The Pharmacological Management of Schizophrenia and Antipsychotic Medication
- Slides: 50
The Pharmacological Management of Schizophrenia and Antipsychotic Medication Pearls John Trnka, Pharm. D. , R. Ph. MN NACNS Conference October 5, 2018
Objectives • Describe the various pathophysiological hypotheses of schizophrenia • Compare and contrast the mechanisms of action of antipsychotic medications • Develop a pharmacologic management plan for a patient experiencing adverse effects due to an antipsychotic medication
Which of the following pathophysiological pathways is thought to be most responsible for the symptoms of schizophrenia? A. Glutamate Pathway B. Serotonin Pathway C. Acetylcholine Pathway D. Dopamine Pathway
Which of the following pathophysiological pathways is thought to be most responsible for the symptoms of schizophrenia? A. Glutamate Pathway B. Serotonin Pathway C. Acetylcholine Pathway D. Dopamine Pathway
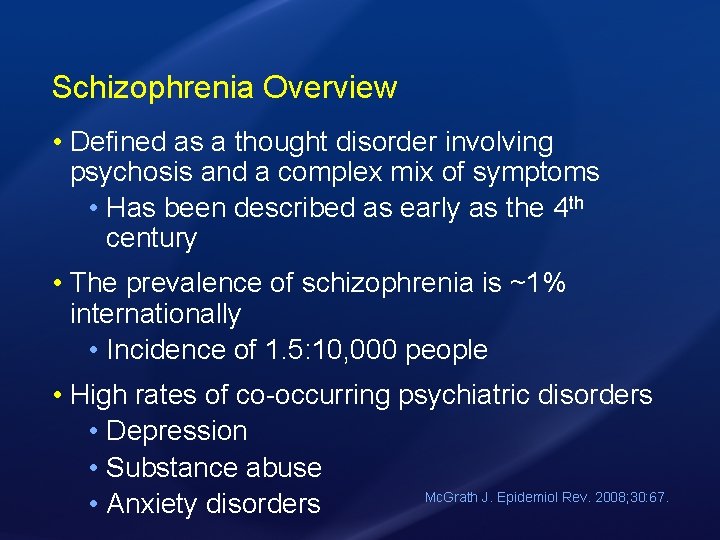
Schizophrenia Overview • Defined as a thought disorder involving psychosis and a complex mix of symptoms • Has been described as early as the 4 th century • The prevalence of schizophrenia is ~1% internationally • Incidence of 1. 5: 10, 000 people • High rates of co-occurring psychiatric disorders • Depression • Substance abuse Mc. Grath J. Epidemiol Rev. 2008; 30: 67. • Anxiety disorders
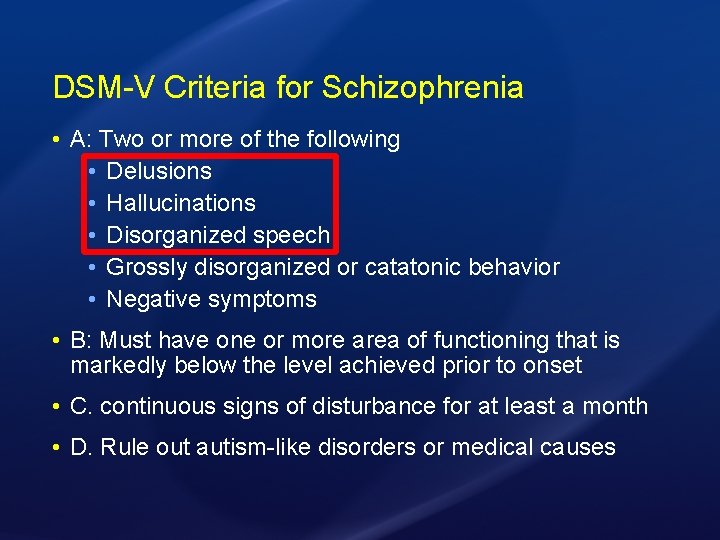
DSM-V Criteria for Schizophrenia • A: Two or more of the following • Delusions • Hallucinations • Disorganized speech • Grossly disorganized or catatonic behavior • Negative symptoms • B: Must have one or more area of functioning that is markedly below the level achieved prior to onset • C. continuous signs of disturbance for at least a month • D. Rule out autism-like disorders or medical causes
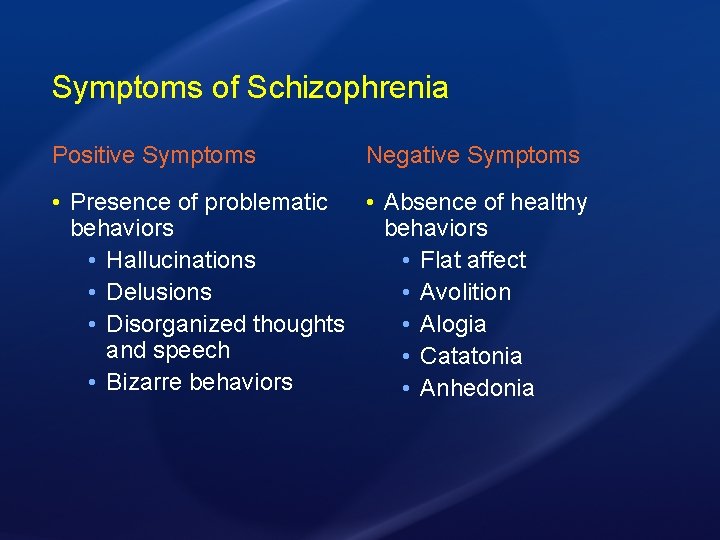
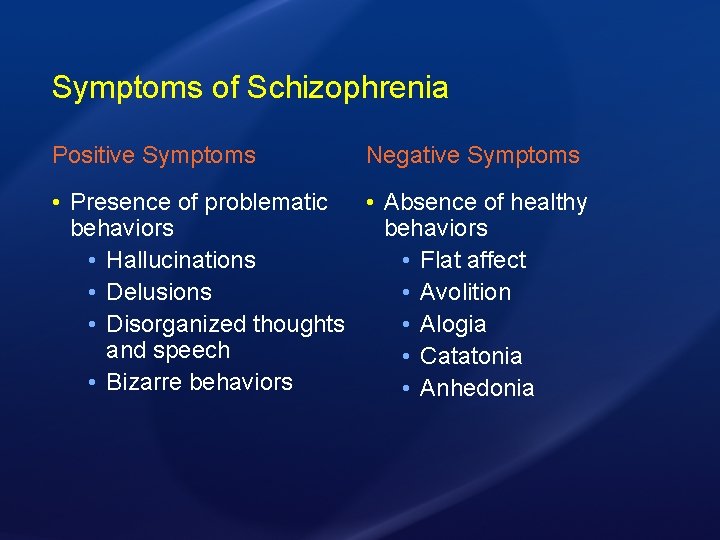
