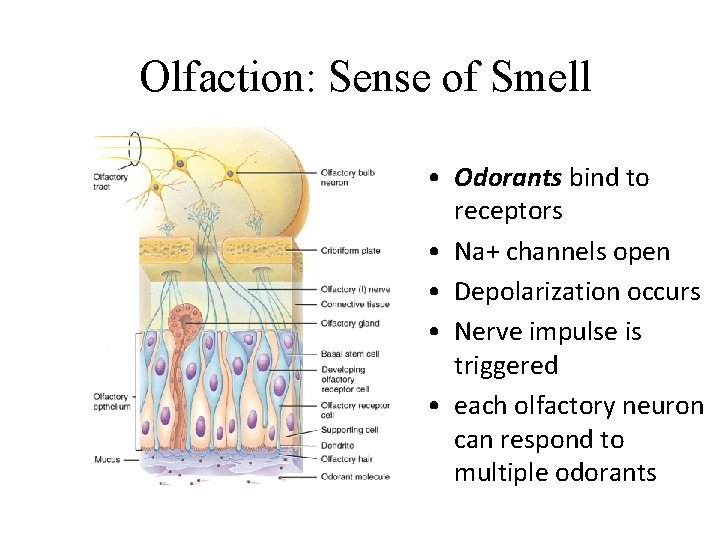
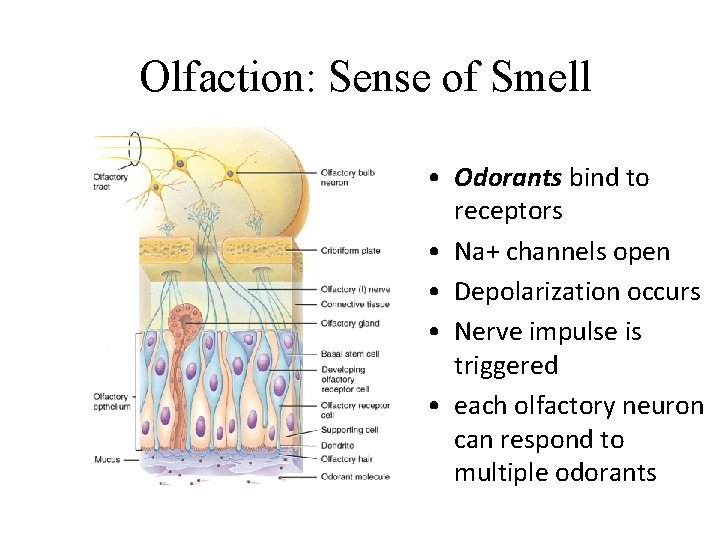
Olfaction: Sense of Smell • Odorants bind to receptors • Na+ channels open • Depolarization occurs • Nerve impulse is triggered • each olfactory neuron can respond to multiple odorants
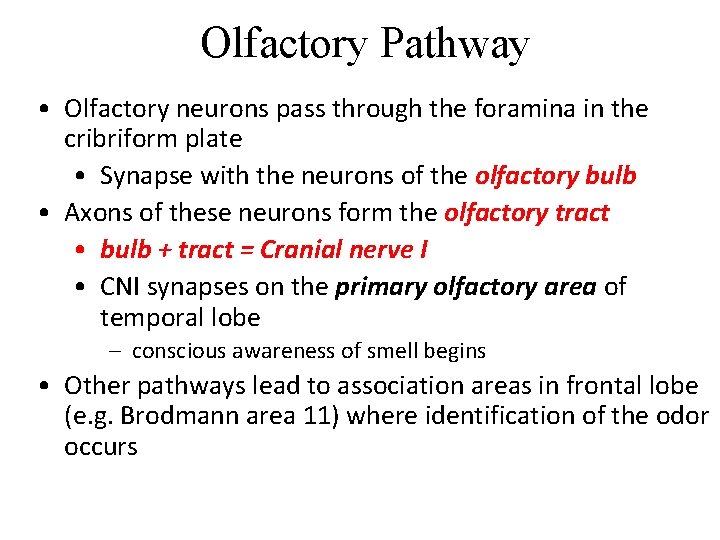
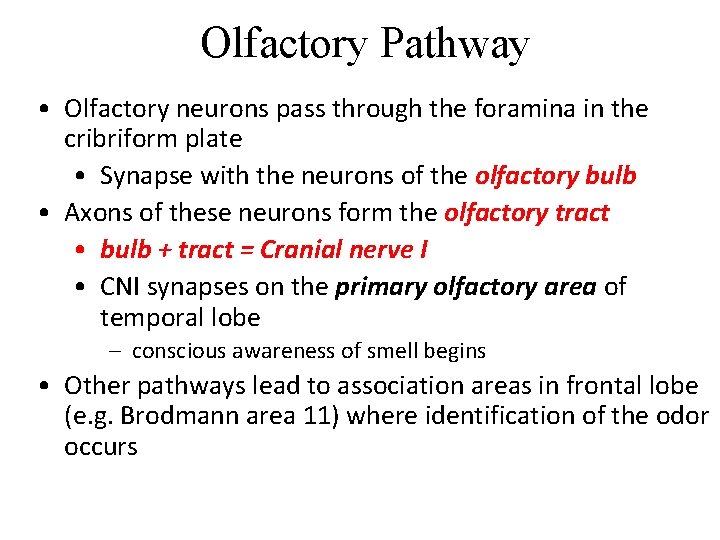
Olfactory Pathway • Olfactory neurons pass through the foramina in the cribriform plate • Synapse with the neurons of the olfactory bulb • Axons of these neurons form the olfactory tract • bulb + tract = Cranial nerve I • CNI synapses on the primary olfactory area of temporal lobe – conscious awareness of smell begins • Other pathways lead to association areas in frontal lobe (e. g. Brodmann area 11) where identification of the odor occurs
Adaptation & Odor Thresholds • Adaptation = decreasing sensitivity of repeated stimuli over time • Olfactory adaptation is very rapid – 50% in 1 second – complete in 1 minute • Low threshold – only a few molecules need to be present e. g. methyl mercaptan added to natural gas as warning
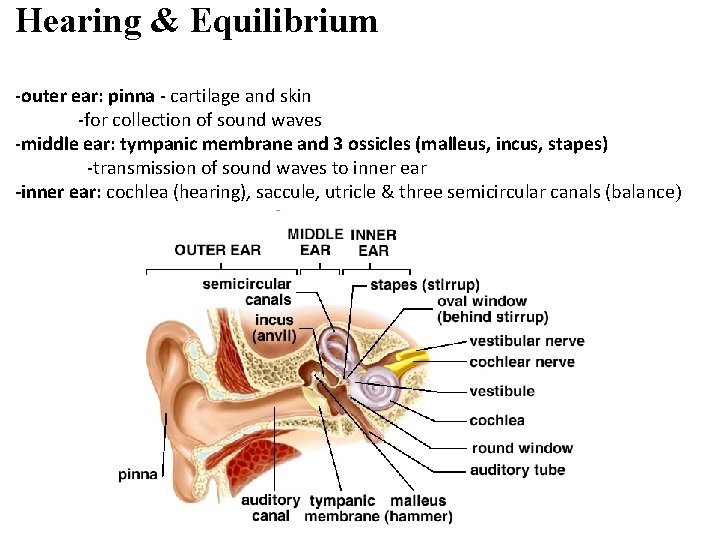
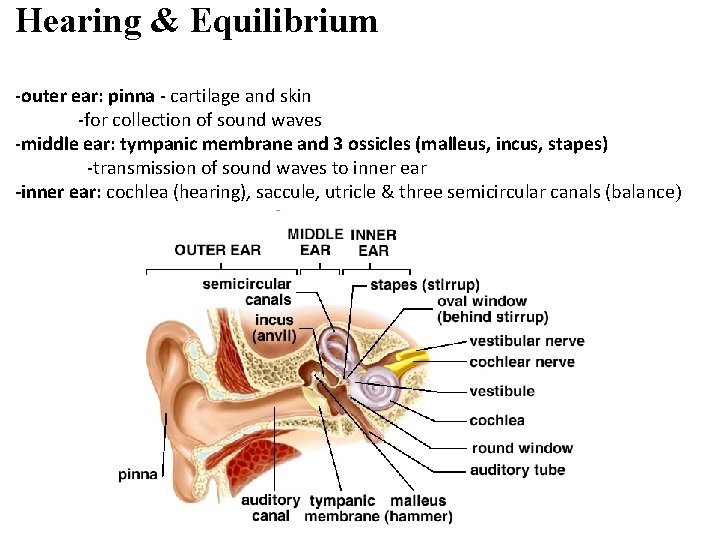
Hearing & Equilibrium -outer ear: pinna - cartilage and skin -for collection of sound waves -middle ear: tympanic membrane and 3 ossicles (malleus, incus, stapes) -transmission of sound waves to inner ear -inner ear: cochlea (hearing), saccule, utricle & three semicircular canals (balance)
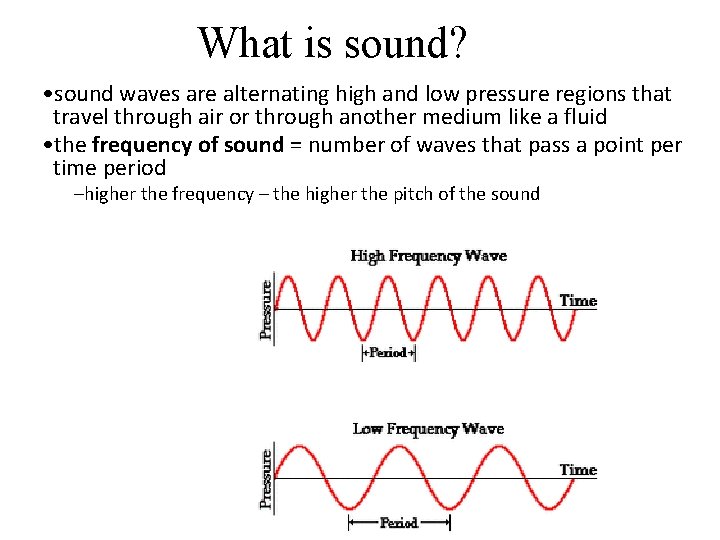
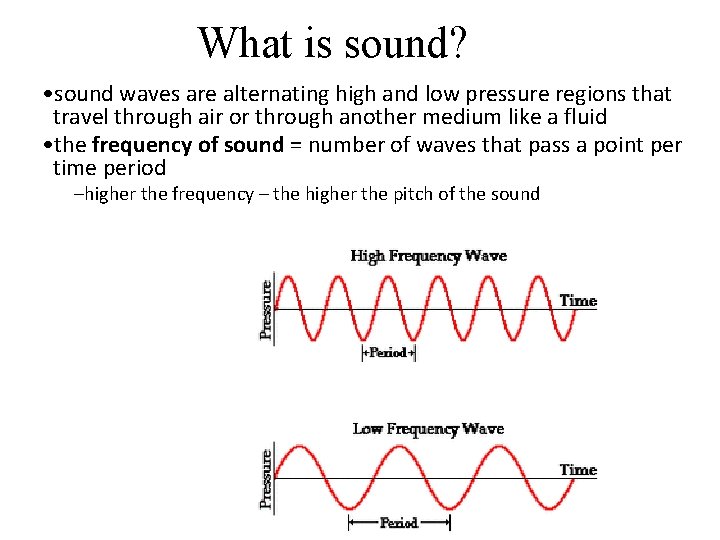
What is sound? • sound waves are alternating high and low pressure regions that travel through air or through another medium like a fluid • the frequency of sound = number of waves that pass a point per time period –higher the frequency – the higher the pitch of the sound
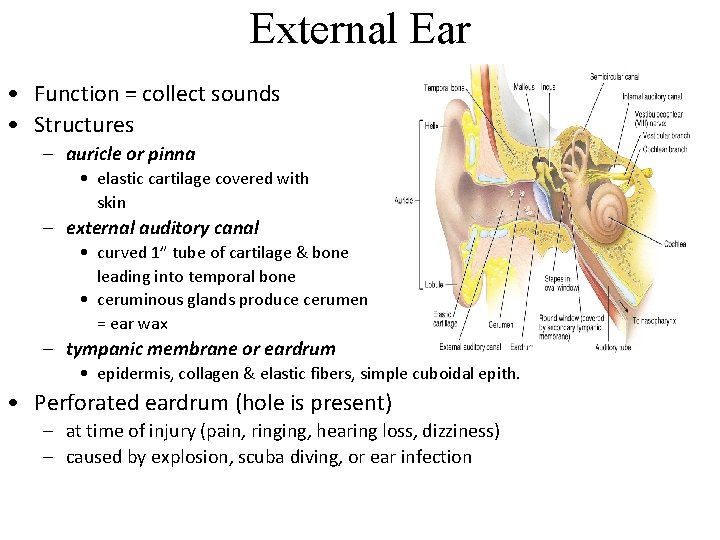
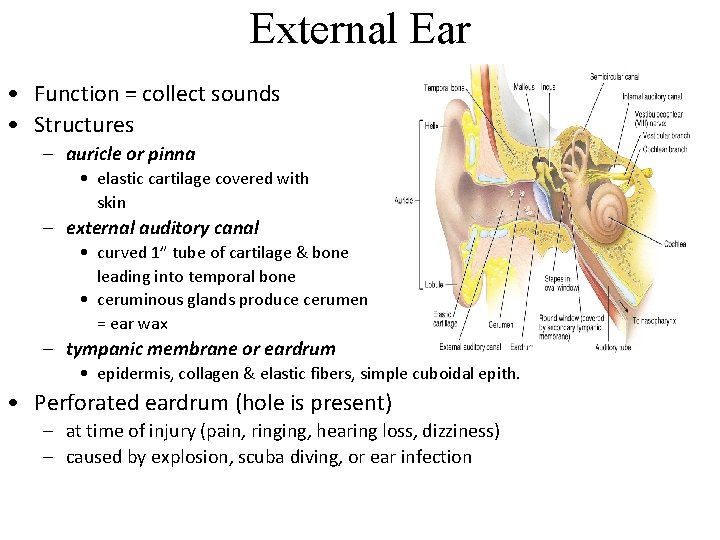
External Ear • Function = collect sounds • Structures – auricle or pinna • elastic cartilage covered with skin – external auditory canal • curved 1” tube of cartilage & bone leading into temporal bone • ceruminous glands produce cerumen = ear wax – tympanic membrane or eardrum • epidermis, collagen & elastic fibers, simple cuboidal epith. • Perforated eardrum (hole is present) – at time of injury (pain, ringing, hearing loss, dizziness) – caused by explosion, scuba diving, or ear infection
