The Oregon Health Insurance Experiment Evidence from the










- Slides: 31
The Oregon Health Insurance Experiment: Evidence from the First Year Amy Finkelstein, MIT and NBER Sarah Taubman, NBER Bill Wright, CORE Jonathan Gruber, MIT and NBER Mira Bernstein, NBER Joseph Newhouse, Harvard and NBER Heidi Allen, CORE Katherine Baicker, Harvard and NBER And the Oregon Health Study Group: Matt Carlson (Portland State University), Tina Edlund (Oregon Health Authority), Charles Gallia (Oregon DHS), Eric Schneider (RAND), and Jeanene Smith (Office for Oregon Health Policy and Research) 1
Collaborative Effort n Oregon – crucial partners q OHPR, DMAP, OHREC, OHA. . . n Providence CORE n Boston/Cambridge q Harvard, MIT, NBER n Expert consultants n Generous funders (NIA, RWJ, Sloan, Mac. Arthur, CHCF, SRF, SSA, ASPE, . . . ) 2
Question n What are the effects of expanding access to public health insurance for low income adults? q n Magnitudes (and even signs) uncertain Limited existing evidence q IOM review of evidence – suggestive, but much uncertainty n n q Observational studies confounded by selection into HI Quasi-experimental work often focuses on elderly and kids Only one RCT in a developed country: Rand HIE n n 1970 s experiment on a general population Randomized cost-sharing, not coverage itself 3
The Oregon Health Insurance n. Experiment Setting q q q n OHP Standard: Oregon’s Medicaid expansion program for poor adults Opened waiting list for limited number of new slots in 2008 Randomly selected names from waiting list – about 30, 000 out of 90, 000 selected to get 10, 000 new enrollees Study design q q q Evaluate effects of public HI on utilization, health, other outcomes using lottery as RCT Massive data collection effort Answers specific to context, but some broader lessons 4
Examine Broad Range of Outcomes n Costs: Health care utilization q q q n Benefits I: Financial risk exposure q q n Insurance increases resources (income) and lowers price, increasing utilization But improved efficiency (and improved health), decreasing utilization (“offset”) Additional uncertainty when comparing Medicaid to no insurance Insurance supposed to smooth consumption But for very low income, is most care de jure or de facto free? Benefits II: Health q Expected to improve (via increased quantity / quality of care) 5

Data n Pre-randomization demographic information q n State administrative records on Medicaid enrollment q n From lottery sign-up Primary measure of first stage (insurance coverage) Outcomes q Administrative data n n q Mail surveys n n q Hospital discharge data, mortality, credit reports ~16 months after notification, 14 after coverage ~15 months post-notification, 13 post-coverage Some questions ask 6 -month look-back, some current In-person survey and measurements – on the way 6
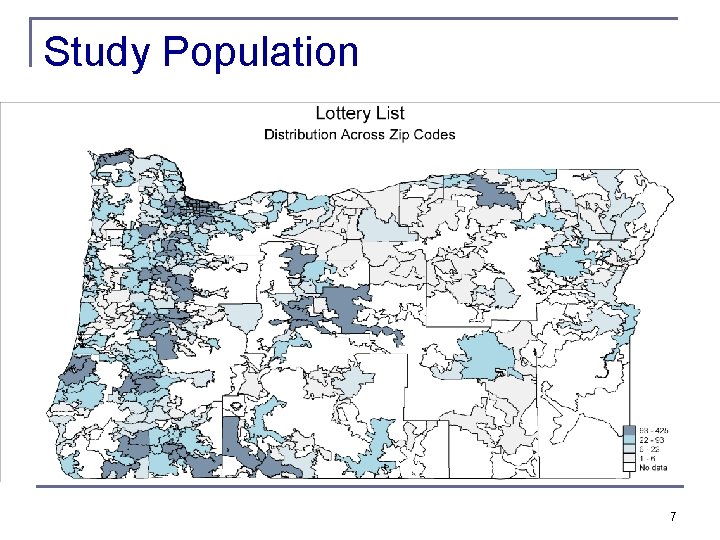
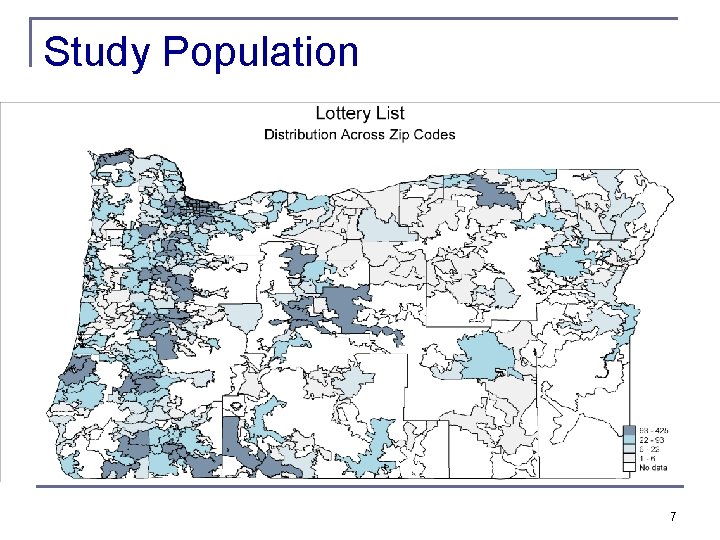
Study Population 7