Symptoms of Schizophrenia Positive Symptoms Negative Symptoms • Presence of problematic • Absence of healthy behaviors • Hallucinations • Flat affect • Delusions • Avolition • Disorganized thoughts • Alogia and speech • Catatonia • Bizarre behaviors • Anhedonia
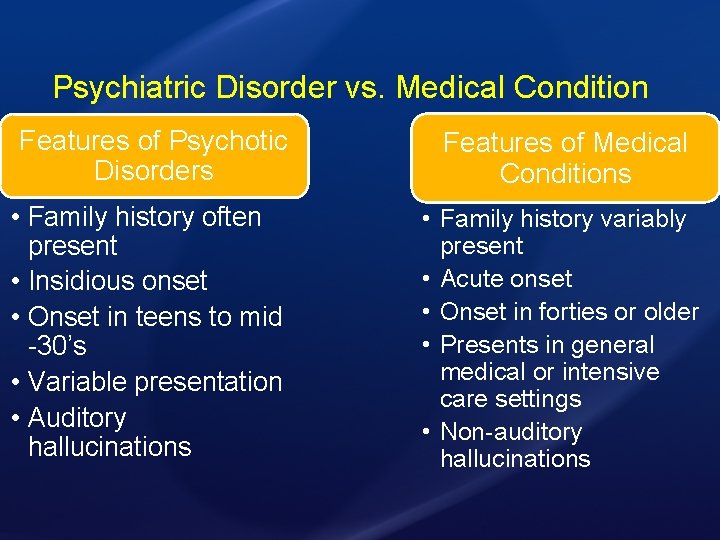
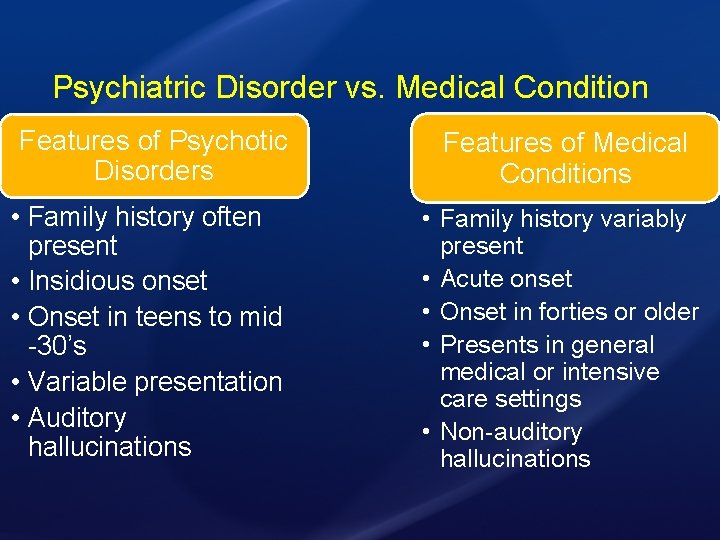
Psychiatric Disorder vs. Medical Condition Features of Psychotic Disorders • Family history often present • Insidious onset • Onset in teens to mid -30’s • Variable presentation • Auditory hallucinations Features of Medical Conditions • Family history variably present • Acute onset • Onset in forties or older • Presents in general medical or intensive care settings • Non-auditory hallucinations
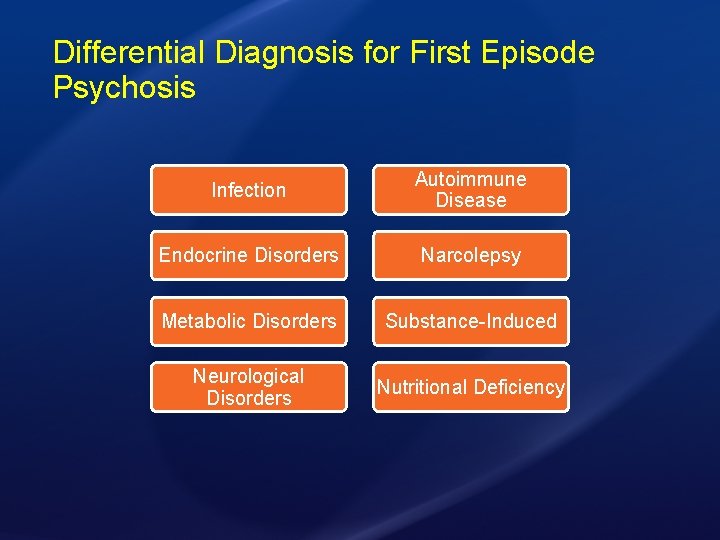
Differential Diagnosis for First Episode Psychosis Infection Autoimmune Disease Endocrine Disorders Narcolepsy Metabolic Disorders Substance-Induced Neurological Disorders Nutritional Deficiency
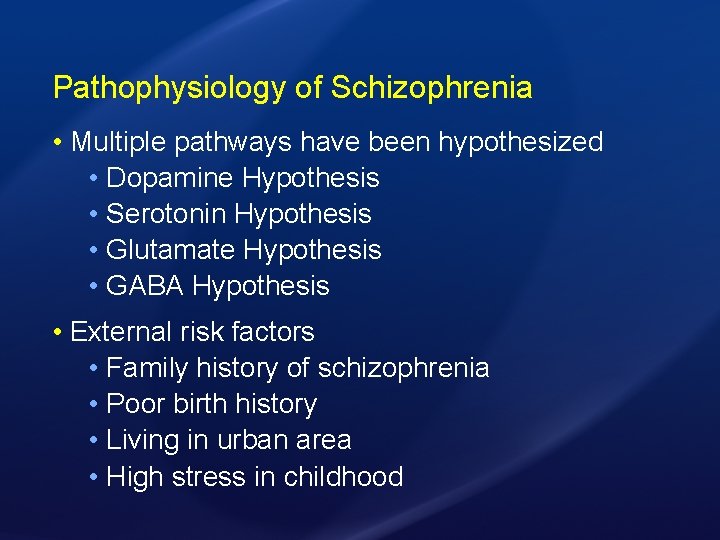
Pathophysiology of Schizophrenia • Multiple pathways have been hypothesized • Dopamine Hypothesis • Serotonin Hypothesis • Glutamate Hypothesis • GABA Hypothesis • External risk factors • Family history of schizophrenia • Poor birth history • Living in urban area • High stress in childhood
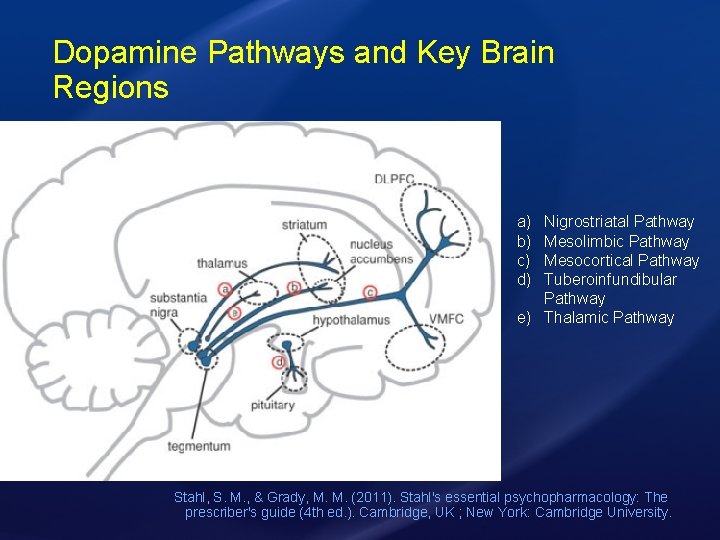
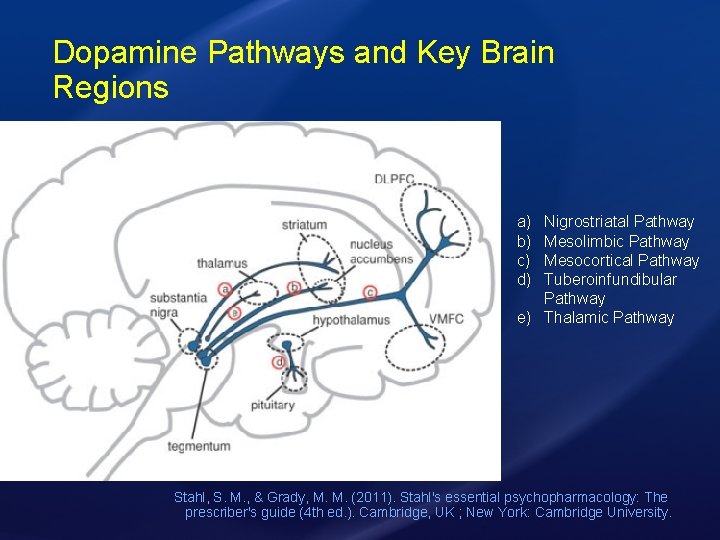
Dopamine Pathways and Key Brain Regions a) b) c) d) Nigrostriatal Pathway Mesolimbic Pathway Mesocortical Pathway Tuberoinfundibular Pathway e) Thalamic Pathway Stahl, S. M. , & Grady, M. M. (2011). Stahl's essential psychopharmacology: The prescriber's guide (4 th ed. ). Cambridge, UK ; New York: Cambridge University.
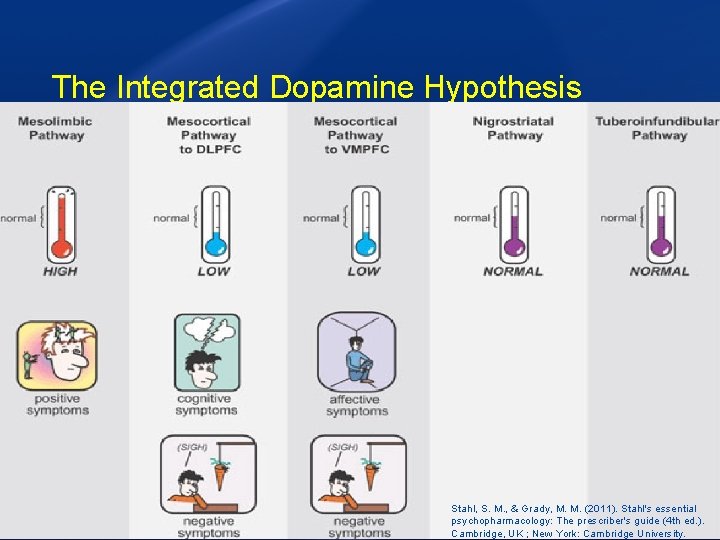
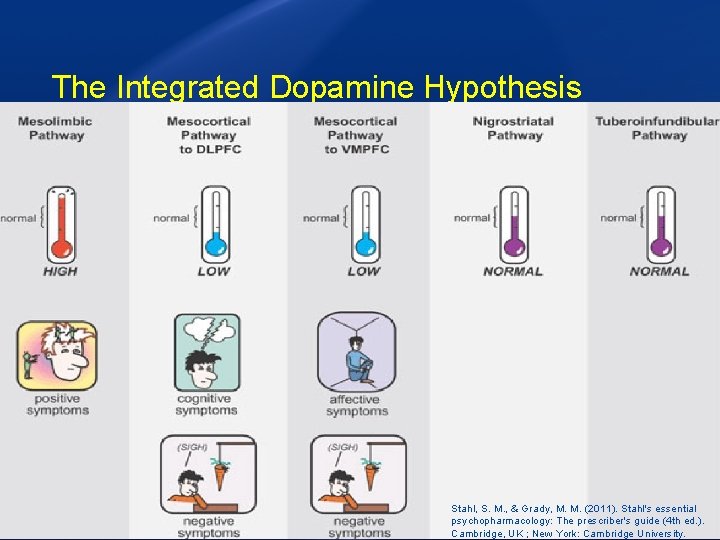
The Integrated Dopamine Hypothesis Stahl, S. M. , & Grady, M. M. (2011). Stahl's essential psychopharmacology: The prescriber's guide (4 th ed. ). Cambridge, UK ; New York: Cambridge University.