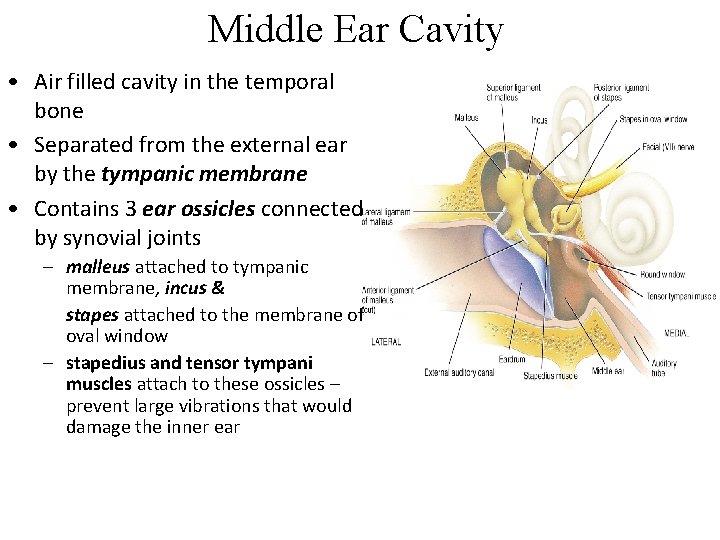
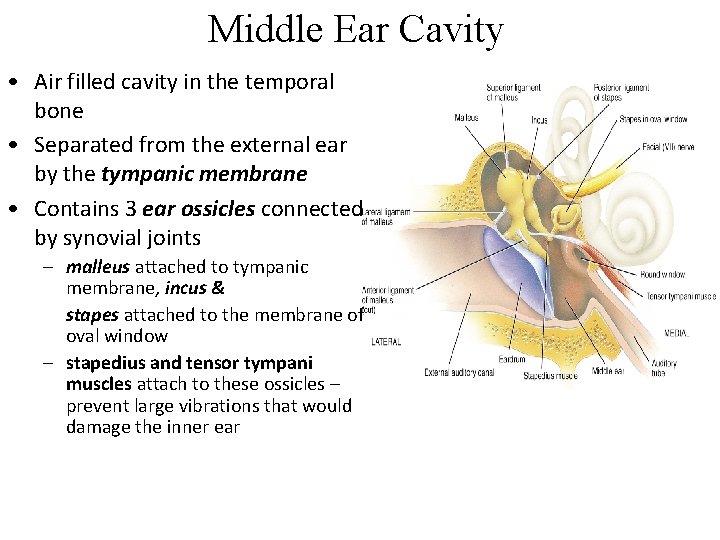
Middle Ear Cavity • Air filled cavity in the temporal bone • Separated from the external ear by the tympanic membrane • Contains 3 ear ossicles connected by synovial joints – malleus attached to tympanic membrane, incus & stapes attached to the membrane of oval window – stapedius and tensor tympani muscles attach to these ossicles – prevent large vibrations that would damage the inner ear
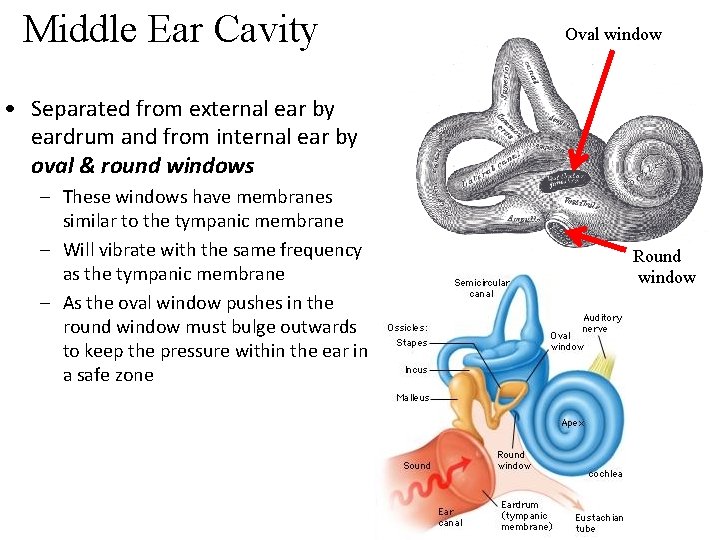
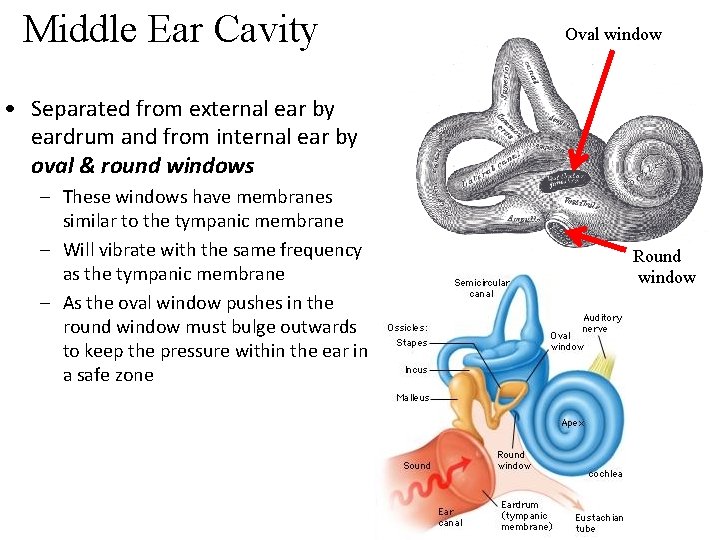
Middle Ear Cavity Oval window • Separated from external ear by eardrum and from internal ear by oval & round windows – These windows have membranes similar to the tympanic membrane – Will vibrate with the same frequency as the tympanic membrane – As the oval window pushes in the round window must bulge outwards to keep the pressure within the ear in a safe zone Round window
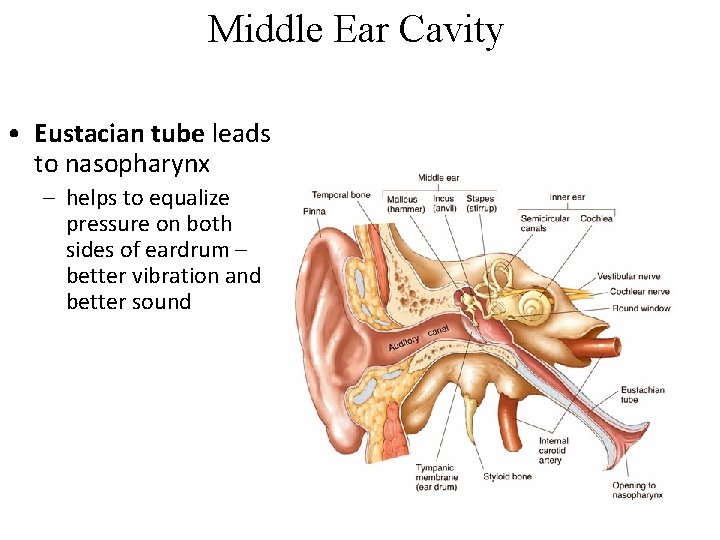
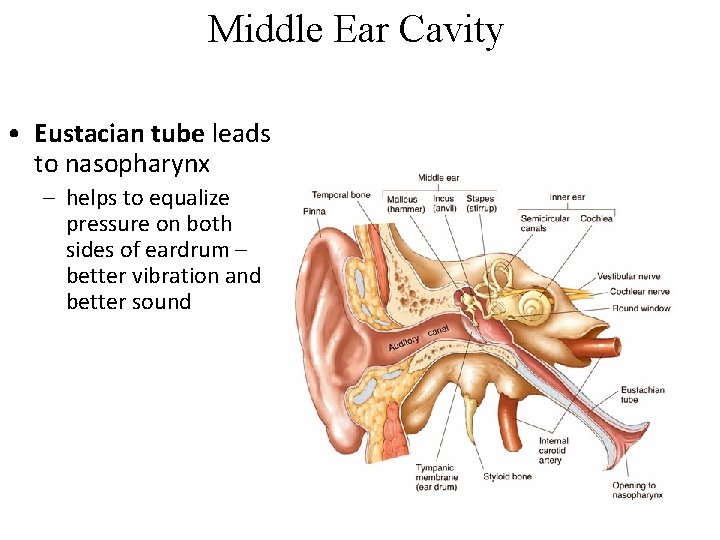
Middle Ear Cavity • Eustacian tube leads to nasopharynx – helps to equalize pressure on both sides of eardrum – better vibration and better sound
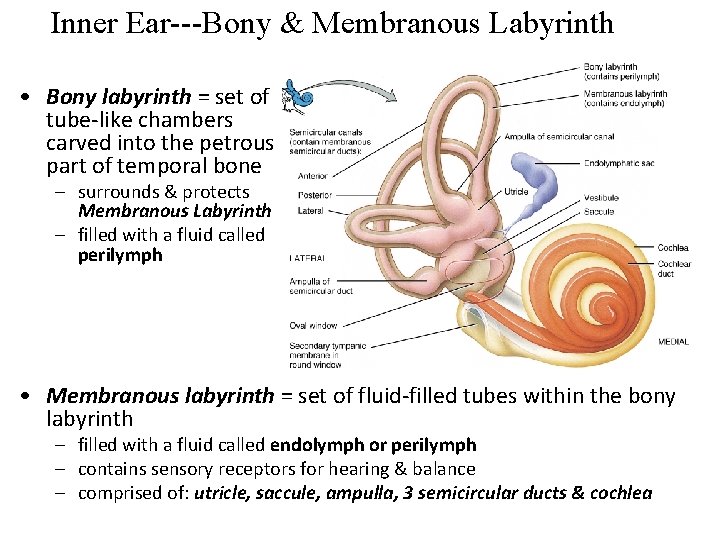
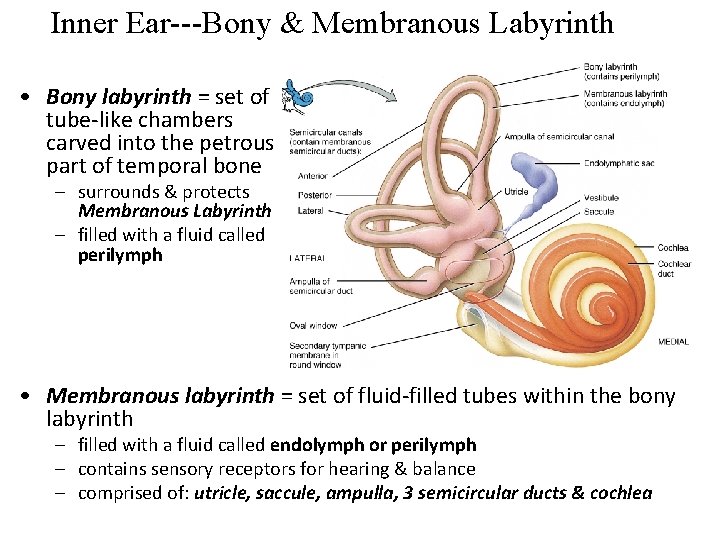
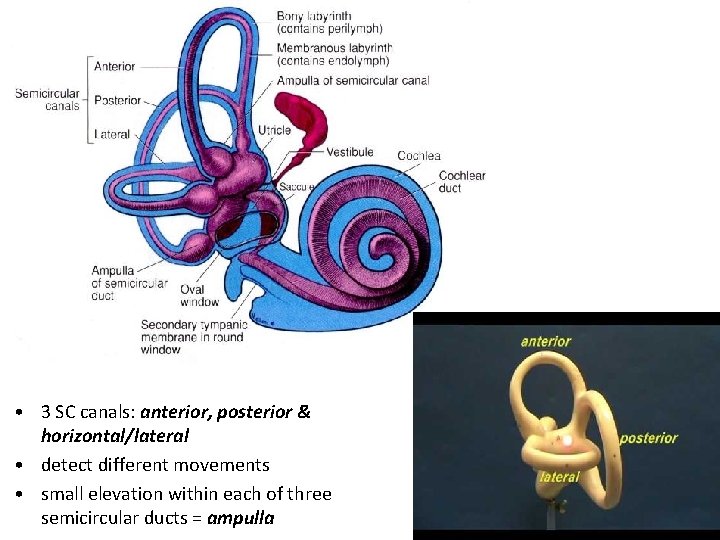
Inner Ear---Bony & Membranous Labyrinth • Bony labyrinth = set of tube-like chambers carved into the petrous part of temporal bone – surrounds & protects Membranous Labyrinth – filled with a fluid called perilymph • Membranous labyrinth = set of fluid-filled tubes within the bony labyrinth – filled with a fluid called endolymph or perilymph – contains sensory receptors for hearing & balance – comprised of: utricle, saccule, ampulla, 3 semicircular ducts & cochlea
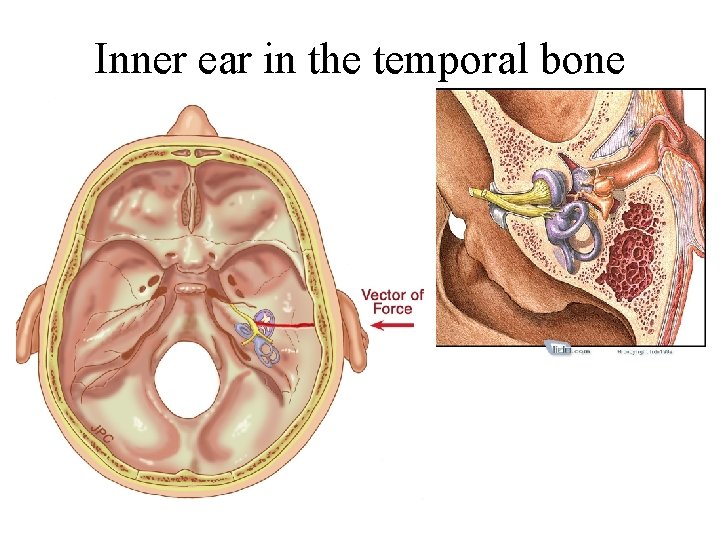
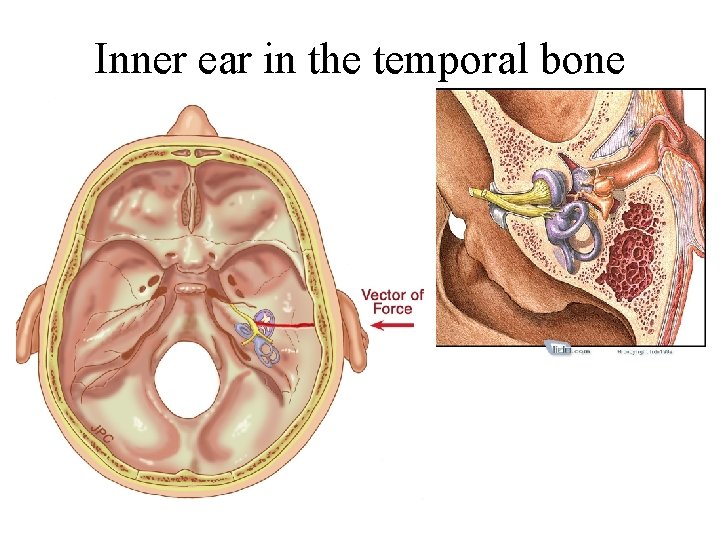
Inner ear in the temporal bone
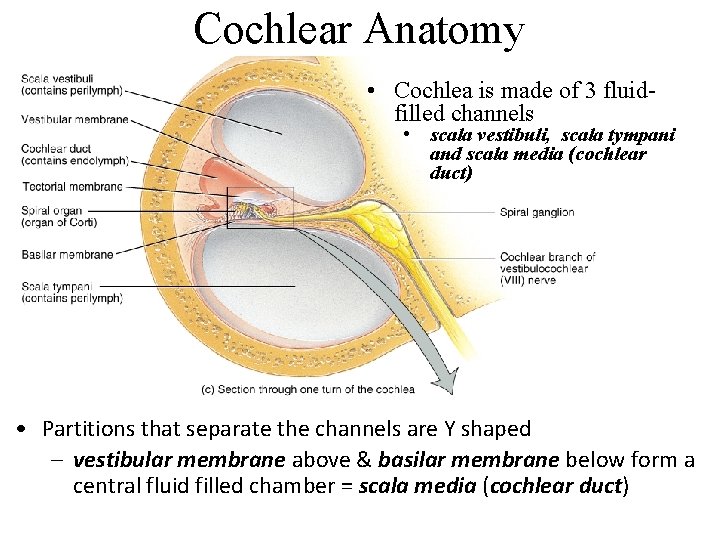
