The Peripheral Arterial Disease Guideline EvidenceBased Management of
The Peripheral Arterial Disease Guideline: Evidence-Based Management of Patients With PAD Core Curriculum Slide Set A Collaborative Product Co-Developed by: American College of Cardiology; American Heart Association; American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung and Blood Institute; Peripheral Arterial Disease Coalition; Society for Cardiovascular Angiography and Interventions; Society of Interventional Radiology; Society for Vascular Nursing; Society for Vascular Medicine and Biology; Society for Vascular Surgery; Trans. Atlantic Inter-Society Consensus; and Vascular Disease Foundation.
The Peripheral Arterial Disease Task to be Accomplished Is Encompassed in the Title: ACC/AHA Guidelines for the Management of Patients With Peripheral Arterial Disease: A Collaborative Report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society for Vascular Medicine and Biology, and the ACC/AHA Task Force on Practice Guidelines. Also endorsed by the: American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; Trans. Atlantic Inter-Society Consensus; and The Vascular Disease Foundation.

Supported by an educational grant from Bristol-Myers Squibb and Sanofi Pharmaceuticals Partnership were not involved in the development of this slide set and in no way influenced its contents.
Contributors The PAD Guidelines Implementation Task Force Slide Set Co-Editors Mark A. Creager, MD, & Alan T. Hirsch, MD Alan T. Hirsch, Co-Chair Vascular Medicine/Cardiology Harvey M. Wiener, DO, Co-Chair, Interventional Radiology Carolyn Robinson, NP, Co-Chair, Vascular Nursing John White, MD, Co-Chair, Vascular Surgery Thomas A. Biggs, MD Arthur L. Riba, MD Frank C. Brosius, III, MD Kerry J. Stewart, Ed. D Mark A. Creager, MD Diane Treat-Jacobson, RN, Ph. D James B. Froehlich, MD, MPH Rose Marie Robertson, MD William R. Hiatt, MD Mark Sanz, MD Karen Lui, RN, MS Peter Sheehan, MD Timothy Murphy, MD H. Eser Tolunay, Ph. D Jeffrey W. Olin, DO Christopher White, MD
Special Thanks to The PAD Guidelines Writing Committee Members Alan T. Hirsch, MD, FACC, FAHA, Chair Jules B. Puschett, MD, FAHA Ziv J. Haskal, MD, FAHA, FSIR, Co-Chair, Kenneth A. Rosenfield, MD, FACC Norman R. Hertzer, MD, FACS, Co-Chair David Sacks, MD, FACR, FSIR Curtis W. Bakal, MD, MPH, FAHA James C. Stanley, MD, FACS, FACR, FSIR Mark A. Creager, MD, FACC, FAHA Lloyd M. Taylor, Jr. , MD, FACS Jonathan L. Halperin, MD, FACC, FAHA Christopher J. White, MD, FACC, FAHA, FSCAI Loren F. Hiratzka, MD, FACC, FAHA, FACS John White, MD, FACS William R. C. Murphy, MD, FACC, FACS Rodney A. White, MD, FACS Jeffrey W. Olin, DO, FACC
