The Partograph DEFINITION The partograph is a graphical


- Slides: 35
The Partograph
DEFINITION; The partograph is a graphical presentation of the progress of labour, and of fetal and maternal condition during labour. you should always use a partograph while attending a woman in labour
THE VALUE OF USING THE PARTOGRAPH It is the best tool to help you detect whether labour is progressing normally or abnormally. warn you as soon as possible if there are signs of fetal distress or if the mother’s vital signs deviate from the normal range. Detection of cephalopelvic disproportion before the obstruction appears. Helps to make quick and logical decisions for managing labour. Identifies the necessary interventions. Simple, low cost, accessible and clear. maternal and fetal complications due to prolonged labour were less common when the progress of labour was monitored by the birth attendant using a partograph.
What is the difference between a woman who is a multigravida and one who is a multipara? multigravida is a woman who has been pregnant at least once before the current pregnancy. A multipara is awoman who has previously given birth to live babies at least twice before now
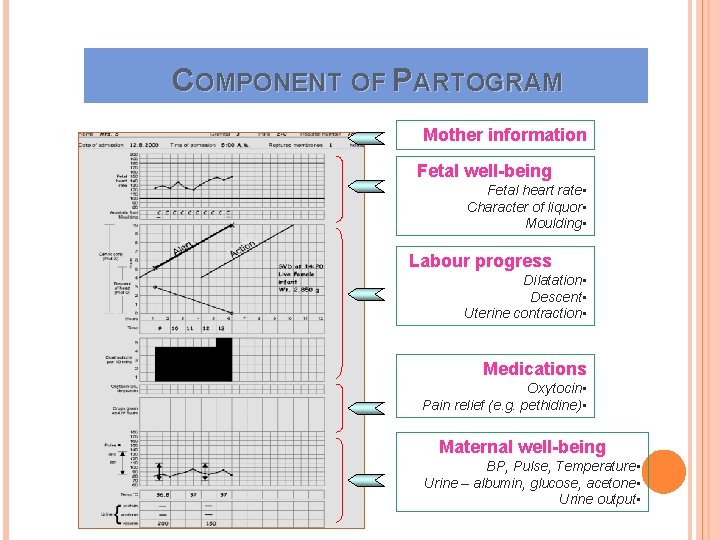
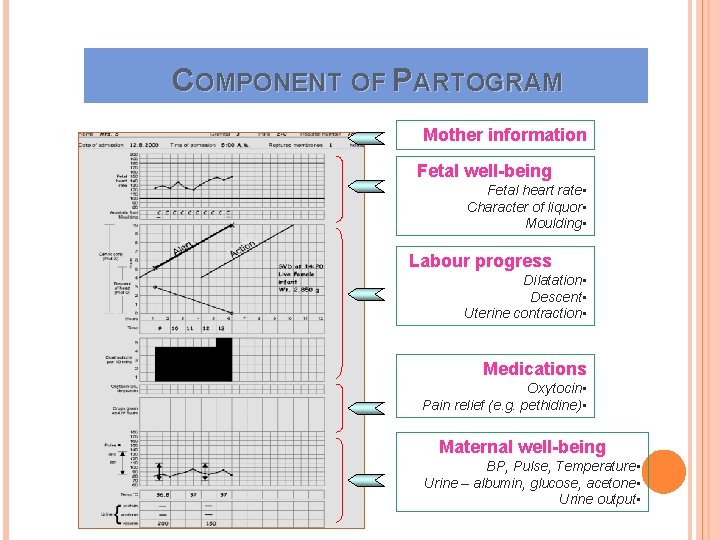