Schizophrenia Pharmacotherapy
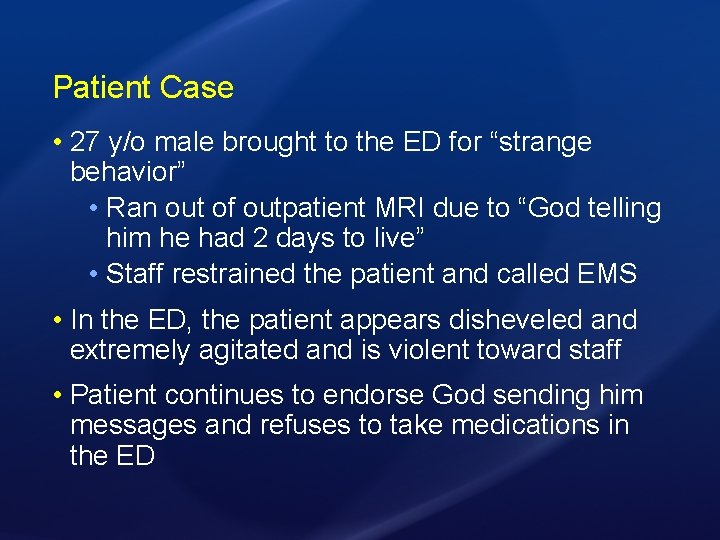
Patient Case • 27 y/o male brought to the ED for “strange behavior” • Ran out of outpatient MRI due to “God telling him he had 2 days to live” • Staff restrained the patient and called EMS • In the ED, the patient appears disheveled and extremely agitated and is violent toward staff • Patient continues to endorse God sending him messages and refuses to take medications in the ED
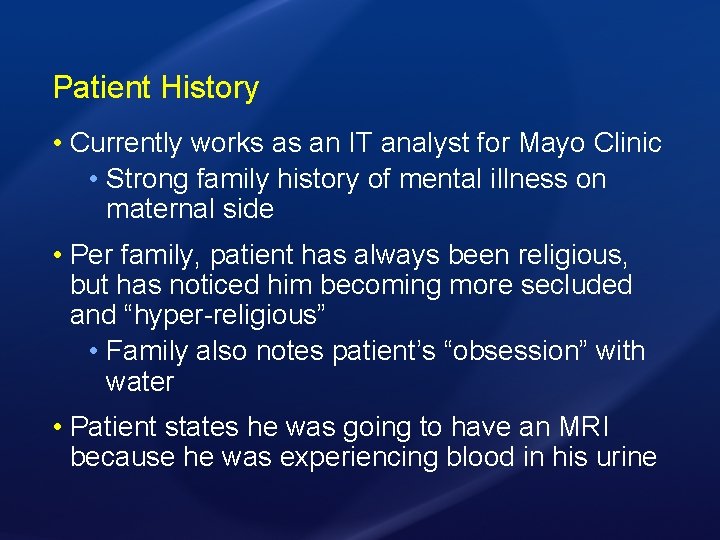
Patient History • Currently works as an IT analyst for Mayo Clinic • Strong family history of mental illness on maternal side • Per family, patient has always been religious, but has noticed him becoming more secluded and “hyper-religious” • Family also notes patient’s “obsession” with water • Patient states he was going to have an MRI because he was experiencing blood in his urine
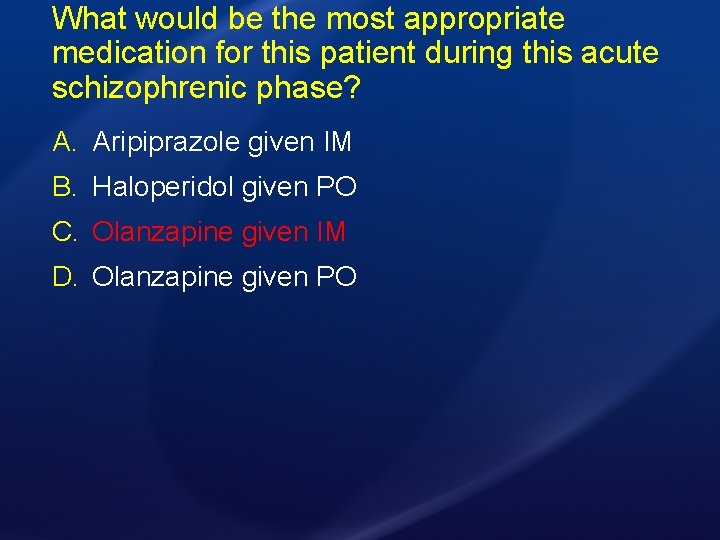
What would be the most appropriate medication for this patient during this acute schizophrenic phase? A. Aripiprazole given IM B. Haloperidol given PO C. Olanzapine given IM D. Olanzapine given PO
What would be the most appropriate medication for this patient during this acute schizophrenic phase? A. Aripiprazole given IM B. Haloperidol given PO C. Olanzapine given IM D. Olanzapine given PO
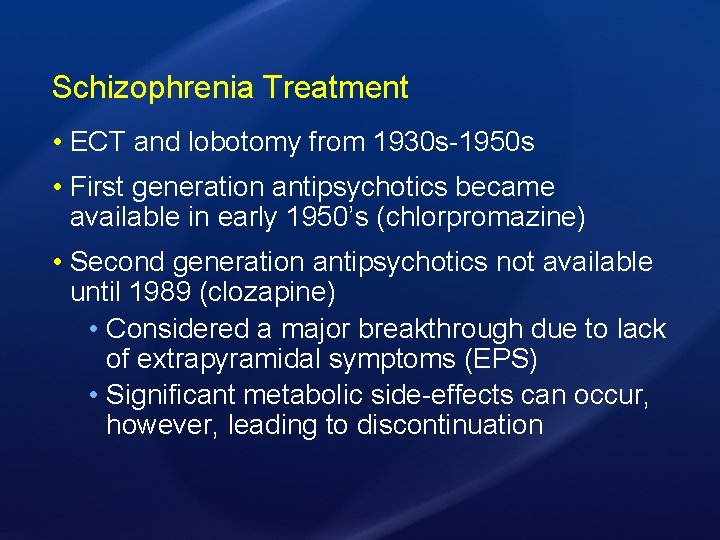
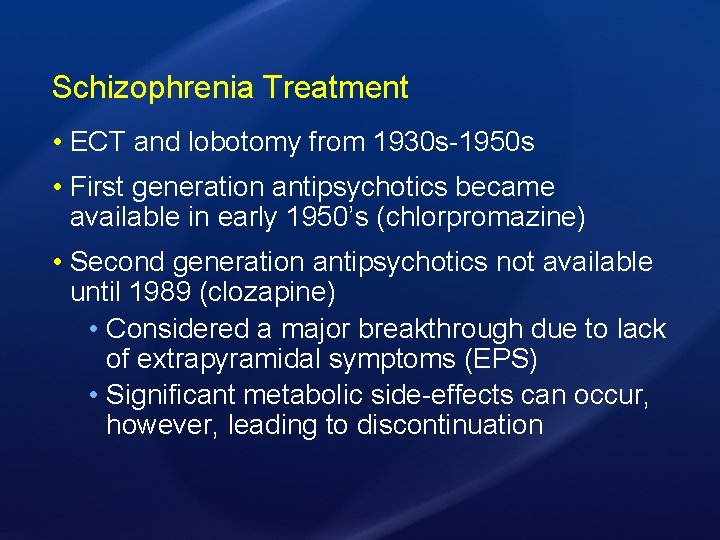
Schizophrenia Treatment • ECT and lobotomy from 1930 s-1950 s • First generation antipsychotics became available in early 1950’s (chlorpromazine) • Second generation antipsychotics not available until 1989 (clozapine) • Considered a major breakthrough due to lack of extrapyramidal symptoms (EPS) • Significant metabolic side-effects can occur, however, leading to discontinuation
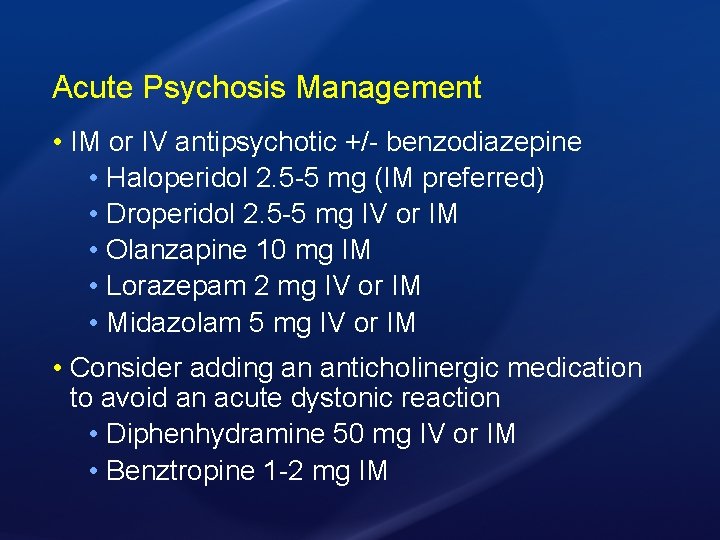
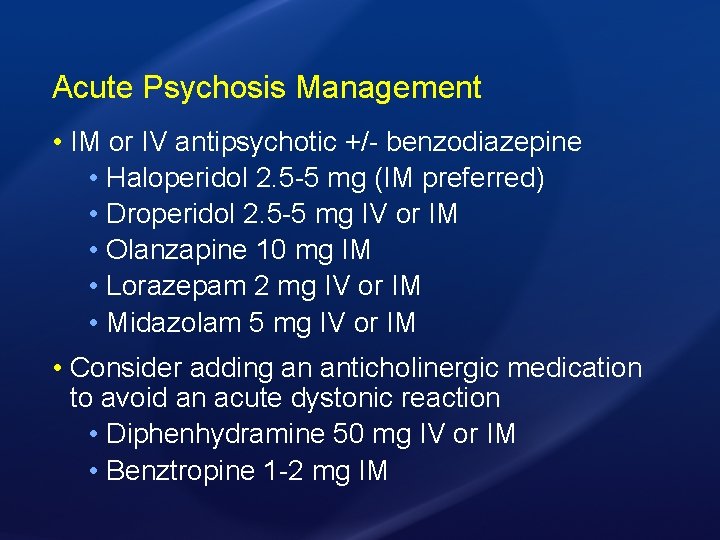
