The Pancreas Dr Rahmani MD APCP The Pancreas












- Slides: 64

The Pancreas Dr. Rahmani MD, APCP
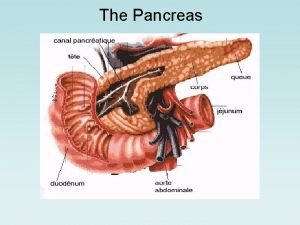
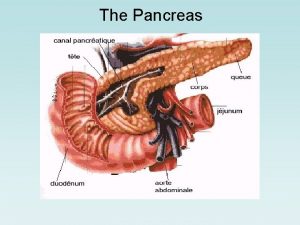
The Pancreas The adult pancreas is a transversely oriented retroperitoneal organ extending from the "C" loop of the duodenum to the hilum of the spleen adjacent vessels and ligaments can demarcate the organ into a head, body, and tail
The Pancreas A complex lobulated organ with distinct endocrine and exocrine elements The endocrine portion constitutes only 1% to 2% of the pancreas Composed of about 1 million cell clusters, the islets of Langerhans secrete insulin, glucagon, and somatostatin
The Pancreas The exocrine pancreas § acinar cells produce mostly proenzyme forms of the digestive enzymes § ductules and ducts convey them to the duodenum The epithelial cells lining the ducts § cuboidal epithelial cells lining the smaller ductules secrete bicarbonate-rich fluid § columnar epithelial cells lining the larger ducts produce mucin
The Pancreas The exocrine products secreted as enzymatically inert proenzymes (e. g. trypsinogen) Amylase and lipase are exceptions (secreted in an active form) The strategy of producing most pancreatic enzymes in an inactive zymogen form is largely to prevent self-digestion
The Pancreas A number of "fail-safe" mechanisms have evolved to minimize the risk of autodigestion of the pancreas: § The majority of pancreatic enzymes are synthesized as inactive proenzymes § The proenzymes are sequestered in membrane-bound zymogen granules

The Pancreas § Activation of proenzymes requires conversion of trypsinogen to trypsin by duodenal enteropeptidase (enterokinase) § Trypsin inhibitors § Trypsin contains a critical self-recognition cleavage site
The Pancreas § Most of the secreted enzymes are relatively inactive in the bicarbonate-rich pancreatic fluid § Enzymes within lysosomes can degrade zymogen granules if normal acinar secretion is blocked § Acinar cells are remarkably resistant to the action of activated enzymes such as trypsin, chymotrypsin, and phospholipase A 2.
The Pancreas Diseases of the exocrine pancreas § § § cystic fibrosis congenital anomalies acute pancreatitis chronic pancreatitis neoplasms

CONGENITAL ANOMALIES Agenesis § Very rarely § The pancreas may be totally absent § Usually (but not invariably) associated with additional severe malformations § incompatible with life
CONGENITAL ANOMALIES Pancreas divisum § the most common clinically significant congenital pancreatic anomaly(3% to 10%) § It occurs when the fetal duct systems of the pancreatic primordia fail to fuse § As a result, the main pancreatic duct (Wirsung) is very short and drains only a small portion of the head of the gland § predisposes to chronic pancreatitis
CONGENITAL ANOMALIES Annular pancreas § relatively uncommon variant on pancreatic fusion § the outcome is a ring of pancreatic tissue § completely encircles the duodenum § It can present with signs and symptoms of duodenal obstruction such as gastric distention and vomiting
CONGENITAL ANOMALIES Ectopic Pancreas § about 2% of the population § favored sites are the stomach and duodenum § are typically small § located in the submucosa § composed of normal pancreatic acini with occasional islets § usually incidental and asymptomatic § Approximately 2% of islet cell tumors arise in ectopic pancreatic tissue
CONGENITAL ANOMALIES Congenital cysts § anomalous ductal development § In polycystic disease pancreas can contain cyst § range from microscopic to 5 cm in diameter § lined by duct-type cuboidal epithelium or lack a cell lining § unilocular cysts tend to be benign § multilocular cysts are more often
PANCREATITIS Acute Pancreatitis § reversible lesions § relatively common § Approximately 80% of cases are attributable to either biliary tract disease or alcoholism § 5% of patients with gallstones develop acute pancreatitis § gallstones are implicated in 35% to 60% of cases
Etiologic Factors in Acute Pancreatitis Metabolic § Alcoholism § Hyperlipoproteinemia § Hypercalcemia § Drugs (e. g. , thiazide diuretics) § Genetic Ø Vascular § Shock § Atheroembolism § Polyarteritis nodosa
Etiologic Factors in Acute Pancreatitis Mechanical § Trauma § Gallstones § Iatrogenic injury § Perioperative injury § Endoscopic procedures with dye injection Infectious § Mumps § Coxsackievirus § Mycoplasma pneumoniae Ø 10% to 20% (idiopathic pancreatitis)
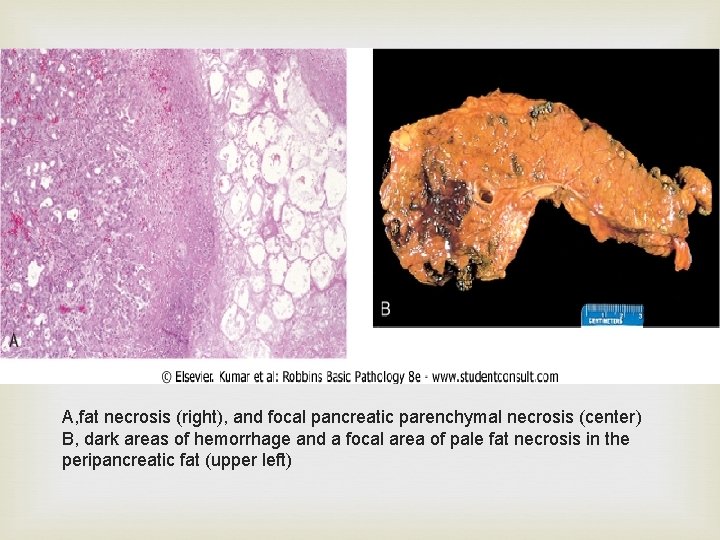
Acute Pancreatitis Morphology § ranges from trivial inflammation and edema to extensive necrosis and hemorrhage The basic alterations (1) microvascular leakage causing edema (2) necrosis of fat by lipases (3) an acute inflammatory reaction (4) proteolytic destruction of pancreatic parenchyma (5) destruction of blood vessels with hemorrhage.