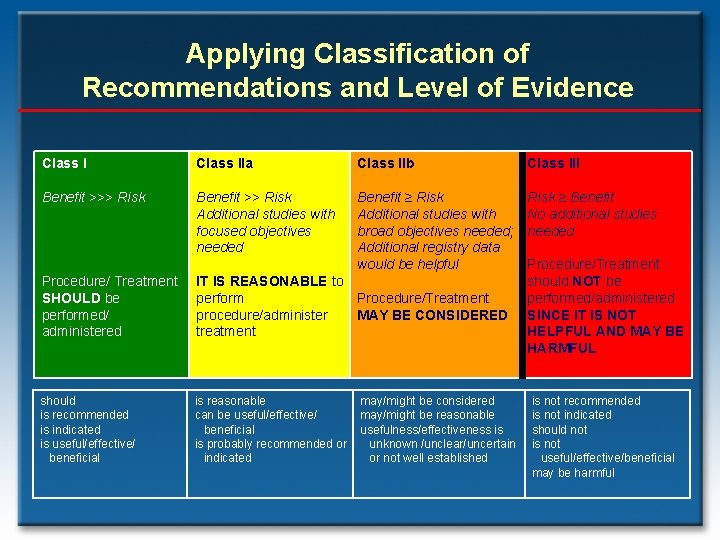
Applying Classification of Recommendations and Level of Evidence Class IIa Class IIb Class III Benefit >>> Risk Benefit >> Risk Additional studies with focused objectives needed Benefit ≥ Risk Additional studies with broad objectives needed; Additional registry data would be helpful Risk ≥ Benefit No additional studies needed Procedure/ Treatment SHOULD be performed/ administered IT IS REASONABLE to perform Procedure/Treatment procedure/administer MAY BE CONSIDERED treatment should is recommended is indicated is useful/effective/ beneficial is reasonable can be useful/effective/ beneficial is probably recommended or indicated may/might be considered may/might be reasonable usefulness/effectiveness is unknown /unclear/uncertain or not well established Procedure/Treatment should NOT be performed/administered SINCE IT IS NOT HELPFUL AND MAY BE HARMFUL is not recommended is not indicated should not is not useful/effective/beneficial may be harmful
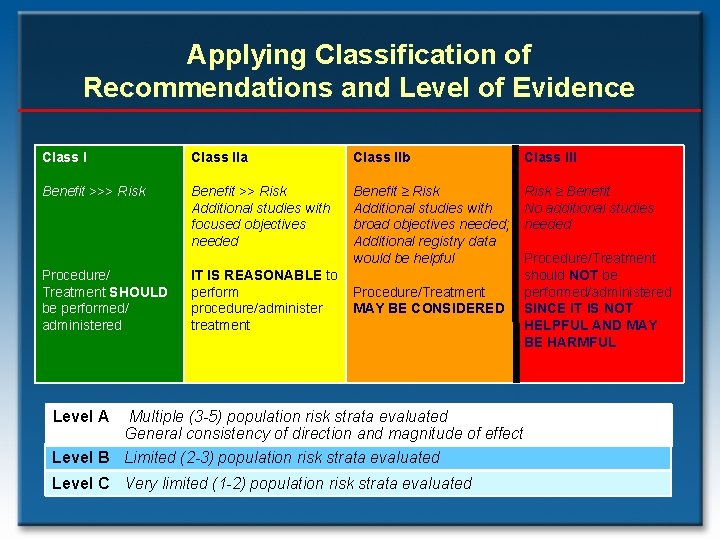
Applying Classification of Recommendations and Level of Evidence Class IIa Class IIb Class III Benefit >>> Risk Benefit >> Risk Additional studies with focused objectives needed Benefit ≥ Risk Additional studies with broad objectives needed; Additional registry data would be helpful Risk ≥ Benefit No additional studies needed Procedure/ Treatment SHOULD be performed/ administered IT IS REASONABLE to perform procedure/administer treatment Procedure/Treatment MAY BE CONSIDERED Level A Procedure/Treatment should NOT be performed/administered SINCE IT IS NOT HELPFUL AND MAY BE HARMFUL Multiple (3 -5) population risk strata evaluated General consistency of direction and magnitude of effect Level B Limited (2 -3) population risk strata evaluated Level C Very limited (1 -2) population risk strata evaluated
Why a PAD Guideline? • To enhance the quality of patient care • Increasing recognition of the importance of atherosclerotic lower extremity PAD: – High prevalence – High cardiovascular risk – Poor quality of life • Improved ability to detect and treat renal artery disease • Improved ability to detect and treat abdominal aortic aneurysm • The evidence base has become increasingly robust, so that a data-driven care guideline is now possible