Acute Psychosis Management • IM or IV antipsychotic +/- benzodiazepine • Haloperidol 2. 5 -5 mg (IM preferred) • Droperidol 2. 5 -5 mg IV or IM • Olanzapine 10 mg IM • Lorazepam 2 mg IV or IM • Midazolam 5 mg IV or IM • Consider adding an anticholinergic medication to avoid an acute dystonic reaction • Diphenhydramine 50 mg IV or IM • Benztropine 1 -2 mg IM
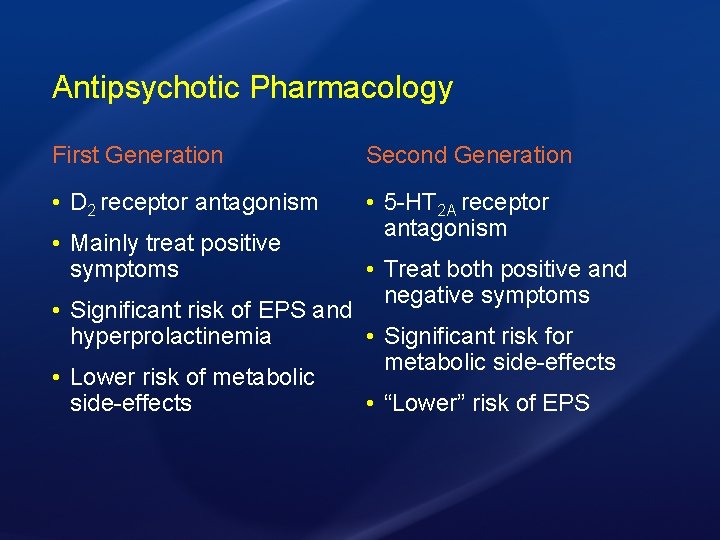
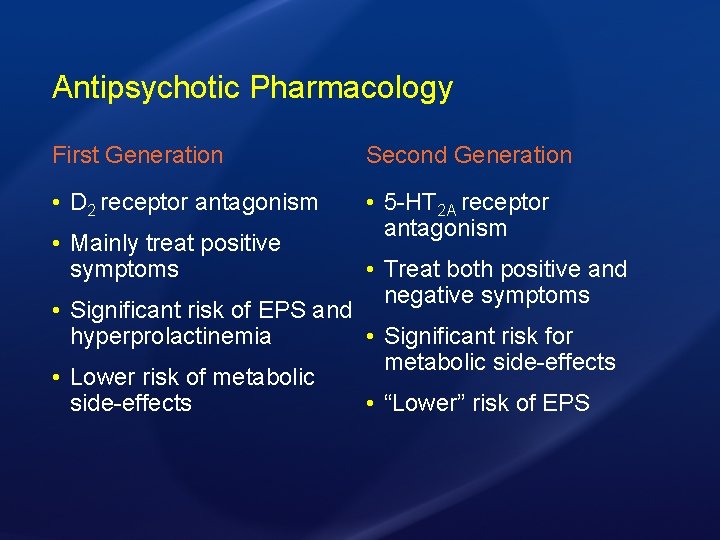
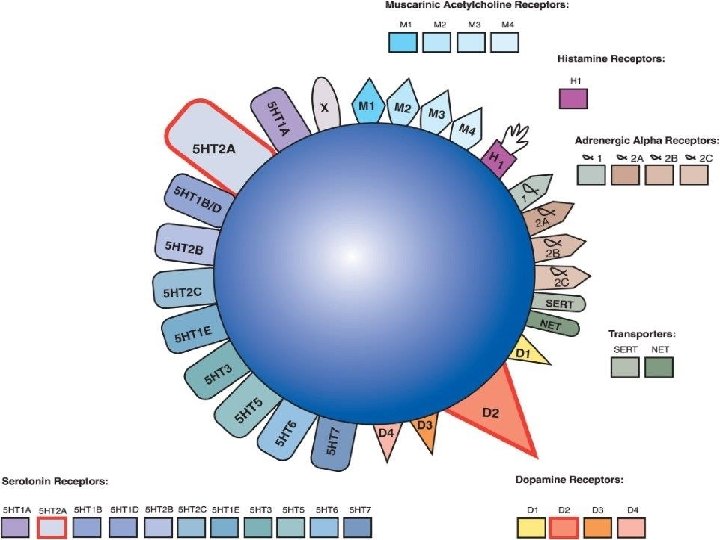
Antipsychotic Pharmacology First Generation Second Generation • D 2 receptor antagonism • 5 -HT 2 A receptor antagonism • Mainly treat positive symptoms • Treat both positive and negative symptoms • Significant risk of EPS and hyperprolactinemia • Significant risk for metabolic side-effects • Lower risk of metabolic side-effects • “Lower” risk of EPS
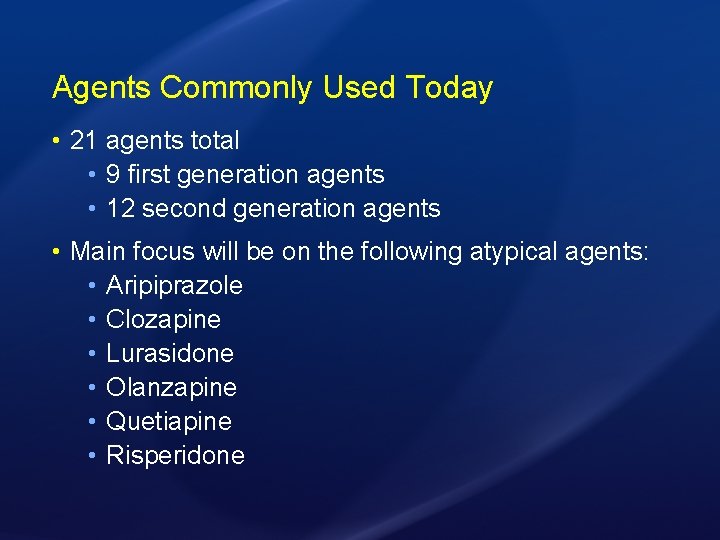
Agents Commonly Used Today • 21 agents total • 9 first generation agents • 12 second generation agents • Main focus will be on the following atypical agents: • Aripiprazole • Clozapine • Lurasidone • Olanzapine • Quetiapine • Risperidone
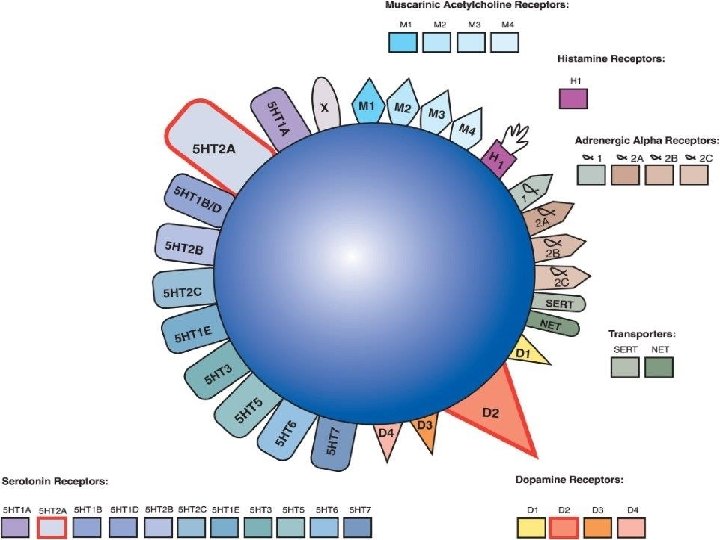
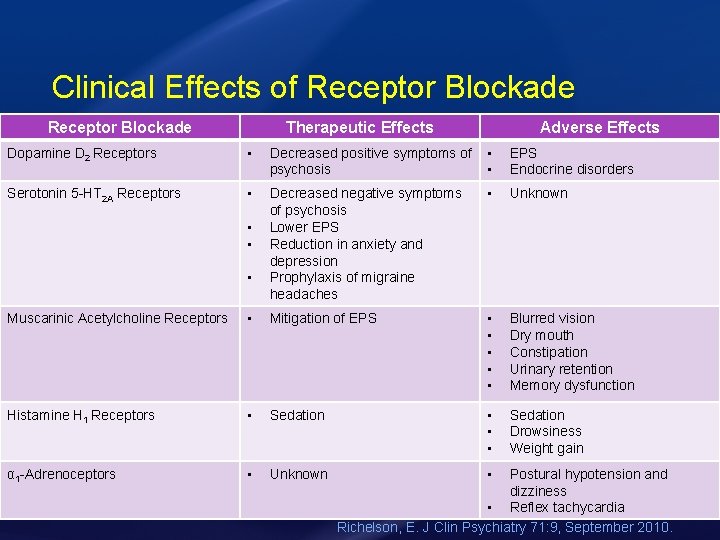
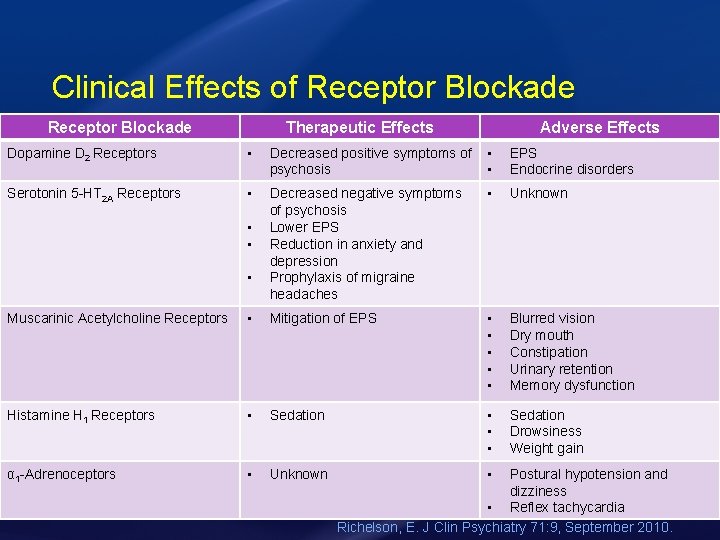
Clinical Effects of Receptor Blockade Therapeutic Effects Adverse Effects Dopamine D 2 Receptors • Decreased positive symptoms of • psychosis • Serotonin 5 -HT 2 A Receptors • Decreased negative symptoms of psychosis Lower EPS Reduction in anxiety and depression Prophylaxis of migraine headaches • Unknown • • • EPS Endocrine disorders Muscarinic Acetylcholine Receptors • Mitigation of EPS • • • Blurred vision Dry mouth Constipation Urinary retention Memory dysfunction Histamine H 1 Receptors • Sedation • • • Sedation Drowsiness Weight gain α 1 -Adrenoceptors • Unknown • Postural hypotension and dizziness • Reflex tachycardia Richelson, E. J Clin Psychiatry 71: 9, September 2010.