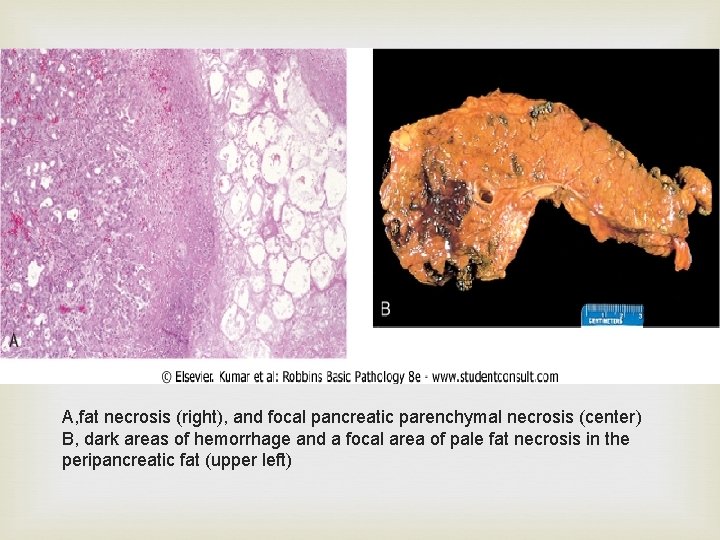
A, fat necrosis (right), and focal pancreatic parenchymal necrosis (center) B, dark areas of hemorrhage and a focal area of pale fat necrosis in the peripancreatic fat (upper left)
Acute Pancreatitis The histologic changes seen in acute pancreatitis strongly suggest autodigestion of the pancreatic substance by inappropriately activated pancreatic enzymes Activation of trypsin is a critical triggering event Can activate other proenzymes (e. g. , phospholipases and elastases) Trypsin also converts prekallikrein to its activated form, Activation of factor XII (Hageman) Sets in motion the clotting and complement
Acute Pancreatitis Three possible pathways can incite the initial enzyme activation § Pancreatic duct obstruction § Primary acinar cell injury § Defective intracellular transport of proenzymes within acinar cells

Pathogenesis
Acute Pancreatitis Clinical Features § Abdominal pain § Its severity varies from mild to severe § "acute abdomen": painful, rigid abdomen and the ominous absence of bowel sounds § the pain is constant and intense and is often referred to the upper back
Acute Pancreatitis Suspected acute pancreatitis is primarily diagnosed by: Ø elevated plasma levels of amylase and lipase Ø exclusion of other causes of abdominal pain: § ruptured acute appendicitis § perforated peptic ulcer § acute cholecystitis with rupture § mesenteric vessels infarction
Acute Pancreatitis severe acute pancreatitis § Increased vascular permeability § Leukocytosis § DIC § Acute respiratory distress syndrome § Diffuse fat necrosis § Peripheral vascular collapse (shock)
Acute Pancreatitis Laboratory findings § markedly elevated serum amylase during the first 24 hours, followed (within 72 -96 hours) by rising serum lipase levels § Hypocalcemia Ø Result from precipitation of calcium in the extensive areas of fat necrosis Ø If persistent, it is a poor prognostic sign
Acute Pancreatitis The management is supportive therapy most individuals eventually recover 5% die from shock ominous complications: § acute respiratory distress syndrome § acute renal failure sequelae include sterile pancreatic abscesses or pancreatic pseudocysts