COMPONENT OF PARTOGRAM Mother information Fetal well-being Fetal heart rate • Character of liquor • Moulding • Labour progress Dilatation • Descent • Uterine contraction • Medications Oxytocin • Pain relief (e. g. pethidine) • Maternal well-being BP, Pulse, Temperature • Urine – albumin, glucose, acetone • Urine output •
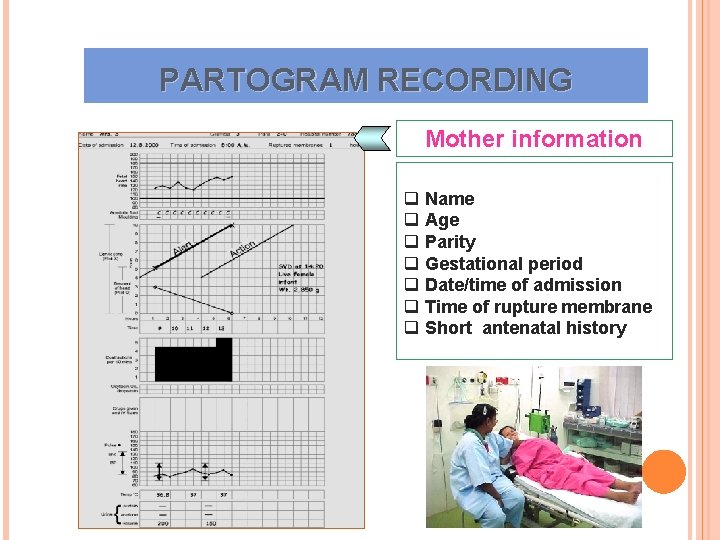
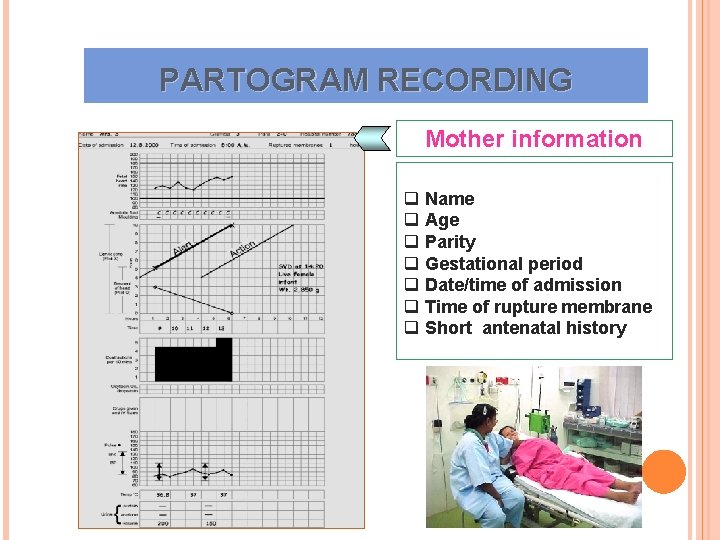
PARTOGRAM RECORDING Mother information q Name q Age q Parity q Gestational period q Date/time of admission q Time of rupture membrane q Short antenatal history
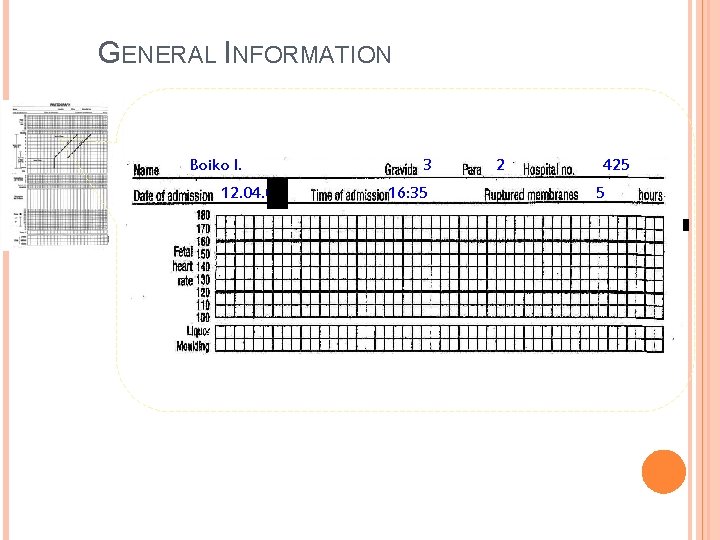
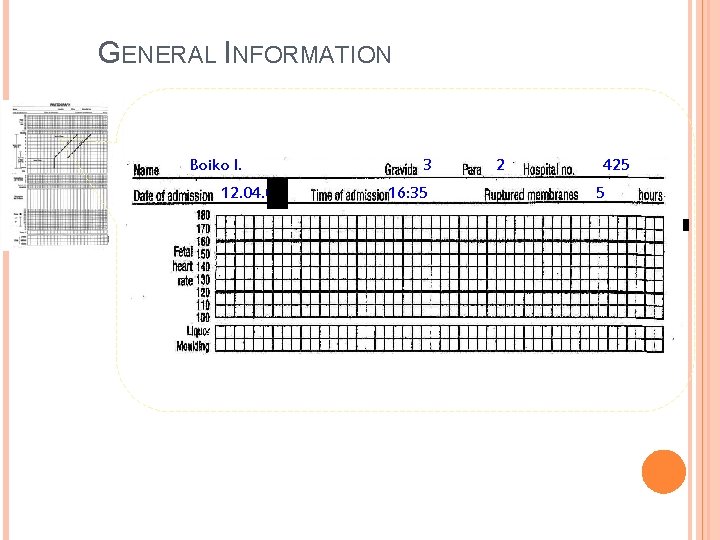
GENERAL INFORMATION Boiko I. 12. 04. 06 3 16: 35 2 425 5
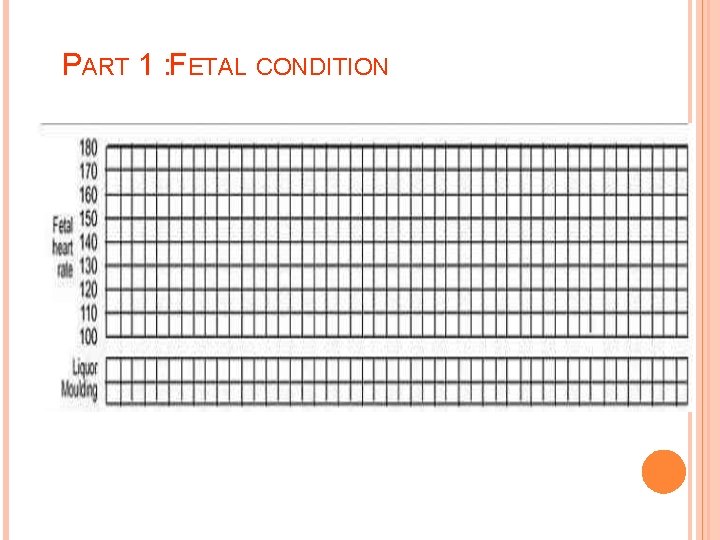
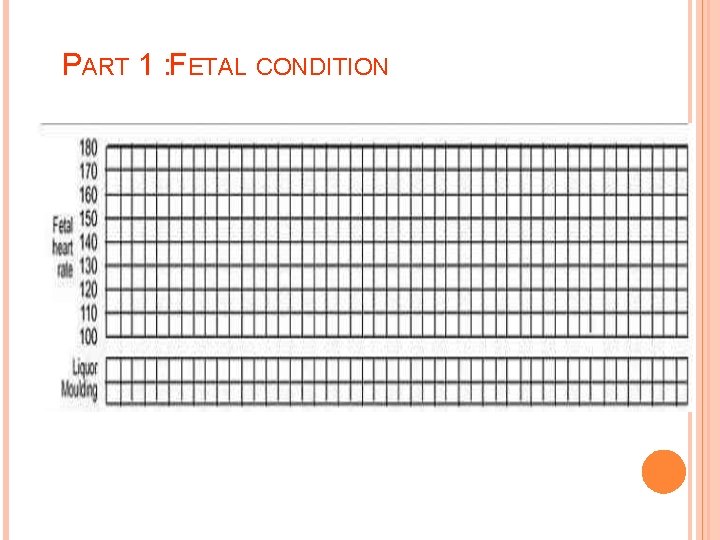
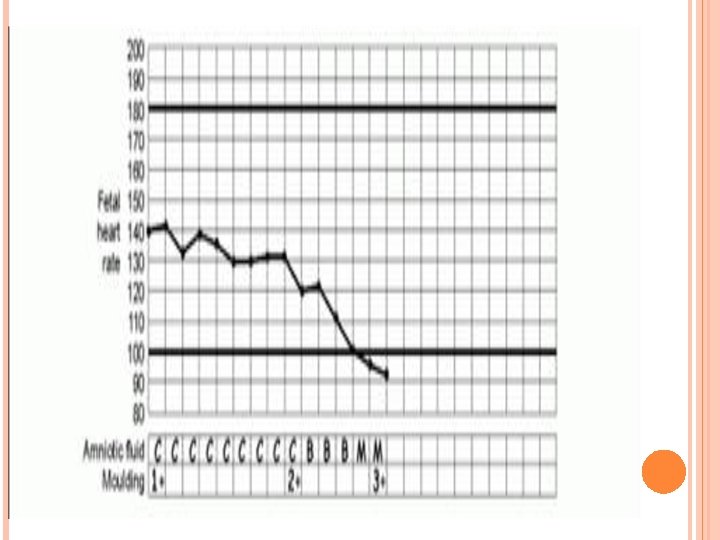
PART 1 : FETAL CONDITION
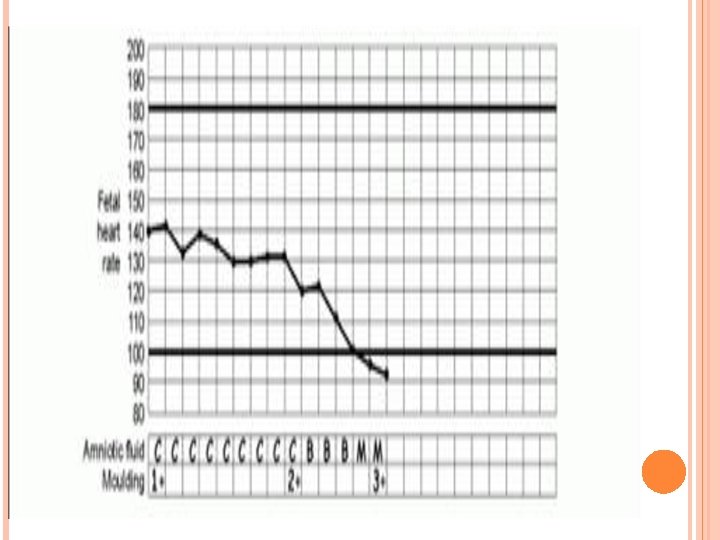
AMNIOTIC FLUID I – the membranes intact C – clear amniotic fluid В – blood-stained amniotic fluid M – meconium-stained amniotic fluid A – absent amniotic fluid
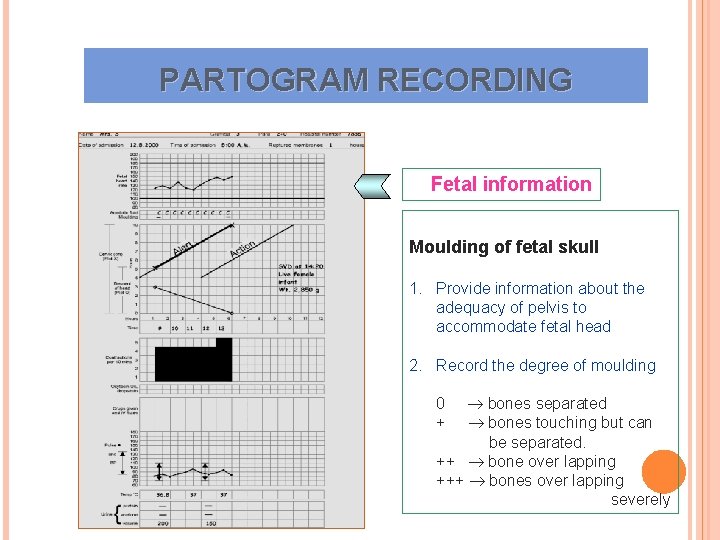
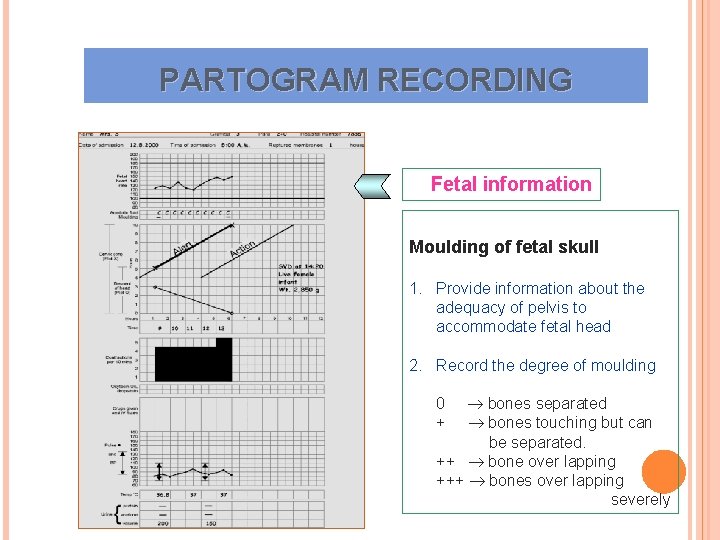
PARTOGRAM RECORDING Fetal information Moulding of fetal skull 1. Provide information about the adequacy of pelvis to accommodate fetal head 2. Record the degree of moulding bones separated bones touching but can be separated. ++ bone over lapping +++ bones over lapping severely 0 +
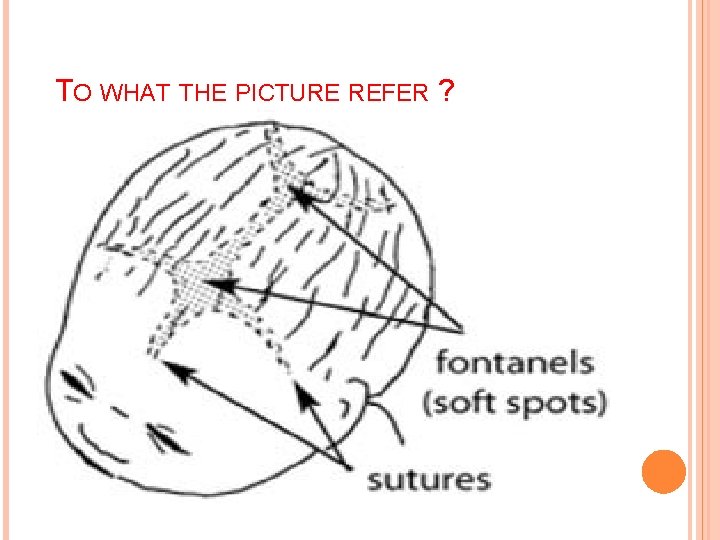
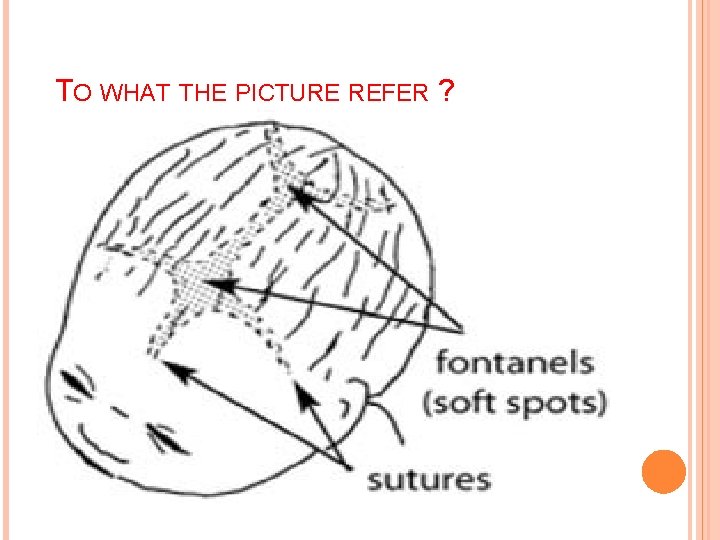
TO WHAT THE PICTURE REFER ?