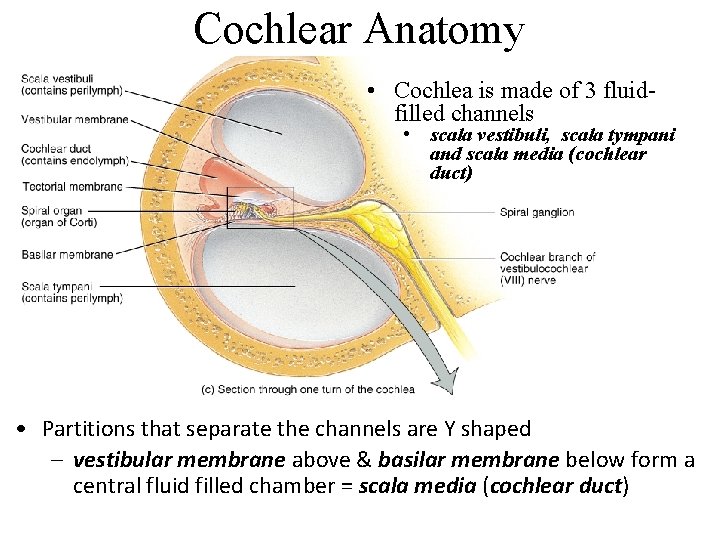
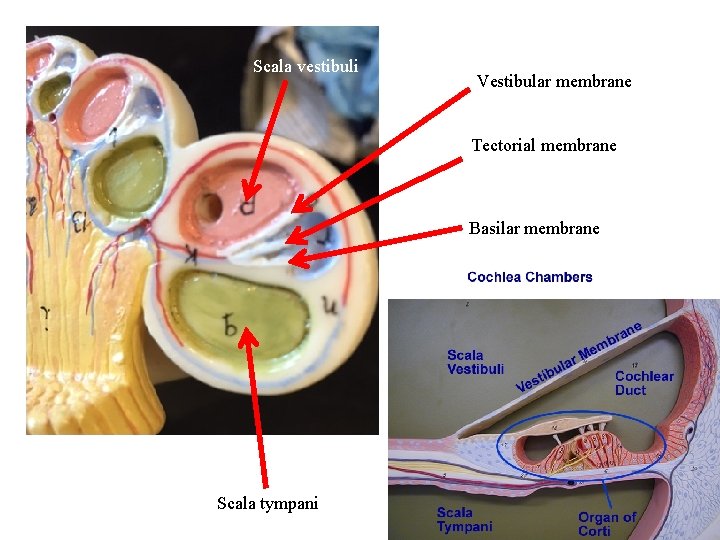
Cochlear Anatomy • Cochlea is made of 3 fluidfilled channels • scala vestibuli, scala tympani and scala media (cochlear duct) • Partitions that separate the channels are Y shaped – vestibular membrane above & basilar membrane below form a central fluid filled chamber = scala media (cochlear duct)
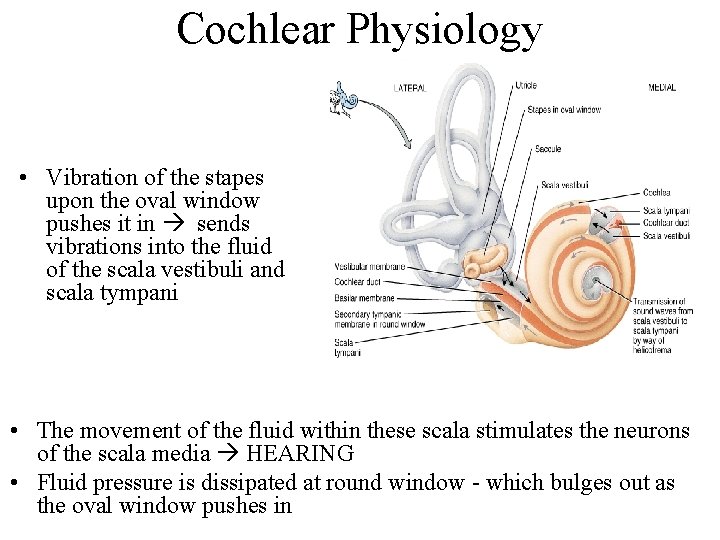
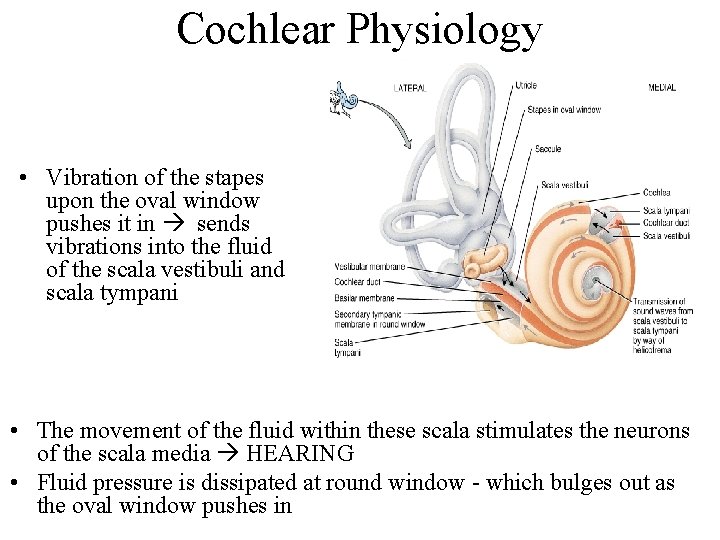
Cochlear Physiology • Vibration of the stapes upon the oval window pushes it in sends vibrations into the fluid of the scala vestibuli and scala tympani • The movement of the fluid within these scala stimulates the neurons of the scala media HEARING • Fluid pressure is dissipated at round window - which bulges out as the oval window pushes in
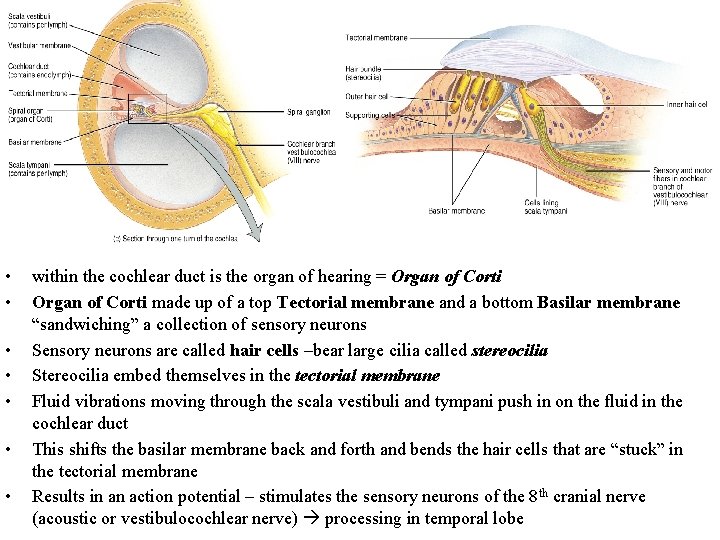
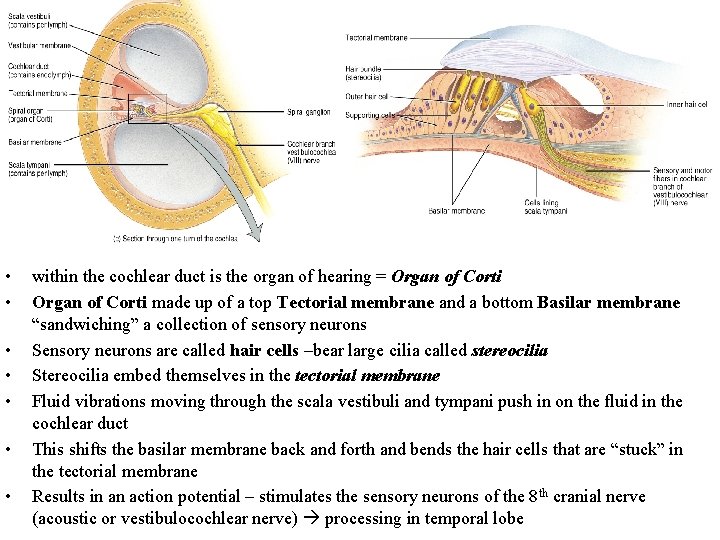
• • within the cochlear duct is the organ of hearing = Organ of Corti made up of a top Tectorial membrane and a bottom Basilar membrane “sandwiching” a collection of sensory neurons Sensory neurons are called hair cells –bear large cilia called stereocilia Stereocilia embed themselves in the tectorial membrane Fluid vibrations moving through the scala vestibuli and tympani push in on the fluid in the cochlear duct This shifts the basilar membrane back and forth and bends the hair cells that are “stuck” in the tectorial membrane Results in an action potential – stimulates the sensory neurons of the 8 th cranial nerve (acoustic or vestibulocochlear nerve) processing in temporal lobe
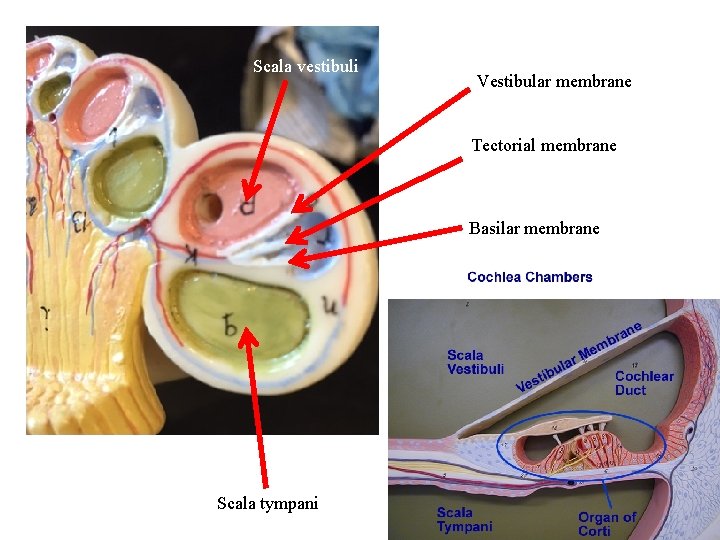
Scala vestibuli Vestibular membrane Tectorial membrane Basilar membrane Scala tympani
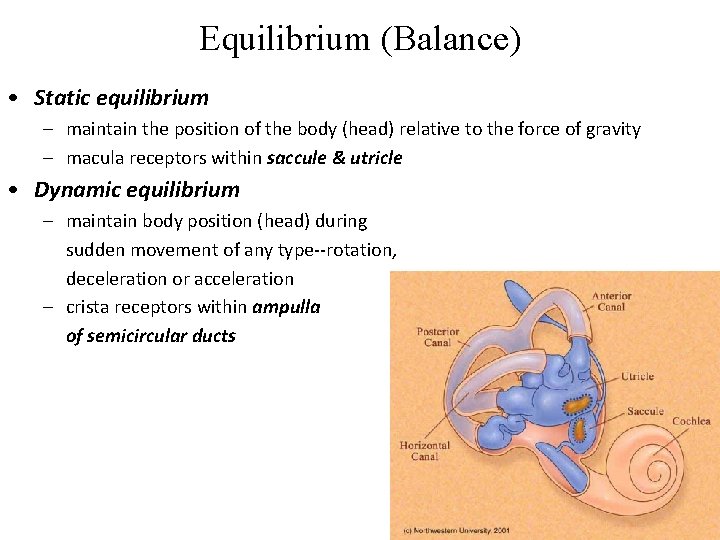
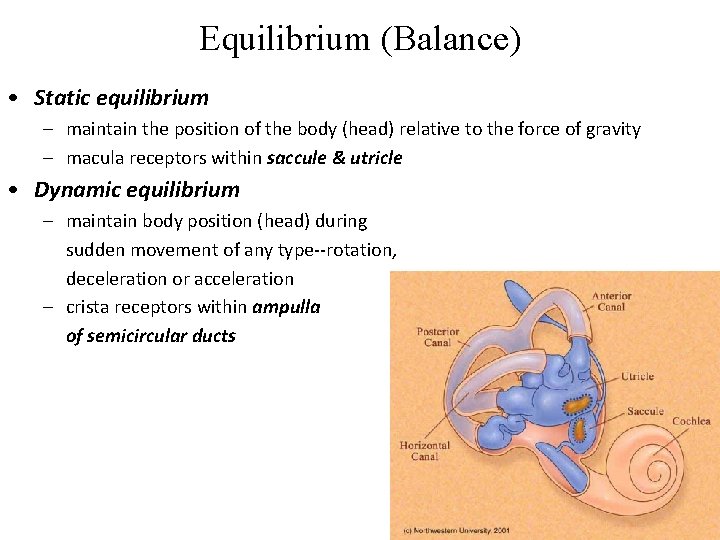
Equilibrium (Balance) • Static equilibrium – maintain the position of the body (head) relative to the force of gravity – macula receptors within saccule & utricle • Dynamic equilibrium – maintain body position (head) during sudden movement of any type--rotation, deceleration or acceleration – crista receptors within ampulla of semicircular ducts