PAD Guideline: The Target Audiences Are Diverse • Primary care clinicians – Family practice – Internal medicine – PA, NP, nurse clinicians • Cardiovascular/vascular medicine, vascular surgical, & interventional radiology trainees • Vascular specialists This is not intended to be a procedural guideline; it is intended to provide a guide to optimal lifelong PAD care.
PAD Epidemiology
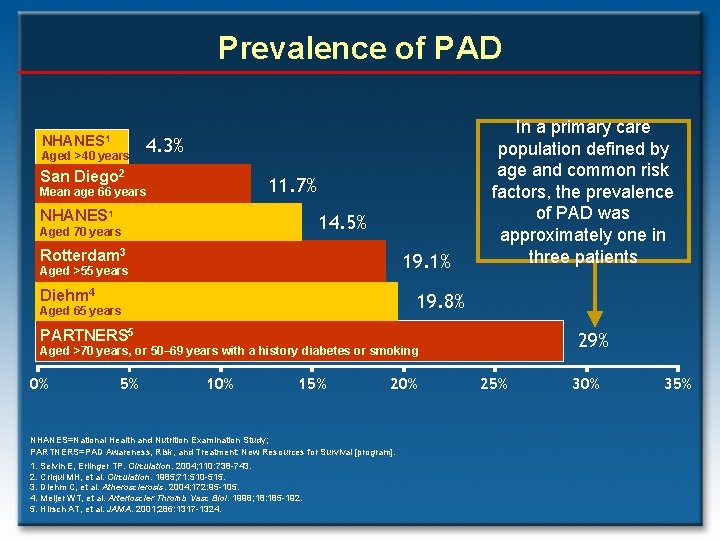
Prevalence of PAD NHANES 1 Aged >40 years 4. 3% San Diego 2 11. 7% Mean age 66 years NHANES 1 14. 5% Aged 70 years Rotterdam 3 19. 1% Aged >55 years Diehm 4 In a primary care population defined by age and common risk factors, the prevalence of PAD was approximately one in three patients 19. 8% Aged 65 years PARTNERS 5 29% Aged >70 years, or 50– 69 years with a history diabetes or smoking 0% 5% 10% 15% 20% NHANES=National Health and Nutrition Examination Study; PARTNERS=PAD Awareness, Risk, and Treatment: New Resources for Survival [program]. 1. Selvin E, Erlinger TP. Circulation. 2004; 110: 738 -743. 2. Criqui MH, et al. Circulation. 1985; 71: 510 -515. 3. Diehm C, et al. Atherosclerosis. 2004; 172: 95 -105. 4. Meijer WT, et al. Arterioscler Thromb Vasc Biol. 1998; 18: 185 -192. 5. Hirsch AT, et al. JAMA. 2001; 286: 1317 -1324. 25% 30% 35%
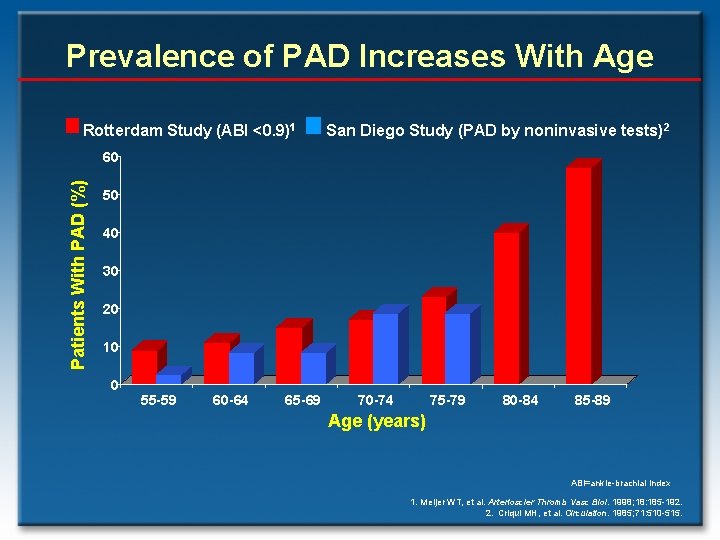
Prevalence of PAD Increases With Age Rotterdam Study (ABI <0. 9)1 San Diego Study (PAD by noninvasive tests)2 Patients With PAD (%) 60 50 40 30 20 10 0 55 -59 60 -64 65 -69 70 -74 75 -79 80 -84 85 -89 Age (years) ABI=ankle-brachial index 1. Meijer WT, et al. Arterioscler Thromb Vasc Biol. 1998; 18: 185 -192. 2. Criqui MH, et al. Circulation. 1985; 71: 510 -515.
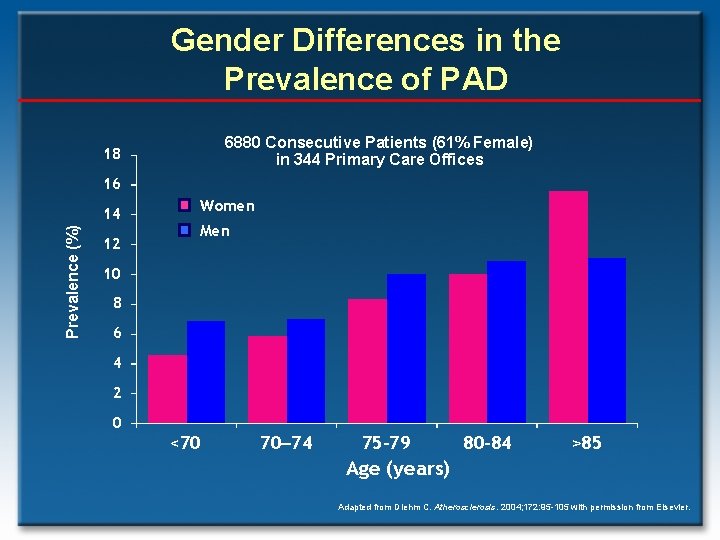
Gender Differences in the Prevalence of PAD 6880 Consecutive Patients (61% Female) in 344 Primary Care Offices 18 16 Prevalence (%) 14 12 Women Men 10 8 6 4 2 0 <70 70– 74 75– 79 80– 84 >85 Age (years) Adapted from Diehm C. Atherosclerosis. 2004; 172: 95 -105 with permission from Elsevier.
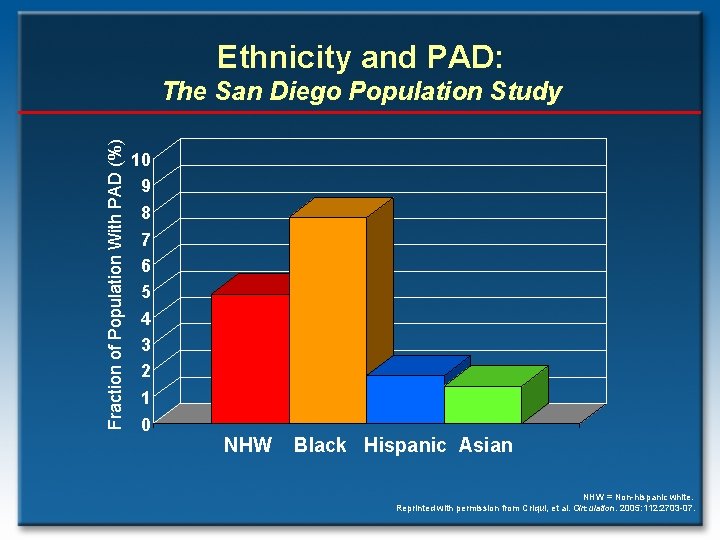
Ethnicity and PAD: Fraction of Population With PAD (%) The San Diego Population Study 10 9 8 7 6 5 4 3 2 1 0 NHW Black Hispanic Asian NHW = Non-hispanic white. Reprinted with permission from Criqui, et al. Circulation. 2005: 112: 2703 -07.