Acute Pancreatitis Pancreatic Pseudocysts § § A common sequela many pseudocysts spontaneously resolve can become secondarily infected larger pseudocysts can compress or even perforate into adjacent structures
Acute Pancreatitis Morphology § usually solitary § commonly involve peripancreatic tissues such as the lesser omental sac or the retroperitoneum between the stomach and transverse colon or liver § range from 2 to 30 cm § composed of necrotic debris encased by fibrous walls of granulation tissue lacking an epithelial lining

Pancreatic pseudocyst A, a poorly defined cyst with a necrotic brownish wall B, the cyst lacks a true epithelial lining and instead is lined by fibrin, granulation tissue, and chronic inflammation
Chronic Pancreatitis characterized by § § Longstanding inflammation Fibrosis Destruction of the exocrine pancreas In late stages, the endocrine parenchyma is also lost
Chronic Pancreatitis can result from recurrent bouts of acute pancreatitis irreversible impairment in pancreatic function The prevalence between 0. 04% and 5% the most common cause is long-term alcohol abuse middle-aged males constitute the bulk of this group
Chronic Pancreatitis Less common causes § Long-standing pancreatic duct obstruction (e. g. , by pseudocysts, calculi, neoplasms, or pancreas divisum) § Tropical pancreatitis attributed to malnutrition § Hereditary pancreatitis § Idiopathic(40%)
Chronic Pancreatitis Morphology Grossly § the gland is hard § sometimes with extremely dilated ducts § visible calcified concretions
Chronic Pancreatitis Microscopy § parenchymal fibrosis § reduced number and size of acini(constant feature) § dilation of the pancreatic ducts § relative sparing of the islets of Langerhans § chronic inflammatory infiltrate around remaining lobules and ducts § The ductal epithelium may be atrophied, hyperplastic, or exhibit squamous metaplasia
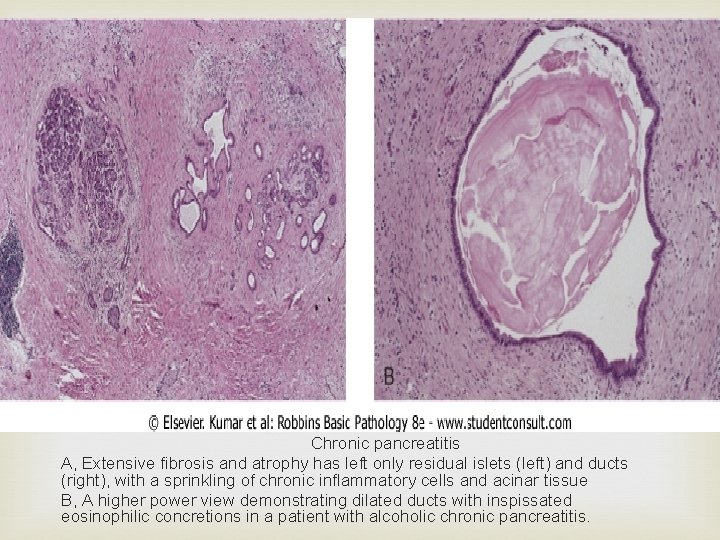
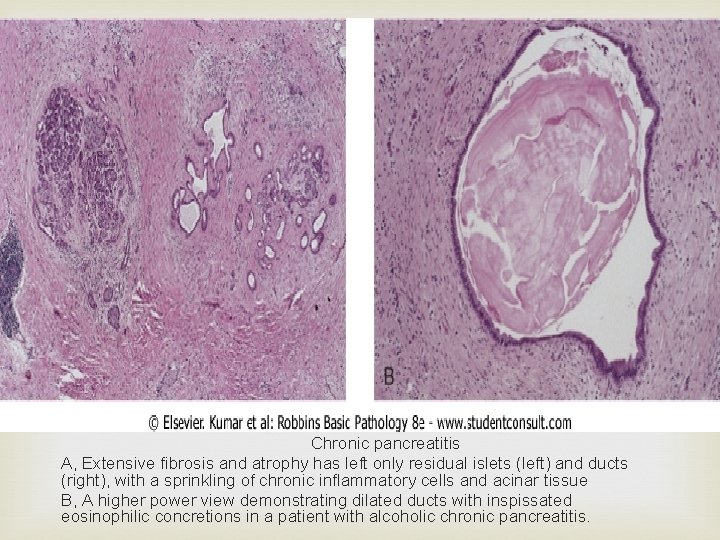
Chronic pancreatitis A, Extensive fibrosis and atrophy has left only residual islets (left) and ducts (right), with a sprinkling of chronic inflammatory cells and acinar tissue B, A higher power view demonstrating dilated ducts with inspissated eosinophilic concretions in a patient with alcoholic chronic pancreatitis.