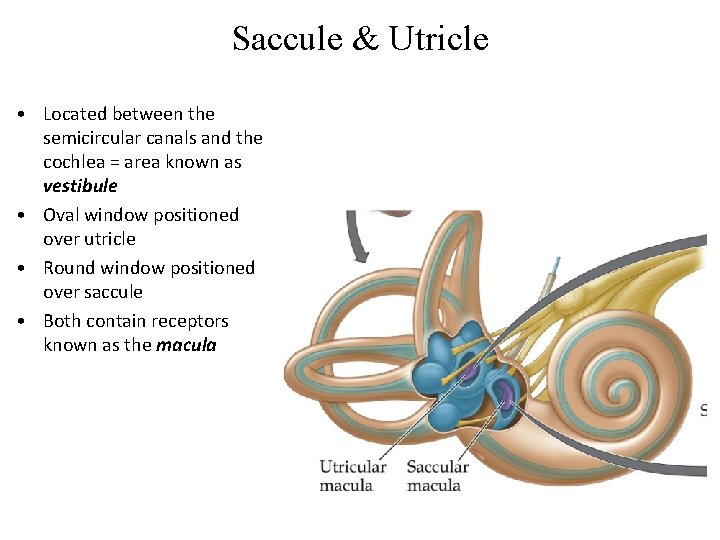
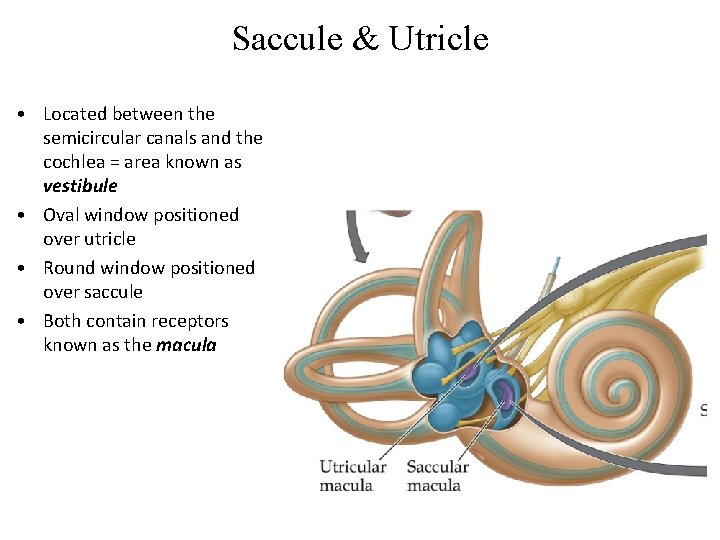
Saccule & Utricle • Located between the semicircular canals and the cochlea = area known as vestibule • Oval window positioned over utricle • Round window positioned over saccule • Both contain receptors known as the macula
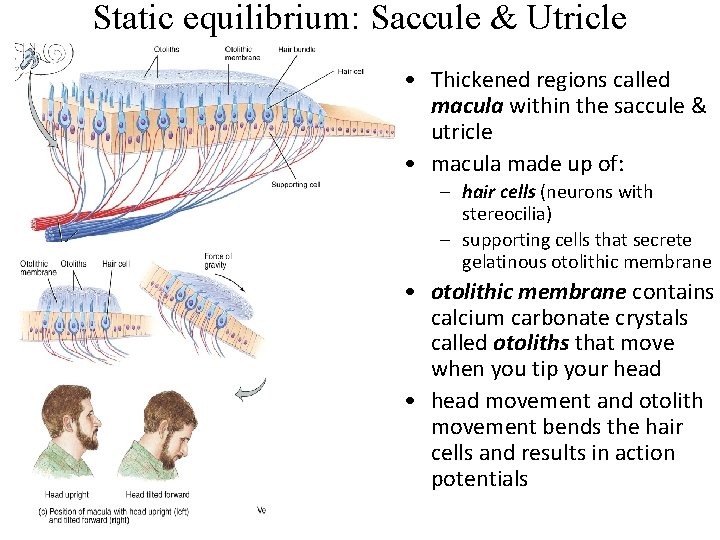
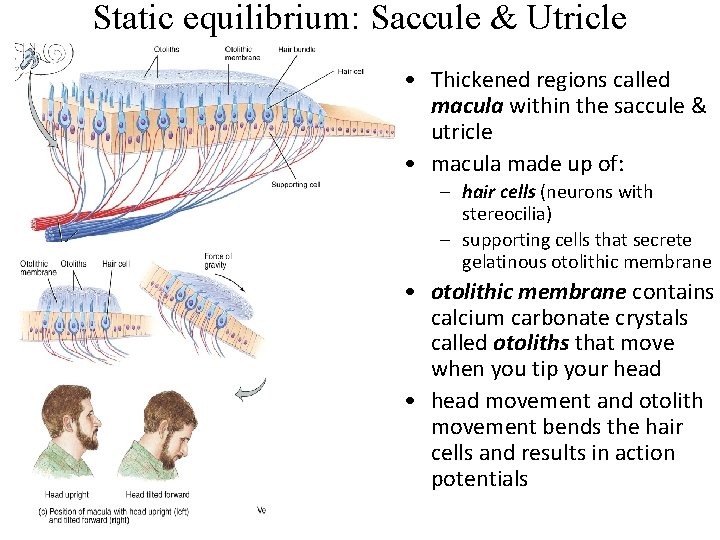
Static equilibrium: Saccule & Utricle • Thickened regions called macula within the saccule & utricle • macula made up of: – hair cells (neurons with stereocilia) – supporting cells that secrete gelatinous otolithic membrane • otolithic membrane contains calcium carbonate crystals called otoliths that move when you tip your head • head movement and otolith movement bends the hair cells and results in action potentials
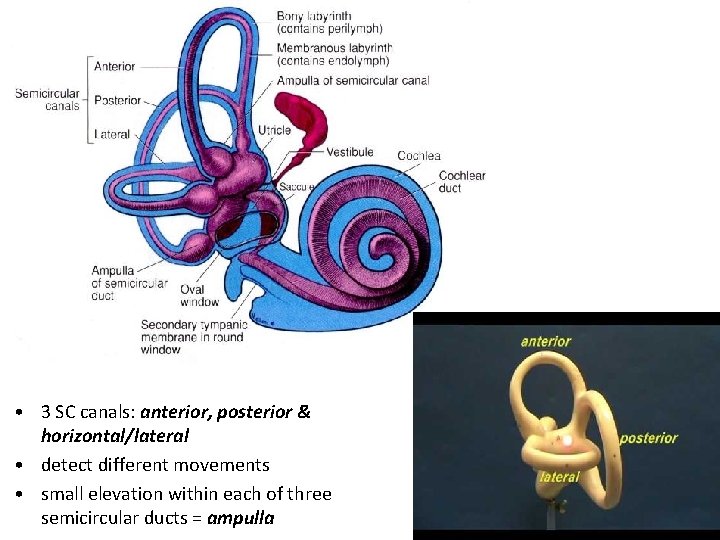
• 3 SC canals: anterior, posterior & horizontal/lateral • detect different movements • small elevation within each of three semicircular ducts = ampulla
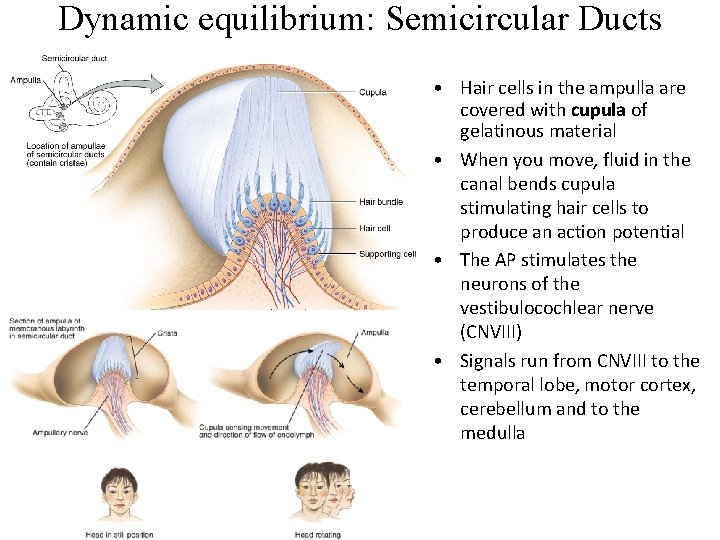
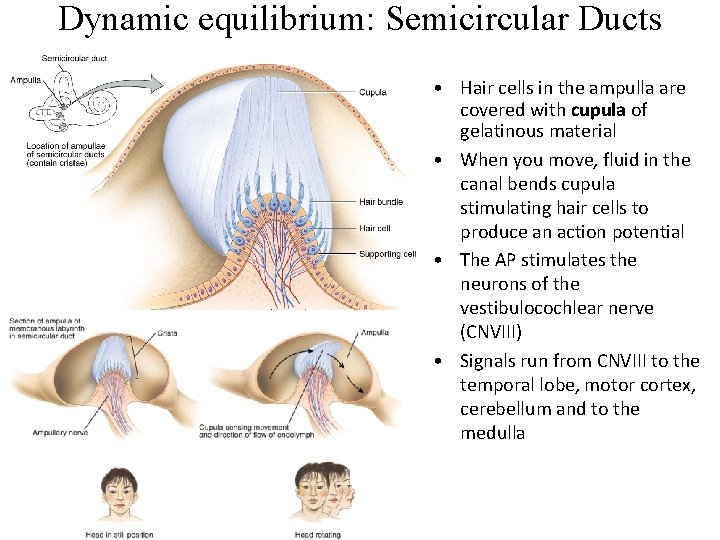
Dynamic equilibrium: Semicircular Ducts • Hair cells in the ampulla are covered with cupula of gelatinous material • When you move, fluid in the canal bends cupula stimulating hair cells to produce an action potential • The AP stimulates the neurons of the vestibulocochlear nerve (CNVIII) • Signals run from CNVIII to the temporal lobe, motor cortex, cerebellum and to the medulla
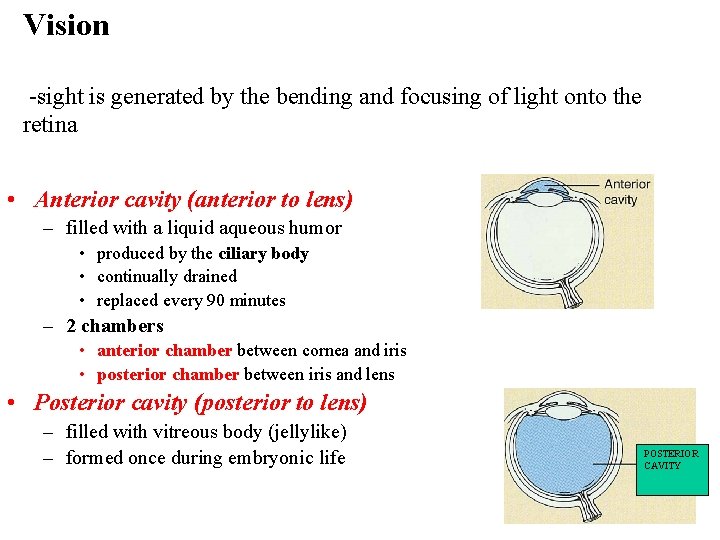
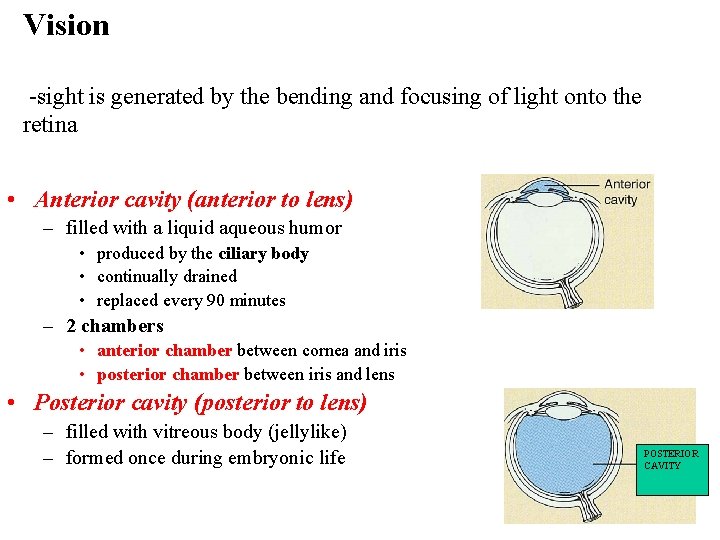
Vision -sight is generated by the bending and focusing of light onto the retina • Anterior cavity (anterior to lens) – filled with a liquid aqueous humor • produced by the ciliary body • continually drained • replaced every 90 minutes – 2 chambers • anterior chamber between cornea and iris • posterior chamber between iris and lens • Posterior cavity (posterior to lens) – filled with vitreous body (jellylike) – formed once during embryonic life POSTERIOR CAVITY
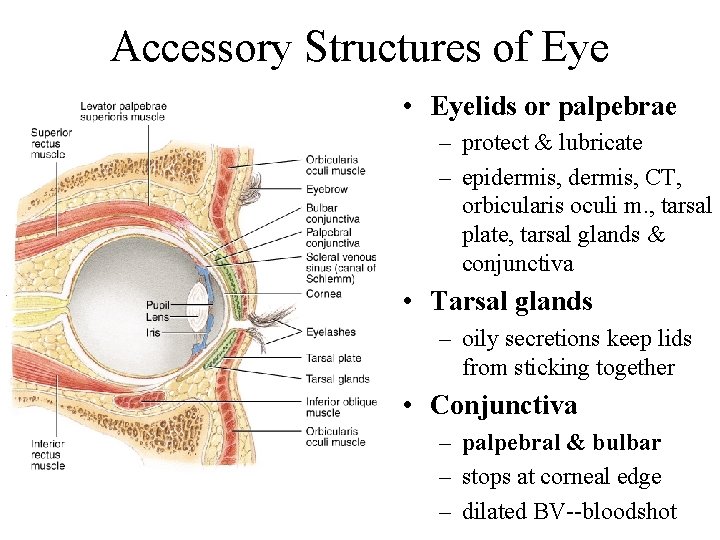
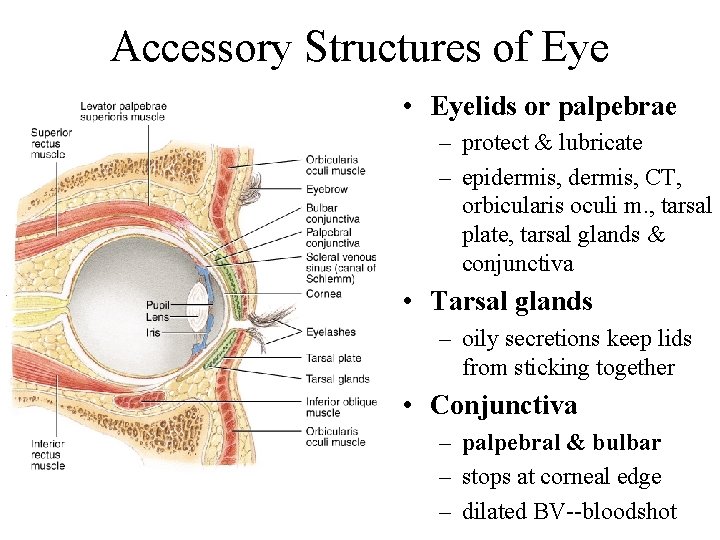