First Generation Antipsychotics (FGAs) • Potency at the D 2 receptor can be split into high and low • High potency: increased EPS, few off-target effects • Low potency: decreased EPS, but more offtarget effects • Majority of FGAs are not used commonly in clinical practice
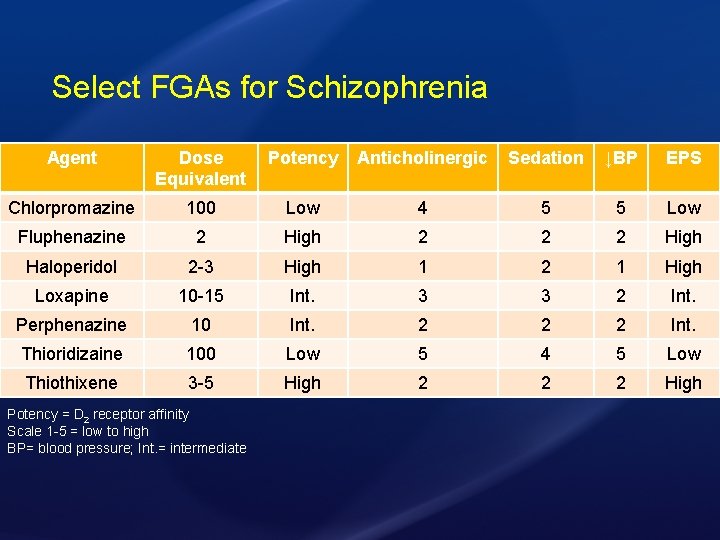
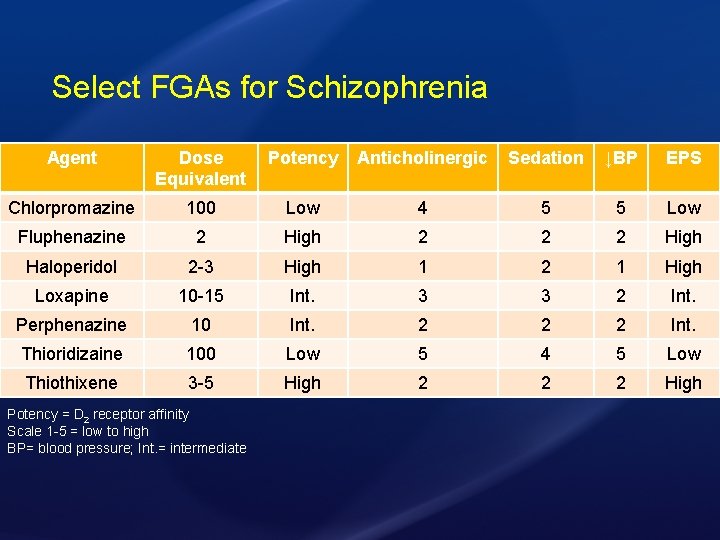
Select FGAs for Schizophrenia Agent Dose Equivalent Potency Anticholinergic Sedation ↓BP EPS Chlorpromazine 100 Low 4 5 5 Low Fluphenazine 2 High 2 2 2 High Haloperidol 2 -3 High 1 2 1 High Loxapine 10 -15 Int. 3 3 2 Int. Perphenazine 10 Int. 2 2 2 Int. Thioridizaine 100 Low 5 4 5 Low Thiothixene 3 -5 High 2 2 2 High Potency = D 2 receptor affinity Scale 1 -5 = low to high BP= blood pressure; Int. = intermediate
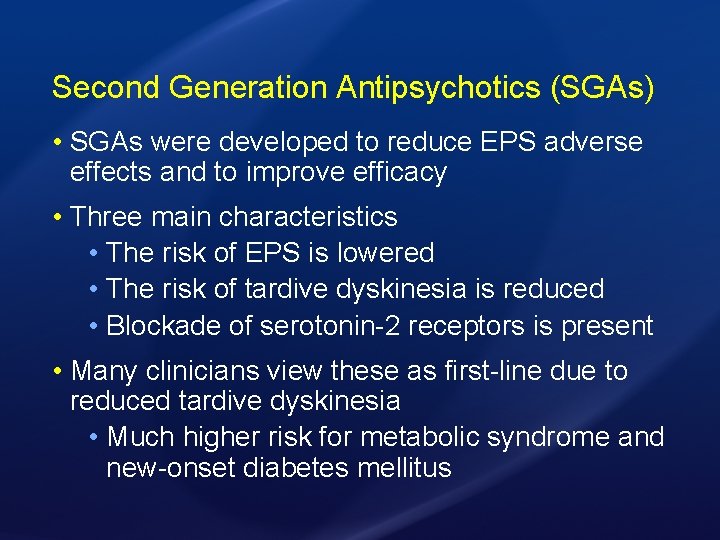
Second Generation Antipsychotics (SGAs) • SGAs were developed to reduce EPS adverse effects and to improve efficacy • Three main characteristics • The risk of EPS is lowered • The risk of tardive dyskinesia is reduced • Blockade of serotonin-2 receptors is present • Many clinicians view these as first-line due to reduced tardive dyskinesia • Much higher risk for metabolic syndrome and new-onset diabetes mellitus
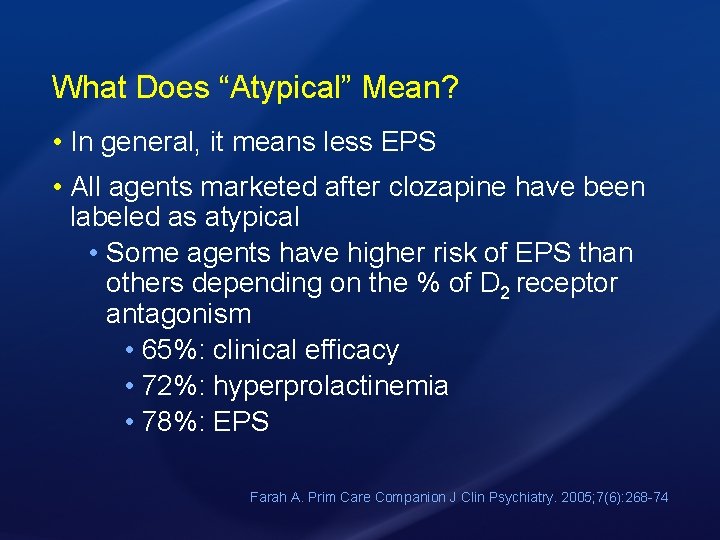
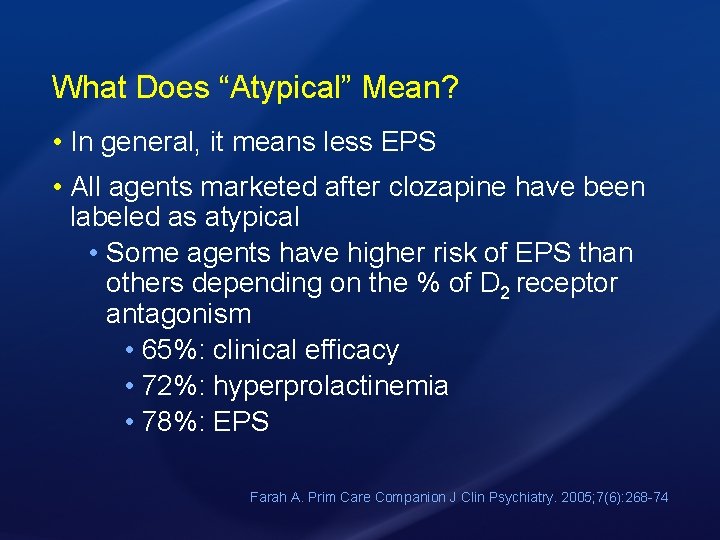
What Does “Atypical” Mean? • In general, it means less EPS • All agents marketed after clozapine have been labeled as atypical • Some agents have higher risk of EPS than others depending on the % of D 2 receptor antagonism • 65%: clinical efficacy • 72%: hyperprolactinemia • 78%: EPS Farah A. Prim Care Companion J Clin Psychiatry. 2005; 7(6): 268 -74
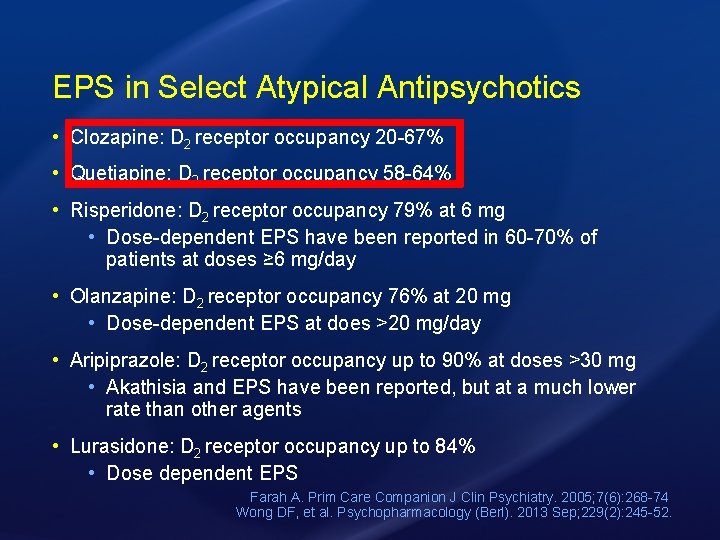
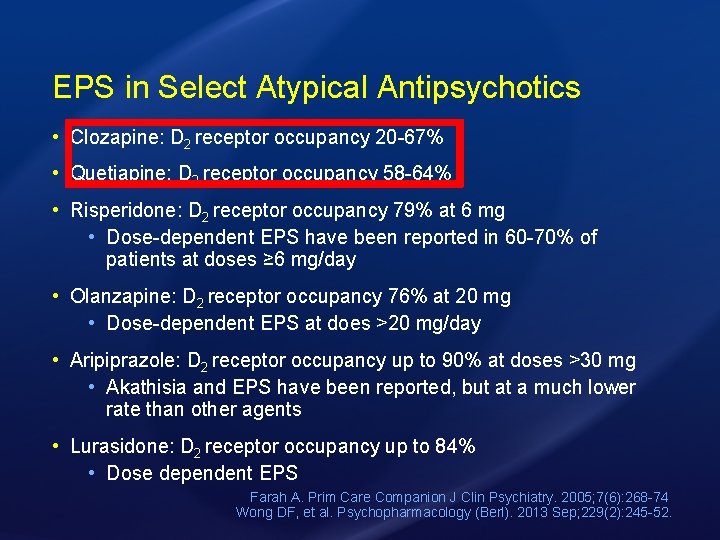
EPS in Select Atypical Antipsychotics • Clozapine: D 2 receptor occupancy 20 -67% • Quetiapine: D 2 receptor occupancy 58 -64% • Risperidone: D 2 receptor occupancy 79% at 6 mg • Dose-dependent EPS have been reported in 60 -70% of patients at doses ≥ 6 mg/day • Olanzapine: D 2 receptor occupancy 76% at 20 mg • Dose-dependent EPS at does >20 mg/day • Aripiprazole: D 2 receptor occupancy up to 90% at doses >30 mg • Akathisia and EPS have been reported, but at a much lower rate than other agents • Lurasidone: D 2 receptor occupancy up to 84% • Dose dependent EPS Farah A. Prim Care Companion J Clin Psychiatry. 2005; 7(6): 268 -74 Wong DF, et al. Psychopharmacology (Berl). 2013 Sep; 229(2): 245 -52.