Chronic Pancreatitis Pathogenesis § Ductal obstruction by concretions § Toxic-metabolic § Alcohol-induced oxidative stress § Necrosis-fibrosis

Chronic Pancreatitis Clinical Features § repeated bouts of jaundice § vague indigestion § persistent or recurrent abdominal and back pain § may be entirely silent until pancreatic insufficiency and diabetes mellitus develop
Chronic Pancreatitis Attacks § alcohol abuse § overeating (increases demand on pancreatic secretions) § opiates § drugs that increase the muscle tone of the sphincter of Oddi
Chronic Pancreatitis Diagnosis § requires a high degree of suspicion § During an attack of abdominal pain, there may be mild fever and modest elevations of serum amylase § Gallstone-induced obstruction may present as jaundice or elevations in serum levels of alkaline phosphatase § A very helpful finding: calcifications within the pancreas by CT or ultrasonography § Weight loss and hypoalbuminemic edema from
Chronic Pancreatitis the long-term outlook is poor 50% mortality rate over 20 to 25 years Severe pancreatic exocrine insufficiency and chronic malabsorption may develop, as can diabetes mellitus Pancreatic pseudocysts develop in about 10% Individuals with hereditary pancreatitis have a 40% lifetime risk of developing pancreatic cancer
PANCREATIC NEOPLASMS Cystic Neoplasms § 5% to 15% of all pancreatic cysts are neoplastic § Less than 5% of all pancreatic neoplasms § Some are entirely benign (e. g. , serous cystadenoma) § Mucinous cystic neoplasms have malignant potential
PANCREATIC NEOPLASMS Serous Cystadenomas § A quarter of all pancreatic cystic neoplasms § Composed of glycogen-rich cuboidal cells surrounding small cysts containing clear, strawcolored fluid § Typically present in the seventh decade of life § Present with nonspecific symptoms such as abdominal pain § Female-to-male ratio is 2 : 1 § Almost uniformly benign § Surgical resection is curative

Serous cystadenoma A, Cross-section through a serous cystadenoma. Only a thin rim of normal pancreatic parenchyma remains. The cysts are relatively small and contain clear, straw-colored fluid B, The cysts are lined by cuboidal epithelium without atypia

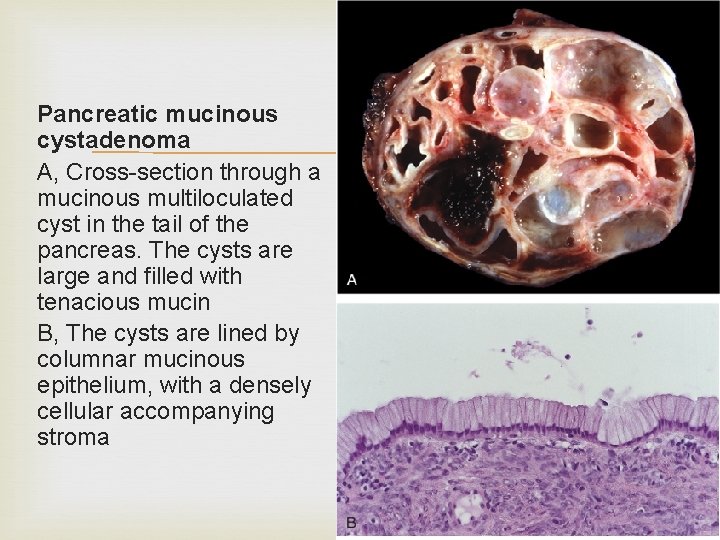
PANCREATIC NEOPLASMS Mucinous Cystic Neoplasms § almost always arise in women § usually in the body or tail of the pancreas § present as painless, slow-growing masses § The cystic spaces are filled with thick, tenacious mucin, and the cysts are lined by a columnar mucinous epithelium with an associated densely cellular stroma § These tumors can be benign, borderline malignant, or malignant
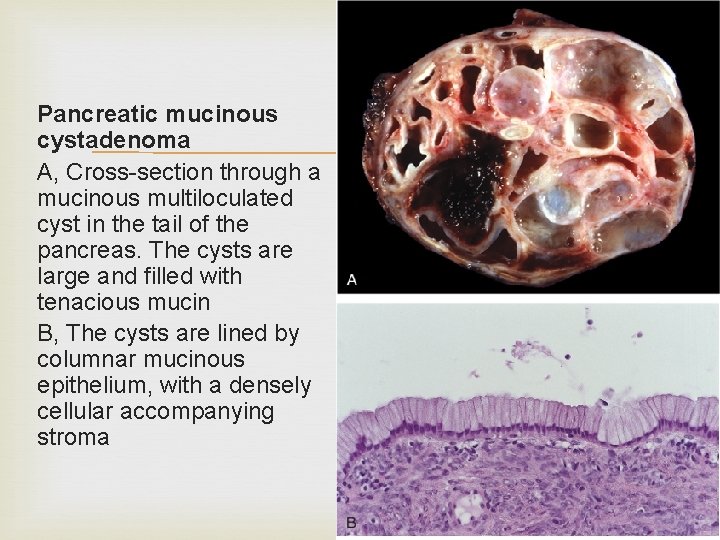
Pancreatic mucinous cystadenoma A, Cross-section through a mucinous multiloculated cyst in the tail of the pancreas. The cysts are large and filled with tenacious mucin B, The cysts are lined by columnar mucinous epithelium, with a densely cellular accompanying stroma

PANCREATIC NEOPLASMS Intraductal papillary mucinous neoplasms (IPMNs) § produce cysts containing mucin § can be benign, borderline malignant, or malignant § In contrast to mucinous cystic neoplasms, IPMNs arise more frequently in men and more frequently involve the head of the pancreas § IPMNs arise in the main pancreatic ducts and lack the cellular stroma seen in mucinous cystic neoplasms

Intraductal papillary mucinous neoplasm A, Cross-section through the head of the pancreas showing a prominent papillary neoplasm distending the main pancreatic duct B, The papillary mucinous neoplasm involved the main pancreatic duct (left) and is extending down into the smaller ducts and ductules (right).