Accessory Structures of Eye • Eyelids or palpebrae – protect & lubricate – epidermis, CT, orbicularis oculi m. , tarsal plate, tarsal glands & conjunctiva • Tarsal glands – oily secretions keep lids from sticking together • Conjunctiva – palpebral & bulbar – stops at corneal edge – dilated BV--bloodshot
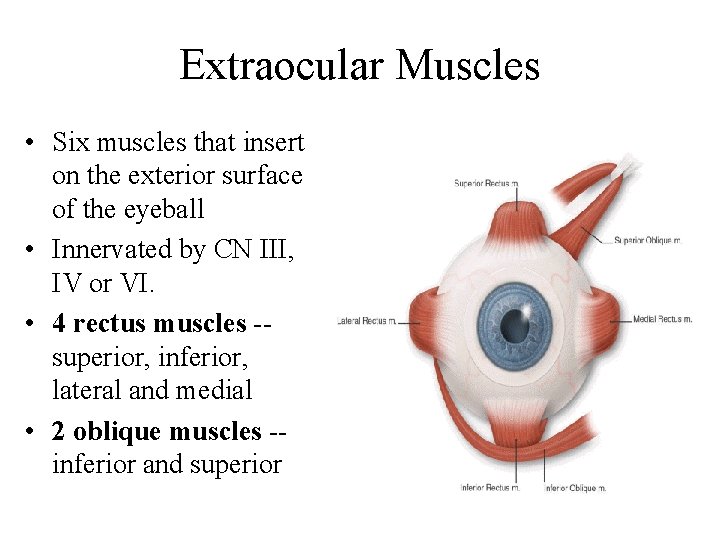
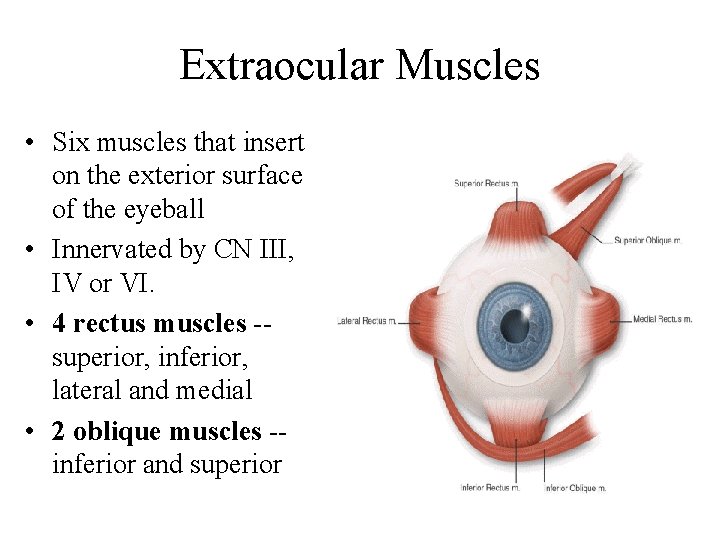
Extraocular Muscles • Six muscles that insert on the exterior surface of the eyeball • Innervated by CN III, IV or VI. • 4 rectus muscles -superior, inferior, lateral and medial • 2 oblique muscles -inferior and superior
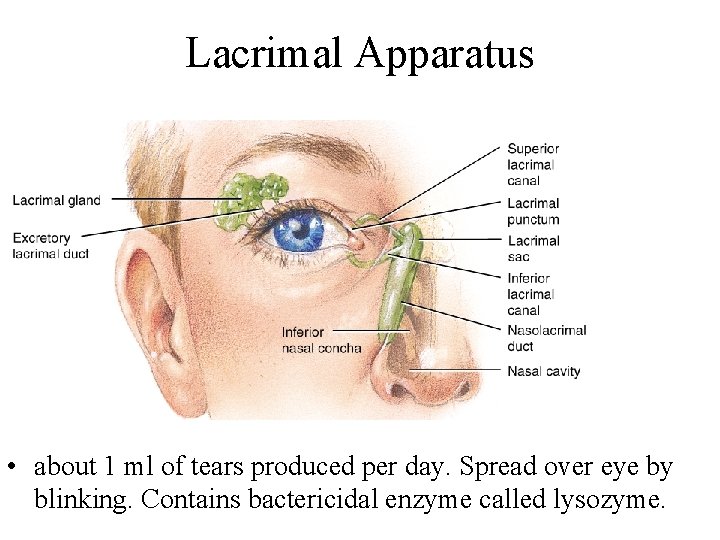
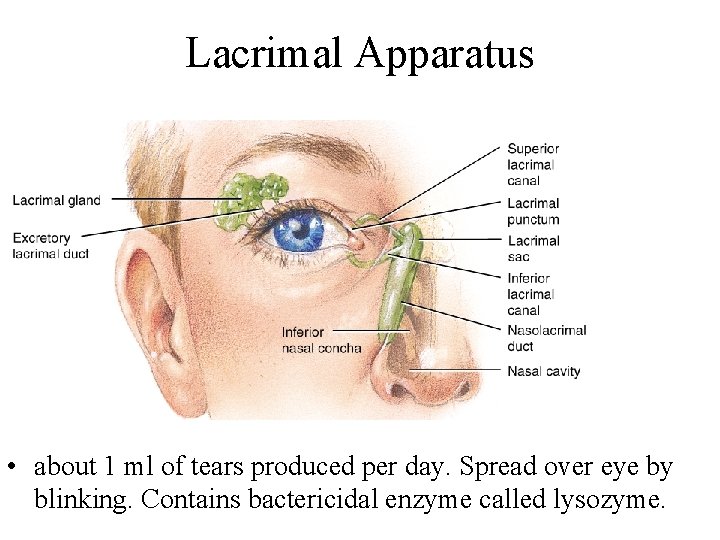
Lacrimal Apparatus • about 1 ml of tears produced per day. Spread over eye by blinking. Contains bactericidal enzyme called lysozyme.
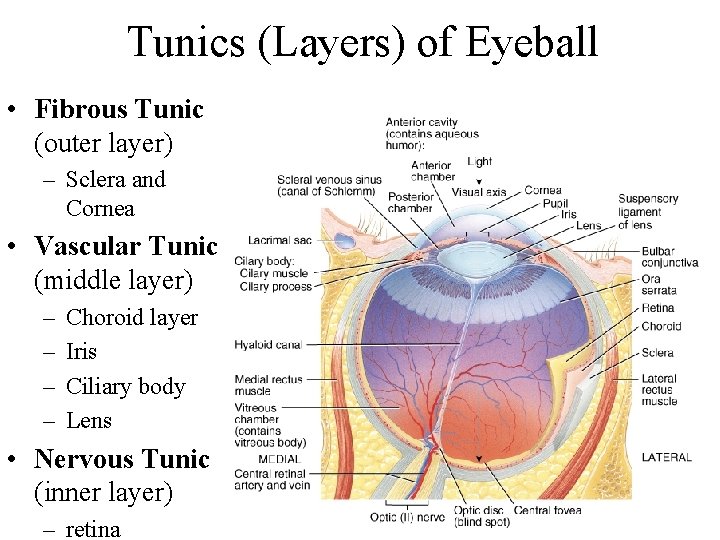
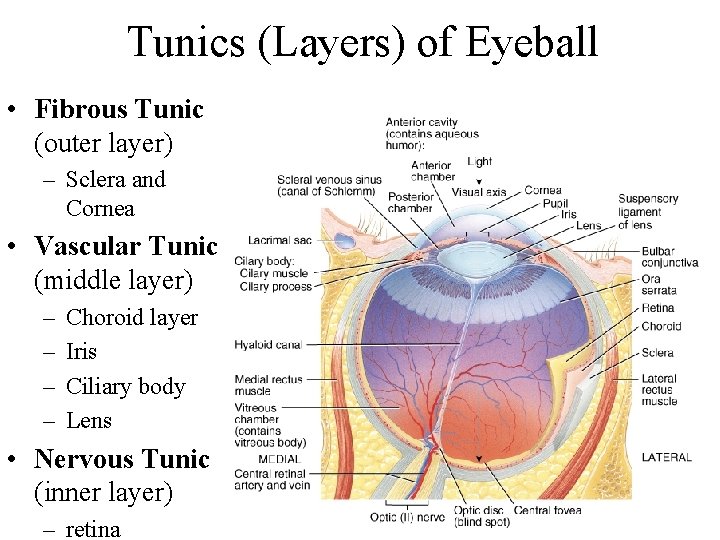
Tunics (Layers) of Eyeball • Fibrous Tunic (outer layer) – Sclera and Cornea • Vascular Tunic (middle layer) – – Choroid layer Iris Ciliary body Lens • Nervous Tunic (inner layer) – retina
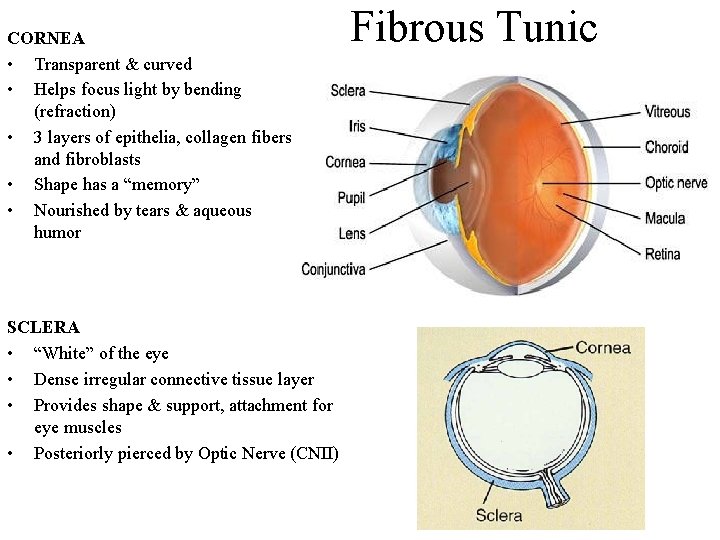
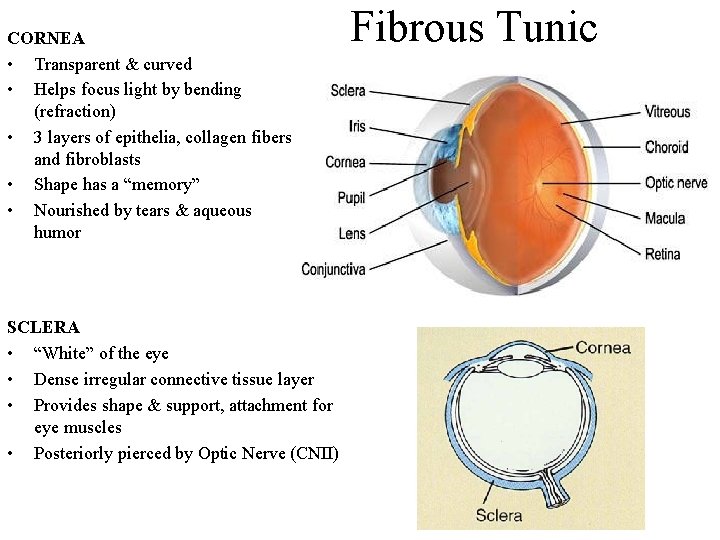
CORNEA • Transparent & curved • Helps focus light by bending (refraction) • 3 layers of epithelia, collagen fibers and fibroblasts • Shape has a “memory” • Nourished by tears & aqueous humor SCLERA • “White” of the eye • Dense irregular connective tissue layer • Provides shape & support, attachment for eye muscles • Posteriorly pierced by Optic Nerve (CNII) Fibrous Tunic
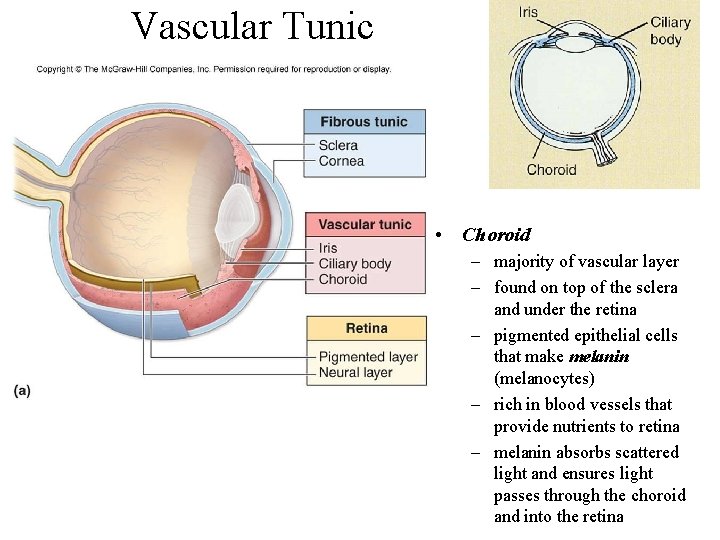
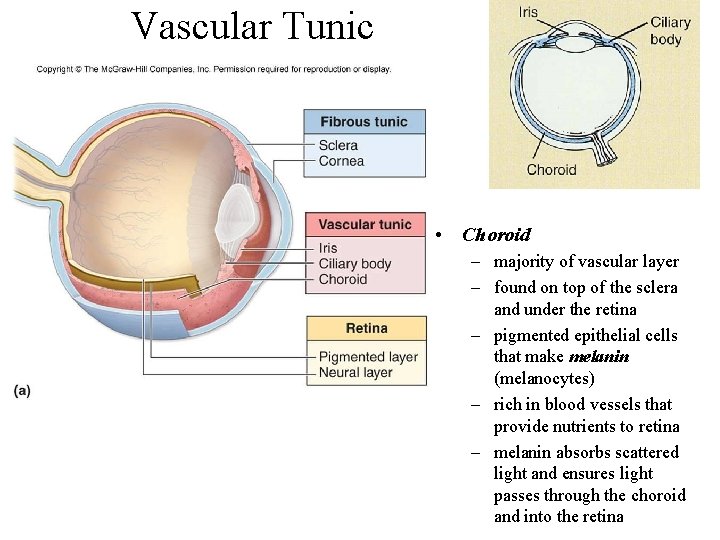
Vascular Tunic • Choroid – majority of vascular layer – found on top of the sclera and under the retina – pigmented epithelial cells that make melanin (melanocytes) – rich in blood vessels that provide nutrients to retina – melanin absorbs scattered light and ensures light passes through the choroid and into the retina
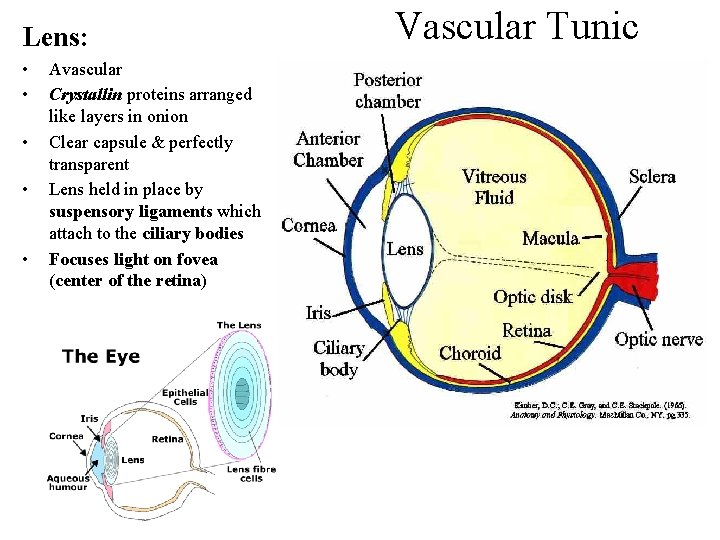
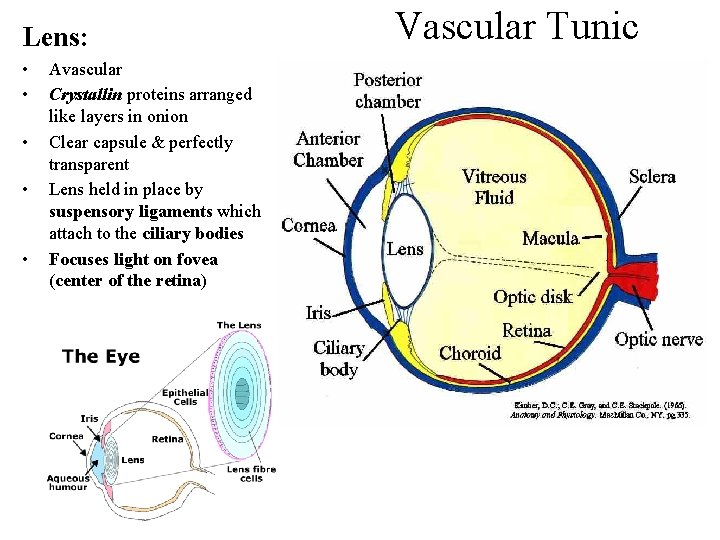
Lens: • • • Avascular Crystallin proteins arranged like layers in onion Clear capsule & perfectly transparent Lens held in place by suspensory ligaments which attach to the ciliary bodies Focuses light on fovea (center of the retina) Vascular Tunic