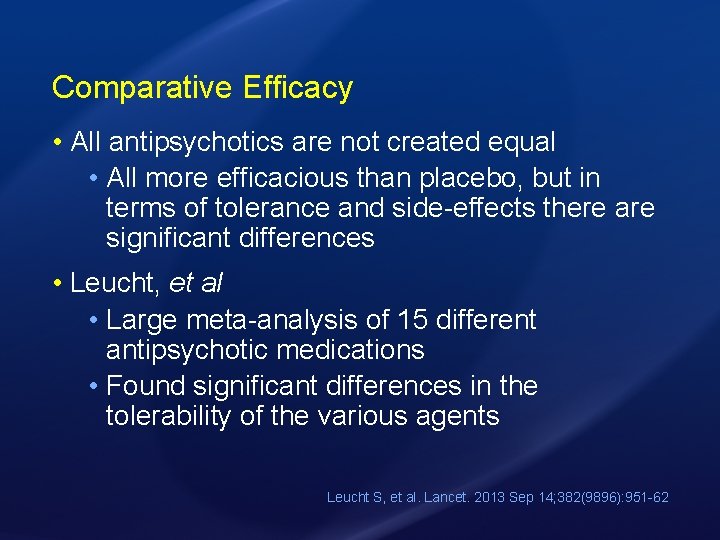
Comparative Efficacy • All antipsychotics are not created equal • All more efficacious than placebo, but in terms of tolerance and side-effects there are significant differences • Leucht, et al • Large meta-analysis of 15 different antipsychotic medications • Found significant differences in the tolerability of the various agents Leucht S, et al. Lancet. 2013 Sep 14; 382(9896): 951 -62
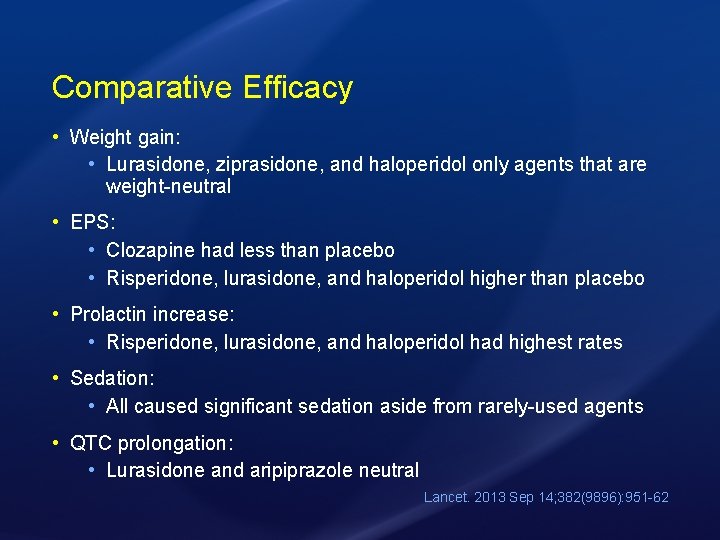
Comparative Efficacy • Weight gain: • Lurasidone, ziprasidone, and haloperidol only agents that are weight-neutral • EPS: • Clozapine had less than placebo • Risperidone, lurasidone, and haloperidol higher than placebo • Prolactin increase: • Risperidone, lurasidone, and haloperidol had highest rates • Sedation: • All caused significant sedation aside from rarely-used agents • QTC prolongation: • Lurasidone and aripiprazole neutral Lancet. 2013 Sep 14; 382(9896): 951 -62
Patient Case Continued • After receiving 5 mg IM haloperidol, the patient became much less agitated and was transferred to the inpatient psychiatric unit • Upon discussion with care team regarding oral antipsychotic therapy, the patient notes he would like to avoid sexual dysfunction and risk of EPS
Which of the following medications would be the best option for an oral antipsychotic based off discussion with the patient? A. Quetiapine B. Haloperidol C. Risperidone D. Clozapine
Which of the following medications would be the best option for an oral antipsychotic based off discussion with the patient? A. Quetiapine B. Haloperidol C. Risperidone D. Clozapine
Antipsychotic Pearls and Side-Effect Management
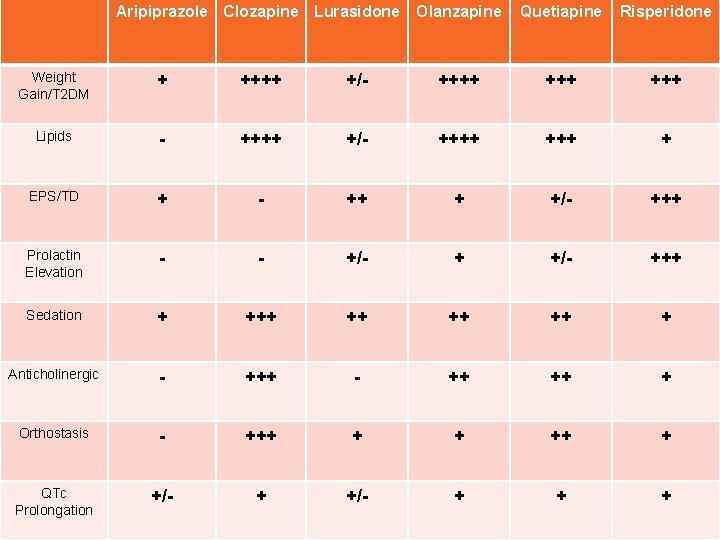
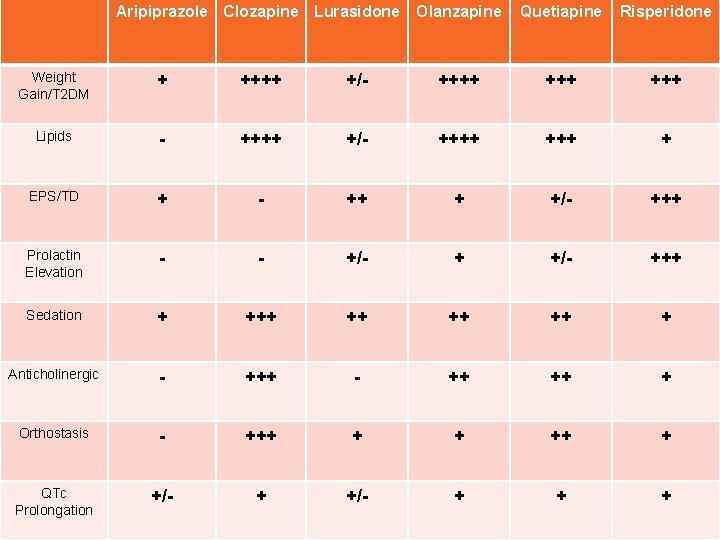
Aripiprazole Clozapine Lurasidone Olanzapine Quetiapine Risperidone Weight Gain/T 2 DM + ++++ +/- ++++ +++ Lipids - ++++ +/- ++++ + EPS/TD + - ++ + +/- +++ Prolactin Elevation - - +/- +++ Sedation + ++ ++ ++ + Anticholinergic - +++ - ++ ++ + Orthostasis - +++ + + ++ + QTc Prolongation +/- + + +
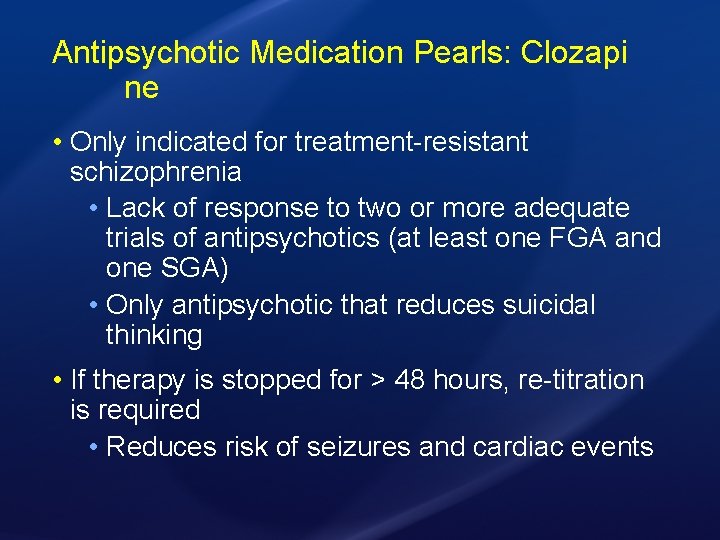
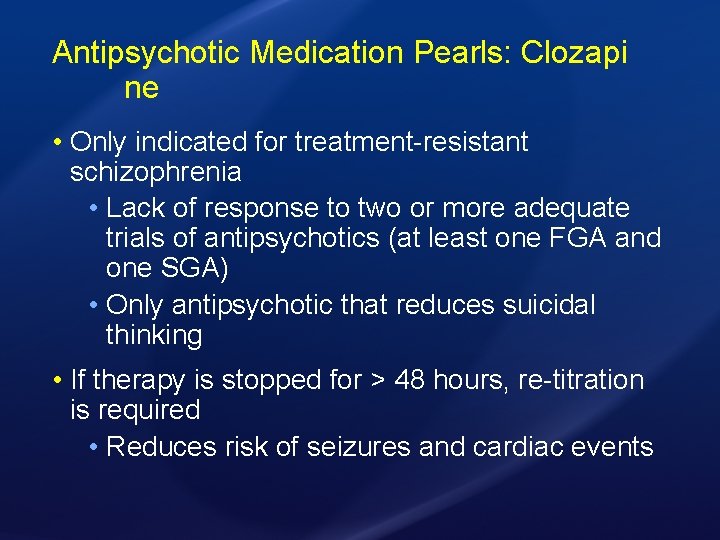