PANCREATIC NEOPLASMS Pancreatic carcinoma § the fourth leading cause of cancer death in the United States, preceded only by lung, colon, and breast cancers § the highest mortality rates § the 5 -year survival rate is dismal-less than 5%
PANCREATIC NEOPLASMS Pathogenesis § consequence of inherited and acquired mutations in cancer-associated genes § there is a progressive accumulation of genetic changes in pancreatic epithelium § it proceeds from non-neoplastic, to noninvasive lesions in small ducts and ductules, to invasive carcinoma
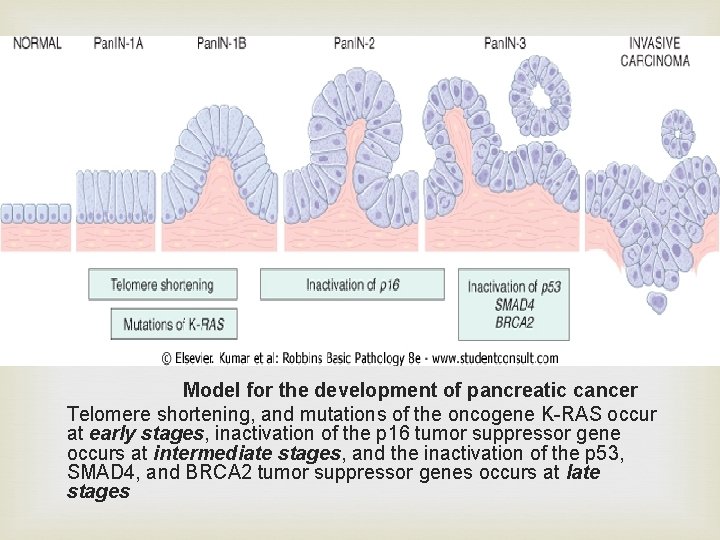
PANCREATIC NEOPLASMS Antecedent lesions are called "pancreatic intraepithelial neoplasias" (Pan. INs) they are often found adjacent to infiltrating carcinomas and share a number of the same genetic mutations the epithelial cells in Pan. INs show dramatic telomere shortening, potentially predisposing these lesions to accumulating additional chromosomal abnormalities The more common molecular alterations in pancreatic carcinogenesis affect K-RAS, p 16, SMAD 4, and p 53
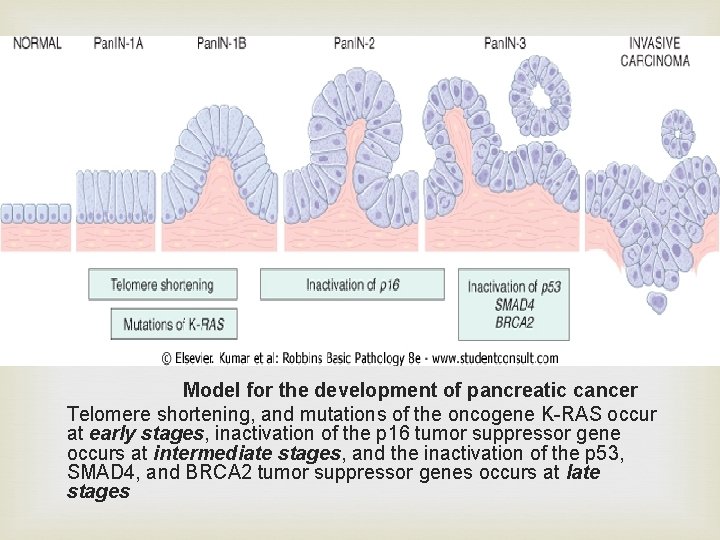
Model for the development of pancreatic cancer Telomere shortening, and mutations of the oncogene K-RAS occur at early stages, inactivation of the p 16 tumor suppressor gene occurs at intermediate stages, and the inactivation of the p 53, SMAD 4, and BRCA 2 tumor suppressor genes occurs at late stages
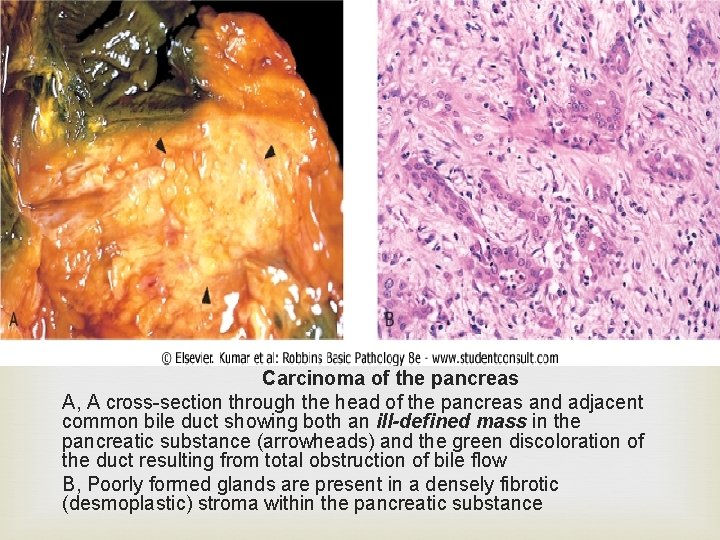
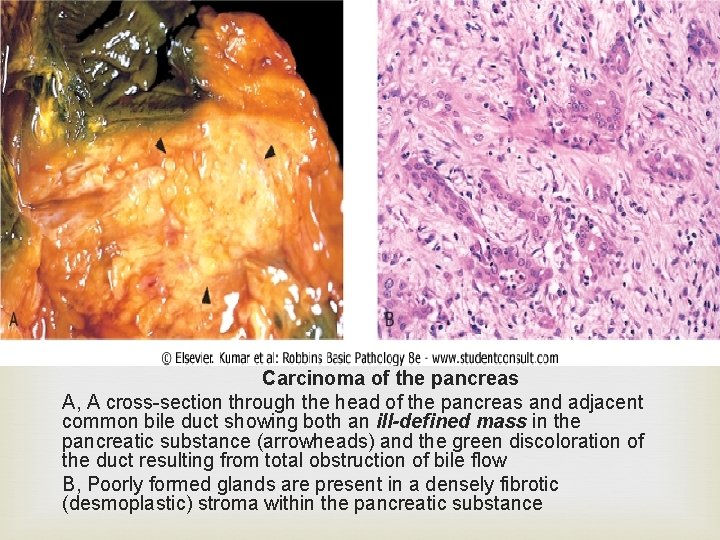
Carcinoma of the pancreas A, A cross-section through the head of the pancreas and adjacent common bile duct showing both an ill-defined mass in the pancreatic substance (arrowheads) and the green discoloration of the duct resulting from total obstruction of bile flow B, Poorly formed glands are present in a densely fibrotic (desmoplastic) stroma within the pancreatic substance
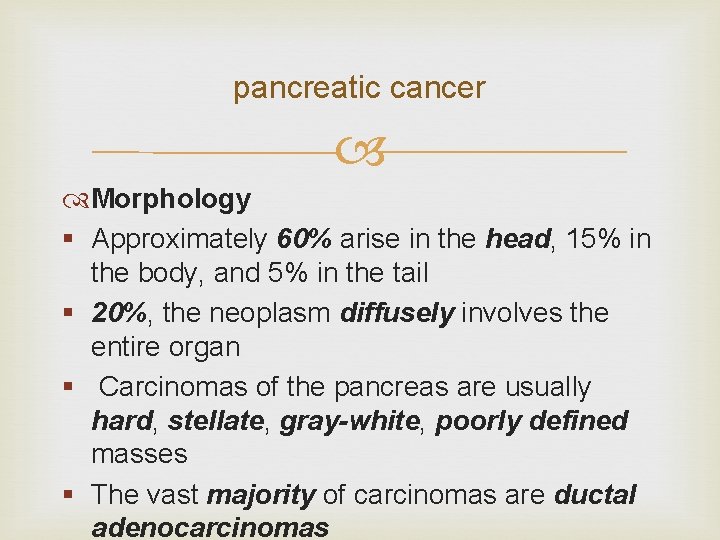