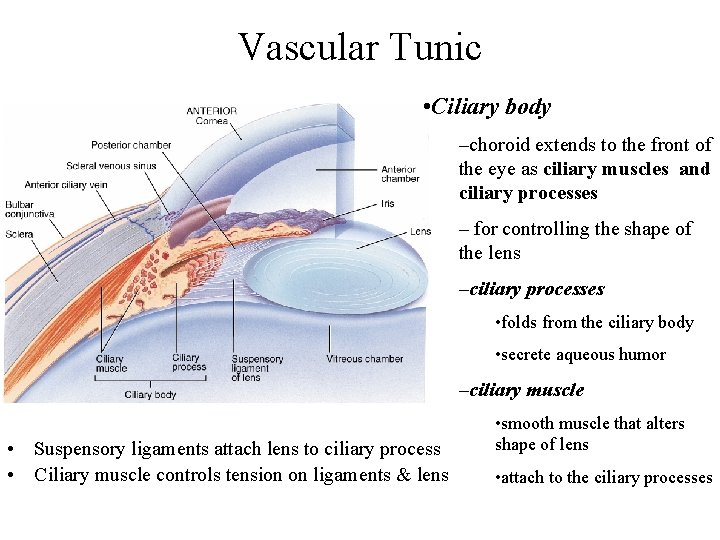
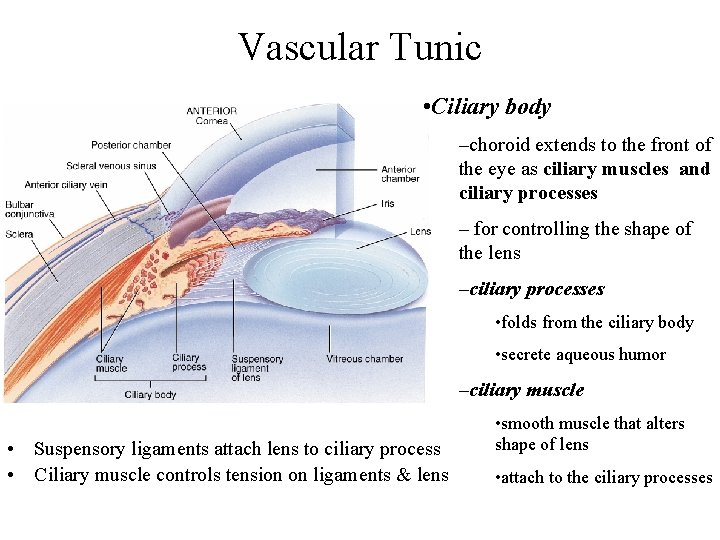
Vascular Tunic • Ciliary body –choroid extends to the front of the eye as ciliary muscles and ciliary processes – for controlling the shape of the lens –ciliary processes • folds from the ciliary body • secrete aqueous humor –ciliary muscle • Suspensory ligaments attach lens to ciliary process • Ciliary muscle controls tension on ligaments & lens • smooth muscle that alters shape of lens • attach to the ciliary processes
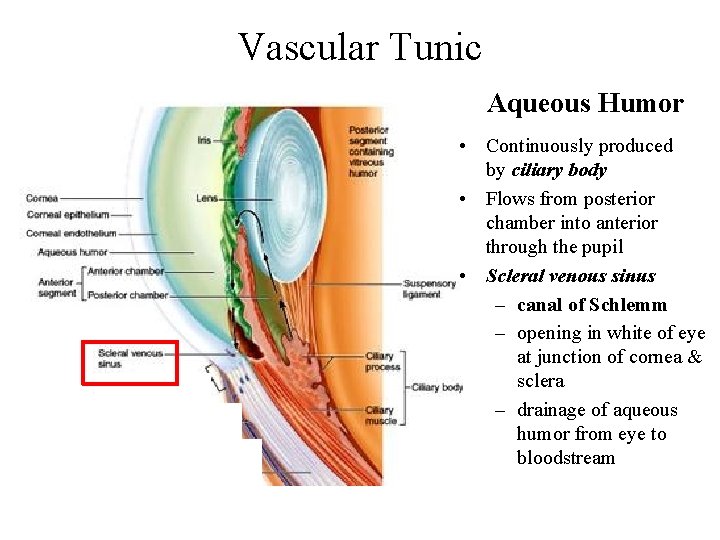
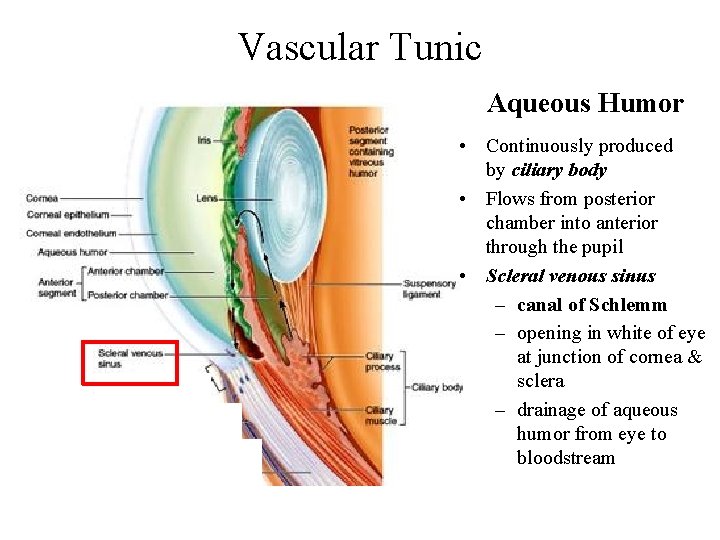
Vascular Tunic Aqueous Humor • Continuously produced by ciliary body • Flows from posterior chamber into anterior through the pupil • Scleral venous sinus – canal of Schlemm – opening in white of eye at junction of cornea & sclera – drainage of aqueous humor from eye to bloodstream
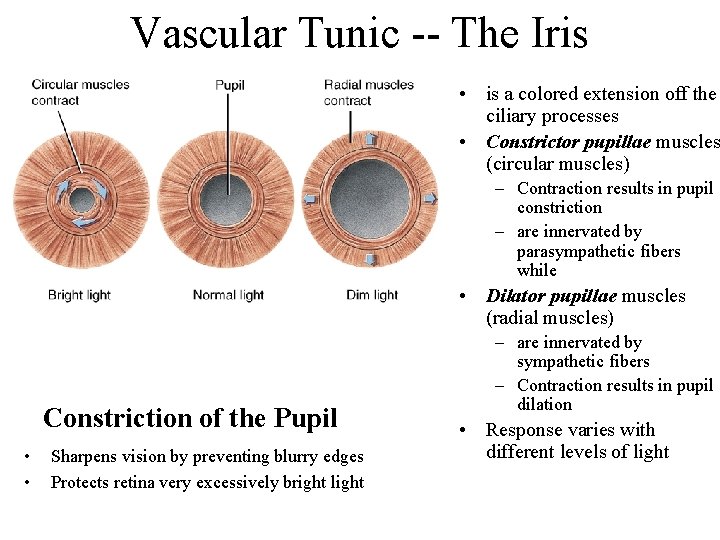
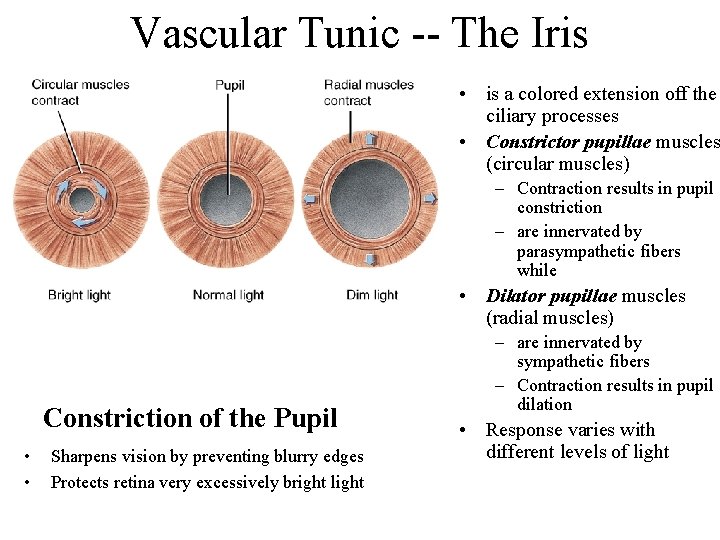
Vascular Tunic -- The Iris • is a colored extension off the ciliary processes • Constrictor pupillae muscles (circular muscles) – Contraction results in pupil constriction – are innervated by parasympathetic fibers while • Dilator pupillae muscles (radial muscles) Constriction of the Pupil • • Sharpens vision by preventing blurry edges Protects retina very excessively bright light – are innervated by sympathetic fibers – Contraction results in pupil dilation • Response varies with different levels of light
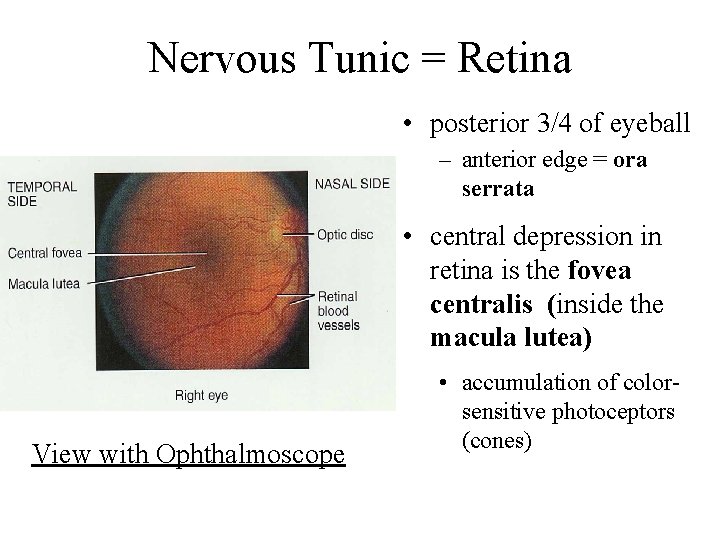
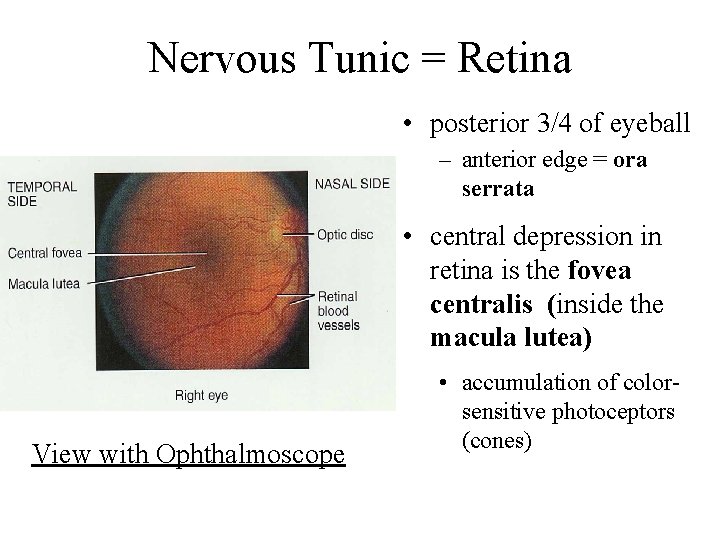
Nervous Tunic = Retina • posterior 3/4 of eyeball – anterior edge = ora serrata • central depression in retina is the fovea centralis (inside the macula lutea) View with Ophthalmoscope • accumulation of colorsensitive photoceptors (cones)
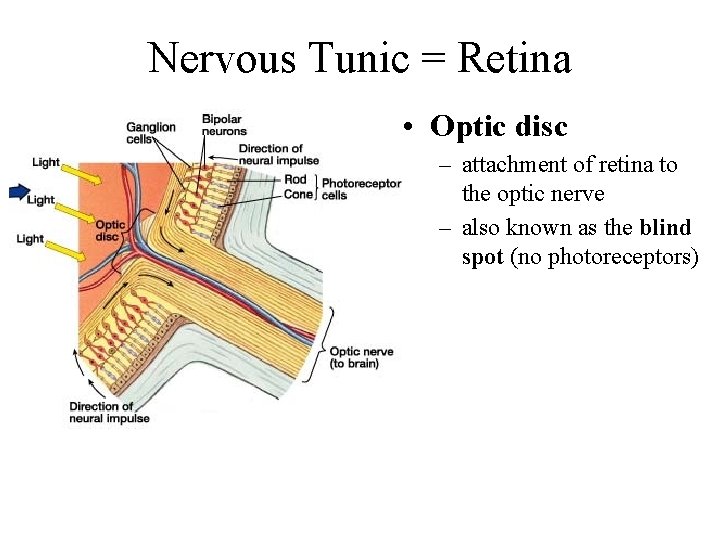
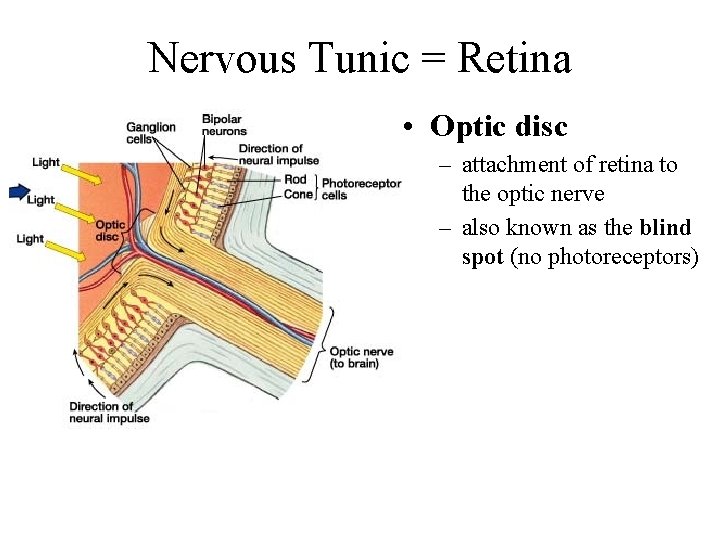
Nervous Tunic = Retina • Optic disc – attachment of retina to the optic nerve – also known as the blind spot (no photoreceptors)
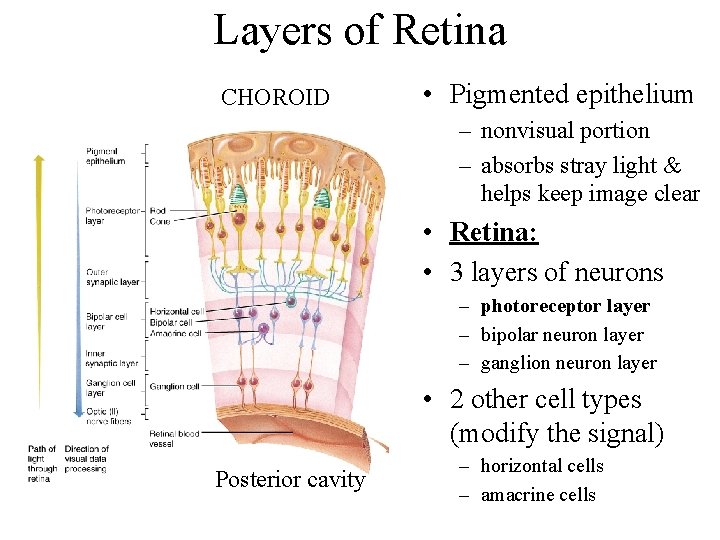
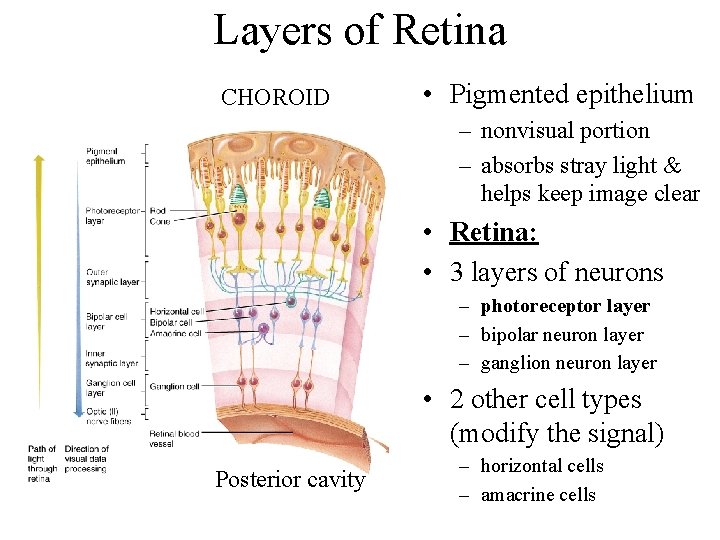