Antipsychotic Medication Pearls: Clozapi ne • Only indicated for treatment-resistant schizophrenia • Lack of response to two or more adequate trials of antipsychotics (at least one FGA and one SGA) • Only antipsychotic that reduces suicidal thinking • If therapy is stopped for > 48 hours, re-titration is required • Reduces risk of seizures and cardiac events
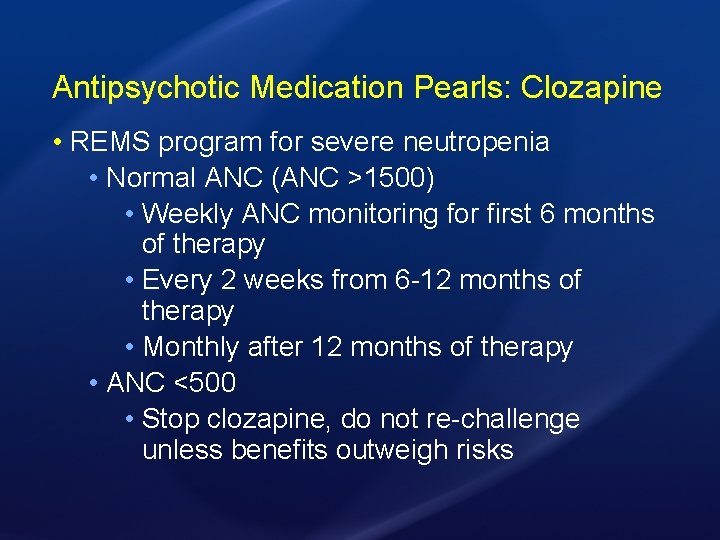
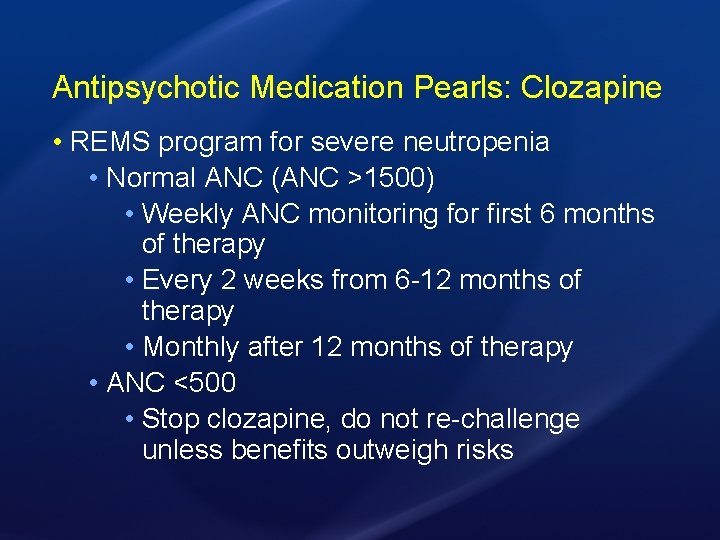
Antipsychotic Medication Pearls: Clozapine • REMS program for severe neutropenia • Normal ANC (ANC >1500) • Weekly ANC monitoring for first 6 months of therapy • Every 2 weeks from 6 -12 months of therapy • Monthly after 12 months of therapy • ANC <500 • Stop clozapine, do not re-challenge unless benefits outweigh risks
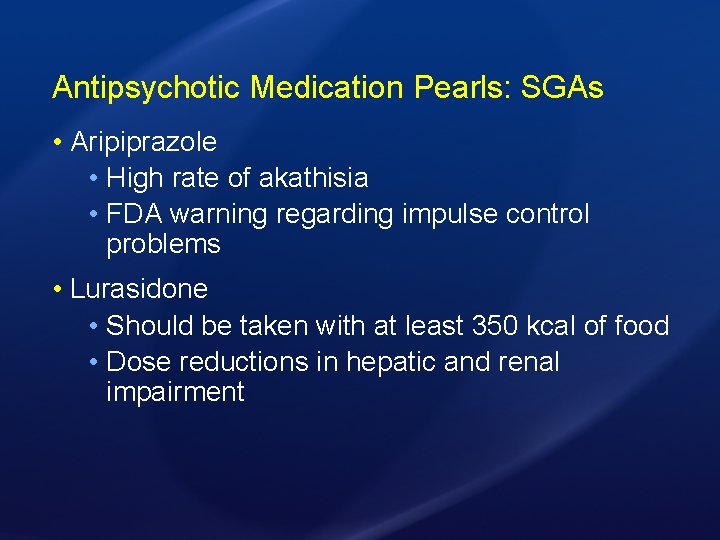
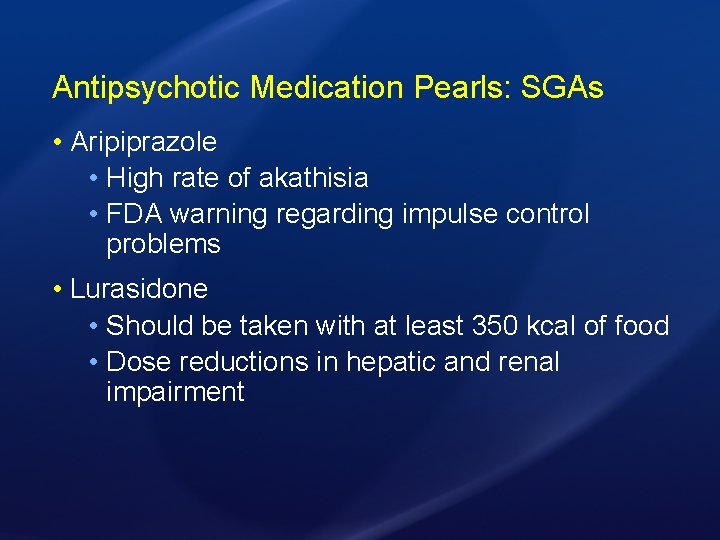
Antipsychotic Medication Pearls: SGAs • Aripiprazole • High rate of akathisia • FDA warning regarding impulse control problems • Lurasidone • Should be taken with at least 350 kcal of food • Dose reductions in hepatic and renal impairment
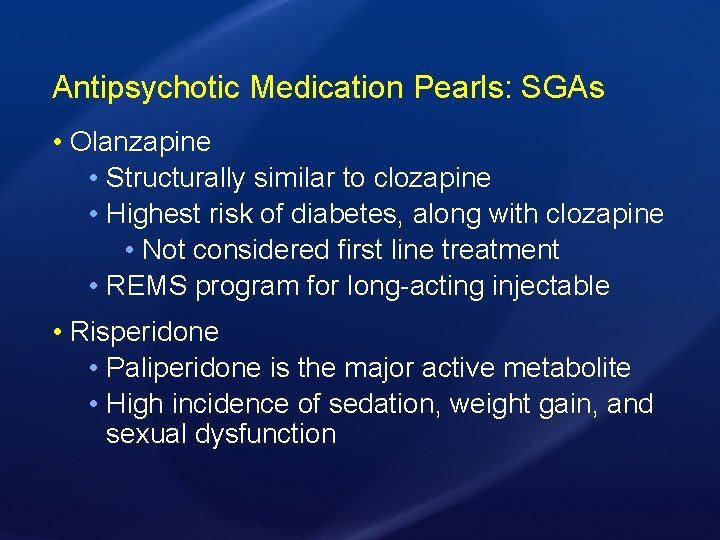
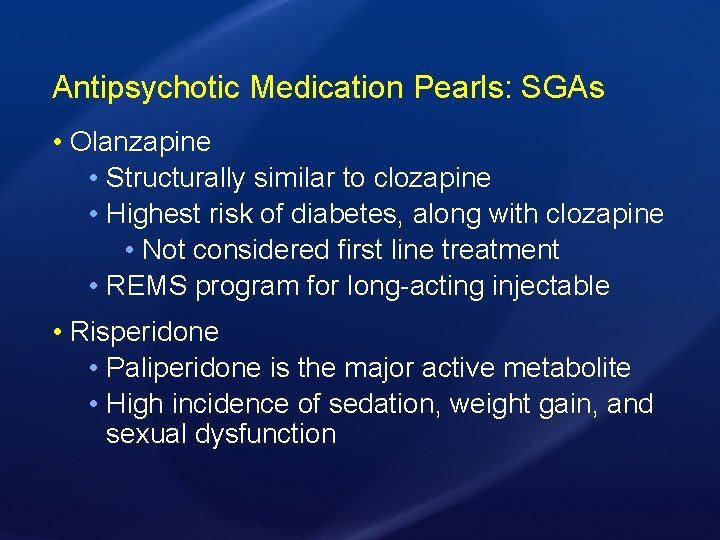
Antipsychotic Medication Pearls: SGAs • Olanzapine • Structurally similar to clozapine • Highest risk of diabetes, along with clozapine • Not considered first line treatment • REMS program for long-acting injectable • Risperidone • Paliperidone is the major active metabolite • High incidence of sedation, weight gain, and sexual dysfunction
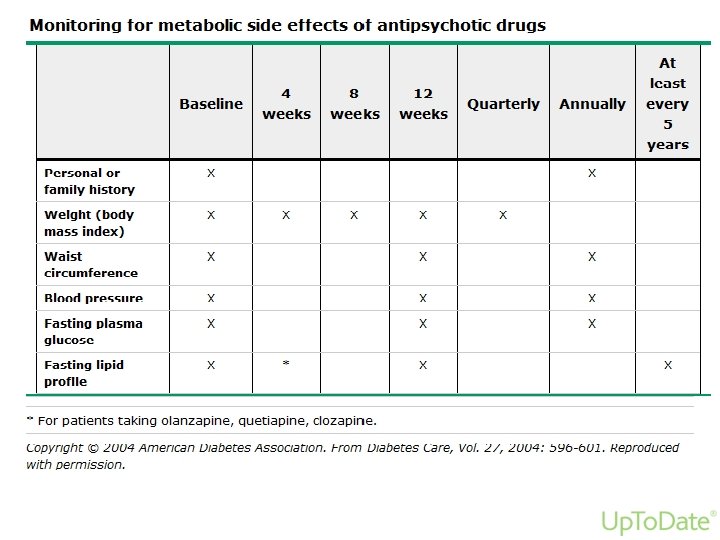
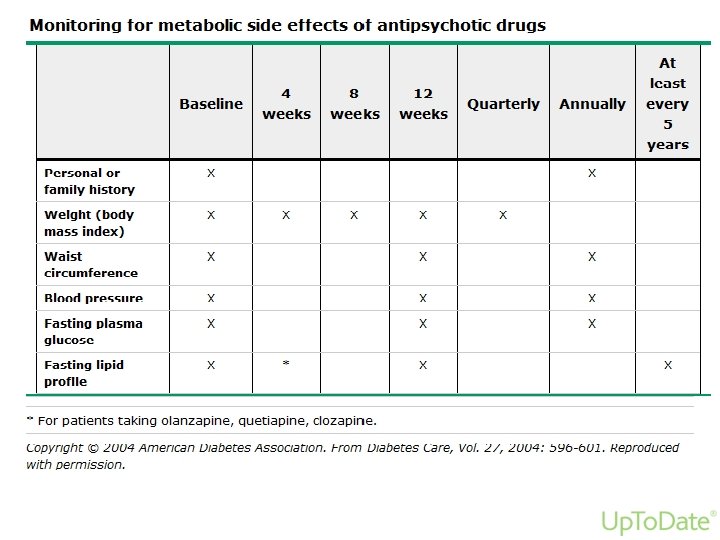
Clinical Monitoring
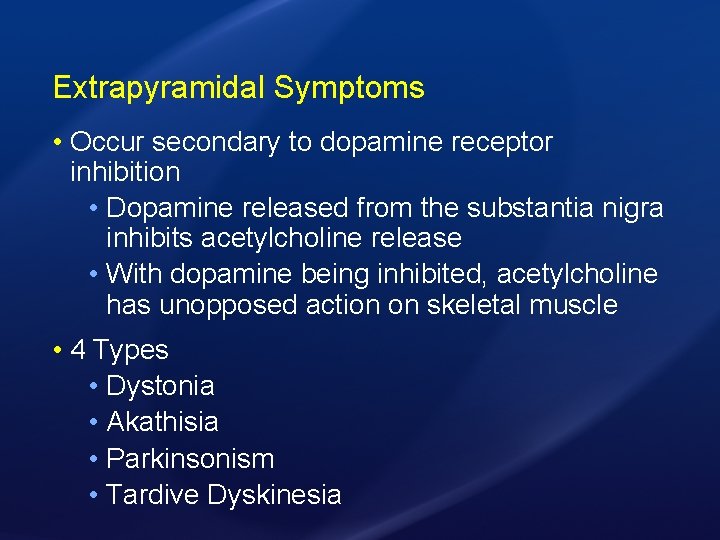
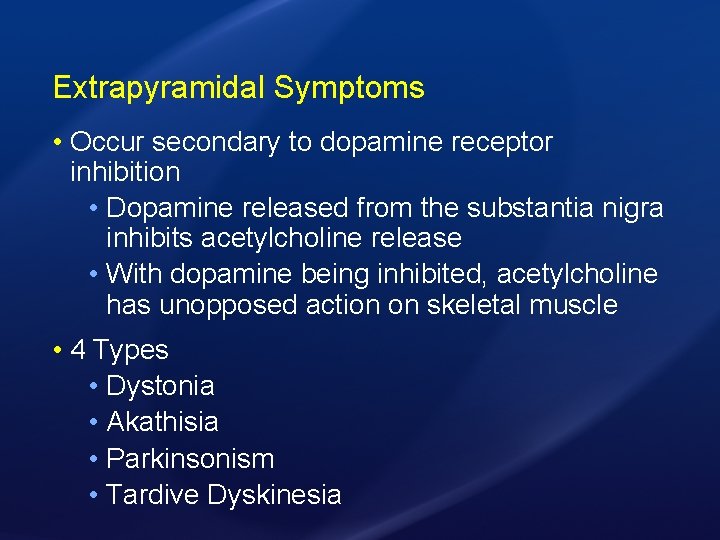
Extrapyramidal Symptoms • Occur secondary to dopamine receptor inhibition • Dopamine released from the substantia nigra inhibits acetylcholine release • With dopamine being inhibited, acetylcholine has unopposed action on skeletal muscle • 4 Types • Dystonia • Akathisia • Parkinsonism • Tardive Dyskinesia
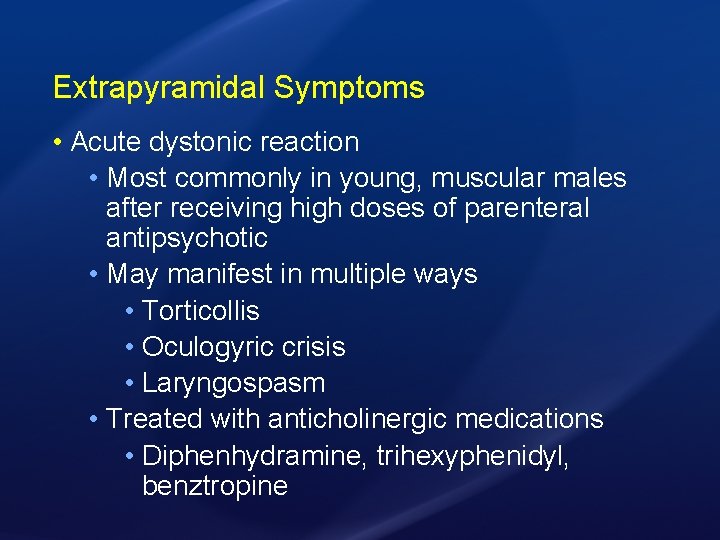
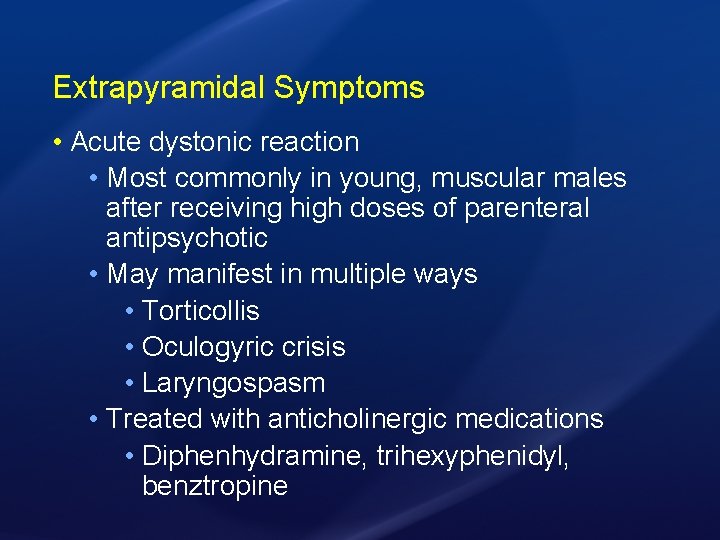
Extrapyramidal Symptoms • Acute dystonic reaction • Most commonly in young, muscular males after receiving high doses of parenteral antipsychotic • May manifest in multiple ways • Torticollis • Oculogyric crisis • Laryngospasm • Treated with anticholinergic medications • Diphenhydramine, trihexyphenidyl, benztropine