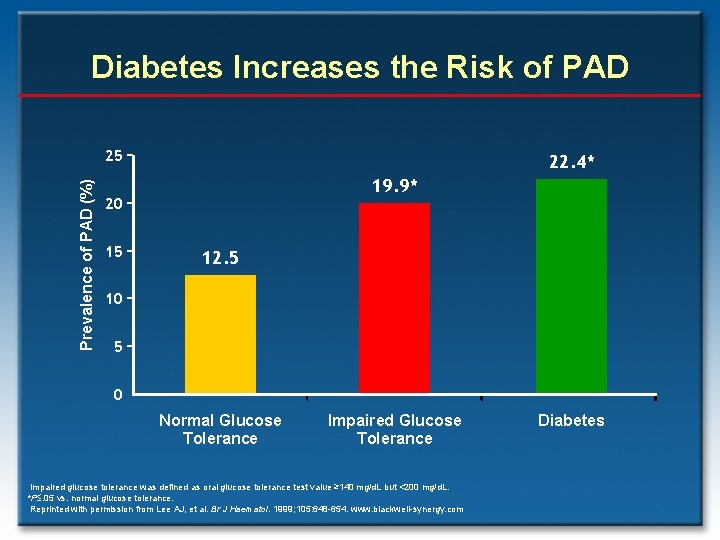
Diabetes Increases the Risk of PAD Prevalence of PAD (%) 25 22. 4* 19. 9* 20 15 12. 5 10 5 0 Normal Glucose Tolerance Impaired glucose tolerance was defined as oral glucose tolerance test value ≥ 140 mg/d. L but <200 mg/d. L. *P. 05 vs. normal glucose tolerance. Reprinted with permission from Lee AJ, et al. Br J Haematol. 1999; 105: 648 -654. www. blackwell-synergy. com Diabetes
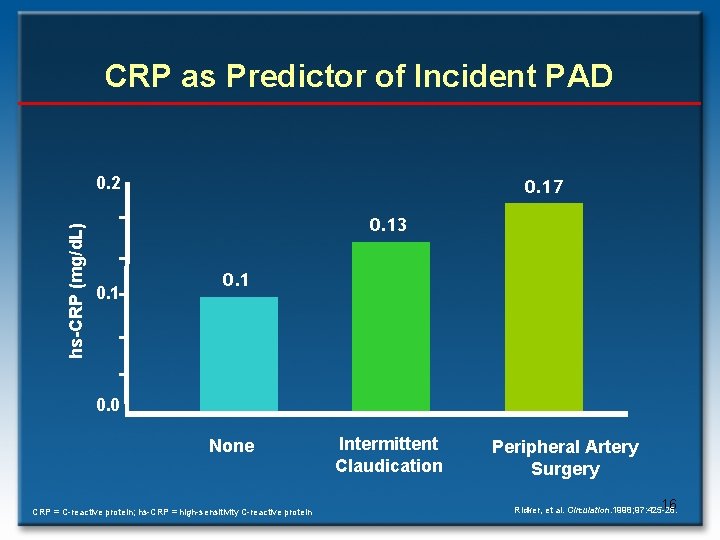
CRP as Predictor of Incident PAD hs-CRP (mg/d. L) 0. 2 0. 17 0. 13 0. 1 0. 0 None CRP = C-reactive protein; hs-CRP = high-sensitivity C-reactive protein Intermittent Claudication Peripheral Artery Surgery 16 Ridker, et al. Circulation. 1998; 97: 425 -28.
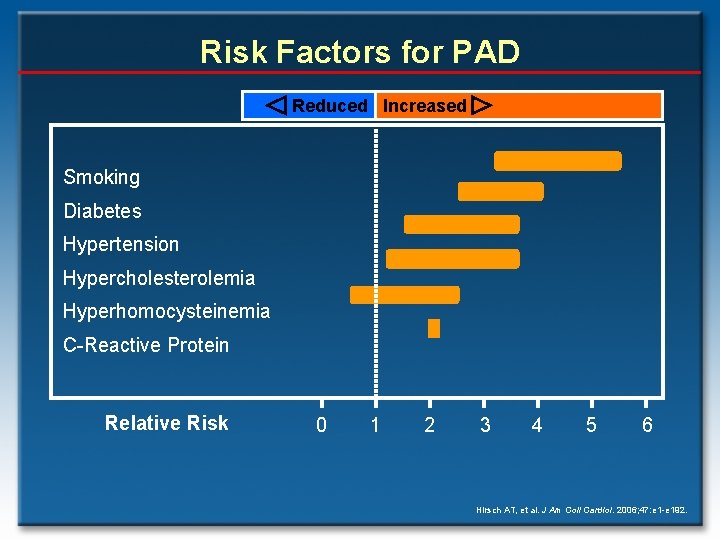
Risk Factors for PAD Reduced Increased Smoking Diabetes Hypertension Hypercholesterolemia Hyperhomocysteinemia C-Reactive Protein Relative Risk 0 1 2 3 4 5 6 Hirsch AT, et al. J Am Coll Cardiol. 2006; 47: e 1 -e 192.