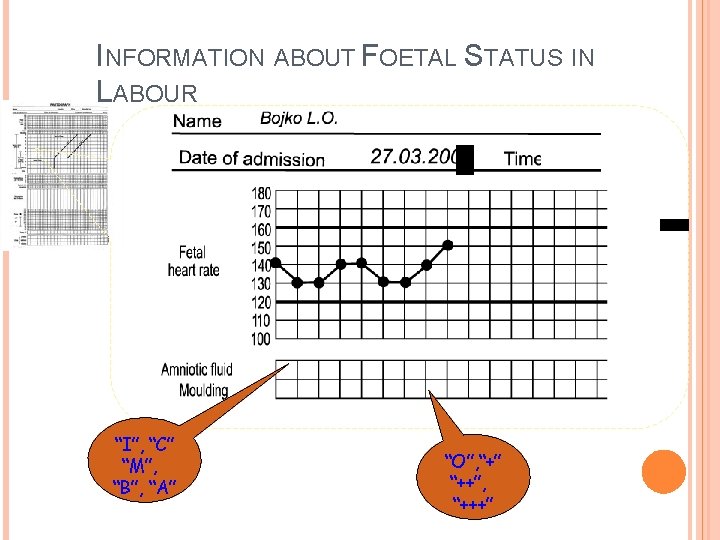
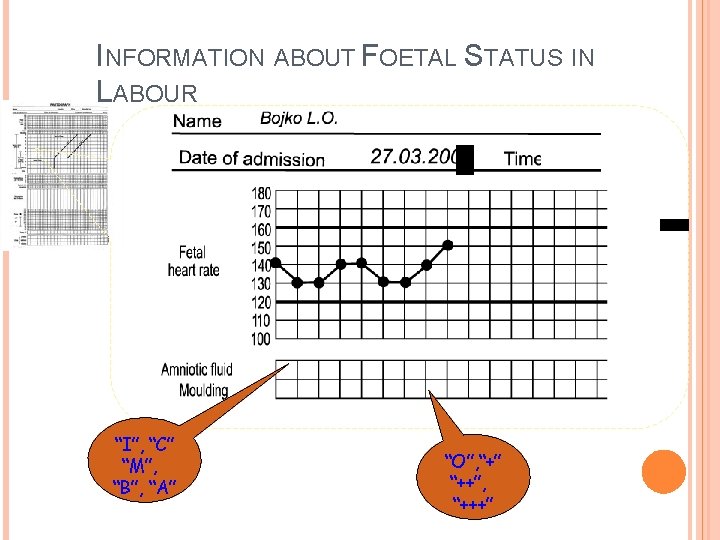
INFORMATION ABOUT FOETAL STATUS IN LABOUR “I”, “C” “M”, “B”, “A” “O”, “+” “++”, “+++”
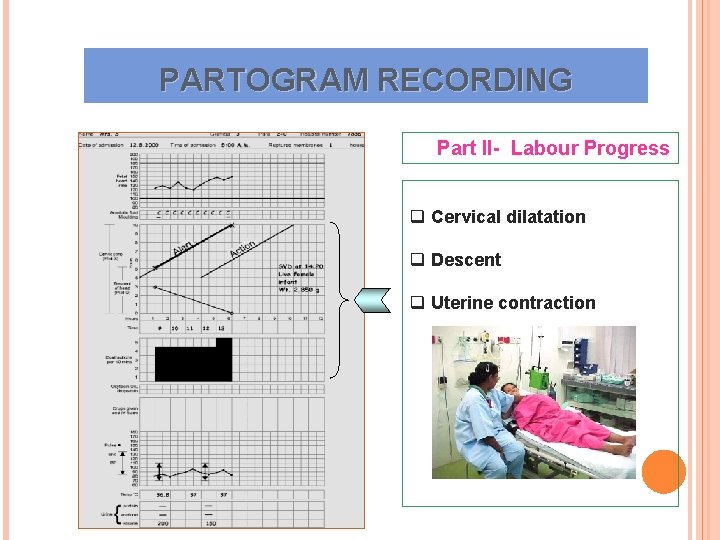
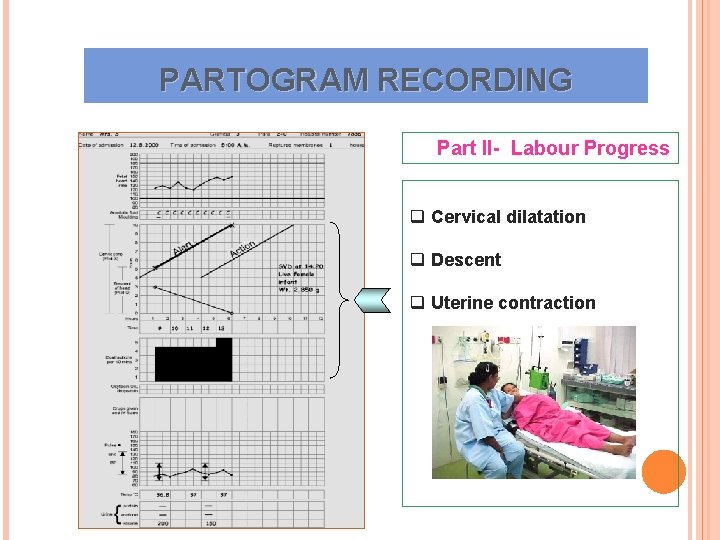
PARTOGRAM RECORDING Part II- Labour Progress q Cervical dilatation q Descent q Uterine contraction
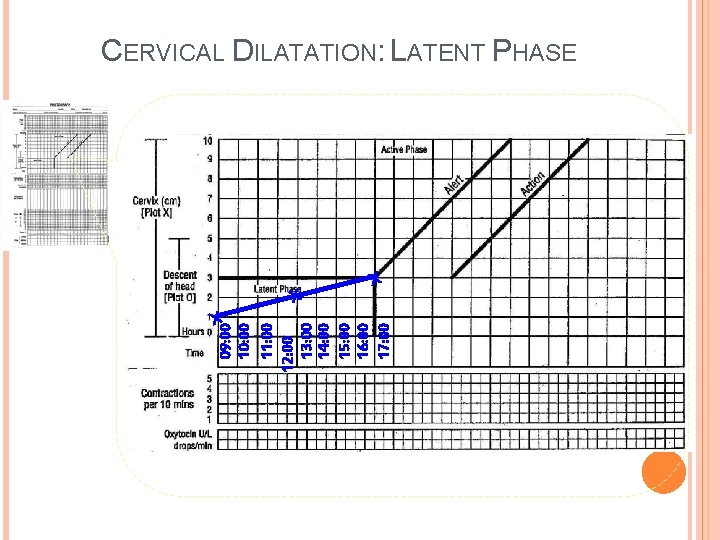
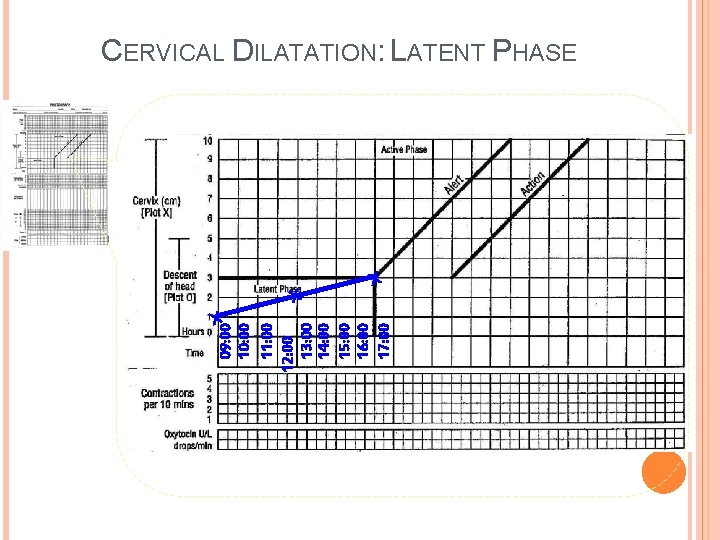
X 09: 00 10: 00 11: 00 12: 00 13: 00 14: 00 15: 00 16: 00 17: 00 CERVICAL DILATATION: LATENT PHASE X X
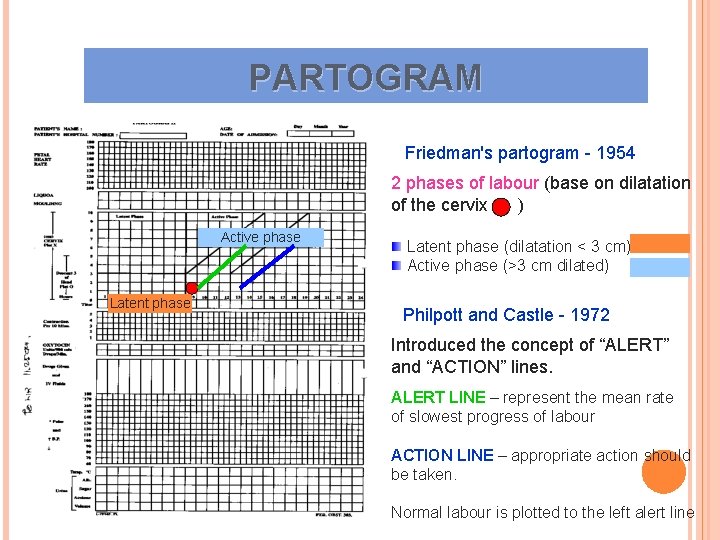
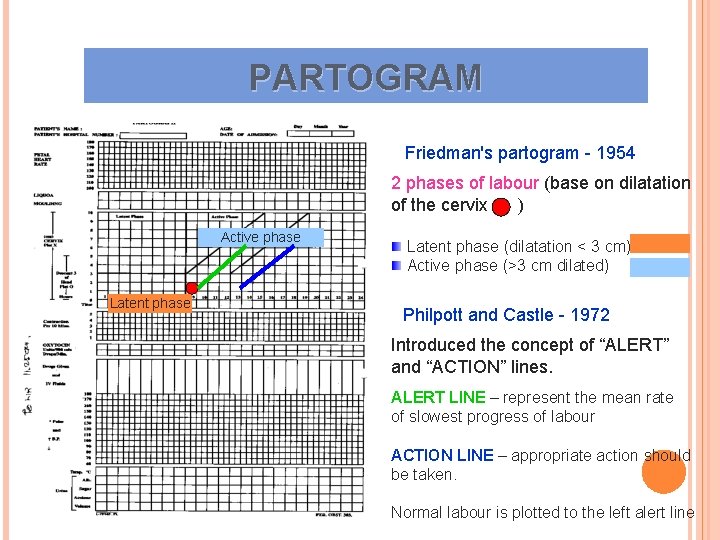
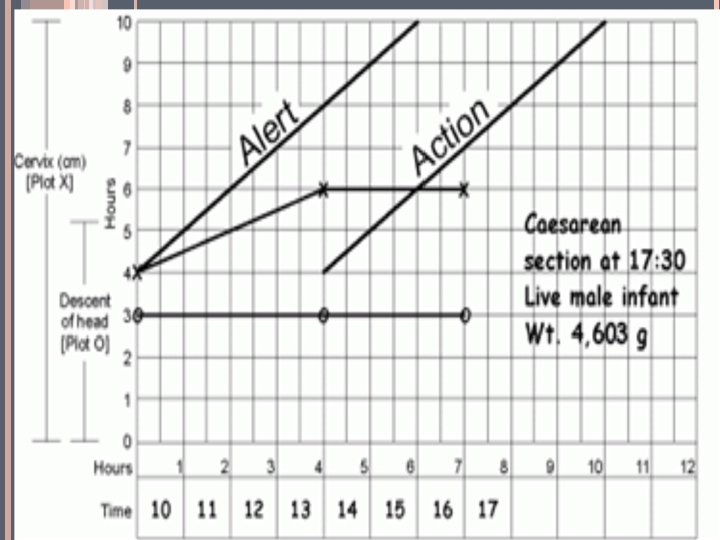
PARTOGRAM Friedman's partogram - 1954 2 phases of labour (base on dilatation of the cervix ) Active phase Latent phase (dilatation < 3 cm) Active phase (>3 cm dilated) Philpott and Castle - 1972 Introduced the concept of “ALERT” and “ACTION” lines. ALERT LINE – represent the mean rate of slowest progress of labour ACTION LINE – appropriate action should be taken. Normal labour is plotted to the left alert line