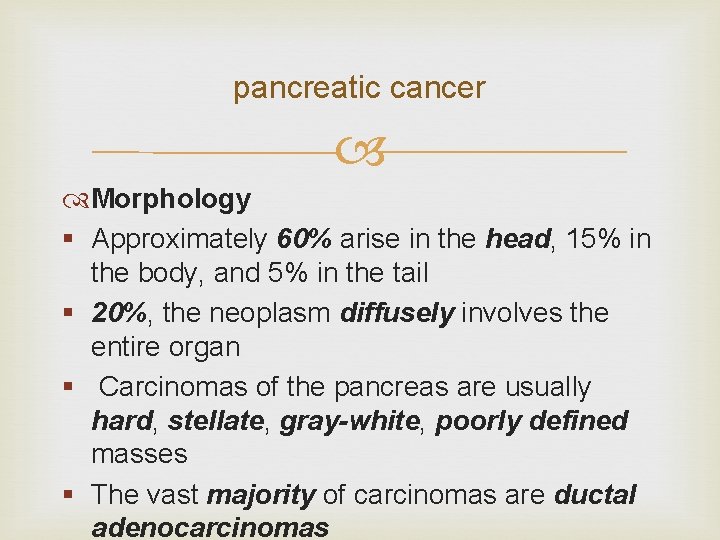
pancreatic cancer Morphology § Approximately 60% arise in the head, 15% in the body, and 5% in the tail § 20%, the neoplasm diffusely involves the entire organ § Carcinomas of the pancreas are usually hard, stellate, gray-white, poorly defined masses § The vast majority of carcinomas are ductal adenocarcinomas
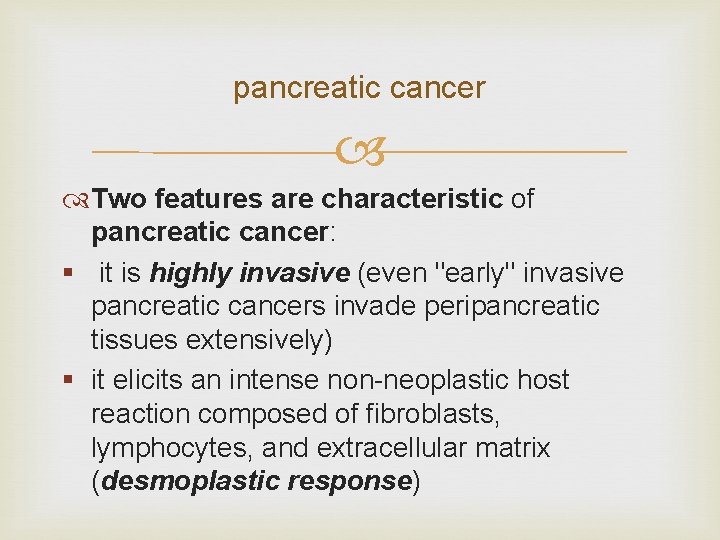
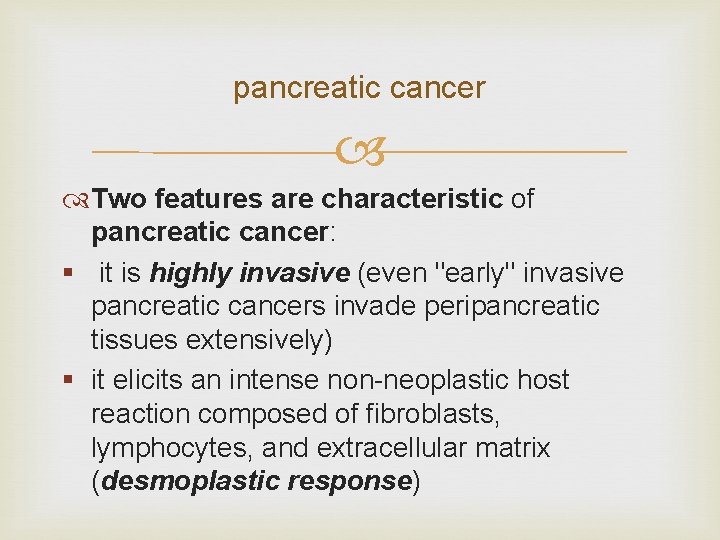
pancreatic cancer Two features are characteristic of pancreatic cancer: § it is highly invasive (even "early" invasive pancreatic cancers invade peripancreatic tissues extensively) § it elicits an intense non-neoplastic host reaction composed of fibroblasts, lymphocytes, and extracellular matrix (desmoplastic response)
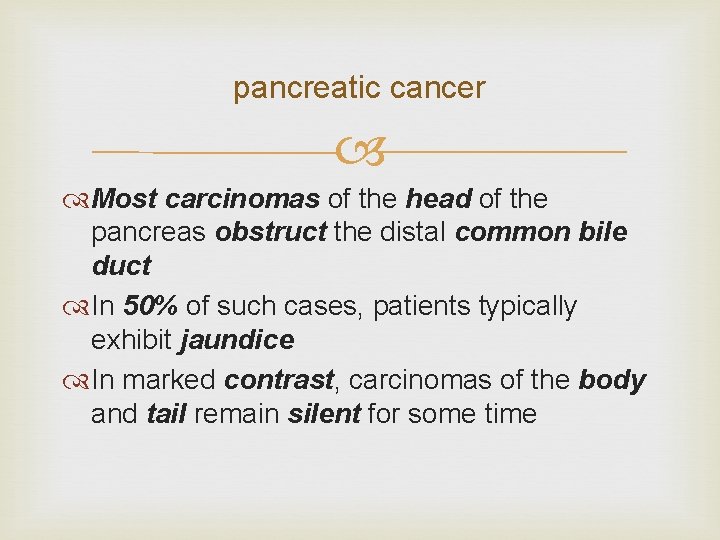
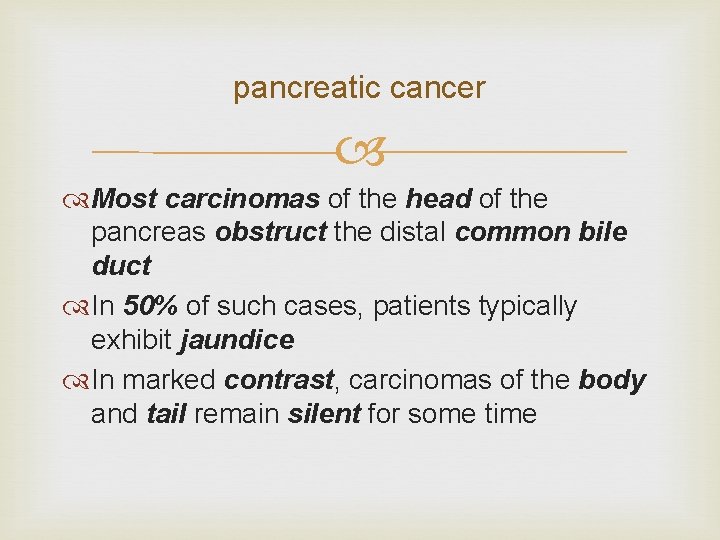
pancreatic cancer Most carcinomas of the head of the pancreas obstruct the distal common bile duct In 50% of such cases, patients typically exhibit jaundice In marked contrast, carcinomas of the body and tail remain silent for some time
pancreatic cancer often extend through the retroperitoneal space entrapping adjacent nerves occasionally invade the spleen, adrenals, vertebral column, transverse colon, and stomach
pancreatic cancer Peripancreatic, gastric, mesenteric, omental, and portahepatic lymph nodes are frequently involved liver is often enlarged because of metastatic deposits Distant metastases occur, principally to the lungs and bones

pancreatic cancer Microscopy Usually a moderately to poorly differentiated adenocarcinoma Forming abortive tubular structures or cell clusters Exhibiting an aggressive, deeply infiltrative growth pattern Dense stromal fibrosis Proclivity for perineural invasion Lymphatic invasion is commonly seen