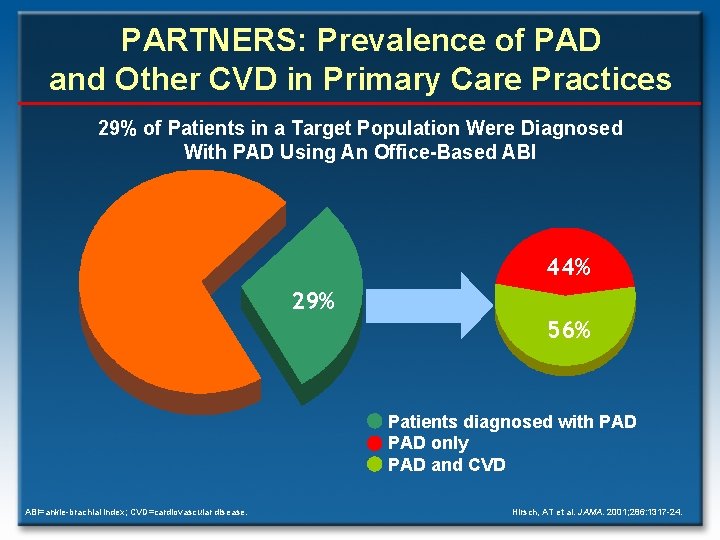
PARTNERS: Prevalence of PAD and Other CVD in Primary Care Practices 29% of Patients in a Target Population Were Diagnosed With PAD Using An Office-Based ABI 44% 29% 56% Patients diagnosed with PAD only PAD and CVD ABI=ankle-brachial index; CVD=cardiovascular disease. Hirsch, AT et al. JAMA. 2001; 286: 1317 -24.
Individuals “At Risk” for Lower Extremity PAD Based on the epidemiologic evidence base, an “at risk” population for PAD can be objectively defined by: • Age less than 50 years with diabetes, and one additional risk factor (e. g. , smoking, dyslipidemia, hypertension, or hyperhomocysteinemia) • Age 50 to 69 years and history of smoking or diabetes • Age 70 years and older • Leg symptoms with exertion (suggestive of claudication) or ischemic rest pain • Abnormal lower extremity pulse examination • Known atherosclerotic coronary, carotid, or renal artery disease
PAD Prognosis
The Natural History of PAD • Individuals with PAD are at increased risk for cardiovascular ischemic events due to concomitant CAD (fatal and non-fatal MI) and cerebrovascular disease (fatal and non-fatal stroke). • Cardiovascular events are more frequent than ischemic limb events in any lower extremity PAD cohort, regardless of the clinical presentation.
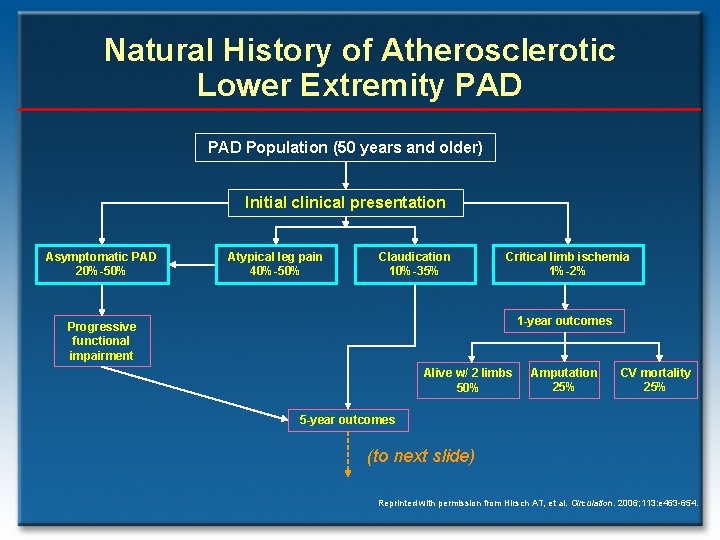
Natural History of Atherosclerotic Lower Extremity PAD Population (50 years and older) Initial clinical presentation Asymptomatic PAD 20%-50% Atypical leg pain 40%-50% Claudication 10%-35% Critical limb ischemia 1%-2% 1 -year outcomes Progressive functional impairment Alive w/ 2 limbs 50% Amputation 25% CV mortality 25% 5 -year outcomes (to next slide) Reprinted with permission from Hirsch AT, et al. Circulation. 2006; 113: e 463 -654.
