The Pillars of Medical Ethics and the Ethical








- Slides: 47
The Pillars of Medical Ethics and the Ethical Basis for Law Charles Ellington, MD, JD SIU School of Medicine Decatur Family Medicine Residency
Objectives • Describe the pillars of medical ethics, including non-maleficence, beneficence, autonomy, and justice • Explain their limitations and clinical application • Discuss basic legal principles that flow from the above, including informed consent

Pillars of Medical Ethics • • Non-Maleficence Beneficence Autonomy Distributive Justice


Non-Maleficence • Primum non nocere: First do no harm • Hippocratic oath: “I will use treatment to help the sick according to my ability and judgment, but will never use it to injure or wrong them. ”
First rule of ethics • Many argue overrides all other ethical concerns • Clinical Case – A transplant surgeon kills a death row inmate so he may harvest his heart and liver, thus saving two lives. Is this ethical?

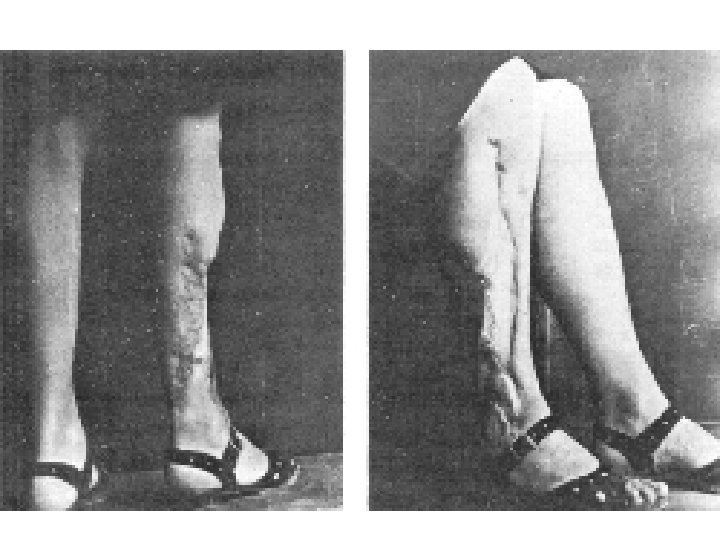
First rule of ethics? • An oncologist gives chemotherapy to a woman with breast cancer in hopes of curing her cancer. Unfortunately, she develops congestive heart failure as a result of her treatment. Is this ethical?
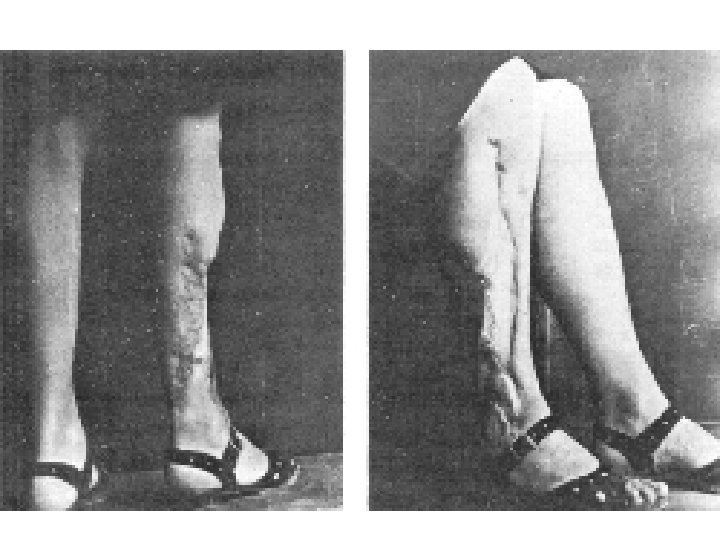
Negligence • The concept of medical malpractice or negligence is related to the duty no to harm • Medical negligence occurs when a physician breaches a duty and as a result of that breach, harms a patient
Beneficence • An action done to benefit others • Hippocratic Oath: physicians will “come for the benefit of the sick” • Differs from non-maleficence in that beneficence is a positive requirement for action, whereas non-maleficence is a negative prohibition against action
Is Beneficence Obligatory? • A physician is driving down the street and sees an automobile accident. Is the physician morally obligated to respond? • What if the physician is an opthalmologist? • Are there times when beneficence is required by ethics? By law?
Required Beneficence • Specific beneficence: directed at specific parties such as children, patients, etc. • General beneficence: directed to society in general
Required Beneficence • What are some specific positive actions the law requires of physicians or others?
Physician-Patient Relationship • Is created when a patient requests and a physician agrees to provide medical care • Creates special obligations for physician – Provide medical care in accordance with standard of care – Not abandon patient (provide care if needed until relationship properly terminated)