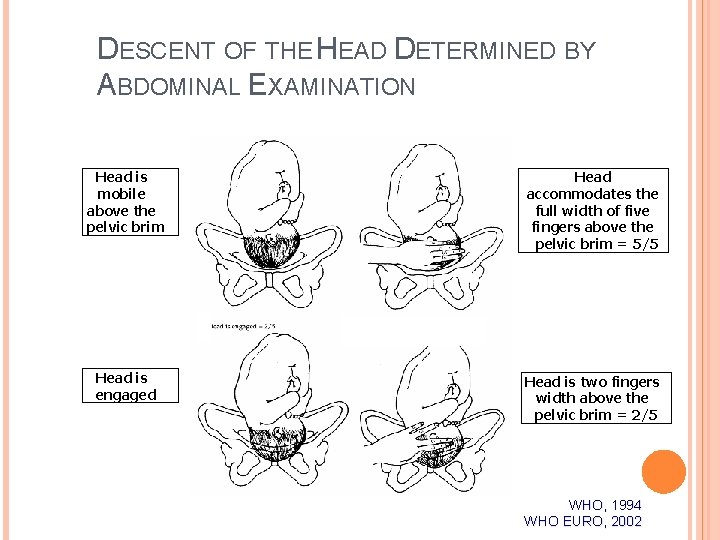
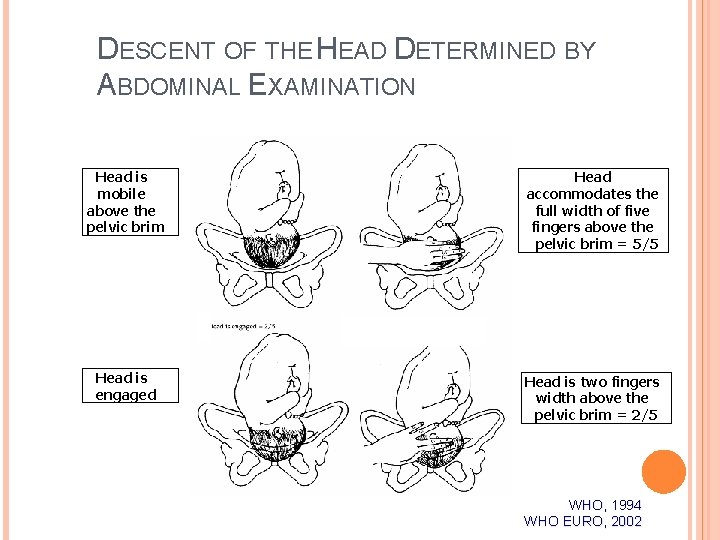
DESCENT OF THE HEAD DETERMINED BY ABDOMINAL EXAMINATION Head is mobile above the pelvic brim Head accommodates the full width of five fingers above the pelvic brim = 5/5 Head is engaged Head is two fingers width above the pelvic brim = 2/5 WHO, 1994 WHO EURO, 2002
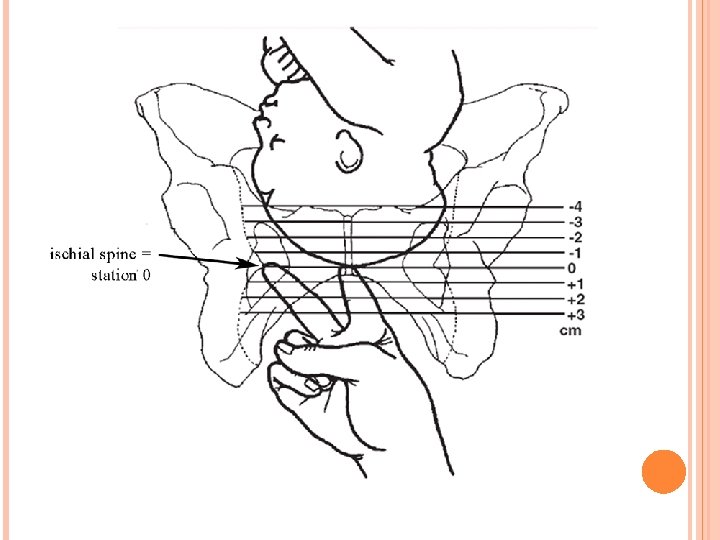
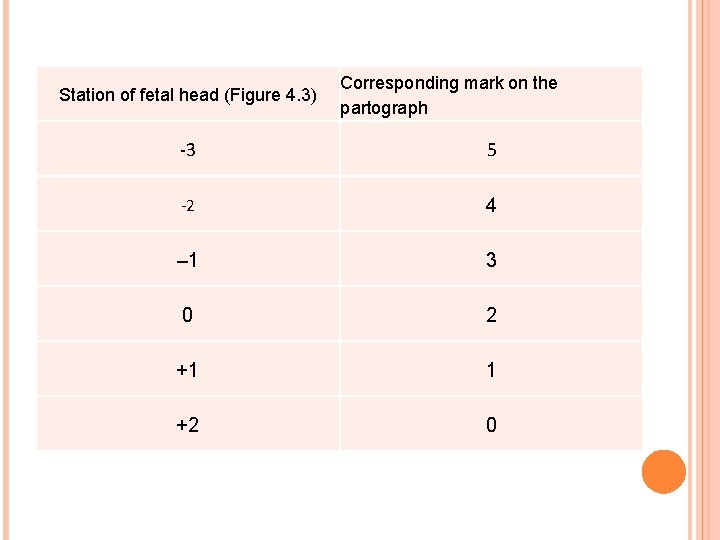
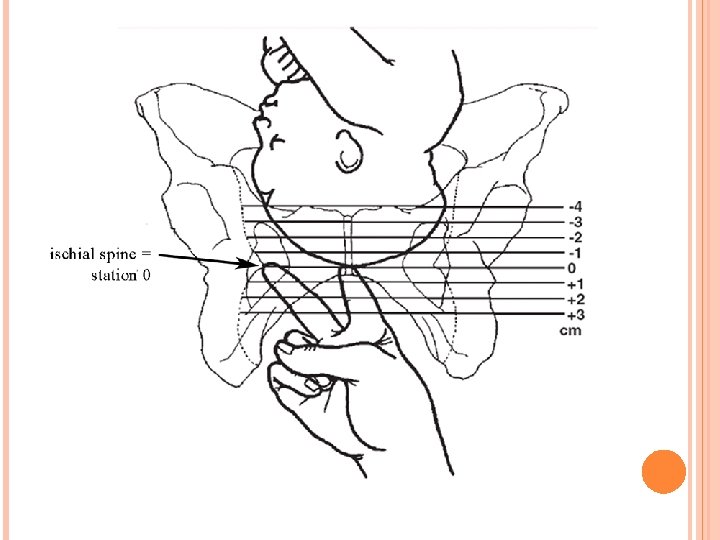
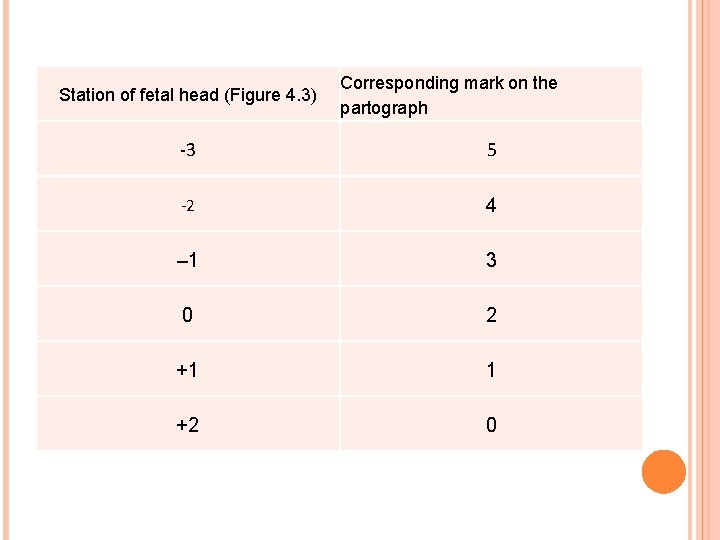
Station of fetal head (Figure 4. 3) Corresponding mark on the partograph -3 5 -2 4 – 1 3 0 2 +1 1 +2 0
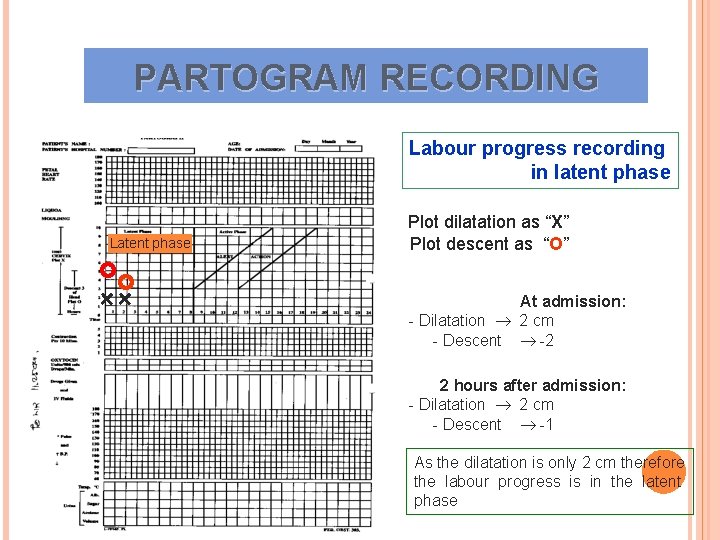
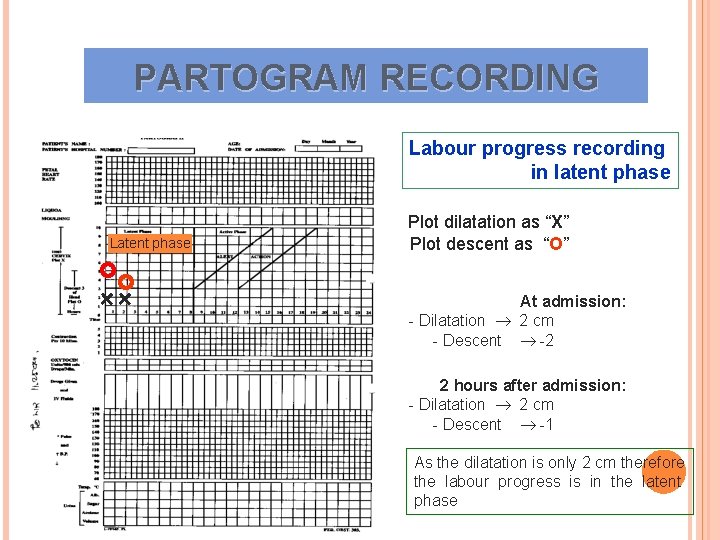