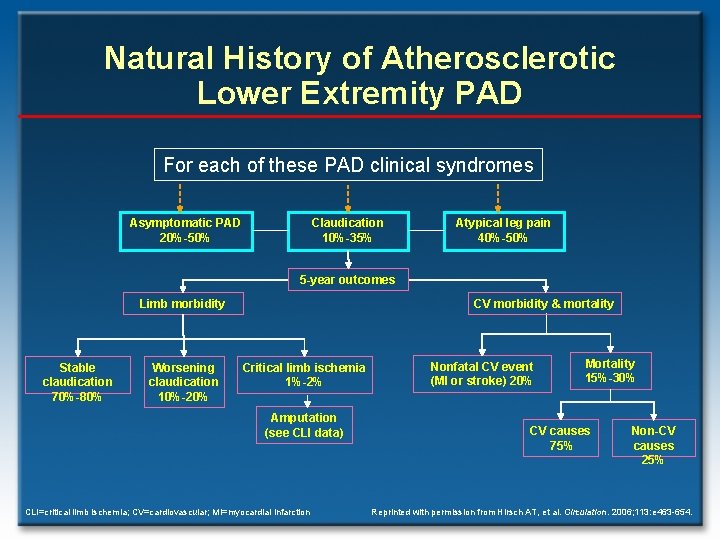
Natural History of Atherosclerotic Lower Extremity PAD For each of these PAD clinical syndromes Asymptomatic PAD 20%-50% Claudication 10%-35% Atypical leg pain 40%-50% 5 -year outcomes Limb morbidity Stable claudication 70%-80% Worsening claudication 10%-20% CV morbidity & mortality Critical limb ischemia 1%-2% Amputation (see CLI data) CLI=critical limb ischemia; CV=cardiovascular; MI=myocardial infarction Nonfatal CV event (MI or stroke) 20% Mortality 15%-30% CV causes 75% Non-CV causes 25% Reprinted with permission from Hirsch AT, et al. Circulation. 2006; 113: e 463 -654.
Contemporary PAD Rates of Myocardial Infarction and Death Percentage 3649 subjects (average 64 years) followed up for 7. 2 years Hooi JD, et al. J Clin Epid. 2004; 57: 294– 300.
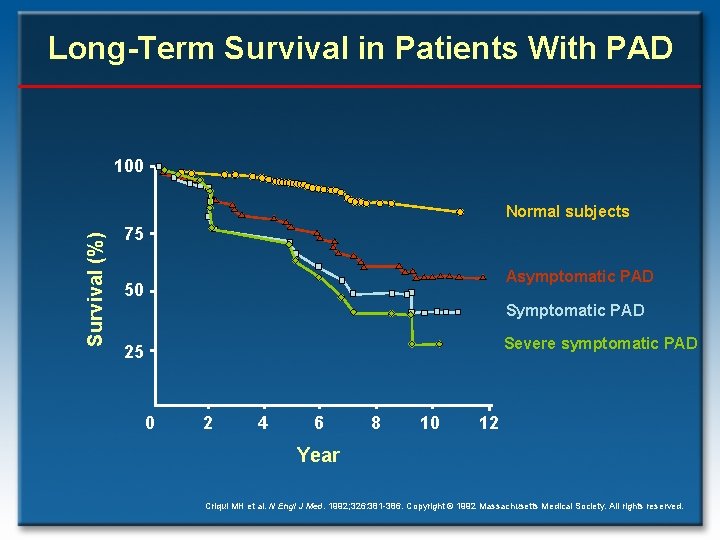
Long-Term Survival in Patients With PAD 100 Survival (%) Normal subjects 75 Asymptomatic PAD 50 Symptomatic PAD Severe symptomatic PAD 25 0 2 4 6 8 10 12 Year Criqui MH et al. N Engl J Med. 1992; 326: 381 -386. Copyright © 1992 Massachusetts Medical Society. All rights reserved.
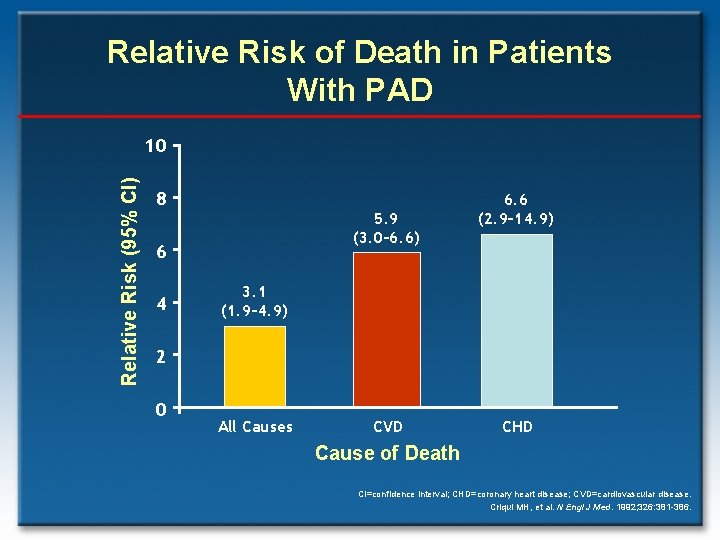
Relative Risk of Death in Patients With PAD Relative Risk (95% CI) 10 8 5. 9 (3. 0– 6. 6) 6 4 6. 6 (2. 9– 14. 9) 3. 1 (1. 9– 4. 9) 2 0 All Causes CVD CHD Cause of Death CI=confidence interval; CHD=coronary heart disease; CVD=cardiovascular disease. Criqui MH, et al. N Engl J Med. 1992; 326: 381 -386.