Paternalism • Deciding what is best for another person and overriding their preferences or choices • At tension with autonomy
Paternalism • At a routine visit, you notice a 55 year-old patient of yours has never had a mammogram. On questioning, the patient says she prefers not to have one—that they are uncomfortable and she does not see the need. You explain mammograms save lives, and instruct your nurse to schedule a mammogram as soon as possible. Is this ethical? What if you simply handed her an order and told her to make the appointment?
Paternalism • A 68 year-old male patient of yours suffers from alzheimer’s dementia. He develops hemoptysis, hoarseness, and weight loss. CT scan shows suspected late stage bronchogenic carcinoma. The patient’s wife pleads with you not to tell her husband the suspected diagnosis because she is concerned he may kill himself if he finds out. What should you do?

Autonomy • Principle of self-rule or self-governance • Based on respect for individual and value of a person as an end in itself • Also influenced by humility—it is difficult or impossible to know what is best for someone else
Preconditions for Autonomy • Liberty or freedom to choose • Agency or capacity to choose
Rules Flowing from Autonomy • Truth telling • Confidentiality and privacy • Informed consent
Informed Consent • A communication process between the physician and patient whereby a fully informed patient can participate in healthcare decision-making
Legal Duty • A physician has a legal duty to inform the patient of the condition, differential diagnoses, the purpose of tests, treatment options, risks, alternatives, prognosis and expectations Canterbury v. Spence, 464 F. 2 d 772 (D. C. Cir. 1972)
Preconditions • Patient must have capacity to consent – If at issue, document process for determining if someone has capacity • If a patient lack capacity, a surrogate decision-maker must provide informed consent
What Must Be Disclosed • Nature of treatment or procedure • Expected outcome and likelihood of success • Reasonable alternatives • Material risks
Material Risks • Risks that are very slight or rare do not have to be disclosed • Some states require any risk that would impact a patient’s decision be disclosed • Alternative treatments that carry fewer risks must be disclosed
Legal Standard Applied • Professional disclosure standard (majority including IL): Was the disclosure or nondisclosure consistent with the community medical practice
Special Cases • • • Pediatric patients Emancipated minors Mature minors Pregnant patients Minors seeking certain care (STD treatment or birth control; drug, ETOH, or psychiatric treatment) • Emergencies
Exceptions • • Therapeutic privilege Patient asks not to be informed Common knowledge Emergency
Informed Refusal • Corollary to informed consent • Places a duty on physician to disclose material risks for refusing to undergo low risk procedure (e. g. pap smear) Truman v. Thomas, 165 Cal Rptr. 308, 611 P. 2 d 902 (1980).