PARTOGRAM RECORDING Labour progress recording in latent phase Latent phase Plot dilatation as “X” Plot descent as “O” + + At admission: - Dilatation 2 cm - Descent -2 2 hours after admission: - Dilatation 2 cm - Descent -1 As the dilatation is only 2 cm therefore the labour progress is in the latent phase
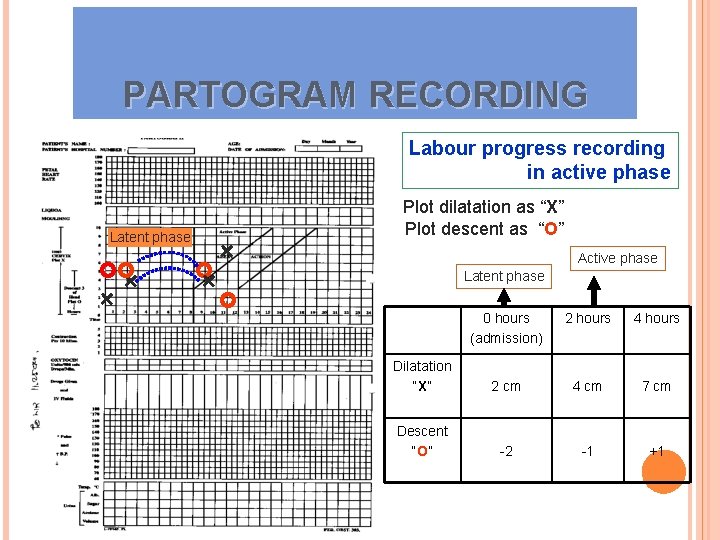
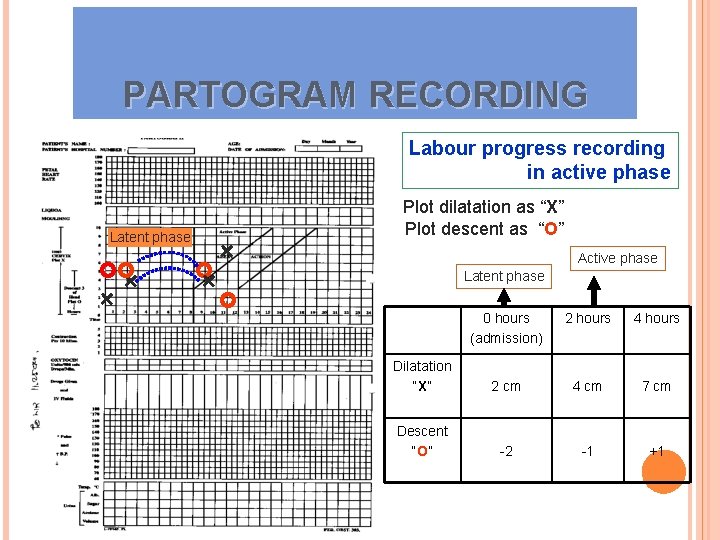
PARTOGRAM RECORDING Labour progress recording in active phase Plot dilatation as “X” Plot descent as “O” Latent phase + Active phase + + Latent phase + 0 hours (admission) 2 hours 4 hours Dilatation “X” 2 cm 4 cm 7 cm Descent “O” -2 -1 +1
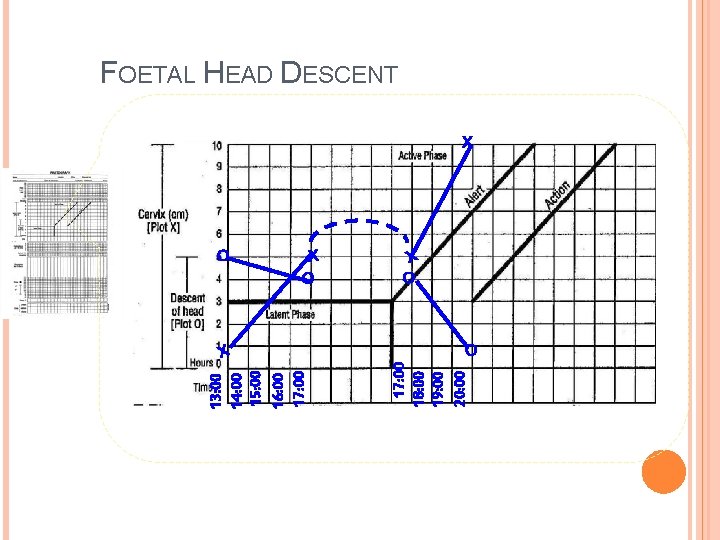
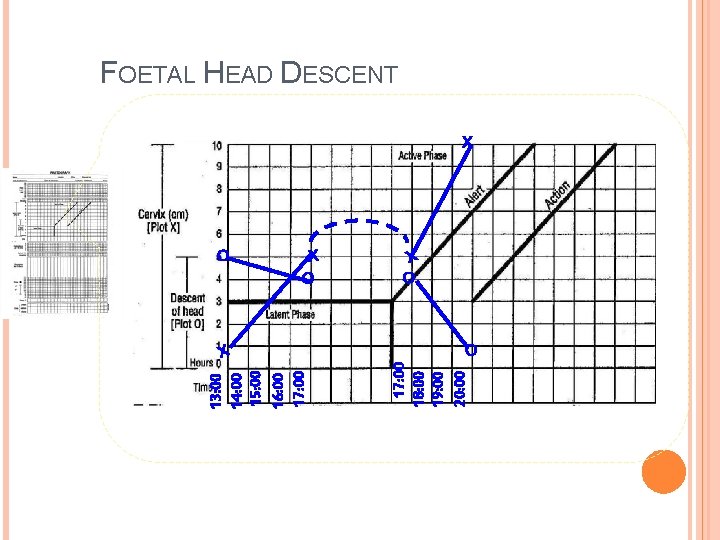
O X 17: 00 18: 00 19: 00 20: 00 13: 00 14: 00 15: 00 16: 00 17: 00 FOETAL HEAD DESCENT X X O O
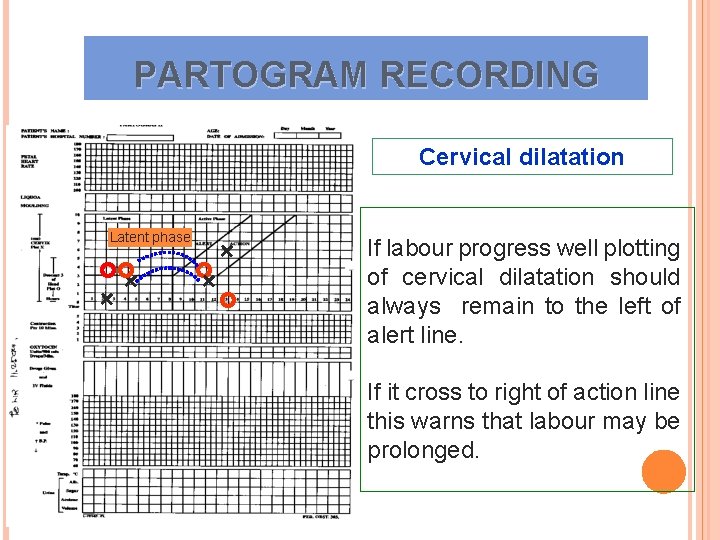
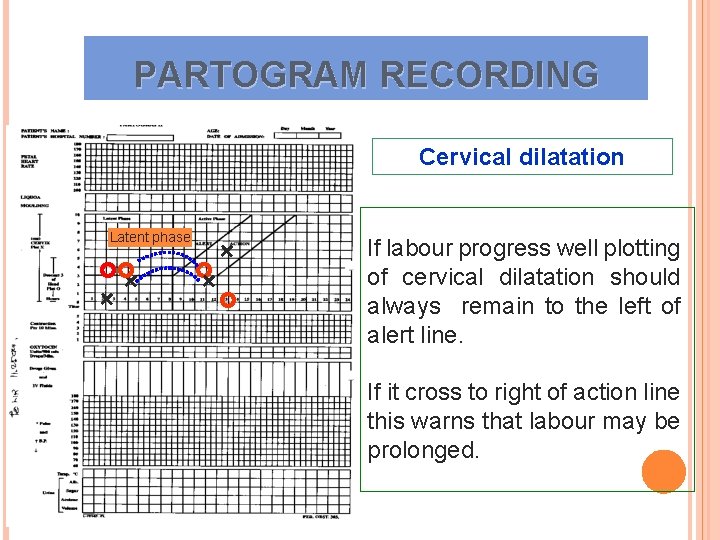
PARTOGRAM RECORDING Cervical dilatation Latent phase + + If labour progress well plotting of cervical dilatation should always remain to the left of alert line. If it cross to right of action line this warns that labour may be prolonged.