pancreatic cancer Less common variants § Acinar cell carcinomas showing prominent acinar cell differentiation § Adenosquamous carcinomas with focal squamous differentiation § Undifferentiated carcinomas with osteoclast -like giant cells
pancreatic cancer Clinical Features § Carcinomas of the pancreas typically remain silent § Pain is usually the first symptom § Obstructive jaundice can be associated with carcinoma in the head of the pancreas § Weight loss, anorexia, and generalized malaise and weakness are signs of advanced disease
pancreatic cancer Migratory thrombophlebitis (Trousseau syndrome) § about 10% of patients § is attributable to the elaboration of plateletaggregating factors and procoagulants from the tumor or its necrotic products
pancreatic cancer The symptomatic course of pancreatic carcinoma is distressingly brief and progressive Fewer than 20% of pancreatic cancers are resectable at the time of diagnosis serum levels of many enzymes and antigens (e. g. , carcinoembryonic and CA 19 -9 antigens) are elevated, but these markers are neither specific nor sensitive imaging techniques, are helpful in diagnosis but are not useful as screening tests

 Allahumma inni as'aluka birahmatika
Allahumma inni as'aluka birahmatika Shinta rahmani
Shinta rahmani Tawbah dua
Tawbah dua Shinta rahmani
Shinta rahmani Allahumma rahmani birahmatika
Allahumma rahmani birahmatika Asad rahmani
Asad rahmani Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Hổ sinh sản vào mùa nào
Hổ sinh sản vào mùa nào Diễn thế sinh thái là
Diễn thế sinh thái là Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau 101012 bằng
101012 bằng Tư thế worm breton
Tư thế worm breton Lời thề hippocrates
Lời thề hippocrates đại từ thay thế
đại từ thay thế Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Công của trọng lực
Công của trọng lực Bổ thể
Bổ thể Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập Dạng đột biến một nhiễm là
Dạng đột biến một nhiễm là Biện pháp chống mỏi cơ