Distributive Justice • Fair, equitable, and appropriate distribution of resources • Especially relevant for healthcare – 45 million Americans uninsured – Significant healthcare disparities • Distribution of scarce resources always requires hard choices
Theories of Justice • Utilitarian: the greatest good for the greatest number • Libertarian: focuses on protecting liberty and property • Communitarian: focuses on responsibility of the community to the individual and based on pluralism • Egalitarian: basic equalities among individuals
Is healthcare a right? • What is the scope of the right? • Against whom is this right asserted? • What are the responsibilities of those possessing such a right? • Is the right to healthcare a positive or negative right?
Clinical Case • You’re a physician serving on a state healthcare reform task force. One issue that has arisen is whether the state will pay for liver transplants for alcoholic related end stage liver disease. One proposal is not to pay at all. Another proposal is to pay for it, but place these patients below those without alcohol related disease. What will you recommend and what programs are you willing to cut to pay for it?
Summary • The four pillars of medical ethics provide important guidance for physician behavior • Non-maleficence is considered the first principle of medical ethics but cannot be viewed as isolated from the other principles • Beneficence requires acting in the best interest of another but can become paternalistic
Summary-Cont. • Autonomy is grounded in respect for the individual and serves as the basis for several ethical rules including informed consent • Informed consent requires a physician disclose the nature of the proposed treatment or procedure, expected benefit of proposed treatment and liklihood of success material risks, and alternatives
Summary—Cont. • Distributive justice seeks to make and equitable distribution of scarce resources but always requires hard choices • Ethical theories often overlap and not always separable
 4 pillars of medical ethics
4 pillars of medical ethics The perceived relevance or importance of an ethical issue
The perceived relevance or importance of an ethical issue Perbedaan ethical dilemma dan ethical lapse
Perbedaan ethical dilemma dan ethical lapse Ethical lens of the ethical reasoning model
Ethical lens of the ethical reasoning model Chapter 4 business ethics and social responsibility
Chapter 4 business ethics and social responsibility Medical legal and ethical issues chapter 3
Medical legal and ethical issues chapter 3 Medical legal and ethical issues chapter 3
Medical legal and ethical issues chapter 3 Chapter 3 legal and ethical issues
Chapter 3 legal and ethical issues Macro and micro ethics
Macro and micro ethics Ethical principles of scholastic ethics
Ethical principles of scholastic ethics Ethical dilemma in social work
Ethical dilemma in social work Emancipated minors definition
Emancipated minors definition Medical law and ethics 5th edition
Medical law and ethics 5th edition Ethical problems in the practice of law 5th edition
Ethical problems in the practice of law 5th edition Law versus ethics chapter 3
Law versus ethics chapter 3 What is environmental ethics
What is environmental ethics Briefly summarise
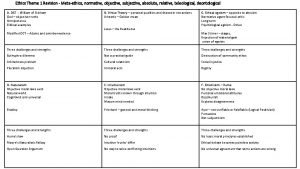
Briefly summarise Descriptive ethics vs normative ethics
Descriptive ethics vs normative ethics Methaethics
Methaethics Descriptive ethics vs normative ethics
Descriptive ethics vs normative ethics Descriptive ethics vs normative ethics
Descriptive ethics vs normative ethics Metaethics vs normative ethics
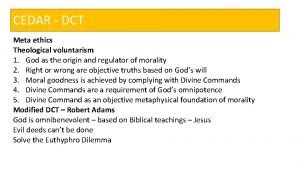
Metaethics vs normative ethics Meta ethics
Meta ethics What is deontological ethics
What is deontological ethics Teleological ethics vs deontological ethics
Teleological ethics vs deontological ethics Difference between medical report and medical certificate
Difference between medical report and medical certificate Medical ethics
Medical ethics Avma principles of veterinary medical ethics
Avma principles of veterinary medical ethics Warning notice in medical ethics
Warning notice in medical ethics Concepts of medical ethics
Concepts of medical ethics Medical ethics lecture
Medical ethics lecture Ethics in medical education
Ethics in medical education Introduction to medical ethics
Introduction to medical ethics Autonomy in greek
Autonomy in greek Professional secrecy in medical ethics
Professional secrecy in medical ethics Medical marijuana ethics
Medical marijuana ethics Noha cosmetics indeed
Noha cosmetics indeed Medical ethics 101
Medical ethics 101 California medical license for foreign medical graduates
California medical license for foreign medical graduates Greater baltimore medical center medical records
Greater baltimore medical center medical records Torrance memorial map
Torrance memorial map Cartersville medical center medical records
Cartersville medical center medical records Nhs 7 pillars
Nhs 7 pillars Media legal issues
Media legal issues Legal and ethical issues in information security
Legal and ethical issues in information security Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Bổ thể
Bổ thể