24
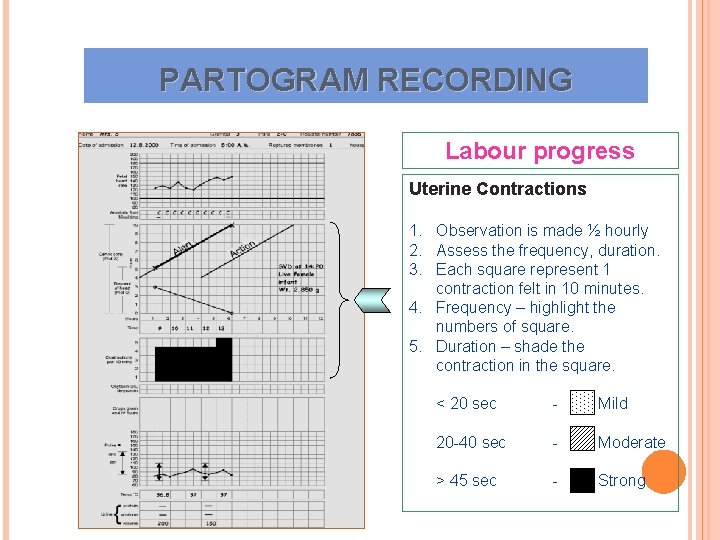
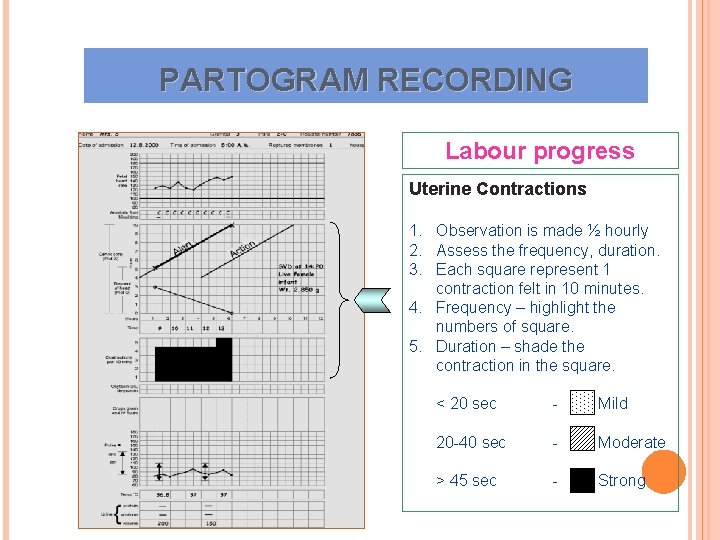
PARTOGRAM RECORDING Labour progress Uterine Contractions 1. Observation is made ½ hourly 2. Assess the frequency, duration. 3. Each square represent 1 contraction felt in 10 minutes. 4. Frequency – highlight the numbers of square. 5. Duration – shade the contraction in the square. < 20 sec - Mild 20 -40 sec - Moderate > 45 sec - Strong
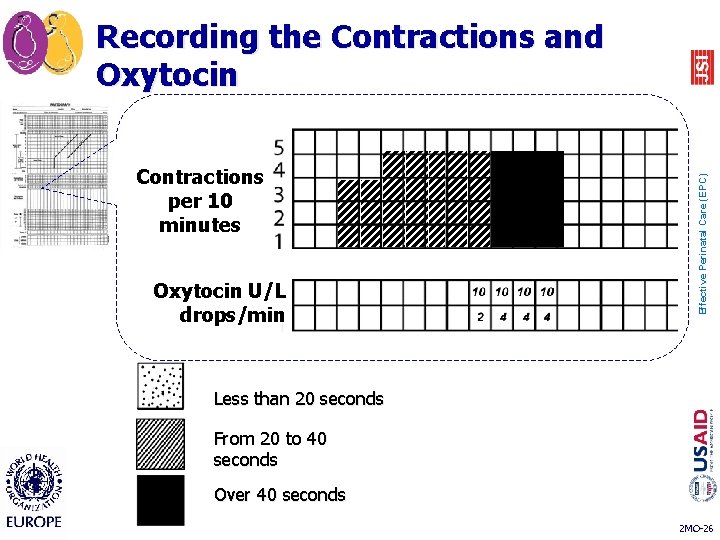
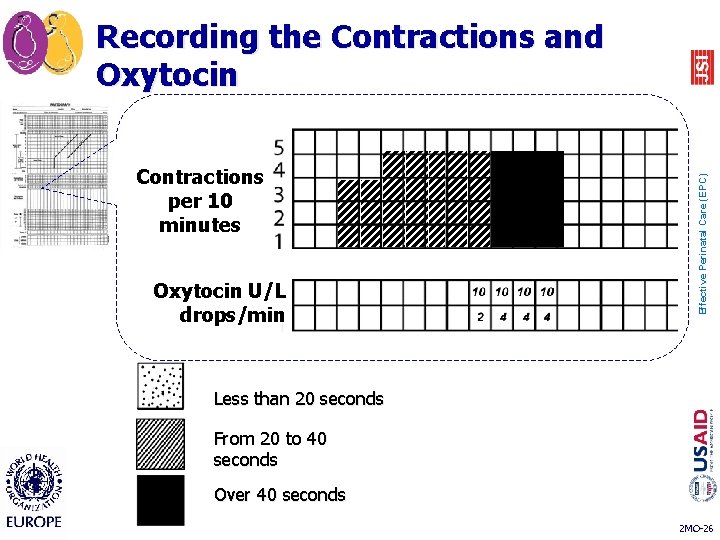
Contractions per 10 minutes Oxytocin U/L drops/min Effective Perinatal Care (EPC) Recording the Contractions and Oxytocin Less than 20 seconds From 20 to 40 seconds Over 40 seconds 2 MO-26
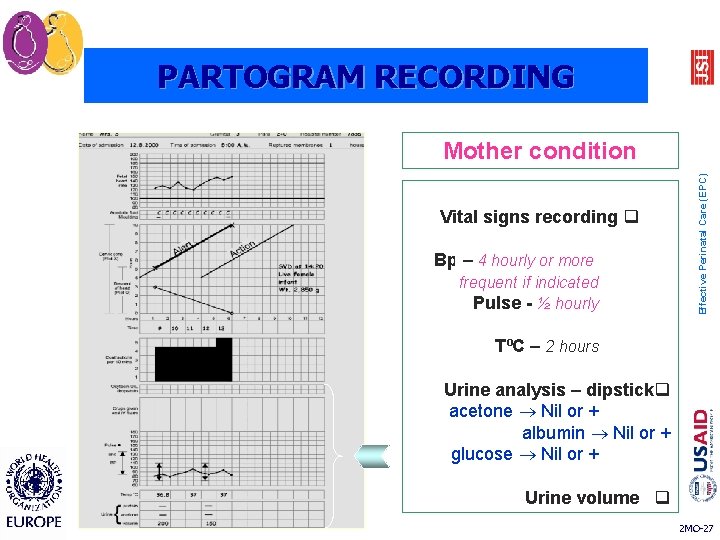
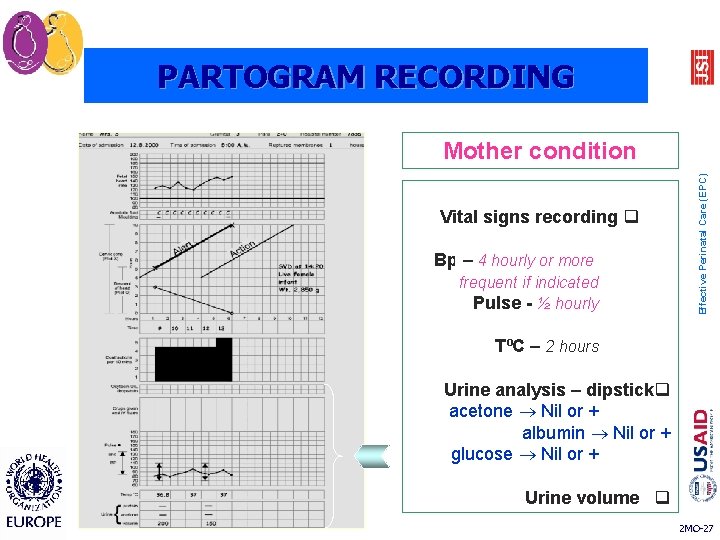