Biện pháp chống mỏi cơ Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Phản ứng thế ankan
Phản ứng thế ankan Hát lên người ơi
Hát lên người ơi Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan điện thế nghỉ
điện thế nghỉ Một số thể thơ truyền thống
Một số thể thơ truyền thống Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Số nguyên tố là số gì
Số nguyên tố là số gì đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Fecboak
Fecboak Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Sơ đồ cơ thể người
Sơ đồ cơ thể người Môn thể thao bắt đầu bằng từ đua
Môn thể thao bắt đầu bằng từ đua Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể ưu thế lai là gì
ưu thế lai là gì Tư thế ngồi viết
Tư thế ngồi viết Cái miệng xinh xinh thế chỉ nói điều hay thôi
Cái miệng xinh xinh thế chỉ nói điều hay thôi Cách giải mật thư tọa độ
Cách giải mật thư tọa độ Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Tư thế ngồi viết
Tư thế ngồi viết Giọng cùng tên là
Giọng cùng tên là Thẻ vin
Thẻ vin Thể thơ truyền thống
Thể thơ truyền thống Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Pancreas blood supply
Pancreas blood supply Cadaver stomach labeled
Cadaver stomach labeled ¿qué es la homeostasis y ejemplos
¿qué es la homeostasis y ejemplos Pancreas exocrino y endocrino
Pancreas exocrino y endocrino Irrigacion del pancreas
Irrigacion del pancreas Role du pancreas
Role du pancreas Pancreas canino anatomia
Pancreas canino anatomia Pancreas anatomy histology
Pancreas anatomy histology Liver lobules
Liver lobules Digestion in pancreas
Digestion in pancreas Vascolarizzazione pancreas
Vascolarizzazione pancreas Neutraliza
Neutraliza Vascolarizzazione pancreas
Vascolarizzazione pancreas Pancreas wiki
Pancreas wiki Cistoadenoma mucinoso pancreas
Cistoadenoma mucinoso pancreas Disacharides
Disacharides Pancreas produces insulin
Pancreas produces insulin