Sample Characteristics 8
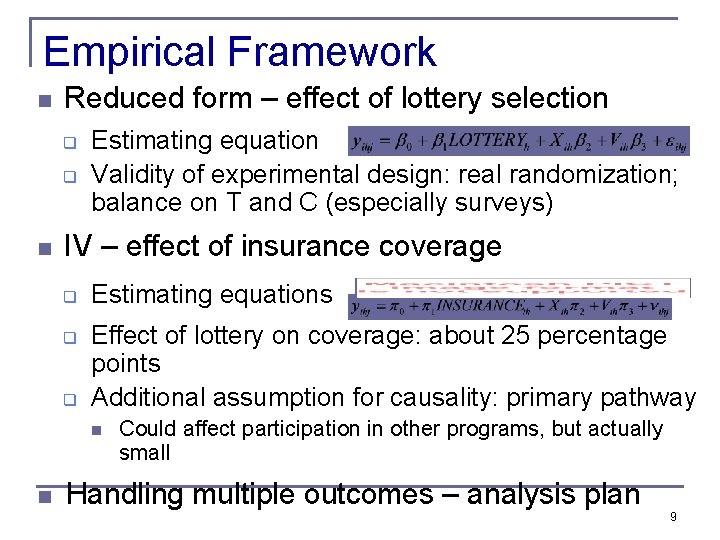
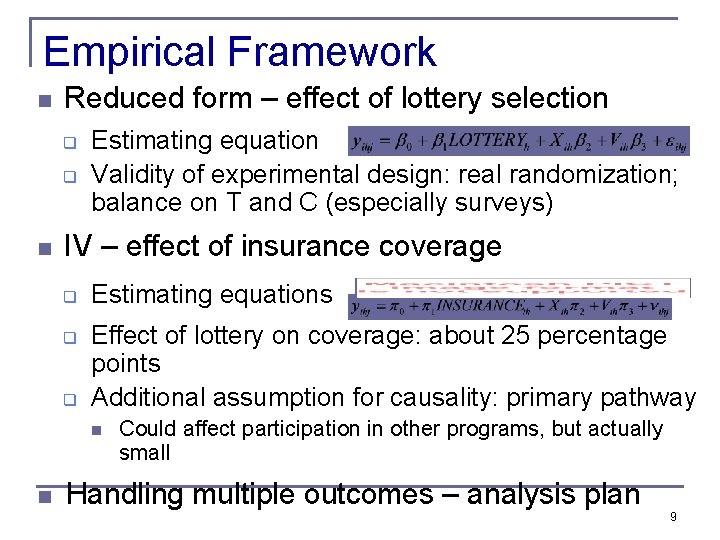
Empirical Framework n Reduced form – effect of lottery selection q q n Estimating equation Validity of experimental design: real randomization; balance on T and C (especially surveys) IV – effect of insurance coverage q q q Estimating equations Effect of lottery on coverage: about 25 percentage points Additional assumption for causality: primary pathway n n Could affect participation in other programs, but actually small Handling multiple outcomes – analysis plan 9
Results n Health care use q q n Financial strain q q n Hospital discharge data Surveys Credit reports Surveys Health q q Mortality from vital stats Surveys 10
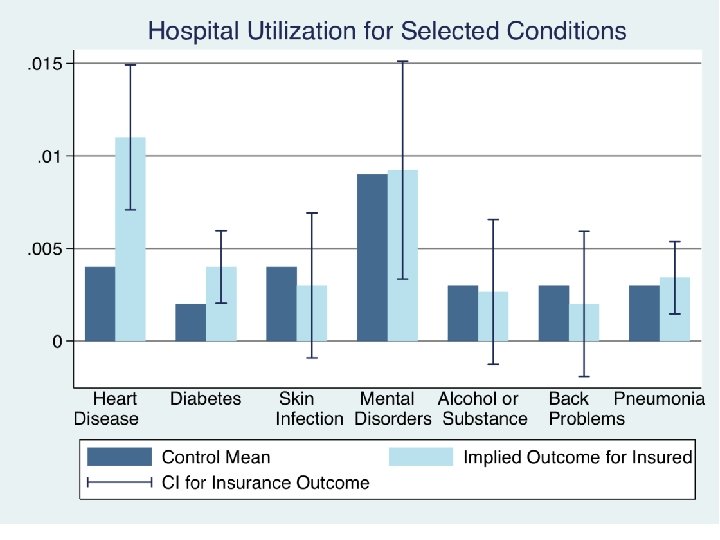
Utilization Results n Hospitalizations (discharge data) q q n Other use (self-reports) q q n 30%↑probability of hospital admission – concentrated in non-ERorigin Substantial (but imprecise) increase in total resource use By condition: increase in heart disease use (not shown) No change in mix of private/public use; no power to detect change in quality of hospitals used 35% ↑ probability of outpatient visit 15% ↑ probability of taking prescription drugs 0. 3 standard dev ↑ in compliance with recommended preventive care No discernable change in ER use (imprecise) Implied $777 increase in spending for insured q 25% increase 11
Financial Strain Results n Reduction in collections (credit reports) q q q n Limitations: time lags, extreme events, lack of data on informal channels (more heavily used by poor) Reduction in strain, OOP, money owed (selfreports) q q n 25% ↓ probability of unpaid medical bills sent to collection No observed effects on other measures Substantial reduction across measures Captures additional channels Implications for distribution of burden/benefits q Some borne by patients, some by providers (or those to whom passed through) – only 2% of bills sent to 12 collection ever paid
Health Results n Large improvements in self-reported physical and mental health q q Mental health indices correlate well with clinical diagnoses Physical health measures open to several interpretations n n Improvements consistent with increased utilization Also see reports of improved quality and access q n But these results appear shortly after insurance coverage q q n Usual place of care; reported quality of care ~2/3 magnitude, in advance of changes in utilization Although lottery selection “glow” may be stronger earlier Suggestive of increase in perceived overall well- 13