Layers of Retina CHOROID • Pigmented epithelium – nonvisual portion – absorbs stray light & helps keep image clear • Retina: • 3 layers of neurons – photoreceptor layer – bipolar neuron layer – ganglion neuron layer • 2 other cell types (modify the signal) Posterior cavity – horizontal cells – amacrine cells
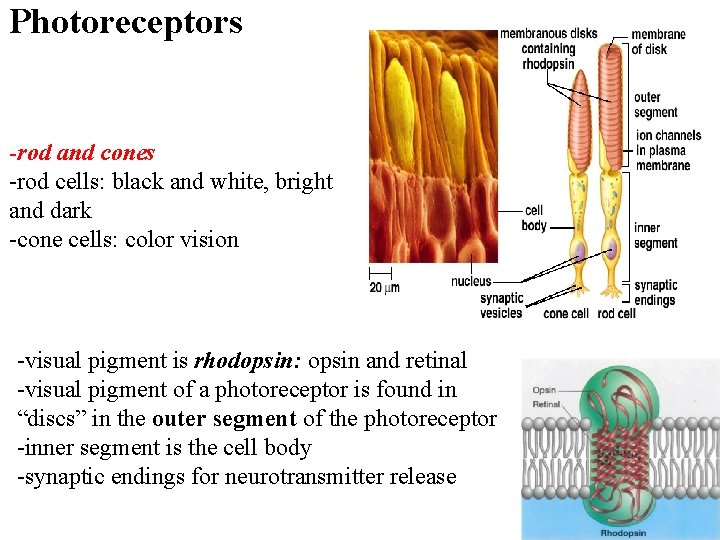
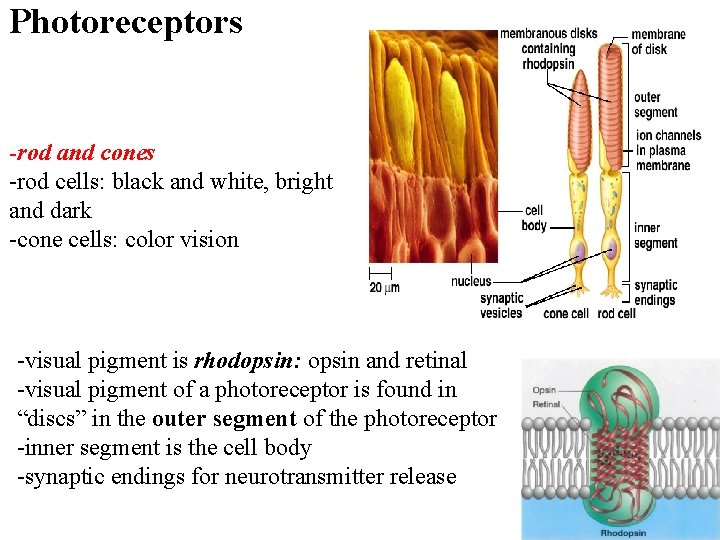
Photoreceptors -rod and cones -rod cells: black and white, bright and dark -cone cells: color vision -visual pigment is rhodopsin: opsin and retinal -visual pigment of a photoreceptor is found in “discs” in the outer segment of the photoreceptor -inner segment is the cell body -synaptic endings for neurotransmitter release
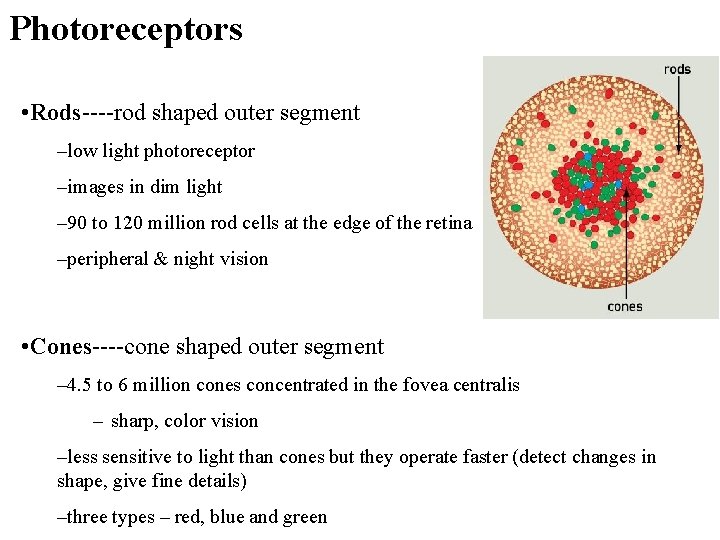
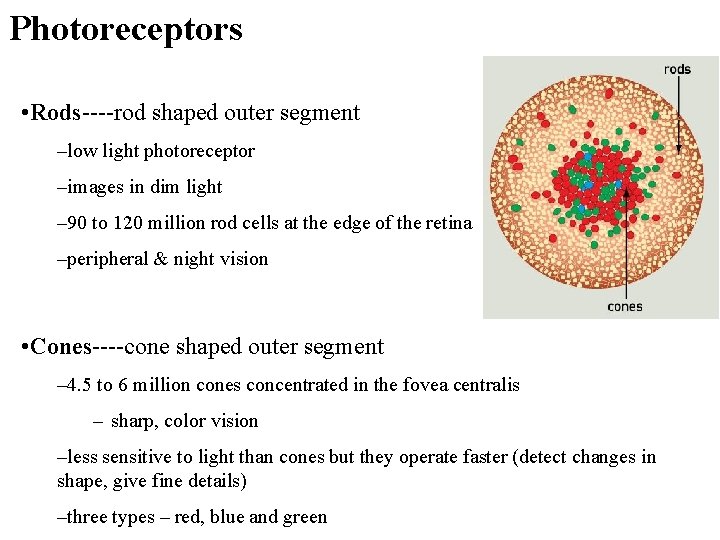
Photoreceptors • Rods----rod shaped outer segment –low light photoreceptor –images in dim light – 90 to 120 million rod cells at the edge of the retina –peripheral & night vision • Cones----cone shaped outer segment – 4. 5 to 6 million cones concentrated in the fovea centralis – sharp, color vision –less sensitive to light than cones but they operate faster (detect changes in shape, give fine details) –three types – red, blue and green
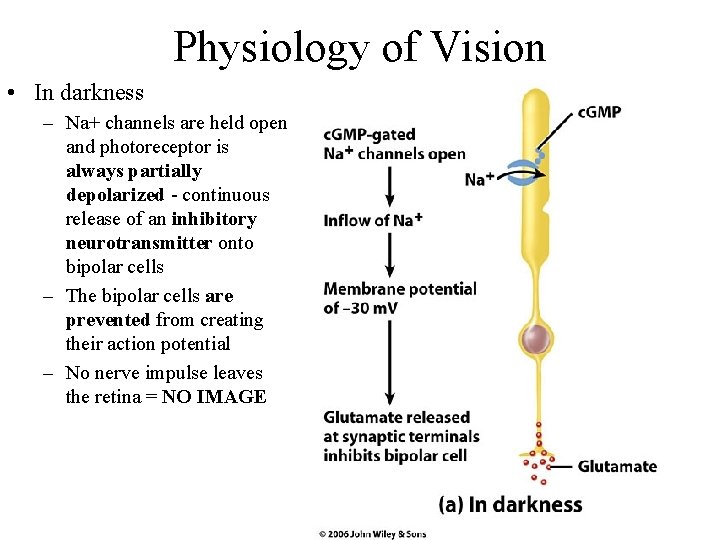
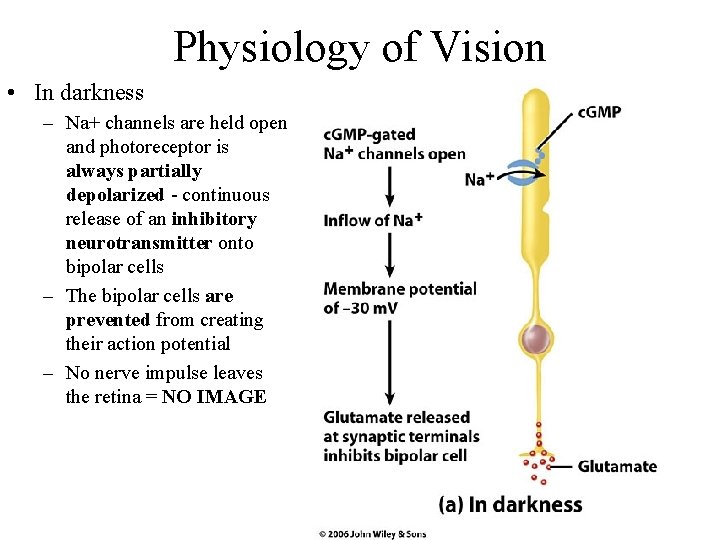
Physiology of Vision • In darkness – Na+ channels are held open and photoreceptor is always partially depolarized - continuous release of an inhibitory neurotransmitter onto bipolar cells – The bipolar cells are prevented from creating their action potential – No nerve impulse leaves the retina = NO IMAGE
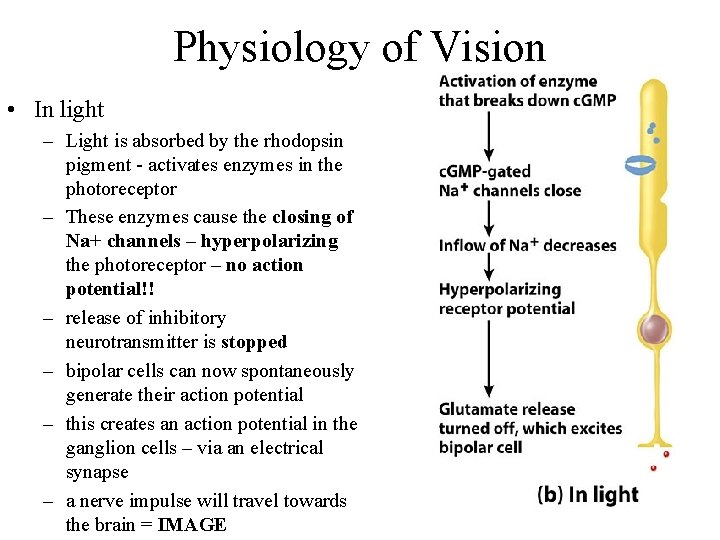
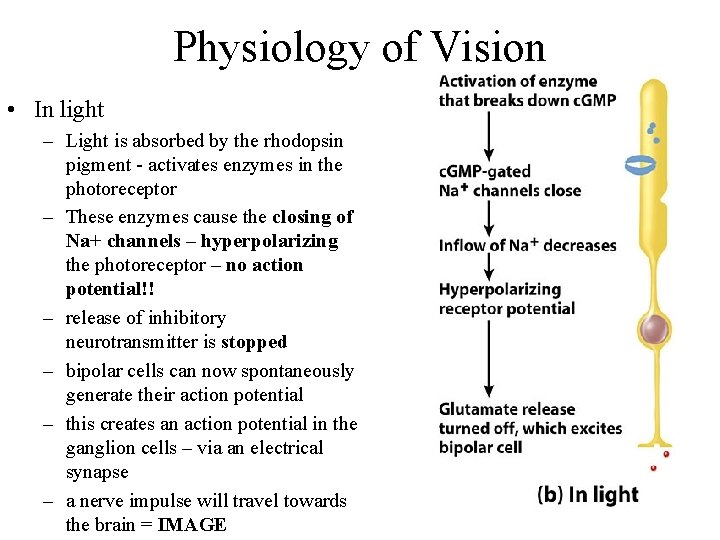
Physiology of Vision • In light – Light is absorbed by the rhodopsin pigment - activates enzymes in the photoreceptor – These enzymes cause the closing of Na+ channels – hyperpolarizing the photoreceptor – no action potential!! – release of inhibitory neurotransmitter is stopped – bipolar cells can now spontaneously generate their action potential – this creates an action potential in the ganglion cells – via an electrical synapse – a nerve impulse will travel towards the brain = IMAGE