PARTOGRAM RECORDING Vital signs recording q Bp – 4 hourly or more frequent if indicated Pulse - ½ hourly Effective Perinatal Care (EPC) Mother condition TºC – 2 hours Urine analysis – dipstickq acetone Nil or + albumin Nil or + glucose Nil or + Urine volume q 2 MO-27
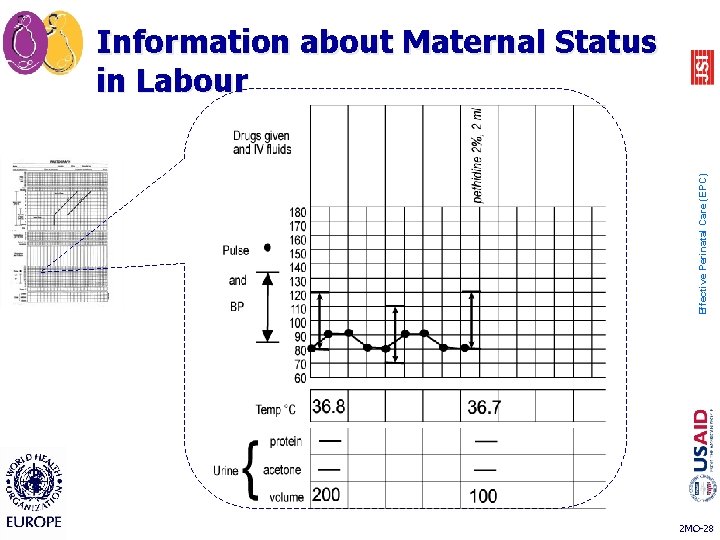
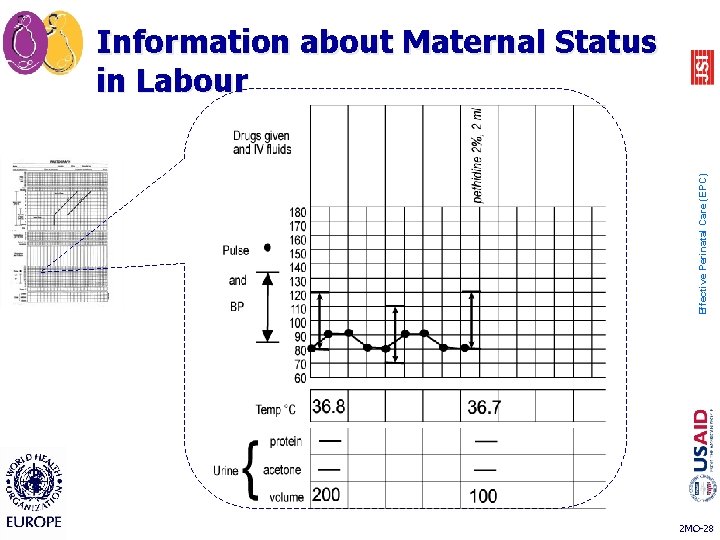
Effective Perinatal Care (EPC) Information about Maternal Status in Labour 2 MO-28

Effective Perinatal Care (EPC) Partograph showing normal labor 2 MO-29
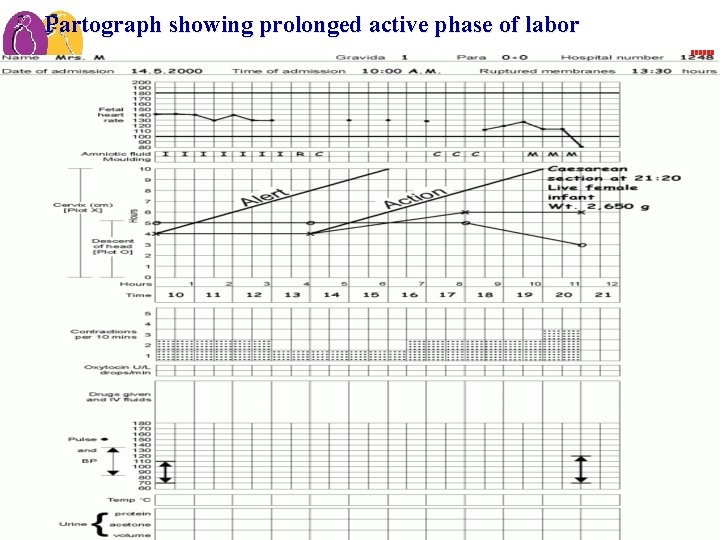
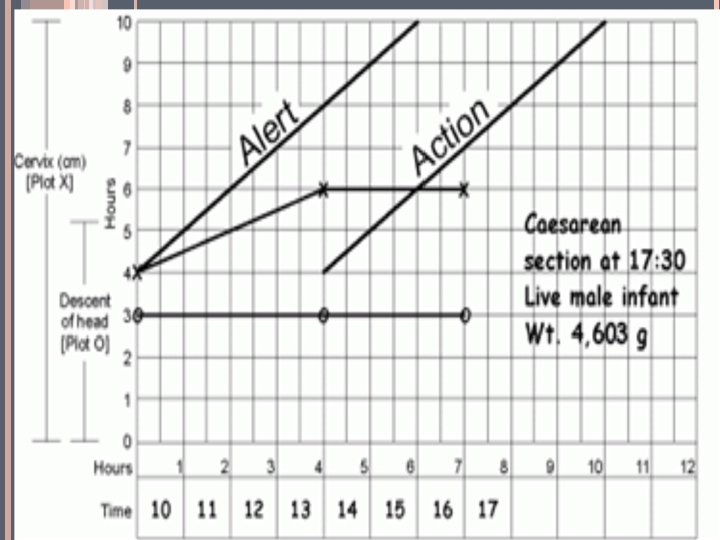
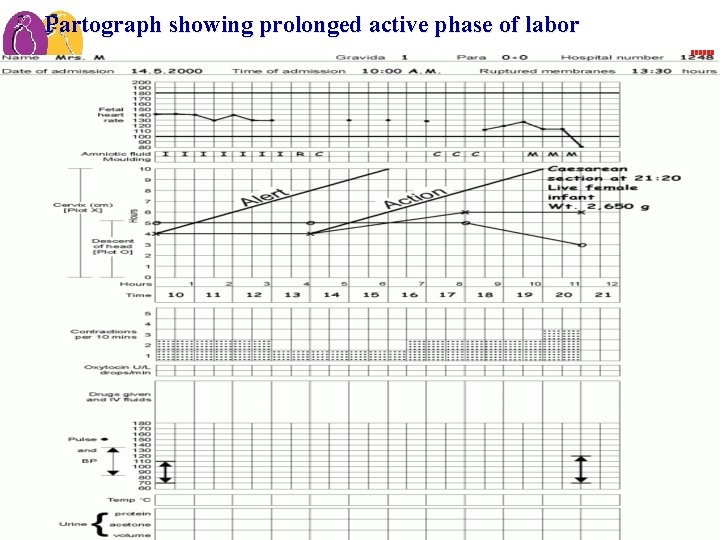
Effective Perinatal Care (EPC) Partograph showing prolonged active phase of labor 2 MO-30
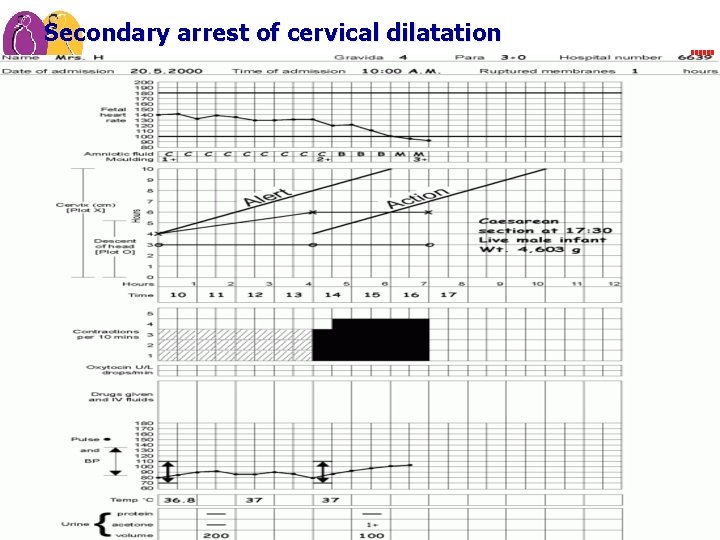
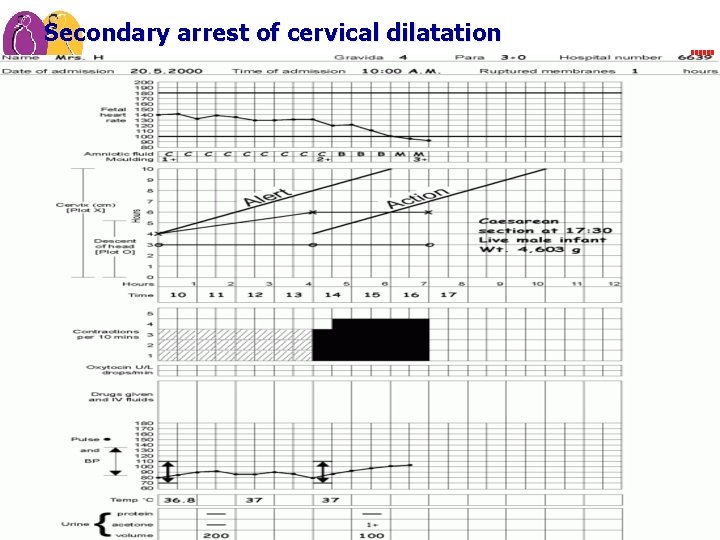
Effective Perinatal Care (EPC) Secondary arrest of cervical dilatation 2 MO-31
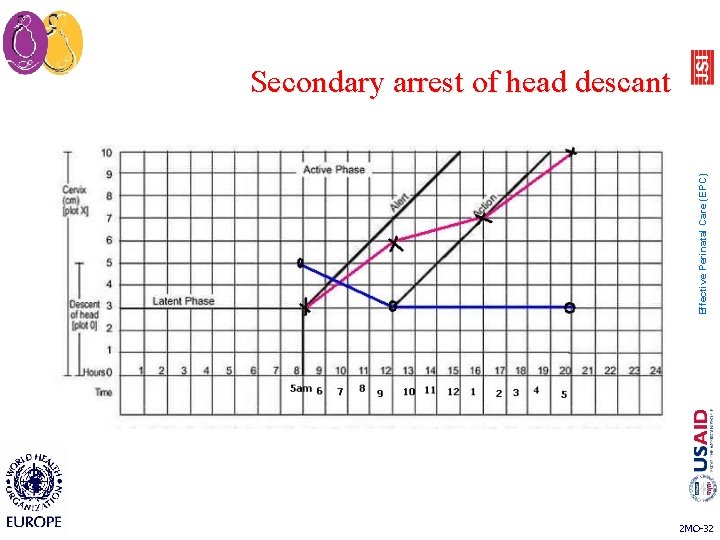
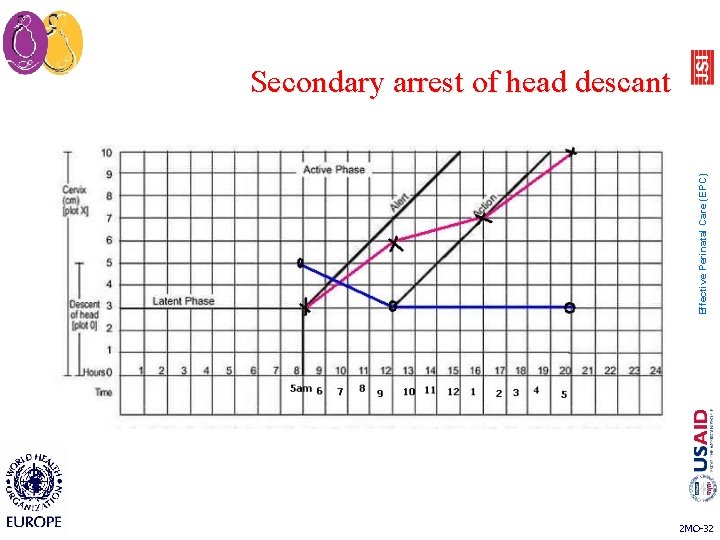
Effective Perinatal Care (EPC) Secondary arrest of head descant 2 MO-32