Health Results n If only we had objective physical measures! q q Physical measures collected at ~2 years can help shed light Even then, many improvements in health hard to measure objectively n e. g. pain – a real burden for this population 14
Discussion n n OR collaboration created unique research opportunity One year after expanded access to insurance, we find: q q q n Increases in hospital, outpatient, Rx use; compliance with recommended preventive care; improvements in access/quality Reductions in OOP costs, financial strain, medical collections Improvements in self-reported physical and mental health Broader policy lessons q Population very similar to PPACA target population 15

Always an Adventure
Additional Slides 17

Study Population 18

Alternate Channels? Food Stamps 19

Probability of Hospitalization 20
Total Hospital Utilization 21
Health Care Use (Survey) 22

Preventive Care (Survey) 23
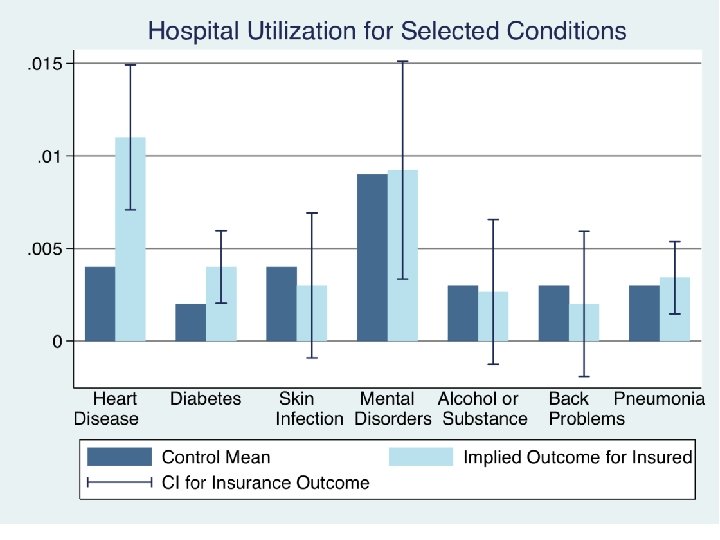
Total Use By Condition 24
Financial Strain (Credit Reports) 25

Types of Collections (Credit Reports) 26
Financial Strain (Surveys) 27
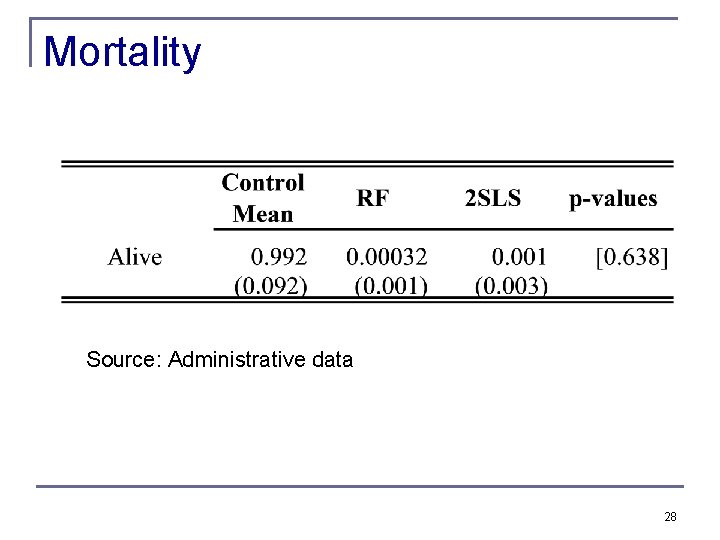
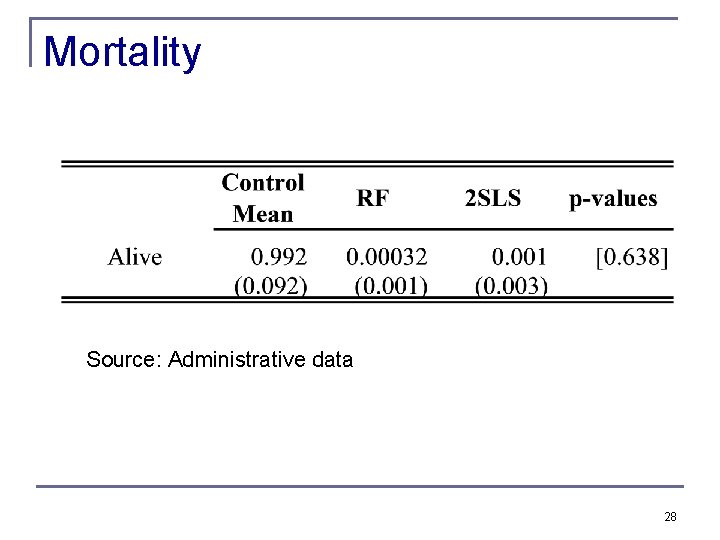
Mortality Source: Administrative data 28
Health Effects (Survey) 29
Access and Quality 30

Timing of Effects 31