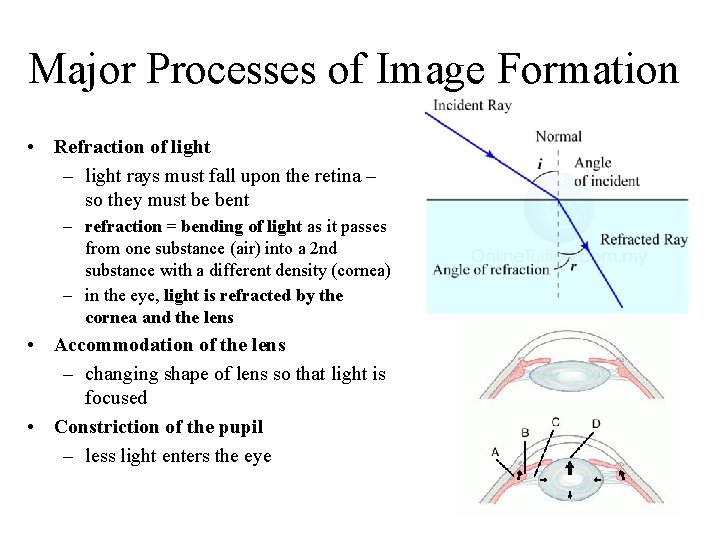
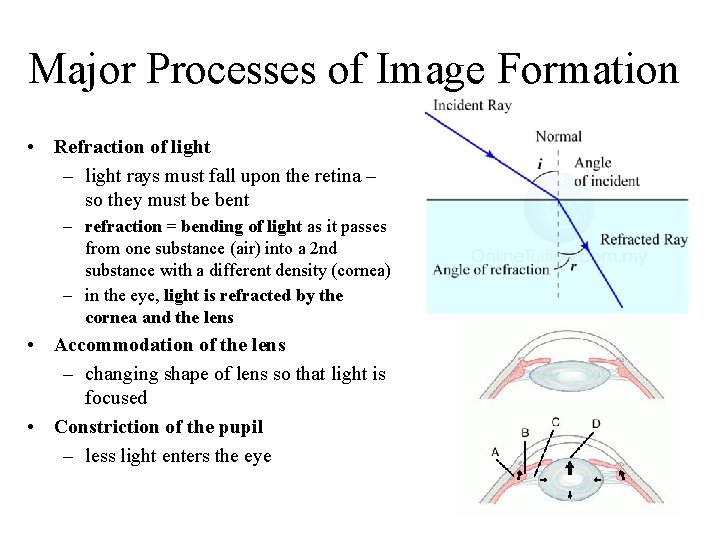
Major Processes of Image Formation • Refraction of light – light rays must fall upon the retina – so they must be bent – refraction = bending of light as it passes from one substance (air) into a 2 nd substance with a different density (cornea) – in the eye, light is refracted by the cornea and the lens • Accommodation of the lens – changing shape of lens so that light is focused • Constriction of the pupil – less light enters the eye
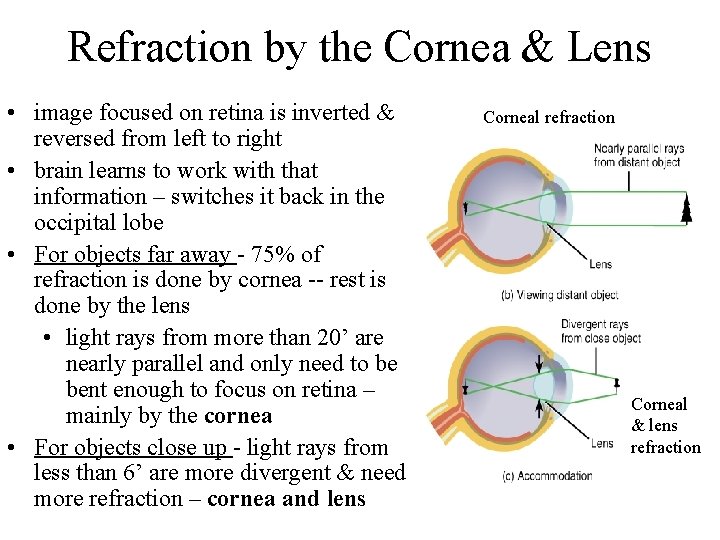
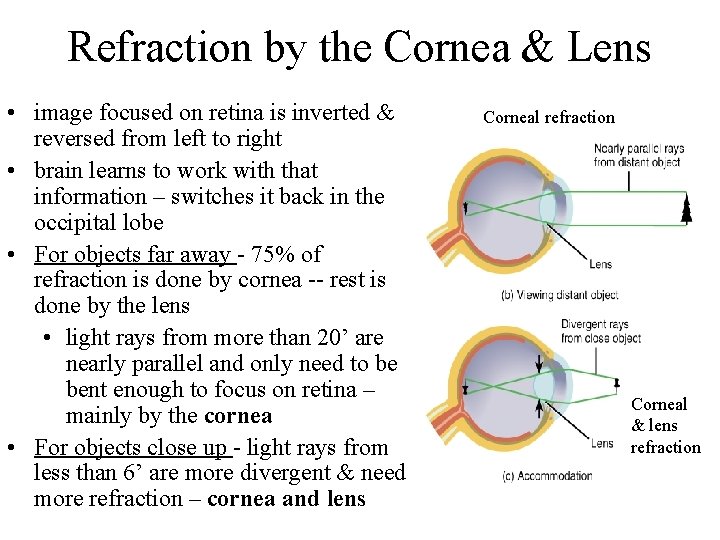
Refraction by the Cornea & Lens • image focused on retina is inverted & reversed from left to right • brain learns to work with that information – switches it back in the occipital lobe • For objects far away - 75% of refraction is done by cornea -- rest is done by the lens • light rays from more than 20’ are nearly parallel and only need to be bent enough to focus on retina – mainly by the cornea • For objects close up - light rays from less than 6’ are more divergent & need more refraction – cornea and lens Corneal refraction Corneal & lens refraction
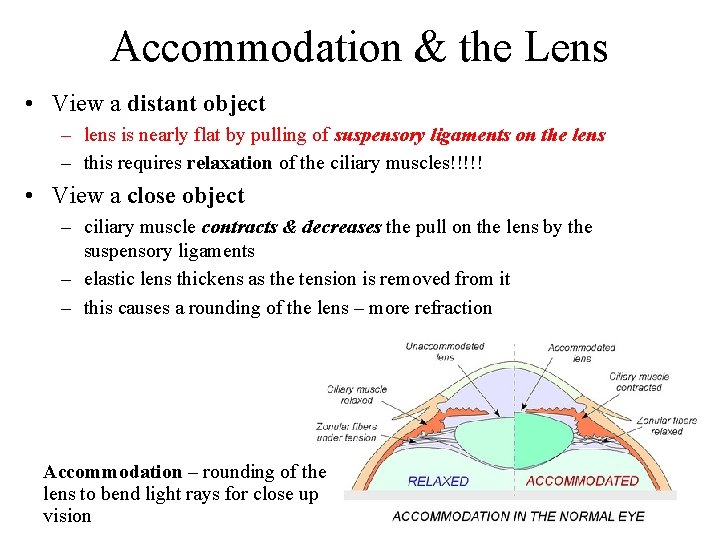
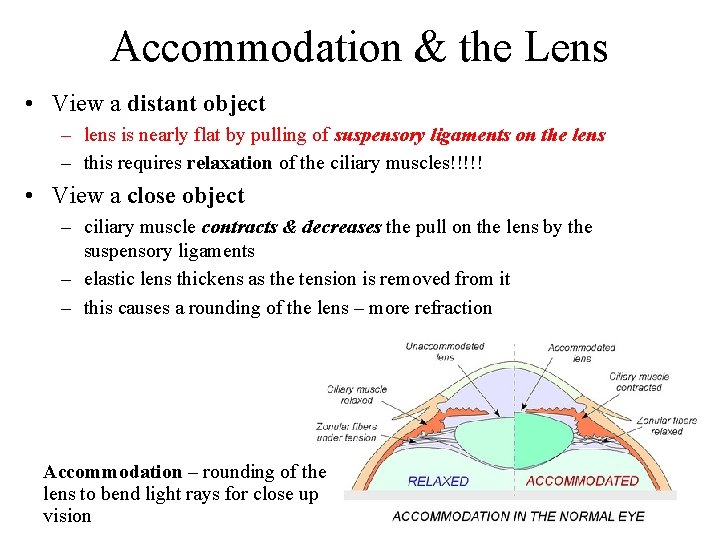
Accommodation & the Lens • View a distant object – lens is nearly flat by pulling of suspensory ligaments on the lens – this requires relaxation of the ciliary muscles!!!!! • View a close object – ciliary muscle contracts & decreases the pull on the lens by the suspensory ligaments – elastic lens thickens as the tension is removed from it – this causes a rounding of the lens – more refraction Accommodation – rounding of the lens to bend light rays for close up vision
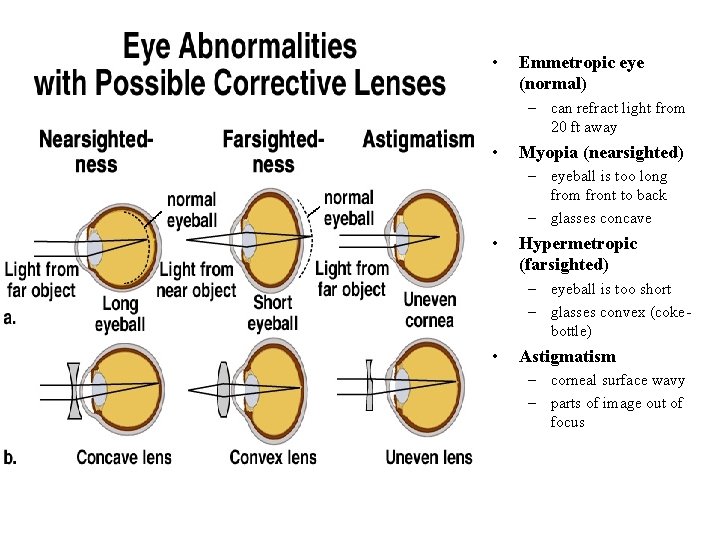
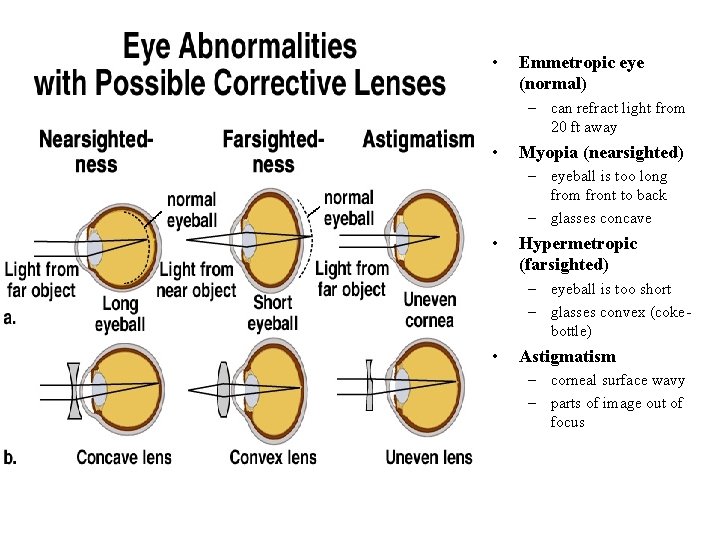
• Emmetropic eye (normal) – can refract light from 20 ft away • Myopia (nearsighted) – eyeball is too long from front to back – glasses concave • Hypermetropic (farsighted) – eyeball is too short – glasses convex (cokebottle) • Astigmatism – corneal surface wavy – parts of image out of focus