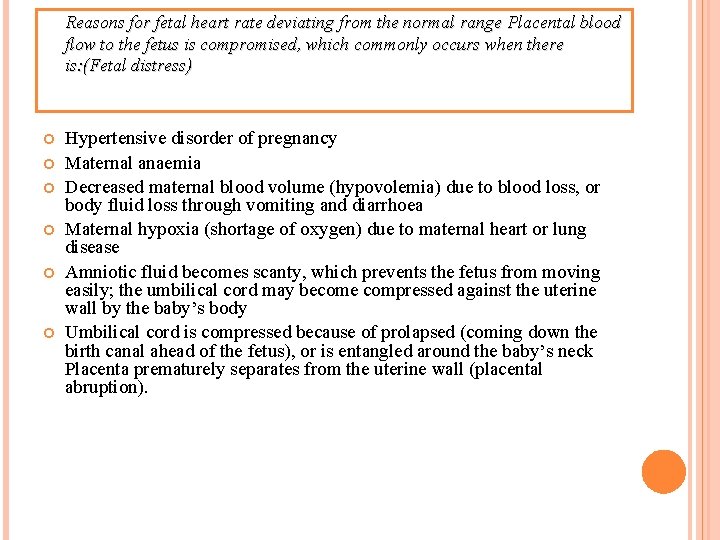
Reasons for fetal heart rate deviating from the normal range Placental blood flow to the fetus is compromised, which commonly occurs when there is: (Fetal distress) Hypertensive disorder of pregnancy Maternal anaemia Decreased maternal blood volume (hypovolemia) due to blood loss, or body fluid loss through vomiting and diarrhoea Maternal hypoxia (shortage of oxygen) due to maternal heart or lung disease Amniotic fluid becomes scanty, which prevents the fetus from moving easily; the umbilical cord may become compressed against the uterine wall by the baby’s body Umbilical cord is compressed because of prolapsed (coming down the birth canal ahead of the fetus), or is entangled around the baby’s neck Placenta prematurely separates from the uterine wall (placental abruption).

Any Question?
Thank YOU With My Best Wishes, Clinical Demonstrator. Eman A. Magraby