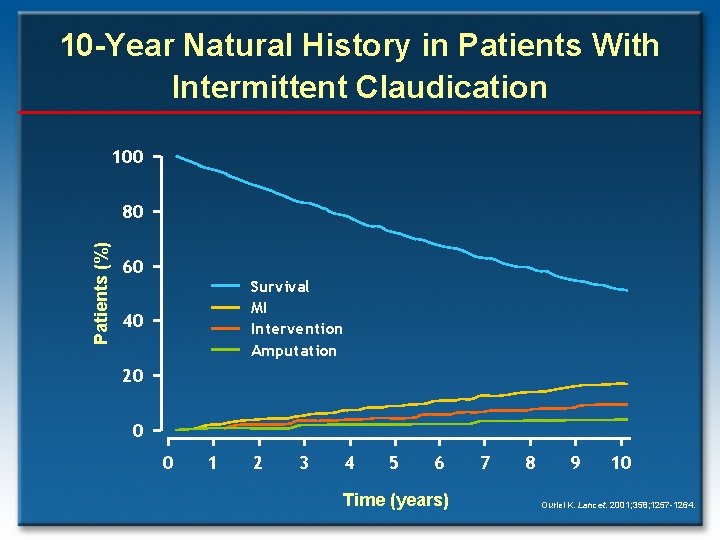
10 -Year Natural History in Patients With Intermittent Claudication 100 Patients (%) 80 60 Survival MI Intervention Amputation 40 20 0 0 1 2 3 4 5 6 Time (years) 7 8 9 10 Ouriel K. Lancet. 2001; 358; 1257 -1264.
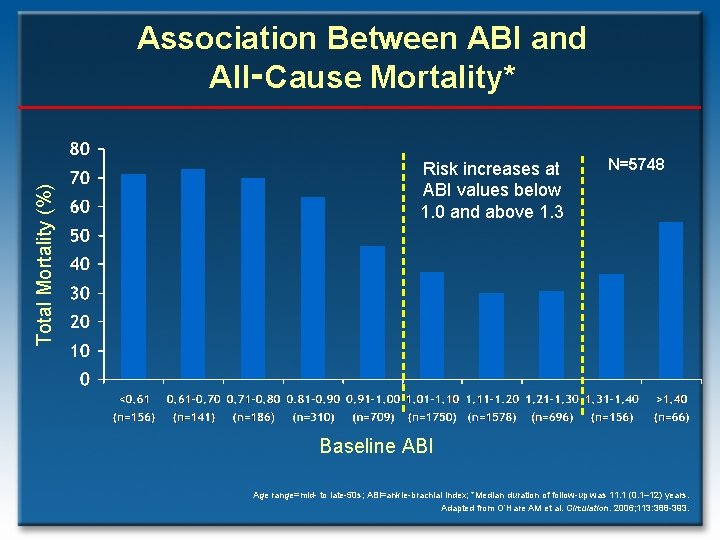
Total Mortality (%) Association Between ABI and All‑Cause Mortality* Risk increases at ABI values below 1. 0 and above 1. 3 N=5748 Baseline ABI Age range=mid- to late-50 s; ABI=ankle-brachial index; *Median duration of follow-up was 11. 1 (0. 1– 12) years. Adapted from O’Hare AM et al. Circulation. 2006; 113: 388 -393.
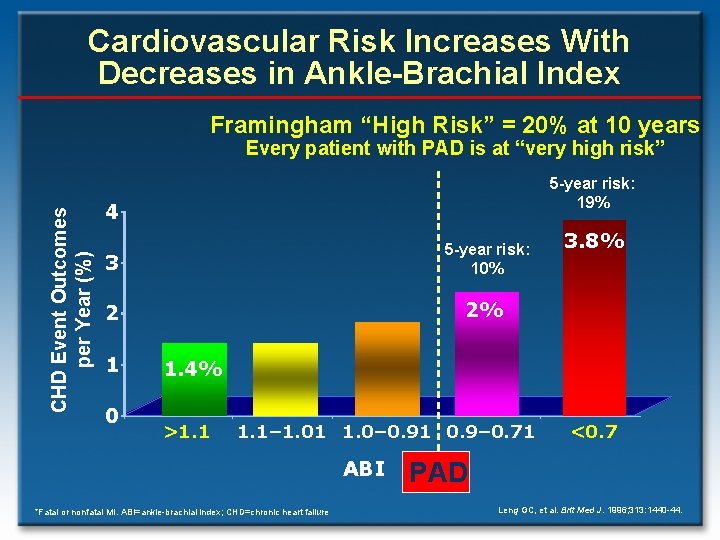
Cardiovascular Risk Increases With Decreases in Ankle-Brachial Index Framingham “High Risk” = 20% at 10 years CHD Event Outcomes per Year (%) Every patient with PAD is at “very high risk” 5 -year risk: 19% 4 3 5 -year risk: 10% 2 2% 1 0 3. 8% 1. 4% >1. 1– 1. 01 1. 0– 0. 91 0. 9– 0. 71 ABI *Fatal or nonfatal MI. ABI=ankle-brachial index; CHD=chronic heart failure <0. 7 PAD Leng GC, et al. Brit Med J. 1996; 313: 1440 -44.