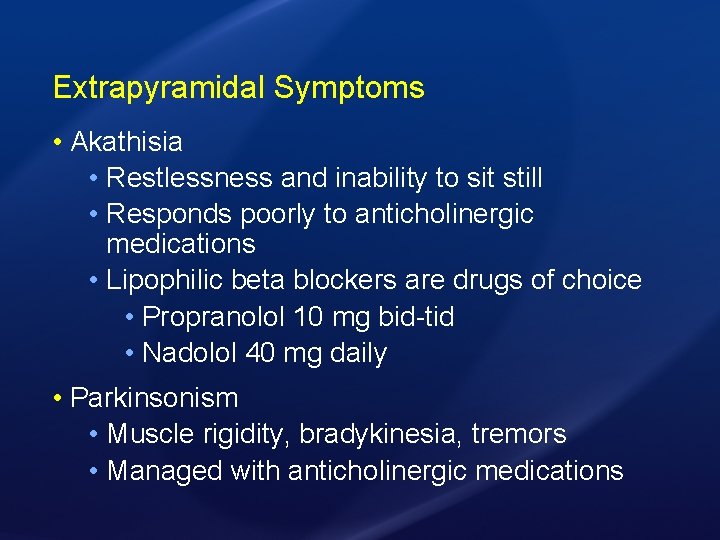
Extrapyramidal Symptoms • Akathisia • Restlessness and inability to sit still • Responds poorly to anticholinergic medications • Lipophilic beta blockers are drugs of choice • Propranolol 10 mg bid-tid • Nadolol 40 mg daily • Parkinsonism • Muscle rigidity, bradykinesia, tremors • Managed with anticholinergic medications
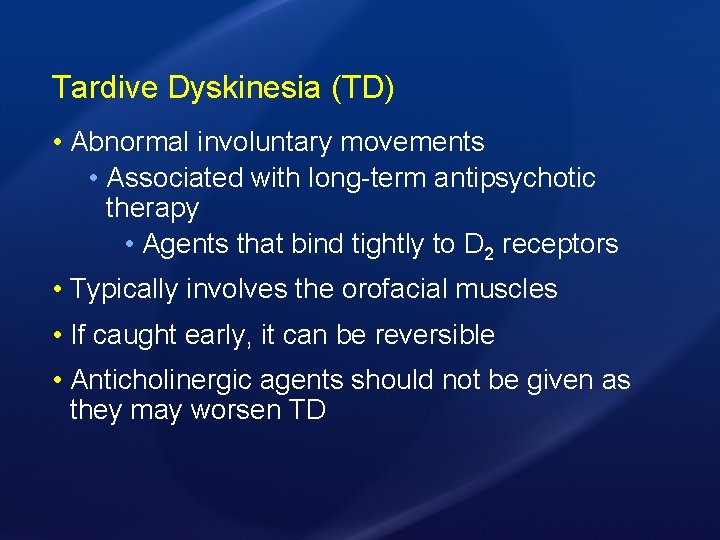
Tardive Dyskinesia (TD) • Abnormal involuntary movements • Associated with long-term antipsychotic therapy • Agents that bind tightly to D 2 receptors • Typically involves the orofacial muscles • If caught early, it can be reversible • Anticholinergic agents should not be given as they may worsen TD
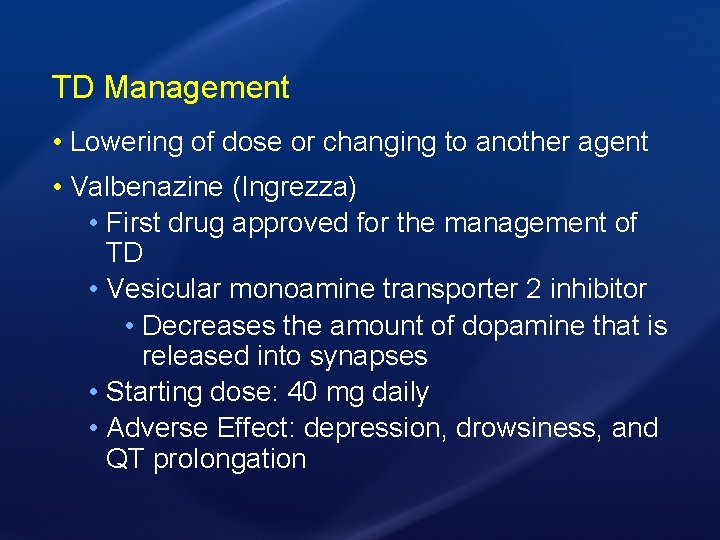
TD Management • Lowering of dose or changing to another agent • Valbenazine (Ingrezza) • First drug approved for the management of TD • Vesicular monoamine transporter 2 inhibitor • Decreases the amount of dopamine that is released into synapses • Starting dose: 40 mg daily • Adverse Effect: depression, drowsiness, and QT prolongation
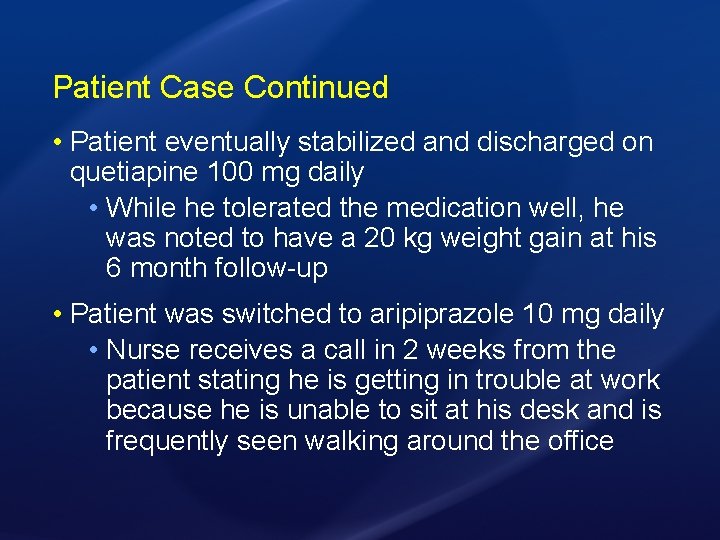
Patient Case Continued • Patient eventually stabilized and discharged on quetiapine 100 mg daily • While he tolerated the medication well, he was noted to have a 20 kg weight gain at his 6 month follow-up • Patient was switched to aripiprazole 10 mg daily • Nurse receives a call in 2 weeks from the patient stating he is getting in trouble at work because he is unable to sit at his desk and is frequently seen walking around the office
What would be the best treatment option for the patient’s symptoms? • A. Stop aripiprazole indefinitely • B. Start benztropine 1 mg BID • C. Start propranolol 10 mg TID • D. Start valbenazine 40 mg QD
What would be the best treatment option for the patient’s symptoms? • A. Stop aripiprazole indefinitely • B. Start benztropine 1 mg BID • C. Start propranolol 10 mg TID • D. Start valbenazine 40 mg QD
Conclusion • While multiple theories exist, the most wellaccepted theory of the mechanism of schizophrenia is the dopamine hypothesis • Antipsychotic medications have varying sideeffect profiles and differences in tolerability • Must make patient-centered decisions to reduce discontinuation rate
Questions & Discussion