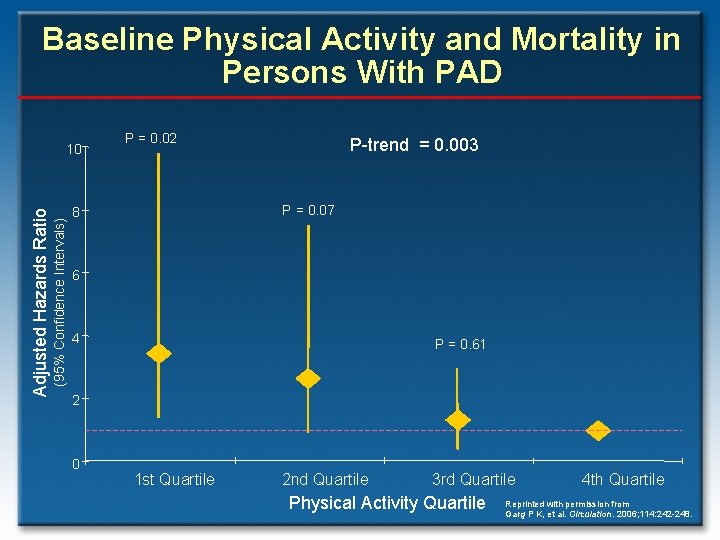
Baseline Physical Activity and Mortality in Persons With PAD (95% Confidence Intervals) Adjusted Hazards Ratio 10 P = 0. 02 P-trend = 0. 003 P = 0. 07 8 6 4 P = 0. 61 2 0 1 st Quartile 2 nd Quartile 3 rd Quartile Physical Activity Quartile 4 th Quartile Reprinted with permission from Garg P K, et al. Circulation. 2006; 114: 242 -248.
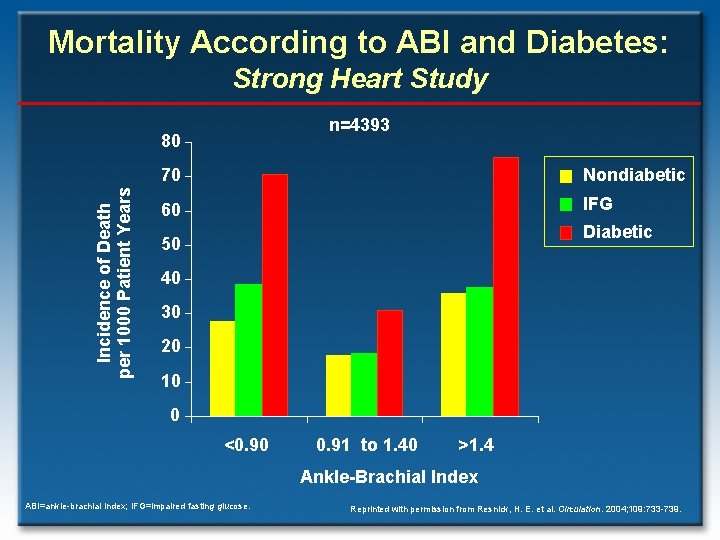
Mortality According to ABI and Diabetes: Strong Heart Study n=4393 Incidence of Death per 1000 Patient Years 80 70 Nondiabetic 60 IFG Diabetic 50 40 30 20 10 0 <0. 90 0. 91 to 1. 40 >1. 4 Ankle-Brachial Index ABI=ankle-brachial index; IFG=impaired fasting glucose. Reprinted with permission from Resnick, H. E. et al. Circulation. 2004; 109: 733 -739.
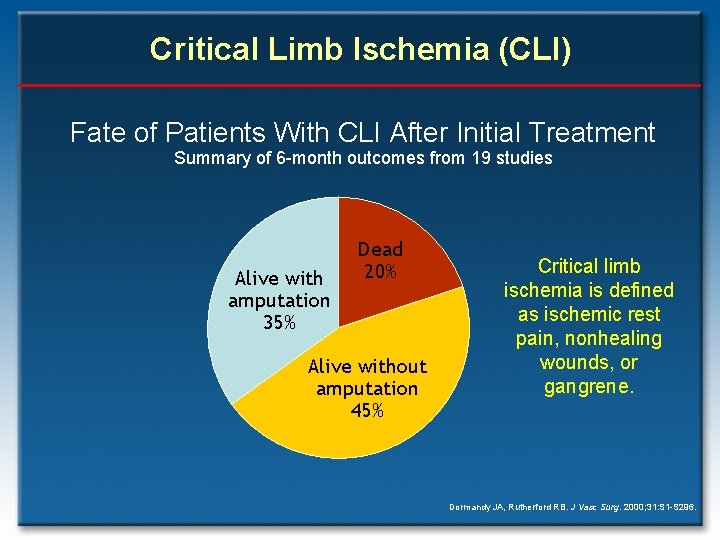
Critical Limb Ischemia (CLI) Fate of Patients With CLI After Initial Treatment Summary of 6 -month outcomes from 19 studies Alive with amputation 35% Dead 20% Alive without amputation 45% Critical limb ischemia is defined as ischemic rest pain, nonhealing wounds, or gangrene. Dormandy JA, Rutherford RB. J Vasc Surg. 2000; 31: S 1 -S 296.
- Slides: 32